
Integrating Physical Activity Data with Electronic Health Record
Rishi Saripalle
School of Information Technology, Illinois State University, Normal, Illinois, 61790, U.S.A.
Keywords: HL7 Fast Health Interoperability Resources (FHIR), Physical Activity Resource, EHR Physical Activity,
OpenEMR, Exercise, Wearables.
Abstract: Wearables allow individuals to track, analyze, and visualize their physical activities and associated data
such as vitals, activity information, etc. across time. But, none of this activity data is anywhere to be found
in an electronic health record - the primary source of patient medical data for the healthcare providers. This
inability doesn’t allow experts to view the complete health summary of an individual and also, activity data
can play a key role in healthcare decisions. This problem is due to the lack of standards that can capture
activity data from disparate sources (e.g., wearables, smart watches, trackers, etc.) and integrate it with an
EHR. This research article identifies and provides a detailed analysis of the key factors contributing to the
problem. Based on the detailed analysis, we design an interoperable model by leveraging HL7 FHIR
standard to capture activity data from wearables and develop it using FHIR HAPI - an implementation of
HL7 FHIR. This initial prototype is tested by capturing Fitbit data and integrating it with OpenEMR - an
open source EHR.
1 INTRODUCTION
Digitalization of healthcare data in the form of
Electronic Health Record (EHR) eliminated many
healthcare issues and is leveraged by the industry to
capture, aggregate, and analyse the patient data.
Currently, many EHR systems, both proprietary and
open-source, allow providers to capture a variety of
patient data such as diagnosis, encounters,
observations, procedures, medications, family
medical history, etc. The patient data can be shared
across healthcare systems using different healthcare
standards such as ASTM CCR, Health Level 7
(HL7) CCD (D’Amore et al., 2011), HL7 V2 and V3
(Boone, 2011, Dolin et al., 2001) messaging format,
and HL7 FHIR (Saripalle, in press). However, the
physical activity data of a patient is not captured in
an EHR and is not shared across diverse healthcare
systems. Physical activity is defined as “any bodily
movement produced by skeletal muscles that result
in energy expenditure” (Caspersen, Powell &
Christenson, 1985). Exercise is a subset of physical
activity which is defined as “a planned, structured,
and repetitive and has as a final or an intermediate
objective the improvement or maintenance of
physical fitness” (Caspersen et al., 1985). Both
physical activity and exercise will be referred as to
“activity” for the rest of the article unless stated
explicitly.
Before wearables, tracking activities and
quantifying their output was practically impossible
or expensive for an individual/patient. Hence, there
is none or minimal activity data recorded in the
health records. However, the introduction of
wearables and smartwatches (e.g., Fitbit, Apple
Watch, LG Watch, etc.) have revolutionized the
personal health space and the behavior/attitude of
the consumers towards activities. Using these
affordable digital instruments, an individual can
track their physical activity (e.g., walking, running,
etc.) and any associated data (e.g., heart rate,
calories, distance, elevation, route, time, etc.).
According to market analysts (Hunn, 2015, Kaul,
Wheelock, 2015), there is an accelerating market for
wearables where the valuations are expected to reach
~30 billion by 2020 from ~$600 million in 2013.
Researchers (Shin, Jarrahi, Nov 15 2014, Hillsdon,
2015, Fanning et al., 2012, Lim et al., 2011) also
found evidence that the wearables served as a
valuable tool for quantifying and visualization an
individual’s physical activities and provided them
motivational affordances to do more.
Even as individuals can track their activities and
quantify its output, healthcare providers cannot see
Saripalle, R.
Integrating Physical Activity Data with Electronic Health Record.
