
Electrodes Device for Impedance Diagnostics of the Blood Flow in the
Ophthalmic Artery
Petr V. Luzhnov
1
, Anna A. Kiseleva
1
and Elena N. Iomdina
2
1
Bauman Moscow State Technical University, Moscow, Russian Federation
2
Moscow Helmholtz Research Institute of Eye Diseases, Moscow, Russian Federation
Keywords: Impedance Diagnostics, Transpalpebral Rheoophthalmography, Blood Flow, Eye.
Abstract: The paper presents new electrodes device for diagnostics of the eye blood filling based on the registration of
rheographic signals. The methods of bipolar rheoophthalmography and tetrapolar transpalpebral
rheoophthalmography are briefly discussed. The elastic tape is presented as electrodes device. All main
parameters of new electrodes device are chosen. An electrodes system has been developed for recording the
pulse blood filling of main large arteries near eye: ophthalmic artery, internal carotid artery, anterior
cerebral artery and middle cerebral artery. The application of this technique was shown in the example.
Calculations made in analyzing signals obtained from patients without an ophthalmopathology are
presented, which show that eye blood filling in the ophthalmic artery was 30-42 % above, than at research
of an eye by a technique transpalpebral rheoophthalmography.
1 INTRODUCTION
A comprehensive analysis of blood flow is necessary
for obtaining complete information about the eye
blood flow and forming effective diagnostic
conclusions on this basis. Currently, for studying the
blood flow in the eye arteries, the transpalpebral
ultrasound method is known - ultrasound color
mapping (Machekhin and Vlazneva, 2009; Kiseleva,
2004). In addition, contactless optical methods are
known - optical coherence tomography, angiography
(Kurysheva et al., 2017) and laser Doppler
flowmetry (Kiseleva and Adzhemyan, 2015).
Electrical impedance methods are now known,
including methods for obtaining the impedance
distribution in a human body through non-invasive
electrical sounding, calculations and reconstruction
algorithms (Patterson, 2005). The rheography is the
electrical impedance method for studying the pulse
oscillations of the blood flow in the vessels of
various organs and tissues which based on the
graphic recording of changes in the total electrical
resistance of tissues (Sokolova et al., 1977). In
electrical impedance diagnostics the
ophthalmoplethysmography and the
rheoophthalmography are also known (Avetisov et
al., 1967; Lazarenko et al., 1999; Lazarenko and
Komarovskikh, 2004). Rheoophthalmography
(ROG) is the method for assessing the state of the
blood flow in the eye. ROG is a method for studying
the pulse blood filling in the vessels of various
organs and tissues, based on recording changes in
the total electrical resistance of tissues. In the
classical method of ROG registration, the electrodes
are mounted directly on the surface of the eye near
the lens. It leads to necessity of anesthesia for
conducting diagnostic researches.
To solve the limitations of the classical
technique, a new registration technique has been
developed - the method of transpalpebral
rheoophthalmography (TP ROG) (Luzhnov et al.,
2015; Luzhnov et al., 2017; Luzhnov et al., 2018;
Shamaev et al., 2018). In this version of the study,
the electrodes for TP ROG are positioned on the
closed upper eyelid. This method provides for
applying the special device for positioning the
electrodes during the research (Luzhnov et al.,
2017). The method is designed for obtaining
quantitative parameters of uveal ocular blood flow.
The main disadvantage of this method and device
for its implementation is the impossibility of
simultaneous evaluation of the blood flow in the
ophthalmic artery and cerebral arteries.
The rheography electrodes system proposed by
K.K. Yarullin are used in the studying of the brain
256
Luzhnov, P., Kiseleva, A. and Iomdina, E.
Electrodes Device for Impedance Diagnostics of the Blood Flow in the Ophthalmic Artery.
DOI: 10.5220/0007570802560260
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 256-260
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
(Yarullin et al., 1980). This electrodes system allow
to estimate the blood flow in the main cerebral
arteries: the anterior cerebral, middle cerebral,
posterior cerebral and vertebral arteries (Bodo,
2010). The main drawback of this method is the
impossibility of registration the pulse volume of the
ophthalmic artery.
