
Sturge Weber Syndrome: Abnormalities in the Brain, Skin and Eyes
from Birth - A Case Report
Vina Amalia
1
, Patricia Maria
1
1
Department of Physical Medicine and Rehabilitation, Dr Soetomo Hospital ,
Airlangga University, Surabaya, Indonesia
Keywords: SWS, Sturge Weber Syndrome, Port-wine Stain, Glaucoma, Dermal Angioma
Abstract: A 23-year-old woman was referred from neurologic outpatient clinic with Hemiparesis Dextra (atrophy) e.c
Sturge Weber Syndrome. She complained weakness of right extremities since she was a child (4 month-old)
after she experienced a seizure. She felt easily tired after walking 100 meter, especially on the right leg.
There was numbness on right face and extremity. She felt pain on right eye, and routinely controlled to
Ophthalmology department. There was red skin on the left face. Physical examination revealed numbness,
weakness, atrophy, increased physiological reflex and spasticity on right extremities. There was also
numbness on her right face. Redness on the left face (port wine stain) and eye (glaucoma and buftalmos),
pain on left eye and blurred vision. There was parese on left facial, vestibulocochlear, glossopharynx and
hipoglossus nerve. MRI Brain discovers Sturge Weber Syndrome. The rehabilitation program consists of
ROM exercise, strengthening exercise, sensory resensitisation, hand function exercise, breathing exercise,
balance exercise and gait training.
1 INTRODUCTION
Sturge-Weber Syndrome is a sporadic, congenital
neurocutaneous disorder, characterized by
intracranial leptomeningeal vascular malformations
associated with a facial port wine stain (nevus
flaemmus) (Chhabria et al, 2017). Sturge–Weber
syndrome (SWS) or encephalotrigeminal
angiomatosis is a congenital, non-hereditary,
condition of unknown etiology. The disease shows
facial port-wine stain, ocular abnormalities
(glaucoma and choroidal hemangioma), and
leptomeningeal angioma. It belongs to a group of the
disorder known as the phacomatoses (“mother-spot”
diseases). SWS was first described by Schirmer in
1860 and later more specifically by Sturge in 1879.
He associated dermatological and ophthalmic
changes of the disease to neurologic symptoms.
Weber, in 1929, stated the radiologic alterations seen
in patients of SWS. (Kulkarni, 2015).
It is rare disorder occurring with no racial
predilection equally affecting males and females the
leptomeninges epilepsy, Port-wine stain, ocular
involvement, dermal angiomas, mental retardation,
hemiplegia, and abnormalities in skull radiographs
(Kulkarni, 2015).
The syndrome occurs almost always sporadically
and have no definite hereditary influence. Patient
with unilateral facial port wine stains of upper eye
lid increases the risk of glaucoma and regularly had
seizures and hemiparesis of the contralateral side
and that is the result of an intracranial hemangioma.
Sturge weber syndrome appear as a congenital lesion
usually benign tumors of blood vessels and have no
chance of malignant transformation (Moly et al,
2016).
2 CASE PRESENTATION
A 24 years old woman, Javanese from Lamongan
city, East Java. She hasn’t married yet with low
economic stage and doesn’t work. She was referred
from neurologic outpatient clinic with weakness of
right extremities (atrophy) because of Sturge Weber
Syndrome. She complained weakness of right
extremities since she was a child (4 month-old) after
she experienced a seizure (figure 1C). She felt easily
tired after walking 100 meter, especially on the right
leg. There was numbness on right face and
extremity. She felt pain on right eye, and routinely
controlled to Ophthalmology department. There was
Amalia, V. and Maria, P.
Sturge Weber Syndrome: Abnormalities in the Brain, Skin and Eyes from Birth - A Case Report.
