
The Nature of Digital Innovation and
What Can Be Learned for Information Systems Management
Stefanie Kaczmarek
a
, Martin Benedict
b
and Marcel Susky
Chair of Wirtschaftsinformatik, esp. Systems Development, Technische Universität Dresden, Dresden, Germany
Keywords: Digital Innovation, Information Systems Management, Systematic Literature Review, Quantitative/
Qualitative Analysis.
Abstract: In all spheres of life, the ongoing digital transformation has led to an increasing variety of definitions, types,
and characteristics of digital innovation. However, the diversity of terminology regarding digital innovation
may cause confusion about the general concepts in this context. Therefore, the objective of this study is to
provide a descriptive insight into the nature of digital innovation. Our paper shows how digital innovation has
altered since its emergence in the field of information systems re-search. This change of understanding has
an impact on the design of information systems. Following a systematic literature review, a quantitative and
qualitative analysis of the identified vocabulary was conducted to gain types and characteristics of digital
innovation. Based on these characteristics, we describe how digital innovation influences information systems.
We focus on hospital information systems as a case example from the healthcare sector.
1 INTRODUCTION
The use of novel digital technologies, such as virtual
reality, cloud computing, and artificial intelligence,
leads to changes in business models, internal com-
pany processes, products, and services. For compa-
nies and their customers, new opportunities in infor-
mation acquisition, communication and consumption
arise through digital technology (Rachinger et al.,
2018). These changes by novel digital technology are
named as Digital Innovation (DI). Not only tradi-
tional IT companies such as Apple or Google are in-
volved in the development of DI, but also companies
in finance, mobility and other industries (Fichman,
Dos Santos & Zheng, 2014). Well-known success sto-
ries for business models based on DI include Airbnb,
Uber, and Spotify, which conduct their business ac-
tivities via digital peer-to-peer platforms. While
SAP’s Simple Finance Add-on is a highly automated
and standardized solution for digitizing business pro-
cesses, Fitbit and Amazon’s Kindle are examples of
digital product innovations (de Reuver et al., 2018).
The term “Digital Innovation” was coined by
Yoo, Henfridsson & Lyytinen (2010) and refers to the
possibility of developing new products by combining
a
https://orcid.org/0000-0001-8204-7010
b
https://orcid.org/0000-0003-4262-9029
physical components with digital technologies. Since
digitalization offers the opportunity to fundamentally
change former product experiences, DI are an essen-
tial step and foundation for competitive advantage for
companies (Yoo, 2010). It is undisputed that DI plays
a central role in the context of companies and in re-
search on business information systems too (Hevner
et al., 2019). However, as several different defini-
tions, types, and characteristics of DI have prevailed,
there is still confusion about the nature of DI and what
DI means in the context of specific information sys-
tems. This diversity needs to be considered when aim-
ing to improve existing information systems through
DI. Different objectives may arise from different un-
derstandings of DI in different sectors of the econ-
omy.
For example, the healthcare domain is essential
for every society and economy, but the potential for
integrating DI into this domain has not been fully ex-
ploited yet (Jung & Padman, 2015). Especially hospi-
tals, as major medical care providers, are affected by
DI. However, it is less researched which aspects of DI
may improve the success and utility of information
systems in hospitals.
Addressing this gap, this paper analyses the na-
ture and understanding of DI in information systems
Kaczmarek, S., Benedict, M. and Susky, M.
The Nature of Digital Innovation and What Can Be Learned for Information Systems Management.
DOI: 10.5220/0009311607870797
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 787-797
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
787

research. Based on this analysis, the paper derives im-
plications for the management of Information Sys-
tems (IS) in hospitals. Consequently, the paper ad-
dresses the following research question:
RQ: How have Digital Innovations changed in
the course of digital transformation and
what implications can be derived for the
management of Information Systems in hos-
pitals?
The remainder of this paper is structured as fol-
lows. After this introductory chapter, the research
method used for the study is explained in chapter 2.
The results of the systematic literature review are pre-
sented in chapter 3 and discussed in chapter 4. The
paper concludes with a conclusion and gives an out-
look on further research needs.
2 METHOD
2.1 Literature Analysis and Review
In order to gain a comprehensive understanding of DI,
we conduct a systematic literature review following
Fettke (2006) and Cooper & Hedges (1994). We ana-
lyze the existing literature using a quantitative de-
scription of the literature and a qualitative analysis of
the full texts to conceptualize the understanding of
DI. The knowledge gained from the quantitative and
qualitative data analysis contributes both to a broader
conceptualization of DI and to the provision of impli-
cations for theory and practice in the management of
HIS. The quantitative analysis supports understanding
of the context, in which DI is used and conceptualized.
Therefore, we analyze the meta-data of the papers.
For a broader overview of papers, we searched in
the electronic databases Scopus and Web of Science.
These interdisciplinary databases were selected be-
cause DI is a phenomenon that can be found in all sci-
entific disciplines. Hence, the search term “digital in-
novation“ was used in title, abstract and keywords.
The search carried out in July 2019 yielded in a total
of 677 (Scopus) and 318 (Web of Science) hits. After
the removal of duplicates and incomplete sources,
792 publications remain for further consideration.
