
Restraint in Psychiatric Patients: A Literature Review
Sri Novitayani
1
, Aiyub
1
, Maulina
1
and Martina
1
1
Department of Psychiatry and Mental Health Nursing, Faculty of Nursing, Syiah Kuala University, Darussalam, Banda
Aceh, 23111, Indonesia
Keywords: Restraint, Violent Behavior, Psychiatric Illness, Schizophrenia
Abstract: Nowadays, many cases of violence in psychiatric patients visit to psychiatric emergency unit. Restraint is
basically efficacious in managing violence. So, it also can prevent injuries to both the patient and those
around the patient. This literature review explores the positive and negative effect of restraint, criteria for
using restraint, guideline of restraint and standard documentation of restraint. Twenty papers were selected
from electronic database of ProQuest, Pumed, Google Scholar and Google web site. A literature review of
these papers showed that restraint can manage violent behavior, but it has physical and psychological
negative impacts on psychiatric patient. In this review, it also explores about criteria using restraint based on
JCAHO, APNA, and Department of Health for England and Wales; standard of restraint provide by
JCAHO, APNA, Department of Health for England and Wales, and Park and Tang; and standard
documentation for restraint by JCAHO, APNA, Park and Tang, and Reeves. We sum up that it is important
for nurse to use appropriate techniques for restrain dan standard or guideline of restraint in order to prevent
the negative impact of restraint and ensure the patients safety. Another important thing that must be
considered by nurses is the standard documentation for restrain.
1 INTRODUCTION
Violence is act by someone or group to harm other
with physical or threatened that may cause from
such problem as disordered or paranoid thinking and
belief, substance intoxication, or anger (Mohr,
2009). Violence can be danger to other or harm
himself. According to retrospective study by Schory,
Piecznski, Nair, and El-Mallakah (2003), it reported
3804 person from 4717 person who visit to
emergency psychiatric service are with violence act.
Aggresive behavior and violence are seriously
emergency that can be difficult to cope by staff in
mental health hospital (Wynn, 2002). Based on
Fortinash (2007), there are two interventions in
psychiatry emergency on patient with violence or
aggressive behavior, including verbal intervention
and restrain intervention. Verbal intervention is
important intervention when interacting with client
whose behavior is escalating as a result of conflict,
regardless of the reason and it use to prevent
escalation of aggressive behavior or violence (Mohr,
2009). While the patient express a severe aggressive
behavior or violence and the nurse cannot control it
by using verbal intervention or other intervention,
the nurse have to use restraint intervention, such as
pharmacological restraint, physical restraint, or
seclusion (Wynn, 2002). Stuart (2013) stated that the
nurse needs to use restraint as nursing interventions
in managing violent behavior on psychiatric patients
in range of detention strategy.
According to retrospective study at a Norwegia
university hospital during a five and a half year
period (January 1989 to June 1994) by Wynn
(2002), there were 797 episodes of physical restraint,
384 episodes of chemical restraint, and 88 episodes
of seclusion. Another study by Reitan, Helvik and
Valentina (2018) is also found that there were 863
cases with mechanical restraint and 595 cases with
chemical restraint during 7 years period (January
2004 to December 2011). So, the physical or
mechanical restraint was used higher than chemical
restrain and seclusion. Restraint intervention is a
necessary intervention to ensure safety to other and
patient from patient who has escalation aggressive
behavior or violence (Mohr, 2009).
Even though the restraint can prevent the patient
to harm other or him/her self, it can cause physical
trauma, emotional trauma, or sometime death
(National Executive Training Institute as cited in
234
Novitayani, S., Aiyub, ., Maulina, . and Martina, .
Restraint in Psychiatric Patients: A Literature Review.
DOI: 10.5220/0008396900002442
In Proceedings of the Aceh International Nursing Conference (AINC 2018), pages 234-241
ISBN: 978-989-758-413-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Mohr, 2009). The patient can be death during
restraint because inappropriate device application or
lack of monitoring (Abrahamsen, 2001). The
Hartford Courant series reported that 142 human
who experienced restrain or seclusion was death in
the previous 10 years (Office of the Ombudsman for
Mental Health and Mental Retardation, 2002). The
staffs or nurses need guideline for restrain to prevent
death for patient who gets restraint.
There are some guidelines or standards on
restraint and seclusion that provide by some
organization, such as the Joint Commission on
Accreditation of Healthcare Organization (JCAHO),
the American Psychiatric Nurses Association, The
National Institute for health and Clinical Excellence
(NICE), the British Institute of Learning Disabilities
(BILD), etc. They have different form to explain the
guideline. However, they have similar focus on the
point that important as standards or guideline in
restraint and seclusion. All of these guidelines have
purpose to ensure client safety and can prevent the
negative effect of restraint, such as death. So, it is
important to know various of guideline and compare
it which one is more complete.
