
Development of a Virtual Reality Environment for Rehabilitation of
Tetraplegics
Gabriel Augusto Ginja
1 a
, Renato Varoto
2 b
and Alberto Cliquet Jr.
1,2,3 c
1
Bioengineering Post Graduate Program, University of S
˜
ao Paulo, Av. Trabalhador S
˜
ao Carlense,
400, CEP 13566-590, S
˜
ao Carlos, Brazil
2
Electrical and Computing Engineering Department, University of S
˜
ao Paulo, S
˜
ao Carlos, SP, Brazil
3
Orthopedics & Traumatology Department, Faculty of Medical Sciences, University of Campinas, Campinas, SP, Brazil
Keywords:
Virtual Reality, Spinal Cord Injury, Biomechanics.
Abstract:
Treatments based on Virtual Reality have been successfully used in motor rehabilitation of issues such as
Spinal Cord Injury and Stroke. Highly immersive Virtual environments combined with biofeedback can be
utilized to train functional activities on patients with these motor disabilities. This work details the develop-
ment of a portable Virtual Reality environment to train upper limbs activities on Spinal Cord Injury subjects.
The Virtual Reality environment depicts a personalized physiotherapy room where the user trains elbow and
shoulder by reaching 5 spots on table. Also the user have a biofeedback of both hands’ position. Finally this
system will be integrated a pilot biomechanical analysis using The Motion Monitor system to compare a group
of patients before and after a 6 week intervention with Virtual Reality.
1 INTRODUCTION
Spinal Cord Injury (SCI) afflicts from 50 to 1218
cases per million worldwide according to Spinal Cord
Injury Evidence (Devivo and Chen, 2011) and most
of these cases are caused by vehicles accidents. SCI
is classified by the neurological level of the injury
so that motor and sensory functions below the in-
jury are disabled. Because of that, SCI impacts so-
cial life and it limits the capacity to execute Activities
of Daily Life (ADLs). Most of tetraplegic’s ADLs
use reach and grasp movements (Varoto and Cliquet,
2015) which involve complex biomechanical analysis
of upper limbs in order to develop new techniques of
rehabilitation of these subjects. Therefore, tetraplegic
patients have a increasingly demand for innovative
and creative solutions that integrate technology with
physiotherapy to improve rehabilitation.
One of the main goals of motor rehabilitation is to
induce neuroplasticity on the patients. Neuroplastic-
ity or neural adaptation is the foundation of learning
(Montgomery and Connolly, 2003) and it’s the brain
ability to reorganize itself as a response to external
stimuli and consequently recover partially or com-
a
https://orcid.org/0000-0002-1021-0701
b
https://orcid.org/0000-0001-5333-7123
c
https://orcid.org/0000-0002-9893-5204
pletely motor and sensory functions. Some examples
of stimuli are Functional Electrical Stimulation (FES)
(Bergmann et al., 2019) and Motor Imagery. Mental
practice of a muscular activity as well of the visual-
ization of a muscular movement activates the corre-
sponding area of the brain that would be activated in
the actual movement (Edmund Jacobson, 1932). An
application of motor imagery is on training of athletes
by imaging the movement that would be executed dur-
ing a real competition. Mizuguchi (Mizuguchi et al.,
2012) made a study which stated that around 70 to 90
percent of a group of elite athletes agreed that motor
imagery alongside real training improved their perfor-
mance in real competition. Also his study concluded
that motor imagery treatment could be used in motor
rehabilitation.
An important example of motor imagery is Vir-
tual Reality (VR). VR can be defined as an advance
interface system that represents a 3D environment in
real time. It encompasses both non-immersive sys-
tems such as video games or pc and immersive like
Oculus Rift and HTC Vive. Villiger (Villiger et al.,
2015) performed a study with incomplete SCI sub-
jects using VR to train lower limbs by flexing ankle
and knee in the VR environment. The results were a
boost in motivation and in motor performance as well
as increase of brain capacities.
