
The Effectiveness of Original Honey Treatment toward Diabetic
Foot Infection Wounds Healing
Rentawati Purba, Rostiodertina Girsang,Dewi Tiansa Barus, Nur Mala Sari
Health Institute of DELI HUSADA, Jl.Besar Delitua No 77, Medan
Keywords: Diabetic Foot Infection and Original Honey
Abstract: Diabetes Mellitus (DM) is a group of heterogeneous abnormalities characterized by an increase in blood
glucose levels or hyperglycemia. The impact is very broad which will affect the quality of patient’s life.
One of the most common complications is diabetic foot infection wounds; it is predicted surge up to 14.1
million people with prevalence rate of 6.67% in the adult population. Dysabetic wounds are very easy to
cause complications in the form of infections due to bacterial invasion and the presence of hyperglycemia
being the optimal place for bacterial growth. Honey is believed since the time of ancestors in curing various
diseases, including wound infections. This study aimed to determine the effectiveness of honey treatment
for diabetic foot infection wounds healing. The study design was one group pre-post test with comparison
group. The samples number were 20 respondents with wound care for 50 days, the study results were good
indicators seen from changes in wound diameter from day to day. In this study, the data were analyzed with
Wilcoxon test and the results were 0.001 (p <0.05). Then it showed that original honey usage was more
effective in diabetic foot infection wounds healing. Recommendations from the study results that honey
therapy can be done as one of the replacement therapies to treat wounds caused by diabetic foot infections.
1 INTRODUCTION
Word Health Organization (WHO) 2012 estimates
that the number of people with diabetes mellitus in
Indonesia will increase by two to three times in
2030, coming from 8.4 million to even 21.3 million
people. While Indonesia ranks fourth most DM
sufferers in the world as many as 8.4 million, after
that India reached 31.7 million, China 20.8 million,
and US reached 17.7 million people with diabetic
patients. Diabetic foot due to its complications is the
most common non-traumatic cause. Extremities
under the risk of amputation are more than 15-46
times higher in diabetics than non diabetics.
Complications of foot injuries in diabetic patients
are very difficult to treat and more routine in treating
diabetic foot injuries so as not to expand the diabetic
patient's foot injuries. In the treatment of these
wounds it is better to use Honey because it has been
widely used for the treatment of various types of
infections with many types of wounds such as burns,
venous legs of mixed etiology, diabetic foot ulcers).
While according to RISKESDA report
(2016), the prevalence of diabetes diagnosed by
doctors is 2.1%. The prevalence is higher than
RISKESDA (2007), which is around 1.1%. There
are some provinces that have a higher prevalence
than the national average, namely Central Sulawesi
(3.7%), North Sulawesi (3.6%), South Sulawesi
(3.4%) and East Nusa Tenggara 3.3%. The
prevalence of diabetes tends to be higher in women
than in men and is more common in urban
communities (RI Health Ministry, 2016). Unlike in
Western countries, in Indonesia there are several
studies on the prevalence and factors related to DFU.
The main complications of DM in Indonesia are
neuropathy (13% - 78%), vascular
microcomplications (16% - 53%) and DFU (7.3% -
24%) (Nuwa, 2018).
Diabetes Mellitus (DM) is a group of
heterogeneous abnormalities characterized by an
increase in blood glucose levels or hyperglycemia.
The impact is very broad which will affect the
quality of patients life, especially in patients with
diabetic foot ulcer complications, one of the causes
of this complication occurs due to nerve damage
(neuropathy), in this condition patients can no longer
distinguish between hot temperatures and cold, less
pain. The patient leg who has neuropathy is twice as
likely to develop a diabetic wound. Diabetic foot
36
Purba, R., Girsang, R., Barus, D. and Sari, N.
The Effectiveness of Original Honey Treatment toward Diabetic Foot Infection Wounds Healing.
