
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive
and Immersive Scenarios
Vanesa Herrera
1 a
, Ana Reyes-Guzm
´
an
2 b
, David Vallejo
1 c
, Jos
´
e Castro-Schez
1 d
,
Dorothy N. Monekosso
3 e
, Gonz
´
alez-Morcillo Carlos
1 f
and Javier Albusac
1 g
1
School of Computer Science, University of Castilla-La Mancha, Ciudad Real, Spain
2
Hospital Nacional de Parapl
´
ejicos de Toledo, Toledo, Spain
3
Department of Computer Science, University of Durham, Durham, County Durham, U.K.
Keywords:
Virtual Reality, Immersive Environments, Upper Limb Rehabilitation, Hand Tracking, Free-Hand Interaction.
Abstract:
In recent years, new technologies have contributed to an improvement in the upper limb rehabilitation pro-
cess as a complement to the conventional therapy received by patients. In this context, technologies should
facilitate accurate monitoring of the hands and serve to collect data on patient performance during functional
tasks in order to objectively assess the patient’s potential evolution. Mechanical and wearable devices provide
greater accuracy in measurements. However, the physical limitations of patients requires the use of hands-free
solutions. This article investigates controller-free hand technologies for accurate hand tracking in the Box and
Block test (BBT) benchmarked against the real test, validated and standardized in the context of the Hospital
Nacional de Parapl
´
ejicos (Toledo, Spain). In particular, the performance in the execution of therapeutic ex-
ercises is analyzed in three different scenarios: i) physical environment without the use of technologies, ii)
non-immersive virtual environment and, finally, iii) fully immersive virtual environment. The results demon-
strate the similarity between therapies developed in physical scenarios without the use of technologies, and
those carried out in virtual reality-based scenarios.
1 INTRODUCTION
The interdisciplinary use of new technologies has fa-
vored their expansion into areas not originally de-
signed for. Robotics as an aid to physical movement
(Mekki et al., 2018), robots that interact with the pa-
tient, wearable devices (Bravo and Mu
˜
noz, 2022), se-
rious games (Pereira et al., 2020), and even the com-
bination of several of them (Guill
´
en-Climent et al.,
2021) has become an increasingly widespread prac-
tice to help improve patients with different physical
or psychological pathologies. A clear example is the
case of video games and virtual reality, whose pur-
pose originally intended for entertainment, has re-
a
https://orcid.org/0000-0002-6187-4794
b
https://orcid.org/0000-0003-2905-2405
c
https://orcid.org/0000-0002-6001-7192
d
https://orcid.org/0000-0002-0201-7653
e
https://orcid.org/0000-0001-7322-5911
f
https://orcid.org/0000-0002-8568-9542
g
https://orcid.org/0000-0003-1889-3065
sulted in great interest in fields such as education,
health, or digital marketing. In particular, the use
of virtual reality in medicine and rehabilitation is
increasingly employed in hospitals and other health
centers. One main reason is the results obtained
through non-immersive, semi-immersive, and immer-
sive applications in patients affected by a wide range
of problems: neurological problems (Lamash et al.,
2017), eating disorders (Clus et al., 2018), phobias,
or spinal cord injuries (de Ara
´
ujo et al., 2019), among
others. It is the case of the Hospital Nacional de
Parapl
´
ejicos de Toledo (Spain)
1
, a center specializing
in patients with spinal cord injuries. The hospital em-
ploys an interdisciplinary team to evaluate, analyze,
intervene, and guide the patient to achieve the highest
degree of recovery and independence.
Spinal cord injury (SCI) affects conduction of sen-
sory and motor signals across the site(s) of lesion(s),
as well as the autonomic nervous system (Rupp et al.,
2021). This type of injury can be caused by trauma or
1
https://hnparaplejicos.sanidad.castillalamancha.es/
Herrera, V., Reyes-Guzmán, A., Vallejo, D., Castro-Schez, J., Monekosso, D., González-Morcillo, C. and Albusac, J.
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive and Immersive Scenarios.
DOI: 10.5220/0011711800003467
In Proceedings of the 25th International Conference on Enterprise Information Systems (ICEIS 2023) - Volume 2, pages 231-242
ISBN: 978-989-758-648-4; ISSN: 2184-4992
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
231

medical conditions such as degenerative diseases, tu-
mors, or infections. The incidence rate of SCI patients
has been increasing and ranges from 13,019 per mil-
lion to 163,420 per million people worldwide (Kang
et al., 2017). Most patients with SCI have impaired
function of the upper limbs (Wyndaele and Wyndaele,
2006). In this context, one of the most common con-
sequences after injury is loss of muscle strength and
numbness, increased muscle tone (spasticity) (Hod-
kin et al., 2018), weakness or paralysis. Thus, reha-
bilitation is essential to improve muscle strength and
hand/arm function in both early and chronic stages.
Rehabilitation aims to improve the patient’s quality
of life so that he or she can perform activities of daily
living autonomously or at least achieve the highest de-
gree of autonomy possible (Spooren et al., 2011).
Specifically, occupational therapy focuses on the
patient’s ability to cope with most everyday tasks.
A team of functional rehabilitation specialist, phys-
iotherapists, and other specialists plan treatment tai-
lored to the needs of each patient. Rehabilitation be-
gins at an early stage and can last for life, so it is
important to maintain the patient’s motivation and in-
volvement. The repetition of inadequate movements
has a negative impact on recovery, and it is necessary
to prevent the patient from performing compensatory
movements with other parts of the body. Furthermore,
the repetition of compensatory movements prevents
strengthening the area to be treated.
In accordance with the above problems, new tech-
nologies can help capture each patient’s kinematics
with the dual objective measuring movements and
evaluation of the execution of each exercise. There
are different alternatives for motion capture: 2D or 3D
cameras, magnetic sensors, mechanical skeletons, and
inertial sensors, among others. Some systems provide
complete solutions, such as virtual reality headsets.
They are Head Mounted Display (HMD) combined
with IMUs (Inertial Mesure Unit) that allow the user
to immerse in virtual worlds and interact with the el-
ements of the 3D environment. Some of the best-
known are Oculus Go, Oculus Rift, Oculus Quest,
Oculus Quest 2, HTC Vive Focus, HTC Vive Pro 2,
HTC Vive Focus 3, among others. In this type of de-
vice, the main form of interaction is via controllers.
However, some of these HMDs, thanks to the cam-
eras and sensors they integrate, are beginning to pro-
vide libraries that allow the development of applica-
tions. The main form of interaction is made through
the movement and gestures of the hands. This is the
case of Meta Quest 2 VR headset.