Ginja, G., Varoto, R. and Cliquet Jr., A.
Development of a Virtual Reality Environment for Rehabilitation of Tetraplegics.
DOI: 10.5220/0009103002210226
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 1: BIODEVICES, pages 221-226
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
221

Other VR based systems helped to enhance motor
rehabilitation. Park (An and Park, 2018) used a semi-
immersive VR system to evaluate standing position in
SCI subjects. Other example was a VR environment
alongside an instrumented glove (Dimbwadyo-Terrer
et al., 2016) used to train reach movements also on
SCI subjects.
This paper describes the development of a VR en-
vironment to train upper limbs’ exercises in SCI sub-
jects. The hardware chosen was Oculus Quest (Face-
book Technologies, Irvine, California, EUA) and the
VR environment was made with Unity 3D (Unity
Technologies, Copenhagen, Denmark). Oculus Quest
is a portable device thus it can be easily used in hospi-
tals and small places. This project is part of a collab-
orative work of Laboratory of Biocybernetics and Re-
habilitation Engineering from University of S
˜
ao Paulo
and Laboratory of Biomechanics and Rehabilitation
of the Locomotor System of University of Campinas
that contributed by developing the VR system and for
the treatment of SCI patients. This paper’s final part
is the description of the biomechanical analysis that
will be used to validate the VR Environment.
2 METHODOLOGY
2.1 Characterizing SCI Population and
ADL Protocol
The criteria for selection SCI population for this study
were the following: Tetraplegics, neurological level
of lesion from C4 to C8 according to American Im-
pairment Scale (AIS) from American Spinal Injury
Association (ASIA), no autonomic dysreflexia and
more than one year of lesion.
The main goal of this work is to improve ADLs
of SCI tetraplegics by training functional activities
with VR. C8 patients may still have hands movement
whereas C4 patients barely can move arms. For this
reason, the protocol chosen to be trained in the VR
environment is a movement that utilizes shoulder and
elbow to hands to reach 5 spots in a table. Starting
with the left hand in the bottom left spot, the patient
tries to reach every other spot in the table. Similarly,
the same protocol is made with the right hand.
All the patient will be divided in two groups: a
control group and a group that will make an interven-
tion with VR. Subsequently, both groups will make an
initial biomechanical analysis of upper limbs. Lastly,
the intervention group will be subjected to a 6 week
training with VR and, afterwards, another biomechan-
ical analysis.
2.2 Head Mounted Display and Oculus
Quest
Head Mounted Display (HMD) is a headset used to
display VR. Each HMD has two lens and each one of
them represents a image slightly displaced between
them resulting in a 3D perception of the image. This
effect is called stereoscopy and is one of the basis of
VR since it turns a 2D non-immersive experience into
a 3D immersive experience.
Another aspect of HMD that improves the immer-
sive experience is the head tracking. Gyroscope and
Accelerometers from HMD are responsible for track-
ing rotation and position respectively. Both sensors
combined with stereoscopic vision results in 3D vi-
sual environment where the user can see objects as
if they where real objects. In addition to the visual
experience of VR some HMDs have input devices to
capture commands of the user and turn them into ac-
tions in the virtual environment.
Oculus Quest is a portable HMD with two con-
trollers with motion sensors that are used to track
hand position (figure 1). In order to use the controllers
with tetraplegics, each controller is attached to the
wrist with a ribbon. Even though the protocol trains
shoulder and elbow movement, Oculus Quest’s con-
trollers only need to collect hand’s position and rota-
tion data so the program can check if the user made
the correct movement.
Figure 1: Oculus Quest HMD and Controllers.
2.3 VR Development and Setup
The VR environmnent was made using Unity 3D
which is one of the most popular game engine world-
wide. Oculus have a library with prefabricated assets
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
222
that get data from the Oculus Quest HMD and con-
trollers and convert them into variables in Unity 3D.
Unity 3D assets are capable of inherit classes from
other library. As an example, the initial position in
the VR scene is inherited from HMD real position.
