
The Implementation of Patient Safety by Nurses at Inpatient Rooms
of Community Health Centers
Srimawati
1,2
, Hajjul Kamil
3
, Marthoenis
3
, Endang Mutiawati R
4
, Teuku Tahlil
3
1
Master Program of Nursing Science, Faculty of Nursing, Syiah Kuala University, Banda Aceh, 23111
2
Nursing Academy Programme, Jabal Ghafur Sigli Pidie
3
Lecturer at Nursing Faculty of Syiah Kuala University,23111
4
Nueroscience Department, Faculty of Medicine , Syiah Kuala University, Banda Aceh, 23111
ttahlil@unsyiah.ac.id
Keywords: Patient safety, nurse, puskesmas, comparative
Abstract: The issue of patient safety has become a global issue since the Institute of Medicine (IOM) in the United
States published a paper titled “to Err Is Human: Building A Safer Health System.” However, the issue of
patient safety at the community health centers (hereinafter-termed puskesmas) is not as dynamic as that of
the hospital level. The aspect of clinical quality and patient safety in puskesmas is only recently
implemented in Indonesia.This study aimed to identify the implementation of patient safety by the nurses in
the inpatient rooms of two Puskesmas in Aceh. This comparative study employed the cross-sectional
design. All nurses at Puskesmas Pidie and Pidie Jaya, 65 nurses and 40 nurses respectively, involved in the
study. Using the independent t-test, the results show that there were no differences in the implementation of
patient safety (p = 0.322), patient identification (p=0.238), correct drug administration (p=0.889), absence
of errors in medical and nursing procedures (p=0.421), and infection prevention (p=0.388) in the two
puskesmas. Only in the prevention of patients from being injured was a difference observed (p=0.048). It is
necessary that the nurses improve their knowledge, skill, and motivation toward patient safety to increase
medical services at the Puskesmas.
1 INTRODUCTION
The issue of patient safety has become a global issue
since the Institute of Medicine (IOM) in the United
States published a paper titled "to Err Is Human:
Building A Safer Health System." Medication
errors have caused the death of 44,000 to 98,000
people every year. This figure is more than the
deaths caused by accidents, breast cancer and
Acquired Immune Deficiency Syndrome (AIDS). In
2004, The World Health Organization (WHO)
conducted a preliminary study in the United States,
Australia, New Zealand, Canada, and Europe and
learned that the incidence percentage of the patient
adversary was between3.2% and 16.6% in these
countries (Utarini, Getrud, & Hill.P, 2009).
The issue of patient safety at puskesmas is not as
dynamic as that of the hospital level. Patient safety
in puskesmas is only recently implied in the
Indonesian Ministry of Health Regulation Number
75, 2014 regarding puksemas. The regulation states
that puskesmas provides comprehensive,
sustainable, and quality primary health services and
carries out health services that prioritize the safety of
patients, health workers and visitors alike, which
was later included in the puskesmas accreditation
standard (as part of the accreditation standard for
first-level health facilities in addition to clinics and
private physician practice) (Permenkes RI, 2014).
The Ministry of Health Regulation No. 46, 2015
concerning Puskesmas Accreditation Standards
mentions clinical quality and patient safety in article
7, 11, 15, 16, and 17. However, no implementation
guide such as at that of hospital accreditation was
made (AIPKI, 2015).
Many incidences of patient safety in the
healthcare facilities were recorded in Aceh. Some
notable cases in 2016 include the blood transfusion
error performed by the nurse in Lhokseumawe
(Tribun News, 2016), the death of a baby in certain
hospitals laced by cables in incubators, the death of
the mothers and babies after surgery and other cases
136
Srimawati, ., Kamil, H., Marthoenis, ., Mutiawati R, E. and Tahlil, T.
The Implementation of Patient Safety by Nurses at Inpatient Rooms of Community Health Centers.
DOI: 10.5220/0008395500002442
In Proceedings of the Aceh International Nursing Conference (AINC 2018), pages 136-140
ISBN: 978-989-758-413-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
that cannot be brought up to the public. This study
aimed to learn the implementation of patient safety
by the nurses in the inpatient rooms of puskesmas in
Pidie and Pidie Jaya.
