
Pattern of Muscle Activation During Sit to Stand Task
in Feet Forward with 80° Knee Flexion using Surface EMG
Taufiq Nashrulloh
1
, Vitriana Biben
1
, Farida A Santi
1
, Rachmat G.Z
1
, Marina A Moeliono
1
, Dedy
H.B.Wicaksono
2
, Nabil el Hasnaoui
3
1
Department of Physical Medicine and Rehabilitation, Dr. Hasan sadikin General Hospital
University of Padjadjaran, Bandung, Indonesia.
2
Department of Biomedical Engineering, Faculty of Life Sciences and Technology,
Swiss German University (SGU) Tangerang, Indonesia
3
Biomedical Engineering, Delft University of Technology, Delft, Netherland
Keywords: Muscle Activation, sEMG, Sit to Stand
Abstract: The sit-to-stand (STS) in feet forward is one type of STS with a characteristic of delayed contraction of
Tibialis anterior. Surface EMG (sEMG) signals are recorded by non-invasive electrodes and are preferably
used to obtain information about the time or intensity of superficial muscle activation. This study aims to
find the pattern of muscle activation when STS in feet forward. This is a retrospective study using sEMG for
the pattern of muscle activation of 14 males and 14 females in Hasan Sadikin General Hospital Bandung
Indonesia, in March 2019. The average height, weight, body fat, and fat-free mass in men were significantly
different from women participants. The muscle activation of muscle group stabilizer (Rectus Femoris (RF)
and Biceps femoris lateral (BFL)) is bigger than muscle group sequence (Tibialis anterior (TA) and
Gastrocnemius medialis (GM) during STS in this research. Rectus femoris was the muscle that had the
highest mean maximum force in every STS phase. The mean maximum force of RF, BFL, and GM in
Phase II was the highest compared to another phase. On the other hand, the mean maximum force of TA
was the highest in Phase V. Feet Forward with 80° knee flexion is the strategy foot positioning during sit to
stand to increase the force of sequence muscle group than stabilizer muscle group
1 INTRODUCTION
Sit to stand movement is a movement that is
frequently done by people. This ability is an
important skill that is considered as a fundamental
task for daily activities and is a prerequisite for
functional independence. (Carr JH, 1992; Shepherd
RB & Koh HP, 1996; Ng, Shamay S M, et al, 2015).
Sit To Stand (STS) is a movement of the body’s
center of mass (CoM) upward from a sitting position
to a standing position without losing balance.
(Roebroeck et al, 1994) An individual needs to bring
his CoM from a relatively large and stable base of
support in sitting to a considerably smaller base of
support in standing. To achieve this transition, CoM
must first move forward then reach its maximal
velocity at the preparatory phase. At seat-off, CoM
switches into vertical movement and its velocity
continues to accelerate until it reaches a maximum
in the middle of the extension phase. Subsequently,
the CoM velocity decelerates progressively until
reaching zero, when the standing position is
achieved. (Hirschfeld, 1999).
In the literature, two ways to performed STS
define the strategy for implementing the STS task
were found. Defined as the “momentum-transfers
strategy,” the first method implies that the subject in
question makes a small trunk flexion of the weight
transferring forwards and then begins the separation
of the seat, ending with the starting foot. This form
is most common among healthy people. Another
way to make the sequence is increasing trunk flexion
before starting to move from the chair, which is
usually performed by people with muscle weakness
in the legs. If the results obtained in this study are
analyzed, in both groups four muscles act primarily
as stabilizers of motion (tibialis anterior, rectus
abdominis, soleus) and others that are responsible
82
Nashrulloh, T., Biben, V., Santi, F., GZ, R., Moeliono, M., Wicaksono, D. and Hasnaoui, N.
Pattern of Muscle Activation During Sit to Stand Task in Feet Forward with 80 Knee Flexion using Surface EMG.
DOI: 10.5220/0009064000820087
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 82-87
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
for implementing the sequence (quadriceps rectus
femoris, quadriceps vastus medialis and biceps
femoris. (Antoni I, 2013).