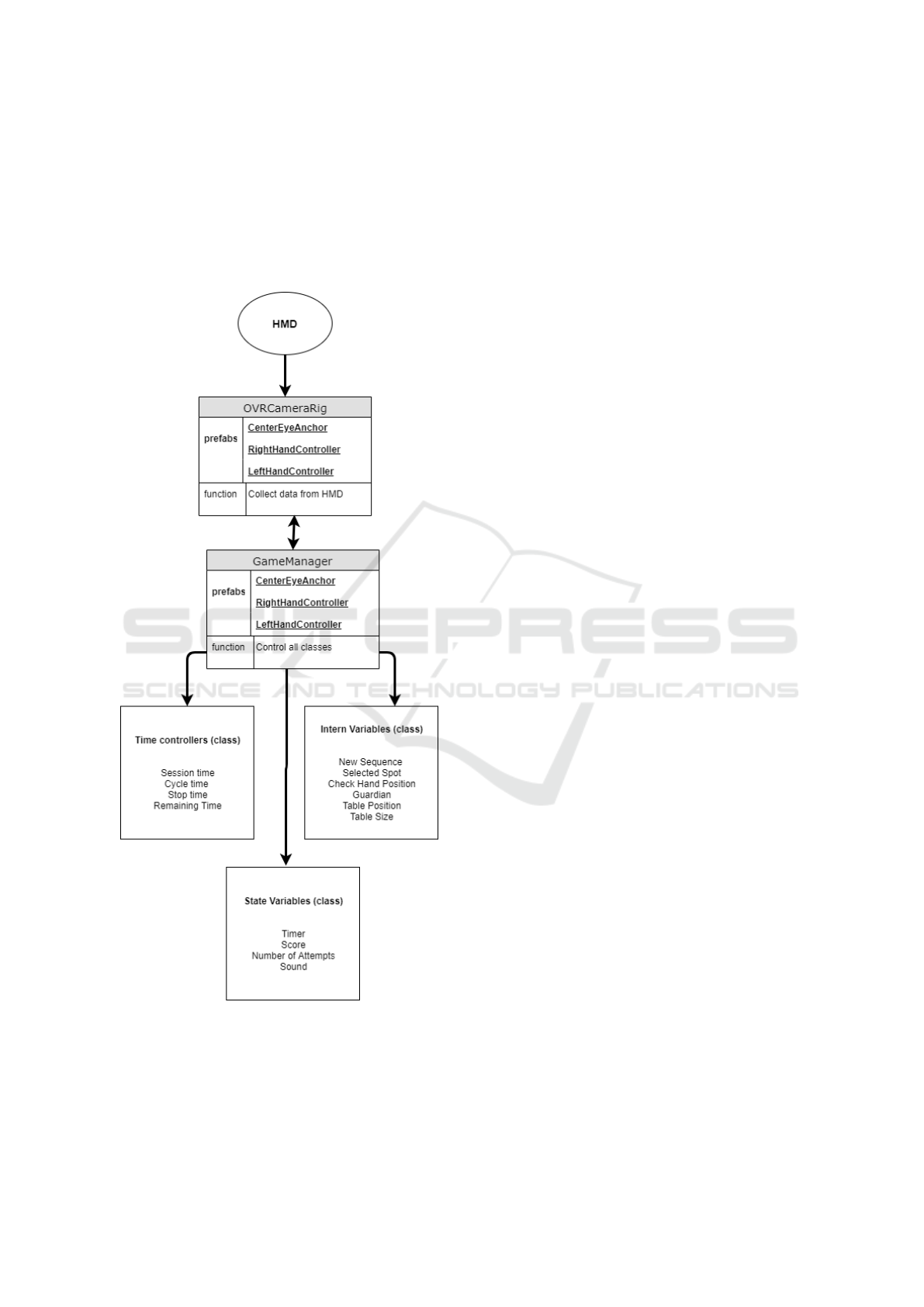
The figure 2 shows the main prefabs and scripts used
in the project.
