
Improving Nurse Managers’ Competencies: A Systematic Review
Priscylia Maria Sandehang
1
and Muthmainnah
2
1
Fakultas Ilmu Keperawatan, Universitas Pelita Harapan, Karawaci, Tangerang, Indonesia
2
Universitas Andalas, Kampus Limau Manis, Padang, Sumatera Barat, Indonesia
Keywords: Competence, Healthcare Service, Nursing Care, Nurse Manager, Nurses’ Role, Review Literature.
Abstract: Nurse managers’ competencies greatly influence the quality of services and nursing care. Consequently, the
aim of this study is to identify and to define the competencies of nurses working in management roles in the
healthcare system so they can undertake their roles effectively. This research used a systematic literature
review design and analysed 40 articles. Twenty-five studies were from Europe and 15 from outside Europe.
The literature was limited to articles published in English between November 2003 and 2018 that were
searched using these keywords: nurse manager, competence, nurses, career plan, improving, assessment
tools, clinical competence, professional competence. In this study, six dimensions of nursing managers’
competencies emerged: sociodemographics, technical, networking, administrative, staff development, and
legal and ethical. This literature review provided scientific evidence for decision makers to consider the
implementation of a nurse manager competency system, including leadership development, the redesigning
of managers’ role, building networks, clinical skills and climbing the career ladder. Future studies are
suggested to investigate the usefulness of the competency model for assessing nursing managers’ readiness
to between job applicants, implement continuing education programmes for nurse managers, and develop
and plan their careers.
1 INTRODUCTION
Competence is a critical attribute for safe, ethical,
high-quality care (Kendall, Gallagher & Blegen,
2009). It is essential to one’s contribution in
ensuring healthcare delivery (Flinkman & Salanterä
2015). Competence development has been described
as a process that occurs over time (Benner, 2001;
Keane, Lincoln, & Smith, 2012). Hence, the process
of forming competence, especially for nurses, is not
done briefly. There is a sustainable process through
education, clinical experience and self-capacity
building to reach comprehensive competence.
Nowadays, globalisation and science-tech
developments are causing huge changes in the
world. Nursing services is an integrative part which
is not separate from these changing needs. Thus, this
field must undergo improvement and innovation so
it does not get left behind. Based on that perspective,
nursing organisations must change and review their
management models to improve the quality of their
service.
The nurse manager has played an important role
in health services, especially in the hospital sphere,
since this professional is responsible for managing
nursing services and for taking measures that include
administration, the delivery of care and teaching–
research. The work requirements of nurse managers
include nursing management, knowledge and
interaction with the entire organisational
environment to contribute to an institution’s success
(Furukawa & Cunha 2011).
Generally, the ability of leaders in health services
consists of communication, creating a vision,
managing, managing strategies and motivating
others, engaging in openness and being
approachable, making decisions and becoming role
models, knowing their roles, becoming experts and
solving problems. However, the definition of
competencies has become complex, and there is no
consensus among scholars on nurse manager
competencies (Kantanen, Kaunonen, Helminen, &
Suominen, 2015; Pihlainen, 2016). Moreover, there
are various models of nurse manager competency –
and in several countries, the nurse manager is not
even legally recognised.
Thus, it has become a challenge for nurses and
academicians working in nursing to think seriously
Sandehang, P. and Muthmainnah, .
Improving Nurse Managers’ Competencies: A Systematic Review.
DOI: 10.5220/0008201300570066
In Proceedings of the 1st International Conference of Indonesian National Nurses Association (ICINNA 2018), pages 57-66
ISBN: 978-989-758-406-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
57

about and formulate the vital aspects of nurse
managers’ competency. Chase (1994, 2010)
developed a Nurse Manager Competencies Model
that classifies nurse manager competencies into five
main categories: human resource skills, technical
skills, leadership skills, financial management
conceptual skills. The key competencies synthesised
by Pihlainen, Kivinen and Lammintakanen (2015)
from Chase (2010) found the highest self-reported
nurse manager competency ratings included human
resource management and leadership. The lowest
self-reported nurse manager competencies involved
conceptual skills and knowledge. Perhaps critical
thinking and problem analysis are not yet entrenched
in the nursing profession.
Although there were various literature about
nursing competencies, but there were still lack of
finding about main dimension of nurse manager in
all healtcare setting. This, coupled with a lack of
motivation to learn and understand caring concepts,
are essential issues for the identity of the nurse
manager competencies Furthermore, the existing
studies of nurse manager competencies have
analysed only the proficiency level in competencies
of nurse managers working in hospitals and
neglected the question of why nurse managers differ
from each other regarding their management
capacity. So this study aims to close this research
gap by syntesized the main competencies of nurse
manager.
2 METHOD
A systematic literature review was conducted for
five months. The researchers used the systematic
review for identifying studies to describe diverse
types of nurse manager competencies in a clinical
setting during a certain time period. This paper
focuses on a competence-based approach for leaders
and managers, instead of merely the profession-
centred view of point, even though the profession-
centred approach dominates previous studies.
Searches have probed systematic reviews
published in the journal. A review of literature
published over the past 15 years uses databases:
PubMed, CINAHL, PsycINFO, Scopus, Proquest
and EBSCO. The search period spanned 2003 and
2018 because there are dramatically increasing of
the amount of the literature regarding the
competence-based approach to management and
leadership during this period.
The literature was searched using these
keywords: nurse manager, competence, nurses,
career plan, improving, assessment tools, clinical
competence, professional competence. These words
were searched for in combination and individually.