The aim was to analyze the most important publica
1
The area Science covers Mathematics; Biology; Psychol-
ogy; Physics and Chemistry. Humanities and Social Sci-
ences consists of Social Sciences (SS); Education, Linguis-
tics; Cultural Studies, Arts and Humanities (CSAH) as well
as Law and Public Administration. Computer Science (CS);
Engineering (E) and Mechanical Science belong to the su-
tions regarding DI. Therefore, we sorted and recorded
the literature sources according to their citation fre-
quency. Publications cited at least 50 times were in-
cluded in a detailed qualitative analysis. In this case,
50 was chosen as the reference value, since the cita-
tion frequency of subsequent publications was rapidly
decreasing. After examining the full-text of the most
frequently cited publications, two of them were ex-
cluded. Thus, 12 publications remain (see Table 1, up-
per part). To expand the data basis for analysis, further
papers were searched from the resulting list of the da-
tabase search. Six additional publications (see Table 1,
lower part) were identified. These were selected by
their title. In the backward search, we selected papers
that directly treat digital innovation in the title.
Table 1 shows the publication year and the num-
ber of citations of the twelve most frequently cited
publications in the field of DI. The number of cita-
tions of publications from the reference list search re-
fers to the citation frequency of Scopus. In addition,
the subject areas to which the publications can be as-
signed are presented. According to the two selected
databases, it is possible to search/classify document
results by subject area. Since both databases use dif-
ferent categories in relation to the subject areas, a new
classification has been created for reasons of compa-
rability. For this purpose, five superordinate areas –
Science, Humanities and Social Sciences, Engineer-
ing Sciences, Civil and Environmental Engineering,
Medicine – were identified, to which 17 newly cre-
ated classes of subject areas can be assigned.
1
The next step is to evaluate the identified litera-
ture, i.e. the check for relevance, the processing and
systematization, as well as the analysis and interpre-
tation of the results against the background of the
problem (Fettke, 2006). In the full-text analysis, we
analyzed the definitions of DI and screened the papers
for DI characteristics.
2.2 Case Study
The characteristics of DI are used to systematize im-
plications for Hospital Information Systems argumen-
tatively. As a case study, we selected the healthcare
sector because this sector is faced with a lot of barriers
and issues regarding the implementation of digital
technology (Alkraiji et al., 2013; Lluch, 2011).
perordinate area Engineering Sciences. To Civil and Envi-
ronmental Engineering count Architecture, Civil Engineer-
ing; Transportation and Traffic Sciences; Business, Man-
agement and Economics and also Environmental Sciences
(ES). The fifth area includes Medicine.
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
788

As a specific digital innovation, we selected the
implementation of the Health Level Seven Fast
Healthcare Interoperability Resources (HL7 FHIR)
standard in Hospital Information System (HIS). A
HIS is a comprehensive and integrated subsystem of
a hospital that includes information on administrative,
financial and clinical aspects. The HIS serves to map
all information acquisition, information processing
and information storage processes resulting from the
interaction between human and machine actors. It
supports the people involved in clinical everyday life
in carrying out daily work processes, such as planning
bed occupancy, optimal utilization of operating
rooms or diagnosis, in all functional areas of the hos-
pital (Khalifa & Alswailem, 2015; Moghaddasi et al.,
2018; Moser, 2013; Winter et al., 2011). The goal of
a HIS is to contribute to adequate patient care that
considers the concept of cost-effectiveness on the one
hand and satisfies legal framework conditions on the
other hand. The HIS has the task of providing the
right information about patients to the right recipient
at the right time, at the right place, in the required
quantity and quality. The automated subsystems of
HIS are referred to as Hospital Application Systems
(HAS). Examples of HAS are the Clinical Documen-
tation and Management System (CDMS), the Labor-
atory Information System as well as the Picture Ar-
chiving and Communication System (Haux, Winter,
Ammenwerth & Brigl, 2013; Moser, 2013). We se-
lected HIS because they are important for the imple-
mentation of DI in the healthcare sector (Scheplitz et
al., 2019). They are a focal point of data management
in integrated care settings and store versatile data
about the patient’s treatment chain.
Besides the installation of new digital devices, the
integration of DI into HIS is also the implementation
of software or the reconfiguration of existing HAS
and the integration of them. For example, the imple-
mentation of a generic and reusable Application Pro-
gramming Interface (API) for third party applications
can be treated as DI. The HL7 FHIR standard pro-
vides such an approach (Bender & Sartipi, 2013). It
describes a generic resource-oriented representation
of clinical data structures. Like a building block sys-
tem, these resources can be combined for different
use cases. A CDMS could publish such resources and
another HAS can use them for different use cases.
3 RESULTS
3.1 Quantitative Analysis
A total of 792 publications with regard to time per-
spective, the geographical perspective, and the sub-
ject area were examined in the course of the quantita-
tive analysis. For this purpose, data sets from Scopus
and Web of Science were recorded in spreadsheets.
Afterward, the data sets were graphically processed
using diagrams.
Table 1: Digital Innovation papers and their publication year, number of citations, country, subject area.