The above-mentioned methods do not allow a
comprehensive assessment of the blood flow in the
eye vessels, due to the fact of examining the blood
flow in each vessel separately. At the same time,
with the help of the electrical impedance method, it
is possible to evaluate the blood flow not only in the
individual arteries, but also in the whole vascular
system of the eye. The main task of this work is a
development of a device for the integrated
assessment of blood circulation in the vessels of the
eye and in addition of the brain, namely in the
ophthalmic artery, (from which all the vessels of the
eye branch off), and in the vessels of the anterior
brain, the anterior cerebral artery and middle
cerebral artery.
2 MATERIALS AND METHODS
2.1 Problem Statement
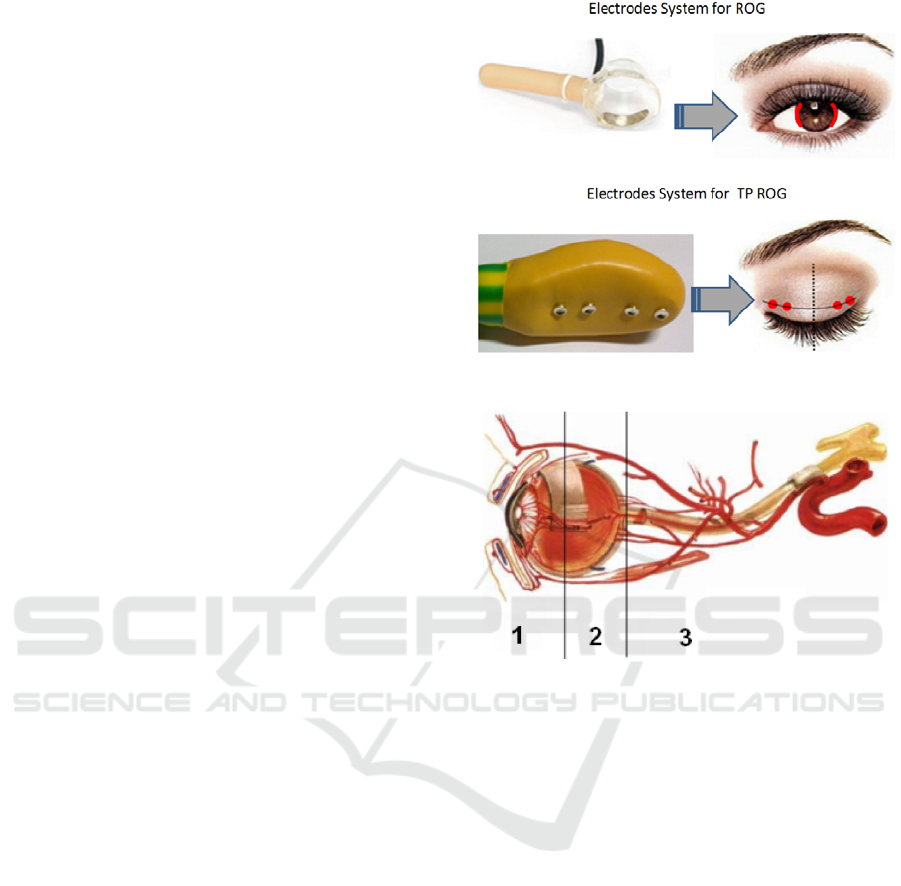
The electrical impedance methods ROG and TP
ROG require to placing electrodes (see the Figure 1)
for estimating the pulse volume of blood in
intraocular vessels.
Both of these methods survey blood vessels from
the first area (see the Figure 2) in diagnostic
procedures. The rheoencephalography method
(Sokolova et al., 1977) allows to estimate the blood
flow in the third area in the Figure 2.
The diagnosing, for example, of patients with
glaucoma (Luzhnov et al., 2018), demands a blood
flow definition in vessels from the second area.
Electrodes systems for ROG or TP ROG do not
approach for this purpose.
Therefore the special electrodes device has been
developed in our work. A distinctive feature is the
possibility of conducting a comprehensive analysis
of the blood flow in the ophthalmic artery and the
vessels of the anterior part of the brain for further
diagnosing, including early hemodynamic disorders
in eye diseases and evaluating the effectiveness of
their therapy. It is achieved through using sixteen
electrodes system, positioned in accordance with the
anatomical location of the analyzed vessels parts
(internal carotid artery, anterior cerebral artery,
middle cerebral artery and ophthalmic artery).