However, not all VR-based technologies are suit-
able for use in this type of patient. The use of ele-
ments such as controllers limits the functional move-
ments and grasps that can be performed by humans
(Everard et al., 2022). In addition, virtual appli-
cations with controllers cannot be used by a large
number of patients with SCI with affecting the upper
limbs. These patients generally, do not have sufficient
strength or mobility. Also the use of controllers do not
allow the natural movements and grasps of the hand
to be performed freely. These movements include:
flexion-extension of the wrist, flexion-extension of the
index finger, gripping ability, hand and arm move-
ments and end-terminal pinches.
There are different tests to assess the grasp func-
tion of the hand. In rehabilitation and occupational
therapy, the Box and Block test (BBT) is widely used
because it allows unilaterally measuring the degree of
manual dexterity (Oliveira et al., 2016).
This article uses the BBT in three different sce-
narios. First, a physical scenario without the use
of technologies. Secondly, a non-immersive virtual
environment in which the Leap Motion Controller
(LMC) sensor is used for hand tracking and a screen
to display hands and objects virtually. Finally, the
last scenario is fully immersive and uses the Oculus
Quest 2. Virtual reality scenarios are tested by thera-
pists and clinical staff in charge of rehabilitation ses-
sions for patients with spinal cord injuries affecting
the upper limbs. These tests are carried out thanks
to the joint development with the Hospital Nacional
de Parapl
´
ejicos de Toledo in Spain. The study de-
scribed in this article stands out from others because
the comparison between the different environments
(real, non-immersive and immersive) is performed
with the same parameters and sample. In both virtual
environments, the interaction is executed with one’s
own hands, ruling out possible biases introduced by
the use of controllers or other devices. In addition, al-
though the objective of the test is to count the number
of blocks moved correctly, certain variables of inter-
est have been included for further study. On the other
hand, unlike other implementations, immersive VR-
BBT is performed using hand tracking provided by
the virtual reality device itself, thus achieving a more
realistic immersion.
The rest of the article is structured as follows. Sec-
tion 2 sets the context of the problem. Section 3
presents different scenarios and immersive and non-
immersive methods employed to support upper limb
rehabilitation. Section 4 describes the clinical study
and the results obtained. Finally, the article ends with
Section 5 where the conclusions are presented.
ICEIS 2023 - 25th International Conference on Enterprise Information Systems
232

2 PROBLEM CONTEXT
2.1 Upper Limb Rehabilitation and
Occupational Therapy
Occupational therapy plays a significant role in the re-
habilitation of patients with spinal cord injuries. Ther-
apists assess the most appropriate treatment according
to each individual’s needs and functional goals. The
therapy aims to achieve as much independence as pos-
sible for the patient in daily living activities like eat-
ing, turning lights on and off, dressing, or writing.
The recovery process of patients with SCI is
linked to early mobilization and a multidisciplinary
approach. To achieve improved and optimized long-
term outcomes, it is necessary to involve experts in
nutrition and physical and occupational therapists.
Hence the importance of having an interdisciplinary
team from the beginning of rehabilitation in the hos-
pital.
2.2 Upper Limb Exercises
One of the types of exercises used in upper limb re-
habilitation focuses on improving manipulative skills.
The aim is to achieve the highest possible degree of
hand functionality. In its execution, the hand(s) to be
rehabilitated must be able to grasp and manipulate ob-
jects of different sizes.
Based on the above, there are different classifica-
tions of the movements and grasps required for the
hand to be functional. One such grasp is described by
(Vergara et al., 2014). The classification is based on
the common grasps used by adults during the perfor-
mance of activities of daily living: cylindrical grasp
(the palm is involved and the thumb is in abduc-
tion or neutral), oblique palmar grasp (the thumb is
adducted), hook grasp (palm and thumb are not in-
volved), lumbrical grasp (thumb and proximal part
of the fingers), intermediate power-precision grasp,
pinch (thumb and fingertips), lateral pinch (lateral
part of fingers and usually the thumb), special pinch
and non-prehensile grasp (without grasping).
Another type of grasp that is widely used in pa-
tients with tetraplegia is the so-called tenodesis grasp.
This is made by actively extending the wrist, and then
the passive tension of the flexor muscles puts them
under tension, generating a grip between the thumb
and fingers (Jung et al., 2018).
Patients with SCI often need external aids to hold
certain objects, such as a toothbrush or cutlery. In
addition, the supervision by a specialist is essential
when performing the exercises. Incorrect execution
can lead to non-optimal rehabilitation and even to
other secondary problems. These characteristics and
limitations must be taken into account in the develop-
ment of VR applications for rehabilitation.
3 REHABILITATION THROUGH
VIRTUAL REALITY THERAPY
Virtual reality is an emerging tool that is becom-
ing increasingly widespread in the field of rehabil-
itation. Studies corroborate the positive effects of
this technology in patients with different types of dis-
eases. Due to the diversity of existing pathologies
and the goals to be achieved, it is difficult to unify
the benefits of virtual reality rehabilitation, although
it is worth highlighting the following: improvement
in motor functions and quality of life (Toldo et al.,
2021), cognitive functions (Maggio et al., 2018), mus-
cle strength (Lee et al., 2016) and increased motiva-
tion (Dias et al., 2019).
Depending on the part of the body to be reha-
bilitated, the devices and virtual environments must
comply with some characteristics. In the case of up-
per limb rehabilitation, it is essential that the user can
move his/her hands freely. Virtual applications that
need controllers to interact with virtual elements do
not simulate natural grasping. Thus, it is necessary to
rely on an efficient hand tracking system from which
it is possible to obtain:
• The position of the hand and fingers in 3D space
with the least possible error.
• The interaction of the hand on the virtual objects
in the environment.
• An objective measurement of the degree of mobil-
ity and achievements of the patient.
In order to meet these needs, the following issues
must be resolved: the first is the modeling of the dif-
ferent grasp types and their recognition by the system.
The second is the grab, displacement and release of
the virtual objects. And last, the objective measure-
ment of the results using a standardized test such as
the BBT.
3.1 Modeling Grasp Types
As described in the previous section, various func-
tional grasp allow humans to grasp and move virtual
objects. In the case of virtual reality, this problem is
solved by using a virtual 3D hand that internally relies
on an associated bones and joints (see Figure 1), sim-
ilar to that of a human. In this way, the type of grasp
can be recognized according to the direction vector of
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive and Immersive Scenarios
233

Figure 1: Virtual hand in immersive environment with as-
sociated skeleton for accurate finger position detection.
the bones, position and rotation of the individual fin-
gers in relation to each other or in relation to the palm
of the hand.
In addition to pose recognition, it is also impor-
tant to detect the level of effort. The effort of each
patient can be key in determining when an object is
considered to be attached to a virtual hand. Effort can
be defined as the distance between two or more bones
involved in the grasp. Above a certain threshold, con-
tact is considered to exist between two or more fingers
or between the fingers and palm. On the other hand,
below a certain threshold, it is considered that they is
no contact at all. In the case of grasping a given ob-
ject, it is necessary to take into account both the con-
tact distance between fingers (or fingers and palm of
the hand) and the distance between the hand and the
object. If a grasp pose is recognized but the object is
not within reach, then the grasp will not be executed.