No. Reference year # citations Subject area
1 Yoo, Henfridsson & Lyytinen 2010 545 CS, SS, BME
2 Yoo, Boland, Lyytinen & Majchrzak 2012 428 BME
3 Lusch & Nambisan 2015 240 CS, CSAH, BME
4 Boudreau 2012 198 BME
5 Fichman, Dos Santos & Zheng 2014 169 CS, BME
6 Y. Yoo 2013 103 CS
7 Barrett, Oborn, Orlikowski & Yates 2012 92 BME
8 Nylén & Holmström 2015 84 BME
9 Nambisan & Lyytinen 2017 66 CS, CSAH, BME
10 Nambisan 2013 65 CS, SCAH, BME
11 Svahn, Mathiassen & Lindgren 2017 51 CS, BME
12 de Reuver, Sørensen & Basole 2018 50 CS, SS, BME
13 Lee & Berente, 2012 38 BME
14 Huang, Henfridsson, Liu & Newell 2017 36 CS, BME
15 Henfridsson, Mathiassen & Svahn 2009 27 CS
16 Sørensen & Landau 2015 23 SC, BME
17 Svahn & Henfridsson 2012 23 E
18 Selander, Henfridsson & Svahn 2010 21 CS
19 Svahn, Lindgren & Mathiassen 2015 7 E
20 Yoo, Lyytinen, Boland, Berente, Gaskin,
Schutz & Srinivasan
2010 not speci-
fied
CS, BME
The Nature of Digital Innovation and What Can Be Learned for Information Systems Management
789
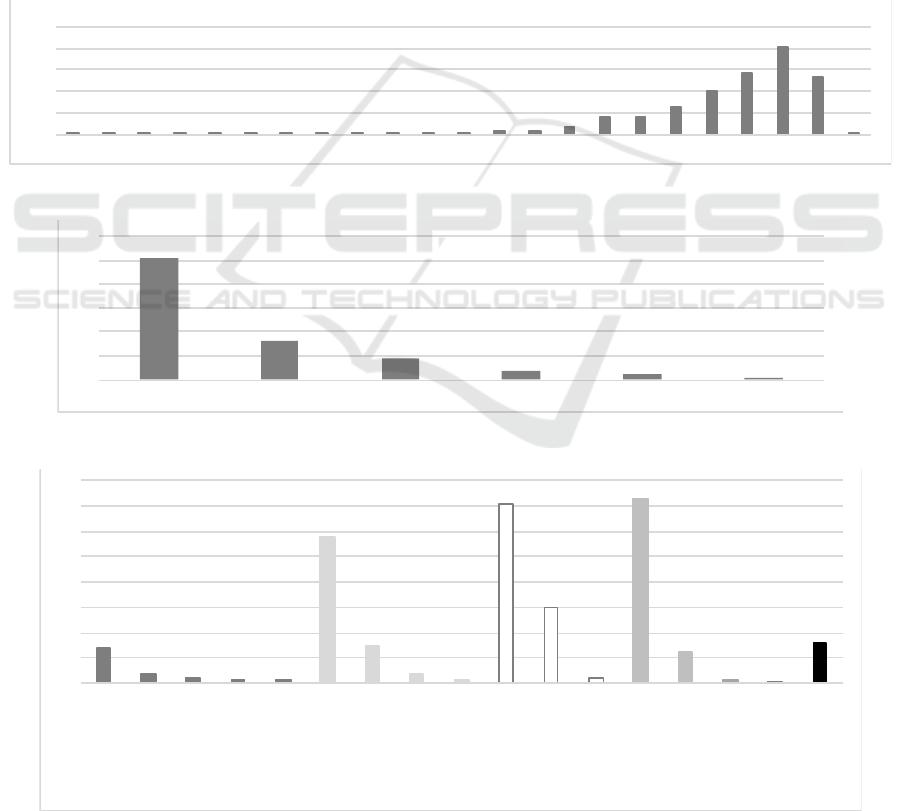
Time Perspective. Figure 1 shows the development
of the number of public ations over time. The number
of publications increased continuously, especially
since 2010. Since 2010, the number of publications
almost increased by thirty times and has had a strong
increase up to 202 papers in 2018.
Geographical Perspective. In total 881 authors were
counted from 58 different countries of origin. For
56 authors (about 6 percent) no assignment to a given
country was possible due to missing information. Fig-
ure 2 shows the continental distribution of authors
with the region of origin and publications devoted to
DI (n = 825). Nearly 61 percent (n = 507) of the au-
thors originate from Europe, followed by North
America with about 20 percent (n = 164) and Asia
with about 11 percent (n =88). The remaining 8 per-
cent (n = 66) of authors originate from Australia, Af-
rica and South America. At the level of countries, the
five topmost are: United States (about 18 percent,
n = 145), United Kingdom (12 percent, n = 99), Ger-
many (about 10 percent, n = 79), Italy (about 7 per-
cent, n = 54) and Sweden (about 6 percent, n = 48).
Subject Area. Figure 3 depicts the number of assign-
ments per subject area and highlights the five super-
ordinate subject areas build from the 17 created sub-
ject areas shown. As the figure illustrates, most of the
publications on DI are found in the superordinate sub-
ject areas Engineering Sciences (white, n = 514),
Civil and Environmental Engineering (middle gray,
n = 437) and Humanities and Social Sciences (light
gray, n = 386). By comparison, those in the areas of
Figure 1: Number of Publications focusing on Digital Innovation per Year.
Figure 2: Regional distribution of publications focusing on Digital Innovation.
Figure 3: Number of Publications focusing on Digital Innovation per subject.