2 METHOD
This comparative quantitatif study used a cross-
sectional design. The data were collected through
surveys by distributing questionnaires to the
respondents. This study was conducted at two
Puskesmas (Public Health Center) in Pidie and
Pidie Jaya distric. The study population was the
nurses at one puskesmas in Pidie and one Pidie
Jaya with a total of 105 nurses using total sampling
tehnic. Independent t-test was then used for the
statistical analysis. Ethical committee of Nursing
Faculty, Syiah Kuala University had granted the
ethic for this study. The study used the following
ethical principles: respect for human dignity, respect
for jusctice inclusiveness,respect for privacy and
confidentialy
3 FINDINGS
3.1 Respondents Characteristics
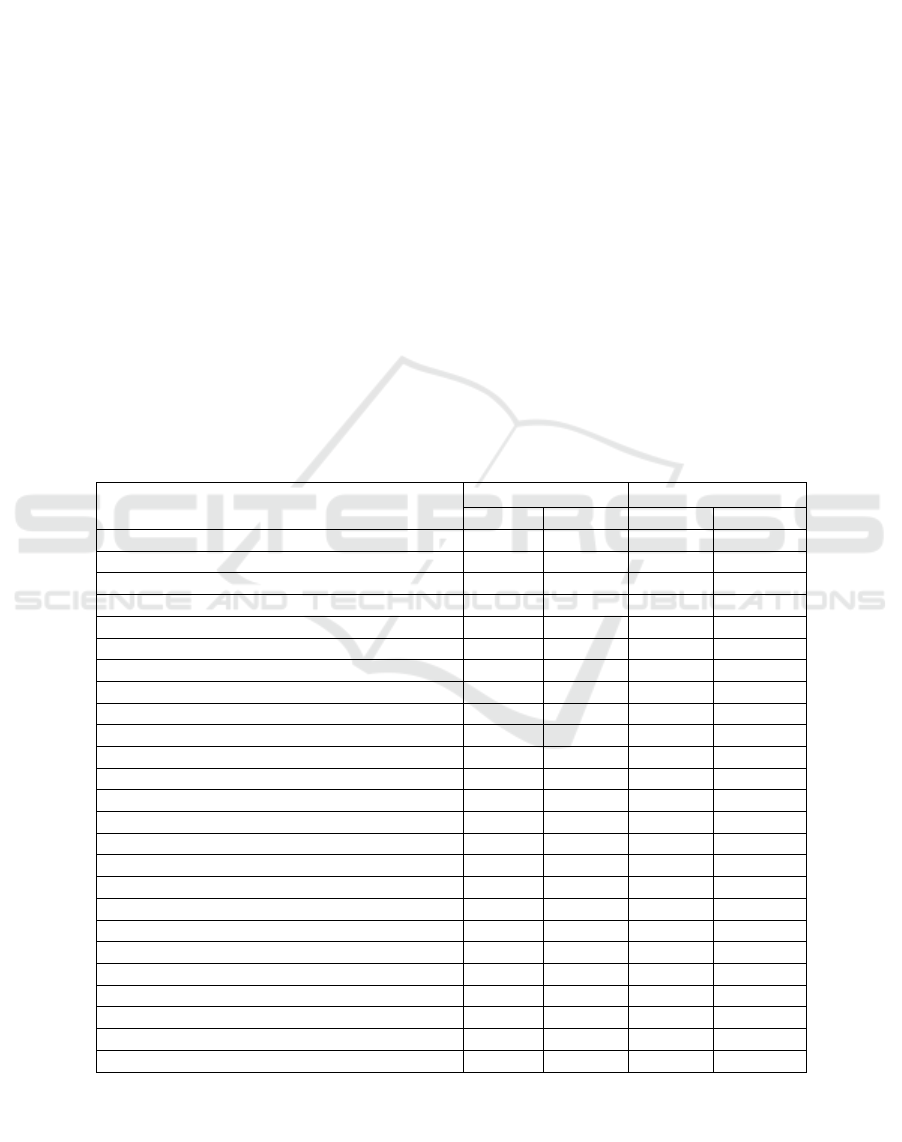
Characteristics of respondents include education,
age, gender, length of work and training attended by
the nurses (Table 1). The majority of the nurses had
an education Nursing Diploma, 38 people (95%) for
Pidie Puskesmas and 59 people (90.8%) for Pidie
Jaya Puskesmas. Most of the nurses were aged
between 20-35 years old, 31 people (77.5%) for
Pidie Puskesmas and 50 people (76.9%) for Pidie
Jaya Puskesmas. While Pidie Jaya Puskesmas
employed 55 female nurses (84.6%), Pidie
Puskesmas contracted only 30 female nurses (75%).