Figure 1: The electrodes systems for ROG and TP ROG.
Figure 2: The areas of ocular blood vessels.
2.2 Electrodes Device
The device is an elastic tape with holes for further
accommodation of 16 electrodes. 12 holes are
located on the tape itself, and 4 holes are on 4 plates
attached to the tape and protruding beyond tape’s
borders. The tape has a pair of Velcro fasteners.
They are providing, if necessary, the length
changing of the tape.
A schematic picture of the device is shown at the
Figure 3.
On the Figure 3 are shown:
1 – The elastic tape with a hexagonal hole in the
center;
2 – Velcro fasteners at the borders of the tape,
separated by a notch in the tape;
3 – The plates with holes for the electrodes
protruding beyond tape’s borders;
4 – The holes for electrodes.
Velcro fasteners (at the borders of the tape) provide,
if necessary, changing in the length of the tape in
accordance with the anthropometric data of the
Electrodes Device for Impedance Diagnostics of the Blood Flow in the Ophthalmic Artery
257

patient's head and the necessary level for pressing
the device to the patient's head. A pair of Velcro
fasteners is located on the left and right ends of the
tape. Structurally they are separated from each other
by a notch in the tape, preferably 10.0 ± 1.0 mm
wide. It allows to adjust the tension of the tape
separately along its upper and lower edges, also for
avoiding warping tape while fixing it on the
patient’s head.
As a result, the perimeter of the tape in the
buttoned state can vary in the range of 550-600 mm
and can be chosen individually for each patient. The
distance can be 20.0 ± 2.0 mm between the holes of
the electrodes. The attachment points of the outside
electrodes on the left and right sides of the tape (four
electrodes on each side) are used for registration the
pulse volume of the internal carotid artery, the
anterior cerebral artery and the middle cerebral
artery.
Figure 3: The elastic tape as electrodes device.
The holes for mounting the electrodes can have a
diameter of Ø7.0 ± 0.7 mm. Each hole for mounting
the electrode can be equipped with an insulating
stopper, which allows to mount reusable metal
electrodes.
Four plates (pos.3 in the Figure 3), made, for
example, of ABS plastic (acrylonitrile butadiene
styrene), are fixed on the tape. The location of the
plates in the device is selected in accordance with
the anatomical location of the ophthalmic artery.
Each plate can be located at a distance of 25.0 ± 2.5
mm from the horizontal symmetry axis of the tape.
Each plate has two holes for fixing the electrodes.
One of the holes is taken out of the tape’s borders,
and the other coincides with the corresponding hole
in the tape.
The mounting holes for the electrodes preferably
have a diameter of Ø7.0 ± 0.7 mm. Each hole of the
electrode can be equipped with an insulating stopper
in the case of mounting reusable metal electrodes.
2.3 Using in Clinical Practice
The device is used as follows: a device with
electrodes located in it, fixed on an elastic tape and
its plates, is mounted on the patient's head in the
periorbital region (on the closed eye). The location
of the plates is determined in accordance with the
patient's nasal bone - the plates should be placed at a
distance of 15 ± 3 mm from the nasal septum.
Further, fixation on the patient's head is carried out
with the help of Velcro elastic tape. After that, the
device is ready for operation and further connection
to the device of recording electrical impedance
signals.
While using the device, it is possible to
simultaneously obtain quantitative parameters of the
blood flow in the ophthalmic artery and the blood
flow in the vessels of the anterior part of the brain.
An example of the electrodes positioning scheme
is shown at the Figure 4. This example shows use of
the device for studying the left hemisphere of the
brain. The scheme for studying the right hemisphere
is symmetric relative to the sagittal plane.
In our research, TP ROG signals were analyzed
in a group of patients without an
ophthalmopathology. In total, four pairs of records
with duration of two minutes each were analyzed.
Each pair contained TP ROG signal (as in the Figure
1) and ROG signal from new electrodes device (as
shown in the Figure 4).
Figure 4: The registration of impedance signals for
studying the left hemisphere of the brain.
BIODEVICES 2019 - 12th International Conference on Biomedical Electronics and Devices
258
This study was performed in accordance with the
Declaration of Helsinki and was approved by the
Local Committee of Biomedical Ethics of the
Moscow Helmholtz Research Institute of Eye
Diseases. A written informed consent was obtained
from all participants.
