
Conceptualization of WECARE: A Community-based Platform for
Minimizing Consequences of Fall in Elderly People
Tanawat Chansophonkul
1
, Jean Baptise Dusenge
1
, Daniel Pichler
2
, Volha Samusevich
3
,
Anatole Jimenez
4
, Séverine Koeberle
5,6
, Régis Aubry
5,6,7
, Thomas Lihoreau
5
and Thomas Tannou
5,6,7
1
Institut Supérieur d'Ingénieurs de Franche-Comté, University of Franche-Comté, Besançon, France
2
School of Medicine, Technical University of Munich, Munich, Germany
3
Business Administration and Innovation in Healthcare, Copenhagen Business School, Frederiksberg, Denmark
4
Engineering for Health, Université Pierre et Marie Curie, Paris, France
5
CHU Besançon, Inserm, CIC 1431, Centre d'Investigation Clinique, Besançon, France
6
Geriatric Department, University Hospital of Besançon, Besançon, France
7
EA 481 Neurosciences, UBFC, Besançon, France
Keywords: Assisted Living, Geriatrics, Mobile Applications, Elderly, mHealth, Community-based Care.
Abstract: The number of aged population is growing consistently, and is expected to triple by few next decades. One of
the most threatening risk aged population have to face in their daily life is falling. Falling can pose serious
injuries and consequences to elderly people, especially when they live alone or have cognitive dysfunction. If
the elderly lives alone when an accident happens, it is more likely to take a long time until someone notices
and provides rescue. Moreover, if the elderly has cognitive disorder such as Alzheimer’s disease, it is possible
that he or she will not try to seek help. In this paper, an online platform called WECARE is proposed.
WECARE aims to minimize the consequence of delayed rescue after a fall accident. The main advantage of
the platform is the integration of community volunteers into the already widespread technologies such as fall
detection systems and automatic doors. The benefits of volunteers could be a faster response after a fall
accident and social connection provided to elderly people, especially the ones who live alone. This paper also
describes how the idea was originated, modified, and improved through methodology. It also discusses
advantages of the platform, limitations, as well as its future.
1 INTRODUCTION
In the world, the proportion of elderly people is
increasing in almost every country. The number of
people aged 65 or above was 615 million in 2017, and
expected to rise to 1,6 billion in 2050 (Wan et al.,
2016). The world is transforming into an aging
society. In France, the percentage of elderly age 65 or
above is 18,8% of the total population, which means
12.5 million people in total (Eurostat, 2016). Many of
the elderly people want to remain autonomous and to
stay independent as long as possible. In comparison
to retirement homes, they prefer to stay at home
(Boland et al., 2017). However, by staying at home,
elderly are exposed to the risk of facing an accident
without receiving help. And one of the said accident
is fall. Fall is very common, 30% of the elderly fall
each year, and up to 10% of the falls can lead to
severe consequences like head injury and bone
fracture (Silvia et al., 2010).
A factor contributing greatly to the severity of fall
in elderly people is the time that elderly spend on the
floor after the fall. Indeed, some of the elderly will
not be able to get up without help and therefore spend
long time lying on the floor. When elderly fall and
spend time on the floor for more than one hour, they
can develop rhabdomyolysis, pressure sore, and
dehydration (Mallison and Green, 1985; Tinetti et al.,
1993). Other than physical injuries, fall can cause
psychomotor disadaptation syndrome, and
posttraumatic stress disorder (Eric et al., 2010). Also,
when elderly fall and spent a long time on the floor,
they are five times more likely to die within six to
twelve months in comparison to the elderly in the
same age and gender group who did not experience a
fall (Wild et al., 1981). Falls are caused by
Chansophonkul, T., Dusenge, J., Pichler, D., Samusevich, V., Jimenez, A., Koeberle, S., Aubry, R., Lihoreau, T. and Tannou, T.
Conceptualization of WECARE: A Community-based Platform for Minimizing Consequences of Fall in Elderly People.
DOI: 10.5220/0007685505870594
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 587-594
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
587

multifactorial parameters in older adults, with
dementia increasing the number of falls significantly
(Fernando et al., 2017; Petersen et al, 2018).