In the case of non-prehensil movements used to
lift an object, it is necessary to know the orientation
of the hand, as it must be placed with the palm facing
the ground.
3.2 Holding of Virtual Objects
In order to simulate, in a virtual environment, the hu-
man ability to grasp and release objects, it is neces-
sary to evaluate the shape and position of the object
in relation to the hand with which it interacts within
the 3D environment.
First of all, the interactive elements of the scene
must be defined along with the kind of interaction.
For this, the physical properties of the object, its
weight or gravity, the collision area of the object and
the state of the object from the interaction point of
view must be specified. The states related to the inter-
action are as follows: non-selectable (it is away from
the hand), selectable (the hand can interact with it),
grabbed (it is attached to the hand and follows the
movements of the hand) and released (it will be sub-
ject once more to the established physical principles).
In order to recognize the different types of grasps with
respect to the object, the collision area of the object
has to be considered. This area can be the same size
as the object or vary slightly whether a more fluid in-
teraction is required.
Once the object is considered to be grabbed, it is
dependent on the actions of the hand. When grasp
strength is detected to be less than a certain threshold,
the item will behave according to its physical charac-
teristics.
3.3 Box and Block Test (BBT)
Once the different types of grasping and the interac-
tion of the hands with objects in the virtual world have
been established, it is necessary to determine how the
manipulative ability of a user can be measured. There
are different scales and tools to measure motor dex-
terity, such as the Gross Motor test, the Movement
Assessment Battery, the Action Research Arm Test
(ARAT), or the Motor Assessment Scale (MAS) (Carr
et al., 1985).
Particularly, in order to assess manipulative dex-
terity, BBT is widely used by patients with differ-
ent diagnoses: spinal cord injury, geriatrics, multiple
sclerosis and fibromyalgia, among others. Therefore,
in this work, BBT has been performed in three differ-
ent scenarios: a) real physical environment without
the use of technologies, b) non-immersive environ-
ment with virtual elements and, finally, c) immersive
environment based on virtual reality. In scenarios b)
and c), technological solutions have been adopted so
that the user does not need to have their hands occu-
pied with a controller device or attach wearables to
the body.
3.3.1 Scenario 1: BBT in Physical Environment
The BBT, requires a 53.7 cm x 25.4 cm x 8.5 cm
wooden box divided into two compartments of equal
size. Initially, 150 blue, yellow, or red wooden blocks
with a dimension of 2.5 cm are placed in one of the
compartments. This configuration depends on the
hand to be assessed: if it is the right hand, the blocks
are initially placed in the right compartment; if the
dexterity of the left hand is to be measured, the blocks
are placed in the left compartment.
The patient is seated in front of the box and has to
move as many blocks as possible from one compart-
ment to another within 60 seconds (Mathiowetz et al.,
1985). In order to perform the test, the patient is first
given 15 seconds to trial period. Once the test has
started, the examiner must count the displaced blocks
correctly: only one block can be carried in each move-
ment (otherwise, only one is counted), the patient’s
ICEIS 2023 - 25th International Conference on Enterprise Information Systems
234
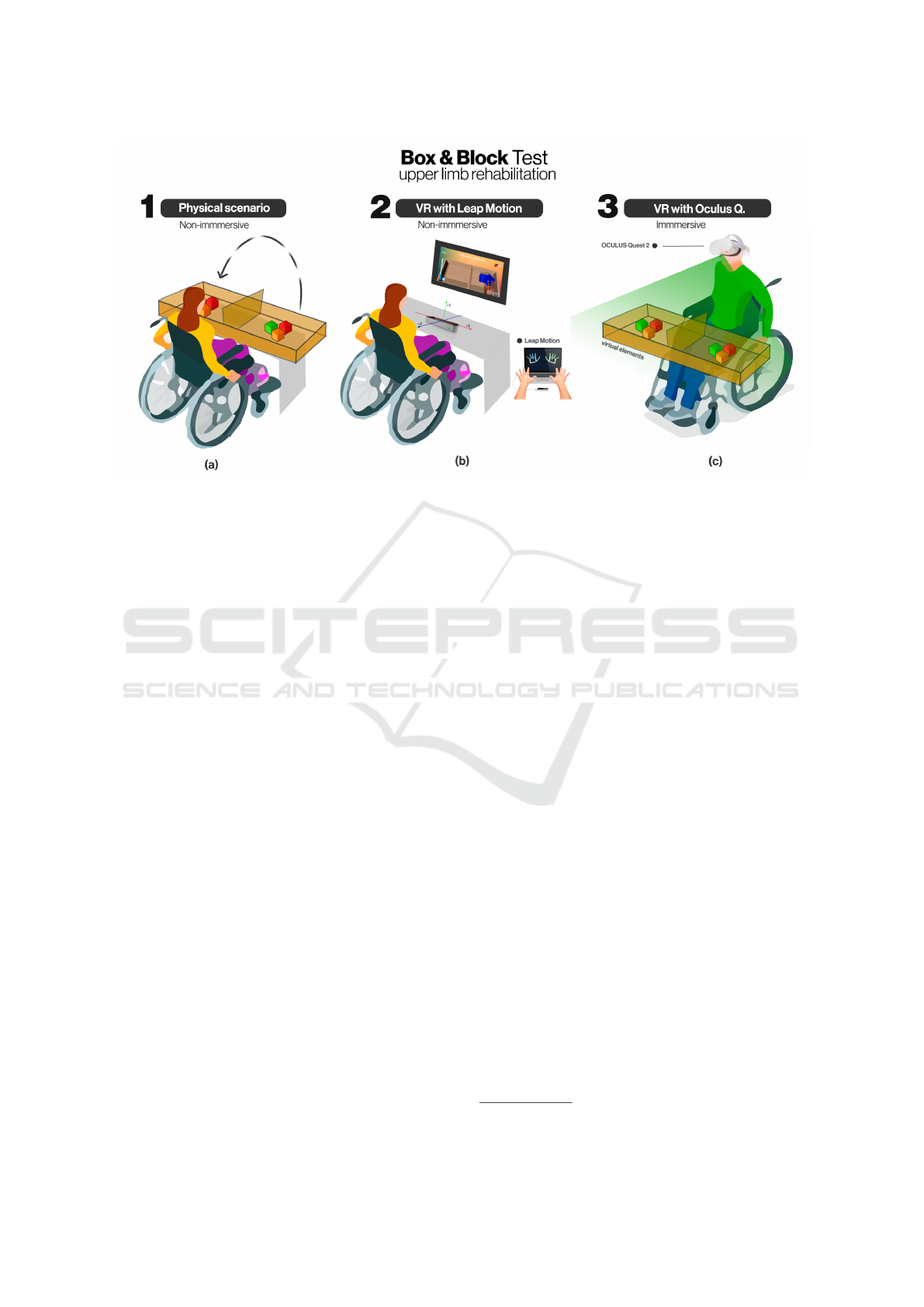
Figure 2: Analysis of hand movement accuracy and performance in the execution of therapeutic exercises using the Box and
Block test in three types of scenarios: a) physical scenario without the use of technologies, b) use of virtual components in a
non-immersive scenario and, finally, c) use of virtual components in a fully immersive scenario.
hand must pass over the partition of the box and re-
lease the block when it is in the target partition.
