
Evaluation of Dosimetric Properties in Full Field Digital
Mammography (FFDM)
Development of a New Dose Index
Chiara Sottocornola
1,2,5
, Antonio Traino
2
, Patrizio Barca
1,5
, Giacomo Aringhieri
1,4
, Carolina Marini
3
,
Alessandra Retico
5
, Davide Caramella
4
and Maria Evelina Fantacci
1,5
1
Dipartimento di Fisica “E. Fermi”, Università di Pisa, L.go B. Pontecorvo 3, 56127 Pisa, Italy
2
U. O. Fisica Sanitaria, Azienda Ospedaliero-Universitaria Pisana, via Roma 67, 56122 Pisa, Italy
3
S. D. Radiologia Senologica, Azienda Ospedaliero-Universitaria Pisana, via Roma 67,56122 Pisa, Italy
4
Dipartimento di Ricerca Traslazionale e delle Nuove Tecnologie in Medicina e Chirurgia, via Savi 10, 56126 Pisa, Italy
5
Istituto Nazionale di Fisica Nucleare (INFN), Sezione di Pisa, Italy
Keywords: Mammography, Dose-Index in Mammography, Average Glandular Dose, Breast Absorbed Dose, Dosimetry
in Mammography.
Abstract: According to the World Health Organization (WHO), breast cancer is the most common cancer in women,
constituting 29% of all cancers related to the female population. In this context, Full Field Digital Mammog-
raphy (FFDM) is the reference imaging technique for breast cancer early detection and diagnosis and it is
widely employed in screening programs. Therefore, the absorbed radiation dose for each examination shall
be evaluated in order to ensure proper radiation exposures for the patient. In addition, the new European
Directive 59/2013/EURATOM requires that dosimetric data referred to the radiation exposure should be in-
serted in the radiological report. For these reasons, we designed a multidisciplinary research project with the
intention of realizing and validating a new method for calculating the Average Absorbed Breast Dose (2ABD)
by the patient during a mammography procedure. The innovative aspect regards the availability of a quanti-
tative and personalized dosimetric parameter, providing an index that is patient-specific rather than related to
the X-ray machine output, directly related to the risk of radiation. Specifically, in this work we present our
scientific approach as well as the initial results.
1 INTRODUCTION
Breast cancer is the most common cancer among
women both in developed and developing countries
and it is also the principal cause of death from cancer
among women (De Santis et al., 2014; Ferlay et al.,
2010). It affects 1 in 8 women in their lifetime, and
represents 29% of all cancers related to the female
population. Based on these data it is of fundamental
importance to both do an early diagnosis and submit
the patients suffering from this pathology to periodic
checks, in order to offer appropriate treatments with
the goal of reducing mortality.
FFDM (Full Field Digital Mammography) is a
non-invasive high sensitive method for early stage
breast cancer detection and diagnosis, and represents
the reference imaging technique to explore the breast
in a complete way (Dance et al., 2014). Hence,
mortality from breast cancer can be reduced by
mammographic screening (Myers et al., 2015).
However, in a mammographic screening program
healthy people are exposed to ionising radiation.
Besides, the breast is a significant radiosensitive
organ, so special care is required in the evaluation of
the patient exposure (EUREF 2006). Additionally, the
new European Directive 59/2013/EURATOM
highlights the importance of controlling the doses
delivered during radiological procedures and requires
that a dosimetric data referred to exposure should be
inserted in the radiological report
(59/2013/EURATOM). The weight factor for breast
tissue increased from 0.05 to 0.12 in the new
directive, following the ICRP recommendations.
212
Sottocornola, C., Traino, A., Barca, P., Aringhieri, G., Marini, C., Retico, A., Caramella, D. and Fantacci, M.
Evaluation of Dosimetric Proper ties in Full Field Digital Mammography (FFDM) - Development of a New Dose Index.
DOI: 10.5220/0006644302120217
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 1: BIODEVICES, pages 212-217
ISBN: 978-989-758-277-6
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

In order to satisfy these necessities, this
experimental work was accomplished with the
ambition of identifying a quantitative and
personalized dosimetric index to evaluate the
radiation dose absorbed by each patient during a
mammographic procedurebased on dosimetric
measurements and mathematical calculations.