Moreover, cognitive impairment is a factor that
contributes to both prevalence of falls and inability to
get up after falls (Jane and Carol, 2008).
The first data provided by the exploration of
seniors' perceptions of the behavioural factors
associated with falls (Robson et al., 2018) shows the
importance of maintaining elderly’s independence
despite the risk of falling. Unfortunately, for reasons
of safety, instead of giving them home-care, relatives
may decide to admit elderly people to retirement
homes (Lord et al., 2016). Cognitive impairment
could be a reason given by families to do so despite
the patient's willingness to stay at home (Lord et al.,
2015). Thus, promoting home care for the elderly
leads to the question of fall management, from
detection to care.
Out of 12,5 million elderly which live in France,
37,5% of them live alone (Eurostat, 2015). Living
alone not only makes them prone to lie on the floor
for a long time without anyone noticing but also
subjects them in their daily routine to the possibility
of social isolation. Many research has shown that
social isolation and loneliness can have negatives
effect on health and wellbeing of people (Hanbyul et
al., 2015; John et al., 2011; Tomaka et al., 2006). On
the contrary, social activities and human interaction
can promote good health and preserve cognitive
function (Glei et al., 2005; Joe et al., 2003). In this
context, caregivers involvement, both formal and
informal, can be a way to provide elderly people with
care and social interactions.
Therefore, it would benefit the society and seniors
greatly, especially those with dementia, if we could
provide them a fall detection environment offering
fast rescue, respecting their privacy and preventing
the negative effects of social isolation by giving them
the social context.
2 TECHNOLOGICAL CONTEXTS
At present, there is no system which represents as the
gold standard for minimizing consequences of fall.
To address the fall problems, one topic that is widely
researched and developed is the use of fall detection
systems which can be generally represented as shown
in Figure 1. In the market, there are various
companies that offer active fall detection systems
which require interactions from users. The active
devices are usually presented as a wearable devices
such as wrist watches or pendants incorporate with a
trigger button that is pushed by users in case of fall
accident (Muhammad and Ling, 2013). However, the
situation is more complex for elderly with dementia,
because they can easily forget to wear or how to
operate the device (Koldo et al., 2017).
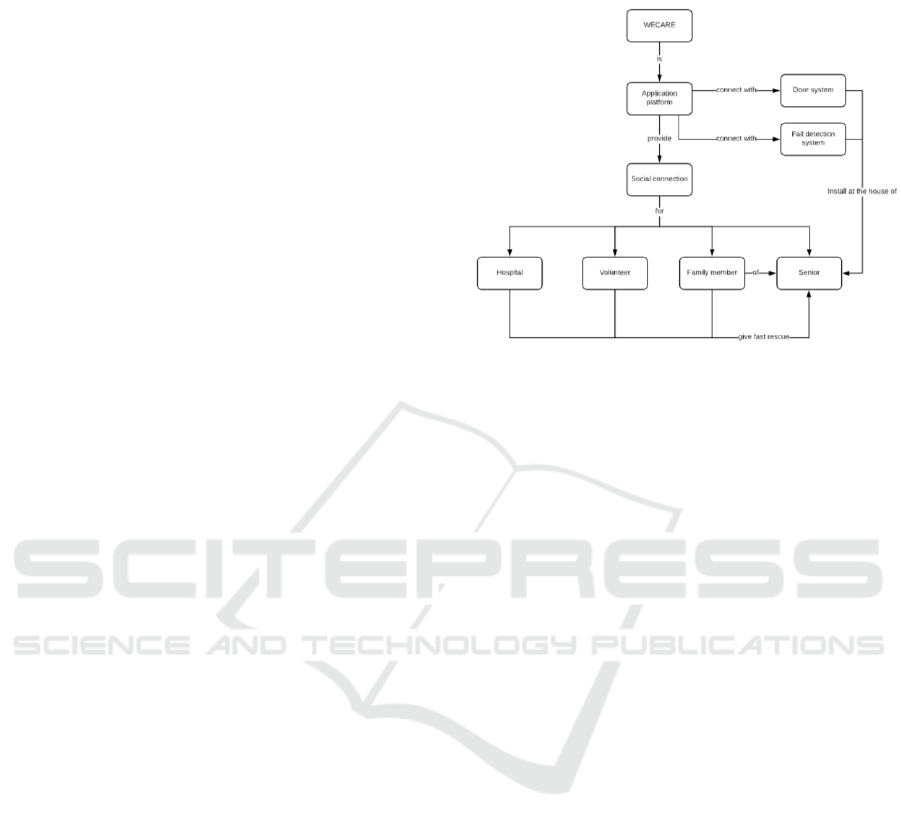
Figure 1: General representation of a fall detection system.