Figure 2: Main prefabs, classes and variables used to con-
trol the vr project.
One of the most important prefabs is the OVR-
CameraRig which is the prefab that inherits data from
the HMD. It contains a player controller scripts that
allows the user to control the main camera and a
3D vector that have the same direction that the user
is looking. This vector is named CenterEyeAnchor.
Alongside the center anchor there are two other chil-
dren prefabs of the OVRCameraRig that are receiv-
ing data from the controllers. They are named Left-
HandAnchor and RightHandAnchor and their posi-
tion and rotation are referenced by the cylinder used
as the proprioceptive feedback.
Another significant aspect of the VR environment
is the main scene setup process. Before a VR ses-
sion the objects size and positioning must be defined
related to the real position of the user. This is made
by an introductory scene where the user looks to a
grid to select where the table will be created. Each
point of the grid corresponds to a potential initial po-
sition and the user stares at the desired spot for a
few seconds and it is selected. Tetraplegics could ac-
complish this procedure since it uses basically head
movements in order to select the spawn spot for the
table. Afterwards, he chooses the size of the table
and the blue spots are positioned automatically. In the
next step, the patient defines the size of the guardian.
The guardian of Oculus Quest is the region where the
user can move safely without hitting any objects in
the real room. If the patients somehow trespasses the
guardian, Oculus Quest will show the real room and
the guardian’s grid.
Finally, all the prefabs are organized by the Game-
Manager which is a singleton class that holds all other
classes of the project. Unity 3D allows the creation
of classes in form of scripts and each script contains
variables and functions used to control the game. As
shown in figure 2, the classes were separated in 3
types in order to help to identify any incidental er-
ror and correct it. Time controllers define when each
session and each cycle starts and ends as well they let
the user stop the game at any moment. Intern vari-
ables generate random sequences at the beginning of
each cycle and stores every action of the user. Finally,
state variables record time remaining, score and cy-