STS strategy related determinants such as speed,
foot positioning, trunk positioning, arm movement,
terminal constraint, fixed joint, knee position, and
training. (Lamberts, 2008) Individual normal
healthy, using 100o knee flexion during STS task
and shows muscle activation of stabilizer group
muscle is bigger than sequence group muscle.
(Antonio I et al, 2013; Brunt, 2002) Stroke patients
are reported have weakness in the lower extremity,
making it difficult to do STS. Sit to stand in stroke
patients is reported to have a longer duration than
normal. (Baukadida et al., 2015). It was reported that
in hemiplegia patients, usually using feet forward
strategy 750 knee flexion in foot positioning during
STS. The foot positioning of an uninvolved limb in
feet forward, an extended position (75o of knee
flexion) and normal position (100o of knee flexion)
in involved limb causes the activity muscle of the
sequence group bigger than stabilizer. (Brunt, 2002)
A step foot position during the STS task by
manipulating the foot placement of the unaffected
limb was proved will improving the static and
dynamic postural balance in patients with
hemiplegia (Han Jintae, Kim youngmi, Kim Kyung,
2015). Few studies have described the effect of the
nonparetic foot positioning during STS in patients
but there is no standardization about the degree of
foot positioning. Therefore, in this pilot study, we
want to investigate muscle activity of stabilizers
group muscle and sequence group muscle in STS
task in feet forward position (80o of knee flexion) in
healthy younger adults to add information about foot
positioning impact. Hopefully, the result will be
developed to a bigger study to find out the
standardization method of STS procedure that
effective for patients with stroke to achieve better
performance with their paretic limb.
2 METHODS
Twenty-eight participants, 14 males, and 14 females,
in Hasan sadikin Bandung Indonesia, General
Hospital were recruited in March 2019. Participants
were included if their age between 20-35 years old,
able to walk without an assistive device and had no
heart, vascular, lung or bone/joint problems that may
impaired standing activity from a chair. Participants
were excluded if have a musculoskeletal deformity,
muscle weakness, and pain. The study was approved
by the Faculty of Medicine Universitas Indonesia
ethical committee (No.0438/UN2.F1/ETIK/2018)
and written consent was obtained from all
participants prior take part in this study. Before
measurement was taken, each participant was given
an explanation about the sit to stand (STS) protocol
and make a trial of the movement for familiarization.
All of the participants were instructed to seat with
feet forward (800 knee flexion) in a chair without
