
Comparison of the Effectiveness in Administration of Lactulose,
Probiotics and a Combination of Lactulose and Probiotics against
Hepatic Encephalopathy in Patients with Liver Cirrhosis
Fauzi Yusuf
1*
, Wahyuni
1
, Azzaki Abubakar
1
, Desi Maghfirah
1
1
Division of Gastroenterology-Hepatology, Department of Internal Medicine, Faculty of Medicine University of Syiah
Kuala/ Dr. Zainoel Abidin Centre Hospital, Banda Aceh, Indonesia
Keywords: Hepatic Encephalopathy, Lactulose, Probiotics, Cirrhosis
Abstract : Hepatic Encephalopathy (HE) is one of the most common complication of decompensated liver cirrhosis.
In chronic liver disease there will be a disruption of ammonia metabolism resulting in an increase of 5-10
times ammonia levels which will disrupt the physiology of the brain and brain metabolism. Treatment with
laktulosa and probiotics can provide benefits in improving hepatic encephalopathy. The research subjects
were divided into three groups: group A consisted of 17 people receiving 30-60ml/day lactulose, group B
received one capsule probiotic taken three times per day (each capsule containing 2 billion of Lactobacillus
acidophilus Rosell-52, 2 billion of Lactobacillus rhamnosus Rosell-11 2, 211 mg of Maltodextrin, 8mg of
Magnesium stearate and 1 mg of ascorbic acid) and group C received both lactulose and probiotics. In our
study, we found that there was an improvement in the degree of Hepatic Encephalopathy from severe HE to
mild HE in two people (40%) from group A and one person (50%) from group C with p> 0.05.
1 INTRODUCTION
Liver cirrhosis is an end-stage progressive hepatic
fibrosis characterized by distortion of hepatic
architecture and regenerative nodule formation
(Nurjannah S, 2009). The Indonesian Liver Research
Association known as Perhimpunan Peneliti Hati
Indonesia (PPHI) stated that the prevalence of
patients with liver cirrhosis is 3.5% of all patients
treated in internal medicine inpatient unit, or an
average of 47.4% of all liver disease patients treated
(PPHI-INA ASL., 2013).
Hepatic Encephalopathy (HE) is one of the
most common complication of decompensated liver
cirrhosis. It is a neuropsychiatric syndrome found in
patient with both acute and chronic liver failure. The
clinical features are mental disorders, neurological
disorders, presence of liver parenchymal
abnormalities and laboratory abnormalities.
HE is
caused by the failure of hepatocellular function,
decreased ability of the liver to detoxify ammonia
and other toxins along with a portosystemic shortcut
causing toxic materials to enter the systemic blood
and brain directly without previously being cleaned
in the liver (Zubir N, 2009).
Lactulose has laxative characteristics causing
a decrease in the synthesis and uptake of ammonia
by decreasing colon pH and also reducing glutamine
uptake. Lactulose is converted into monosaccharide
by normal flora and used as a food source so that the
growth of normal intestinal flora will suppress other
bacteria that produce urease. This process produces
lactic acid and also gives hydrogen ions to ammonia
so that the molecules change from ammonia (NH
3
)
and become ammonium ions (NH
4+
). The presence
of this ionization attracts ammonia from the blood
towards the lumen (Nielsen B et al, 2004; Luo M et
al, 2011). Sharma et al (2011) and Watanabe et al
(1997) found that lactulose is effective in preventing
HE in patients with liver cirrhosis and upper
gastrointestinal bleeding.
Probiotics are defined as non-pathogenic
living microorganisms, which if consumed in a
certain amount will give beneficial effects for the
host. Ammonia is also produced by flora in the
intestine so that manipulation of intestinal flora is
one of the HE therapy strategies. Probiotics given to
HE patients can reduce total ammonia in the portal
blood by decreasing bacterial urease activity,
decrease absorption of ammonia by decreasing pH,
decrease intestinal permeability and increase
nutritional status of intestinal epithelium and reduce
inflammation caused by oxidative stress in
hepatocytes thus increasing hepatic clearance of
68
Yusuf, F., Wahyuni, ., Abubakar, A. and Maghfirah, D.
Comparison of the Effectiveness in Administration of Lactulose, Probiotics and a Combination of Lactulose and Probiotics against Hepatic Encephalopathy in Patients with Liver Cirrhosis.