The inclusion criteria for the articles were as
follows: (1) full paper was publication in English;
(2) focus on a nurse manager; (3) focus on a
competence and its predictors or determinants, both
in all research methods of literature reviews; and (4)
a full-text paper. The criteria for excluding articles
were as follows: (1) the study was not published as a
full paper, (2) lack of reliable or valid testing and (3)
publication more than 15 years according the
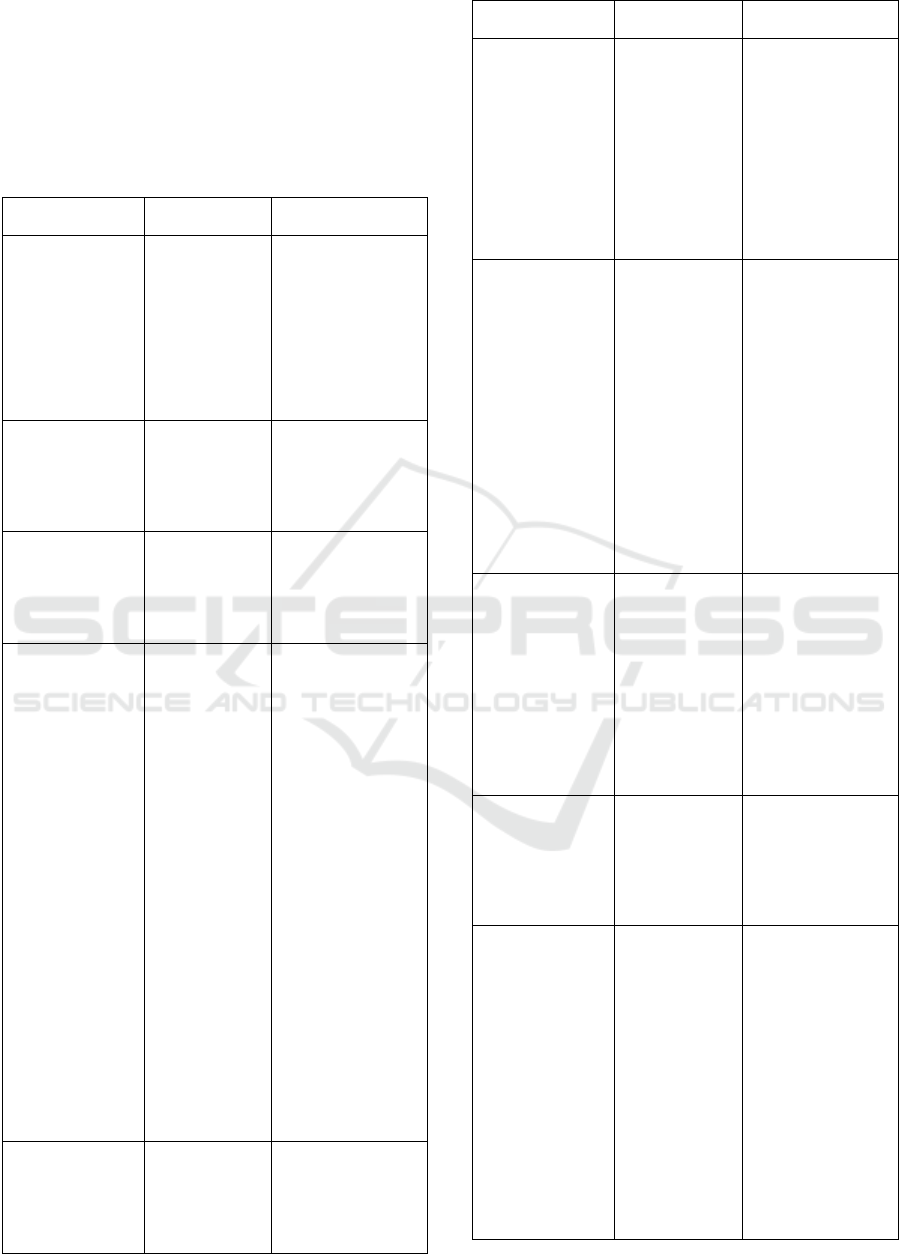
COSMIN checklist (see figure 1). After evaluating
studies with relevant titles and abstracts, the
researchers identified 40 relevant articles targeting
competence and nurse managers. The metodological
quality of each study were review. Both of authors
(PMS, M) directly filters the titles, abstracts and
complete and relevant articles. Then, the researchers
independently review each 20 articles and consensus
was reached through discussion.
3 RESULT
3.1 Study Characteristics
The systematic review involved 40 studies, which
were mainly quantitative and conducted in
municipal care, hospitals and all healthcare settings.
All level of competence were analysed in all studies.
Figure 1 explains the steps according to which
databases were searched.
Figure 1: Diagram of database search.
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
58

3.2 Study Findings
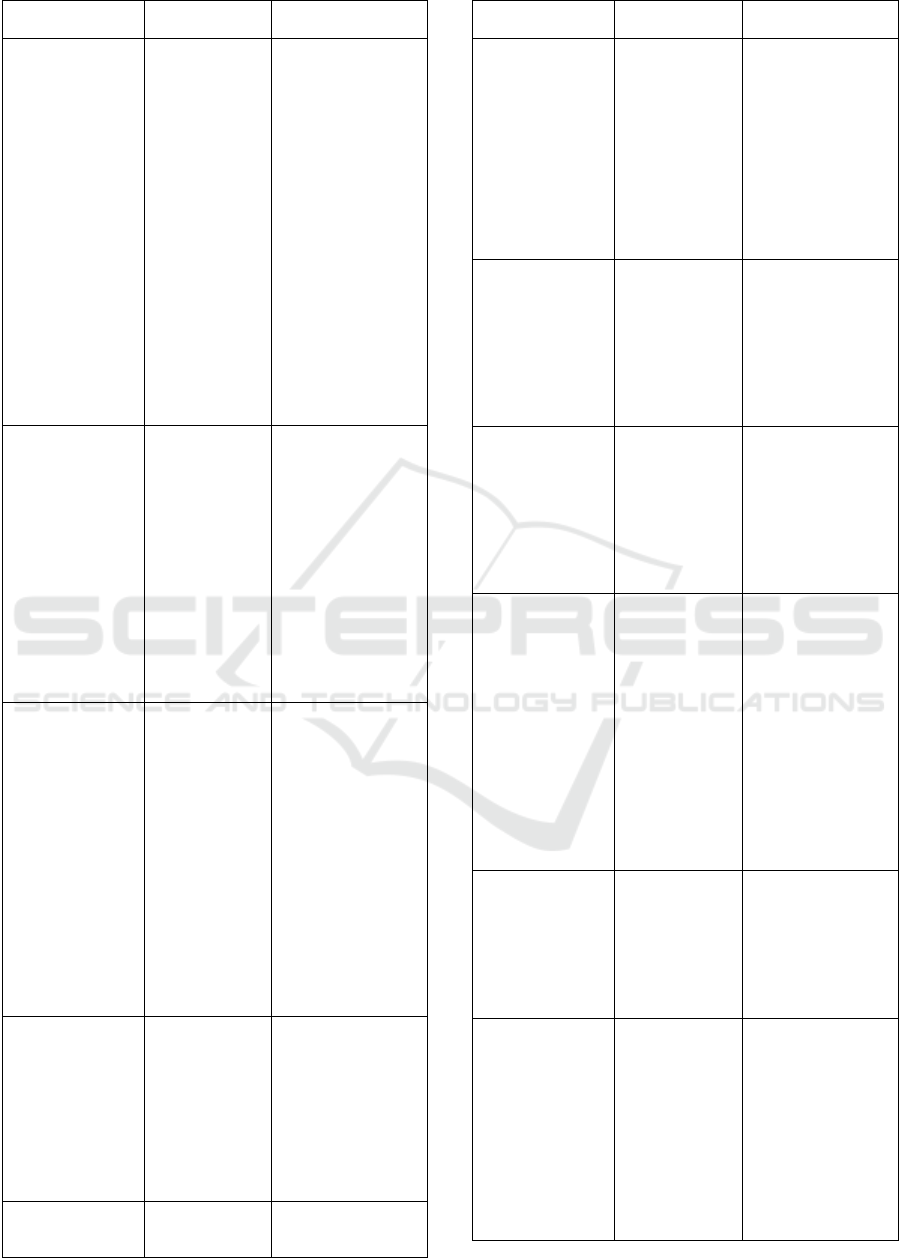
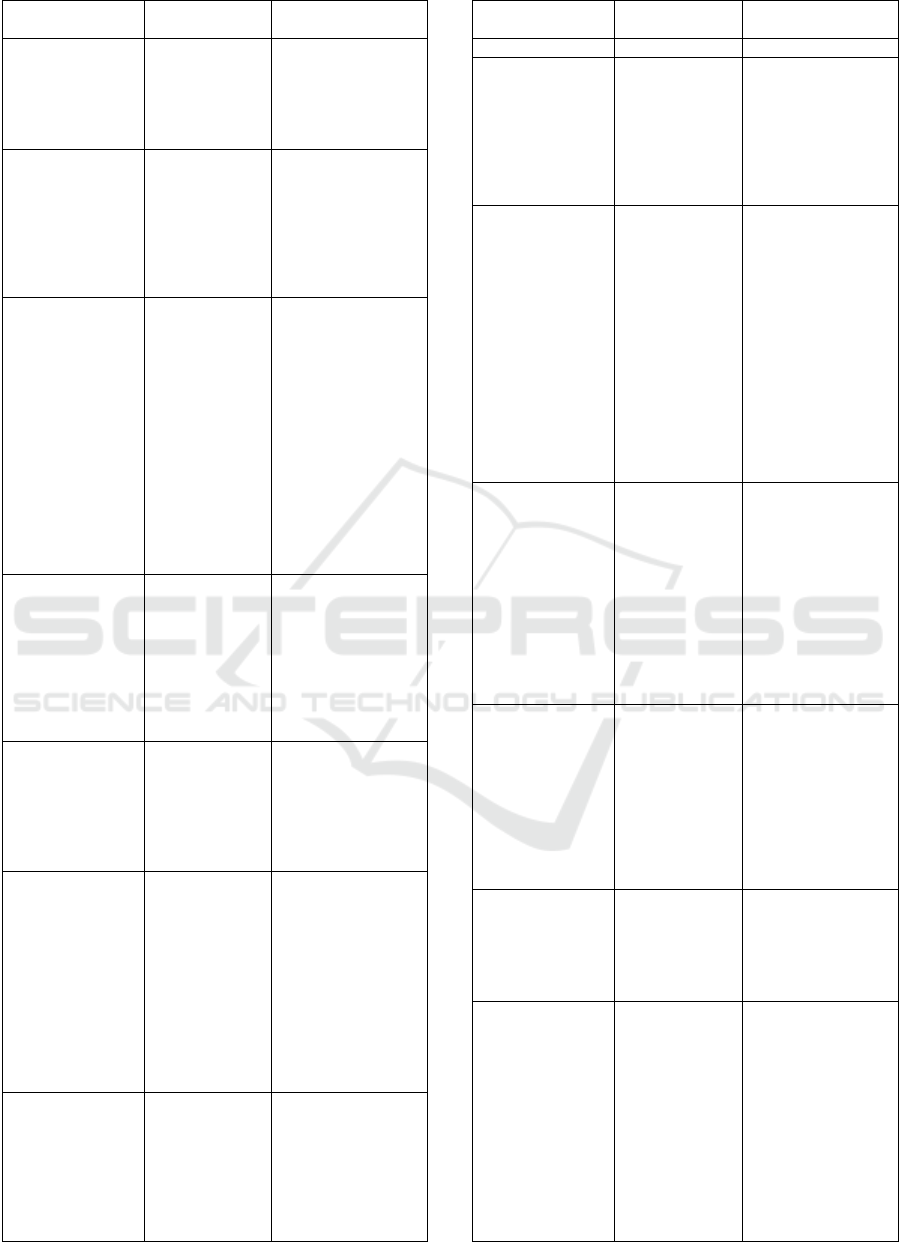
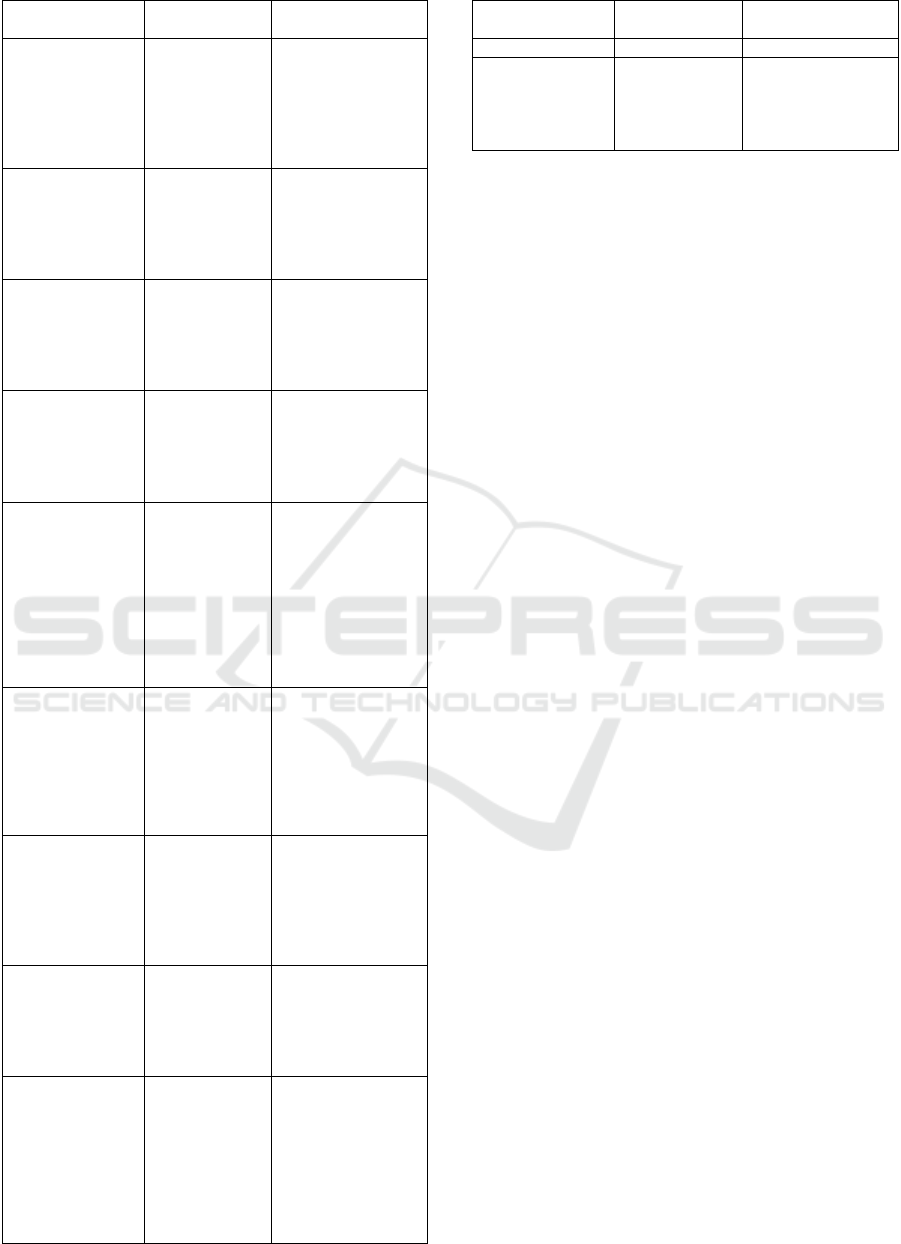
The findings of this study are summarised in Table 1
in the Table 1 appendix that was extracted from 40
publication printed from 2003 from 2018. In this
study, six dimensions of nursing manager
competencies emerged: sociodemographics,