BBT is a simple test, portable, efficient, and in-
expensive to perform. It provides information on the
speed of performance but not on other aspects such as
the quality of the performed movement (Alt Murphy
et al., 2015). There is no single trajectory to perform
the exercise, apart from the different initial positions
of the cubes in the box. In recent years, new tech-
nologies have been adopted to mitigate the disadvan-
tages derived from the test, so that objective measure-
ments of the user’s movements can be obtained. One
of them is the modified BBT which allows the assess-
ment of movement in upper-limb impairment with the
help of motion capture techniques, and may help mea-
sure the effect of interventions to improve upper-limb
function (Hebert et al., 2014). Other studies make
use of wearable sensors to obtain, among other things,
information on the speed or time spent moving each
block (Zhang et al., 2019).
3.3.2 BBT with Virtual Reality (Scenarios 1 and
2)
Recently, and thanks to the rise of virtual reality, ap-
plications have begun to be developed to simulate
BBT to exploit the advantages of the virtual world
with an accurate capture of movements.
In tests conducted by Gieser et al. (Gieser et al.,
2016) the number of blocks moved in the real BBT
was much higher than those achieved with the non-
immersive VR-BBT. Hashim et al. (Hashim et al.,
2021) in their study with an immersive VR-BBT sup-
ports this result, although this number of achieve-
ments increases in line with the number of training
sessions. Other studies, such as those conducted by
Onat et al. (O
˜
na et al., 5 13) have shown that these
differences are reduced when the environment is im-
mersive, and no additional controllers are used.
This paper presents two solutions to VR-BBT:
non-immersive and immersive. The implementation
of the virtual world has been developed following the
guidelines of the clinical experts of the Hospital de
Parapl
´
ejicos de Toledo. To this end, the physical char-
acteristics of both the box and the blocks, as well as
the colors used, have been taken into account to elim-
inate possible biases in the results obtained with tra-
ditional BBT and virtual BBT.
Both solutions were developed in Unity
2
. The
wooden box and blocks were designed following the
guidelines of the real test. A virtual object is modeled
and instantiated as many times as necessary at run-
time to represent the cubes. Each cube has two basic
elements: Rigidbody and Box Collider. The first one
allows the cube to act under the control of physics,
defining mass and gravity, among others. The sec-
ond is a box collider that simulates physical collisions
with other elements. In order to be faithful to the real
model, the color of each cube is determined randomly,
according to the colors used in the BBT test: red, blue,
or yellow. The position in the scene is also set ran-
domly, and inside the zone of origin (right side for the
right hand or left side for the left hand).
In both proposals, audio and graphical aids have
2
https://unity.com/
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive and Immersive Scenarios
235
Sensor
Layer
Leap Motion Controller (LMC) Oculus Quest 2
Non-immersive
Immersive VR
Hand
Analysis
Hand Pose
Recognition
Hand Tracking
Hand Pose
Recognition
Hand Tracking
Logic
Layer
BBT Virtual Application BBT Virtual Application
Event Controller
Cube Generator
Physics Engine
Object Gripping Module
Event Controller
Cube Generator
Physics Engine
Object Gripping Module
Visualization
Layer
Screen Display
Visualization
Figure 3: Multilayer architecture of the two proposed solutions for virtual BBT. Main hardware components, software and
connection between modules.
been added to help the patient to know the state of
the interaction. Both immersive and non-immersive
solutions have a sound when the cube is grabbed and
another one when the cube is released. In addition,
when a cube is grabbed then it changes to a greyish
colour.
Moreover, both virtual solutions have a pre-
calibration phase to adjust the object grip. In the event
that a user/patient has severe movement limitations,
the test is run in “autogrip” mode. In other words,
the cube is automatically grasped by proximity to the
hand and will be released when it comes into contact
with the target compartment.
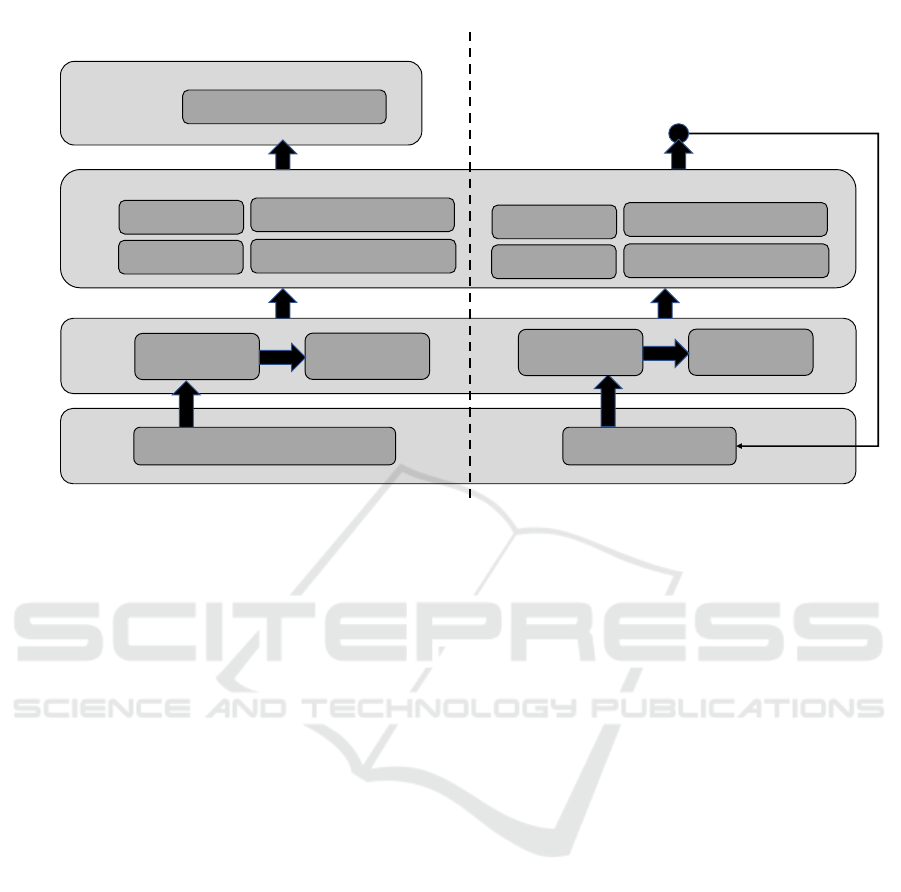
Each of the two VR-based solutions mentioned
above is described in more detail in the following sec-
tion. Figure 3 shows a multilayer architecture of the
two solutions developed. On the left a VR-based and
non-immersive solution, on the right the solution is
fully immersive. The design is divided into four main
layers. The lowest level layer captures the movement
of the hands through a set of sensors. This informa-
tion is processed at a second level to track hands and
recognize grasping gestures. The information gener-
ated at the second level progresses to the logic layer,
where the most significant processing load is located.
