
The Nurses’ Compliance in Femoral Sheath Removal Procedure in
Relation to the Incidence of Hematoma in Patients after PTCA
Jati, Christina Yuliastuti and Nisha Dharmayanti Rinarto
STIKES Hang Tuah Surabaya, East Java, Indonesia
Keywords: Hematoma, Nurses’ Compliance, PTCA, Sheath Removal.
Abstract: Femoral hematomas may occur after Percutaneous Transluminal Coronary Angioplasty (PTCA). The
objective of this study was to identify the correlation between the nurses’ compliance of femoral sheath
removal with the incidence of hematoma in patients after PTCA. This observational study enrolled 20 nurses
and 20 patients after PTCA in Intensive Care Unit, taken by simple random sampling. Data collection was
undertaken using a set of observation sheet based on Standard Operating Procedure and the presence of
hematoma. The data were analyzed with Spearman Rank test with significance level of 0,05. Results showed
that there was a significant correlation between compliance of nurses in performing the procedure of sheath
removal with the incidence of hematoma (ρ = 0.000). A properly performed compression manual on removal
of the arterial sheath, ie, for 15-20 minutes until hemostasis is reached where no bleeding through the catheter
inserts will minimize the incidence of the hematoma. Supervision, training and simulation will improve the
capacity of nurses’ knowledge and skills in performing sheath removal procedures.
1 BACKGROUND
Percutaneous Transluminal Coronary Angioplasty
(PTCA) is a procedure whereby a balloon catheter is
inserted through a wire, and then developed at the site
of stenosis to increase the lumen diameter (Philip,
2010), it is expected to improve blood flow to the
myocardium, myocardial damage is not widespread,
chest pain and symptoms of tightness can be reduced
even disappeared by the inclusion of ring or stent in
blood vessels that have blockage. Elective PTCA
within 30 days post IMA may reduce mortality and
risk of complications when compared with medical
therapy especially in patients with unstable
conditions, but in patients with stable asymptomatic
and stable hemodynamic risk the results are no better
than optimal medical therapy (Subagyo, 2012).
Klemsová and Žiaková (2014) said that both
approaches to catheterization carry the risk of
complications associated with the removal of cannula
sheath. The most common complication after cardiac
catheterization through the femoral artery is the
development of vascular complications (bleeding,
hematoma, pseudoaneurysm). From history it is
known that complications associated with the
removal of cannula (sheath) from the femoral artery
were up to 11%. Hamon et al. (2007) indicate, based
on a systematic review and meta-analysis of
randomized trials, incidence of complications in the
femoral approach in 2–5% of patients after
interventional procedures. Studies in 90 patients
undergoing cardiac interventional procedures were
randomly selected to undergo one of 3 sheath removal
methods : manual compression, mechanical
compression with Compressar, and mechanical
compression with Femostop. The results showed that
patients undergoing sheath removal manually had
fewer complications than patients who underwent
sheath removal using Compressar or Femostop
(Benson et al., 2005). Research on 413 patients with
Following Sheath Removal With Percutaneous
Coronary Intervention, as many as 60 (16.5%) had
complications. Sixty-four (15.5%) had hematoma, 6
(1.5%) had bleeding, 4 (1%) had arteriovenous fistula
and 3 (0.7%) had pseudoaneurysms. No significant
difference in complications either using manual
compression, C-Clamp or arterial vascular closure
device (Sulzbach-Hoke, Ratcliffe, Kimmel,
Kolansky, & Polomano, 2010).
Walker, Cleary, & Higgins (2001) conducted a
comparative study (FemoStop compression versus
manual compression) in order to reduce the
complications at the injection site. The results showed
Jati, ., Yuliastuti, C. and Rinarto, N.
The Nurses’ Compliance in Femoral Sheath Removal Procedure in Relation to the Incidence of Hematoma in Patients after PTCA.