1111212
454467
10
20
40 40
64
101
142
202
132
2
0
50
100
150
200
250
1983 1996 1999 2000 2001 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020
507
164
88
37
21
8
0
100
200
300
400
500
600
Eu ro pe No rt h Am erica As ia Au str alia Afr ica Sou th Am erica
69
17
10
96
287
73
18
8
353
150
11
366
63
7
1
80
0
50
100
150
200
250
300
350
400
M
a
th
emati
c
s
P
sychol
o
gy
B
i
ol o
g
y
C
h
em
i
st
r
y
P
hy s ic
s
Soc
i
al
S
ci
e
nc
e
s
C
ul
t
ur
al
S
tudi
e
s,
A
r
ts
a
nd
Hum
a
n
i
ties
E
d
uc
at i
on,
Li
n
g
u
i
s
t
ic
s
L
a
w
a
nd
P
ublic
A
dmi
nistration
C
omp
u
t
e
r
S
c
ien
c
e
E
ngi
n
eerin
g
M
e
ch
a
ni
c
al
S
ci
en
c
e
B
usiness,
M ana gem en t
and Econo
m
i
cs
En
vi
r
o
n
m
en
t
al S
c
ie
nce s
Arch
i
tec
ture, C
i
vi
l
E
ng i
n
e
eri
n
g
Trans
p
or
ta ti
o
n
a
n
d
Traff
i
c
S
c
iences
M
e
di cin e
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
790

Science (dark gray) and Medicine (black) are low.
With respect to the illustrated disciplines, publica-
tions on DI are mainly found in Business Manage-
ment and Economics (n = 366), Computer Sciences
(n = 353) as well as Social Sciences (n = 287).
3.2 Qualitative Analysis
A total of 20 publications with regard to the underly-
ing definition of DI, type of innovation and character-
istics of DI was examined in the qualitative analysis.
Table 2 depicts the seven distinct definitions found,
except those that refer repeatedly to the fundamental
publication by Yoo, Henfridsson & Lyytinen (2010)
or without novelty content with respect to the other
publications analyzed.
Definition and Types of DI. Seven of the 20 publi-
cations propose an own definition of DI (Fichman,
Dos Santos & Zheng, 2014; Huang, Henfridsson, Liu
& Newell, 2017; Lusch & Nambisan, 2015; Nam-
bisan & Lyytinen, 2017). Among them are three def-
initions by Yoo et al. (2010; 2010; 2012)
which differ
marginally. They define DI as a product innovation
in which physical and digital components merge.
They see the advancing digitalization as a necessary
prerequisite for this. In the other 13 cases, their defi-
nition was reused. As adoption to the fundamental
definition, Lusch & Nambisan (2015) as well as
Huang, Henfridsson, Liu & Newell (2017) emphasize
the aspect that DI can create a new kind of benefit or
value in a certain context. The advantage of this defi-
nitional approach is that it is not the value of the result
Table 2: Definitions, types, and characteristics of Digital Innovation.
No. Definition Type Characteristic
1 „We define digital innovation as the carrying out of new combina-
tions of digital and physical components to produce novel prod-
ucts. […] A necessary but insufficient condition for digital inno-
vation is that the new combination relies on digitization […].”
(Yoo, Henfridsson & Lyytinen, 2010 , p. 725)
product in-
novation
reprogrammability, data
homogenization,
self-referential nature
2 “A defining characteristic of pervasive digital technology is the in-
corporation of digital capabilities into objects that previously had
a purely physical materiality.” (Yoo, Boland, Lyytinen &
Majchrzak, 2012, p. 1398)
product in-
novation
convergence, generativity
3 „Service innovation can then be considered the rebundling of di-
verse resources that create novel resources that are beneficial (i.e.,
value experiencing) to some actors in a given context; […].”
(Lusch & Nambisan, 2015, p. 161)
service in-
novation
service ecosystem, service
platforms, value cocrea-
tion
4 “We define digital innovation quite broadly as a product, process,
or business model that is perceived as new, requires some signifi-
cant changes on the part of adopters, and is embodied in or enabled
by IT.” (Fichman, Dos Santos & Zheng, p. 330)
product,
process,
business
model inno-
vation
not specified, but in ac-
cordance to (Yoo, Hen-
fridsson & Lyytinen,
2010)
5 „We conceptualize digital innovation as the creation of (and con-
sequent change in) market offerings, business processes, or models
that result from the use of digital technology. Stated differently, in
digital innovation, digital technologies and associated digitizing
processes form an innate part of the new idea and/or is develop-
ment, diffusion, or assimilation.“ (Nambisan & Lyytinen, 2017, p.
224)
product,
platform,
service, cus-
tomer expe-
rience, other
value path-
way innova-
tion
malleable, editable, open,
transferable, continue to
evolve, unpredictability,
dynamic
6 “We define digital innovation as the recombination of digital com-
ponents in a layered, modular architecture to create new value-in-
use to users or potential users of a service.” (Huang, Henfridsson,
Liu & Newell, 2017, p. 302)
service in-
novation
separation of function and
form, separation of con-
tents and medium
7 “By digital innovation, we mean an innovation enabled by digital
technologies that leads to the creation of new forms of digitaliza-
tion.“ (Yoo, Lyytinen, Boalnd, Berente, Gaskin, Schutz & Sriniva-
san, 2010, p. 13)
product in-
novation
programmability, address-
ability, senesability, mem-
orability, traceability,
communicability, associa-
bility
The Nature of Digital Innovation and What Can Be Learned for Information Systems Management
791

as such that is considered, but the value perceived by
the customer. The customer, therefore, plays an active
role in the development of digital service innovations.
The bundling of different resources in digital service
innovation depends on the degree of digitization
(Lusch & Nambisan, 2015). According to Fichman,
Dos Santos & Zheng (2014), DI not only refer to
products but also to processes and business models,
which implies a broader view of DI. A further adap-
tation of the initial definition lies in the requirement
that users have to change. Nambisan & Lyytinen
(2017) provide the most comprehensive view by de-
fining DI as the introduction of novel “market offer-
ings”. The term “market offerings” is deliberately
kept open, as it conceals a multitude of outcomes,
such as products, platforms, services, customer expe-
riences, and value pathways. To enable these out-
comes, different digital technologies (digital tools, in-
frastructure) are needed, which themselves represent
an essential component of innovation and “may be
diffused, assimilated, or adapted to specific use con-
texts […].” (Nambisan & Lyytinen, 2017, p. 224).