DOI: 10.5220/0007310100210029
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 21-29
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
21

this data in an EHR. The primary reason is due to
the lack of an interoperable model/structure within
the existing healthcare standards that can capture
activity data. These are the same healthcare
standards that are used to share EHRs. Figure 1
renders the current wearable infrastructure and it’s
working. In most cases, logs are used to record the
exercise routine/plan, a non-digital format facing the
same issues as paper-based medical records. Activity
data captured using the wearables (e.g., Fitbit, most
popular among wearables) is synchronized to the
organization data repositories through a mobile app
(e.g., Fitbit, LG Sport, etc.) and is accessible via an
API (e.g., Fitbit or Google Fit API) but is formatted
in the organization own data format. In the case of
Apple Watch, data is only accessible within iOS
ecosystem using Apple HealthKit or download
through its Health App, making it difficult to access
the data outside the iOS environment. In Android,
the devices use Google Fit to record and access the
activity data. Most of the other fitness wearables
(e.g., Garmin, etc.) fall under the same pattern –
record, report, and access the data via an API if
provided or download the data. From Figure 1, it is
evident that the activity instruments, digital or non-
digital, collect (and report) data in a non-standard
format and report the data to a proprietary data store,
creating data silos. These data repositories or the
devices cannot communicate the captured data with
a healthcare information entity such as an EHR due
to the lack of an agreed “standard” to capture and
share the activity and any associated data. Focusing
on integrating individual devices with an EHR out of
the box is unfeasible, aunting, and practically not
scalable.
Another issue due to the inability to integrate
activity data with an EHR is that the experts cannot
provide evidence-based physical activity plans,
exercise routines, etc. For example, an individual,
say, John Doe, age 25 with no serious medical
condition approaches a trainer to improve his fitness.
Most of the trainers use their knowledge and
experience to design a exercise routine to help John
Doe reach his/her goal. How will the trainer prove
the provenance of the routine? What kind of
evidence can the trainer provide to John Doe that
supports the plan or at least in majority cases? John
Doe might have a positive attitude towards the
exercise routine if the trainer shows evidence that
the exercise routine worked previously with other
individuals. In biomedical and health informatics,
questions related to the patient's treatments or care
can be answered with clinical evidence. This
evidence is obtained by analyzing copious amounts
of de-identified aggregated patient data using
various computational algorithms and techniques.
The same cannot be said about physical activity and
exercise routine/plan(s).
The aim of this research is to design and develop
an interoperable model/structure using existing
healthcare standard to capture activity data and share
it across healthcare information systems. The rest of
the paper is organized as follows. Section 2 provides
the background knowledge and analysis of the
current situation. Section 3 presents the solution
using the HL7 FHIR and OpenMRS – an open
source EHR. Section 4 summarizes the research.
Figure 1: Interoperability issues with current physical activity and exercise digital and non-digital instruments.
HEALTHINF 2019 - 12th International Conference on Health Informatics
22

2 BACKGROUND AND
ANALYSIS
Experts unanimously agree that physical activity has
many health benefits and numerous research studies
spanning across multiple decades has proven to
show its impact the overall health of an individual
and nation’s economy. With the goal to improve the
activity level of individuals across the United States,
in 2007, the American Medical Association and the
American College of Sports Medicine (ACSM)
collaborated to launch the program - Exercise is
Medicine (EIM) (Lobelo et al., 2014). The goal of
the program is to make physical activity a standard
and adapt scientifically proven benefits of physical
activity into the mainstream healthcare. The idea is
for the physicians to access the activity level of the
patient (use of the Physical Activity Vital Sign
(PAVS) questionnaire (Lobelo et al., 2014, Sallis,
2011) during the patient’s encounter and prescribe
physical activity based on the identified health risks
and ACSM evidence-based guidelines. The physical
activity prescription, similar to medication
prescription, must be saved and tracked along with
other data. The most effective way to achieve this
goal is to integrate activity data with an EHR. The
intention of the EIM is congruent with the research
statement and supports the need for healthcare
standard(s) to integrate the activity data with an
EHR.
Beyond EIM framework, there are only a few
research studies that have identified and reported the
need to save physical activity data for longitudinal
healthcare analysis and benefits. Sallis (2011)
pushed to treat physical activity as a vital sign.