Another approach is a passive system which can
be classified by the type of sensor, such as cameras,
kinect cameras, floor-embeded sensors, or
microphone arrays (Natthapon, 2014). The passive
fall detection system can be a more logical solution
for elderly people with dementia due to the fact that it
requires no interactions from the users both in cases
of normal usage and in events of fall. However, some
of the solutions are considered as too privacy-
intrusive, especially the cameras or microphones
based solutions (Brownsell and Hawley, 2004).
Therefore, the privacy of elderly, acceptability of the
devices and how the elderly with dementia react to
the technologies are important factors that need to be
considered.
Following the advancement of information
technology in health care, the involvement of non-
professional in out-of-hospital care services is
increasing (Elina, 2017). Although not in the context
of fall, there have been several projects that
successfully integrating volunteers into the system.
They are mobile-based alert systems for out-of-
hospital cardiac arrest. Non-professional personnel,
including laypersons and trained-volunteers, will be
notified and dispatched to act as a fast respondent in
cases of cardiac arrest. These systems showed
promising results in increasing survival rate of the
cardiac arrest victims and reducing the responding
time lag following the incident (Mattias et al., 2015;
Pijls et al, 2016; Christopher et al., 2017).
Fall accident
Data measured by sensors
Processing
Send alert
Family members
Caregivers
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
588

In this paper, the development of a platform called
WECARE is presented. It was initiated during a
summer school event promoted by EIT Health
(European Institute of Innovation & Technology for
Health) which is a European health innovators
network. The proposed solution is a platform which
integrated volunteer networks and a mobile phone
application that can connect with specified fall
detection systems and automatic doors installed in the
house of elderly people.
3 METHODOLOGY
The concept of WECARE platform originated from a
multidisciplinary team composed of a medical
student, a healthcare business analyst, a healthcare
technologist and biomedical engineers. With the help
of open innovation events as well as specific project
management, the concept was developed through
means and methods described as follow.
3.1 ClinMed
ClinMed2018 was a summer school organized by
clinical investigation center in innovative
technologies (CIC-IT) national network and held in
France (ClinMed, 2018). It was the first ClinMed
summer school with the objective of providing
participants with perspective of how to develop an
idea in the field of innovative technologies for health,
from initial concept until reaching the market.
The summer school was organized into two
phases. The first phase allowed the participants to
experience and perceive the problems from an actual
perspective. The second phase focused on incubating
and developing the idea into a concrete concept.
In the first phase, the team was given a subject by
geriatricians, aiming to minimize the severity of fall
in elderly people suffering from dementia and living
alone. To understand more the issues and needs
related to the ageing society and the loss of autonomy,
the team spent three days of immersive experience in
the geriatric department of university hospital of
Besançon, France, and with methodological supports
from CIC INSERM 1431. Several meetings were
conducted in order to gather requirements and needs
from every stakeholders including healthcare
providers, medical doctors, patients, and their family
members.
Visiting of geriatric care units and retirement
homes, along with explanations and inputs from
geriatrician provided great benefits to the first
conceptualization of a solution. Moreover, to
understand what ageing is, the team experienced the
aging simulation arranged by the geriatric
department. The experiences consisted of several
activities performed while wearing handicapped-
equipment such as weighted outfits and blinded
goggles. This kind of simulation aimed to make
participants realize and understand the feeling of aged
body and associated impairments.