DOI: 10.5220/0009462200360042
In Proceedings of the International Conference on Health Informatics and Medical Application Technology (ICHIMAT 2019), pages 36-42
ISBN: 978-989-758-460-2
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

ulcers are a major cause of morbidity and disability
in diabetic patients. They often lead to lower limb
amputations especially when associated with
neuropathy and / or ischemia. At the national level,
foot ulceration often occurs, it affects 6.9% of
diabetics throughout their lives, moreover ulceration
is the most common cause of hospitalization and
precedes 80% of amputations of the lower
extremities ( Jeffcoate W, 2017).
Some researchers conducted research by
using diabetic-foot herbs treatment namely original
honey. Wound care used honey because it contains
fructose and glucose which is a type of
monosaccharide sugar that is easily absorbed by the
intestine. Then the way to treat diabetic foot wounds
regularly with honey would be better, from the era
when it was very trusted by the public for various
types of treatment including honey wounds, it was
also easy to obtain besides it was effective in the
wound healing process because of its low water
content, also the PH of the acidic honey and its
content of hydrogen peroxida could kill bacteria and
microorganisms that enter our body. In addition,
honey also contains antibiotics as an antibacterial
and antiseptic to protect the wound from worsening
(Nabhani and Widiyastuti, 2017).
Diabetic foot injury is a serious complication
of diabetes, which can result prolonged
hospitalization and can lead amputation of the lower
limbs in. Research has shown more than 15% of
diabetics suffer from diabetic foot. The annual
incidence of diabetic foot injury is estimated at 25–
80%. The prevalence of diabetic foot injuries
worldwide has been reported to be 4–27%. In
developed countries, more than 5% people with
diabetes suffer from diabetic feet, and 20% health
care resources spent on treating diabetic foot
injuries. In US, the cost of diabetic foot is 7,000-
10,000 USD, and this figure increases by 65,000
USD in complicated cases which require amputation
of what diabetic foot injury, which indicates the high
cost of health care (Karimi, 2019).
Diabetic foot injury is an important factor in
the mortality and disability of diabetics. Despite,
there is much progress in the diagnosis and
treatment of diabetes; diabetic foot problems have
not been resolved. Many patients suffer some degree
of diabetic foot; as result, they are treated with
drugs. After ineffective medical treatment, surgery is
considered for the patient. One of the most
challenging tasks in diabetes foot health care is the
treatment of diabetic foot injuries. One of them is
honey. Honey is used to cure diabetic feet, and its
efficiency and effectiveness have been investigated
by many studies (Karimi, 2019). Honey has been
known for thousands of years which can be used in
the process of wound healing. Honey has
antibacterial characteristics, stimulates the release of
cytokines, and stimulates cell growth, so that the
wound can undergo a healing process (Nuwa, 2018).
Diabetic wounds easily develop into
infections due to the entry of germs or bacteria and
the presence of high blood sugar becomes a strategic
place for germ growth. If the diabetic wound is not
handled properly it will cause disability and even
lead to amputation. Honey has been used as a natural
medicine for healing various diseases since
thousands of years ago. Previous people have been
using honey as a therapeutic treatment for several
millennia and lately it has been rediscovered as a
potential treatment in wound care mentioning that
honey can accelerate the wound healing process.
The study results conducted by Subrahmanyam et al
(2015) about the effectiveness difference of wound
care by using honey and sulphadiazin silver on 21
st
day, all wounds treated with honey underwent
epithelialization, whereas wounds treated with silver
sulphadiazine only 20% undergo epithelialization
(Nuwa, 2018).
The benefits of honey are curing heartburn,
enhance immunity, for beauty and moisturize the
skin, cure asthma, increase intelligence and memory,
and can also heal wounds quickly and can cure
various other diseases. The research problem is to
find out the effectiveness of original honey treatment
is diabetic foot infection wounds healing. Several
studies have shown that honey has the ability to
repair, protect and prevent infection and make
antibacterial moist healing. In addition honey has a
debriding effect by osmotic action that causes lymph
flow out, remove dead skin tissue from the bottom
of the wound quickly, tissue regeneration, reduce
pain during wound care and reduce edema by anti-
inflammatory action. The same results seen in the
Farouk A et al research mentioned in their study that
many patients had ulcers that did not heal due to
different causes and did not improve with
conventional treatment; the results were good by
giving honey to repair tissue in the wound (El-Nahas
M, 2018).