DOI: 10.5220/0008791000680071
In Proceedings of the 2nd Syiah Kuala International Conference on Medicine and Health Sciences (SKIC-MHS 2018), pages 68-71
ISBN: 978-989-758-438-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

ammonia and toxins and reducing toxin uptake (Saji
S et al, 2011; Bousvaros A et al, 2005).
Several studies have shown that lactulose and
probiotics have good ability to prevent the
recurrence of hepatic encephalopathy and
significantly show improvement in psychometric
tests in patients with mild hepatic encephalopathy.
This is the underlying purpose to compare the
effectiveness between the administration of
lactulose, probiotics and the combination of
lactulose and probiotics to patients with liver
cirrhosis and hepatic encephalopathy.
2 PATIENTS AND METHODS
2.1 Research Methods
Clinical trials with paired categorical analytic
studies was carried out in the internal medicine
inpatient unit at Dr. Zainoel Abidin Hospital in
Banda Aceh. The study samples were taken from
patients who were diagnosed with decompensated
cirrhosis with hepatic encephalopathy and fulfilled
the inclusion and exclusion criterias (diarrhea, using
alcohol ≥ 20 g/day, decreased level of consciousness
caused by other conditions than HE, having
spontaneous bacterial peritonitis for the past 6
weeks, and taking antibiotics such as Neomycin,
Metronidazole and Rifaximin).
The diagnosis of decompensated liver
cirrhosis is based on medical history, physical
examination, laboratory findings and abdominal
ultrasonography. The research subjects were taken
by consecutive sampling, then all research subjects
were carried out simple randomization with a
random table system and subjects were allocated
into three groups: A, B, and C. Group A was given
lactulose 30-60 ml per day until the patients secreted
soft defecation 2-3 times per day. Group B was
given one capsule probiotics three times per day
(each capsule containing 2 billion of Lactobacillus
acidophilus Rosell-52, 2 billion of Lactobacillus
rhamnosus Rosell-11, 211 mg of Maltodextrin, 8 mg
of Magnesium stearate and 1 mg of ascorbic acid).
And group C received both lactulose and probiotics.
The therapy is carried out for two weeks.
Ammonia examination using an ammonia test
kit was done by taking capillary blood from the
patient's fingertip as much as 20 µl, dropping it in
the reagent then inserting it into the device, the
results were read in µg/dl after 3 minutes.
Ethical clearance was obtained from the
Ethics Committee of the Faculty of Medicine, Syiah
Kuala University.
2.2 Operational Definition
Liver cirrhosis is diagnosed based on medical
history, physical examination, laboratory findings
and upper abdominal ultrasonography. Hepatic
encephalopathy is a disorder of cognitive function in
patients with liver disease that cannot be identified
only with complete medical history and neurological
examination including family member interviews.
To diagnose hepatic encephalopathy, we need to
find some abnormalities from neuropsychometric or
neurophysiological tests using NCT A/B and West
Haven criteria. In this study, HE degrees were
measured using West Haven criteria. Ammonia is a
major factor in the pathogenesis of hepatic
encephalopathy. Increased ammonia levels can be
due to high protein intake, constipation,
gastrointestinal bleeding, infection, azotemia,
hypokalemia. Normal level of blood ammonia is 0-
150 µg/dl.
2.3 Statistical Analysis
Statistical analysis was carried out by
computerization, with a significance level of p
<0.05. Normal data distribution was analysed by
repeated anova test and continued with Bonferroni
post-hoc analysis to find out which groups have
significant result.
3 RESULTS
The research subjects were divided into three
groups: 17 people in lactulose group, 17 people in
probiotic group and 17 people in lactulose +
probiotic group. During the research two people
from the lactulose + probiotic group resigned. The
number of subjects that followed the research until
the end were 49. The lactulose group received
standard cirrhosis therapy plus lactulose 30-60
ml/day, the probiotic group received standard
cirrhosis therapy plus probiotics 1 capsule 3 times
per day (each capsule containing 2 billion of
Lactobacillus acidophilus Rosell-52, 2 billion of
Lactobacillus rhamnosus Rosell-11, 211 mg of
Maltodextrin, 8 mg of Magnesium stearate and 1 mg
ascorbic acid), while the third group received both
lactulose and probiotics. The study was conducted
for two weeks and the parameters assessed were
Comparison of the Effectiveness in Administration of Lactulose, Probiotics and a Combination of Lactulose and Probiotics against Hepatic
Encephalopathy in Patients with Liver Cirrhosis
69
ammonia level in the blood and the degree of hepatic
encephalopathy. Before the study begins, all subjects
were examined for hepatitis B and C markers,
endoscopy examination, albumin level, bilirubin
level and liver function. We found that all the basic
characteristics in the subjects were the same in the
three groups.