42 nurses (64.4%) at Pidie Puskesmas reported as
having 5 to 10 years experience while only 22 nurses
in Pidie Puskesmas had the equivalent length of
work. The The majority of the respondents, 33
nurses (82.5%) in Pidie Puskesmas and 60 nurses
(92.3%) in Pidie Jaya Puskesmas had not
participated in any training.
Tabel 1: Characteristics of Respondents.
Characteristics
PHC Pidie
PHC Pidie Jaya
f
%
f
%
Education
Nursing Specialist
1
2.5
4
6.2
Nursing Diploma
38
95.0
59
90.8
Bach.of Nursing+Nurse
1
2.5
2
3.1
Age
20 -35 years old
31
77.5
50
76.9
>35 years old
9
22.5
15
23.1
Gender
Male
10
25.0
10
15.4
Female
30
75.0
55
84.6
Length of Work Exp.
< 5 years
11
27.5
18
27.7
5 s/d 10 years
22
55.0
42
64.4
11 s/d 15 years
5
12.5
2
3.1
> 15 years
2
5.0
3
4.6
Training Participated
BTCLS
2
5.0
0
0
KESWA
0
0
1
1.5
MTBS
2
5.0
0
0
EKG
1
2.5
2
3.2
Infection Prevention
1
2.5
0
0
Resuscitation
0
0
1
1.5
HIV/AIDS
0
0
1
1.5
Rabies
0
0
1
1.5
No Training
33
82.5
60
92.3
The Implementation of Patient Safety by Nurses at Inpatient Rooms of Community Health Centers
137

Table 2: Implementation of Patient Safety
Variable / sub-
variables
PHC
Mean
Means
difference
95 % CI
P value
t value
Low
Up
Count
Table
Patient safety
Pidie Distrcit
141.95
2.112
-2.116
6.339
0.322
0.999
2.400
Pidie Jaya District
144.06
Patient
identification
Pidie District
30.93
-0.787
-2.100
0.527
0.238
-1.188
1.983
Pidie Jaya District
30.14
Correct drug
administration
Pidie District
42.90
0.100
-1.311
1.511
0.889
0.141
1.983
Pidie Jaya District
43.00
Absence of errors
in medical and
nursing
procedures
Pidie District
20.38
0.533
-0.780
1.845
0.421
0.810
1.996
Pidie Jaya District
20.91
Infection
Prevention
Pidie District
25.00
0.523
-0.675
1.721
0.338
0.866
1.993
Pidie Jaya District
25.52
No patient injured
Pidie District
22.75
1.650
0.016
3.284
0.048
2.021
2.001
Pidie Jaya District
24.40
3.2 The Implementation of Patients
Safety
The Implementation of patient safety is described in
Table 2. There is no difference in the
implementation of patient safety between nurses in
Puskesmas in Pidie and Pidie Jaya (p-value = 0.32).
The patient identification in Pidie Puskesmas (30.93)
was not significantly better compared to in Pidie
Jaya Puskesmas (30.14) (p-value = 0.24). The
implementation of correct drug administration in
Pidie Jaya Puskesmas (43.00) was not significantly
better compared to in Pidie Jaya Puskesmas (42.90)
(p-value = 0.89). The error-free practices in medical
and nursing procedures among nurses in Pidie Jaya
Puskesmas (20.91) was not significantly better
compared to in Pidie Puskesmas (20.38) (p-value =
0.42). The implementation of infection prevention
among nurses in Pidie Jaya Puskesmas (25.52) was
not significantly better compared to nurses in Pidie
Puskesmas (25.00) (p-value = 0.38). There is a
difference in the prevention of patients from being
injured between puskesmas in Pidie and Pidie Jaya
(p-value = 0.048).
4 DISCUSSION
Regarding the implementation of patients safety,
finding of this study shows that there was no
difference in the implementation of patient safety at
both puskesmas. The fact that all nurses in both
puskesmas have not participated in training about
patient safety contributed to the poor
implementation of patient safety. The absence of
training or socialization on patient safety also added
to the lack of nurses' knowledge on patient safety. A
study conducted at one public hospital in Banda
Aceh revealed that there is a correlation between
knowledge and the efforts to implement patient
safety (Dahliana, 2014). A similar study reported
that patient safety training influenced effective
communication, organizational climate, and patient
safety culture (Triana S, 2017).