2 METHODS
Data were collected through ProQuest data base,
Pumed data base, Google Scholar, and Google web
site. The following terms that used to search the
literature reviews are restraint, effectiveness of
restraint on violent behavior, physical restraint,
impact of restraint, negative effect of restraint,
physical effects of restraint, psychological effects of
restraint, criteria using restraint, guideline of
restraint, guideline for physical restraint, and
standard documentation for restraint
There are several objectives in this literature
review as the following:
To identify benefit of restraint;
To identify negative impact of restraint;
To identify criteria for using restrain;
To describe standard of restraint;
To describe standards of documentation for
restraint.
2.1 Inclusion Criteria
The selected papers in this literature review had one
or more criteria as the following:
Discuss about restraint in psychiatric field;
Discuss about negative effects of restraint;
Discuss about criteria for using restraint;
Discuss about guideline of restraint;
Discuss about standard documentation for
restraint;
Written in English or Indonesian.
Those papers were not restricted in the year of
publication. However, each article was confirmed to
be related to a restraint.
2.2 Exclusion Criteria
Papers that discussed restraint on psychiatry health
problem which is not focused on violent behavior,
and physical health problem were excluded in this
literature review. We also excluded papers about
restraint in nursing homes and community.
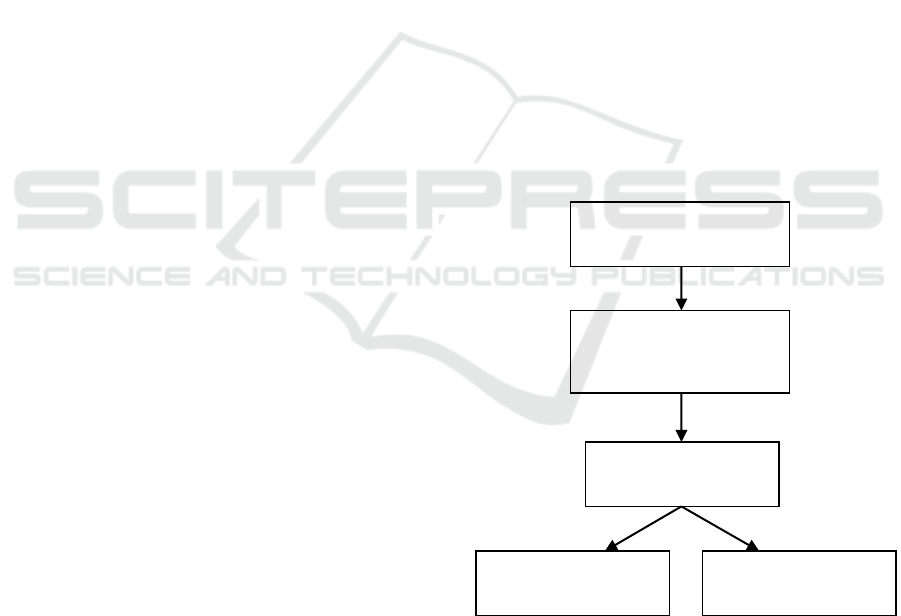
2.3 Selection of the Studies
Initially, we found 51 papers while we searched
from electronic data based. Moreover, we excluded
23 papers after reading the title and abstract. After
fully reading 28 papers, there were excluded 8
papers because they did not meet inclusion criteria
and had exclusion criteria. Finally, twenty papers
were relevant.
Figure 1: Flow diagram of article selection process
56 papers were found
in firstly searches
28 papers were
excluded after reading
title and abstract
28 papers fully
reading
9 papers were
excluded
19 papers were
relevant
Restraint in Psychiatric Patients: A Literature Review
235

3 FINDINGS
3.1 Effectiveness of Restraint
According to several studies, the results showed that
restraint was effective in reducing violent behavior
among psychiatric patient (Saseno & Kriswoyo,
2013; Sulistyowati & Prihantini, 2014). In study by
Saseno and Kriswoyo, after schizophrenic patients
with violent behavior received mechanical restraint,
the violent behavior was observed by using chek list
of The Violent Behavior Observation Questionnaire.
It showed the violent behavior of all respondents
was decreased.
Moreover, study that developed by Sulistyowati
and Prihantini (2014) used physical and/or
mechanical restraint to manage violent behavior
among schizophrenic patients with violence. In that
study, the result showed that the restraint had
significant effect to reduce behavioral, emotional,
and verbal response related to aggression. The final
result was proved that the restraint effectively
reduced violent behavior.
The results from those studies are in accordance
with purpose of restraint that is controlling the
patient’s violent behavior (Poniatowski, 2000). So, it
can prevent injury to patient, nurse and others.
3.2 Negative Impacts of Restrain
Even thought restraint has effect to manage violent
behavior, it also has physical and psychological
reaction as negative impact to Psychiatric patients.