arm support (F. R. Goulart and J. Valls-Sol´e, 1999).
Their arms were being folded across their chest in all
of the phases of STS, with their feet being open wide
align with the shoulder. Each subject performed
three times of STS with the speed transition of each
phase of STS indicated by a metronome. The values
considered for statistical analysis were the best score
of maximal voluntary contraction.
The muscle activity (MA) was recorded using
surface electromyography (sEMG) machine
(Gymna, type myo 200, Belgium). Muscles that
evaluated were muscle group sequences such as
Rectus Femoris (RF), Biceps Femoris (BFL), and
muscle group stabilizer such as Tibialis Anterior
(TA), Gastrocnemius (GM). On each muscle three
circular adhesive Ag-AgCl electrodes were placed
based on SENIAM (Surface EMG for non-invasive
assessment of muscles) protocol guidance at a
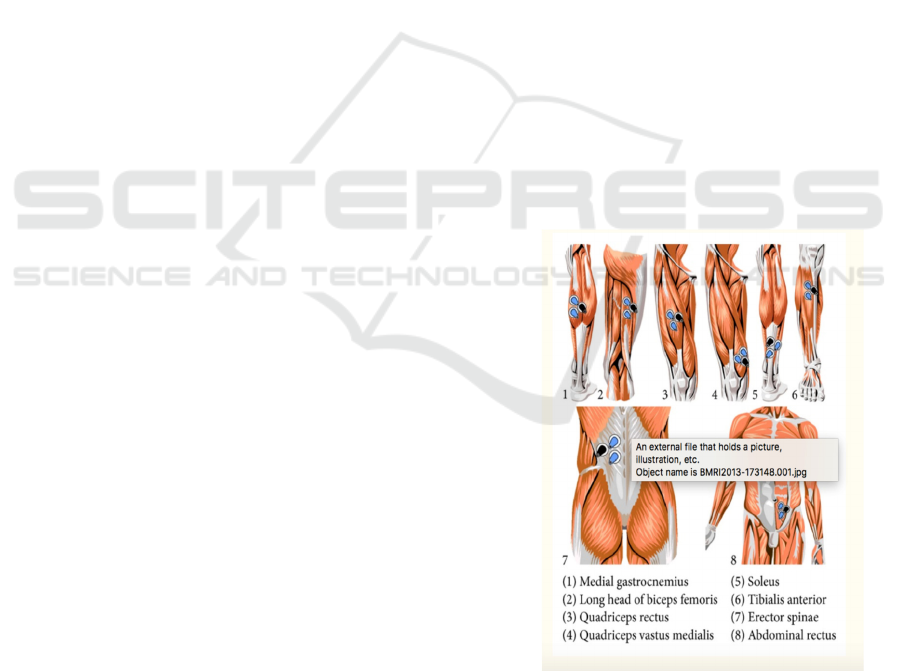
distance of two inches between the electrode (figure
1) (I Antonio et al, 2013)
Figure 1: Schematic placement of surface electrodes on
each muscle. From MegaWin 3.0.
The STS movement for analysis is classified into
6 phases based on Schenkman et al study. The seat-
off, which refers to the moment when only the feet
Pattern of Muscle Activation During Sit to Stand Task in Feet Forward with 80 Knee Flexion using Surface EMG
83
are in contact with the grounds and no force is
applied on the seat, is often used to identify STS
phases. Phase I (flexion-momentum phase) starts
with the initiation of the movement and ends just
before the buttocks/thighs are lifted from the seat of
the chair. Phase II (momentum-transfer phase)
begins as the buttocks are lifted and end when
maximal ankle dorsiflexion is achieved (anterior and
upward CoM displacement). The anterior
displacement of the CoM brings it close to the center
of pressure (CoP) to reach a quasi-static stability
position. Phase III (extension phase) is initiated just
after maximum ankle dorsiflexion and ends when
the hips first cease to extend; including leg and trunk
extension. Phase IV (stabilization phase) begins after
hip extensions are reached and end when all motion
associated with stabilization is completed. Phase V
is reverse-phase II and Phase VI is reverse-phase I.
(Janssen et al, 2002; Boukadida A et al, 2015;
Schenkman M, 1990).
This research is a descriptive, cross-sectional
study with the convenient sampling method. The
data collection was analyzed using IBM SPSS
statistical software version 20. Independent Samples
Test and Mann Whitney test was used to compare
demographic characteristics between different
gender of the subject.
3 RESULTS
Table 1 showed there were differences in the
anthropometry of the sample between women and
men, except the age.
Table 1: General characteristics of participants.