Physicians must record and observer the patient’s
physical activity levels during their medical visits
once recognized as a vital sign by the healthcare
community. Coleman et al., (2012) presented facts
and validity of Exercise Vital Sign (EVS), similar to
PAVS, for its use in an outpatient electronic medical
record. After analysing the current research and
healthcare standards, the primary reason for the
interoperability issues is due to the lack of agreed
healthcare standards, both structural and semantic,
for representing and sharing activity data. As the
standards are a foundation for interoperability, it’s
surprising that the experts have not yet designed an
interoperable standard to capture physical activities
and exercises. Without an agreed standard, it’s not
feasible to capture, share and integrate the activity
data into the healthcare systems. Few standards are
scalable and can be extended to meet various
healthcare requirements, in our case capture activity
data. For instance, HL7 V2 (Boone, 2011)
messaging format is a pipe (|) and hat (^) encoding
format that allows clinicians to exchange data.
However, this standard is not supported by a
software model with a well-defined structure and
semantics. Due to this drawback, experts developed
the HL7 V3 (Boone, 2011) messaging format. Thus,
it doesn’t add any value to extend the HL7 V2
format to achieve our goal. The HL7 V3 is built
using HL7 Reference Information Model (RIM)
(Boone, 2011) – a sound object-oriented model with
a well-defined structure, semantics, and constraints
that can be extended. The current HL7 RIM model
can be repurposed to capture and communicate a
limited set of activity data. For example, activities
such as jogging, swimming, etc. and the vitals
generated during the activities can be represented
and communicated using HL7 V3 messages. Figure
2a shows the activity jogging (the subject of the
message) and heartbeat (outcome (OUTC)
relationship), an outcome of the subject in HL7 V3
format.
Saripalle (2017) extended the HL 7 RIM model
with required classes to capture the activity data.
Later, HL7 V3 messages were constructed based on
the extended model to share the activity data across
healthcare systems that accept HL7 V3 messaging
format. Figure 2b shows the extended model. The
classes, PhysicalActivity and ExercisePlan, that
capture the required data. authors to use this
document for the preparation of the camera-ready.
There are two key lessons learned from this
research. First, the HL7 RIM is a complex model
that can be difficult to comprehend. Further,
understanding HL7 V3 messaging format has a steep
learning curve that requires expertise in computing.
Second, there are only a few open-source healthcare
systems and tools, specifically EHR's, which can be
extended and are designed to accept HL7 V3
messages. This makes implementation of the
research very difficult.
The knowledge required to design the new
classes (Figure 2b) to extend the RIM is adapted
from PhysicalActivity and ExercisePlan schemas
defined by Schema.org. Schema.org (2012) is an
open source effort to define schemas/data structures
to describe any data, especially the data published on
the web. Schema.org describes, i.e., provide