In the logic layer, there is a module for generating
BBT cubes, the module that determines the grip be-
tween hands and virtual objects, the event controller
module (any given situation in the virtual environ-
ment), and the physics engine to provide the virtual
elements with realistic behavior. Once all the infor-
mation has been processed, the last layer is responsi-
ble for displaying the changes in the virtual environ-
ment. The major difference between the two solutions
is that in the non-immersive solution the changes are
displayed on a screen and the user does not stop per-
ceiving the real world at any time. In contrast, the
second solution feeds back to the first layer, as the
changes are displayed again in the VR goggles and
the user is completely isolated from the real world.
3.3.3 Scenario 2: BBT in a Non-Immersive
Scenario With Virtual Reality
In a non-immersive scenario, the patient interacts
with his/her own hands and the results of the ac-
tions are displayed in real-time on a screen. In the
non-immersive virtual BBT presented in this paper,
Leap Moption Controller (LMC) has been used for
hand motion capture (see Figure 4). The Leap Mo-
tion Controller is an optical hand-tracking module
to capture hand and finger movement. It is a small
size and low-cost sensor with two cameras and in-
frared LEDs. The connection is made via USB 2.0,
it has two 640x240-pixel near-infrared cameras with
infrared-transparent typically operating at 120Hz, but
the hardware is capable of 240+ (lea, 2022). LMC can
track both hands simultaneously, recognizing gestures
and allowing real-time interaction: pushing, pinching,
ICEIS 2023 - 25th International Conference on Enterprise Information Systems
236

grabbing, etc. Besides, Ultraleap offers an API for
different programming languages and supports inte-
gration with both Unity and Unreal engines for build-
ing real-time 3D projects.
Figure 4: BBT in a non-immersive scenario using LMC and
on-screen display.
The different functional hand grasps are detected
when they come into contact with the collision area
defined in the cube. For this implementation (see Fig-
ure 4), the methods provided by the API were used
to determine the grab strength and pinch strength.
Firstly, we calculate the strength of a hand grasping
posture based on how close the hand is to being a
fist. Secondly, the pinch strength indicates the holding
strength of a pinch hand (between the thumb and an-
other finger of the same hand). In both cases, the do-
main of definition of the variable is a numerical value
belonging to [0,1]. The value 0 indicates no grip,
whereas the value 1 refers to the highest strength.
A set of variables that inform about the execution
of the exercise is stored in real-time. These variables
are: hand used, reliability (degree of confidence of
the hand), palm position (X,Y,Z), palm position in
magnitude, hand speed, grasp capacity understood
as opening and closing the hand (grasp strength) [0-
1], thumb grip capacity with any of the other fin-
gers (grip strength) [0-1], wrist flexion expressed in
degrees (arm.Direction.AngleTo(hand.Direction) ∗
180/( f loat)π) and the pronation of the forearm from
the hand’s roll angle(normal.Roll ∗ 180/( f loat)π +
90).
Finally, it is worth mentioning that the application
has an initial menu to select the difficulty level ac-
cording to time, size, and the number of targets de-
pending on the pinch or grip performed. The menu
design contemplates accessibility aspects so that pa-
tients with physical limitations can interact without
external assistance.
3.3.4 Scenario 3: BBT in Immersive
Environment with Virtual Reality
In immersive VR-BBT, the patient is completely im-
mersed in the virtual world (see Figure 5). The envi-
ronment that the user views and feeds back to is iso-
lated from the real world. Moreover, unlike other pro-
Figure 5: BBT in an immersive scenario in which the pa-
tient perceives only virtual elements.
posals, the solution presented here uses the patient’s
hands as a natural form of interaction. It should be
noted that hand tracking is performed by the virtual
reality device itself, Oculus Quest 2. Unlike other
developments in which was used with virtual reality
glasses (O
˜
na et al., 5 13), the immersive VR-BBT we
propose uses the device’s own hand tracking. From
the clinical study carried out in this work, it was found
that Oculus Quest 2 offer better tracking accuracy
compared to the LMC. This fact results in improved
patient performance as will be discussed in future sec-
tions.
Oculus Quest 2 is a Head-Mounted Display
(HMD) with 6 DoF inside-out via four integrated
cameras for tracking and allows interaction with the
immersive world through the dynamic controllers and
the user’s hands. Hand tracking has been significantly
improved in the new version 2.0 (April 2022), which
allows faster movements and solves occlusion issues,
so more applications integrating this type of interac-
tion are starting to emerge. Meta
3
provides develop-
ers with SDKs for integration into both Unity and Un-
real engines.
The VR-BBT immersive has been developed in
Unity (v.2020.3.23f1) and uses the Hand Tracking
API v2.0. The SDK allows the configuration of cer-
tain parameters; one of the most relevant is the track-
ing rate that can be low, medium or high. The latter
reaches 60 Hz and is the one used in our VR-BBT
application.
The development of the virtual environment has
been implemented following feedback from clinical
specialists. Special attention has been paid to provide
the VR-BBT with a high configurability so that a wide
variety of patients can use it. The primary consider-
ations taken into account to adapt to each patient’s
needs are listed below.
• Recognition of any possible grasp, including ten-
odesis grasp and release. The block grasp is per-
formed by proximity to the hand in case no func-
3
https://www.meta.com/
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive and Immersive Scenarios
237

tional grasp detected.
• Initial configuration of the positioning of the box.
This static element can be adapted to each patient,
i.e., its position in the three axes (X, Y, Z) can be
modified before starting the BBT. The box con-
taining the blocks must be positioned at a suitable
height, i.e., the patient must remain seated, with
the box in front of him/her and a 90° angle must be
formed between the arm and forearm. This avoids
forced shoulder, arm, and forearm positions and
even prevents some of the blocks from being in-
accessible. For this reason, the location of the box
can be configured from the menu, adapting it to
each patient.