The current dosimetric index employed in
estimating the radiation dose in mammography is the
Average Glandular Dose (AGD) that is representative
of the dose absorbed by glandular tissue. The most
common algorithms for the AGD evaluation in
mammography are based on the works of Dance
(Dance et al., 1990) and of Wu (Wu et al., 1994). Both
methods are based on incident air kerma (k
a,i
)
measurements and the AGD is obtained through an
empirical expression by applying tabulated factors
(Dance et al., 1990; Wu et al., 1994). The only
measurable quantity in the AGD computation is k
a,i
,
which is an X-ray output related quantity rather than
a patient dose related quantity.
Thus, we propose the Average Absorbed Breast
Dose (2ABD), defined as the mean value of the
energy imparted per unit of mass in a considered
volume of interest, which could represent a more
suitable physical quantity to evaluate patient
exposure in a mammographic procedure.
In this paper, we present the 2ABD method, show
the preliminary results obtained and discuss its
potential impact on radiological workflow, further
development of the whole project and other possible
applications of the same method.
2 MATERIALS AND METHODS
The absorbed dose in mammography depends mainly
on the quality of the beam and the breast thickness.
Following the mathematical definition, the 2ABD
(mGy) for a specific total breast thickness t (cm) can
be expressed as:
(1)
where μ
en
is the energy absorption coefficient(cm
-1
)
and k
a,i
is the incident air kerma at the breast surface
(mGy).
While the tube voltage (kVp), mAs, anode-filter
combination and t are supplied by the mammographic
device, k
a,i
and μ
en
have to be assessed in order to
compute the 2ABD. It is important to notice that μ
en
depends on kVp and anode-filter combination, while
k
a,i
depends on kVp, tube current-exposure time
product (mAs), anode-filter combination and focus-
to-breast surface distance. Therefore, an experimental
evaluation of these dependences is required to ensure
a reliable assessment of the 2ABD value.
In this first stage we employed a square water-
equivalent phantom (1 g/cm
3
) for breast tissue
simulation. The phantom is composed of a set of
slabs, which allow selecting a specific thickness.
A solid-state detector coupled to a Piranha
multimeter (RTI-Electronics AB
®
) and calibrated
termo-luminescent (TL) dosimeters have been
employed in our measurements. The measurements
were performed on the GE Senographe DS machine
(GE Healthcare, Waukesha, WI, USA).
The first step of our work was the beam
characterization in order to evaluate k
a,i
as a function
of kVp, mAs, t and Focus-to-Image Distance (FID).
We set a wide range of nominal kVp (24-34) and mAs
(10-100) values and we measured k
a,i
, kVp and mAs
by placing the solid-state detector 6 cm from the chest
wall edge in the centre of the flat support plate (t=0)
with the compression paddle between X-ray tube
focus and the detector. We chose the Rh-Rh anode-
filter combination for all measurements.
We found the following relationship between k
a,i
and the other parameters:
(2)
where the terms a and b were estimated fitting our
experimental data. The dependence of the k
a,i
on kVp
is linear as a first approximation and this relationship
is valid only in the considered energy range. Repeated
measurements of k
a,i
varying the kVp value were
performed keeping fixed the value of mAs. Each
measurement of k
a,i
was repeated five times and the
average value was considered. The parameters a and
b were obtained by fitting the experimental
measurements to Eq. 2.
The second step was to determine the energy
absorption coefficient μ
en
. A set of experimental
measurements was performed varying the kVp (range
22-34) and setting 40 mAs for the Rh-Rh anode-filter
combination. The TL dosimeters were placed
between the phantom slabs at specific depths to
evaluate the absorbed dose for different phantom
thicknesses (Fig. 1).
In order to estimate μ
en
for each kVp value, the
data were fitted according to the exponential
attenuation law:
(3)
in which D(t) represents the absorbed dose measured
by TL dosimeters at depth t. Repeated measurements
Evaluation of Dosimetric Properties in Full Field Digital Mammography (FFDM) - Development of a New Dose Index
213

varying the kVp value were performed in order to
evaluate a possible dependence of the energy
absorption coefficient μ
en
from kVp.
Figure 1: Experimental setup of water equivalent phantoms
and TLDs: four different dosimeters were placed each time
at the centre of the area irradiated by the beam. At each ir-
radiation the thickness over the TLDs was increased, up to
the maximum thickness of 5.5 cm.
Once k
a,i
and μ
en
were derived as functions of the
input parameters described above, we computed the
2ABD values in different clinical conditions and we
compared them to the AGD values computed (for the
Rh-Rh anode-filter combination) through the Dance
and Wu methods. Uncertainties in AGD (using Dance
and Wu methods) were estimated considering an
overall 20% error (Hauge et al., 2013). The
uncertainty in 2ABD was estimated considering the
error propagation on a, b, kVp, t, FID and μ
en
. The
comparison between AGD and 2ABD took into
account the overlap between data within their
uncertainties.