During requirement gathering, the preservation of
autonomy and security of people with dementia came
out as the main needs. Although there are a lot of
technological solutions for fall accident, privacy
invasion and cognitive dysfunction of people with
dementia are major obstacles for dissemination. A
suitable solution needs then to find an agreeable
balance between security and privacy of users.
The approach of brainstorming was used in order
to find the suitable solution for the problem. Every
possible ideas were proposed by team members. The
second step consisted in selecting the most suitable
ideas that the entire member agreed on. Although the
issue of security-privacy balanced was not clearly
settled, the first idea of solution was then proposed.
Thus, originated the idea of a system that aim to
minimize the lag time between fall accident and
rescue attempt, and it is called WECARE.
The second phase of ClinMed2018 was a seven-
day incubation process to develop further the first
solution into a concrete and tangible concept. Under
lessons, guidance and advices from experts in various
fields, the first idea of WECARE was improved. The
improvement of the concept was then done with the
help of a team of mentors composed of clinicians,
regulatory affairs specialists, experts in quality
management system of medical devices, business
analyst, and clinical research specialists.
After the second phase of ClinMed2018, the
problem of balance between privacy and security was
addressed. With the summer school event, the various
aspects of WECARE along the life cycle of the
product were considered and the concept of the
solution was designed. Thus the next step was to
develop a first prototype.
3.2 Hacking Health Besançon
Hacking Health is an event organized in order to bring
together all the stakeholders in healthcare domain to
tackle the problem of healthcare (Hacking Health
Besançon, 2018). With various key players, this event
can provide funding opportunities, resources, and
help incubating ideas for new healthcare innovation
especially for projects owned by an independent party
(Walker et al., 2016).
Conceptualization of WECARE: A Community-based Platform for Minimizing Consequences of Fall in Elderly People
589
To go on with the design and development of a
first prototype of WECARE, a team of software
developer was required. As the initial team did not
possess the skill required, an event like Hacking
Health Besançon presented a great opportunity.
During the event, a team was formed, composed of
people from the initial team WECARE and a group of
back-end and front-end developers. After two days in
the event, the main principle of WECARE platform
was defined, the system was designed and an early
prototype was developed in the form of a mobile
application. The aim was to demonstrate the function
of WECARE platform and to further facilitate the
development. WECARE was awarded by juries with
the “Best patient-centric solution” prize given by the
representative of patient association. This led to the
possible cooperation of targeted patients in the
development processes so that the product will be
well received by the end-users.
3.3 Preparation for Calls
Following Hacking Health, a larger team was formed.
It included members from research and evaluation
center, biomedical and computer engineers from
engineering schools, and patient representatives.
After that, a new and more detailed development
plan was structured in order to allow the preparation
for the calls from EIT Health and French national
research agency which can potentially provide the
project with necessary funding and partnerships. The
development plan is briefly explained in the
subsection §6.4.
4 RESULT
After the conceptualization steps, WECARE was
defined as a platform that connects with ambient fall
detection systems and automatic doors installed in the
user’s house. The aim of the platform is to integrate
all the people including healthcare providers,
volunteers in the community, family members and
senior peoples themselves into the system, and to
facilitate a fast rescue in case of fall accidents. When
there is a fall, WECARE will inform the elderly’s
family and the nearest available volunteers to the
patient so that they can provide a fast intervention
with the help of geo-localization and automatic home
accessed permission. Moreover, by integrating
volunteers and involved parties, the system also aims
to provide social connections and all the linked
benefit to both seniors and community around them.