DOI: 10.5220/0008329806210625
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 621-625
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
621
that the incidence of hematoma has a great
relationship to the method of compression used on the
femoral artery. Walker said that although using
manual pressure compression the hemostasis was
achieved faster than with FemoStop, both methods
are considered as effective to reduce complications in
the groin. However, non-compliance of nurses in the
procedure of removing the femoral sheath will lead to
hematoma, discomfort, healing period and elongated
day. Risk factors predisposing patients to these
complications are both modifiable (procedure
technique, medications, hemostasis method) and
nonmodifiable (sex, age, body mass index, blood
pressure, renal function). Patients’ risks can be
reduced by nurses who are knowledgeable about
these risk factors and identify complications before
they become problematic (Merriweather & Sulzbach-
Hoke, 2012). The objective of this study was to
identify the correlation between the nurses’
compliance of femoral sheath removal with the
incidence of hematoma in patients after PTCA.
2 METHODS
This study used observational analytic and conducted
to identify the correlation between the nurses
compliance of femoral sheath removal with the
incidence of hematoma in patients after PTCA.
Samples were taken by simple random sampling
consisting of 20 nurses and 20 patients after PTCA in
Intensive Care Unit, aged 40-60 years and take anti-
platelet drugs (Pavix, aspilet and the like), not
suffering from Diabetes mellitus and
thrombocytopenia. Data collection was undertaken
using a set of observation sheet based on Standard
Operating Procedure (SOP) and the presence of
hematoma. The applicable SOP in Intensive Care
Unit consisted of 15 steps of the procedure. Both
nurses compliance in performing sheath removal and
the incidence of hematoma were observed only one at
a time. The data were analyzed with Spearman Rank
test with significance level of 0.05.
3 RESULTS
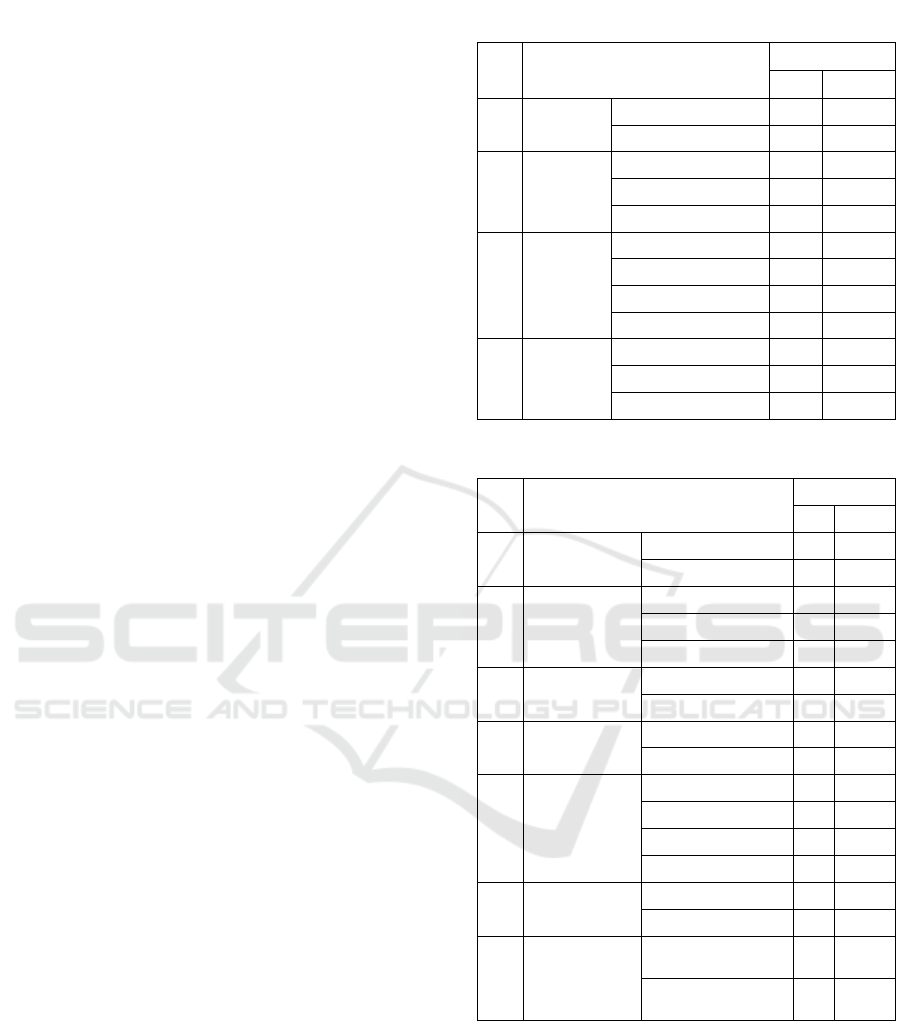
Overall, from 20 respondents, the majority of patient
were male (60%) and The average age was 51≤60
years old (50%) and has suffered from the disease for
0-1 years (50%). Mostly get CPG as a drug therapy.