3.2.1 Physical Impacts
Several papers in this literature review found that
psychiatric patients experienced physical negative
impact after receiving restraints, especially physical
and/or mechanical restraint. According to qualitative
study by Asher et al. (2017), the result reported that
the psychiatric patients experienced physical injury
after being restrained. In addition, pressure sores and
abrasion also occur in psychiatric patients with
restraint by nurse (Kalula & Petros, 2016). Physical
injury and /or abrasion on patient could be happen
because of the attachment of the strap to physical
restraint that is too tight (Saputra, 2017).
Furthemore, Kandar and Pambudi (2014) found
physical discomfort, abrasions on the mounting area
of restrain, urinary incontinence, ineffective
circulation, risk of contractures and skin irritation
were some physical effects toward restraint based on
their observation on psychiatric patient as
respondent. Most of nurses (79.7%) reported that
skin breakdown was experienced by psychiatric
patients who were being restrained (Gandhi et al.,
2018).
Next, study by Kamel, Maximos, and Gaafar
(2007) showed that psychiatric inpatients who
received physical restraint had general body aches
and severe pain in extremities. Beside body aches,
psychiatric patient with violence reported that
physical discomfort during having restraint (Saputra,
2017). Moreover, Abrahamsen (2001) assumed that,
strangulation, muscle loss, bone weakness,
pneumonia, contractures, urinary incontinence and
retention, and death were potential problem while
use restraint.
A review paper by Mohr, Petti, and Mohr (2003)
proved that restraint caused death to psychiatric
patient by several reasons, such as aspiration, blunt
trauma to the chest, etc. Milliken (1998) mentioned
that deaths are reported due to using vest type
restraint and bed rails, being tied to a prone position
toward young people, and using choke holds on
restraint in prone position.
3.2.2 Psychological Impacts
Based on literature review, there are psychological
impacts on psychiatric patient toward physical or
mechanical restraint. Qualitative study by Asher et
al. (2017) reported that respondent who is being
restrained had increased the risk of violence toward
others and felt hopeless. The risk of violence could
be happen because the patients cannot accept that
they were restrained and angry with the person who
caused him to be restraint. Mostly, the psychiatric
patients’ anger increased while the nurse was doing
restraint to them and they experienced aggressive
after receiving restraint (Kandar & Pambudi, 2014).
Moreover, feelings hopeless could be occurred on
the patients while they had been restrained and
keeping them in the room for long time. Another
study found that humiliation, worthlessness, rage,
resentment, sadness, despair, as well as injustice, felt
guilty, and fear insecurity were the psychiatric
patients’ feeling during restraint (Kamel, Maximos,
& Gaafar, 2007). Similar result also found in study
by Lanthen, Rask, and Sunnqvist (2015) that stated
mechanical restraint may affect powerlessness,
feelings of unreality, anger, and fear on psychiatric
patient who received it. In that study, fear usually
occurred to the patients because of a sense about
what was going to happen next and how long the
mechanical restraints would attach to their body.
Moreover, while the patients were being excluded or
AINC 2018 - Aceh International Nursing Conference
236

exposed form the others; it was partially connected
to their feeling of insecurity.
3.3 Criteria for Restrain
Based on these papers, there are four organizations
(the Joint Commission Accreditation of Health Care
(JCAHO), American Psychiatric Nurse Association
(APNA), Department of Health for England and
Wales) and one of evidence based guideline (Park
and Tang, 2007) have explore about criteria for
using restraint.
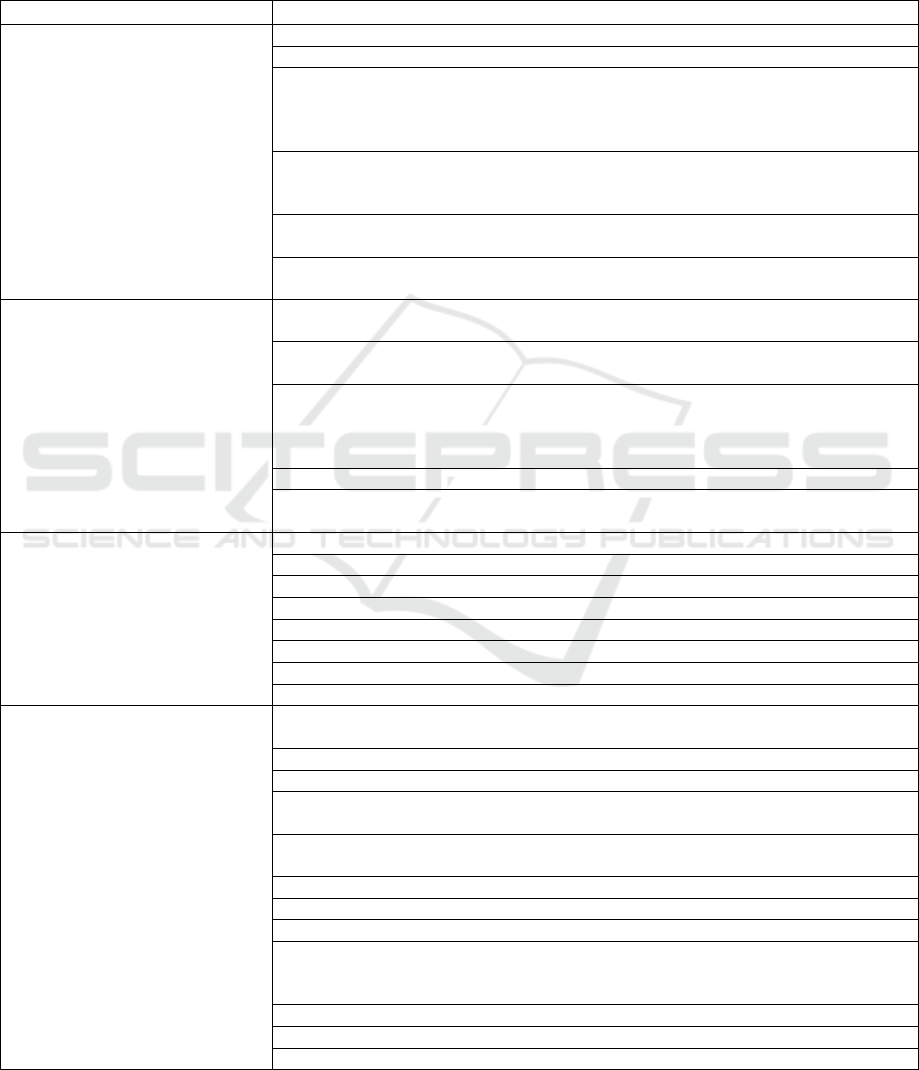