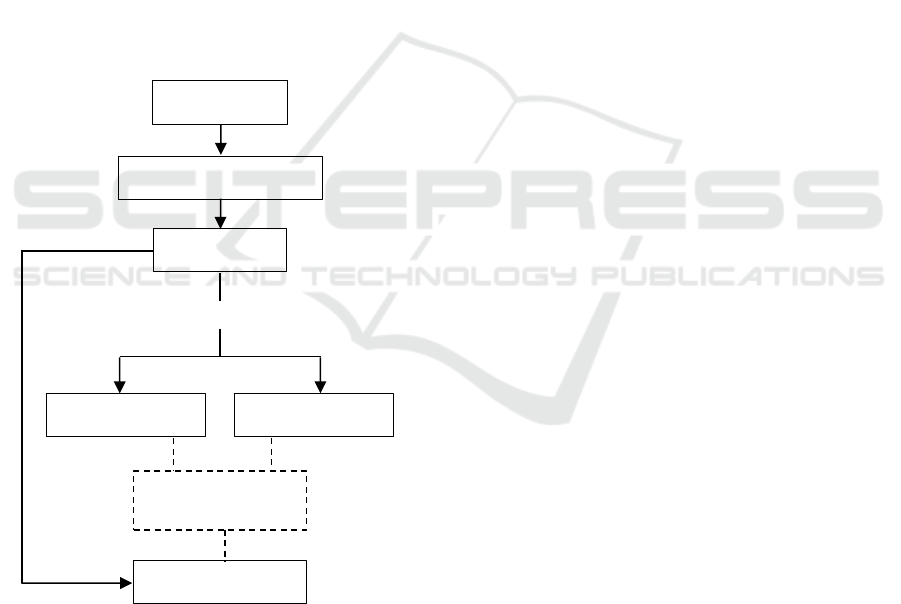
The concept of the platform is represented as a
map in Figure 2.
Figure 2: Concept map of WECARE.
4.1 Main Working Principle
When a fall accident happens, WECARE application
will get a trigger signal from ambient fall detection
sensors installed at the user’s residence. The
application will then send a notification to family
members of the elderly.
After receiving the notification, the family
members will decide if they can go to see their elder
or not. If not, the notification will be forwarded to the
nearest volunteer or nearby hospital depending on the
availability of volunteers. The rescuer will receive
information about the address location in the form of
GPS map.
The rescuer will be able to enter the house with
the automatic door and provide help if possible. In
case of volunteer involvement, WECARE application
will allow him to communicate with patient’s family
and nearby hospitals staff. The working principle of
WECARE is shown in Figure 3.
4.2 Volunteers
WECARE platform will be used by volunteers who
want to be the rescuer for elderly people in case of fall
accident. The first step to become a volunteer is to
create an account by filling all the information and
upload all identification documents requested by the
system. Once the requested document and
information are properly validated and confirmed, he
will get the confirmation email of successful
registration; he/she could be asked to provide the
missing information or document.
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
590
Once the registration is confirmed, the volunteer
will have access to an online training of WECARE
platform. The training will include recommendations
for system usage as well as guidelines of patients
rescuing procedure. After the training, there will be a
meeting between seniors, family members,
volunteers and healthcare providers. This will initiate
and strengthen the connection between people and
community. Finally, after confirmation and consent
from the elderly and family members, the volunteer
will be included in WECARE platform.
WECARE considers the social aspect
representing by the volunteers’ involvement as its
main advantage. The platform not only focused on
technology but also creating link between generations
and improving safety for seniors in the community.
Even in cases of false alarm which is currently a
problem for fall detection systems, with volunteers
involved, it can be turned into an opportunity to
connect elderly people with the volunteers to prevent
social isolation.
Figure 3: Working principle of WECARE.
4.3 Security-privacy Balance
The platform aims to provide security for elderly
people while respecting their privacy. The most
important part is that volunteers should be someone
that elderly people and their family members trust.
Therefore, to mitigate this problem, family members
will have options to predetermine the preferred
volunteers or avoid unwanted ones. In this way, the
platform facilitates the acceptance and respect the
consent of the users.
5 DISCUSSION
In conceptualization steps, WECARE is a platform
that can provide numerous great benefits to both
elderly people and the community around them. It
aims to be a central piece by connecting already
existing fall detection technologies and automatic
door systems to facilitate a fast rescue. By integrating
community volunteers into the technological
solutions, the platform will be able to minimize the
time patients spend on the floor after fall accidents. It
also has a potential to provide social context and
prevent isolation for elderly people who live alone.
However, WECARE is not without its limitations.