Table 1. Basic Characteristics of The Subjects.
Variable
Groups
P
Lactulose
(n=17)
Probiotics
(n=17)
Lactulose
+Probiotic
(n=15)
Age (years) 53,11±12,81 56,41±12,97 57,86±17,42 p
>0,05
Gender
Male
Female
10(29,4%)
7(46,7%)
12(35,3%)
5(33,3%)
12(35,3%)
3(20,0%)
Liver cirrhosis
Etiology
HBV
HCV
Non B dan C
7(25,0%)
1(25,0%)
9(52,9%)
12(42,9%)
1(25,0%)
4(23,5%)
9(32,1%)
2(50,0%)
4(23,5%)
p
>0,05
HE degree (%)
Mild
Severe
12(30,8%)
5(50,0%)
14(35,9%)
3(30,0%)
13(33,3%)
2(20,0%)
p
>0,05
Endoscopy (%)
VE
PHG
VE/PHG
12(42,9%)
3(50,0%)
2(13,3%)
6(21,4%)
3(50,0%)
8(53,3%)
10(35,7%)
-
5(33,3%)
p
>0,05
Albumin (g/dl) 2,50±0,43 2,55±0,61 2,46±0,43 p
>0,05
Bilirubin
(mg/dl)
6,15±8,23 3,21±2,39 4,16±6,18 p
>0,05
SGOT (U/1) 146,35±97,99 133,94±87,71 113,33±68,4
1
p
>0,05
SGPT (U/1) 92,94±66,21 94,82±73,87 91,80±63,77 p
>0,05
Ammonia
(ug/dl)
198,29±21,44 197,35±22,20 188,53±26,0
4
p
>0,05
HBV = Hepatitis B Virus, HCV = Hepatitis C Virus, HE = Hepatic Encephalopathy, VE
= Varices Esophagus, PHG = Portal Hypertension Gastropathy, SGOT = Serum
Glutamic Oxaloacetic Transaminase, SGPT = Serum Glutamic Piruvic Transaminase
There was a decrease in ammonia level in
average in all three groups around 194.97 ± 16.05
ug/dl. The reduction in ammonia level in each group
was statistically significant. But the difference
between the ammonia levels in the three groups is
8.59 ug/dl which is not statistically significant (p>
0.05).
Table 2. Ammonia level in three groups before and after two
weeks of therapy
Groups
Ammonia levels
before therapy
(ug/dl)
Ammonia levels
after two weeks
of therapy (ug/dl)
P
Lactulose
Probiotic
Lactulose+
Probiotic
198,29±21,44
197,35±22,20
188,53±26,04
136,11±19,99
143,76±29,73
129,93±22,4
p< 0,05
p < 0,05
p < 0,05
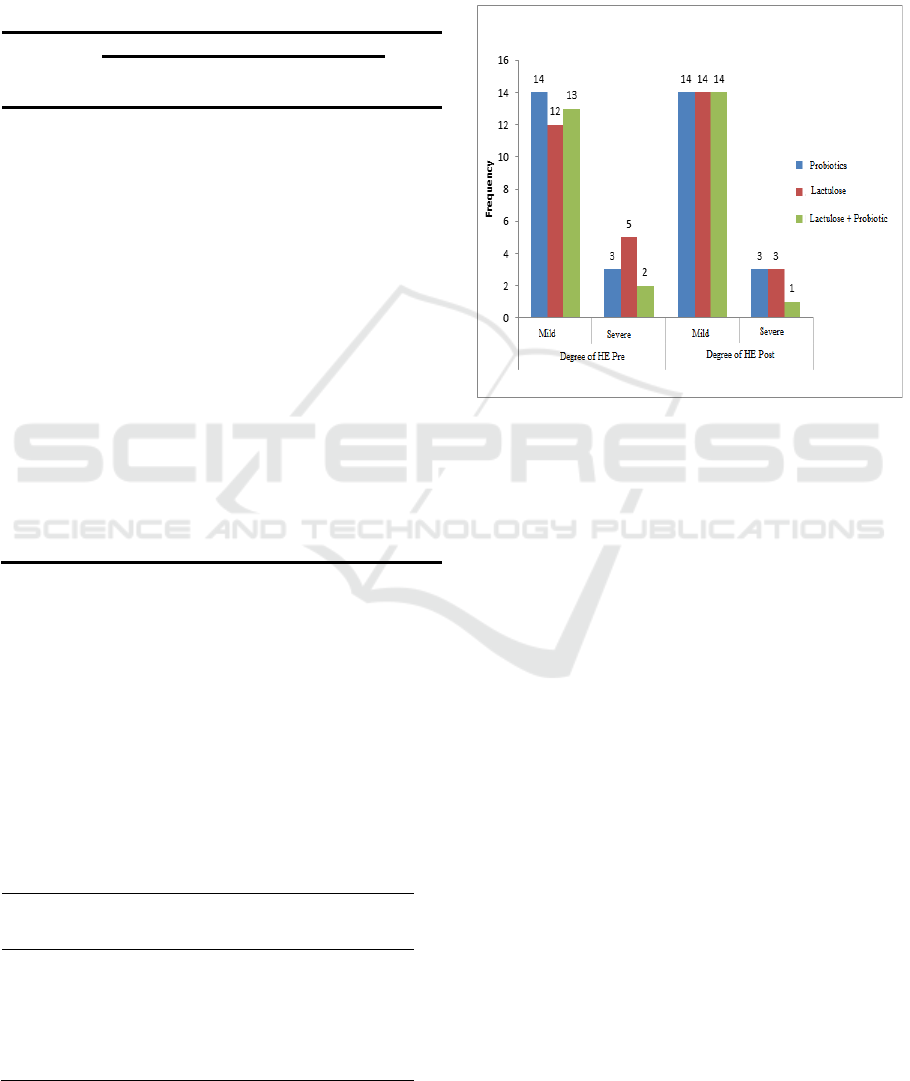
There was an improvement in the degree of
hepatic encephalopathy from severe HE to mild HE
in two people from goup A (40%) and one person
from group C (50%). The improvement in HE
degree was not statistically significant (p> 0.05).
Figure 1. The change in the Hepatic Encephalopathy degree