Characteristics of patients can be seen in Table 1.
While the participant nurses, mostly were female
(65%) and aged 25≤30 years old (65%). Mostly
educated diplomas (90%), not married (55%), and the
average nurse has worked >3 years in Intensive Care
Unit, as a nurse ascociate (90%) and never
participated in any specific training on sheath
removal procedures (75%). Characteristics of nurses
can be seen in Table 2.
Table 1: Patients characteristic.
No
Patients Characteristic
Frequency
n
%
1
Gender
Male
12
60.0%
Female
8
40.0%
2
Age
30-<40 years old
5
25.0%
40-<50 years old
5
25.0%
51-<60 years old
10
50.0%
3
Length
of
suffering
disease
0-1 year
10
50.0%
2-3 year
3
15.0%
3-5 year
2
10.0%
>5 year
5
25.0%
4
Drugs
CPG
17
85.0%
Plavix
3
15.0%
Blistra
0
0.0%
Table 2: Nurses characteristic.
No
Nurses Characteristic
Frequency
n
%
1
Gender
Male
7
35%
Female
13
65%
2
Age
20-<25 years old
6
30%
25-<30 years old
13
65%
30-35 years old
1
5%
3
Last
Education
Diplomas
18
90%
Bachelor
2
10%
4
Marital
status
Not Married
11
55%
Married
9
45%
5
Length of
work in ICU
0-6 months
4
20%
6 months - 1 year
3
15%
1-3 years
6
30%
>3 years
7
35%
6
The position
of nurse
Nurse ascociate
18
90%
Nurse team chief
2
10%
7
Experience
in special
training
Have attended
training
5
25%
Never
15
75%
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
622
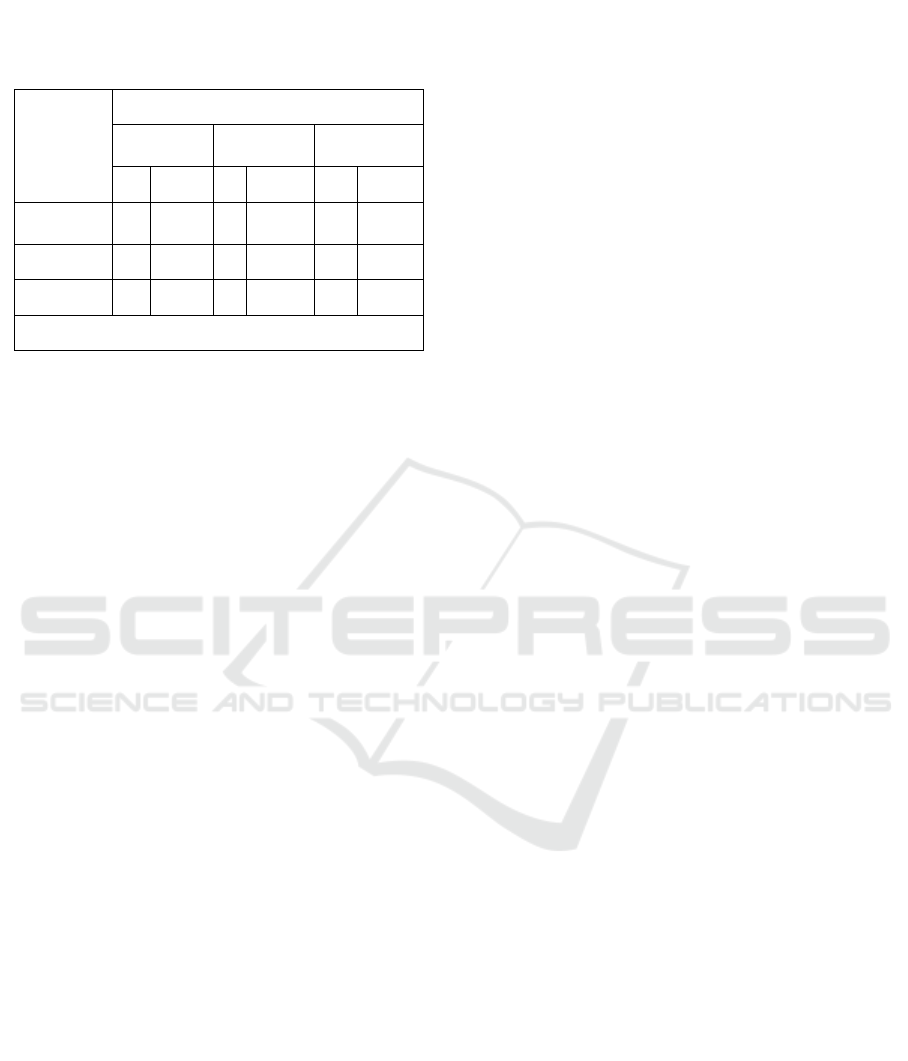
Table 3 showed that 7 (77.8%) non-adherent
nurses on the procedure of femoral sheath removal
causing hematoma in patients and 11 nurses (100%)
who adhered to the procedure did not cause
hematoma in patients after PTCA. This study found
that there was a significant correlation between
compliance of nurses in the femoral sheath removal
procedure and the incidence of hematoma (p = 0.000).