Table 1: Criteria for restraint based on organizations.
Organizations
Criteria
JCAHO
(Crisis Consultant Group,
2011)
Use restraint only to protect the immediate physical safety of the patient, staff, or others
Do not use restraint as a means of coercion, discipline, convenience, or staff retaliation
Use restraint or seclusion only when less restrictive interventions are ineffective
Use the least restrictive form of restraint that protects the physical safety of the patient,
staff, or others
Discontinue restraint at the earliest possible time, regardless of the scheduled expiration
of the order
APNA
(APNA, 2007)
Restraint used only when less restrictive measures have proven ineffective and the
behavioral emergency poses serious and imminent danger to the person, staff or others
Restraint should not be used as a means of coercion or punishment, for the convenience
of the staff, or when less restrictive measures to manage behaviors are available
The risks and benefits considered must include an individualized assessment of the
person’s known history of physical or sexual abuse as well as current physiological and
psychological status
Department of Health for
England and Wales
(Horsburgh, 2003)
When other strategies have failed; even when restraint is required
It should comprise one component of an overall care plan for the service user and in an
emergency situation when the risk of inaction outweighs the risks of restraint
Park and Tang (2007)
Using restraint only after assessment of the patient, the environment, and the situation
have been completed
Precipitating factors have been identified and eliminated whenever possible
Consultation with other health care professionals have occurred
A physician’ a order for use of restraints has been attained
Interventions to relieve discomforting behaviors have been used
According to these criteria for using restraint, the
criteria of restraint by JCAHO, APNA, Department
of Health for England and Wales, and Park and Tang
have almost similar criteria. From those criteria,
there are some important things to consider using
restraint on psychiatric patient with violence. Firstly,
restraint is used only to protect the patient, staff, or
other from imminent danger after the less restrictive
used before is ineffective to control the patient’s
behavior. In study by Saseono and Kriswoyo (2013),
while the psychiatric patients had experienced
raging behavior, threatening, trying to hurt himself
or others, talking harshly, insulting others,
demanding, angry, unstable, tense expressions, sharp
eyes, red faces and high blood pressure, the nurses
did restraint on these patients. The reason for doing
restraint by the nurses in that study was because
those behavior of the patients showing the imminent
danger. Several least restrictive interventions can
used to control violent behavior before deciding to
use restraint. There are anger control assistance,
cognitive intervention, behavior intervention,
thought stopping, and biological intervention
(Kamel, Maximos, & Gaafar, 2007).
Secondly, use of restraint on the patient has
ordered by physician and has been consulted with
other health care professionals. Generally, nurse
uses restraint on psychiatric patient with violence
without physician’s instruction. In this situation, if
the nurse does not restraint the patient, it will be
danger to the patient and the others. So, restraint can
be given without instruction by a physician while it
is in emergency and should be given in order to
prevent imminent danger to patient and others
(Australian Capital Territory (ACT), 2011).
The last point, the nurse must conduct a
complete assessment to the patient, the environment,
and the situation. However, it cannot be done by
nurse in emergency situation. Usually, the complete
assessment will be done after the psychiatric patient
with violence is being restraint. All of the
information should be documented.