before and after two weeks of therapy in the three groups.
4 DISCUSSION
Based on this study, there was a significant
reduction in ammonia level in the blood after two
weeks of therapy in the three groups. Lactulose can
reduce ammonia levels in the blood and improve the
results of psychometric tests thus affect the quality
of life of patients with liver cirrhosis who
experienced HE. The results of this study are
consistent with the study of Nie et al in 2003, who
conducted a study of lactulose administration for 8
to 28 weeks in patients with liver cirrhosis who had
hepatic encephalopathy. There was reduction in
ammonia levels in the blood, improved
psychometric tests and prevention of recurrent
encephalopathy (Nie YQ et al, 2003).
In 2011, Saji S et al. conducted a study by
administering probiotics to 21 patients with liver
cirrhosis who had been diagnosed with hepatic
encephalopathy for at least 6 months. The results
showed that ammonia levels decreased from 140.29
± 7.28 to 122.38 ± 10.69 and there was a significant
decrease in the second and third days compared to
the first day.
Probiotics can reduce blood ammonia
levels by increasing the concentration of non-urease
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
70

bacteria and acting as a beneficial agent for the
balance of intestinal flora (Pawar RR et al, 2012).
In 2000, Dhiman et al. conducted a study by
administering lactulose for 3 months in subclinical
patients with hepatic encephalopathy. After that,
they performed NCT examination, FCT, block
design and picture assembly. And later, they found
some improvements in psychometric tests and
minimal hepatic encephalopathy.
In 2014, Shavakhi et al. administered probiotics
and lactulose to liver cirrhosis patients with mild
hepatic encephalopathy for 2 weeks and 8 weeks
follow-up. They found that lactulose and probiotics
were effective for minimal improvement of hepatic
encephalopathy. In comparison, probiotics are
superior to lactulose in improving hepatic
encephalopathy.