Characteristics
Men Women
p-Value
Mean(SD) Mean(SD)
Age (years) 30,86(4,52) 30,71(2,46) 0,918
Height (cm) 167,57(4,48) 158,43(6,21) <0,001*
Weight (kg) 71,96(7,52) 59,64(11,79) 0,003*
Body Mass Index
(kg/m
2
)
25,67(2,99)
23,66(3,82)
0,133
Body Fat (%) 22.08 (4.41) 32.15 (7.04) <0.001*
Fat-free mass
(kg)
52.90 (3.16) 37.29 (4.23) <0.001*
Note: *p-value<0.05 indicates the significant predictors in the model; SD: Standard Deviation
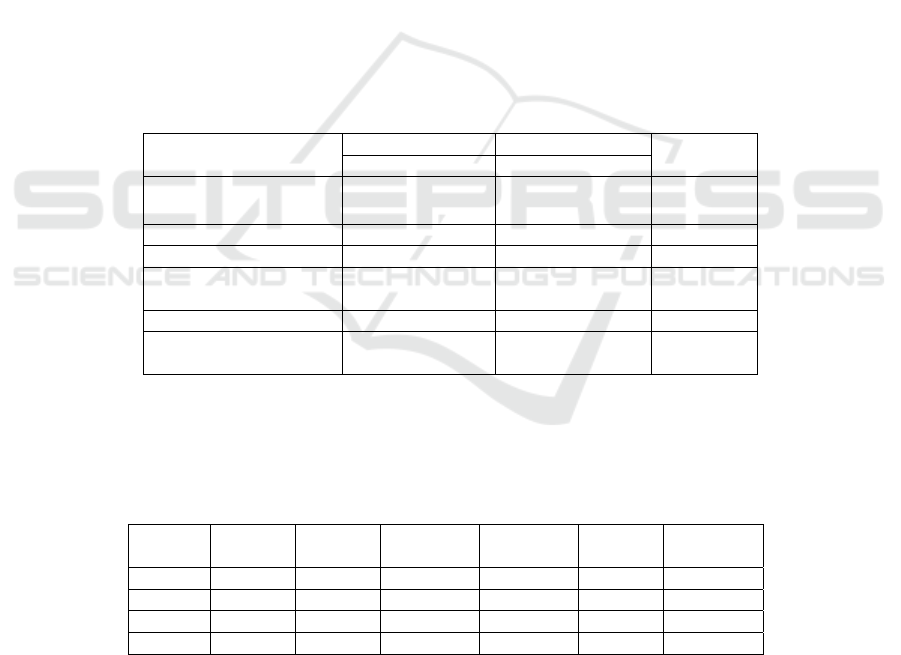
Table 2: The mean maximal force of Rectus Femoris, Biceps Femoris Lateral, Gastrocnemius and Tibialis Anterior muscle
in each phase of Sit-to-Stand.
Note: RF: Rectus Femoris muscle, BFL:Biceps femoris lateral muscle, GM: Gastrocnemius muscle, TA:Tibialis Anterior
muscle
Muscle
Phase I
(µV)
Phase II
(µV)
Phase III
(µV)
Phase IV
(µV)
Phase V
(µV)
Phase VI
(µV)
RF 37,37 73,11 51,60 50,99 61,74 37,28
BFL 19,07 47,97 23,87 27,53 36,90 17,28
GM 11,77 22,77 19,99 20,13 17,95 11,53
TA 17,80 31,05 23,25 23,98 35,87 15,90
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
84

Figure 2: An overview of muscle activation of RF, BFL,
GM AND TA using sEMG evaluation during all STS
Phases.
In phase II, all muscle group have the biggest
muscle activation compare to another phase, and the
muscle group sequence was bigger than muscle
group stabilizer. The rectus femoris has the biggest
muscle activation in all phases. On the other hand,
the mean maximal activation of TA was the highest
in Phase V. The overview of mean maximal force
for RF, BFL, GM and TA in each phase was also
described in Figure 2.
4 DISCUSSIONS
The subjects of the study were mostly men (90,9%).
Although women could have higher CRP levels than
men due to hormonal factors (O’Connor, 2009),
this condition may not significantly influence the
CRP results.
CRP levels did not change significantly due to
several factors, one of them is the high CRP level
since the beginning, although there was no sign of
infection during the study since the leucocyte count
did not increase. The CRP level could be influenced
by BMI, the level and severity of the lesion and
smoking habits. Most of the subjects in this study
were included in the underweight category with an
average BMI was 18.72 ± 2.173 kg/m2. The BMI
values are related to body fat composition. Low BMI
could be caused by decreased fat-free muscle mass
due to reduction in physical activity and atrophy
caused by paralysis. Greater adipose tissue
composition due to impaired fat and carbohydrate
metabolisms can lead to increased CRP levels
(Wang, 2007).
Lesion levels and severity of SCI itself can
influence the CRP levels. The higher lesion levels
and severe SCI indicate higher CRP levels. Those
with tetraplegia have a greater risk of CVD
compared to those with paraplegia in chronic SCI
Gibson, 2008). SCI lesions of the subjects in this
study were as high as the thoracic cord. Since most
of the subjects had complete SCI, high CRP levels
of the subjects were discovered since the beginning.