By using native honey the wound healing
process occurs faster, as evidenced within 2 weeks
of tissue gradation in growing diabetic wounds. in
honey contains a lot of vitamins, acids, minerals, and
enzymes, which are very useful for the body as
traditional treatment, antibodies, and inhibit the
growth of cancer cells or tumors. In addition to
organic acids, honey also contains amino acids that
The Effectiveness of Original Honey Treatment toward Diabetic Foot Infection Wounds Healing
37
are related in making body proteins (non-essential
amino acids). In addition to non-essential amino
acids there are also essential amino acids including
lysine, histadine, tryptophan, etc. (Fain, A. 2017).
According Saldi's study (2012), the wound
treatment by using 0.9% NaCl liquid to wash the
wound and provide honey dressing to the wound.
The observation results obtained wound healing
process treated with 0.9% NaCl liquid and honey
showed the results of the granulation process is quite
fast, the tissue looks moist, and the pus contained in
the wound dries quickly. Under these conditions, the
researchers are interested in further researching
about the effectiveness of wound cleansing by using
0.9% NaCl liquid and honey is given for the healing
of diabetic wounds. Diabetic patients have poor
blood circulation and lack the ability to fight
infections. Diabetic foot infections can be treated by
systemic antibiotics with long time usage that can
develop drug-resistant organisms toward medicine
and honey in wound treatment that have antibiotic-
resistant bacteria.
Dunford C, et al, (2016), examined the
effectiveness of honey in diabetic foot injuries and
found that on the seventh day of observation, 87% of
patients treated with foot injuries by using honey
showed satisfactory epithelialisation and on the 21
st
day 92% epithelalization was achieved by wounds
treated using honey. He identifies that time of
diabetic foot wound healing by using honey is more
effective.
To prevent diabetic wounds complications
that last long time and prevent worse, it should be
noted how to treat wounds in diabetics where there
are four principles of diabetic wound management to
optimize the process of healing diabetic foot
wounds, namely: basic preparation of wounds,
wound protection, wound dressing, and wound
oxygenation. The usage of this principle is expected
to be 80%, the problem of diabetic wounds will be
cured, so as to avoid the amputation occurrence (El-
Nahas M, 2018).
2 METHODOLOGY
The population in this study were all patients who
suffered diabetic foot infection wounds of 20
respondents. This study used sampling technique
with total sampling by using quasi-experimental
method with one-group pre-post test approach.
This research used original honey which has
water content less than 18%, gauze, anatomical
tweezers, cirugis tweezers, plaster, nierbeken, NaCl
liquid, and observation sheets. Based on research
conducted on 20 respondents with the provision of
original honey for respondents as much as 3-5 cc,
coupled with wound cleansing by using 0.9% NaCl
liquid, then it is done dressing bandage on the
wound which is applied original honey within period
of 50 days conducted in 1 day treatment for diabetic
foot injury. By inclusion criteria is willing to be
respondents in writing, the foot injuries degree in
grades 1 to 3. The exclusion criteria are not willing
to be respondents, the degree of diabetes foot
injuries in grades 4 and 5.