The upcoming challenge of the system will be
compatibility of the platform with the already existing
technologies, both fall detection sensors and
automatic doors. The implementation of the whole
system to the already existing buildings could be
difficult and possibly expensive. The management of
signal that originate from various type of fall
detection sensors will be a crucial step that needed to
be considered.
The main advantage of WECARE relies on the
social aspect, however the idea of letting someone
who is not a family member into the house of elderly
people is a bit ambitious, unless that such a volunteer
is a trusted person like caregiver and healthcare
provider. The creation and management of the
volunteer network will be a challenging part of the
project as well as how to make the system more
acceptable for users. By continuous questioning and
evaluation of the solution in terms of how sufficient
(number and quality) is the network, will without a
doubt lead to its improvement along all the life cycle
of the project.
6 FUTURE WORKS
The next steps of the work will focus on the
connectivity of the platform to the rest of the systems
including fall detection sensors and automatic doors.
Other issues that will need to be developed are the
ethical aspect as well as usability and acceptability of
the solution, and finally, to develop the volunteer
network.
Fall accident
Data processed by sensors
Send alert
Family members
Nearest volunteers
Family members are available?
yes
no
Healthcare providers
Shared contact
information
Conceptualization of WECARE: A Community-based Platform for Minimizing Consequences of Fall in Elderly People
591

6.1 Fall Detection Sensors
WECARE aims to connect with ambient fall
detection sensors which are sensors that are directly
installed in the environment of the users. Due to
cognitive dysfunctions of dementia patients, wearable
devices are ill suited because the interactions with the
device can be perceived as too complex. Therefore, it
raises the issue of integration to WECARE. Another
requirement for the sensors is that they should not be
perceived by users as invasion of their privacy, such
as camera-based sensors.
6.2 Automatic Door Systems
It is important to consider the type of automatic doors
to be used depending on the location where they are
going to be installed. A private location such as single
house will pose little to no problem for the
installation. However, if the location is an apartment
or shared residence, the problem could become much
more complex due to the possibility of having more
than one-layer access such as a common door before
entering the apartment. Other solution apart from the
doors, such as key-containing boxes, should be
considered.
Specifications of WECARE system will then take
into account the existing possibilities for both fall
detectors and automatic doors, in order to select the
most relevant ones and manage communications with
the more efficient technologies.
6.3 Ethics and Acceptability
Other essential aspects are ethics, acceptability, and
usability of the solution. During the successive
development phases of WECARE, surveys, tests, and
evaluations should be done to further improve the
concept of the system. The usability, acceptability
and ethical aspect of the platform should be
evaluated. Moreover, as some users of WECARE can
consist of dementia patients, more investigations into
concerned laws and regulations will be needed.
Further explorations will evaluate usability and
acceptability of the platform as perceived by all the
users. Finally, specific evaluations will permit the
quantification of the security, clinical efficiency and
possible economic impacts of the solution.
6.4 Development Plan
As a result of various events, consultations with
experts, and continuous reformation of the project,
the next steps of WECARE were planned as follow.
6.4.1 Literature Review
A systematic literature review and an analysis of
state-of-the-art are essential for the early stage of the
project. Following PRISMA guidelines (Moher et al.,
2015), the reviews will provide insights on the
existing technologies and present the opportunities to
identify advantages and disadvantages of other
similar community-based projects. The important
aspect of community-based system is the
sustainability of both end-users and volunteers.
6.4.2 System Development
Planification and development of the minimum viable
product (MVP) should be considered after the
literature review. MVP, a system with just enough
functions and features to answer the needs of users, is
needed in order to facilitate and conduct the necessary
studies which including feasibility and acceptability
studies. MVP should be a functional product which
included every possible parts of the full system
including server, application, website, and database.
6.4.3 Studies
The involvement of end-users in all of development
processes is very crucial, especially in the feasibility
study. To test the feasibility of the system in the first
phase of the study, the targeted populations can be
elderly people without dementia and people from
their community. Then, in the second phase of the
study, the targeted populations will be elderly people
with dementia, their family, and volunteers. The
project will be assessed and redesigned with
cooperation of this user group.