4 DISCUSSION
Percutaneous Transluminal Coronary Angioplasty
(PTCA) is a coronary angioplasty action using a
technique with balloons inserted into a stenotic
coronary vessel, after which the balloon is developed
and thus the stenosis disappears or is greatly reduced,
then the balloon is deflated and removed (Sudoyo,
2006). Percutaneous transluminal coronary
angioplasty (PTCA), formerly known as balloon
angioplasty (European Society of Cardiology, 2010).
The sheath removal procedure should be performed
carefully and in accordance with the procedure so as
not to cause vascular complications such as
hematoma. Sabo, Chlan, & Savik (2008) found that
the most frequently occurring Vascular
Complications (VCs) after sheath removal following
a percutaneous coronary intervention procedure were
ecchymosis, hematoma, and oozing. Body surface
area significantly influenced hematoma formation.
The results showed that of the 11 nurses who
adhered to Standard Operational Procedure (SOP), 6
nurses (54.5%) had worked >3 years, while from 9
non-compliant nurses to SOPs, 4 (44.4%) were new
nurses working between 0-6 months. In addition, 5
nurses who had attended the training, all complied
with SOP, while from 15 nurses who never received
special training, as many as 9 (60%) did not comply
with SOP. It can be explained that experience affects
nurse compliance in performing procedures
according to the rules, but this ability needs to be
rehearsed and repeated continuously in order to create
habits. This is in accordance with the research of
(Schiks, Verheugt, & Achterberg, 2007) about
performance evaluation of arterial femoral sheath
removal by registered nurses after PCI that was
perform in 1999 and 2005, they explained that
registered nurses achieved the norm for good
performance (80–89%) of removing arterial sheaths
according to protocol after a training programme and
this is stable in time. Since the norm for excellent
performance (≥90%) was not achieved, current
performance could be improved. e.g. by yearly
repetition of training and observation of skills.
The study founds 9 nurses (45%) who did not
comply with SOPs. The non-compliance was also
caused by the lack of supervision from the supervisor,
so the nurses performed the sheath removal
procedure, sometimes less cautious, because they
assumed that no one was watching during or after the
procedure. This is as stated by (Niven, 2002) that the
quality of interaction between health professionals is
an important part in determining the degree of non-
compliance due to the lack of reprimand and sanction
for nurses who have disobedient behavior in doing aff
sheath, lack of interaction between nurses because
there is no mutual reminded to be obedient to the
SOP.
Hematoma is an accumulation of external
bleeding or it can also hide inside a tissue (Ramzi S,
2004). Hematoma when evaluated in terms of extent
may be small, with only one blood point or can
become large and cause significant swelling. The
blood vessels in the body are always under constant
repair. Minor flocs occur routinely and the body is
usually able to repair damaged vessel walls by
forming fibrin patches. Sometimes the repair fails
when extensive damage and major damage lead to
continuous bleeding. Likewise, if there is great
pressure in the blood vessels, for example the main
artery, the blood will continue to leak and the
hematoma will dilate. Blood coming out of the
bloodstream is very irritating and may cause
inflammatory symptoms including pain, swelling and
redness. Symptoms of a hematoma depend on
location, size and whether it causes swelling and
edema. (Walker et al., 2001) said that the incidence
of hematoma has a great relationship to the method of
compression used on the femoral artery. This study
found that 7 (77.8%) non-adherent nurses on the
procedure of femoral sheath removal causing
hematoma in patients and 11 nurses (100%) who
Table 3: Correlation between compliance of nurses
in the femoral sheath removal procedure and the
incidence of hematoma.