Furthermore, DI can also be seen as a means for cre-
ating DI, but also as a result of it, and thus lead to new
forms of digitization (Yoo, Lyytinen, Boland, Ber-
ente, Gaskin, Schutz & Srinivasan, 2010).
Most often, DI is associated with product innova-
tion (Fichman, Dos Santos & Zheng, 2014; Nambisan
& Lyytinen, 2017; Yoo, Boland, Lyytinen &
Majchrzak, 2012; Yoo, Henfridsson & Lyytinen,
2010; Yoo, Lyytinen, Boland, Berente, Gaskin,
Schutz & Srinivasan, 2010), but also with service in-
novations (Huang Henfridsson, Liu & Newell, 2017;
Lusch & Nambisan, 2015). Fichman, Dos Santos &
Zheng (2014) define DI more broadly and include
process and business model innovations. Ultimately,
DI are much more than that: they can be product, ser-
vice, process, business model, application software,
platform, customer experience or other value innova-
tions (Nambisan & Lyytinen, 2017).
Characteristics of DI. Yoo, Henfridsson & Lyytinen
(2010) describe an initial set of the key characteristics
of DI. They name reprogrammability, data homoge-
nization, and self-referencing. Reprogrammability
signifies the separation of the form of the physical ob-
ject and its function. This means, that the behavior of
physical products can be changed during their life-
time. An example is the implementation of program-
mable operating systems on different physical de-
vices. Data homogenization offers the opportunity to
capture, process and display any type of digital con-
tent on the same digital device. An example is the use
of smartphones, which allows access to different
kinds of data and services. These can be integrated by
defined technological interfaces. Different digital
data can be combined and accomplish different func-
tions because the content is separated from the me-
dium. These two fundamental aspects are under-
pinned by Huang, Henfridsson, Liu & Newell (2017).
Self-reference, as the third unique characteristic,
points to the fact that the usage of digital technology
broadens the availability of digital devices and in con-
sequence leads to lower entry-barriers and higher dif-
fusion rates.
Also, Yoo, Lyytinen, et al. (2010) propose a more
detailed view and introduce six dimensions of DI:
digital materiality (and its properties program-mabil-
ity, addressability, senseability, memorability, com-
municability, traceability and associability), hetero-
geneity, locus of innovation, pace, convergence and
generativity (Yoo, Lyytinen, et al., 2010). Digital ma-
teriality is described as the inseparable integration of
social, physical and digital aspects.
Heterogenity de-
notes the variety of data, knowledge, and tools used
by DI. The locus of innovation draws on the location-
independent development of DI to save communica-
tion and storage costs. The speed at which new solu-
tions could be developed is referred to as pace. This
is possible because existing physical components as
well as established digital infrastructures are reused,
and re-combined. Convergence means the integration
of devices, networks, services and contents enabled
through data homogenization. Generativity is used as
a synonym for the ambiguity of DI due to the fact,
that DI is reinterpreted, expanded and refined perma-
nently. Yoo, Boland, Lyytinen & Majchrzak (2012)
generalized the latter two dimensions, convergence
and generativity, two years later, in 2012. According
to the generalization, convergence suggests the use of
digital technologies that creates a link between previ-
ously separated user experiences and industries as
well as embeds digital technologies into physical
products. Whereas their previous description of gen-
erativity is summarized to the terms dynamic and
malleability. Nambisan & Lyytinen (2017) refer to
the terms malleable, editable, open and transferable
as characteristics of digital artifacts. Further, since the
nature of DI is subject to constant change, they also
characterize DI by unpredictability and dynamism.
Lusch & Nambisan (2015) address central themes of
digital service innovations instead of characteristics.
3.3 Course of Digital Innovation
To show how the nature of DI have changed in the
course of the ongoing digital transformation, Figure 4
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
792

illustrates the development of DI over time. The hor-
izontal axis indicates the publication years, whereas
the vertical axis denotes the emerged innovation
types. A number in square brackets represents the ref-
erence and the publication year accordingly. Each of
those is enclosed by an ellipse, covering the innova-
tion types named in the respective publication. The
DI characteristics mentioned in the publication is rep-
resented as label. Ellipse overlaps illustrate the inter-
section of characteristics. Ellipses below the next
higher innovation type mark do not include this inno-
vation type. The central themes of digital service in-
novation have been included to complete the figure
(see dashed ellipse), but are not considered further
(see chapter 3.2).
Figure 4 shows that two papers by the same au-
thors were published almost simultaneously. While
one paper, published as a report, deals very thor-
oughly with six dimensions of DI (Yoo, Lyytinen, et
al., 2010), the other paper focuses on the distinction
between digital and conventional technologies (Yoo,
Henfridsson, Lyytinen, 2010). Two years later, the
authors published a third paper highlighting the char-
acteristics convergence and generativity (Yoo, Bo-
land, Lyytinen & Majchrzak, 2012), which were al-
ready part of the six dimensions of the report. Over a
period of four years, the three characteristics of the
fundamental paper (reprogrammability, data homog-
enization, self-referencing) were considered as the
prevailing view. In 2017, the aspect of dynamism and
unpredictability became prominent, and emphasized
the need for editability, openness, and transferability.
At the same time, the separation of function and form,
as well as the separation of contents and medium, was
established.