This study had several limitations. Firstly, the
number of samples was relatively small thus there
can be a bias in processing. Secondly, the
examination of hepatic encephalopathy only used
West Haven criteria, so we cannot assess the
changes in the degree of mild hepatic
encephalopathy to non-hepatic encephalopathy
which can be confirmed by a more accurate
examination such as Critical Flicker Frequency
(CFF). Thirdly, the limited time for the research
made us unable to observe the long term side effect
of lactulose and probiotics administration.
5 CONCLUSIONS
Administering lactulose, probiotics and a
combination of both probiotics and lactulose have
the same effectiveness in reducing ammonia levels
in the blood, as well as decreasing HE degree from
severe to mild degree.
REFERENCES
Bousvaros A, Guandalini S, Baldassano RN, Botelho C,
Evans J, et al., 2005. A randomized, double blind trial
of Lactobacillus GG versus placebo in addition to
standard maintenance therapy for children with
Crohn’s disease. Inflamm Bowel Dis. 11:833-9.
Dhiman RK, Sawhney MS, Chawla YK, Das G, Ram S, et
al., 2000. Dila. Efficacy of lactulose in cirrhotic
patients with subclinical hepatic encephalopathy. Dig.
Dis. Sci.45:1549-52.
Luo M, Li L, Lu CZ, and Cao WK., 2011. Clinical
efficacy and safety of lactulose for minimal hepatic
encephalopathy: a meta-analysis. Eur J Gastroenterol
Hepatol. 23:1250-57
Nie YQ, Zeng Z, Li YY, Sha WH, Ping L, et al., 2003.
Long term efficacy of lactulose in patients with
subclinical hepatic encephalopathy. Zhonghua. Nei.
Ke. Za. Zhi. 42 (4):261-3.
Nielsen B, Gluud LL, and Gluud C., 2004. Non-
absorbable disaccharides for hepatic encephalopathy:
systematic review of randomised trials. BMJ.
328:1046.
Nurjanah S., 2009. Sirosis hati.dalam : Buku ajar ilmu
penyakit dalam. Edisi kelima, jilid I. editor: Sudoyo
AW. Jakarta.Interna publishing. 668-72.
Pawar RR, Pardeshi ML, and Ghongane BB., 2012. Study
of effects probiotic Lactobacilli in preventing major
complication in patients of liver cirrhosis.
International Journal of Research in Pharmaceutical
and Biomedical Sciences. 3 (1) Jan-Mar, p.206-11.
PPHI-INA ASL., 2013. Sirosis Hati. Perhimpunan
Peneliti Hati Indonesia. Availabel :Pphi-
online.org/alpha.
Saji S, Kumar S, and Thomas V., 2011. A randomized
double blind placebo controlled trial of probiotics in
minimal hepatic encephalopathy. Tropical
Gastroenterology. 32(2):128-32.
Sharma P, Agrawal A, Sharma BC, and Sarin SK., 2011.
Prophylaxis of hepatic encephalopathy in acute
variceal bleed: A randomized controlled trial of
lactulosa versus no lactulosa. Journal of
Gastroenterology and Hepatology.26:996-1003
Shavakhi A, Hashemi H, Tabesh E, Derakhshan Z,
Farzammia S, et al., 2014. Multistrain probiotic and
lactulose in the treatment of minimal hepatic
encephalopathy. Journal of Research in Medical
Sciences. 19:703-8.
Watanabe A, Sakai T, Sato S, Imai F, Ohto M, et al., 1997.
Clinical efficacy of lactulose in cirrhotic patients with
and without subclinical hepatic encephalopathy.
Hepatology. 26:1410-14
Zubir N., 2009. Koma hepatik. Dalam: Buku Ajar Ilmu
Penyakit Dalam Jilid I, Edisi V, Pusat Penerbitan
Departemen Ilmu Penyakit Dalam Fakultas
Kedokteran Universitas Indonesia. 677-80.
Comparison of the Effectiveness in Administration of Lactulose, Probiotics and a Combination of Lactulose and Probiotics against Hepatic
Encephalopathy in Patients with Liver Cirrhosis
71