technical, networking, administrative, developing
staff and legal ethics. Each dimension consisted of a
nursing manager’s explanation of a role concerning
related sections.
Sociodemographics. The aspect of
sociodemographics aligned with nurse manager
competence consists of several aspect such as: age,
higher education, the duration of one’s work
experience, employment status and participation in
educational programmes.
Technical. The dimension concerning technical skill
includes the planning and delivery of care,
therapeutic intervention, ensuring the quality of
nursing care, modifying care plans according to
individual needs, integration of nursing sciences, IT
development and current nursing or healthcare
research, and developing effective communication.
Networking. Nurse managers must have networking
skills, such as building and managing relationships,
interprofessional collaboration, involving
stakeholders and community.
Administrative. The next most important
competence of nursing managers is administrative
skill, which includes the ability to manage financial
aspects of the job, allocating and using resources
effectively, ensuring cost-effective services and
controlling documentation.
Developing staff. The nurse manager must support
and develop the nursing staff, providing supervision
and coaching for staff, inspiring and motivating,
team building and teamwork, knowing employees’
needs, empowering staff, managing conflict,
providing fair rewards and punishments for staff and
arranging the Contionuing Professional
Development (CPD) for nursing staff.
Legal and ethical. The nurse manager must display
competence with laws and ethics to protect nursing
services and nursing staff and to safely serve