3 RESULTS
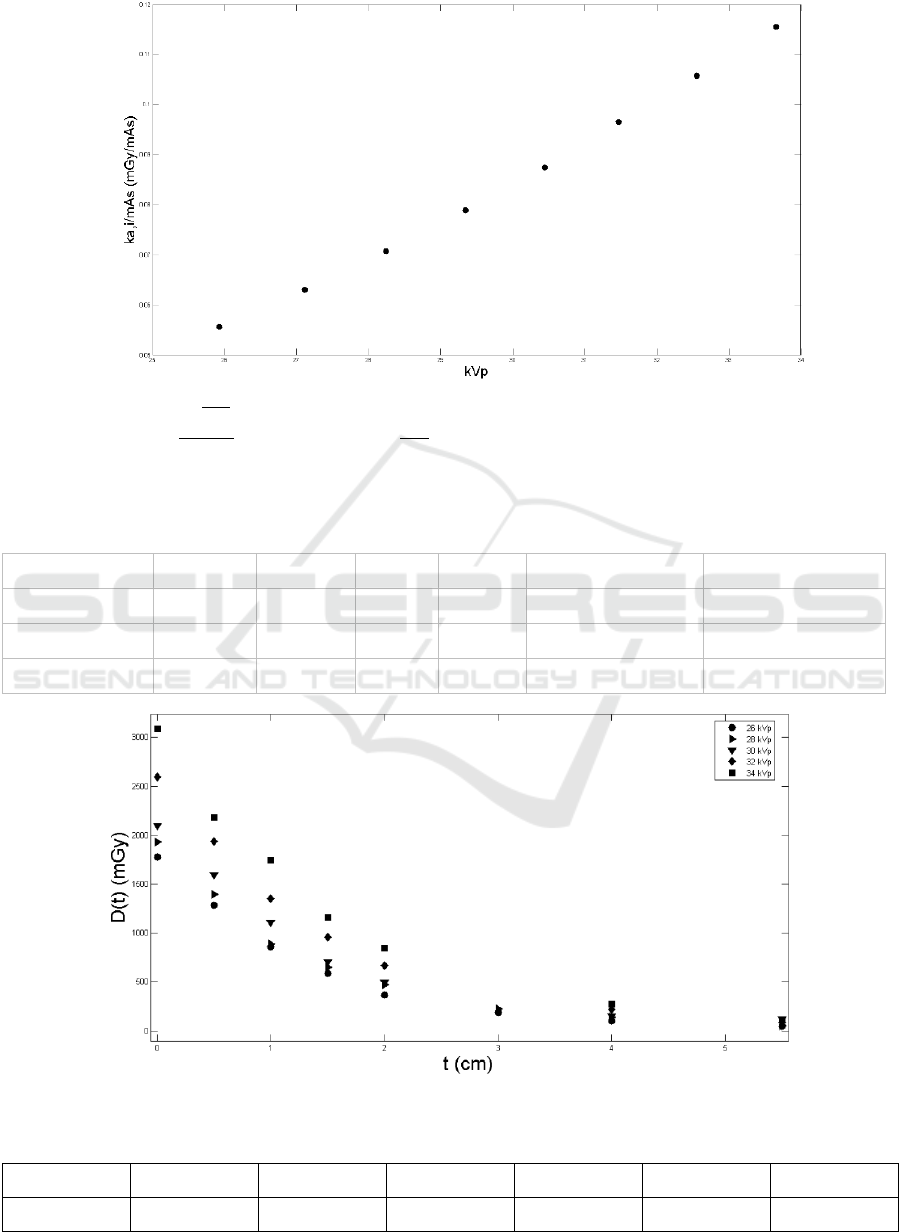
In Fig. 2 we show the X-ray tube yield (i.e. k
a,i
/mAs)
as a function of kVp for the Rh-Rh anode-filter
combination (Eq. (2)). As we said previously, the tube
yield is approximately linear with respect to kVp in
the energy range of interest. The repeatability of the
kerma measurements (based on five repeated
measurements for each value of kVp) is < 2%
(standard deviation). a and b values allow to estimate
the incident air kerma k
a,i
for any breast thickness t,
mAs and kVp values (Eq. 2).