schema/structure for numerous concepts (e.g.,
Person, ScholaryArticle, Book, Organization, etc.)
across various domains (e.g., Auto, Health, Books,
Biology, etc.). Currently, most of the data published
on the web is unstructured. The developers use the
Schema.org schemas to annotate (using Microdata or
Integrating Physical Activity Data with Electronic Health Record
23
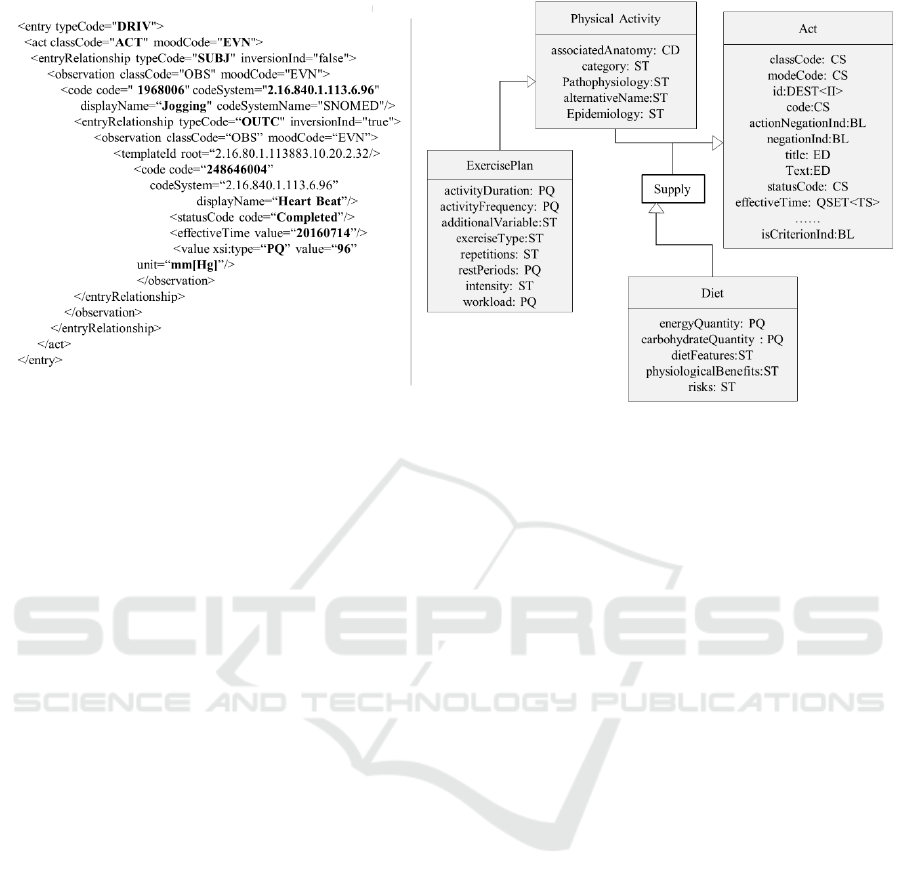
(b) HL7 V3 message representing the activity jogging and
resultant vital data using the RIM model Act and Observation
class.
(a) Extended HL7 RIM model to capture activity data.
Figure 2: HL7 V3 message format and extended HL7 RIM model.
RDFa or JSON-LD formats) their data before
publishing. This also allows machines to understand
and link data efficiently. Many modern websites use
Schema.org to annotate their webpages to provide
meaning to their data and also make the website
search engine friendly. The PhysicalActivity and
ExercisePlan schemas from the Schema.org that are
adapted by Saripalle (Saripalle, 2017) to design the
new RIM classes (Figure 2b) and are also used for
this research. Similar to the Schema.org, Open
mHealth (Open mHealth, 2015) is a data-driven
approach to provide schemas specifically for
describing, collecting, and sharing healthcare data
such as blood pressure, body weight, body height,
heart rate, etc.
Further, apart from developing the structural
standard(s) for activity data, the idea of this
research, experts must also define semantic
standard(s) to standardize the physical activity and
exercise vocabulary. Few existing terminologies
capture concepts related to the physical activity and
exercise. For example, SNOMED (2007) is an
internationally recognized biomedical semantic
terminology that captures concepts spanning across
multiple clinical disciplines. For example, jogging
(code 1968006), running (418060005), walking
(129006008), chest press exerciser (46778600), etc.
However, currently, there is no dedicated standard
semantic terminology that comprehensively captures
the concepts of physical activities and exercises.
Designing and developing standards itself
doesn’t solve the problem. The standards also need
support from the healthcare community, information
technology, healthcare experts, public and private
organizations. Most importantly, the healthcare
community must adopt the new/extended standard to
existing systems and applications. The healthcare
experts might have to tweak their protocols, best
practices, and include physical activity check during
a regular patient’s visit.
3 INTEGRATING ACTIVITY
DATA WITH EHR USING HL7
FHIR
To capture the activity data and seamlessly integrate
it with a healthcare system such as an EHR, this
research will leverage HL7 Fast Health
Interoperability Resource (FHIR) (HL7, 2015) – the
new HL7 member, OpenEMR – an open source
electronic health record system (OpenEMR, 2001)
and schemas defined by Schema.org and Open
mHealth. The research design has two phases. First,
extend FHIR to design a new model to capture the
activity data. Second, implement the new FHIR
model and interface it with the OpenEMR. This
research doesn't handle semantic standard(s)
required for the physical activity and exercise.