patients. The ability to display legal and ethical
competence, such as in decision making, is guided
by ethical values, ensuring patient and staff rights,
understanding the legal aspect of nursing services,
maintaining a nursing code of ethics and staying
current with nursing and healthcare policies.
4 DISCUSSION
Competence is determined by one’s qualifications,
education, skilfulness and experience. In addition, it
is judged by a group of people, including colleagues
who are specialists or competent in certain practices
(Jennings, Mutsch & Schleman 2009). This process
includes the determination of clinical competence,
whereby nurses are considered competent (Petri &
Govern, 2013). Competence is the ability to work
properly, so that it is known as the main component
of professional standards. Competence is considered
the biggest contributor to differentiating managerial
effectiveness as seen from expertise, habits and
attitudes (McCarthy & Fitzpatrick 2009).
In addition, the competency of nurse managers
must be assessed continuously to ensure safe within
the scope of the competent delivery of nursing care.
Robust and reliable assessment methods are
important for assessment to be more objective.
Assessment tools represent a particular
conceptualisation of competence, both in the nature
and range of competences presented and the
language used for assessment (Watson et al. 2002).
Competency-based career mapping supports health
workers’ collaborations that can increase patients’
safety, ease access and coordinate effective health
services, optimise the health of health service
providers, share knowledge and skills, as well as
escalate roles and communications (Burton 2015).
