
Model of Trauma Healing Policy for Mitigation Communities in the
COVID-19 Pandemic Period in Padang Pariaman District - Indonesia
Aulia Asman
1,*
a
, Rina Alfina
2
b
and Auzia Asman
2
c
1
Departement of Diploma III Nursing, Universitas Negeri Padang, Indonesia
2
Departement of Food Crops, Politeknik Pertanian Negeri Payakumbuh, Indonesia
Keywords: COVID-19, Policy Model, Trauma Healing.
Abstract: Padang Pariaman Regency is one of the top 5 largest COVID-19 cases in West Sumatra. Coronavirus Disease
2019 or COVID-19 is a disease caused by the corona virus with the fastest spread in the time and way, so that
it becomes a pandemic in the world, including in Indonesia and West Sumatra. -existing psychological
problems and secondary traumatic stress (STS), so this study aims to develop a trauma healing policy model
for the community during the COVID-19 pandemic in Padang Pariaman Regency so that the community
adapts and mitigates this pandemic. This research is a quantitative descriptive study, using in-depth interview
data collection techniques to expert respondents whose results were analyzed using the Analytical Hierarchy
Process. In formulating the policy model, stigma or point of view, mental or mental health and behavior are
used as policy criteria. The results of the study indicate that the priority policies to be considered for the
Padang Pariaman Regency Government are: (1) Promoting and socializing the prevention of COVID-19
transmission directly or online to the community, then getting people used to implementing it in daily life by
applying various rules in the community. public environment (84.9%); (2) Conduct socialization and increase
public knowledge and awareness about COVID-19, its transmission and prevention, so that the negative
stigma of the community can change and become support for positive sufferers (75.4%); (3) Increasing
vertical and horizontal cooperation from the community to the government (73.5%); and (4) Improving the
adaptation and recovery of COVID-19 through re-centering, personal awakening, emotion stabilizing, and the
implementation of the buddy system (64.3%).
1 INTRODUCTION
The COVID-19 virus or Coronavirus Disease 2019
became a disease with human-to-human transmission
in the fastest time and way, so it was declared a world
pandemic by WHO (Bender, 2020). The COVID-19
virus originated from Whuhan City, China (WHO,
2020), which finally arrived in Indonesia due to
Indonesia's geographical location which is directly
adjacent to several countries affected by the spread of
the COVID-19 virus, the development of
globalization and the increasingly smooth traffic
between countries. Indonesia is one of many
countries that are facing a non-natural disaster,
namely the COVID-19 virus pandemic.
a
https://orcid.org/0000-0001-5837-9306
b
https://orcid.org/0000-0002-2220-7630
c
https://orcid.org/0000-0002-2820-0675
Indonesia, from the beginning of the case on
March 2, 2020 to May 20, 2020, has reached 19,189
people with 4,575 recoveries and 1,242 people who
died from the site https://covid19.go.id (Asman et al.,
2020). The speed of the spread of this virus is due to
the fact that transmission can occur only by touching
a contaminated surface or object, which then
knowingly or not touches the eyes, nose or mouth
(Steffens, 2020). The large number of cases of
COVID-19 from time to time, one of which is
because a vaccine for a cure has not yet been found,
so the government can only carry out treatment and
care with symptoms that are still early as well as
control and prevent the spread of virus transmission
(Yi et al., 2020) .
Asman, A., Alfina, R. and Asman, A.
Model of Trauma Healing Policy for Mitigation Communities in the COVID-19 Pandemic Period in Padang Pariaman District - Indonesia.
DOI: 10.5220/0011094600003368
In Proceedings of the International Conference of Mental Health (Icometh 2021), pages 33-38
ISBN: 978-989-758-586-9
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
33

This COVID-19 has spread to all provinces in
Indonesia, where of 34 provinces, West Sumatra
Province which is located in the west of Sumatra
Island which consists of 19 regencies/cities is the
province with the most positive cases of COVID-19,
namely 428 people or 2, 2% or in position 9. The
results from West Sumatra's corona response on May
20, 2020 from the website
https://corona.sumbarprov.go.id/details/peta_covid1
9 it is Including the top 5 highest cases, Padang
Pariaman Regency can be caused because Padang
Pariaman Regency, which is a regency with a large
area, close to the provincial capital, namely Padang
City, is a crossing point for migrants who will go to
other districts/cities in West Sumatra Province
(Asman et al., 2020). In addition, the transmission
and spread of COVID-19 in Padang Pariaman
Regency tends to be local transmission or
transmission that occurs locally, with the center of the
spread being at several points such as the markets of
each Nagari in Padang Pariaman Regency, the border
with the City of Padang, Bukittingi and Pasaman. ,
and hospitals. Pariaman Padang.