HEALTHINF 2019 - 12th International Conference on Health Informatics
24

Briefly, the HL7 FHIR standard is designed by
combining the HL7 RIM model, lightweight HTTP-
based RESTful web services and the lessons learned
from using HL7 V3 format. HL7 FHIR is a mashup
of HL7 RIM and REST protocol with backward
compatibility with the HL7 V3. The atomic unit of
FHIR is a Resource. The health data in the FHIR
environment is captured and shared as an FHIR
resource. The FHIR standard defines multiple
resources to represent different types of healthcare
data. For example, MedicationStatement resource
captures a patient’s prescription, Encounter resource
captures patient-provider visit information,
Observation resource captures vital data (e.g., heart
rate, blood pressure, pulse, BMI, weight, etc.) or
symptom data, DiagnosticReport captures test
results information including images, and Vision
resource captures patient’s optical data. HL7 FHIR
also has resources to capture administrative and
health insurance aspects such as Claim, Coverage,
PaymentNotice, etc. For comparison, FHIR
resources are equivalent to various sandwich
ingredients such as bread, spreads, vegetables, meat,
sauces, etc. As the different ingredients are
combined to make a user’s sandwich, multiple FHIR
resources are aggregated to build a patient record or
an EHR. Figure 3 exemplifies the usage of
individual FHIR resources to build a patient’s
record. Currently, FHIR defines 117 resources that
can be categorized into clinical (e.g., Condition,
Observation, NutiritionOrder, etc.), foundation (e.g.,
CapabilityStatement, Provenance, etc.), base (e.g.,
Patient, Person, Organization, etc.), financial (e.g.,
Claim, Coverage, etc.), and specialized (e.g.,
ResearchStudy, Questionnaire, etc.). It’s beyond the
scope of this paper to further deluge into the
fundamentals of FHIR standard and its inner
workings. For further documentation and a complete
list of the FHIR resources can be accessed at the
FHIR specification website (HL7, 2017).
The HL7 FHIR standard designers are aware that
the current set of resources might not meet all the
current and future healthcare and policy
requirements. Thus, the FHIR design team ensured
that the standard is extendable, i.e., experts can
define new FHIR resources or existing resources can
be modified to meet any requirement. In software
engineering terms, FHIR embraced the classic open-
closed principle. This research will leverage this
feature to design a new FHIR resource to capture the
patient’s physical activity and exercise data and
share it across healthcare information systems. The
context and knowledge required to define the new
FHIR resource, named PhysicalActivity, that
captures the activity data is obtained from the
PhysicalActivity and ExercisePlan schemas defined
in Schema.org, PhysicalActivity and related schemas
from Open mHealth, PAVS questionnaire, and
knowledge from the experts in the field of exercise
science. Table 1 shows the primary attributes of
PhysicalActivity and ExercisePlan (some attributes
are ignored as they are unrelated to the research
goal) defined by Schema.org.
Table 1: Attributes associated with PhysicalActivity and
ExercisePlan schema defined in Schema.org.
Physical Activity
Attribute Name Explanation
associatedAnatomy
The anatomy of the underlying
organ system or structures
associated with this entity.
category A category this activity belongs to
epidemiology
The characteristics of associated
patients, such as age, gender, race
etc.
code
The code from a controlled
vocabulary or ontology such as
ICD, MeSH, SNOMED-CT, etc.
recognizingAuthority
The organization that officially
recognizes this activity
pathophysiology
Changes in functions associated
with this activity.
Exercise Plan
Attribute Name Explanation
activityDuration
Length of time to engage in the
exercise.
activityFrequency
How often one should engage in the
exercise.
exerciseType
Type(s) of exercise, such as strength
training, aerobics, etc.
intensity
Degree of force involved in the
exercise. E.g., heartbeats
Repetitions
Number of times one should repeat the
activity.
Workload
Measure of the exercise output or
energy expenditure
On further analysis, the attributes of the
PhysicalActivty schema defined by Open mHealth
are a subset of PhysicalActivity schema attributes of
Schema.org. The Open mHealth doesn’t provide a
standard data structure to capture exercises. Apart
from the ExercisePlan schema from Schema.org, the
research also considered the paper-based (exercise
Integrating Physical Activity Data with Electronic Health Record
25

Figure 3: FHIR resources are aggregated to define a patient profile.
logs) structure followed by various organizations
(e.g., LA Fitness, Gold gym, etc.), and expert’s
knowledge into the new FHIR resource design
consideration.