Three central ideas demonstrate the reasons for
differences among nurse managers according to
nurse manager competencies: job security, degree of
autonomy and executive power in different
healthcare organisations (Erjavec & Starc 2017).
Competencies are interconnected with education and
formal and informal training. Nurses’ competencies
merit a clear understanding based on the stages.
Additionally, higher education is conducted to
improve the profession and ensure quality nursing
cares.
Human Resources management executes
recruitment and maintains the retention of skilful
employees so hospitals can provide quality services
(Porkodi & Haque 2012). Organisations can reach
competitive superiority through their talented, skilful
and experienced staff. One way to ensure nurses are
working at their maximum performance in working
is through the career stages (Shammot 2014).
The sociodemographic dimension, which
consists of variables such as older age, higher
education and permanent employment were
associated with higher competence for a nurse
manager (Flinkman et al. 2016; Wangensteen et al.
Improving Nurse Managers’ Competencies: A Systematic Review
59

2015; Numminen et al. 2017). It is conceivable that
a nurse manager who adapts maturely in various
situations can think critically, a skill inculcated by
education level, and is aware of the need to keep
improving their ability and be loyal to the
organisation. In addition, there is a correlation
between higher self-assessed competence and the
length of work experience (Numminen et al. 2017;
Flinkman et al. 2016). Nurse managers play vital
roles in an organisation. They must ensure nursing
delivery and care are implemented according the
rules. They must also possess a science-based
education and a minimum competency certificate
that will guarantee the community of their
proficiency (Kerfoot, 2012). Nurse managers require
additional competencies because of the uniqueness
of the healthcare environment and conceptual
philosophy, since nurses have a social responsibility
for the health of individuals, families and
communities.
Technical skills are the most important for a
manager to possess, especially for the first-line
manager. First-line managers (FLMs) must have a
comprehensive understanding of a change’s
implementation so they can facilitate it in their areas
of responsibility (Kumah et al. 2016). Even in the
research conducted by Kumah et al. (2016), as a
group, nurse managers from specific healthcare
organisations felt most competent in terms of
technical healthcare skills.
The dimensions of technical skill include the
planning and delivery of care, therapeutic
intervention, ensuring the quality of nursing care,
modifying a care plan according to individual needs,
integration between nursing science, IT development
and current nursing or healthcare research, and
developing effective communication. Rapid
innovations in science and technology can lead to
increased levels of concern in nurses about security
and safety of patient and nurse, as well as nurse
competency (Karami et al. 2017). Therefore, nurse
managers must be responsible for ensuring the
quality of nursing delivery care and services. In
addition, nurse managers at all levels are asked to
integrate concepts regarding current science and
technology developments into nursing practice.
Nurse manager roles requiring healthcare,
context-related competencies comprise social,
organisational, business and financial dimensions.
Within the operational category of competencies,
they identified technic, process, clinical and
development competencies to be a vocal point for
their managerial role. Communication skills were
described with diverse attributes such as: dialogue,
networking, giving a clear information, clarity of
written and oral fluency, facilitating discussion and
active listening (Furukawa & Cunha, 2011).
Additionally, communication skills work in
conjunction with the healthcare strategy, vision and
mission.
A study in the UK about the development of
nurse network managers found they support each
other, provide an environment that helps develop
ideas and solutions, communicate between members
with communication tools and face to face, and vote
to influence government policies and strategies
(Chapman, 2012). Research in Indonesia found data
that internal factors, namely, knowledge, skills,
values and external factors (organisational culture)
affect the leadership competencies of the head nurse
in a hospital. Cultural background in an organization
also depends on the nature and the culture of the size
and type of organization, the number of employees
and senior manager roles. Organizational culture
impacts on the effectiveness of nursing care
delivery. Culture is a set of shared mental
assumptions that guide the way we think, act, and
behave in the workplace. Those who do things in the
“proper” way will lead to the success of
competencies. Those who chose not to do things in
the proper way do not last long with an organization.
However, the organizational culture is closely
associated with senior managers. Every top manager
has different expressions and understandings in
influencing the culture of the organization.
Leadership competencies influence the motivation
and performance of nurses.
Healthcare institutions have two customers, that
is the internal customer and external customer.
Consequently, a healthcare institution must maintain
and develop its staff. The implication is that nurse
managers have the responsibility to build an
effective team, nurse, coach staff through changes,
problem solve and provide a reward system for
nurses. Nowadays, healthcare is facing the problem
in which nurses, especially newly graduated nurses,
feel fatigue, insecure and uncomfortable regarding
their daily routine as a nurse. Accordingly, the rate
of nurse turnover has increased, leading to negative
conditions for health organisations and eventually
harming nursing delivery care.
Nurse managers must also deal with
administration, such as finance and budgeting,
allocating and using resources effectively, ensuring
cost-effective services and controlling
documentation. They often learn experientially to
reach a blend of clinical and business management
capabilities, often with little to no training and many
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
60

other challenges encountered while on the job.
Having a clear understanding of the need to develop
these skills is critical when selecting managers.
However, it is more important when a nurse decide
to prepare themselves to be a nurse manager (Chase,
2010).
The important competence that nurse managers
must gain is managing ethical and legal issues. The
combination of the needs of patients, colleagues and
managers may lead to moral stress for nurse
managers. Reinforcing the skills of nurses,
especially their ethical competency, could be a
solution to reduce moral stress, as Kälvemark-
Sporrong et al. declared. In instances where unit
managers supported best practices, nurses also
experienced them as ethical practices. Above all, this
is important since nurses are more likely to leave
jobs because of moral stress, combined with lack of
managerial support when acting ethically.
5 CONCLUSIONS
A large collection of literature on the competence of
nurse managers was found in this search. The author
summarised the literature search that made a sincere
contribution to the improvement of nurse manager
competencies. In this study, six dimensions of
nursing manager competencies emerged:
sociodemographic, technical, networking,
administrative, staff development and legal-ethical.
The results highlighted that nurse manager have
to be more committed and more competent to their
organisations. However, it is necessary to conduct
more comprehensive studies for exploring the gaps
in the human resource management of healthcare in
different contexts and cultures, especially between
Western country (such as Europe and United State)
and Eastern country, such as Asia. It is been
important thing as cultural background determines
the competencies of nurse manager and profile of
the organization.