Concerning the innovation type, it is obvious, that
DI arise from digital product innovation. In addition,
there is a trend for DI in the direction of digital service
innovation. The innovation types of customer experi-
ence innovation and other value innovation were not
mentioned before its appearance in 2017.
3.4 Implications for the Management
of Information Systems in Hospitals
When questioning how the conceptualization of digi-
tal innovation influences the implementation and
management of HIS, the characteristics of DI can help
to systematize design criteria. In the following, we
use the characteristics of Y
OO ET AL. (2010) as guid-
ing characteristics. The implementation of DI in HIS
is challenging both from a technological and an or-
ganisational perspective. Different barriers exist on
different layers. We mainly focus on the enablers and
barriers at the information, application and infrastruc-
tural layer following S
CHEPLITZ ET AL. (2019). These
layers mainly comprise the view on products and
technological services. Therefore the selection of the
three characteristics of Y
OO ET AL. (2010) is adequate
as they focus on digital innovation with a product fo-
cus. The implementation of FHIR addresses the ena-
bler of the concerted definition of contents of medical
records and the barrier of faulty and incompatible
data models.
Reprogrammability in HIS implies that the HIS
must be able to react at any time to changing require-
ments by adapting HAS functions. The requirements
resulting from new tasks and goals in care of patients.
These are formulated by the healthcare professionals.
New functionality needs to be included, immediately
when it is needed. The implementation of FHIR in
HIS gives this opportunity because it enables third-
parties to connect to well-defined interfaces and to
add functionality through new applications. Further-
more, FHIR supports the migration of HAS to modu-
larized systems and allows the implementation of
technological decoupled services. As an example, an
architecture for pathway-based patient integration
can be named (Benedict et al., 2019). New applica-
tions can be connected to FHIR interfaces and create
unanticipated functionality. This saves costs since the
interfaces are purchased once, but used multiple times
in different ways.
Data homogenization means that the HIS must
support the acquisition of health-related data with a
high degree of reusability and interoperability. For
example, a smartwatch measures the patient’s heart
rate permanently and sends the data via FHIR Obser-
vations to the vital data API of the CDMS. Due to ho-
mogeneity of data, the measurement data can be
transferred from one digital device to another system,
(in this case from the smartwatch to the CDMS). It
can be directly interpreted by the CDMS, because
FHIR ensures the interoperability. At the same time,
the physician is able to examine and integrate the
findings in a case record, including the patient’s heart
rate. He can use different vital data provided by dif-
ferent sensors via FHIR graphically on his tablet pc.
He can mix data of the patient for individual dossiers
and share them with colleagues. For example, he can
retrieve the data via a web-interface created by the in-
formaticians in the hospital’s IT department. This
web-interface also accesses the FHIR interfaces of the
CDMS to gain the relevant observations which result
from the smartwatch.
The Nature of Digital Innovation and What Can Be Learned for Information Systems Management
793

Figure 4: The Course of Digital Innovation since 2010.
Self-reference in the context of HIS means, that
the availability of reusable technology eases the inte-
gration of new DI into the HIS. The availability of
FHIR interfaces eases the integration of new digital
technologies. For example, the integration of legacy
patient sensor systems can be more facilitated by
providing a standard-based vital data FHIR interface
which is originally created to record the heart rate.
The implementation of FHIR in a hospital eases ac-
cess to machine-readable data. The knowledge about
the existence of standardized interface lowers the bar-
riers for investing in interfaces.
4 DISCUSSION
Based on the findings of the literature analysis de-
scribed in the previous chapter, the results obtained
are discussed in more detail below. The explanation
starts with general or methodological aspects, fol-
lowed by a discussion of the quantitative and qualita-
tive results.
Methodological Aspects. The amount of the most
frequently cited publications which were analyzed
(n = 12) in relation to the total number of identified
articles (n = 792) is 1.5 percent. This amount is com-
paratively too low to be able to draw general conclu-
sions about the nature of DI. Nevertheless, the cita-
tion frequency is an appropriate measure to assess the
relevance of scientific contributions. However, by fo-
cusing on the citation frequency, relevant publica-
tions may have been excluded. In order to address this
problem and to expand the database, a search using
backward references was included in the literature
search process. A detailed analysis of the 18 publica-
tions has shown that the majority (65 percent) of all
contributions refer to the contents published by Yoo,
Henfridsson & Lyytinen (2010).
Quantitative Analysis. The number of publications
on DI has been growing steadily since 2010. This can
be explained by the growing pace of digitalization
and by the seminal work of Y
OO
,
H
ENFRIDSSON
&
L
YYTINEN
(2010) that has laid the foundation for re-
search in the field of DI. The number of publica-
tions (n = 202) reached a high level in 2018 and the
trend seems to continue. More than 101 publications
have already been published in the first half of the
year 2019. However, it is possible that some publica-
tions of 2018 and the first half of 2019 were not yet
registered in the databases.
The majority of publications descend from Eu-
rope. One possible explanation for this could be the
fact that two of the three authors of the initial paper
(Henfridsson and Lyytinen) come from Scandinavia.
With their ten respectively four publications on DI,
they have made a significant contribution to the re-
search in this field. Most publications have been pub-
lished in the United States and United Kingdom. This
is probably because papers are usually published in
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
794

the English-speaking field of information systems re-
search and organizational management to be accessi-
ble to a wide audience and there are fewest language
barriers.
The majority of publications are assigned to the
subject area Business, Management and Economics.