cles done. This last category is used as a feedback of
the user’s performance during the VR session.
2.4 User’s Interface (UI)
So far this paper has focused on movement based in-
teraction. However, some of the basic interaction such
as selecting an option or a scene should be adapted for
tetraplegics. The following section will discuss how
an adapted User’s Interface (UI) was created in a way
that only head movements are used to trigger events
in the VR environment.
Virtual Reality has a feature called Gaze Input
Development of a Virtual Reality Environment for Rehabilitation of Tetraplegics
223
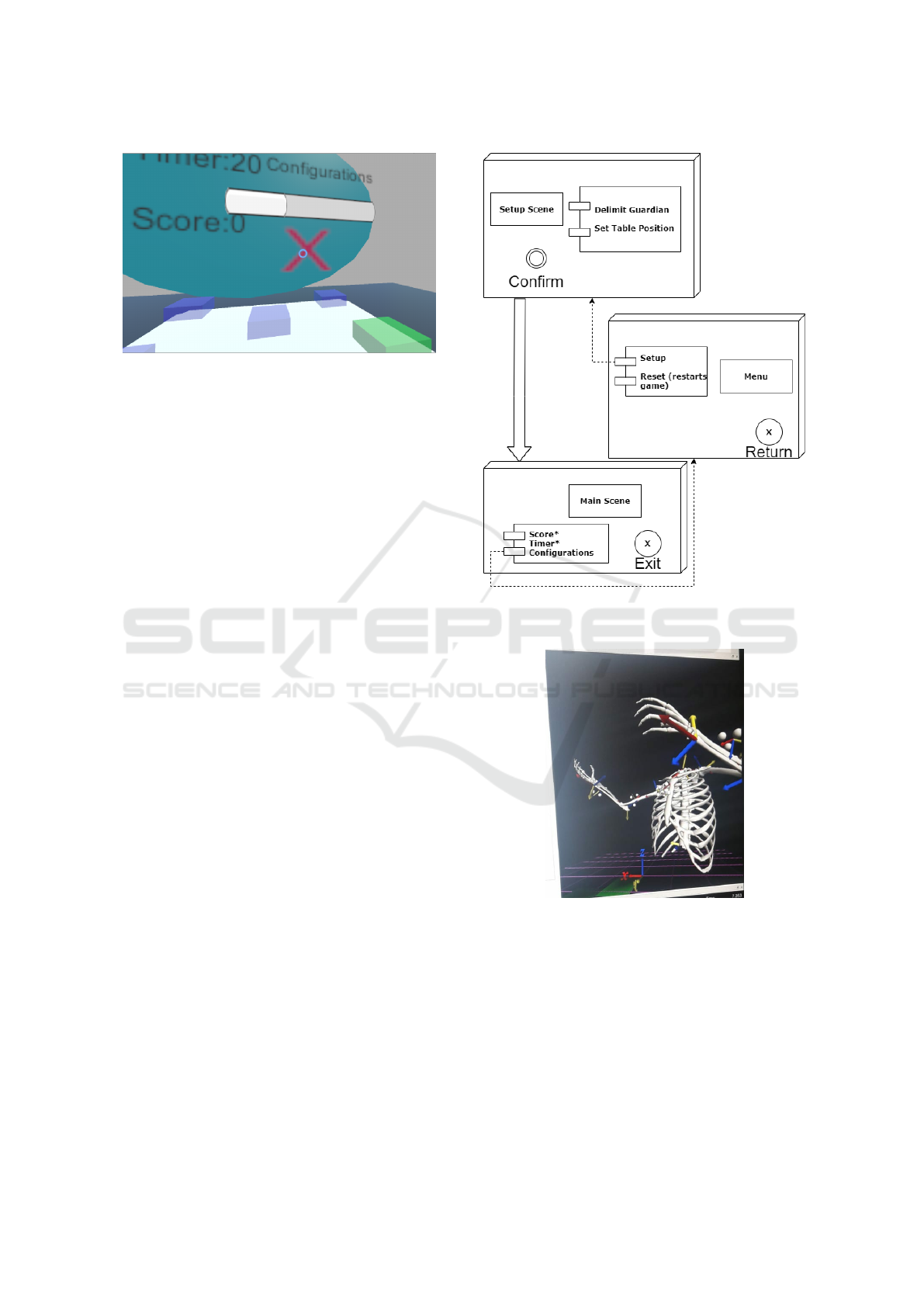
Figure 3: Gaze Input Controller and Slider example.
Controller (GIC) that is a pointer symbolized by a
small blue circle, as shown in the figure 3.
GIC uses a raycaster that inherits the direction of
the CenterEyeAnchor. Raycaster is a 3D vector used
to interact with Unity native UI. In other words, GIC
is a 3D vector that points to the direction where the
user is looking and it is used to trigger events in the
VR environment.
The UI is organized in several canvas and each
one of them has buttons that have a component called
event trigger which function is to switch in between
scenes. When the user looks at a canvas, GIC collides
with the canvas and a slider bar starts to charge. When
the slider is fully charged, the next scene in sequence
is displayed. The figure 4 shows all the scenes in the
VR environment and how they are related.
2.5 The Motion Monitor and
Biomechanical Analysis
This VR project will be used in a Biomechanical
analysis to validate if the VR intervention improved
the functional activities on tetraplegics. The Motion
Monitor system that will be used in this analysis in-
tegrates 12 Vicon (Vicon Motion Systems Ltd, Ox-
ford, United Kingdom) cameras with a data analysis
software as well it uses clusters instead of markers to
capture motion data. Hence, it reduces the number of
markers that are normally used with Vicon (over 20
markers) to a set of 9 cluster for a full body motion
capture.
For this study, only 5 clusters are used to capture
motion data from upper limbs: left and right arms
and forearms and thorax. For analysing motion data,
the Motion Monitor software reconstructs a 3D model
representing real time data of the upper limbs. The
figure 5 shows an example of upper limbs’ 3D model.