Figure 4 shows the PhysicalActivity FHIR
resource. The exercise entity is modeled as an inner
element of the PhysicalActivity resource as an
exercise is a structured and repetitive physical
activity in the exercise science (Caspersen et al.,
1985). In an object-oriented language, the exercise
element has a composition relationship with
PhysicalActivity resource. Figure 4 provides a
detailed description of each attribute in the
PhysicalActivity resource and the data it captures.
The attributes vital and patient are of type
Observation and Patient FHIR resources
respectively. The types of other attributes are FHIR
defined datatypes such as Identifier, Quantity,
CodeableConcept, string, etc. As previously stated,
some attributes (Table 1) from PhysicalActivity and
ExercisePlan schemas from Schema.org are in the
PhysicalActivity resource. The designed resource
also captures the crucial data requested in the PAVS
questionnaire through the attributes activeTime and
Workload (e.g., calories burned). The
PhysicalActivity resource can also be extended, like
any other FHIR resource to meet any future
requirements.
The second phase is the implementation of the
designed research and integrating the captured data
with an EHR – OpenEMR. The HL7 FHIR is only a
standard specification, but not an executable
software. The research used the FHIR specification
to design the new PhyscialActivity FHIR resource,
but to prototype the solution this research will use
HAPI FHIR (Velykis, 2014). The HAPI FHIR is an
open-source Java implementation of HL7 FHIR
specification that has both server and client. The
Open Medical Record System (OpenEMR) is used
to integrate the activity data captured as an FHIR
resource. The OpenEMR is chosen for this research
due to an active community, has a larger audience,
and focused on natively supporting the FHIR
standard. The OpenEMR is modified to accept the
new FHIR resource, persist the data and display the
data on the system.
Figure 5 shows the architecture of the
implementation. The HAPI server is the main
module of the architecture interfacing with the
Translator and the OpenEMR database. The
Synchronizer extracts the activity data using the
wearable API (e.g., Fitbit API) and authenticating
using the provided OAuth credentials from the
respective wearable datastores and pass the data to
the Translator.The Translator translates the activity
data into an instance of PhysicalActivity FHIR
resource and passes it to the HAPI server. Currently,
the implementation can handle Fitbit, Jawbone data
and Google Fit data. The FHIR server saves the data
in the OpenEMR database using its OpenEMR API
and physician can access the same data using
OpenEMR user interface. The wearable, with an
API, has to be configured only once and the data is
extracted periodically. Currently, the wearable
configuration, primarily authentication, needs be
done at the programming level, but not through
OpenEMR UI. As the diverse activity data formats
are translated into an FHIR resource, any healthcare
application that supports the extended FHIR
standard can replace the OpenEMR. Also, the
designed research solution is in line with the EIM
solution the experts are seeking. The implemented
solution is accessible at
http://umls.it.ilstu.edu:8100/openemr/index.php and
further details are available on request. Figure 6
(top) shows a screenshot of the OpenEMR physician
interface displaying “Physical Activity” (bottom
right) as a member of any other medical entity such
as medication, allergy, prescription, etc. Figure 6
(below) shows the physician a quick snapshot of the
weekly summary (calories burned and time in
minutes) which is equivalent to PAVS.