Restraint in Psychiatric Patients: A Literature Review
237
3.4 Guideline of Restrain
This literature review, the standards of restraint will
provide by JCAHO, APNA, Department of Health
for England and Wales, and Park and Tang.
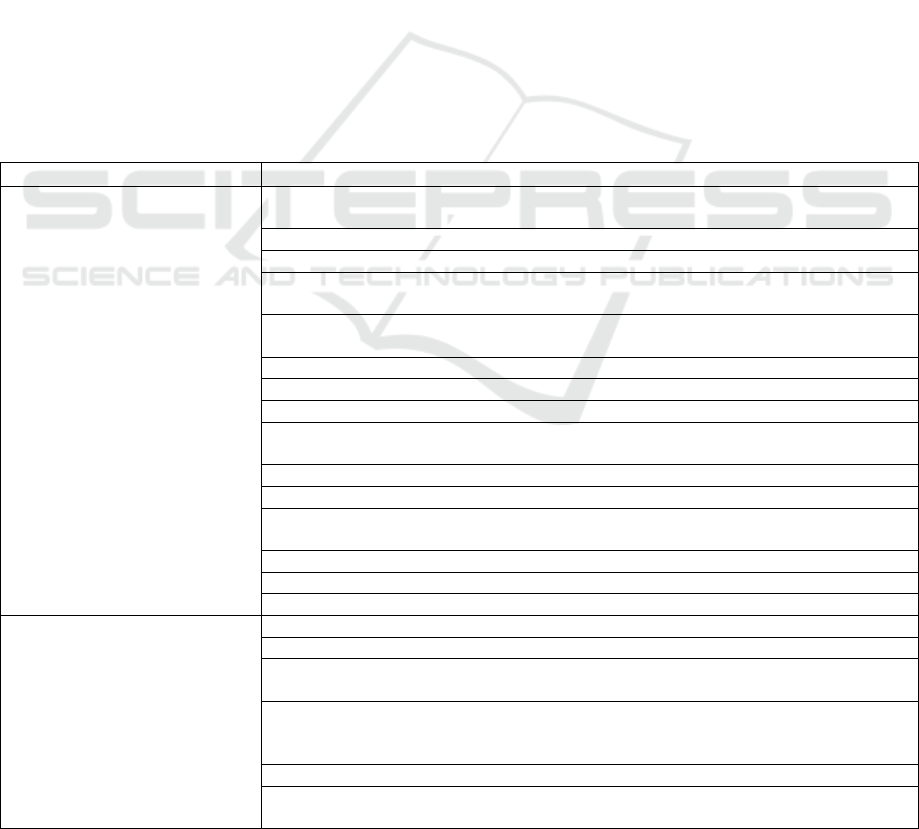
Table 2: Standard of restraint based on organizations.
organizations
Elements
JCAHO (Crisis Consultant Group,
2011)
the staff or nurse using restraint or seclusion with safe technique
the hospital or organization initiates restraint or seclusion based on an individual order
the time limits for a maximum of 24 consecutive hours (it means the staff Licensed
Independence Practitioners (LIP) primarily responsible for the patient’s ongoing care
sees and evaluates the patient before writing a new order for restraint or seclusion
used every 24 hours)
the time limit of restraint is longer (4 hours) for adult with 18 years old or older than
children and adolescents with 9 to 17 years old (2 hours), and children with under 9
years old (1 hour)
the staff evaluates and reevaluates the patient who is restrained or secluded and he/she
has licensed independent practitioners or staff who have been trained
they evaluate a patient through face to face within one hour of the initiation of
restraint
APNA (APNA, 2007)
clear explanation to the person of the reason for restraint and the behavioral criteria
for release
the physician, LIP, or RN must see and evaluate a patient through face to face within
one hour of initiation of restraint
monitoring and assessment a client in restraint every 15 minutes to ensure the patient
safe (eg. sign of injury, psychological and psychological status, nutrition, hydration,
skin integrity, circulation,, hygiene, eliminate, physical discomfort or emotional
distress)
range of motion exercises must be performed every two hours
the RN or LIP release the restraint as soon as possible while the behavioral criteria are
met
Department of Health for England
and Wales (Horsburgh, 2003).