The smoking habits were not limited during the
study, these may cause a high of CRP level.
Smoking can increase the release of
proinflammatory cytokines in the blood and lung
circulation. It also can cause oxidative stress and
vascular inflammation occurs marked by increased
IL-6 and CRP levels. A previous study presented
that higher CRP levels were mostly found in the
subjects who smoked (O’Connor, 2009).
Unfortunately, this study did not have any data to
analyaze the correlation between the number of
cigarettes (packs per year) and nicotine levels with
distinctive measurements in each subject.
Exercise can decrease inflammatory cytokines in
the blood (Alves, 2013). Muscle contractions can
stimulate the release of IL-6 from muscle cells,
namely muscle derived IL-6.
IL-6 has important
anti-inflammatory effects since it plays a role in the
formation of anti-inflammatory cytokines such as
interleukin-1 receptor antagonist (IL-1ra) and
interleukin-10 (IL-10).
The appearance of IL-10 and
IL-1ra in the circulation contributes to mediating the
anti-inflammatory effects of exercise and induces a
reduction in CRP levels and suggests that physical
activity may suppress systemic low-grade
inflammation.
The increased plasma IL-6 is related to exercise
intensity, duration, the mass of muscle recruited and
one’s endurance capacity (Peterson, 2005). Physical
activities with moderate intensity are recommended
to reduce CRP levels (Zonneveld, 2014). IS exercise
in this study counted as moderate intensity based on
Borg scale 11-13. Most of the subjects had the same
occupation as a craftsman and did their daily
activities independently, but still there were no
complete data and objective assessment of physical
activities collected.
The IS exercise given in this study had not
decreased the inflammation marker of CRP. This
study given different result from the previous studies
that after 4 weeks of physical training was
associated with significantly improved plasma
concentrations of adiponectin and CRP (Oberbach,
2006), IS exercise for 4 weeks (twice daily, 30
breaths a set for 30 days) in COPD patients was
Pattern of Muscle Activation During Sit to Stand Task in Feet Forward with 80 Knee Flexion using Surface EMG
85

already showed a significant result in reducing IL-6
and TNF-α inflammatory cytokines
(Leelarungrayub, 2017), IMT combined with aerobic
training provides additional benefits in functional
and serum biomarkers of inflammation (CRP) in
patients with moderate CHF (Adamapoulos, 2014).
The differences in the type of exercise, the mass of
muscle recruited, the intensity and duration of
exercise compared with the previous study, the
markers of inflammation which had been examined
may make the differences of the result.
The study has shown that IS exercise can
improve lung function in an individual with chronic
SCI. The similar results showed in another previous
study (Kim, 2017). The study has not shown
significant change in the circulating level of CRP
however, a potential local effect of IS on
diaphragmatic myocyte cytokine production cannot
be excluded. Whether there was a reduction in local
diaphragmatic muscle inflammation marker after IS
was not tested in this study.
The IS exercise given in this study had influenced
fat metabolism marked by the significant reduction
of LDL/HDL ratio. IL-6 is the first cytokine
released into the circulation during exercise, derived
from the contracting muscle. This cytokine will
activate lipolysis independently of elevations in
Growth Hormone (GH) and/or cortisol and become a
potent catalyst for fat oxidation in muscle cells
(Peterson, 2005). The present study was given
different result from the previous studies that IMT
with low inspiratory loading fails to demonstrate any
significant improvements in blood glucose levels,
serum lipids, and/or HOMA-IR in female patients
with type 2 diabetes (Ahmad, 2017) and after 7 days
of IMT had not able to change metabolic variables
(blood glucose and lipid profile) in women with
metabolic syndrome (Feriani, 2017).