To verify if the clusters could be used on a
wheelchair, a healthy subject sat on a chair simulating
a SCI subject. Afterwards, 5 clusters were positioned
Figure 4: Diagram of main interfaces. Names with ”*” are
non-intractable.
Figure 5: Example of a 3D model created with Motion
Monitor.
on arms, forearms and thorax.
The kinematic data analyzed are angles and veloc-
ities from shoulders and elbows in 3 axes. During a
collect session, the patient have to move each arm in
5 spots disposed in a table in the same place that the
ones in the VR environment. This protocol is done
3 times for each hand to minimize eventual errors in
measure. The main goal is to evaluate maximum val-
ues for elbow flexion, shoulder abduction and veloci-
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
224

ties during the protocol before and after the VR treat-
ment and see if they were improved. Also a control
group will be submitted to the same analysis to com-
pare their performance with the intervention group.
3 RESULTS
3.1 VR Environment
The main scene of the VR Environment depicts a ta-
ble with 5 spots positioned in the center and in each
corner of the table (figure 6). In each cycle the user
have to move his hand to 5 different spots in 2 min-
utes. The sequence is generated randomly for each
cycle to prevent the patient to memorize the same se-
quence and to simulate movements more similar to
ADLs of reach.
Figure 6: Main Scene of the VR Environment.
The blue blocks indicate all the possible spots and
the next spot of the sequence is the green one. If the
patient successfully reaches the correct spot it returns
a sound and the next spot of the sequence becomes
green. In the other hand if he reaches the wrong
spot all blocks blinks a red colour and the sequence
restarts. Tetraplegics don’t have sensory functions be-
low the neurological level. Because of this, biofeed-
backs such as colour changes and sound effects are
important to indicate to the patient if an action taken
in the scene is correct or not. Similarly, SCI subjects
need a proprioceptive feedback from the VR system
to know the real position of their hands. The VR en-
vironment have a proprioceptive feedback in form of
two small purple cylinder that have both rotation and
position of the real hands depicted in real time. The
green arrow and the blue arrow of each cylinder in-
dicate parallel and orthogonal vectors related to each
palm respectively.
Each cylinder and each spot have an invisible col-
lider box to verify if the user correctly reached a se-
lected spot. When the cylinder’s collider enters in a
spot, the program checks if the spot is correct and,
when it leaves the spot, the next game action is taken.
Besides that, there is a small menu above the table
that displays time remaining, score, settings and exit
button.
3.2 Preliminary Tests
The VR environment is part of a pilot study where
the main goal is to test viability. Consequently, the
VR system was tested on healthy subjects to guaran-
tee that it would be safe to use it with SCI subjects.
The preliminary tests showed that the VR could check
correctly if the user reached the selected spot only ver-
ifying hand’s data. Other positive result was that the
GIC interface that could be used to navigate through-
out scenes alongside with the controllers. However,
the setup scene had problems such as the floor level of
the environment that was wrong in some cases. This
may occur due to the default configurations of Ocu-
lus Quest. Also the Setup Scene will need to consid-
erate additional information like height to calculate
the user’s baseline. Even though the protocol worked
fine, baseline would increase redundancy and reduce
errors of positioning.
First issue was holding controls using a rib-
bon. Although it hold still the controllers, a support
would be more appropriated to use with SCI subjects.
Nonetheless, both controller could capture data pre-
cisely while attached to the wrists.
3.3 Biomechanical Analysis Pilot
A Biomechanical analysis pilot was made with a
healthy subject sat on a wheelchair. While the arms
and forearms had no issues, some changes had to
be made before positioning the thorax cluster. Nor-
mally, the thorax cluster is positioned on the back,
however that’s not possible with the wheelchair. The
second one was to calibrate the baseline with the sub-
ject seated because it’s normally done with the sub-
ject standing. The solution found to resolve the first
was to change the axis of the 3D model in order to
change the cluster position to the chest. The second
one couldn’t be directly resolved but it didn’t inter-
fere drastically in the analysis. The protocol data can
Development of a Virtual Reality Environment for Rehabilitation of Tetraplegics
225

be segmented and normalized using elbow flexion and
shoulder flexion as reference to identify each part of
the protocol.