restraint should be used only the minimum amount of force
the shortest duration of time
in the best interest of the service user and/or to prevent harm to third parties
doing by staff who have received specialist training
in a way to minimize the risk of physical injury and loss of dignity
ensuring avoidance of contact that could be construed as sexual
with subsequent debriefing for staff and the service user
with formal recording and reporting of the incident
Park and Tang (2007)
contraindications to physical restraints should be assessed on a case by case prior to
restraint use
the patient should have access to call bell
patient’s behavioral status and need for restraints must be frequently assessed
the patient and care giver should be notified promptly and have the restrictive
intervention explained to them in a manner that can be understood
informed consent from the patient or the care giver should be obtained within 24
hours after implementation of restrictive procedures for them to be continued
patients have to monitor continually and their needs must be attended to
protecting the patient or staff from imminent injury
restrictive interventions may be implemented be authorized staff
the staff should be removed as soon as possible after target behavior is diminished or
disappears and criteria for discontinuation include improved mental status (most
frequent)
capacity to adhere to a contract related to expected behavior
availability of direct supervision
discontinuation of tubes or lines
AINC 2018 - Aceh International Nursing Conference
238
According to this review on standard for
restraint, the standard by JCAHO, APNA, and Park
& Tang have similar. They focus on evaluation and
reevaluation that include the time frame and the item
of evaluation, monitoring that include the time frame
and items of concern to monitor, criteria for release
restraint, and only LIP, RN, Physician and the staff
who have been trained restraint can do restraint and
take care the patient in restraint. However, the
JCAHO has explored more detail than others; the
JCAHO was mentioned the limit time of restraint for
patient according to age. Moreover, standards by
Department of Health for England and Wales did not
clearly explore the guideline or the standard, such as
not mention about the time for evaluation and
monitoring, etc.
According to Poniatowski (2000), the RN or LIP
assess some physical assessment for a patient
immediately after getting restraint and every 15
minutes such as signs of injury related to restraint,
the needs such as nutrition or hydration, circulation
and range of motion in the extremities, hygiene and
elimination.
3.5 Standard Documentation for
Restrain
From this literature review, there are standards
documentation for restraint by JCAHO, APNA, Park
& Tang, and Reeves. According to four standards of
documentation, there are quite similar. However, the
standard by Park and Tang does not complete like
the standard of documentation by JCAHO, APNA,
and Reeves. The standard documentation for
restraint that is more complete than other is the
standard by Revees. Revees mixed it from another
guideline from different organization. Reeves (2011)
provide 19 elements of standard documentation for
restraint after Reeves combine from many elements
of standard documentation for restraint by some
organization, such as The National Institute for
health and Clinical Excellence (NICE), the British
Institute of Learning Disabilities (BILD), The
National Institute for Mental Health in England, The
Code of Practice for the Mental Health Act, The
SIRCC and Smallridge and Williamson.
Table 3: Standard documentation for restraint based on organizations.
Organizations
Elements
JCAHO (Crisis Consultant
Group, 2011)
Any in-person medical and behavioral evaluation for restraint or seclusion used to
manage violent or self-destructive behavior
A description of the patient’s behavior and the intervention used
Any alternatives or other less restrictive interventions attempted
The patient’s condition or symptom(s) that warranted the use of the restraint or
seclusion
The patient’s response to the intervention(s) used, including the rationale for continued
use of the intervention
Individual patient assessments and re-assessments
The intervals for monitoring
Revisions to the plan of care
The patient’s behavior and staff concerns regarding safety risks to the patient, staff, and
others that necessitated the use of restraint or seclusion
Injuries to the patient
Death associated with the use of restraint
The identity of the physician or other licensed independent practitioner who ordered the
restraint or seclusion
Orders for restraint or seclusion
Notification of the use of restraint or seclusion to the attending physician
Consultations
APNA (APNA, 2007.
The events and behavior that led to the use of seclusion or restraint