• Configuration for patients with severely reduced
mobility. The calibration stage, in which the pa-
tient tries to grasp a sample block in any possible
way might be advisable. The application runs in
“autogrip” mode if no grasp is detected. Concern-
ing the difficulty of the game, two forms, “nor-
mal” and “easy”’, have been created, which are
linked to the separator between the two areas of
the box. Some patients cannot perform arm lifts,
but with this configuration it is possible, in easy
mode, to correctly score when the hand crosses
the separator between the two cubicles. These op-
tions allow testing with a wider range of patients.
• Visual and audio feedback: in addition to the el-
ements discussed in section 3.3.2 the immersive
environment has the following elements to sup-
port interaction. The fingertips change to purple
when starting to grasp a block and to green when
it is grabbed by the hand. In addition, the correct
movement of a block is accompanied by a sound.
A different sound is played when the block has
been moved incorrectly or placed outside the tar-
get partition.
• The initial menu is easily accessible. The buttons
are large and can be pressed with the whole hand.
Interaction can be done either with the hands or
with the controllers.
During the execution of the VR-BBT a dataset is
stored to facilitate a possible a posteriori evaluation of
the performed exercise: the number of frames since
the beginning of the exercise, time measured in sec-
onds, hand detected/not detected, the degree of con-
fidence and position in 3D space of the hand, pinch
detection (true/false), palm grip detection (true/false),
force realized the thumb with the rest of the fingers
([0-1]), the strength of each finger with respect to the
palm ([0-1]) and HMD position (x,y,z). With these
elements, it is possible to determine the number of
correctly performed grips, the type, and the exerted
force. Furthermore, it is possible to detect false neg-
atives due to inefficient hand tracking thanks to the
degree of hand confidence. One of the variables de-
scribed above is worth mentioning, the HMD posi-
tion. This value is stored to report undesirable trunk
compensatory movements. This is done thanks to the
positioning of the HMD in 3D space. The patient’s
head and trunk performs a displacement when move-
ment is detected in the Z axis of the HMD.
The feeling of complete immersion, the adjust-
ments in the virtual environment according to the pa-
tient’s needs and the variables stored at run-time pro-
vide a powerful tool for both the patient and the reha-
bilitators and therapists. The patient feels more mo-
tivated to perform the exercise, which is also adapted
to his or her particular needs. Rehabilitation special-
ists have objective data on the performance of BBT
and can evaluate not only the blocks moved but also
the quality of each movement as well as the patient’s
evolution.
4 CLINICAL STUDY AND
RESULTS
4.1 Participants
The technologies discussed throughout the article
were initially tested on healthy patients. In later
phases of the project, real patients will be included
in the clinical study. Thus, ten healthy individuals
(32.50±17.25 years) participated in the study. All
of them were right-handed and performed the BBT
task in three different experimental conditions with
the dominant hand:
• The real environment.
• The virtual environment in a non-immersive con-
dition by means of Leap Motion Controller.
• The virtual environment in an immersive condi-
tion by means of Oculus Quest 2
With the aim of controlling the order effects, indi-
viduals’ performance in each condition was random-
ized. The clinical study was carried out at the Hospi-
tal Nacional de Parapl
´
ejicos (Toledo, Spain) and was
approved by the local Ethical Committee.
All the subjects must have neurologically healthy
condition. Exclusion criteria were: not signing the
corresponding informed consent; having visual im-
pairment or any impairment of upper limb function;
having previous history of seizure or motion sickness.
ICEIS 2023 - 25th International Conference on Enterprise Information Systems
238

4.2 Clinical Study Setup
Each participant performed all three experimental
conditions on the same day in a single experimental
session. The BBT in each experimental condition was
performed seated in front of a height-adjustable table
until the elbow was flexed 90º with the palm of the
hand on the table. For the immersive VR condition,
the table was removed and it was performed in the
same chair as the other conditions.
Before performing the first trial within the both
VR conditions, a preliminary trial was performed to
familiarize with each virtual environment. In the case
of the real BBT, no familiarization was considered
needed with the exception of the 15 seconds allowed
by the real test (Mathiowetz et al., 1985).
Three trials of each experimental condition were
performed. The variable measured was the total num-
ber of cubes passed to the other side of the box in one
minute. As the final result, the mean value of the three
trials was considered for analysis for each condition.
4.3 Statistical Analysis and Results
The results of the variable analyzed were expressed as
median and interquartile range. The Wilcoxon non-
parametric test was applied to find possible differ-
ences between the three experimental conditions (see
table 1). The relation between each pair of conditions
was analyzed by the Pearson correlation coefficient.
The performance in the real BBT was significantly
higher than in the both VR modalities (83.67 ± 16.75
in the real test vs. 69.17 ± 20.33 in the immersive
VR version (p < 0.05) and 45.66 ± 16.84 in the non-
immersive version (p < 0.01)) (see Figure 8). More-
over these results were statistically significant be-
tween the both VR modalities (p < 0.01) (see Fig-
ure 7). However, if we selected only participants with
previous experience in virtual environments (n = 8),
no statistically significant differences were found be-
tween the real BBT and the immersive VR version
(see Figure 6).
The correlation between the real BBT and the non-
immersive VR BBT was high (0.858, p < 0.05). This
correlation was statistically significant (p < 0.01) be-
tween the real BBT and the immersive BBT (0.717)
and between both VR conditions (0.763).
4.4 Limitations of the Study
The conducted clinical study has been oriented to-
wards the evaluation of data acquisition and perfor-
mance in relation to the BBT. This is an essential as-
pect when devising a system that allows autonomous
Figure 6: Box plot in relation to the cubes passed for each
experimental condition with practice in VR environments
(n = 8).
Figure 7: Box plot in relation to the cubes passed for each
experimental condition and for all the participants (n = 10).
but guided rehabilitation. This first step is key before
evaluating its usefulness with real patients who have
suffered neurological conditions.
After this first step, a series of clinical studies to
analyze if this trend is maintained in spinal cord in-
jured patients will be conducted in a second phase.
These are intended to be performed in the Hospital
Nacional de Parapl
´
ejicos, where the system will be
deployed.
The technological requirements of the discussed
system are not high (VR headset and an standard lap-
top). The authors of this manuscript do not consider
the system as high-cost, since it aims at improving
the rehabilitation process and mitigating the lack of
specialized staff, which is becoming more and more
challenging from a global point of view (see (Alvarez-
Figure 8: Performance of each participant within each ex-
perimental condition. All the participants maintain the same
trend.
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive and Immersive Scenarios
239

Table 1: Significant statistically differences between the three experimental environments analyzed by means of Wilcoxon
test (a,b(p < 0.05), c,d(p < 0.01)).
Participants Physical environment Non-immersive VR Immersive VR
All (n=10) 83.67(16.75)
a,c
45.66(16.84)
c,d
69.17(20.33)
a,d
With practice (n= 8) 83.67(13.50)
a
45.66(15.50)
a,b
72.17(21.83)
b
Sab
´
ın et al., 2017) for a related discussion that affects
stroke rehabilitation in Spain). At this point, one of
the pursued goals is to show the usefulness, and even
the acceptance, of the system when performing reha-
bilitation. Particularly, the study and analysis the in-
fluence of motivation, in the short term, on the user’s
commitment has been considered.