Also, future studies are suggested to investigate
the usefulness of the competency model for
assessing nursing managers’ readiness to between
job applicants, implement continuing education
programmes for nurse managers, and develop and
plan their careers.
ACKNOWLEDGEMENTS
Acknowledgement and high appreciation to the
editor and anonymous reviewers for their
constructive comments and recommendation.
REFERENCES
Benner, P., 2001. From Novice to expert: Excellence and
power in clinical nursing practice, Upper Saddle
River, New Jersey: Prentice-Hall.
Bjork, I.T. et al., 2007. Evaluation of clinical ladder
participation in Norway. Journal of Nursing
Scholarship, 49(10), pp.89–94.
Burton, S., 2015. Collaborative Practice in Health care.
Leadership in Health Services, 39(1), pp.85–94.
Chapman, N., 2012. Developing the RCN Executive
Nurse Network. , 19(3), pp.24–26.
Chase, L.K., 2010. Nurse manager competencies. Journal
of Nursing Administration, 24, pp.56–64.
Deyo, P., Swartwout, E. & Drenkard, K., 2016. Nurse
manager competencies supporting patient engagement.
Journal of Nursing Administration, 46(3), pp.S19–
S26.
Donaher, K. et al., 2007. The Human Capital
Competencies Inventory for Developing Nurse
Managers. The Journal of Continuing Education in
Nursing, 38(6), pp.277–283. Available at:
http://www.healio.com/doiresolver?doi=10.3928/0022
0124-20071101-08.
Doran, D. et al., 2015. Evaluating the late career nurse
initiative: A cross-sectional survey of senior nurses in
Ontario. Journal of Nursing Management.
Duffield, C. et al., 2014. Job enrichment: Creating
meaningful career development opportunities for
nurses. Journal of Nursing Management.
Efendi, F. et al., 2018. Nursing qualification and
workforce for the Association of Southeast Asian
Nations Economic Community. Nursing Forum,53(2),
197-203.
Erjavec, K. & Starc, J., 2017. Competencies of Nurse
Managers in Slovenia: a Qualitative and Quantitative
Study. Central European Journal of Nursing and
Midwifery, 8(2), p.632. Available at:
https://periodika.osu.cz/ojs/index.php/cejnm/article/vie
w/57.
Flinkman, M. et al., 2016. Nurse Competence Scale : A
systematic and psychometric review. Journal of
Advanced Nurse, 8(2), 1-16.
Flinkman, M. & Salanterä, S., 2015. Early career
experiences and perceptions - a qualitative exploration
of the turnover of young registered nurses and
intention to leave the nursing profession in Finland.
Journal of Nursing Management. 4(1), 26-34.
Furukawa, P. de O. & Cunha, I.C.K.O., 2011. Profile and
competencies of nurse managers at accredited
hospitals. Revista Latino-Americana de Enfermagem,
19(1), pp.106–114. Available at:
http://www.scielo.br/scielo.php?script=sci_arttext&pid
=S0104-11692011000100015&lng=en&tlng=en.
Improving Nurse Managers’ Competencies: A Systematic Review
61

Gunawan, J. & Aungsuroch, Y., 2017. Managerial
competence of first-line nurse managers: A concept
analysis. International Journal of Nursing Practice,
23(1), pp.1–7.
Gunawan, J., Aungsuroch, Y. & Fisher, M.L., 2018.
Competence-based human resource management in
nursing: A literature review. Nursing Forum, 53 (1), 1-
11. Available at:
http://doi.wiley.com/10.1111/nuf.12302.
Jacob, J.I. et al., 2008. Six Critical Ingredients in Creating
an Effective Workplace. , pp.141–161.
Jennings, K., Mutsch, K.S & Schleman, J., 2009. Factors
contributing to decision to participation or not
participate in a clinical ladder program. Nothern
kentucky University: Dissertation.
Johan Tri Agus Yuswanto, 2013. Nursing Leadership
Models Development In 13 Class A Hospital. Journal
of Nursing and Health Science (IOSR-JNHS), 1(5),
pp.24–31. Available at:
http://www.iosrjournals.org/iosr-jnhs/papers/vol1-
issue5/E0152431.pdf.
Kantanen, K. et al., 2017. Leadership and management
competencies of head nurses and directors of nursing
in Finnish. Social and health care Journal, 22 (3),
228-244. DOI :
http://dx.doi.org/10.1177/1744987117702692
Kantanen, K. et al., 2015. The development and pilot of an
instrument for measuring nurse managers’ leadership
and management competencies. Journal of Research
in Nursing, 20(8), pp.667–677.
Karami, A., Farokhzadian, J. & Foroughameri, G., 2017.
Nurses’ professional competency and organizational
commitment: Is it important for human resource
management? PLoS ONE, 12(11), pp.1–16. Available
at: http://dx.doi.org/10.1371/journal.pone.0187863.
Keane, S., Lincoln, M. & Smith, T., 2012. Retention of
allied health professionals in rural New South Wales :
a thematic analysis of focus group discussions.
Kendall-Gallagher D & Blegen M.A, 2009. Competence
and certification of registered nurses and safety of
patients in intensive care unit. American Journal of
Critical Care, 18(2), pp.106–116.
Kerfoot, K.M., 2012. Is Nurse Executive / Nurse
Management?. Journal of Advance Nurse Practice,
30(1), pp.38–40.
Kumah, E., Ankomah, S.E. & Antwi, F., 2016. The role of
first-line managers in healthcare change management :
a ghanaian context. International Journal of
BioSciences, Healthcare Technology and
Management, 6(3), pp.20–33.
Kvas, A., Seljak, J. & Stare, J., 2013. The Use of
Competency Models to Assess Leadership in Nursing.
Iranian journal of public health, 42(9), pp.988–995.
Likupe, G., 2015. Experiences of African nurses and the
perception of their managers in the NHS. Journal of
Nursing Management, 11(4), 180-188.