DOI: 10.5220/0009087701810185
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 181-185
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
181
red skin on the left face. There was no abnormality
of prenatal and natal history. Post natal history, there
was red skin on left face, asymmetric face and left
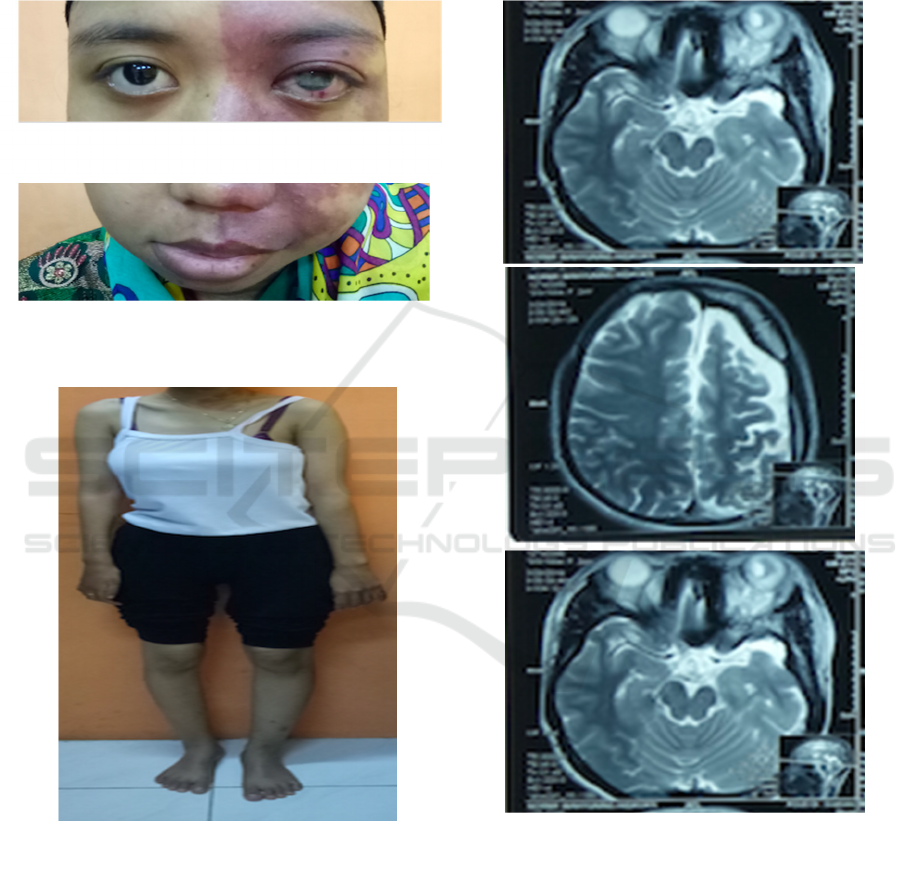
eye is more prominent (figure 1A&B). Her
development was similar to another child. She
experienced seizure routinely since 1 month ago,
twice a day. She often felt pain on her left head in
the last 3 years ago. In 2002, she underwent
glaucoma surgery.
On examination, we found numbness, weakness,
and atrophy of right extremities with Full range of
movement (ROM) and the manual muscle test
(MMT) of right wrist flexor was 1, fingers extensor
was 2, thumb flexor and extensor were 1. The other
still functional. There was increased physiological
reflex and spasticity on right extremities with
Modified Ashworth Scale (MAS) were 1+ on elbow
flexor and extensor, MAS 1 on wrist flexor and
extensor, MAS 2 on knee extensor. There was also
numbness on her right face. Redness on the left face
(port wine stain) and eye (glaucoma and bultalmos),
pain on right eye and blurred vision. There was
parese of left facial, vestibulocochlear,
glossopharynx and hipoglossus nerve. She can’t do
tandem walking. Her dynamic standing balance also
Figure (1A): Port-wine stain, glaucoma and buftalmos.
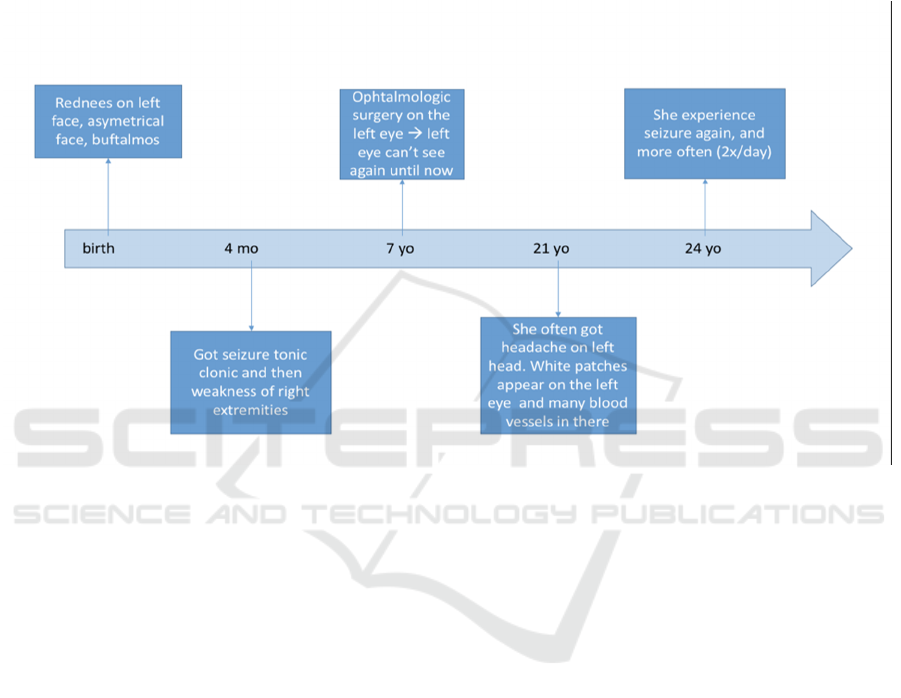
Figure (2A, B, C) : MRI brain : Sturge Weber
Syndrome
Figure (1C) : Atrophy right arm and leg
1A
1B
1C
2A
2B
2C
Figure (1B): Port-wine stain, orbicularis oris weakness
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
182
was poor. Hand function like spherical, cylindrical,
lateral tip and pinch were non functional. Count test
was 23 and chest expansion was still good. MRI
brain with Sturge Weber Syndrome (figure 2A, B,
C).