6.4.4 Economics
The economic aspects of the project will be taken into
account in parallel with feasibility studies. Business
model, operating costs, and reimbursement plan of
the product will be elaborated in order to ensure not
only the economic feasibility of the product but also
to ensure the sustainability in the long run.
7 CONCLUSION
For aged population, the severity of fall accident
depends not only on the impact force of the fall, but
also on the time patients spend on the floor without
rescue. The more time spending on the floor, the more
complicated the treatment will be.
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
592

Through open innovation events and strong
methodology, WECARE project and solution was
conceptualized. ClinMed2018 summer school
initiated the designation of the first concept while
Hacking Health Besançon allowed the development
of the first prototype. This resulted in the definition
of a team with multiple skills, including a
representative of end-users. This made it possible to
draw up a detailed development plan, including
feasibility studies.
WECARE intends to be a platform which aims
to reduce the time patient spend on the floor by
introducing the connection of fall detection sensors
with automatic door systems to facilitate an easy
rescue operation. In addition, the integration of
volunteers into already existing technologies and
rescue procedures can shorten the lag-time between
the accident and the first intervention. It can also
provide social benefits for elderly people even in case
of a false alarm of falls while respecting ethical issue.
This paper proposed the first conceptualization
of the WECARE platform and issues that need to be
addressed before progressing into the next steps of
development. Especially the challenges of legal
considerations regarding the consent of the elderly
people with dementia to use the platform, as well as
the approach to implement protection necessary for
this group of users. Evaluations will also take an
important part in the developments. Such reflexions
and integration of technologies can bring benefits and
care to our aging population.
Finally, this paper proposed also a methodology
for conceptualization of a project. Through the
example of WECARE, each step of how the project
was originated and improved were explained in the
hope that this paper can help facilitate the genesis of
relevant innovations in the field of healthcare.
REFERENCES
Boland, L., et al., 2017. Impact of Home Care Versus
Alternative Locations of Care on Elder health
outcomes: an overview of systematic reviews, BMC
Geriatrics, 17(20).
Brownsell, S., and Hawley, M., 2004. Fall Detectors: Do
They Work or Reduce the Fear of Falling?, Housing,
Care and Support, 7(1), pp.18-24.
Christopher, M. S., et al., 2017. The Use of Trained
Volunteers in The Response to Out-of-hospital Cardiac
Arrest - The GoodSAM Experience, Resuscitation, 121,
pp. 123-126.
Clinmed, 2018. Innovative Technologies in Health; From
the Idea to the Market. Available at:
https://clinmed2018.sciencesconf.org (Accessed: 20
November 2018)
Elina, R., 2017. Using Volunteers for Emergency Response
in Rural Areas: Network Collaboration Factors and IT
support in the Case of Enhanced Neighbors, ISCRAM
Association, 14, pp. 985-995.
Eric et al., 2010. Analysis of Postural Control in Elderly
Subjects Suffering from Psychomotor Disadaptation
Syndrome (PDS), Archives of Gerontology and
Geriatrics, 51(1), pp. e19-e23.
Eurostat, 2016. A Look at the Lives of the Elderly in the EU
Today: What is The Share of the Elderly (65 or Over)
Among The Total Population?. Available at:
ec.europa.eu/eurostat/cache/infographs/elderly/index.h
tml (Accessed: 25 November, 2018).
Eurostat, 2015. A Look at the Lives of the Elderly in the EU
Today: What is the share of the elderly who live alone?.
Available at: ec.europa.eu/eurostat/cache/
infographs/elderly/index.html (Accessed: 25
November, 2018).
Fernando, E., et al., 2017. Risk Factors Associated with
Falls in Older Adults with Dementia: A Systematic
Review, Physiother Can, 69(2), pp. 161-170.
Glei, D.A., et al., 2005. Participating in Social Activities
Helps Preserve Cognitive Function: An Analysis of a
Longitudinal, Population-Based Study of the Elderly,
International Journal of Epidemiology, 34(4), pp. 864-
71.
Hacking Health Besançon, 2018. What is Hacking Health?