McCarthy, G. & Fitzpatrick, J.J., 2009. Development of a
Competency Framework for Nurse Managers in
Ireland. The Journal of Continuing Education in
Nursing, 40(8), pp.346–350. Available at:
http://www.healio.com/doiresolver?doi=10.3928/0022
0124-20090723-01.
Numminen, O. et al., 2017. Development of Nurses’
Professional Competence Early in Their Career: A
Longitudinal Study. The Journal of Continuing
Education in Nursing, 48(1), pp.29–39. Available at:
http://www.healio.com/doiresolver?doi=10.3928/0022
0124-20170110-08.
Onishi, M. et al., 2008. Development of nurses with
specialties: The nurse administrators’ perspective.
Journal of Nursing Management, 7(2), 83-92.
Palmer, S.P., 2014. Nurse retention and satisfaction in
Ecuador: Implications for nursing administration.
Journal of Nursing Management, 14(3), 293-305.
Petri, H.L., & Govern, J., 2013. Motivation: Theory,
research and application (6th ed.), Belmont, CA:
Wadsworth Cengage Learning.
Pihlainen, V., Kivinen, T. & Lammintakanen, J., 2016.
Management and leadership competence in hospitals:
a systematic literature review. Leadership in Health
Services, 29(1), pp.95–110.
Pillay, R. & Pharm, H., 2009. Perceived competencies of
nurse managers : A comparative analysis of the public
and private sectors in South Africa. Journal of
Business, 3(9), pp.495–503.
Porkodi, S. & Haque, A., 2012. Human resource issues:
special emphasis on maintenance and retention of
paramedical employees in Private Hospitals. Journal
of Organisation & Human Behaviour, 1(2), pp.19–31.
Shammot, M.., 2014. The role of human resources
management practices represented by employee’s
recruitment and training and motivating in realization
competitive advantage. International Business
Research, 7(4), pp.55–72.
Silva, J.C.B. da, Silva, A.A.O.B. da & Oliveira, D.A.L.,
2018. Profile of the nurse in the management of
hospital services. Jounal of Nursing, 12(10), pp.2883–
2890.
Supamanee, T. et al., 2011. Preliminary clinical nursing
leadership competency model: A qualitative study
from Thailand. Nursing & Health Sciences, 9(2), 11-
23.
Titzer, J.L. & Shirey, M.R., 2013. Nurse manager
succession planning: A concept analysis. Nursing
Forum, 21(3), 24-36.
Wangensteen, S., Johansson, I.S. & Nordström, G., 2015.
Nurse Competence Scale - Psychometric testing in a
Norwegian context. Nurse Education in Practice,
15(1), pp.22–29.
Watson, R. et al., 2002. Clinical competence assessment in
nursing: a systematic review of the literature. Journal
of Advanced Nursing, 39(5), pp.421–431.
Wilkinson, C.A., 2013. Competency Assessment Tools for
Registered Nurses: An Integrative Review. The
Journal of Continuing Education in Nursing, 44(1),
pp.31–37.
Wong, C.A. et al., 2013. Part 2: Nurses’ career aspirations
to management roles: Qualitative findings from a
national study of Canadian nurses. Journal of Nursing
Management.
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
62
Yeon, H.. et al., 2017. Development and validation of a
nursing profesionalism evaluation model in a career
ladder system. Plos One, 12(10), 1-14.
APPENDIX
Figure 1: Diagram of database search.
Author, year
Research
design
Competency define
(Flinkman et al.
2016)
Systematic
review
Ther are positive
correlation between:
age, higher
education, duration
of work experience,
employment status,
and participation in
educational
programmes with
competence.
(Yeon et al. 2017) Quantitative
The clinical
competence
dimensions were:
Scientific, technical,
ethical, aesthetic and
existential.
(Numminen et al.
2017)
Mixed Method
The 73‐item scale
consists of seven
categories, with
responses on a
visual analogy scale
format.
(Wong et al.
2013)
Qualitative
The major aspects
that influencing
nurses’ decisions to
pursue management
roles are:
‐ personal
demographic (age,
education, clinical
experience and
life
circumstances),
‐ personal
disposition
(intrinsic rewards,
professional
commitment and
leadership skills)
and
‐ situation
(opportunities of
leadership
development,
perception of
manager role
perceptions and
the presence of
mentors).
(Efendi et al.
2018)
Qualitative
Nurses have to
emphasize nursing
as a thinking
profession and
highlight clinical
knowledge and
Author, year
Research
design
Competency define
competence. Nurses
need to affirm their
professional identify
that can be
demonstrated in a
number of ways.
Nursing has to be
view their work as a
career and have to
be proud to attach
the tiltle “nurse” to
their last name.
(Kumah et al.
2016)
Cross sectional
survey
Five important
competencies were
considered by the
first line managers
were effective
communication,
technical
competencies,
ability to organise
staff through
change, skill of
conflict
management,
problem solving
skills, effective team
building and
leadership skill.
(Jacob et al. 2008) Quantitative
Six aspects for
effective workplace
that were: job
autonomy, learning
opportunities,
supervisor support,
coworker team
support,
involvement in
decision making,
and flexibility of
workplace.
(Erjavec & Starc
2017)
An online
survey and in-
depth
interviews
The competencies of
nurse manager are:
technical, human
resources,
conceptual,
leadership and
financial.
(Karami et al.
2017)
Descriptive
analytic study
The competency of
nurses in various
clinical positions
leadership (9 items),
were clinical care
(10 items),
interpersonal
relationships (8
items), professional
development (6
items), legal-ethical
practice (8 items),
teaching-coaching
(6 items) and
research aptitude-
critical thinking (8
items).
Improving Nurse Managers’ Competencies: A Systematic Review
63
Author, year
Research
design
Competency define
(Gunawan et al.
2018)
literature review
Antecedents to
CBHRM in nursing
include
organizational
factors (such as:
organizational size,
culture, the nature of
human resource
(HR) department,
type of organization,
and the number of
employee),
individual factors (
such as
competencies of
human resource
manager, role of top
managers, intention,
and characteristics),
and human
resources policy.