During the current COVID-19 outbreak, with the
enactment of PSBB in almost all of Indonesia
including the Padang Pariaman Regency, people are
required to stay at home and go out only to fulfill
mandatory or daily needs. The enactment of this
PSBB has caused many people to lose their jobs due
to staff reductions, loss of livelihoods, and health
workers who cannot meet their families as well as
large work demands such as working longer hours or
40 hours a week and with a continuous work schedule
compared to normal working hours (Hua & Shaw,
2020). The obligation to stay at home and do physical
distancing, over time makes people who do not have
activities or busy at home experience stress, which
will have an impact on their mental well-being and
health, such as depression, excessive fatigue and
anxiety (Kim & Knesebeck, 2015). This is
exacerbated by the amount of social stigma and
discriminatory behavior towards patients who are
positive for COVID-19 or their families or
communities who come into contact with positive
patients (Pfefferbaum & North, 2020), which then has
an impact on exclusion and cynical or negative views
(ILO, 2020).
These conditions cause people to panic and if they
last for a long time can cause people to experience
psychological problems such as stress and trauma.
Each individual who experiences stress and trauma
has a different response from each other in terms of
intensity and expression, depending on the windows
of tolerance. Windows of tolerance is the extent or
narrowness of an individual's tolerance level when
dealing with stressful or traumatic situations (Dewi,
2020). Dewi also explained that if this window of
tolerance does not work, stress and trauma will
reappear, causing pre-existing psychological
problems such as psychosomatic, depression and
anxiety disorders, post-traumatic stress disorder
(PTSD), obsessive-compulsive disorder (OCD),
interpersonal conflict (attachment issue), self-esteem
issue, chronic emotional problems, aggressiveness
relapse (dropping treatment & care), and family and
marriage problems (Dewi, 2020). There needs to be
the right strategy so that it doesn't increase again in
the number of positive COVID-19 (Asman et al.,
2021).
In addition to experiencing pre-existing
psychological problems, people, especially those
with the highest risk of exposure, can also experience
secondary traumatic stress (STS), such as excessive
worrying and fear of something bad happening, being
easily surprised or alert all the time, experiencing
physical stress (eg: palpitations, cold sweats),
nightmares or recurring thoughts about the traumatic
event, and a feeling that someone else's trauma is his
or her own. This stress and trauma, apart from
occurring in patients with COVID-19 and patients
with ODP and PDP status, also often occurs in health
workers. The impact of COVID-19 showed a high
level of distress (72%), with very high rates of
depression (50%), anxiety (45%) and insomnia
(34%), where symptoms were more severe. arise in
those with prolonged contact with the patient (Muhdi,
2020).
These pre-existing psychological problems and
Secondary Traumatic Stress (STS) can be minimized
by doing trauma healing for vulnerable groups and
groups who really need it. However, until now the
government has not issued a policy regarding trauma
healing which is very much needed for positive
COVID-19 patients, ODP, PDP and health workers in
particular and for the community in general.
Therefore, in this study, the formulation of a trauma
healing policy model for the community in Padang
Pariaman Regency was carried out.
