
Fall Risk Assessment Using Wearable-Based Turn Detection:
Comparison of Different Algorithms During Real-World Monitoring
Jose Albites-Sanabria
1,2 a
, Pierpaolo Palumbo
1b
, Stefania Bandinelli
3c
, Luca Palmerini
1,4 d
and Lorenzo Chiari
1,4 e
1
Department of Electrical, Electronic, and Information Engineering – DEI, University of Bologna, Italy
2
Institute of Advanced Studies, University of Bologna, Italy
3
Azienda Sanitaria Toscana Centro, Firenze, Piero Palagi Hospital, Firenze, Italy
4
Health Sciences and Technologies-Interdepartmental Center for Industrial Research, University of Bologna, Italy
Keywords: Turning, Wearable Sensors, Continuous Monitoring, Older Adults, Falls.
Abstract: Turning deficits have been linked to aging and movement disorders and are a common cause of falls and
fractures. Despite previous works on the automatic identification of turns and on its relation to fall risk,
different algorithms for turn identification have been used, but their agreement and differences have not been
investigated. In this study, we compared the two most-used turn-validated algorithms (El-Gohary and Pham)
using a dataset comprising real-world data from 171 community-dwelling older adults monitored for one
week with a single wearable sensor. The quantity and quality of turn parameters were calculated and used as
predictors of future falls. After the analysis, the El-Gohary and Pham algorithms identified 1,063,810 and
942,845 turns, respectively. The agreement of the algorithms showed a very high to moderate correlation for
all turn parameters. We found that prospective fallers take longer to perform a turn, and their movements are
less smooth when compared to non-fallers. A fall risk assessment model built only on turn parameters showed
reasonable performance for both algorithms (AUC = 0.6). Our results show that differences between turn
parameters in the algorithms, when averaged at the single-subject level, are less of a concern when looking
for associations with prospective falls.
1 INTRODUCTION
Turning represents a major component of everyday
walking behavior, as between 35 and 45% of steps
occur within turns (Glaister et al., 2007). However,
up until recent years, studies only focused primarily
on straight-ahead walking. Turning requires a
continuous change of the center of mass and multi-
limb coordination, so it is not surprising that its
deficits are associated with movement disorders and
the risk of falling.
Several studies have noted that turns can
challenge stability maintenance and increase energy
expenditure, and that turning time, steps per turn, and
variability in the number of steps across different
a
https://orcid.org/0000-0001-7688-6221
b
https://orcid.org/0000-0002-4438-1787
c
https://orcid.org/0000-0002-6491-0850
d
https://orcid.org/0000-0003-4758-662X
e
https://orcid.org/0000-0002-2318-4370
turns are valuable features for distinguishing fallers
from non-fallers (Mancini et al., 2016). Subtle fall-
risk-related gait-based measures may become highly
effective fall-risk indicators when applied to turns due
to the increased challenge to stability compared to
straight walking. Individuals at high risk of falling
employ different turning methods than healthy
individuals.
Assessment of turning is not trivial. Optical
systems have been widely used in previous studies
but are cumbersome, expensive, and can only be used
in controlled environments (Marín et al., 2020;
Thigpen et al., 2000). Wearable sensors, which can
measure for days or even weeks, are a promising
294
Albites-Sanabria, J., Palumbo, P., Bandinelli, S., Palmerini, L. and Chiari, L.
Fall Risk Assessment Using Wearable-Based Turn Detection: Comparison of Different Algorithms During Real-World Monitoring.
DOI: 10.5220/0011727700003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 4: BIOSIGNALS, pages 294-300
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
alternative. Hence, they are ideal in unconstrained
environments over long periods of time.
Algorithms for analyzing the turning movements
of older adults and Parkinson’ disease patients have
already been published. To the best of our knowledge,
only two algorithms based on one inertial sensor
(accelerometer and gyroscope) worn on the lower
back have been validated against video observation
(gold standard) with reasonable agreement. These
algorithms have been and are currently used by other
studies to extract relevant turning parameters
associated with movement disorders and the risk of
falling (Haertner et al., 2018; Leach et al., 2018;
Roussos et al., 2022; Thierfelder et al., 2022).
However, using different algorithms increases
heterogeneity in remote monitoring studies;
validation and adoption of standardized
digital
mobility biomarkers is an ongoing task being
addressed by different initiatives.