(Gunawan &
Aungsuroch 2017)
Literature
review
The attributes of
managerial
competence include
developing self,
management
function (POSAC),
leading, managing
legal and ethical
issues, and
delivering health
care. Antecedents to
managerial
competence are
internal and external
factors.
(Kvas et al. 2013) Quantitative
The norms for the
competency profiles
for three leadership
levels in nursing
were flexibility at
work, creativity,
leadership,
organizational
climate,
networking&influen
cing, realization
skills, ethics,
interprofessional
relationship, positive
attitude towards
knowledge and
education
(Wangensteen et
al. 2015)
A cross-
sectional design
Competence
categories: Planning
and delivery of care,
Teaching functions,
Professional
leadership, Research
utilization and
nursing values and
Professional
awareness.
(Silva et al. 2018)
Integrative
review of
articles
The ability of
communication in
the leadership and
Author, year
Research
design
Competency define
supervision
relationship, conflict
resolution regarding
teamwork, planning
in organizations of
services, technical
competence in
professionals’
qualification, and
prevision and
provision of material
resources.
(Donaher et al.
2007)
An integrative
review
Developing self (16
items), recruiting
(11 items),
developing others
(15 items), utilizing
(8 items), retaining
(8 items), and
managing human
capital (58 items)
(Pihlainen et al.
2016)
systematic
literature review
The characteristics
of management and
leadership
competence were
categorized into the
following groups:
health-care-context-
related, operational
and general.
(McCarthy &
Fitzpatrick 2009)
A cross-
sectional
descriptive
design
Behavioral
indicators are
currently being used
to assess
management skills,
design and
implement
continuing
education programs
for nurse managers,
and provide advice
about career
development and
planning for nurse
managers.
(Bjork et al. 2007)
Cross sectional
survey design
Managers in
cooperation with
unit personel should
become aware of
and develop system
to support learning
and use of
competence.
(Numminen et al.
2017)
Quantitative
Empowerment
increased minimally,
whereas perceptions
of practice
environment, ethical
climate, and
occupational
commitment
decreased.
Empowerment,
satisfaction with
current job and
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
64
Author, year
Research
design
Competency define
quality of care, time
from graduation &
work experience
explained 25.6% of
the change in
competence.
(Wilkinson 2013)
Systematic
literature
A unique set of
dimensions of
continuing
competency are
clinical care,
leadership,
interpersonal
relationships).
(Wong et al.
2013)
Qualitative
(focus group
methodology)
Staff nurses identify
aspect of
management role:
the need for
graduate education,
development of
budget and human
resource
competencies, heavy
workload, large span
of control, job
insecurity, potential
work life imbalance
and reduce patient
contac
t
(Titzer & Shirey
2013)
Analysis
method
Talent management
as a human
resources recruiting
and retaining
strategy whereas
succession planning
was the
responsibility of
current leaders
(Onishi et al.
2008)
Qualitative
It is important to
focus more attention
on qualitative aspect
of nurses’
professional
experience in
service education
(Supamanee et al.
2011)
Qualitative
Nurses’ clinical
leadership
competencies
emerged,
comprising hidden
characteristics
(motive, attitude and
values) and surface
characteristic
(specific knowledge,
management &
nursing informatics)
(Pillay 2009) Quantitative
Management
competency
variables were
delivery of health
care, planning,
organizing, leading,
control, legal and
ethical issues, and
Author, year
Research
design
Competency define
self management.
(Furukawa &
Cunha 2011)
Quantitative
The nurse managers’
most frequent
competencies
according to their
superiors were:
leadership, focus on
patient and
teamwork
(Johan Tri Agus
Yuswanto 2013)
Qualitative and
quantitative
research
Expected leader
attitude on
developed model
based on statistical
counting and also
functioned as
competency are
mentioned below:
good coach for staff,
inspirational
motivation, team
building and team
work, institutional
structured, knowing
staffs’ need
(Kerfoot 2012)
Literature
review
The ability to use
evidence based
management and
leadership processes
is variable based on
the rigor of the
person’s
understanding of
evidence and
research based
clinical processes
and outcomes
(Kantanen et al.
2017)
Quantitative
Head nurses and
directors of nursing
evaluated
themselves to be
most competent in
areas of general
competence and less
competent in the
areas of special
competence.
(Deyo et al. 2016)
Literature
review
It is important to
understand the
competencies and
education required
to support nurse
manager role
(McCarthy &
Fitzpatrick 2009)
Quantitative
and qualitative
General
competencies for
nurse managers:
communication and
influencing skills,
building and
managing
relationships,
integrity, personal
commitment,
resilience and
compsure, service
irritation and
Improving Nurse Managers’ Competencies: A Systematic Review
65
Author, year
Research
design
Competency define
innovation,
promoting evidence
based decision
making, practitioner
competence and
professional
credibility
Machell., et al.
(2009)
Literature
review
Competence gives
you the potential
credibility that you
need with colleagues
if they are accept
your leadership
(Chapman 2012)
Literature
review
Top nurse manager
who work in
positions of
influence with
board-level
authority
(Widhi Sudariani
et al. 2016)
Quantitative
and qualitative
Development of
leadership
competency model
can increase the
motivation and
performance nurse
Mildon, B (2014).
Literature
review
Competencies refer
to specific
knowledge, skills,
and personal
attributes required
clinical nurse
specialist practice
safely and ethically
in a designated role
and setting
(Erjavec & Starc
2017)
Qualitative and
quantitative
Reasons for nurse
managers’
differences in
proficiency levels
are the level of job
security, autonomy,
and support of the
healthcare team.
(Doran et al.
2015)
Quantitative
Leaders need pay to
attention to how late
career nurses are
selected and
matched to
organisational
projects
(Palmer 2014)
Qualitative and
quantitative
Increasing nursing
pay is one strategic
to consider in
decreasing turnover
and increasing
satisfaction
(Likupe 2015) Qualitative
Managers need to be
aware that good
policies can be
misinterpreted and
disadvantage
minorities and
should therefore
take steps to
promote good
Author, year
Research
design
Competency define
practice
(Duffield et al.
2014)
Qualitative
Methods of job
enrichment need to
be considered as
part of career
development policy
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
66