Classically, innovations have
1
been the subject of
Business Administration. Depending on the point of
view, Business Administration is understood as Hu-
manities or Social Science and thus explains the high
number of publications in this field. In addition, there
are numerous publications in the field of Computer
Science. This can be explained by the fact that the au-
thors of the fundamental work have an economical
background, but also explore the field of Computer
Science.
2
Qualitative Analysis. The seven identified defini-
tions have in common that digitization respectively
the use of digital technologies or IT are necessary pre-
requisites for the creation of DI. While Yoo et al.
(Yoo, Boland, Lyytinen & Majchrzak, 2012; Yoo,
Henfridsson & Lyytinen, 2010; Yoo, Lyytinen, Bo-
land, Berente, Gaskin, Schutz & Srinivasan, 2010) in-
evitably associate DI with a combination of digital
and physical components, other authors do not em-
phasize the physical aspect in their definition. This is
due to the fact that the authors focus on different top-
ics (e.g. product development, business process opti-
mization, business model creation). In contrast, the
definition of Nambisan & Lyytinen (2017) is open so
that any market offering can be regarded as an inno-
vation. The reason for this is that the authors consider
DI as a variable socio-technical phenomenon and that
this character can only be considered by looking at it
very broadly.
DI is inseparably associated with the innovation
type product innovation because 67 percent (12 out of
18) of the publications refer to Yoo, Henfridsson &
Lyytinen (2010). The authors consider product inno-
vations opposed to process innovations, which have
already been extensively studied in IT research. Ulti-
mately, innovations can arise in the product or service
area. Software application and platform innovations
are examples of subtypes of service innovations. The
evolution from product innovation type to service in-
novation type over time can be explained by the fact
that service enhancements only become relevant once
a product to which the service relates has been devel-
oped. We observed that the understanding of DI as a
1
2
Yoo is a Korean professor of Entrepreneurship and Infor-
mation Systems in Design and Innovation at Weatherhead
School of Management/Case Western Reserve University.
Henfridsson is a Swedish professor at Warwick Business
concept was getting more comprehensive over time.
This can be explained by the ongoing digital transfor-
mation of the economy, which leads to new business
models and a change to service-dominant logics
(Lusch & Nambisan, 2015).
In summary, it can be stated that the characteris-
tics of DI are named differently in almost every pub-
lication. In two publications two characteristics are
proposed, in other publications three or even seven.
Hereby it becomes clear that the categories are some-
times narrower, sometimes broader and often overlap.
Of particular interest is that although two publications
by the same authors were published in 2010, DI char-
acteristics were named differently. The report pub-
lished in January (Yoo, Lyytinen, et al., 2010) distin-
guishes between characteristics of digital technolo-
gies (data homogenization, programmability, self-ref-
erencing), properties of digital materiality and dimen-
sions of DI (convergence, digital materiality, hetero-
geneity, generativity, locus of innovation, pace). The
publication (Yoo, Henfridsson & Lyytinen, 2010) de-
scribes reprogrammability, data homogenization and
self-referencing as key characteristics of DI. In
2012 (Yoo, Boland, Lyytinen & Majchrzak, 2012),
the authors are talking about only two unique charac-
teristics – convergence and generativity. Thus, the use
of terms is not consistent. For example, the separation
of function and form is assigned in (Yoo, Lyytinen,
Boland, Berente, Gaskin, Schutz & Srinivasan, 2010)
to the characteristic digital materiality, in (Yoo, Hen-
fridsson & Lyytinen, 2010) reprogrammability and in
(Yoo, Boland, Lyytinen & Majchrzak, 2012) as gen-
erativity. The two publications from 2017 (Huang,
Henfridsson, Liu & Newell, 2017; Nambisan & Lyyt-
inen, 2017) describe the properties of the characteris-
tics of (Yoo, Henfridsson & Lyytinen, 2010) in other
words and augment them (e.g. malleable, dynamic).
5 CONCLUSIONS
In the last years the understanding of DI has become
more holistic. While the early innovation discussions
focused more on the materiality of DI, the later dis-
cussions investigated networks and logics of innova-
tion. When integrating DI into existing IS, IS manag-
ers need also consider whether their existing subsys-
tems of the IS are “ready for innovation”. Conse-
quently, there is a need to analyze the ability of IS to
School and was once Head of the Information Systems
Group. Kalle Lyytinen is a Finnish professor of Manage-
ment Design and Design and innovation at Weatherhead
School of Management/Case Western Reserve University.
The Nature of Digital Innovation and What Can Be Learned for Information Systems Management
795

both integrate and create DI. This paper contributes
by introducing different fields of DI from which dif-
ferent characteristics for subsystems of IS (e.g. repro-
grammability, data homogenization, self-referencing)
can be derived. These properties may be used to ana-
lyze, evaluate and to re-engineer existing IS. By de-
scribing implications for HIS, the paper shows how
the characteristics of DI can be instantiated in a spe-
cific domain. Since our focus was on the technologi-
cal implications an analysis of organizational impli-
cations for HIS design is outstanding and needs to be
treated in further research.
This paper offers a detailed description of the na-
ture of DI, but also contains limitations that provide
directions for further research. In order to verify and
extend the analysis results, a much larger data basis
should be considered in the following investigation.
In addition, the results of the descriptive analysis of-
fer the potential to find out, through an in-depth in-
ductive analysis, why new definitions and innovation
types have developed and why certain characteristics
emerged or disappeared – even if this is already partly
the case in this paper. An ontology would be an ap-
propriate approach to visualize and clearly distin-
guish the diversity of terminologies used.