2 RESEARCH METHODS
This research is a quantitative descriptive study, using
interview data collection techniques to expert
respondents to obtain the most prioritized policies in
trauma healing. According to Saaty (1991) and Saaty
(2008) furthermore, using a pairwise comparison
questionnaire between elements at each level to
Icometh 2021 - International Conference of Mental Health
34

obtain a hierarchical structure, which was processed
with Criterium Decision Plus 4.0 software, and
analyzed using the Analytical Hierarchy Process
(AHP) method. According to Marimin (2004) and
Latifah (2005) the working principle of AHP consists
of hierarchical arrangement (decomposition),
assessment of criteria and alternatives (comparative
judgment), prioritization (synthesis of priority), and
logical consistency (local consistency). The basic
concept of the AHP is the use of a pairwise
comparison matrix (matrix of pairwise comparisons)
to generate relative weight values between criteria
and alternatives. A criterion is compared to another in
terms of how important it is to the achievement of the
above objectives (Saaty, 1991)
3 RESEARCH AND
DISCUSSIONS
Padang Pariaman Regency is one of the regencies that
has the 5 highest number of COVID-19 cases on the
island of Sumatra. Of all community activities in
Padang Pariaman Regency, transmission of COVID-
19 will pose a higher risk to people who work on the
front lines, such as health care workers, and in
particular those who are actively involved in handling
the outbreak (first responder from the emergency
medical team, health care workers in emergency
departments and special care units, transportation and
first aid), psychiatrists for providing the services
needed by patients experiencing psychological stress,
fatigue, and negative stigma; sellers of basic
necessities such as in traditional and modern markets;
and workers in the transportation sector such as
online transportation and public transportation.
The extent and high risk of transmission of the
virus, makes the government must implement PSBB
rules to break the chain of transmission. However,
from March to May 2020, the number of patients
affected by COVID-19 continued to increase. This
means that there have been no significant changes due
to the enactment of the PSBB. This can be caused by
the mental weakness of the community in
implementing the PSBB and dealing with the
COVID-19 virus. Therefore, a policy model
regarding trauma healing or trauma recovery that can
be implemented by the Padang Pariaman Regency
government has been formulated to improve mental
health and windows of tolerance for every Covid-19
positive patient, health worker, and the general
public.
In the formulation of this trauma healing
policy model, three criteria were used, namely the
point of view or stigma, mental or mental health, and
behavior. This means that the policies formulated
focus on changing the stigma circulating in the
community regarding COVID-19 and its sufferers,
improving the mental or mental health of positive
patients and the general public in dealing with
COVID-19, and getting used to people's behavior to
be able to live clean and healthy in order to avoid
COVID -19. From these criteria, 9 alternative policies
are produced that can be implemented by the
government which in the implementation will pay
attention to policy priorities. The alternative policies
are as follows:
1. Application of relaxation and therapy methods as
a way to restore mental or mental health.
2. Prioritizing and implementing Occupational
Safety and Health (K3), especially for people who
have the potential to have a high risk of
transmitting COVID-19.
3. Increase positive activities and limit information
containing negative news, especially for patients
with COVID-19 and people who are at the
forefront.
4. Activate and socialize to the public regarding self-
checking services for psychological problems and
telemedicine regarding online drug consultation
services.
5. Improve communication and good cooperation
between family members, including the
application of appreciative parenting.
6. Increase cooperation vertically and horizontally
from the community to the government.
7. Conduct socialization and increase public
knowledge and awareness about COVID-19, its
transmission and prevention, so that the negative
stigma of society can change and become support
for positive sufferers.
8. Improving adaptation and recovery of COVID-19
through re-centering (building each individual's
internal system), personal awakening (rising up
and then adjusting life patterns), emotion
stabilizing (increasing sense of control), and
implementing the buddy system (colleague
system).