There are some limitations to this study that can
be improved in future research. Firstly, the present
study did not measure other cytokines, such as IL-10
and IL-1ra may be needed to confirm that the
observed increase in IL-6 is muscle derived and not
due to other factors, such as the existence of a
catabolic/inflammatory state due to exercise training
(Peterson, 2005). Secondly, this study did not have
any data regarding the number of cigarettes (packs
per year) and nicotine levels with distinctive
measurements in each subject which can correlate
with the inflammatory state. Thirdly,
there was no
complete data and objective assessment of physical
activities and nutritional intake collected.
Further study can be conducted by giving longer-
term IS exercise intervention or with other exercise
combinations including aerobics. Assessment of
detail physical activity level, other routine activity
(such as smoking), nutritional status and other anti-
inflammatory cytokine levels should be done in
further study.
5 CONCLUSIONS
A 4 weeks incentive spirometry breathing exercise
resulted in improvement in lung function and lipid
ratio. Improvement in lung function has not
influenced the systemic inflammatory level (CRP),
although a beneficial influence on LDL/HDL ratio
was recorded. Further follow up and studies are
required to establish the role of inspiratory muscles
in improving the systemic inflammatory status of
patients with chronic spinal cord injury.
REFERENCES
Adamopoulos S, Schmid JP, Dendale P, Poerschke D,
Hansen D, Dritsas A et al. 2014. Combined
aerobic/inspiratory muscle training vs. aerobic training
in patients with chronic heart failure. European
journal of heart failure ; 16(5) : 574-82.
Ahmad AM, Abdelsalam HM, Lotfy AO. 2017. Effect of
Inspiratory Muscle Training on Blood Glucose Levels
and Serum lipids in female patients with type 2
diabetes. International Journal of ChemTech Research
; 10(4): 703-709
Alves E, Lemos V, Silva F, Lira FS, Santos RVT, Rosa
JPP et al. 2013. Low-grade inflammation and spinal
cord injury: exercise as therapy? Mediators of
inflammation; 1-8.
Feriani DJ, Coelho-Júnior HJ, Scapini KB, de Moraes OA,
Mostarda C, Ruberti OM. 2017. Effects of inspiratory
muscle exercise in the lung function, autonomic
modulation, and hemodynamic variables in older
women with metabolic syndrome. Journal of Exercise
Rehabilitation ;13(2):218-226
Gibson A, Buchholz A, Ginis KM. 2008. C-Reactive
protein in adults with chronic spinal cord injury:
increased chronic inflammation in tetraplegia vs
paraplegia. Spinal Cord.;46(9):616-21.
Groah SL, Weitzenkamp D, Sett P, Soni B, Savic G. 2001.
The relationship between neurological level of injury
and symptomatic cardiovascular disease risk in the
aging spinal injured. Spinal Cord ; 39: 310–317.
Hart JE, Goldstein R, Walia P, Teylan M, Lazzari A, Tun
CG, et al. 2017. FEV1 and FVC and systemic
inflammation in a spinal cord injury cohort. BMC
Lung Medicine ; 17: 1-9.
Kamath DY, Xavier D, Sigamani A, Pais P. 2015. High
sensitivity C-reactive protein (hsCRP) &
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
86

cardiovascular disease: An Indian perspective. Indian
J Med Res ; 142: 261-268.
Kunutsor SK, Zaccardi F, Karppi J, Kurl S, Laukkanen
JA. 2017. Is High Serum LDL/HDL Cholesterol Ratio
an Emerging Risk Factor for Sudden Cardiac Death?
Findings from the KIHD Study. J Atheroscler
Thromb; 24: 600-608.
Koyuncu E, Yüzer GFN, Yenigün D, Özgirgin N. 2017.
The analysis of serum lipid levels in patients with
spinal cord injury. The Journal of Spinal Cord
Medicine; 40 (5) : 567-572.
Kim CY, Lee JS, Kim HD, Lee DJ. 2016. Short-term
effects of respiratory muscle training combined with
the abdominal drawing-in maneuver on the decreased
lung function of individuals with chronic spinal cord
injury: A pilot randomized controlled trial. The
Journal of Spinal Cord Medicine; 1-9.