In term of patients identification, the finding
suggests no difference in the implementation of
patient identification at the two puskesmas. Even
though the service area of puskesmas is limited,
errors in identifying patients are inevitable
considering every day tens or even hundreds of
patients visit these community health center. Patient
identification is one of the critical patient safety
standards. Errors during identification will lead to
medication, transfusion, test, and procedural errors
in the patient. The National Patient Safety Agency in
the UK reported 236 cases of errors which are
dangerously close to fatalities from November 2003
to July 2005 due to incorrect use of patient
identification bracelets (WHO, 2007). A study
conducted by Yudhawati & Listiowati (2015)
described that all nurses could identify patients,
explain the benefits of identity bracelets and specify
when patient identification is required. While 40%
of the patients knew the benefits of the wristband
AINC 2018 - Aceh International Nursing Conference
138

worn, only 20% of patients said that the nurses
checked the identity bracelet before carrying the
treatment. It means that the hospital nurses have not
carried out an efficient patient identification.
Result for correct drug administration shows that
there was no difference between the two puskesmas.
Properly administering drugs is important because
incorrect prescription may lead to, in the extreme
case, the death of the patient. A study conducted in
Sanglah General Hospital in Denpasar suggested
that there was a significant relationship between the
implementation of the six rights of medication
administration and the incidence of medication
errors (KresnaYana, 2015). Other study reported no
correlation between the nurses' level of education
and the length of work and the application of the six
right principles in administering drugs. Many other
factors influence the application of the six principles
right in administering drugs by the nurses.
Socialization, supervision, and training may help
affect nurses' motivation to apply the six right
principles (Armiyati, Ernawati, & Riwayati, 2007).
A study conducted at RSPN reported that 64.9%
of the nurses practiced the right patient, 86.5% of the
nurses practiced the right medication, 64.9% of the
nurses practiced the right time, and 100% of nurses
practiced the right dose, the right route, and
documentation (Stepani, Dewanto, & Dwiyanti,
2015). On the other hand, 89% of the inpatient
nurses at RSPN had good knowledge of seven right
principles. The nurses also had a positive attitude
toward the implementation of drug administration
based on seven rights and wanted to implement the
seven rights (Stepani, Dewanto, & Dwiyanti, 2015).
For the implementation of no medical and
nursing procedures errors, finding of this study
suggests that there was no difference between
puskesmas in Pidie Jaya and Pidie. Stetler et al.
(2000) and Hume (1999) showed that 10% to 18%
of reported hospital accidents were related to errors
in treatment. Errors in treatments were caused by
health workers such as doctors and pharmacists
(Mrayyan et al. 2007), and nurses were often the
health workers who made the most errors in terms of
treatment (Khasanah, 2012).
The result of the statistical analysis shows that
both puskesmas had no difference in the
implementation of infection prevention. The WHO
estimated that more than 1.4 million people
worldwide suffer from infectious diseases due to
hospitalization. Healthcare-associated infection
(HAI) reported that 5%-10% of patients in
developed countries suffer from nosocomial
infections. A study by HAI suggested that hand
hygiene can reduce the development of infection.
Hand washing is an essential measure in preventing
infection (WHO, 2007a). Kurniawati, Satyabakti,
Arbianti (2015) reported that health workers who
ignored hand hygiene had a risk of experiencing
multidrug resistance organisms (MDROS) 6,000
times more than those who did otherwise. A total of
42 out of 100 health workers who treated patients in
the intensive care unit (ICU) could avoid MDROS
infection if they care to wash their hand properly and
could prevent 0.42 out of 0.67 or 62.60% of
MDROS infections (Kurniawati, Prijono, & Novita,
2015).
Based on the statistical test, a difference was
observed in the patient prevention from being
injured between the puskesmas in Pidie Jaya and
Pidie. Even though the difference was observed, the
implementation of the patient prevention from
falling in both puskesmas has not reached its best
due to the lack of socialization about this safety
measure. A study conducted in one of the hospitals
in Malang (Budiono, Alamsyah, & Wahyu, 2014)
revealed that after nurses received training and
socialization about the management of patients at
risk of falling and implemented the procedure for
two weeks, the care of nurses to screen patients at
risk of falling increased to 26.5%. The nurses later
put on the identification bracelets and educated both
patients and families about their risk of falling. The
prevention of falling injuries in every health service
can be performed from patient entry to discharge.