9. Promote and socialize the prevention of COVID-
19 transmission directly and online to the
community, then familiarize the community with
applying it in daily life by applying various rules
in the public environment
The criteria and policy alternatives, using
CDP (Criteria Decision Plus) software produce a
policy hierarchy as shown in Figure 1. The policy
Model of Trauma Healing Policy for Mitigation Communities in the COVID-19 Pandemic Period in Padang Pariaman District - Indonesia
35
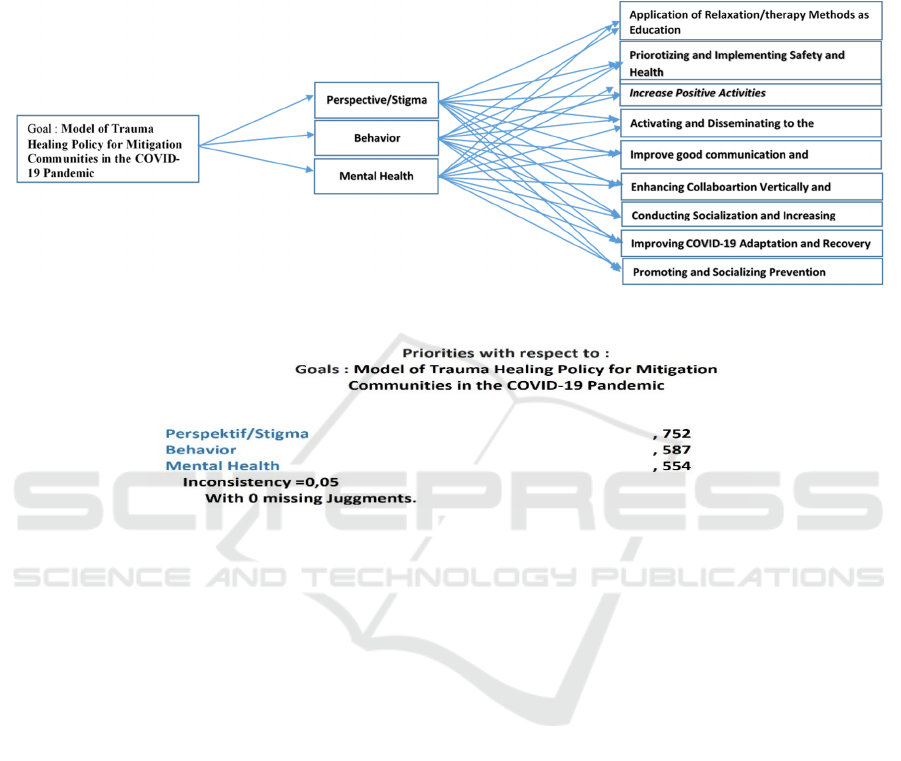
hierarchy shows that in the formulation of the policy
model, the criteria will be interrelated with all policy
alternatives. Furthermore, the consistency ratio value
resulting from the analysis of the pairwise
comparison matrix (paired comparison matrix) is
0.055 or less than 0.1. This means that in compiling a
pairwise comparison matrix, expert respondents or
experts are consistent so that policy priorities can be
determined.
Figure 1: Hierarchy of the Trauma Healing Policy Model.
Figure 2: Consistency Ratio.
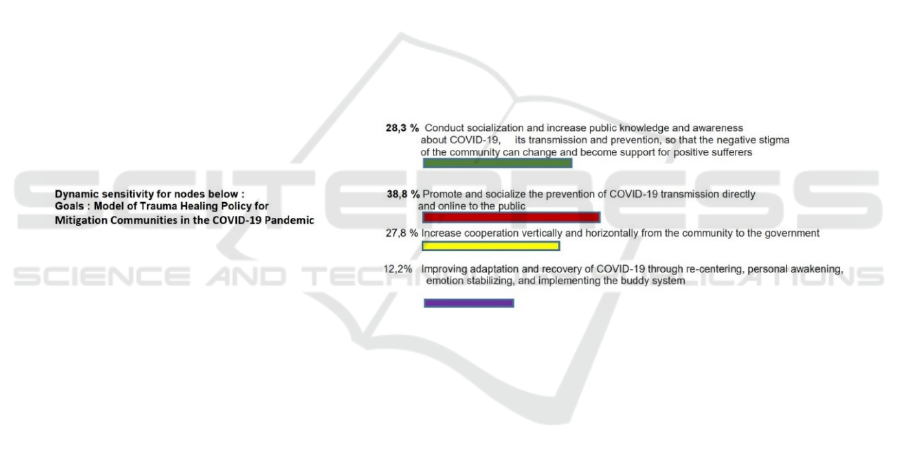
Figure 3 shows that there are 4 policy priorities in
formulating a trauma healing policy model in Padang
Pariaman Regency, which can be applied with the
following strategies:
1. Promote and socialize the prevention of COVID-
19 transmission directly and online to the
community, then familiarize the community with
applying it in daily life by applying various rules
in the public environment
a. Improve communication and openness of health
in the family.
b. Be transparent to the surrounding community.
c. Local governments with Nagari leaders, Korong
leaders, religious leaders or traditional leaders or
community leaders carry out promotions both
directly and online.
d. Involving radio broadcasts and print media in the
promotion of transmission prevention.
e. The teacher always informs the students to get
used to living a healthy and clean life.
f. The government has begun to implement health
protocols in all work and public environments.