4 CONCLUSIONS
This research has identified and reasoned the need to
HEALTHINF 2019 - 12th International Conference on Health Informatics
26
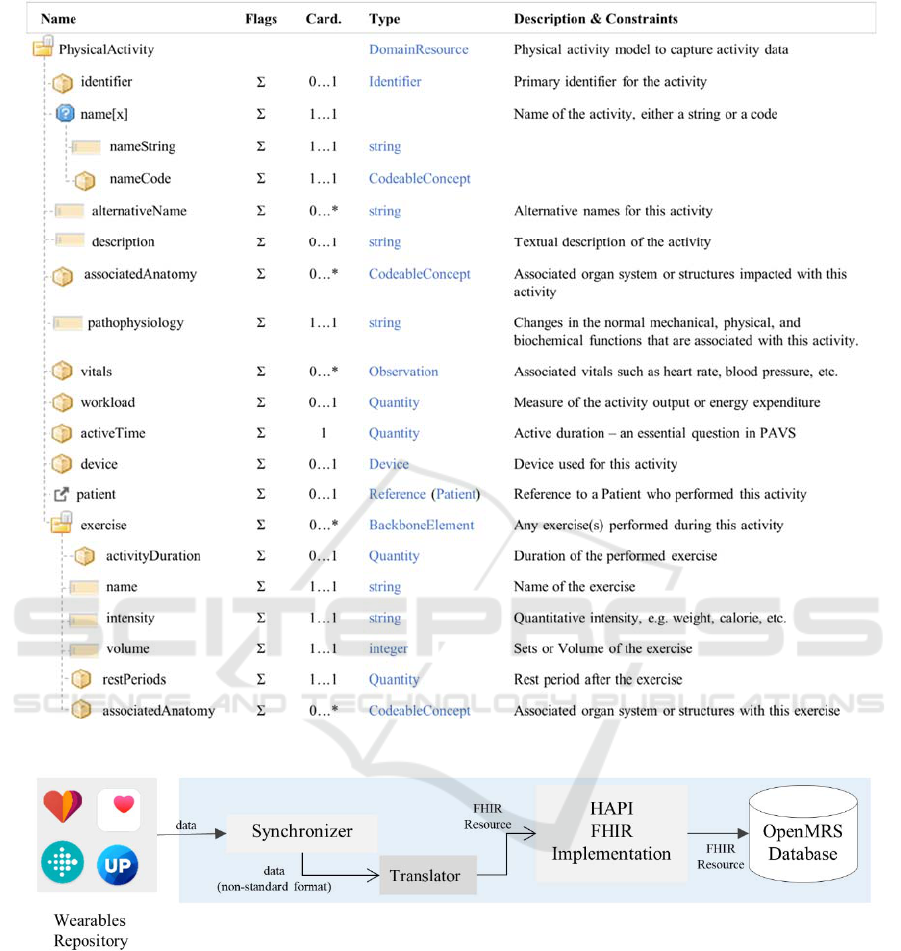
Figure 4: Physical Activity FHIR resource.
Figure 5: Software architecture of the modified OpenEMR system with HAPI FHIR to integrate physical activity and
exercise data.
standardize activity data format and integrate the data
with a healthcare information systems, such as an
EHR, to provide a patient’s complete health
summary to the healthcare provider to make an
informed decision. To this end, the research
identified that the inability to integrate activity data
captured by various instruments (e.g., wearable,
smart watched, logbooks, mobile apps, etc.) with an
EHR or any other healthcare information system is
due to lacks of agreed interoperable structural
standards to represent activity data. Based on the
analysis, background knowledge and previous
research, lessons from EHR development, and
feedback from multiple experts (exercise and health
sciences), this research designed an interoperable
model, PhysicalActivity resource (Figure 4), by
leveraging HL7 FHIR and schemes from Schema.org
and Open mHealth to capture activity data. The
PhysicalActivity resource is implemented using
HAPI FHIR, a client-server implementation of the
Integrating Physical Activity Data with Electronic Health Record
27

HL7 FHIR specification. The research is
demonstrated (Figure 5) by extracting the Fitbit data
via Fitbit API, translating the data into
PhysicalActivity resource and integrating it with
OpenEMR - an EHR. Once in the digital format
within an EHR, the activity data can be de-identified
and aggregated to build large activity datasets
allowing researchers to apply data-driven techniques
to derive actionable knowledge in the field of health
sciences and beyond.
The work presented is an initial step on a long
path. Currently, we are evaluating wearables and
trackers working on Google Fit and will work our
way towards other wearables such as Samsung,
Garmin, etc. The next step worthy of pursuing would
Figure 6: Modified OpenEMR to include physical activity
and exercise data.
be to propose the PhysicalActivity FHIR resource to
the FHIR committee for considering it in the standard
after conducting feasibility and acceptability
analysis. In the prototyped architecture (Figure 6),
the Synchronizer extracts the data and Translator
translates it to the FHIR resource. Research is
required to understand how this process can be
integrated with an EHR and address any security,
privacy and legal concerns.