Preventing patients from falling is made to provide
safe nursing services to the patients (Budiono,
Alamsyah, & Wahyu, 2014).
5 CONCLUSION
The current study found that there were no
differences in the implementation of patient safety
with the p-value of 0.322, patient identification with
the p-value of 0.238, correct drug administration
with the p-value of 0.889, absence of errors in
medical and nursing procedures with the p-value of
0.421, and infection prevention with the p-value of
p=0.388 in the two puskesmas. The difference was
observed in the prevention of patients from being
injured with the p-value of 0.048. All nurses are
expected to improve their knowledge and motivation
and take part in patient safety training to increase
medical services at the Puskesmas.
The Implementation of Patient Safety by Nurses at Inpatient Rooms of Community Health Centers
139

REFERENCES
AIPKI. 2015. Modul pelatihan untuk Pelatih Keselamatan
pasien. Jakarta.
Armiyati, Y., Ernawati, & Riwayati.2007. Hubungan
Tingkat Pendidikan Dan Lama Kerja Perawat Dengan
Penerapan Prinsip “ Enam Tepat ” Dalam Pemberian
Obat Di Ruang Rawat Inap RS Dr. Kariadi Semarang.
Retrieved from http/jurnal.Unimus.ac.id
Budiono, S., Alamsyah, A., & Wahyu, T. S. 2014.
Pelaksanaan Program Manaejemen Pasien Dengan
Resiko Jatuh di Rumah Sakit. Jurnal Kedokteran
Brawijaya, Volume 28.
Dahliana, D. 2014. Hubungan pengetahuan Perawat
dengan Upaya Penerapan Patient Safety di Ruang
Rawat Inap Rumah Sakit Umum Daerah DR. Zainnoel
Abidin Banda Aceh. Idea Nursing Jurnal, V0lume VII.
Khasanah, U.2012. Tindakan Error Prosedur
Keperawatan : Jenis Dan Faktor Penyebab Pada
Mahasiswa Profesi Ners. Jurnal Ners, volume 7.
KresnaYana, I. 2015. Hubungan pelaksanaan prinsip enam
benar terhadap insiden medication errors (kesalahan
pemberian obat).
Kurniawati, A. F., Prijono, S., & Novita, A. 2015.
Perbedaan Resiko Multidrug Resistance Organisms
(MDROS) menurut faktor Resiko dan Kepatuhan Hand
Higiene,. Jurnal Berkala Epidemilogi, Volume 3 ,.
Permenkes RI. 2014. Tentang Pusat Kesehatan
Masyarakat. Nomor 75 tahun 2014.
Stepani, P., Dewanto, A., & Dwiyanti, C. 2015. Faktor
Penghambat Pelaksanaan SPO 7 Benar dala Pemberia
Obat di Ruang rawat Inap Rumah Sakit Panti Nirmala.
Jurnal Kedokteran Brawijaya, Volume 8.
Triana S, R. 2017. Pengaruh Pelatihan Terhadap
Ketrampilan Komuniksai Efektif Patient Safety,
Budaya Keselamatan dan Iklim Organisasi Pada Staf
RSUD Kabupaten Kepulauan Mentawai. Universitas
Gajah Mada Yogyakarta.
Tribun News. (2016). Tiga Perawat Rumah Sakit Arun di
Non Aktifkan. Di Unduh Pada Tanggal 16 Desember
2016,. Retrieved from
http://aceh.tribunnews.com/2016/04/07/3-perawat-rs-
arun-dinonaktifkan
Utarini, A., Getrud, & Hill.P. (2009). Hospital Mangement
Training New Ways to Improve Service in Indonesia.
jakarta: GTZ.
WHO. (2007). Patien Safety Solution Preamble. Di Unduh
Pada Tanggal 20 Juli 2016. Retrieved from
http://www.who.int/patientsafety/events/07/02_05_200
7/en/
Yudhawati, D. D., & Listiowati, E. (2015). Evaluasi
Penerapan Identifikasi Pasien Di Bangsal Rawat Inap
RSI Siti Aisyah Madiun. Program Pasca Sarjana
Inversitas Muhammaddiyah Yogyakarta.
AINC 2018 - Aceh International Nursing Conference
140