2. Conduct socialization and increase public
knowledge and awareness about COVID-19, its
transmission and prevention, so that the negative
stigma of the community can change and become
support for positive sufferers.
a. The government conducts socialization in stages
to save financing.
b. Evaluating the results of socialization on a regular
and consistent basis.
c. Follow up on the evaluation results.
d. Communicate actively with Nagari leaders,
Korong leaders, religious leaders or traditional
leaders or community leaders to be able to convey
information and convince and increase public
awareness so that they no longer have negative
stigma.
e. Spreading facts both online and in person
regarding the transmission and prevention of
COVID-19.
f. Amplifying the voices of people recovering from
COVID-19.
g. Equalize perceptions about COVID-19 so that if
there are positive citizens, they can be given
support.
3. Increase cooperation vertically and horizontally
from the community to the government.
Icometh 2021 - International Conference of Mental Health
36
a. Avoiding miscommunication between the Padang
Pariaman Regency government and the
community.
b. Making Nagari leaders, Korong leaders, religious
leaders or traditional leaders or community
leaders a source of information about COVID-19.
c. Provide support and assistance for residents who
are positive for COVID -19 or self-isolating or
affected by COVID-19 using a local economy-
based approach/ assisting in providing basic
needs.
d. Active involvement of the local community/
Nagari-Korong in supporting the process of
implementing self-quarantine/ isolation by
providing a place for migrants.
e. Forming a task force unit with the aim of
monitoring residents who are either self-isolating
or affected.
4. Improving adaptation and recovery of COVID-19
through re-centering (building an individual's
internal system), personal awakening (rising up
and then adjusting life patterns), emotion
stabilizing (increasing sense of control), and
implementing the buddy system (a coworker
system).
a. Improving the quality of each individual's faith by
worshiping.
b. Build emotional stability by always thinking
positively.
c. the head of the Nagari, Korong, religious or
traditional leaders or community leaders always
urge and invite the community to behave in a
healthy life and exercise.
d. Keeping pet animals for mind distraction.
e. Increase awareness among individuals in the
family, in the neighborhood, workplace and
public places by reminding each other not to
forget the health protocol.
f. Especially for the front row, the government must
pay attention to mental/mental health conditions
by increasing immunity, monitoring mental/
mental health.
Regularly, providing a psychiatrist, setting up
facilities that make them more confident,
comfortable, and stay positive.
Figure 3: Priority Model of Trauma Healing Policy.
Thus, the trauma healing policy model for the
community in Padang Pariaman Regency during the
COVID-19 pandemic can be done by eliminating the
community's negative point of view or stigma first
against positive patients or people who make contact
so that isolation is necessary. This is in accordance
with (Asman et al., 2020) WHO stated that negative
stigma must be annulled with optimal health literacy
from various parties because COVID-19 sufferers are
not people who commit disgraceful acts, so there is
no need to be isolated or shunned. If this stigma is
allowed, it can: 1) encourage people to hide their
illness to avoid discrimination, 2) prevent people
from seeking immediate health care, and 3) prevent
them from adopting healthy behaviors.
Furthermore, trauma recovery will be easier to
overcome if the community has a healthy mental or
spirit. In improving this mental or mental health, it is
very necessary to support the family and the
surrounding environment. Communication is the key
to the success of this mental or mental health, so that
individuals can have good windows of tolerance in
dealing with stress or trauma. Then, trauma and stress
in the community in Padang Pariaman Regency can
also be overcome by changing people's behavior who
have started to get used to maintaining cleanliness
and healthy living, so that indirectly also apply
positive thinking, always be enthusiastic and get used
to being open and transparent about the conditions
experienced. The policy with the above
implementation strategy can be carried out by the
Padang Pariaman Regency government in
collaboration with the community.
4 CONCLUSIONS
Padang Pariaman Regency is one of the regencies on
the island of Sumatra that has the highest 5 major
Model of Trauma Healing Policy for Mitigation Communities in the COVID-19 Pandemic Period in Padang Pariaman District - Indonesia
37

COVID-19 cases. This condition makes the
government issue a policy for implementing PSBB
(Large-Scale Social Restrictions) by requiring people
to only carry out activities at home. As a result, many
people have lost their jobs due to staff reductions, lost
their livelihoods, health workers are unable to meet
their families and high work demands, people who are
at home also experience conditions of boredom,
boredom and stress. This condition, if left unchecked
for a long time can cause pre-existing psychological
problems and secondary traumatic stress (STS), so a
policy is needed to recover the trauma and stress.