In Table 1 we compare k
a,i
measured values and
k
a,i
computed values. The good agreement between
the measured and calculated values allows the
evaluation of k
a,i
by Eq. 2 for each mammographic
equipment. Notice that the determination of a and b
permits to obtain k
a,i
without directly measure it.
In Fig. 3 we show D(t) as a function of depth t for
different kVp values. Data were fitted with Eq. (3)
and the μ
en
for each kVp was obtained. The
experimental data confirm the exponential trend of
the beam intensity as a function of the phantom
thickness.
Numerical results are presented in Table 2. The
energy absorption coefficients μ
en
vary slightly with
kVp. For this reason, the average value was
considered, as shown in Table 2
1
.
Once evaluated a and b values and the energy
absorption coefficient μ
en
the 2ABD can be calculated
according to Eq. 1.
In Table 3 we compare the 2ABD and AGD values
in clinical situations. Five mammograms were
selected from the PACS (Picture Archiving and
Communication System) and the data needed to
compute the AGD through the Dance and Wu
methods were extracted. The most used kVp values
were chosen for each anode/filter combination. For
each kVp value the most frequent thickness was
considered. From Tab. 3 we observe a good
agreement between 2ABD and AGD in every
considered conditions. The two methods provide
results that are consistent within the uncertainties.
4 DISCUSSION
The 2ABD, defined as the mean value of energy
imparted per unit mass in a considered volume of
interest, represents a suitable physical quantity to
evaluate the patient exposure in a mammography
procedure. In fact, we notice a good agreement
between the 2ABD values and the AGD values
computed through the Dance (Dance et al., 1990) and
Wu (Wu et al., 1994) methods for the clinical
situations considered in this work (Table 3).
Our method requires kVp, mAs and breast
thickness values as input parameters, for a specific
anode-filter combination. These parameters can be
1
The difference between 2ABD computed by considering the kVp
dependence of μ
en
and the 2ABD computed considering the
average value of μ
en
was negligible.
BIODEVICES 2018 - 11th International Conference on Biomedical Electronics and Devices
214
easily obtained or selected by the operator before the mammographic exam. Therefore, the 2ABD index
Figure 2: X-ray tube yield (
) as a function of kVp for the Rh-Rh anode-filter combination. Data were fitted using Eq.(2)
with a=(0.0078±0.0002)
and b=(-0.149±0.006)
. Five measurements were averaged and the standard deviation
was computed in order to evaluate the precision of our experimental data.
Table 1: Comparison between k
a,i
(mGy) measured and calculated for different experimental settings. Five measurements
were averaged and the standard deviation was computed in order to evaluate the precision of our experimental data.
Anode-filter
FID (cm)
t (cm)
kVp
mAs
k
a,i
calculated
k
a,i
measured
Rh-Rh
63.5
5
29
50
4.65 ± 0.6
4.80 ± 0.01
Rh-Rh
63.5
3
27
40
2.67 ± 0.4
2.83 ± 0.01
Rh-Rh
63.5
4
28
45
3.57 ± 0.5
3.70 ± 0.01
Figure 3: Absorbed radiation dose at different depths in the water-equivalent phantom for different kVp values.
Table 2: μ
en
values for different kVp and average value of μ
en
for the Rh-Rh anode-filter combination.
kVp
26
28
30
32
34
μ
en_avg
(cm
-1
)
μ
en
(cm
-1
)
0.74±0.05
0.72±0.05
0.69±0.09
0.66±0.04
0.63±0.06
0.69±0.06
Evaluation of Dosimetric Properties in Full Field Digital Mammography (FFDM) - Development of a New Dose Index
215

Table 3: Comparison between 2ABD and AGD values in different clinical situations.
Age (y)
Glandularity (%)
t (cm)
kVp
mAs
AGD (Dance)(mGy)
AGD (Wu) (mGy)
2ABD (mGy)
63
33
5
28
48
1.0±0.2
1.0±0.2
1.1±0.2
59
33
5
29
58
1.4±0.3
1.4±0.3
1.4±0.3
45
35
6
29
73
1.5±0.3
1.5±0.3
1.6±0.3
57
21
6
30
63
1.5±0.3
1.6±0.3
1.5±0.3
60
12
7
30
75
1.7±0.3
1.7±0.3
1.6±0.3
could be easily computed and employed as dosimetric
index for each mammographic procedure (i.e. for
each patient) and recorded in the radiological report.