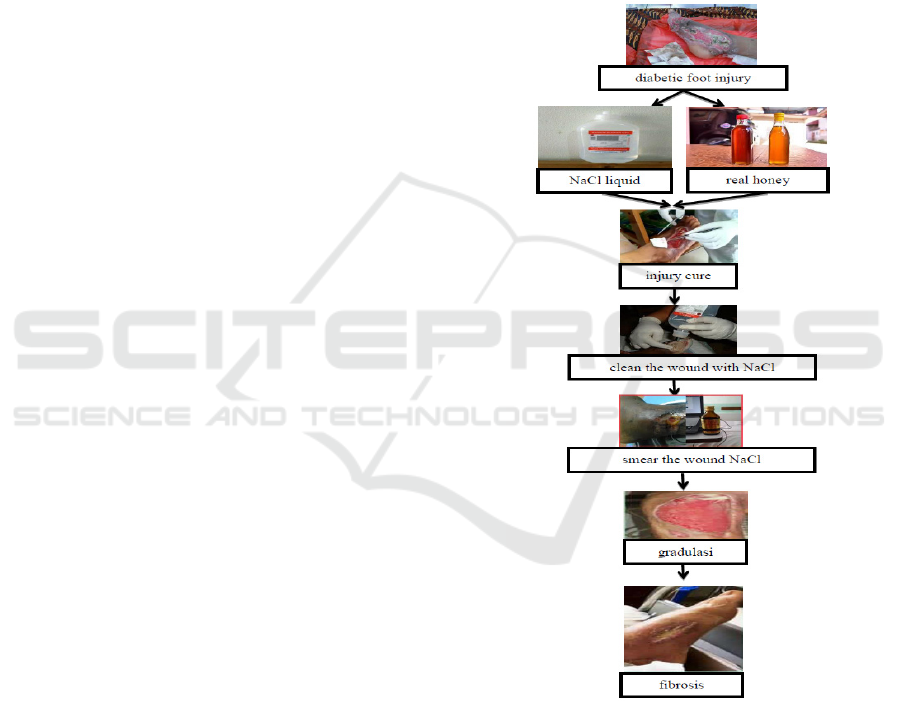
Figure 1: Research Conceptual Framework.
3 RESEARCH RESULT AND
DISCUSSION
Based on the study results, it is known that the
sample were all DM patients who have diabetic
wounds. For the respondents of characteristics,
based on the age of 40-49 years old and ≥ 60 years
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
38

old as many as 4 people or about 20%. And the age
of the majority aged 50-59 years old as many as 9
people or about 45% and for minority ages aged 35-
39 years old as many as 3 people or about 15%.
Based on gender characteristics, the majority
were male as many as 16 people or about 80% and
the minority were women as many as 4 people or
about 20%.
Based on Occupation characteristics, the
majority work were farmers as many as 9 people or
around 45% and the minority work were civil
servants as many as 3 people or around 15%. It can
be seen in Table 1 below.
Table 1: Respondent’s characteristics distributon of giving
original honey for diabetic foot injuries based on age, sex,
and occupation
.
Characteristic N %
Age
35-39 thn 3 15
40-49 thn 4 20
50-59 thn 9 45
>60 thn 4 20
Total 20 100
Gender
Male 16 80
Female 8 40
Total 20 100
Occupation
Entrepreneurship 4 20
Farmer 9 45
Housewife 4 20
Civil Servant 3 15
Total 20 100
Based on univariate analysis on the diabetic
foot injury degree before being given honey to
diabetic foot injuries, the results showed that the
majority of grade 3 injuries were 9 respondents or
around 45.0% and the minority of grade 1 injuries
were 4 respondents or around 20.0%. Based on
univariate analysis on the diabetic foot injury degree
after being given original honey to diabetic foot
injuries, it was found that the majority of grade 2
injuries were 7 respondents or about 35.0%, and the
minority of wound degrees in grades 0 and 3 were 4
people or around 20, 0%. It can be seen in Table 2
below.
Table 2: Respondent’s distribution before and after
original honey administration toward diabetic foot
injuries.
Injuries
Degree
Before After
Subject % Subject %
Grade 0
4 20
Grade 1 4 20
5 25
Grade 2 7 35
7 35
Grade 3 9 45
4 20
Total
20 100
20 100
The research results with wound care by using
0.9% NaCl liquid to wash the wound and provide
honey dressing for the wound. The observation
results obtained wound healing process treated with
0.9% NaCl and honey showed the results of the
granulation process is quite fast, the tissue looks
moist, and the pus contained in the wound dries
quickly. Under these conditions, the researchers are
interested in further researching about the
effectiveness of wound cleansing by using 0.9%
NaCl with Honey for Diabetic Wound Healing
(Andriana, 2016).