3 RESULTS
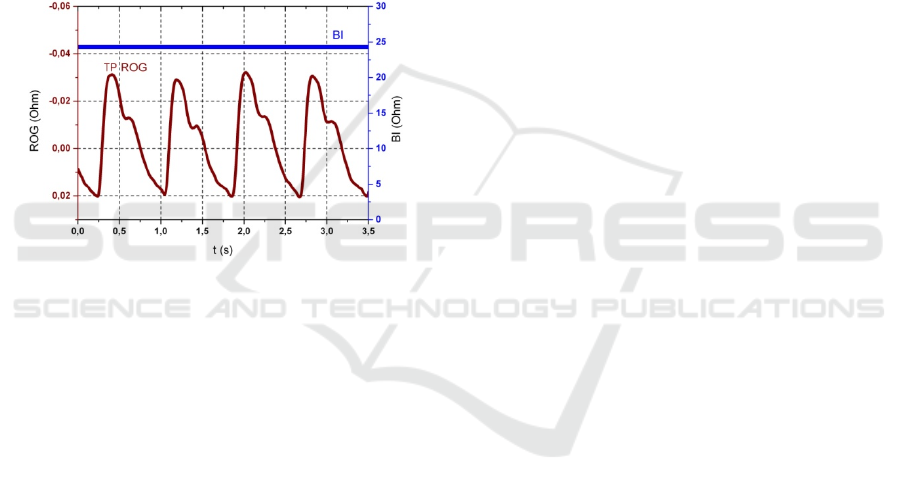
The example of typical TP ROG signal, which is
recorded in the 29 years old patient without an
ophthalmopathology, is shown in the Figure 5. TP
ROG signal shows blood flow pulse oscillations.
Base impedance (BI) reflects blood filling level of
eyes tissues.
Figure 5: The example of TP ROG signal.
The results of using our electrodes device with
such an arrangement of a tape with electrodes
showed compliance with theoretical calculations
which were obtained on the basis of a mathematical
model (Shamaev et al., 2017) for TP ROG.
Value of BI parameter at blood flow research in
the ophthalmic artery was 30-42 % above, than at
research of an eye by a technique TP ROG. This
result coincides with a theoretical estimation which
gives increase of a base impedance parameter in this
case.
4 CONCLUSIONS
The constructed device provides the ability for
conducting multichannel electrical impedance
studies in ophthalmology, with simultaneous
assessment of blood flow in the orbital artery
without contact with the eye surface, as well as in
the vessels of the anterior part of the brain, which
can have great importance in clinical practice - for
the diagnosis of eye diseases and control the
effectiveness of their treatment.
CONFLICT OF INTEREST
The authors declare that they have no conflict of
interest. The paper was supported by a grant from
RFBR (No.18-08-01192).
REFERENCES
Avetisov, E.S., Katsnelson, L.A., Savitskaia, N.F. (1967)
Rheocyclographic examinations in myopia. Vestnik
Oftal’mologii 80(3), 3–7.
Bodo, M. (2010) Studies in Rheoencephalography.
Journal of Electrical Bioimpedance 1, 18–40.
Calvo, P. et al. (2012) Predictive value of retrobulbar
blood flow velocities in glaucoma suspects. Investig.
Ophthalmol. Vis. Sci. 53, 3875–3884.
Caprioli, J., Coleman, A. L. (2010) Blood Pressure,
Perfusion Pressure, and Glaucoma. Am. J.
Ophthalmol. 149, 704–712.
Cherecheanu A.P., Garhofer G., Schmidl D., Werkmeister
R., Schmetterer L. Ocular perfusion pressure and
ocular blood flow in glaucoma. CurrOpinPharmacol.
2013; 13: 36-42. DOI: 10.1016/j.coph.2012. 09.003.
Kiseleva A., Luzhnov P., Dyachenko A. and Semenov Y.
(2018). Rheography and Spirography Signal Analysis
by Method of Nonlinear Dynamics. In Proceedings of
the 11th International Joint Conference on Biomedical
Engineering Systems and Technologies - Volume 1:
BIODEVICES, ISBN 978-989-758-277-6, pages 136-
140. DOI: 10.5220/0006579301360140.
Kiseleva, T.N. (2004) Ultrasonic methods blood flow
studies in the diagnosis of ischemic lesions of the eye.