Lastly, in a third phase, a clinical trial will be
conducted to study the feasibility and effectiveness
of the proposed system, considering its intended use
during longer periods of time. The research hypoth-
esis at this point would be the assessment and vali-
dation of effective, upper-limb rehabilitation through
virtual reality at hospitals and rehabilitation centers.
In this phase, functional resonance magnetic imag-
ing (fRMI) will be included in the study for detect-
ing signs of improvement after the rehabilitation treat-
ment. This feature will allow us to design and de-
scribe a motor paradigm and the corresponding ex-
perimental protocol, suitable for all the participants,
whether healthy or SCI patients. Finally, to extend the
fMRI post-processing for analyzing voxel-based mor-
phometry and voxel-based thickness of T1-weighted
images.
5 CONCLUSIONS
This paper analyzes and compares technologies that
facilitate hand tracking and are applied to upper limb
rehabilitation. For this purpose, non-immersive and
immersive virtual solutions based on virtual reality
have been developed and applied in the context of the
Hospital Nacional de Parapl
´
ejicos de Toledo (Spain).
The proposed solutions are integrated together
with the BBT and three different scenarios are pro-
posed: traditional physical scenario without the use
of technologies, non-immersive scenario and virtual
elements and, finally, fully immersive scenario based
on VR.
The main novelty of the work lies in the simulta-
neous design of both non-immersive and immersive
solutions that take into account the future limitations
of patients. Precisely because of these limitations, we
have opted for implementations in which patients can
perform the exercises without the attachment of real
physical controllers or the adhesion of wearables de-
vices.
The starting hypothesis was that the conditions of-
fered by immersive virtual environments can recreate
scenarios and situations very similar to real ones, to
which should be added the advantages of these virtual
environments such as the elimination of physical bar-
riers and the recreation of any type of object. In the
context of rehabilitation, this factor is crucial since
the precision with which therapeutic exercises are per-
formed directly influences the recovery of damaged
limbs.
Precisely, the results demonstrate this hypothesis.
The number of blocks moved from the point of origin
to the point of destination in the immersive environ-
ment largely resembles the data obtained in a tradi-
tional physical environment. This is due to a proper
perception of the environment and the elements pre-
sented, the correct implementation of grasping pose
recognition and, finally, the control logic that deter-
mines the adhesion of objects to the hands.
As future work, the use of devices that can mea-
sure the muscular activity exerted by the patient dur-
ing virtual rehabilitation is proposed, using, for ex-
ample, EMG-based controllers (Pleva et al., 2022).
As well as mixed reality technologies that would al-
low for greater precision in measuring the patient’s
progress and better adaptation of the intensity and dif-
ficulty of the exercises to the individual needs of the
patient.
ACKNOWLEDGMENTS
This work has been founded by the Spanish Ministry
of Science, Innovation and Universities under the Re-
search Project: Platform for Upper Extremity Reha-
bilitation based on Immersive Virtual Reality (Rehab-
Immersive), PID2020-117361RB-C21 and PID2020-
117361RB-C22.
REFERENCES
(2022). Leap Motion Controller Datasheet. Ultraleap.
Alt Murphy, M., Resteghini, C., Feys, P., and Lamers, I.
(2015). An overview of systematic reviews on upper
ICEIS 2023 - 25th International Conference on Enterprise Information Systems
240

extremity outcome measures after stroke. BMC Neu-
rology, 15(1):29.
Alvarez-Sab
´
ın, J., Quintana, M., Masjuan, J., Oliva-
Moreno, J., Mar, J., Gonzalez-Rojas, N., Becerra, V.,
Torres, C., and Yebenes, M. (2017). Economic impact
of patients admitted to stroke units in spain. The Eu-
ropean Journal of Health Economics, 18(4):449–458.
Bravo, V. P. and Mu
˜
noz, J. A. (2022). Wearables and their
applications for the rehabilitation of elderly people.
Medical and Biological Engineering and Computing,
60(5):1239—1252.
Carr, J. H., Shepherd, R. B., Nordholm, L., and Lynne, D.
(1985). Investigation of a new motor assessment scale
for stroke patients. Physical Therapy, 65(2):175–180.
Clus, D., Larsen, M. E., Lemey, C., and Berrouiguet,
S. (2018). The Use of Virtual Reality in Patients
with Eating Disorders: Systematic Review. Journal
of Medical Internet Research, 20(4):e7898. Com-
pany: Journal of Medical Internet Research Distribu-
tor: Journal of Medical Internet Research Institution:
Journal of Medical Internet Research Label: Journal
of Medical Internet Research Publisher: JMIR Publi-
cations Inc., Toronto, Canada.
de Ara
´
ujo, A. V. L., Neiva, J. F. d. O., Monteiro, C. B.
d. M., and Magalh
˜
aes, F. H. (2019). Efficacy of Vir-
tual Reality Rehabilitation after Spinal Cord Injury: A
Systematic Review. BioMed Research International,
2019:e7106951. Publisher: Hindawi.
Dias, P., Silva, R., Amorim, P., La
´
ıns, J., Roque, E.,
Ser
ˆ
odio, I., Pereira, F., and Santos, B. S. (2019). Using
Virtual Reality to Increase Motivation in Poststroke
Rehabilitation. IEEE Computer Graphics and Appli-
cations, 39(1):64–70. Conference Name: IEEE Com-
puter Graphics and Applications.
Everard, G., Otmane-Tolba, Y., Rosselli, Z., Pellissier, T.,
Ajana, K., Dehem, S., Auvinet, E., Edwards, M. G.,
Lebleu, J., and Lejeune, T. (2022). Concurrent valid-
ity of an immersive virtual reality version of the box
and block test to assess manual dexterity among pa-
tients with stroke. Journal of NeuroEngineering and
Rehabilitation, 19(1):7.
Gieser, S. N., Gentry, C., LePage, J., and Makedon, F.
(2016). Comparing objective and subjective metrics
between physical and virtual tasks. In Lackey, S. and
Shumaker, R., editors, Virtual, Augmented and Mixed
Reality, Lecture Notes in Computer Science, pages 3–
13. Springer International Publishing.
Guill
´
en-Climent, S., Garzo, A., Mu
˜
noz Alcaraz, M. N.,
Casado-Adam, P., Arcas-Ruiz-Ruano, J., Mej
´
ıas-
Ruiz, M., and Mayordomo-Riera, F. J. (2021). A us-
ability study in patients with stroke using MERLIN, a
robotic system based on serious games for upper limb
rehabilitation in the home setting. Journal of Neuro-
Engineering and Rehabilitation, 18(1):41.