Compliance
of nurses
The incidence of hematoma
hematoma
No
hematoma
Total
n
%
n
%
n
%
Not
Obedient
7
77.8%
2
22.2%
9
100%
Obedient
0
0%
11
100%
11
100%
Total
7
13
20
100%
p = 0.000 r = 0.811
The Nurses’ Compliance in Femoral Sheath Removal Procedure in Relation to the Incidence of Hematoma in Patients after PTCA
623

adhered to the procedure did not cause hematoma in
patients after PTCA. There are several systems that
play a role in the hemostatis vascular system, platelets
and blood clotting. Prevention of blood loss, if the
blood vessels that have ruptured through several ways
between other : blood vessel constriction that is
immediately after the blood vessels cut or rupture
wall smooth muscle blood vessels contract so that the
blood flow from blood vessels that rupture will
decrease, the formation of platelet stoppers where
very small blood vessels are usually covered by small
disc-shaped platelets stacked with 1 to 4 micrometres
in bone marrow, clot freezing in ruptured vessels that
begin to form within 1 to 2 minutes and 20 minutes to
60 minutes of clot will experience retraction, this can
close the site of the wound is the formation of fibrous
tissue as a response to rupture of blood vessels occur
complex chemical structures in the blood involving
various factors of blood clotting which the end result
is the formation of a complex of activated substances
that collectively in call the prothrombin activator, the
prothrombin activator catalyzes the conversion of the
protombin to thrombin, thrombin acts as an enzyme
to convert fibrinogen into fibrin fibrils that sequence
platelets of blood cells and plasma to form clots.
(Guyton, A.C., dan Hall, 2008) The use of
thrombolytic therapy also has an effect on the
occurrence of hematoma during sheath removal.
Researchers also found that patients were still taking
thrombolytic therapy before the sheath removal that
resulted in blood thinning. Anticoagulant drugs are
used to prevent the occurrence of thrombosis, which
works to inhibit blood clotting. The mechanism of
action of anticoagulant drugs is to suppress the
synthesis of clotting factors that influence vitamin K
ie protombin, VII, IX, and X. The main work of
anticoagulant drugs is to inhibit the action of
enzymepoxide reductase. After a week of consecutive
treatment, the activity of the clotting factor will be
very low in the blood. Patients taking blood-thinning
drugs (anticoagulation) such as warfarin (coumadin),
aspirin, clopidogrel (plavix), and prasugrel. These
drugs increase the potential for spontaneous bleeding
and for widespread hematoma because the body can
not efficiently repair blood vessels and blood is
constantly out through damaged areas. Besides the
proper compression technique will reduce the
occurrence of hematoma.
This study also founds that there was a significant
correlation between compliance of nurses in the
femoral sheath removal procedure and the incidence
of hematoma (p = 0,000). Manual compression in
sheath removal is done until the hemostasis is reached
where no bleeding occurs through the catheter
insertion mark, which is 15 to 20 minutes.
Compliance of nurses in this case is assessed from the
adherence of the 15 steps based on the standard
operational procedure of femoral sheath removal
applicable in Intensive Care Unit. The researcher
gave a score of 1 if not done and score 2 when done.
This study found that of the 20 nurse respondents, the
highest total score was 40 at the fourth, fitfh, sixth and
eightth steps, this means that all nurses performed
observation/ monitoring of vital signs during the
procedure, palpated the dorsalis pedis pulsation,
placed 2 fingers 2-3 cm above the sheath for touch
pulsation of the femoral artery and perform manual
compression properly until the blood does not come
out. The compression is done by reducing the strength
25% after ± 15 minutes while the patient is observed,
if blood is still out then back to the beginning until no
blood came out, 5 minutes later strength of pressure
minus 50%. When it is stop to came out, then give a
band aid and do a compression bandage. The
researcher assumes that all steps in Standard
Operational Procedure (SOP) must be done properly
and carefully to minimize the complication of femoral
sheath removal (hematoma).