ACKNOWLEDGEMENT
This work is part of the ERDF-project “Häusliche Ge-
sundheitsstation” and is funded by the European Un-
ion and the Free State of Saxony.
REFERENCES
Alkraiji, A., Jackson, T., & Murray, I. (2013). Barriers to
the Widespread Adoption of Health Data Standards: An
Exploratory Qualitative Study in Tertiary Healthcare
Organizations in Saudi Arabia. J Med Sys, 37(2), 9895.
Bender, D., & Sartipi, K. (2013). HL7 FHIR: An Agile and
RESTful approach to healthcare information exchange.
Proceedings of the 26th IEEE International Symposium
on Computer-Based Medical Systems, 326–331.
Benedict, M., Schlieter, H., Burwitz, M., Scheplitz, T.,
Susky, M., & Richter, P. (2019). A Reference Architec-
ture Approach for Pathway-Based Patient Integration.
2019 IEEE 23rd International Enterprise Distributed
Object Computing Conference (EDOC), 58–66.
Cooper, H., & Hegdes, L. V. (1994). Research synthesis as
a scientific enterprise.
de Reuver, M., Sørensen, C., & Basole, R. C. (2018). The
Digital Platform: A Research Agenda. Journal of Infor-
mation Technology, 33(2), 124–135.
Fettke, P. (2006). State-of-the-Art des State-of-the-Art.
Wirtschaftsinformatik, 48(4), 257.
Fichman, R. G., Dos Santos, B. L., & Zheng, Z. E. (2014).
Digital Innovation as a Fundamental and Powerful Con-
cept in the Information Systems Curriculum. MIS
Quarterly, 38(2), 329–343.
Haux, R., Winter, A., Ammenwerth, E., & Brigl, B. (2013).
Strategic Information Management in Hospitals: An In-
troduction to Hospital Information Systems. Springer
Science & Business Media.
Hevner, A., vom Brocke, J., & Maedche, A. (2019). Roles
of Digital Innovation in Design Science Research.
Business & Information Systems Engineering, 61(1),
3–8.
Huang, J., Henfridsson, O., Liu, M. J., & Newell, S. (2017).
Growing on Steroids: Rapidly Scaling the User Base of
Digital Ventures Through Digital Innovaton. MIS Q,
41(1), 301–314.
Jung, C., & Padman, R. (2015). Disruptive Digital Innova-
tion in Healthcare Delivery: The Case for Patient Por-
tals and Online Clinical Consultations. In R. Agarwal,
W. Selen, G. Roos, & R. Green (Hrsg.), The Handbook
of Service Innovation (S. 297–318). Springer London.
Khalifa, M., & Alswailem, O. (2015). Hospital Information
Systems (HIS) Acceptance and Satisfaction: A Case
Study of a Tertiary Care Hospital. Procedia Computer
Science, 63, 198–204.
Lluch, M. (2011). Healthcare professionals’ organisational
barriers to health information technologies—A litera-
ture review. Int J Med Inf, 80(12), 849–862.
Lusch, R. F., & Nambisan, S. (2015). Service Innovation:
A Service-Dominant Logic Perspective. MIS Q, 39(1),
155–175.
Moghaddasi, H., Mohammadpour, A., Bouraghi, H., Azizi,
A., & Mazaherilaghab, H. (2018). Hospital Information
Systems: The status and approaches in selected coun-
tries of the Middle East. Electronic Physician, 10(5),
6829–6835.
Moser, H. (2013). Strategisches Projektmanagement im
Gesundheitswesen: Wie Stakeholder auf ein
Sensitivitätsmodell einwirken - eine Analyse. disserta
Verlag.
Nambisan, Satish, Lyytinen, K., Case Western Reserve
University, Majchrzak, A., University of Southern Cal-
ifornia, Song, M., & Xi’an Technological University.
(2017). Digital Innovation Management: Reinventing
Innovation Management Research in a Digital World.
MIS Q, 41(1), 223–238.
Rachinger, M., Rauter, R., Müller, C., Vorraber, W., &
Schirgi, E. (2018). Digitalization and its influence on
business model innovation. Journal of Manufacturing
Technology Management.
Scheplitz, T., Kaczmarek, S., & Benedict, M. (2019). The
Critical Role of Hospital Information Systems in Digi-
tal Health Innovation Projects. 2019 IEEE 21st Confer-
ence on Business Informatics (CBI), 01, 512–521.
Winter, A., Haux, R., Ammenwerth, E., Brigl, B., Hellrung,
N., & Jahn, F. (2011). Health Information Systems: Ar-
chitectures and Strategies. Springer Science & Business
Media.
Scale-IT-up 2020 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
796

Yoo. (2010). Computing in Everyday Life: A Call for Re-
search on Experiential Computing. MIS Q, 34(2), 213.
Yoo, Y., Boland, R. J., Lyytinen, K., & Majchrzak, A.
(2012). Organizing for Innovation in the Digitized
World. Organization Science, 23(5), 1398–1408.
Yoo, Y., Henfridsson, O., & Lyytinen, K. (2010). The New
Organizing Logic of Digital Innovation: An Agenda for
Information Systems Research. ISR, 21(4), 724–735.
Yoo, Y., Lyytinen, K., Boland, R. J., Berente, N., Gaskin,
J., Schutz, D., & Srinivasan, N. (2010). The Next Wave
of Digital Innovation: Opportunities and Challenges: A
Report on the Research Workshop „Digital Challenges
in Innovation Research“.
The Nature of Digital Innovation and What Can Be Learned for Information Systems Management
797