Hashim, N. A., Razak, N. A. A., and Osman, N. A. A.
(2021). Comparison of Conventional and Virtual Re-
ality Box and Blocks Tests in Upper Limb Amputees:
A Case-Control Study. IEEE Access, 9:76983–76990.
Conference Name: IEEE Access.
Hebert, J. S., Lewicke, J., Williams, T. R., and Vette, A. H.
(2014). Normative data for modified box and blocks
test measuring upper-limb function via motion cap-
ture. Journal of Rehabilitation Research and Devel-
opment, 51(6):918–932.
Hodkin, E. F., Lei, Y., Humby, J., Glover, I. S., Choud-
hury, S., Kumar, H., Perez, M. A., Rodgers, H., and
Jackson, A. (2018). Automated fes for upper limb
rehabilitation following stroke and spinal cord injury.
IEEE Transactions on Neural Systems and Rehabili-
tation Engineering, 26(5):1067–1074.
Jung, H. Y., Lee, J., and Shin, H. I. (2018). The nat-
ural course of passive tenodesis grip in individuals
with spinal cord injury with preserved wrist extension
power but paralyzed fingers and thumbs. Spinal Cord,
56(9):900–906.
Kang, Y., Ding, H., Zhou, H., Wei, Z., Liu, L., Pan, D.,
and Feng, S. (2017). Epidemiology of worldwide
spinal cord injury: a literature review. Journal of Neu-
rorestoratology, Volume 6:1–9.
Lamash, L., Klinger, E., and Josman, N. (2017). Using a
virtual supermarket to promote independent function-
ing among adolescents with Autism Spectrum Disor-
der. In 2017 International Conference on Virtual Re-
habilitation (ICVR), pages 1–7. ISSN: 2331-9569.
Lee, S.-H., Yeh, S.-C., Chan, R.-C., Chen, S., Yang, G.,
and Zheng, L.-R. (2016). Motor ingredients derived
from a wearable sensor-based virtual reality system
for frozen shoulder rehabilitation. BioMed Research
International, 10(6). Publisher: Hindawi.
Maggio, M. G., De Cola, M. C., Latella, D., Maresca, G.,
Finocchiaro, C., La Rosa, G., Cimino, V., Sorbera, C.,
Bramanti, P., De Luca, R., and Calabr
`
o, R. S. (2018).
What about the role of virtual reality in parkinson dis-
ease’s cognitive rehabilitation? preliminary findings
from a randomized clinical trial. Journal of Geriatric
Psychiatry and Neurology, 31(6):312–318. Publisher:
SAGE Publications Inc STM.
Mathiowetz, V., Volland, G., Kashman, N., and Weber, K.
(1985). Adult norms for the box and block test of man-
ual dexterity. The American Journal of Occupational
Therapy, 39(6):386–391.
Mekki, M., Delgado, A. D., Fry, A., Putrino, D., and
Huang, V. (2018). Robotic rehabilitation and spinal
cord injury: a narrative review. Neurotherapeutics,
15(3):604–617.
O
˜
na, E. D., Jard
´
on Huete, A., Cuesta-G
´
omez, A., Baeza,
P., Cano de la Cuerda, R., and Balaguer, C. (2020-05-
13). Validity of a fully-immersive VR-based version
of the box and blocks test for upper limb function as-
sessment in parkinson’s disease. Sensors, 20:2773.
Oliveira, C. S., Almeida, C. S., Freitas, L. C., Santana, R.,
Fernandes, G., Junior, P. R. F., and Moura, R. C. F.
(2016). Use of the box and block test for the evalu-
ation of manual dexterity in individuals with central
nervous system disorders: A systematic review. Man-
ual Therapy, Posturology & Rehabilitation Jour-
nal, pages 1–7.
Pereira, M. F., Prahm, C., Kolbenschlag, J., Oliveira, E.,
and Rodrigues, N. F. (2020). A virtual reality serious
game for hand rehabilitation therapy. In 2020 IEEE
8th International Conference on Serious Games and
Performance Analysis for Upper Limb Rehabilitation in Non-Immersive and Immersive Scenarios
241

Applications for Health (SeGAH), pages 1–7. ISSN:
2573-3060.
Pleva, M., Koare
ˇ
cko, v., Hladek, D., Bours, P., Skudal,
M. H., and Liao, Y.-F. (2022). Biometric user iden-
tification by forearm EMG analysis. In 2022 IEEE
International Conference on Consumer Electronics -
Taiwan, pages 607–608. ISSN: 2575-8284.
Rupp, R., Biering-Sørensen, F., Burns, S. P., Graves, D. E.,
Guest, J., Jones, L., Read, M. S., Rodriguez, G. M.,
Schuld, C., Tansey-Md, K. E., et al. (2021). Inter-
national standards for neurological classification of
spinal cord injury: revised 2019. Topics in spinal cord
injury rehabilitation, 27(2):1–22.
Spooren, A. I. F., Janssen-Potten, Y. J. M., Kerckhofs, E.,
Bongers, H. M. H., and Seelen, H. A. M. (2011). Eval-
uation of a task-oriented client-centered upper extrem-
ity skilled performance training module in persons
with tetraplegia. Spinal Cord, 49(10):1049–1054.
Toldo, J. M. P., Arjona, M., Campos Neto, G. C., Vitor, T.,
Nogueira, S. A., Amaro, E. J., Saba, R. A., Silva, S.
M. C. A., Ferraz, H. B., and Fel
´
ıcio, A. C. (2021). Vir-
tual rehabilitation in parkinson disease: A dopamine
transporter imaging study. American Journal of Phys-
ical Medicine & Rehabilitation, 100(4):359–366.
Vergara, M., Sancho-Bru, J. L., Gracia-Ib
´
a
˜
nez, V., and
P
´
erez-Gonz
´
alez, A. (2014). An introductory study of
common grasps used by adults during performance of
activities of daily living. Journal of Hand Therapy,
27(3):225–234.
Wyndaele, M. and Wyndaele, J.-J. (2006). Incidence, preva-
lence and epidemiology of spinal cord injury: what
learns a worldwide literature survey? Spinal cord,
44(9):523–529.
Zhang, Y., Chen, Y., Yu, H., Lv, Z., Shang, P., Ouyang,
Y., Yang, X., and Lu, W. (2019). Wearable
sensors based automatic box and block test sys-
tem. In 2019 IEEE SmartWorld, Ubiquitous
Intelligence Computing, Advanced and Trusted
Computing, Scalable Computing and Communi-
cations, Cloud and Big Data Computing, Internet
of People and Smart City Innovation (Smart-
World/SCALCOM/UIC/ATC/CBDCom/IOP/SCI),
pages 952–959.
ICEIS 2023 - 25th International Conference on Enterprise Information Systems
242