Non-physical interventions that were attempted and the person’s response
All necessary notifications of attending physicians, LIP, guardian and, if such
notification is designated by the person, the caregiver or significant other
Specifics of the episode, when it was initiated, specific physical holds and evaluation of
the person’s response to the physical interventions including any potential for
complication or injury
Monitoring and assessment of the person while in seclusion or restraint
Interventions provided to promote comfort and safety as well as expedite release and
the person’s response
Restraint in Psychiatric Patients: A Literature Review
239
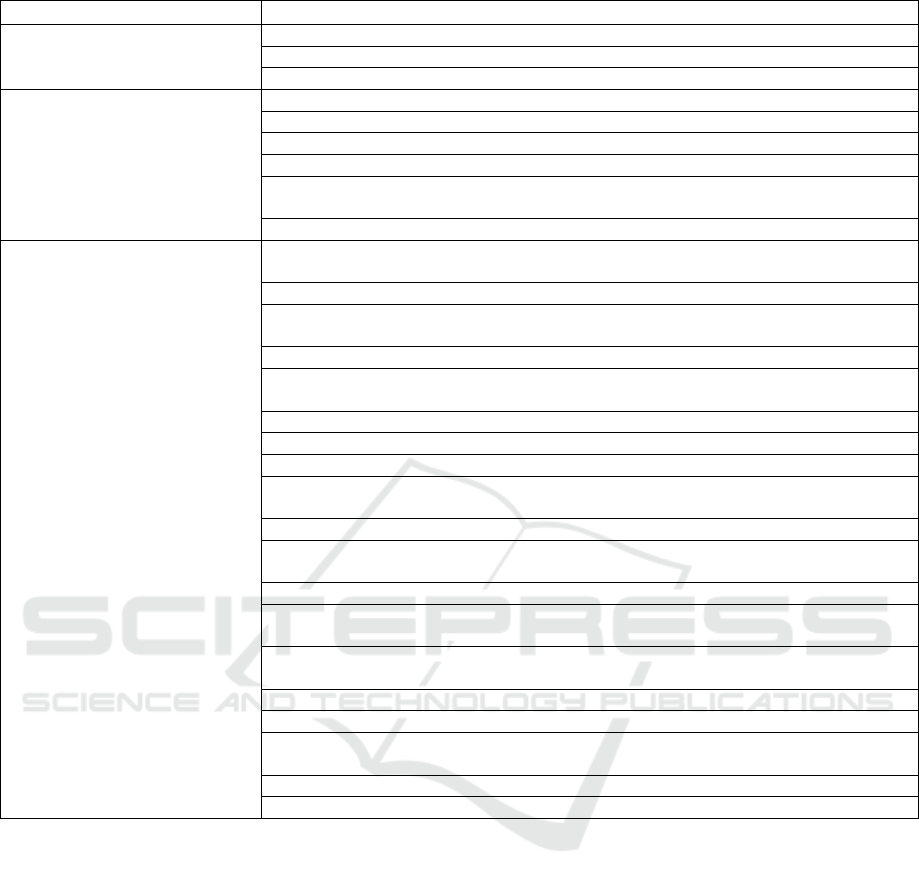
Organizations
Elements
Criteria for release and data used to determine that the person met these criteria
Time of release from seclusion or restraint
Debriefing with the person and caregivers as indicated
Park and Tang (2007)
Type of restraint used
Substance of explanations given to the client and support persons
Exact times the restraint was applied and removed
Client’s behavior while the restraint was applied
Frequency of care given while the restraint was applied and removed (such as
assessment of circulation, range of motion exercise)
Notification of the physician
Reeves (2011)
All people involved in or witness to any stage of the incident, including staff, clients
and visitors, with a full description of their involvement
The restraint training received by staff directly involved in the incident
All events leading up to the incident, including details of the behavior of the client and
the response of staff or others to this behavior
The time and location of the incident
Any alternative strategies that were followed or attempted and any deviations from
relevant plans of care
The reasons why physical interventions were used and the risks involved
The methods of restraint used, including positions and types of hold
The duration of each restraint
Any deliberate application of discomfort or pain, including in breakaway or
disengagement techniques, and justifications for this
All physical observations taken during or after the incident
Any difficulties in monitoring the client’s physical wellbeing and any action taken to
manage these difficulties
How the restraint came to an end
The use of and reasons for rapid tranquillisation, its beneficial or adverse effects, and
justifications for any doses exceeding British National Formulary limits
Additional actions taken or recommended and justifications for any changes in
observation levels
Any injuries to the client, staff or others, and treatments or attention received
Any distress experienced by the client or others, and attention or support received
All those informed of the incident, including managers, medical staff and family or
carers
Any police involvement during or after the incident
Any debriefing of clients, staff or others after the incident
4 CONCLUSIONS
Most person come to the hospital with violence
action and need restraint to prevent them harm other
or him/her self after the other intervention cannot
success or they are not cooperative. To ensure the
patient safety in restraint, it needs standard for
restraint. There are many standards for restraint,
such as the standard for restraint by JCAHO, APNA,
Department of Health for England and Wales, Park
& Tang, and Revees. Every guideline have different
strengthen and weakness. Actually, these standards
have similar, but different way in explore it.
To ensure the patient safety in restraint, not only
focus on the guideline, but also focus on the nurse,
physician and staff who will provide the restraint.
They have trained in restraint program. Moreover,
they have carefully and follow the guideline to make
the patient and others safety, and also to prevent the
negative effect of restraint. Even though the hospital
or organization has a good guideline for restraint, it
is important for director of hospital or organization
to evaluate the nurse follows the guideline of
restraint and seclusion or not. Guideline of restraint
is so important to make safety for the patient and
staff or nurse.
REFERENCES
Abrahamsen, C. (2001). 2002 guide to new technology-
patient restraint: JCAHO and HCFA isuue new
restraint guideline. Nursing Management, 32(12), pp.
69-70
AINC 2018 - Aceh International Nursing Conference
240

Asher, L., Fekadu, A., Teferra, S., Silva, M. D., Pathare,
S., and Hanlon, C. (2017). “I cry every day and night,
I have my son tied in chains”: Physical restraint of
people with schizophrenia in commuity settings in
Ethiopia. Globalization and Health, 13, (47), pp. 1-14.
doi.101.1186/s12992-017-0273-1
Asutralian Capital Territory. (2011). Standard operating
procedure restraint of patient. Australia: Australia
Capital Territory (ACT).