REFERENCES
D’Amore, J.D., Sittig, D.F., Wright, A., Iyengar, M.S. &
Ness, R.B. 2011, "The Promise of the CCD:
Challenges and Opportunity for Quality Improvement
and Population Health", AMIA Annual Symposium
Proceedings, vol. 2011, pp. 285-294.
Boone, K.W. 2011, The CDA
TM
book, 2011th edn,
Springer.
Dolin, R.H., Alschuler, L., Beebe, C., Biron, P.V., Boyer,
S.L., Essin, D., Kimber, E., Lincoln, T. & Mattison,
J.E. 2001, The HL7 Clinical Document Architecture.
Saripalle, R. in press, "Fast Health Interoperability
Resources (FHIR): Current Status in the Healthcare",
International Journal of E-Health and Medical
Communications (IJEHMC), vol. 10, no. 1.
Caspersen, C.J., Powell, K.E. & Christenson, G.M. 1985,
Physical activity, exercise, and physical fitness:
definitions and distinctions for health-related
research.
Hunn, N. 2015, The Market for Wearable Technology: A
Consumer Centric Approach.
Kaul, A. & Wheelock, C. 2015, Wearable Device Market
Forecasts.
Shin, G. & Jarrahi, M. Nov 15 2014, "Studying the Role
of Wearable Health-Tracking Devices in Raising
Users’ Self-Awareness and Motivating Physical
Activities", International Workshop on Interactive
Systems in Healthcare.
Hillsdon, M. 2015, What Influence Does Personal
Physical Activity Tracking Have On Membership
Retention?, http://theretentionpeople.com/what-
influence-does-personal-physical-activity-tracking-
have-on-membership-retention/ edn.
Fanning, J., Mullen, P.S. & McAuley, E. 2012,
"Increasing Physical Activity With Mobile Devices: A
Meta-Analysis", J Med Internet Res, vol. 14, no. 6, pp.
e161.
Lim, B.Y., Shick, A., Harrison, C. & Hudson, S.E. 2011,
"Pediluma: Motivating Physical Activity Through
Contextual Information and Social Influence",
Proceedings of the Fifth International Conference on
Tangible, Embedded, and Embodied InteractionACM,
New York, NY, USA, pp. 173.
Lobelo, F., Stoutenberg, M. & Hutber, A. 2014, The
Exercise is Medicine Global Health Initiative: a 2014
update.
Sallis, R. 2011, Developing healthcare systems to support
exercise: exercise as the fifth vital sign.
Coleman, K.J., Ngor, E., Reynolds, K., Quinn, V.P.,
Koebnick, C., Young, D.R., Sternfeld, B. & Sallis,
R.E. 2012, Initial validation of an exercise "vital sign"
in electronic medical records.
Saripalle, R. 2017, Extending HL7 RIM Model to Capture
Physical Activity Data, Pittsburg.
(b) OpenEMR with physical activity.
(a) Physical activity weekly summary.
HEALTHINF 2019 - 12th International Conference on Health Informatics
28

Schema.org 2012, Schema.org, http://schema.org/ edn.
Open mHealth 2015, Open mHealth Schema library,
http://www.openmhealth.org/documentation/#/schema
-docs/schema-library edn.
SNOMED 2007, Systematized Nomenclature of Medicine.
Available: http://www.ihtsdo.org/snomed-ct [2016,
October].
HL7 2015, Fast Healthcare Interoperability Resources
Documentation. Available:
https://www.hl7.org/fhir/documentation.html.
OpenEMR 2001, June-last update, OpemEMR. Available:
https://www.open-emr.org/ [2018, May 2].
HL7 2017, FHIR Resources,
https://www.hl7.org/fhir/resourcelist.html edn.
Velykis, A. 2014, HAPI FHIR, http://hapifhir.io.
Integrating Physical Activity Data with Electronic Health Record
29