Bulletin of Ophthalmology 4: 3-5.
Kiseleva, T.N., Adzhemyan, N.A. (2015) Methods for
assessing ocular blood flow in vascular eye pathology.
Regional blood circulation and microcirculation 4: 4-
10.
Kurysheva, N.I., Trubilina, A.V., Maslova, E.V. (2017)
Optical coherent tomography - angiography and
pattern-electroretinography in early diagnosis of
glaucoma. Glaucoma news 1: 66-69.
Lazarenko, V.I., Komarovskikh, E.N. (2004) Results of
the examination of hemodynamics of the eye and brain
in patients with primary open-angle glaucoma. Vestnik
Oftal’mologii 120(1), 32–36.
Lazarenko, V.I., Kornilovsky, I.M., Ilenkov, S.S. et al.
(1999) Our method of functional rheography of eye.
Vestnik Oftal’mologii 115(4), 33–37.
Luzhnov P.V., Shamaev D.M., Iomdina E.N., Markosyan
G.A., Tarutta E.P., Sianosyan A.A. (2017) Using
quantitative parameters of ocular blood filling with
transpalpebralrheoophthalmography. In: Eskola H.,
Väisänen O., Viik J., Hyttinen J. (editors). EMBEC &
Electrodes Device for Impedance Diagnostics of the Blood Flow in the Ophthalmic Artery
259

NBC 2017. IFMBE Proceedings, vol. 65; p. 37–40,
DOI:10.1007/978-981-10-5122-7_10.
Luzhnov P.V., Shamaev D.M., Iomdina E.N., Tarutta E.P.,
Markosyan G.A., Shamkina L.A., Sianosyan A.A.
(2015) Transpalpebral tetrapolar reoophtalmography
in the assessment of parameters of the eye blood
circulatory system. Vestnik Rossiiskoi akademii
meditsinskikh nauk 70(3): 372–377,
DOI:10.15690/vramn.v70i3.1336.
Luzhnov P.V., Shamaev D.M., Kiseleva A.A. et al. (2018)
Using nonlinear dynamics for signal analysis in
transpalpebral rheoophthalmography. Sovremennye
tehnologii v medicine 10(3): 160-167,
DOI:10.17691/stm2018.10.3.20
Luzhnov P.V., Shamaev D.M., Kiseleva A.A., Iomdina
E.N. (2018), Analyzing rheoophthalmic signals in
glaucoma by nonlinear dynamics methods. IFMBE
Proceedings 68/2: pp.827-831. DOI: 10.1007/978-
981-10-9038-7_152.
Machekhin, V.A., Vlazneva, I.N. (2009) Study of the
blood supply to the eye using color ultrasound
dopplerography. Siberian National Medical Journal 4:
100-103.
Patterson, R. (2005) Electrical Impedance Tomography:
Methods, History, and Applications (Institute of
Physics Medical Physics Series), Physics in Medicine
and Biology 10: 2427-2428.
Quigley, H. A., Broman, A. T. (2006) Number of people
with glaucoma worldwide. Br. J. Ophthalmol. 90,
262–267.
Shamaev D. M., Luzhnov P. V., Iomdina E. N., (2018),
Mathematical modeling of ocular pulse blood filling in
rheoophthalmography. IFMBE Proceedings 68/1,
pp.495–498. DOI: 10.1007/978-981-10-9035-6_91
Sokolova, I.V., Yarullin, K.K., Maksimenko, I.M.,
Ronkin, M.A. (1977) Analysis of the structure of
rheoencephalogram as a pulse filling of blood. Journal
of Nevropathol 77, 1314–1321.
Venkataraman, S. T., Flanagan, J. G. & Hudson, C.
(2010) Vascular Reactivity of Optic Nerve Head and
Retinal Blood Vessels in Glaucoma- A Review.
Microcirculation 17, 568–581.
Yarullin, K.K., Krupina, T.N., Alekseev, D.A. (1980)
Rheo- and encephalographic criteria for diagnosing
latent cerebral circulation insufficiency in patients
with cervical osteochondrosis. Sovetskaya Meditsina
43(3), 9–15.
BIODEVICES 2019 - 12th International Conference on Biomedical Electronics and Devices
260