We give rehabilitation program that consist of
ROM exercise, strengthening exercise, sensory
resensitisation, hand function exercise (especially
for activity daily living), breathing exercise, balance
exercise and gait training and posture correction.
We suggest this intervention two times per week
(in Lamongan hospital) and evaluated in Soetomo
Hospital every month. We educated the patient to do
exercise at home every day.
In the first month of rehabilitation program, our
main goal was to improve the posture, maintenance
the ROM, improve the gait dan hand function. Due
to the socioeconomic condition and her house far
from hospital, she was given a home-based exercise
program and therapy to the hospital in every week.
The program would be evaluated every 1 month.
Two months later, the patient was evaluated in
Hospital, there was no significant increasing the
MMT, but the patient felt more comfort in walking.
For balance test, we tried to give one leg stand, and
she can do this just on the left leg. The right leg still
weak to support whole her body. We also evaluated
hand function, but there was no significant increase.
She said that she did the exercise program was not
optimal because she still focused on eye treatment.
The right eye very painful and she routinely
control to ophthalmology department.
3 DISCUSSION
Sturge-Weber syndrome (SWS) is a congenital,
sporadically occurring, neurocutaneous syndrome
that presents classically with port-wine stain,
leptomeningeal angiomas, and glaucoma. The
systemic implications of SWS are vast and involve
not only ophthalmic manifestations but also
dermatologic, neurologic, and oral manifestations.
Neuroimaging, in particular, plays an important role
in the diagnosis and management of this disease
(Maslin, 2014). An estimated frequency of 1 per
50,000 live births have SWS, although experts
believe many more people have the disorder but
have not yet been identified. The hallmark
intracranial vascular anomaly is leptomeningeal
angiomatosis, most often involving the occipital and
posterior parietal lobes, but it can affect other
cortical regions and both cerebral hemispheres. An
ipsilateral facial cutaneous vascular malformation
usually affects the upper face in a distribution
consistent with the ophthalmic division
of the
trigeminal nerve. Other clinical findings associated
with SWS are seizures, glaucoma, headache,
Figure 3: Course of the disease.
Sturge Weber Syndrome: Abnormalities in the Brain, Skin and Eyes from Birth - A Case Report
183

transient stroke like neurological deficits, and
behavioral problems. Hemiparesis, hemiatrophy, and
hemianopia may occur contralateral to the cortical
abnormality.
Children with SWS suffer from a variety of
neurologic abnormalities, including epilepsy, mental
retardation, and attention-deficit hyperactivity
disorder, migraine, and stroke like episodes. Seventy
five to 90% of children with SWS have epilepsy.
Focal seizures are initially observed in most children
who have SWS. Fever and infection often precipitate
seizure onset. If noncontrasted computed
tomography obtained in the emergency room setting
after seizure activity is reported as normal or reveals
focal calcification ipsilateral to a cutaneous
angioma, more complete cerebral imaging is
warranted. Most seizures are focal, because the
lesion responsible for the epilepsy in SWS is focal.
Seizures are likely caused by hypoxia and
microcirculatory stasis. Children with radiographic
findings of intracranial angiomatosis usually develop
seizures by the age of 3 years. Approximately half
these children have frank mental retardation,
whereas others display learning disabilities, attention
disorders, or behavioral disturbances.
SWS classically presents with a unilateral
cutaneous nevus PWS or red wine stains on the face.