Available at: https://hacking-health.org/fr/besancon-fr/
(Accessed: 20 November 2018)
Hanbyul, C., et al., 2015. Impact of Social Isolation On
Behavioral Health in Elderly: Systematic Review,
World J Psychiatr, 5(4), pp. 432-438.
Jane, F., and Carol, B., 2008. Inability to Get Up After
Falling, Subsequent Time On Floor, And Summoning
Help: Prospective Cohort Study in People Over 90,
BMJ, 337(a2227).
Joe, V., 2003. Leisure Activities and the Risk of Dementia
in the Elderly, The New England Journal of Medicine,
2003(348), pp. 2508-2516.
John, T.C., et al., 2011. Social Isolation, Annals of the New
York Academy of Sciences, 1231(2011), pp. 17-22.
Koldo, M., et al., 2017. Home Camera-Based Fall Detection
System for the Elderly, Sensors, 17(12), pp 2864.
Lord, K., Livingston, G., and Cooper, C., 2015. A
Systematic Review of Barriers and Facilitators to and
Interventions for Proxy Decision-making by Family
Carers of People with Dementia, International
Psychogeriatrics, 27(8), pp 1301-1312.
Lord, K., Livingston, G., Robertson, S., and Cooper, C.
(2016). How People with Dementia and Their Families
Decide About Moving to A Care Home and Support
Their Needs: Development of A Decision Aid, A
Qualitative Study, BMC Geriatrics, 16, 68.
Mallison, W. J. W., and Green M.F., 1985. Covert Muscle
Injury in Aged Patients Admitted to Hospital Following
Falls, Age and Ageing, 14(3), pp. 174–178.
Mattias, R., et al., 2015. Mobile-Phone Dispatch of
Laypersons for CPR in Out-of-Hospital Cardiac Arrest,
Conceptualization of WECARE: A Community-based Platform for Minimizing Consequences of Fall in Elderly People
593

The New England Journal of Medicine, 372, pp. 2316-
2325.
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati,
A., Petticrew, M., Stewart, L. A. (2015). Preferred
reporting items for systematic review and meta-analysis
protocols (PRISMA-P) 2015 statement. Systematic
Reviews, 4, 1.
Muhammad, M., Ling, S., 2013. A Survey On Fall
Detection: Principles and Approaches,
Neurocomputing, 100, pp. 144-152.
Natthapon, P., et al., 2014. Automatic Fall Monitoring: A
Review, Sensors, 14(7), pp.12900-12936.
Petersen, J. D., Siersma, V. D., dePont Christensen, R.,
Storsveen, M. M., Nielsen, C. T., & Waldorff, F. B.,
2018. The risk of fall accidents for home dwellers with
dementia—A register-and population-based case-
control study, Alzheimer’s & Dementia: Diagnosis,
Assessment & Disease Monitoring.
Pijls, R. W., et al., 2016. A Text Message Alert System for
Trained Volunteers Improves Out-Of-Hospital Cardiac
Arrest Survival, Resuscitation, 105, pp. 182-187.
Robson, K., Coyle, J., and Pope, R., 2018. Exploration of
older people’s perceptions of behavioural factors
associated with falls. Age and ageing.
Silvia, D., 2010. Risk Factors for Falls in Community-
dwelling Older People: A Systematic Review and
Meta-analysis, Epidemiology, 21(5), pp. 658-668.
Tinetti M. E., et al., 1993. Predictors and Prognosis of
Inability to Get Up After Falls Among Elderly Persons,
JAMA, 269(1), pp. 65–70.
Tomaka, J., et al., 2006. The Relation of Social Isolation,
Loneliness, And Social Support to Disease Outcomes
Among the Elderly, Journal of Aging and Health,
18(3), pp. 359-384.
Walker, A., & Ko, N., 2016. Bringing Medicine to the
Digital Age via Hackathons and Beyond. Journal of
Medical Systems, 40(4), 98.
Wan, H., 2016. An Aging World: 2015, International
Population Reports. United States Census Bureau.
Washington D.C.
Wild, D., et al., 1981. How Dangerous Are Falls in Old
People at Home?. British medical journal, 282(6260),
pp. 266-268.
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
594