It is proven by other studies, according to
Faisol's research (2015), the Effectiveness of Giving
Honey on Diabetic Wounds shows that after
treatment, new granulation tissue growth, absence of
inflammatory reactions, and reduced wound depth,
reddish tissue color, and reduced amount of
exudates.
Based on bivariate data, the results of willcoxon
statistics on pre-test were conducted for 20
respondents and obtained a mean of 2.25 and std,
deviation of 0.786, then the post carried out to 20
respondents and obtained a mean of 1.55 and std
deviation of 1.050 then it was obtained p-value of
0.001<α 0.05 then Ho is rejected and Ha is accepted,
which means there is significant influence between
the administration of original honey toward diabetic
foot injuries.
It is also in accordance with Andriana opinion
(2016), which states that honey helps the process of
wound debridement and prevents the scar formation.
Honey also increases the contraction time. If
necrotic tissue around the wound is reduced, the
wound base becomes more aligned indirectly with
the skin around the wound. In addition, tissue
growth gradation and epithelialization cause the
wound base to be lifted so that the wound depth is
reduced.
It is also in accordance with Professor Jennifer
Eddy's theory from the University School of
Medicine and Public Health; honey can kill bacteria
because it is acidic, besides that honey is also
The Effectiveness of Original Honey Treatment toward Diabetic Foot Infection Wounds Healing
39

effective in avoiding the resistant nature of bacteria
because it has antibiotic content. This chemical fact
has been confirmed by scientists who met at the
World Apculture Conference which was held on
September 20-26, 2015 in China. The conference
discussed treatment using herbs derived from honey.
American scientists say that honey, royal jelly,
pollen, and propolis can be used as traditional
medicine. Poland doctors also stated at the
conference that honey can help heal diabetic foot
injuries (Al-Maskari, 2015).
Wound care using 0.9% NaCl + Original Honey
has many benefits such as being cheaper, easier to
use and can be used in areas that are difficult to
reach and are not toxic to tissue. NaCl 0.9% liquid is
isotonic, which means it has the same properties as
the liquid in the human body. NaCl 0.9% liquid is
more recommended as a wound care fluid when
compared with other fluids such as H2O2, povidone
Iodhine, rivanol and other liquids that are toxic to
tissue. The principle of wound care products is to
maintain the wound environment to remain moist to
facilitate the healing process of the wound, maintain
tissue fluid loss and cell death. A moist wound
environment can accelerate the wound healing
process by helping to eliminate fibrin that is formed
in chronic wounds quickly (fibrinolytic) by
neutrophils and endothelial cells in a humid
atmosphere, reducing the incidence of infections
compared with dry treatment, helping to accelerate
the formation of growth factors which plays a role in
the healing process, and accelerates neutrophil
invasion followed by macrophages, monocytes and
lymphocytes into the injured area (Riani, Handayani,
2017).
Based on Riani, Handayani research (2017) state
that DM patients with diabetic foot injuries receiving
wound care, a significant degree of wound reduction
was obtained by using 0.9% NaCl + Honey. It shows
improvement in wound condition i.e. reduced wound
size, type and amount of necrotic tissue, amount of
exudate in the wound, and increased epithelialization
on the wound surface. In wound care management,
the result from Honey + NaCl 0.9%, the most
frequently encountered part by researchers is the
number of exudates patient that appear to be
diminishing, measurements of tissue granulation
before wound care show that most (80%) patients
have bright red granulation tissue or red flesh
covering 25% of the wound area. While a small
proportion (20%) of other patients have not yet
experienced tissue granulation. Observation and
measurement of tissue granulation after wound care
showed that all (100%) patients had bright red or
flesh-red granulation tissue covering 75% to 100%
of the wound area. Observation on the parameters of
tissue epithelialization before treatment of wounds
has not seen the appearance of tissue
epithelialization in all patients.
Nuwa research, 2018 used original honey,
honey works with its moist nature so that it supports
the growth of granulation tissue and epithelialization
which can support the reduction in wound size.