In addition, the computation could be conveniently
automated and this could be advantageous in order to
comply with the European Directive
59/2013/EURATOM. Notice that k
a,i
can be
computed directly from Eq. 2 once kVp, mAs, FID
and t are known and therefore, to assess 2ABD, a
direct measurement of k
a,i
can be
avoided.Furthermore, Table 3 does not show evident
discrepancy between AGD and 2ABD values,
although a different set of radiation exposure and
patient-specific parameters was involved in each
mammographic procedure. Thus, 2ABD could be
employed as surrogate of AGD.
However, our model has some limitations. In fact,
this model could be improved taking into account the
X-ray tube yield variations for different anode-filter
combinations among different mammographic
devices, which can affect the k
a,i
evaluation.
Moreover, breast composition should be considered
and a correction factor might be applied for the μ
en
assessment. In addition, different phantoms with
different shapes could be used so as to better simulate
the breast. Besides, in order to comprehensively
validate this model, the method should be tested in
different clinical conditions on different
mammographic devices. Moreover, breast
composition should be considered and a correction
factor might be applied for the μ
en
assessment. Breast
density is being studied in many epidemiological
works also related to screening programs (Freer 2015,
Berg 2016). We are also realizing image processing
software able to automatically analyse clinical images
to evaluate the breast composition, based on both a
classical approach (comprising a pre-processing step,
a pattern recognition step, a classification step and a
segmentation step) and novel approaches based on
machine learning methods.
As a further development, this method could be
also applied to the tomosynthesis, an advanced
imaging technique that allows the reconstruction of a
three-dimensional view of the breast, overcoming the
projective (two-dimensional) imaging approach
limitations.
5 CONCLUSIONS
In conclusion, in this work we proposed the 2ABD as
a reproducible and easily computable dose index to
assess the radiation dose absorbed by the patient
during a mammography procedure. According to our
preliminary results, the 2ABD could be employed as
dosimetric index to be inserted into the radiological
report as required by the European Directive
59/2013/EURATOM. The development of this new
dose index is a part of a whole project finalized to
optimize the dose in mammographic procedures, give
a correct information about the risk related to ionizing
radiation and maintain high adherence to screening
programs.
REFERENCES
DeSantis, C., Ma, J., Bryan, L., Jemal, A., 2014. Breast can-
cer statistics, 2013. CA Cancer J Clin. Jan-Feb;
64(1):52-62.
Ferlay, J., Héry, C., Autier, P., Sankaranarayanan, R.,2010.
Global Burden of Breast Cancer. Breast Cancer Epide-
miology; 1:1-19.
Dance, D., R., Christodes, S., Maindment, A., D., A.,
McLean, I., D., Ng, K., H., 2014. Diagnostic Radiology
Physics. A Handbook for Teachers and Students. IAEA
International Atomic Energy Agency.
Myers, E., R., Moorman, P., Gierisch, J., M., Havrilesky.,
L., J., Grimm, L., J., Ghate, S., Davidson, B.,
Mongtomery, R., C., Crowley, M., J., McCrory, D., C.,
Kendrick, A., Sanders, G., D., 2015.Benefits and Harms
of Breast Cancer Screening: A Systematic Review.
JAMA Oct 20;314(15):1615-34.
European guidelines for quality assurance in breast cancer
screening and diagnosis 4rd edition, EUREF 2006.
BIODEVICES 2018 - 11th International Conference on Biomedical Electronics and Devices
216

Council Directive 59/2013/EURATOM of 5 December
2013 laying down basic safety standards for protection
against the dangers arising from exposure to ionising
radiation. Official Journal of the European Union L 13,
Volume 57, 17 January 2014.
Dance, D. R., 1990. Monte Carlo calculation of conversion
factors for the estimation of mean glandular breast dose.
Phys Med Biol; 35:1211-1219.
Wu, X., Gingold, E., L., Barnes, G., T., Tucker, D., M.,
1994. Normalized average glandular dose in molyb-
denum target-rhodium filter and rhodium target-rho-
dium filter mammography. Radiology; 193: 83-89.
Freer, P. E., 2015. Mammographic Breast Density: Impact
on Breast Cancer Risk and Implications for Screening.
Radiographics; 35(2):302-315.
Berg W. A, 2016. Breast Density and Choosing Optimal
Breast Screening. HealthManagement; 16(3).
Hauge I. H. R., Olerud H. M., 2013. Uncertainties involved
in the estimation of mean glandular dose for women in
the Norwegian Breast Cancer Screening Program
(NBCSP). Radiat Prot Dosimetry 155:81 –87.
Evaluation of Dosimetric Properties in Full Field Digital Mammography (FFDM) - Development of a New Dose Index
217