Crisis Consultant Group, LCC. (2011). The Joint
Commission Standars on Restraint and Seclusion
Fortinash, K.M. 2007. Psychiatric nursing care plans. (5th
ed.). St. Louis: Elseiver
Gandhi, S., Poreddi, V., Nagarajaiah, Palaniappan, A.,
Reddy, S.S.N., and Badamath, S. (2018). Indian
nurses’ knowledge, attitude and practice towards use
of physical restraints in psychiatric patients.
Investigacion Education Enfermeria, 36, (1).
Horsburgh, D. (2004). How, and when, can I restrain a
patient?. Postgrad Medical Journal,80, pp. 7-12
Kamel, N.M.F., Maximos, M.H.F., and Gaafar, M.M.
(2007). Reactions of patients and psychiatric hospital
staff about physical restraint. Alexandria Scientific
Nursing Journal, 6 (2), pp. 1-22
Kalula, S. Z., and Petros, S. G. (2016). Use of physical
restraint in hospital patients: A descriptive study in
tertiary hospital in South Africa. Curationis, 39 (1)
Kandar and Pambudi, P. S. (2014). Efektivitas tindakan
restrain pada pasien perilaku kekerasan yang
menjalani perawatan di unit pelayanan intensif
psikiatri (UPIP) RSJ Daerah Dr. Amino Gondohutomo
Semarang 2013 [The effectiveness of restraint on
patients with violent behavior who undergo treatment
in the psychiatric intensive care unit Regional Mental
Hospital Dr. Amino Gondohutomo Semarang 2013].
In prosiding konferensi nasional II PPNI Jawa Tengah
2014
Lanthen, K., Rask, M., and Sunnqvist,C. (2015).
Psychiatric patients experiences with mechanical
restraints: An interview study. Psychiatry Journal.
Milliken, D. 1998. Death by restraint. Canadian Medical
Association Journal, 158(12), pp. 1611-1612
Mohr, W. K. (2009). Psychiatric mental health nursing
evidence based concepts, skills, and practices. (7 th
ed.). Philadelphia: Lippincott Williams & Wilkins.
Mohr, W. K., Petti, T. A., and Mohr, B. D. (2003). Review
paper; Adverse Effects associated with physical
restraint. The Canadian Journal of Psychiatry, 48 (5),
pp. 330-337
Office of the Ombudsman for Mental Health and Mental
Retardation. (2002). www.ombudmhdd.state.mn.us
Park, M., and Tang, J.H.C. (2007). Evidence-based
guideline: Changing the practice of physical restraint
use in acute care. In M.G. Titler (Series Ed.). Series on
evidence-based practice for older adults. Iowa
College, Iowa: University of Iowa College of Journal
of Gerontological Nursing Interventions Research
Center, Research Translation and Dissemination Core.
Poniatowski, L. (2000). Revisions cut restraint risk.
Nursing Management, 31(10)
Reeves, J. (2011). Guideline for recording the use of
physical restraint. Mental Health Practice, 15(1), pp.
22-24
Saputra, D. (2017). Pengalaman pasien gangguan jiwa
selama mengalami restrain extremitas di rumah sakit
jiwa arif zainudin Surakarta [Experiences of Patients
with Mental disorder during restraint extremity in the
Mental Hospital Arif Zainudin Surakarta](published
undergraduate’s skripsi). Fakulty of Health Science,
Muhammadiyah Surakarta University, Indonesia.
Saseno & Kriswoyo, P.G. (2013). Pengaruh tindakan
restrain fisik dengan manset terhadap penurunan
perilaku kekerasan pada pasien skizofrenia di ruang
rawat intensif bima Rumah Sakit Jiwa Grhasia Daerah
Istimewa Yogyakarta [the effect of physical restraint
with cuff on increasing violent behavior among
schizophrenic patients in intensive care bima Regional
Mental Hospital Grhasia]. Jurnal Keperawatan Mersi,
4(2), pp. 1-6
Schory, T.J., Piecznski, N., Nair, S., & El-Mallakah, R.S.
(2003). Barometric pressure, emergency psychiatric
visits, and violent acts. Canada Journal Psychiatric,
48(9), pp. 624-627
Staten, P.A. 2001. Restraint, seclusion standars raise
questions. Nursing Management, 32(7), pp. 17
Stuart, G.W. (2013). Principles and practice of psychiatric
nursing. (10 th ed.). Singapore: Elsevier
Sulistyowati, D.A., & Prihantini, E. (2014). Keefektifan
penggunaan restrain terhadap penurunan perilaku
kekerasan pada pasien skizofrenia [Effectiveness of
using restraint on increasing violent behavior among
schizophrenic patients]. Jurnal Terpadu Ilmu
Kesehatan, 3(2), pp. 106-214
Wynn, R. (2002). Medicate restraint or seclude? Strategies
for dealing with violent and threatening behavior in a
Norwegian university psychiatric hospital.
Scandinavian Journal of Caring Sciences, 16(3), pp.
287-291
Restraint in Psychiatric Patients: A Literature Review
241