Leelarungrayub J, Puntumetakul R, Sriboonreung
T,Pothasak Y,Klaphajone J. 2018. Preliminary study:
comparative effects of lung volume therapy between
slow and fast deep breathing techniques on lung
function, respiratory muscle strength, oxidative stress,
cytokines, 6-minute walking distance, and quality of
life in persons with COPD. International Journal of
COPD ; 13: 3909–3921.
Manns PJ, McCubbin JA,Williams DP. 2005. Fitness,
inflammation, and the metabolic syndrome in men
with paraplegia. Arch Phys Med Rehabil ;86: 1176–
1181.
Ma JK, McCracken LA, Voss C, Chan FH, West CR,
Ginis KM. 2018. Physical activity measurement in
people with spinal cord injury: comparison of
accelerometry and self-report (the Physical Activity
Recall Assessment for People with Spinal Cord
Injury). Disability and Rehabilitation ; 1-7.
O’connor MF, Bower JE, Cho HJ, Creswell JD, Dimitrov
S, Hamby ME, et al. 2009. To assess, to control, to
exclude : Effects of biohavioral factors on circulating
inflammatory markers. Brain, Behavior, and
Immunity; 23 : 887-897.
Oberbach A, Anjes A, Kloting N, Fasshauer M, Kratzsch
J, Busse MW, et al. 2006. Effect of a 4 week physical
training program on plasma concentrations of
inflammatory markers in patients with abnormal
glucose tolerance. European Journal of
Endocrinology; 154 : 577–585.
Petersen AM, Pedersen BK. 2005. The anti-inflammatory
effect of exercise. J Appl Physiol ; 98: 1154–1162.
Petersen EW, Carey AL, Sacchetti M, Steinberg GR,
Macaulay SL, Febbraio MA, et al. 2005. Acute IL-6
treatment increases fatty acid turnover in elderly
humans in vivo and in tissue culture in vitro. Am J
Physiol Endocrinol Metab; 288(1):E155-62.
Pedersen BK. 2006. The anti-inflammatory effect of
exercise : its role in diabetes and cardiovascular
disease control. The Biochemical Society; 42 : 105-
115.
Plaisance EP and Grandjean PW. 2006. Physical Activity
and High-Sensitivity C-Reactive Protein. Sports Med;
36 (5): 443-458.
Paiva DN, Assmann LB, Bordin DF, Gass R, Jost RT,
Filhod MB, et al. 2015. Inspiratory muscle training
with threshold or incentive spirometry: Which is the
most effective?Rev Port Pneumol; 21(2):76-81.
Restrepo RD, Wettstein R, Wittnebel L, Tracy M.
Incentive spirometry: 2011. 2011. Respiratory care ;
56(10) : 1600-4.
Tulaar ABM, Karyana M, Wahyuni LK, Paulus AFS,
Tinduh D, Anestherita F et al. 2017. People with
spinal cord injury in Indonesia. Am J Phys Med
Rehabil ; 96(2) : S74-S77.
Vichiansiri R, Saengsuwan J, Manimmanakorn N, Patpiya
S, Preeda A, Samerduen K, et al. 2012. The
Prevalence of Dyslipidemia in Patients with Spinal
Cord Lesion in Thailand. Cholesterol; 2012: 1-6.
World Health Organization. 2013. International
perspective on spinal cord injury. Malta: WHO
Library Cataloguing-in-Publication Data.
Wang T. D., Wang Y. H., Huang T. S., Su T. C., Pan S.
L., and Chen S. Y. 2007. Circulating levels of markers
of inflammation and endothelial activation are
increased in men with chronic spinal cord injury.
Journal of the Formosan Medical Association ; 106
(11) : 919–928.
Zonneveld CN, Bakkum AJ, Bishop NC, Van Tulder MW,
Janssen TW. 2014. Effect of Long-Term Physical
Activity and Acute Exercise on Markers of Systemic
Inflammation in Persons With Chronic Spinal Cord
Injury: A Systematic Review. Archives of Physical
Medicine and Rehabilitation; 1-13.
Pattern of Muscle Activation During Sit to Stand Task in Feet Forward with 80 Knee Flexion using Surface EMG
87