Lomatull works by reducing edema of the wound, so
that the size of the wound looks smaller. Necrotic
tissue type shows that the majority (8%) of patients
treated with honey do not have necrotic tissue. A
small portion (2%) of patients have necrotic tissue in
the form of non-living white tissue and / or peeling
tissue that is yellowish and non-sticky. Patients
treated with honey do not have necrotic tissue and
only small proportion (2%) of patients have necrotic
tissue with <25% of the wound bed. Researchers
assume that the effects of moisture caused by honey
in necrotic tissue will soften the necrotic tissue so
that necrotic tissue in wounds treated using honey is
easier to do. The parameter of exudates number in
the wound care group using honey is obtained by the
majority of patients do not release the exudate and it
is only small proportion of patients still produced a
small amount of exudate.
Honey that is used certainly has the same content
or composition, namely amino acids, total
carbohydrates, protein, vitamin A, vitamin C,
calcium, iron, sodium (sodium), total fat and
cholesterol, but the differenciate is water
composition in honey. Quoted from The National
Honey Board (2004) in Faisol Al Fady research
(2012) Original honey has a water content of 17.10
grams. Honey quality standards in Indonesia,
especially for commercial purposes, refer to SNI 01-
3545-1994. Maximum water content from honey is
22%, however, laboratory testing must still be
carried out beforehand. The activity of low water
content and with high osmolarity in wound care
agents is believed to be something that can prevent
infection and speed up the wound healing process.
This osmosis process absorbs water from bacteria in
the wound so that it can inhibit the growth of
bacteria due to lack of water and dry the bacteria so
that the bacteria are difficult to grow and eventually
die. Besides the water content contained in honey
will provide moisture to the wound, so that the
wound granulation process grows well (Rahman,
Rahmayani, 2016).
Other content in honey that influences wound
granulation is the presence of iron and sodium
solution (NaCl). The content of iron is able to help
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
40

the process of red blood cells formation that function
to provide a supply of nutrients and oxygen in the
wound area, so that with this supply it is very helpful
to stimulate the growth of new tissue in diabetic foot
wounds. The sodium content (NaCl) which functions
as a safe isotonic solution to assist in wound care
(Rahman, Rahmayani, 2016).
The difference in the degree of diabetic wounds
before and after honey is given to patients with
diabetic foot injuries is due to the process of honey
content that maintains and keeps the wound
environment moist to facilitate the healing process
of wounds, maintain tissue fluid loss and cell death
so as to accelerate the regeneration of wound
healing. It is influenced by the achievement of good
intensity during the intervention. When the
intervention of honey is conducted in a pleasant
place and atmosphere, it can increase the enthusiasm
and motivation of respondents during the
intervention. Some respondents who did not
experience a reduction in diabetes after an
intervention were affected by the condition of the
wound (extent, depth of the wound, and length of
wound care) and the costs incurred during wound
care. Management of diabetic wounds should be
carried out on a continuous basis which includes
dietary foods that trigger delay in wound healing, so
that no further complications such as amputation
occur, so wound care is a nursing action aimed at
preventing the risk of amputation, an analysis of the
cost effective use of honey will beneficial in wound
care (Al-Maskari, 2015).
Nabhani and Yuli Widiyastuti (2017), treated
diabetic foot wounds using NaCl and natural honey
(water content less than 1896), where if the wound
was treated using both combination, because NaCl
has isotonic properties (safe for used as a clean
wound) and the nature of honey itself can grow good
granulation of tissue, and cause a moist effect (the
wound will experience healing if the conditions
around the wound are moist). To find out whether
honey is used as natural or not and whether the
water content is really below 1896, laboratory tests
must be done first. But in this study, researchers
used original honey and its water content was tested
at 17%. In addition, it is not only honey that affects
wound healing. The size, the depth and the degree of
wound are also important factors in the wound
healing process. The smaller of wound, the
shallower the wound, and the smaller of wound
degree, the healing is faster. Conversely, if the
wound gets bigger, the deeper and the higher of
wound degree, it will take quite long time to make
the wound healing.