Policy priorities to be able to recover community
stress and stress that can be taken into consideration
for the Padang Pariaman Regency government are (1)
Promoting and socializing the prevention of COVID-
19 transmission directly or online to the community,
then getting people used to applying it in daily life by
applying various rules. in the public environment
(84.9%); (2) Conduct socialization and increase
public knowledge and awareness about COVID-19,
its transmission and prevention, so that the negative
stigma of the community can change and become
support for positive sufferers (75.4%); (3) Increasing
vertical and horizontal cooperation from the
community to the government (73.5%); and (4)
Improving the adaptation and recovery of COVID-19
through re-centering, personal awakening, emotion
stabilizing, and the implementation of the buddy
system (64.3%).
REFERENCES
Asman, A., Asman, A., & Dewi, A. K. (2021). Community
Nursing Strategies for Tourism Health Families during
COVID-19 Pandemic. International Journal of Health
Sciences, 5(3), 224–231.
https://doi.org/10.53730/ijhs.v5n3.1449
Asman, A., Barlian, E., Fatimah, S., Dewata, I., & Asman,
A. (2020). Model of Trauma Healing Policy for
Communities in the COVID-19 Pandemic Period in
Padang City – Indonesia. Journal of Advanced
Research in Dynamical and Control Systems, 12(7),
646–651.
Bender, L. (2020). Pesan dan Kegiatan Utama Pencegahan
dan Pengendalian COVID-19 di Sekolah.
www.who.int. https://www.who.int/docs/default-
source/searo/indonesia/covid19/pesan-dan-kegiatan -
utama-pencegahan-dan-pengendalian-covid-19-di-
sekolah---indonesian--march-2020.pdf
Dewi, L. Z. (2020). Masa Darurat COVID 19 & Kesehatan
Jiwa. PPH ATMADJAYA.
Hua, J., & Shaw, R. (2020). Corona Virus (COVID-19)
“Infodemic” and Emerging Issues through a Data Lens:
The Case of China. International Journal of
Environmental Research and Public Health, 17(7), 1–
12.
ILO. (2020). Dalam Menghadapi Pandemi: Memastikan
Keselamatan dan Kesehatan di Tempat Kerja.
wwwl.ilo.org.
Kim, T. J., & Knesebeck, O. Von Dem. (2015). Is An
Insecure Job Better for Health Than Having No Job At
All? A Systematic Review of Studies Investigating The
Health-Related Risks of Both Job Insecurity and
Unemployment. BMC Public Health, 15(985), 1–9.
Latifah, S. (2005). Prinsip-Prinsip Dasar Analytical
Hierarchy Process. Repositori Institusi Universitas
Sumatera Utara.
Marimin. (2004). Teknik dan Aplikasi Pengambilan
Keputusan Kriteria Majemuk. Jakarta: Grasindo.
Muhdi, N. (2020). Layanan Konseling Tenaga Kesehatan
Era Pandemi COVID-19: Peluang dan Tantangan.
www.persi.or.id.
Pfefferbaum, B., & North, C. S. (2020). Mental Health and
The Covid-19 Pandemic. New England Journal of
Medicine, 383(6), 510–512.
Saaty, T. L. (1991). Pengambilan Keputusan Bagi Para
Pemimpin. Jakarta: Pustaka Binaman Pressindo.
Saaty, T. L. (2008). Decision Making with The Analytic
Hierarchy Process. Int. J. Services Sciences, 1(1), 83–
98.
Steffens, I. (2020). A Hundred Days Into the Coronavirus
Disease (COV ID-19) Pandemic. Euro Surveil, 25(14),
1–4.
WHO. (2020). Stigma Sosial terkait dengan COVID-19.
www.who.int. https://www.who.int/docs/default-so
urce/searo/indonesia/covid19/panduan-untuk-mence
gah-dan-mengatasi-stigmasosial.pdf?sfvrsn=4f8bc7
34_2
Yi, Y., Lagniton, P. N. P., Ye, S., Li, E., & Xu, R. H. (2020).
COVID-19: What Has Been Learned and To Be
Learned About The Novel Coronavirus Disease.
International Journal of Biological Sciences, 16(10),
1753–1766.
Icometh 2021 - International Conference of Mental Health
38