Figure 7: Graphics of Left Shoulder Flexion and Left Elbow
Flexion.
The figure 7 shows raw data from shoulder and
elbow of a test subject. Both graphs shows clearly
that the protocol starts around the 750th time sample
(sample rate of 100Hz) because both shoulder and el-
bow angles have a significant variance starting in this
timestamp. This pattern is repeated for each spot, in-
dicating that is possible to identify when the patient is
reaching each spot. Hence, it’s possible to calculate
maximum and minimum values for flexion angles.
4 CONCLUSIONS
In conclusion, the preliminary study has brought
some evidences that could lead on a innovative treat-
ment for tetraplegics. A few improvements such as
setup and an appropriate support for the controller
should be made before the VR environment is used
with SCI subjects. However, the main mechanics of
the VR environment worked which may suggest that
it could work with SCI. The next steps are: a) Create a
baseline calibration for VR environment; b) Polish the
3D models to create a better immersive experience;
c) Ethics committee approval for VR experiments on
SCI subjects; d) Validate the VR Environment with a
SCI population.
ACKNOWLEDGEMENTS
This work was supported by grants from S
˜
ao Paulo
Research Foundation (FAPESP) and from National
Council for Scientific and Technological Develop-
ment (CNPq)
REFERENCES
An, C. M. and Park, Y. H. (2018). The effects of semi-
immersive virtual reality therapy on standing bal-
ance and upright mobility function in individuals with
chronic incomplete spinal cord injury: A preliminary
study. Journal of Spinal Cord Medicine, 41(2):223–
229.
Bergmann, M., Zahharova, A., Reinvee, M., Asser, T.,
Gapeyeva, H., and Vahtrik, D. (2019). The effect of
functional electrical stimulation and therapeutic exer-
cises on trunk muscle tone and dynamic sitting bal-
ance in persons with chronic spinal cord injury: A
crossover trial. Medicina (Lithuania), 55(10).
Devivo, M. J. and Chen, Y. (2011). Epidemiology of trau-
matic spinal cord injury. In Spinal Cord Medicine:
Second Edition.
Dimbwadyo-Terrer, I., Trincado-Alonso, F., de los Reyes-
Guzm
´
an, A., Aznar, M. A., Alcubilla, C., P
´
erez-
Nombela, S., del Ama-Espinosa, A., Polonio-L
´
opez,
B., and Gil-Agudo,
´
A. (2016). Upper limb rehabili-
tation after spinal cord injury: a treatment based on
a data glove and an immersive virtual reality environ-
ment. Disability and Rehabilitation: Assistive Tech-
nology, 11(6):462–467.
Edmund Jacobson (1932). Electrophysiology of Mental
Activities. The American Journal of Psychology,
44(4):677–694.
Mizuguchi, N., Nakata, H., Uchida, Y., and Kanosue,
K. (2012). Motor imagery and sport performance.
The Journal of Physical Fitness and Sports Medicine,
1(1):103–111.
Montgomery, P. and Connolly, B. (2003). Clinical Applica-
tions for Motor Control.
Varoto, R. and Cliquet, A. (2015). Experiencing Func-
tional Electrical Stimulation Roots on Education, and
Clinical Developments in Paraplegia and Tetraplegia
With Technological Innovation. Artificial Organs,
39(10):E187–E201.
Villiger, M., Grabher, P., Hepp-Reymond, M. C., Kiper, D.,
Curt, A., Bolliger, M., Hotz-Boendermaker, S., Kol-
lias, S., Eng, K., and Freund, P. (2015). Relationship
between structural brainstem and brain plasticity and
lower-limb training in spinal cord injury: A longitu-
dinal pilot study. Frontiers in Human Neuroscience,
9.
BIODEVICES 2020 - 13th International Conference on Biomedical Electronics and Devices
226