It proves that honey is suitable for grade 1 to 3
diabetic foot injuries. But honey can also be used for
wounds that have more than 3 grades. Judging from
the benefits of honey that can attract pus and make
moist wound, honey can also given more than grade
3. For example in grade 3 or 4 diabetes injuries, the
wound has pus and there is a lot of dead tissue as a
result, lack of oxygen in the wound area. Because
the honey benefits can lift dead tissue, so the wound
that has a lot of dead tissue can be removed easily by
professional / expert nurses (surgeons). It is done so
that no errors occur when removing dead tissue,
because if wrong cut will result bleeding in the
wound.
The wound acidification process, on average,
heals wounds very quickly as seen from when the
wound is covered with honey because it can create
moisture that is not affected by the environment.
Honey is effective as a topical therapy because it
contains nurtition which speeds up healing in the
diabetic foot injury. Besides speeding up the wound
healing, honey also helps debridement and prevents
necrotic formation. The effect of honey on wound
healing produces kind of chemical substance for
debridement of damaged and dead tissue (Fain, A.
2017).
According Karimi, 2019, the honey usage in the
treatment of diabetic foot wounds has proven to be
effective. Research conducted on 33 respondents
who were treated with honey, 29 respondents
showed success marked by a good healing process,
and 3 respondents did not show good results because
the client experienced immunodeficiencies. In this
study diabetic foot wound healing was characterized
by wounds becoming cleaner, signs of infection
disappeared, inflammation, swelling, and pain were
quickly reduced, odor was reduced, slough, and
necrotic tissue was reduced, granulation and
epithelialization increased and minimal wound
healing in scars / tissue scar.
4 CONCLUSIONS
Honey is very good as bandage in cases of diabetic
foot injuries, especially in developing countries.
Treatment of diabetic foot wound uses considerable
amount of money and clinically effective pads. More
important, it is very safe because it does not produce
complications (local or systemic), or the emergence
of bacterial resistance. It is very necessary to
improve the general condition of patients to achieve
optimal results. Furthermore, when taking the action
of original honey administration, it must be patient
The Effectiveness of Original Honey Treatment toward Diabetic Foot Infection Wounds Healing
41

and there is trust between patient and medical staff,
besides that the treatment must be routine and the
patient must be obedient when done by the nurse so
that it will get good results. From the data analysis
results and willcoxon test with 20 respondents
obtained p = 0.001 <α = 0.05, it can be concluded
that there is an influence of original honey usage on
the diabetic foot infection wounds healing.
5 SUGGESTIONS
After the research concludes the research results, the
researchers expect the following advices:
a) For nurses, it is expected to further enhance their
knowledge and be able to apply treatment of
diabetic foot infection wounds given honey
(alternative therapy)
b) It is hoped that further studies can examine
diabetic foot infection wounds to different
degrees using other wound care techniques
REFERENCES
Al-Maskari F, El-Sadig M. Prevalence of Risk Factors for
Diabetic Foot Complications. BMCFam Pract
2015;8:59.
American Diabetic Association. Preventive Foot Care in
Patients with Diabetes. Diabet Care 2015;26:S78–9.
Andersen CA, Roukis TS. The diabetic Foot. Surg Clin
North Am 2017;57:1149–77.
Andriana, 2016. Standar Of Medical Care In Diabetik.
Vol 1, Universitas Pahlawan Tuanku Tambusai.
Arikunto, S 2014, Prosedur Penelitian Suatu Pendekatan
Praktek. Jakarta: Rineka Cipta.
Bryant, R. A., and Nix, D. (2017). Acute and chronic
wounds: current management
Burns, N., and Groove. (2015). The Practice of Nursing
Research-Conduct, Critique
Chandalia, & Shah. (2016). Endocrinology, Metabolism &
Diabetes.(1sted.). Mumbai: Printedby United Printers.
Concepts. (3rded.).USA : Mosby Elsevier.
Dunford C, Cooper R, Molan P, White R. The use of
Honey in Wound Management. Nurs Stand
2016;15(11):63–8
El-Nahas M, Gawish H, Tarshoby M, State O, Boulton A.