The cutaneous presentation occurs due to early
embryonic vascular malformation. SWS may also
present with angiomas in the leptomeninges
resulting in epilepsy and hemiparesis and/or
angiomas in the eye causing glaucoma. The most
frequent oral presentation of SWS is hyperplasia of
the gingiva, affecting the maxilla, floor of the
mouth, lips, cheeks, palate and tongue of the same
side. SWS may also present with changes in the
histology and morphology of gingiva, periodontium,
and pulp. (Neerupakam, 2017)
It’s typical manifestations include, cutaneous-
port wine stain on the face, ocular-glaucoma,
choroidal hemangioma and neural features-
leptomeningeal haemangioma, seizures. Oral
involvement in SWS presents as a gingival
haemangiomatous lesion limited to the maxilla and
mandible of the same side. (Neerupakam, 2017)
SWS can be classified into three different types:
Type 1 (most common type) is characterized
by port-wine stain, cerebral malformation
(leptomeningeal angiomas), and the possibility
of glaucoma or choroidal lesions. Seizures may
occur during the first year of life.
Developmental disabilities may be seen during
the first year.
Type 2 is characterized by port-wine stain and
possibly glaucoma without cerebral
malformation (leptomeningeal angiomas).
Headaches or migraines may also occur.
Type 3 is characterized by cerebral
malformation (leptomeningeal angiomas)
exclusively. Port-wine stain is not present and
glaucoma is rare. (Hernandez, 2019)
In this case we got the patient has weakness of
right extremities, unable to use right hand for normal
activity, pain on right eye, redness on left eye
(glaucoma and buftalmos), red skin on left face
(port-wine stain), blurred vision on left eye.
Weakness on left facial nerve, vestibulocochlear
nerve, glossopharynx nerve and hipoglossus nerve.
MRI brain support to Sturge Weber Syndrome. We
give rehabilitation program to improve her quality of
life. The patient felt more comfort to walking after 2
months, and hand function is still not improving.
There was no adverse events or harm while running
this rehabilitation program.
She runs her rehabilitation program at a hospital
near her home, and every months control to Soetomo
Hospital. She didn’t do this rehabilitation program
maximally because she focused on her eye treatment
first that painful and very disturb her. Although there
was no significant increase in MMT, but she felt
more comfort in walking and not easily tired as
before.
The prognosis in SWS varies widely. Although
patients with widespread hemispheral disease or
bihemispheric disease are at greatest risk for
neurologic complications, many function virtually
normally. Clearly, a subgroup of patients with
limited central nervous system involvement as
defined by neuroimaging studies has a particularly
malignant clinical course, with intractable epilepsy,
headache, stroke like episodes, and cognitive
deterioration. There is a greater likelihood of
intellectual impairment when seizure start before the
age of 2 and are resistant to treatment. Prognosis is
worse in the minority of children who have both side
of the brain affected by the blood vessel abnormality
(NINDS, 2019).
4 CONCLUSIONS
It is important to know about the disease to know the
treatment and the obstacle for our rehabilitation
program. We give this program to the patient to help
her improve the quality of life. Although the course
of the disease will go on and cannot be cured. We
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
184

just help patient to get comfort in her daily activity
and adaptation for her condition.
REFERENCES
Chhabria B, et al, 2017. Sturge-Weber Syndrome. Journal
of Clinical and Diagnostic Research, 2017 Feb, Vol
11(2): OJ05-OJ06.
Hernandez A., 2019. Sturge Weber Syndrome
(Encephalotrigeminal Angiomatosis). Epilepsy
Foundation of America, 2019. Website:
https://www.epilepsy.com/learn/epilepsy-due-specific-
causes/neurocutaneous-syndromes/sturge-weber-
syndrome. Access on October 5th,2019.
Korf B, Bebin M., 2017. Neurocutaneous Disorder in
Children. Pediatrics in review Vol 38 No.3
Kulkarni S, et al, 2016. Sturge-Weber Syndrome: A Case
Report and Review of Literature. International Journal
of Scientific Study, Vol 3 Issue 8.
Maslin J, Dorairaj S, Ritch R., 2014. Sturge-Weber
Syndrome (Encephalotrigeminal Angiomatosis):
Recent Advances and Future Challenges. Asia Pacific
Journal of Ophtalmology Vol 3 No.6.
Moly K, Ahsan A, Islam S., 2015 Sturge Weber
Syndrome-Case Report. BSMMU Vol.8 Issue 1
Neerupakam M, et al, 2017. Sturge Weber Syndrome: A
Case Study. Journal of Clinical and Diagnostic
Research Vol.11(5): ZD12-ZD14.
NINDS, 2019. Sturge Weber Syndrome Information Page.
National Institute of Neurological Disorders and
Stroke.
Sturge Weber Syndrome: Abnormalities in the Brain, Skin and Eyes from Birth - A Case Report
185