5 CONCLUSIONS
Percutaneous Transluminal Coronary Angliplasty
(PTCA), or Coronary Angioplasty, is a non-surgical
procedure with minimal incisions used to open
narrowed blood vessels. This procedure uses a
flexible catheter with a balloon at the end, which is
inflated at high pressure inside the narrowed artery
wall. This action will plaque plaque in the blood
vessels and improve blood flow to the heart muscle.
This procedure can eliminate some of the symptoms
of artery blockage, such as chest pain or shortness of
breath. Nurses compliance in the femoral sheath
removal procedure in patients after PTCA is
associated with the incidence of hematoma, The
compression should be performed carefully and in
accordance with the standard operational procedure
to prevent the occurrence of vascular complications,
one of which is a hematoma. Yearly repetition of
training and observation of skills (supervision) will
improve the capacity of nurses’ knowledge and skills
in performing sheath removal procedures.
Limitations of the study were in terms of confounding
variables that can not be controlled by the researchers,
such as body surface, bleeding and blood clotting
period, which may affect the occurrence of
hematoma.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
624

ACKNOWLEGEMENTS
Our deepest appreciation goes to our beloved families
for the endless love, pray, and support to keep going
and never giving up. we gratefully thank to the
principal of Stikes Hang Tuah Surabaya (Hang Tuah
Surabaya, Health Sciences Institute) for allowing us
to move forward and develop ourselves. Our gratitude
also goes to all the respondents.
REFERENCES
Benson, L. M., Wunderly, D., Perry, B., Kbboord, J.,
Wenk, T., Birdsall, B., & Nyirenda, T. (2005).
Determining best practice: comparison of three
methods of femoral sheath removal after cardiac
interventional procedures. Heart & Lung: The
Journal of Acute and Critical Care, 34(2), 115–
121.
European Society of Cardiology. (2010). Guidelines
for Myocardial Revascularisation.
Guyton, A.C., dan Hall, J. . (2008). Buku Ajar
Fisiologi Kedokteran (11th ed.). Jakarta: EGC.
Klemsová and Žiaková. (2014). Standardization of
the Possibility of Specialised Nursing Care After
Cardiac Catetrization, 7.
Merriweather, N., & Sulzbach-Hoke, L. M. (2012).
Managing risk of complications at femoral
vascular access sites in percutaneous coronary
intervention. Critical Care Nurse, 32(5), 16–29.
Niven, N. (2002). Psikologi Kesehatan Pengantar
Untuk Perawat Profesional Kesehatan lain.
Jakarta: EGC.
Ramzi S, dkk. (2004). Buku Ajar Patologi (7th ed.).
Jakarta: EGC.
Sabo, J., Chlan, L. L., & Savik, K. (2008).
Relationships among patient characteristics,
comorbidities, and vascular complications post-
percutaneous coronary intervention. Heart &
Lung: The Journal of Acute and Critical Care,
37(3), 190–195.
Schiks, S., Verheugt, A., & Achterberg. (2007).
Performance evaluation of arterial femoral sheath
removal by registered nurses after PCI. European.
Journal of Cardiovascular Nursing, 6(3), 172–
177.
Subagyo. (2012). Basic Clinical Approach In
Cardiovasculer Management. Surabaya: RSUD
Dr. Soetomo.
Sudoyo, A. (2006). Buku Ajar Ilmu Penyakit Dalam.
Jakarta: Fakultas Kedokteran Universitas
Indonesia.
Sulzbach-Hoke, L. M., Ratcliffe, S. J., Kimmel, S. E.,
Kolansky, D. M., & Polomano, R. (2010).
Predictors of complications following sheath
removal with percutaneous coronary intervention.
Journal of Cardiovascular Nursing, 25(3).
Walker, S. B., Cleary, S., & Higgins, M. (2001).
Comparison of the FemoStop device and manual
pressure in reducing groin puncture site
complications following coronary angioplasty
and coronary stent placement. International
Journal of Nursing Practice, 7(6), 366–375.
The Nurses’ Compliance in Femoral Sheath Removal Procedure in Relation to the Incidence of Hematoma in Patients after PTCA
625