The prevalence of risk factors for foot ulceration in
Egyptian diabetic patients. Diabetes Res Clin Pract
2018;25(9):362–6.
Fain, A. (2017). Diabetes mellitus - Medical surgical
nursing. (6thed.). Harcourt India
Faisol .a (2012), Perbedaan Efektivitas Perawatan Luka
Menggunakan Madu Dab Saffatulle terhadap Proses
Penyembuhan Luka DM Diwilayah Kerja Puskes
Rambipuji Jember.
Jeffcoate W. The incidence of amputation in diabetes.
Acta Chir Belg 2017;105:140–4.
Karimi, 2019. Impact Of Olive Oil And Honey On
Healing Of Diabetic Foot: A Randomized Controlled
Trial. Doi: 10.2147/Ccid.S198577.
Kazemi-Khoo N. Successful treatment of diabetic foot
ulcers with low-level laser therapy. Foot
2016;16(4):184–7.
Kozier, B., et. al. (2015). Fundamentals of nursing-
concepts, process and practice. (7thed.). J. B.
Philadelphia: Lippincott company.
Lerrer B, Zinger-Yosovich K, Avrahami B, Gilboa-Garber
N. Honey and Royal Jelly, Like Human Milk,
Abrogate Lectindependent Infection-Preceding
Pseudomonas Aeruginosa Adhesion. ISME J
2017;1(2):149–55.
Montgomery G, David D, Winkel G, Silverstein J,
Bovbjerg D. The Effectiveness Of Adjunctive
Hypnosis With Surgical Patients: A Meta-Analysis.
Anesth Analg 2015;94(6):1639–45.
Nabhani dan Yuli Widiyastuti, (2017). The Effect of
Honey To Provide Gangren Wound Healing on
Mellitus Diabetes Patients. DOI: 10.26576.
Notoadmodjo, S 2012, Metodologi Penelitian Kesehatan,
Jakarta: Rineka Cipta. Philadelphia: W.B. Saunders
Company.
Nuwa, 2018. Effectiveness of Honey in Treatment
Diabetic Foot Ulcer : A Systematic Review. Faculty
Of Nursing, Universitas Airlangga. International
Nursing Conference. https://www.researchgate.net/
publication/324005567
Rahman, Rahmayani, (2016). Efektivitas Penggunaan
Madu terhadap Proses Penyembuhan Luka Di Poli
Kaki Diabetik Rumah Sakit Umum Daerah Ulin
Banjarmasin. STIKES Sari Mulia Banjarmasin. ISSN:
2086-3454.
Reganson-Tennvaill G, Apelqvist J. Cost effective
management of diabetic foot ulcers. A review.
Pharmacoeconomics 2015;12(1):42–53.
Riani, Handayani, (2017). Comparison Of The
Effectiveness Of Modern Moist Wound Healing Care
And Complementer Therapy 0.9% Nacl + Original
Honey On Healing Of Diabetic Foot Weld Degree II.
ISSN 2580-2194
Saldi, 2012. Tissue Management, Inflamation And
Infection Control, Moisture Balance, Epithelial
Advancement. PPNI
Sari, A.S. (2014). Analisa Faktor- Faktor yang
Mempengaruhi Perawatan Diri Pasien Diabetes
Melitus Tipe 2 Di Kecamatan Medan Johor. Skripsi.
Diakeses Pada Tanggal 6 Maret 2016 Dari
Http://Www.Skripsi keperawatan.Com/Analisa-
Faktor-Faktor-Yang Mempengaruhi-Perawatan-Diri-
Pasien-Diabetes-Melitus-Tipe-2-Dikecamatan-Xx/.
Saunders. Kothari, C. R. (1988). Research methodology,
methods and techniques. (2nded.).
Suparni, Ibunda dan Wulandari, Ari. (2012). Herbal
Nusantara: 1001 Ramuan Asli Indonesia. Yogyakarta:
ANDI utilization (4thed.). Philadelphia: W.B.
Saunders Company.
WHO. (2013). Jumlah Penderita Diabetes Mellitus.
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
42