In this study, we tested two algorithms to identify
turns and extract turning characteristics in real-world
conditions. We aim to compare here the performance
of the two algorithms and their impact on assessed
turn quantity and quality during a week of monitoring
relative to prospective falls. To the best of our
knowledge, this is the first study characterizing
different turning biomarkers worn on the lower back
for fall risk assessment in real-world conditions.
2 METHODS
Study Participants and Settings
The present study is based on data from the 4
th
wave
of the “Invecchiare in Chianti” (InCHIANTI) study.
One hundred and seventy-one community-dwelling
older adults over 65 (79·7±6·6) years, 50·9% female,
were monitored for 5–9 days using a smartphone
(Samsung Galaxy SII), embedded with a tri-axial
accelerometer and gyroscope with a 100 Hz sampling
rate, worn on the midsagittal plane of the lower back
during all waking hours.
Participants brought the device home, used it for
one week, and then returned it to the clinical staff at
the end of the monitoring period. Telephone
interviews were used to collect prospective fall
incidence data between 6 and 12 months after the start
of continuous monitoring. Participants who did not
fall were defined as non-fallers [NFs] and participants
who fell one or more times were defined as fallers
[Fs].
The study protocol was approved by the ethical
committee of the Italian National Institute of
Research and Care of Aging and complies with the
Declaration of Helsinki. All participants received a
detailed description of the study purpose and
procedures and gave their written informed consent.
Turns
Two validated algorithms for turning detection were
implemented in Python 3.8
(El-Gohary et al., 2013) algorithm measures the
angular rotational rate of the pelvis about the vertical
axis (𝑤
). Candidate turns are detected in segments
where the maxima of the low-pass filtered ( 𝑓
=
1.5 𝐻𝑧) 𝑤
exceed a threshold of 15°/s. The start and
end of turns are found when the filtered signal drops
below 5°/s. The direction of the turn (right or left) was
defined by the sign of 𝑤
.
(Pham et al., 2017) algorithm estimates the
angular displacement around the vertical axis through
attitude estimation. The start of a right turn is defined
by a change from an increase to a decrease of the
angular displacement, and the end by a change from
a decrease to an increase of the angular displacement.
The opposite operation is applied to the definition of
a left turn.
Both methods rely on a single inertial sensor worn
on the lower back to detect turns. Still, different post-
processing cutoffs are suggested to improve the
performance of the algorithm based on heuristics. The
thresholds were optimized and validated using video
observations according to the information reported by
the authors of the algorithms. Table 1 presents a
description of both algorithms.
Table 1: Characteristics of turn algorithms.
El-Gohar
y
Pha
m
Sensor accelerometer
+
gy
roscope
accelerometer +
gy
roscope
Location Low bac
k
Low bac
k
Identification
method
Maxima from
filtered vertical
angular
velocit
y
Changes in
vertical angular
displacement
Turn
duration
threshold*
0.5 – 5 s 0.1 – 10 s
Turn angle
threshold*
45° 90°
* Thresholds Suggested by Authors
To standardize the comparison of both algorithms,
turns with angles between 50–200° and durations
between 0.5–5 seconds were applied in the
implementation of the algorithms and were analyzed.
Fall Risk Assessment Using Wearable-Based Turn Detection: Comparison of Different Algorithms During Real-World Monitoring
295

Turns were divided into three subsets based on turn
angle (small (50–100°], medium (100–150°], and
large (150–200°]) to account for different motor
planning strategies within our analysis.
Following what was defined in previous studies,
we calculated different quantity and quality turn
parameters. Turn quantity was characterized by the
number of turns per hour (TPH). Turn quality was
characterized by the turn duration (DUR), turn angle
(ANG), mean velocity (MV), and peak turn velocity
(PV)(Caby et al., 2011; Leach et al., 2018), and the
spectral arc length (SPARC)(Figueiredo et al., 2020;
Gulde & Hermsdörfer, 2018).
Statistical Analyses
The degree of agreement for turn detection between
the two algorithms was calculated using a correlation
matrix of quantity and quality parameters of turns.
Univariate and k-fold cross validation logistic
regression analysis was used to evaluate the
association of turn parameters with prospective falls
for both algorithms. The quantity and quality turn
parameters were included as independent variables in
the univariate model. The correlation between
quantity and quality parameters was used to select a
set of possible explanatory variables in the
multivariate model. All analyses were performed
using Python 3.8. All p values were two-tailed, and p
< 0.05 was considered significant.
3 RESULTS
Cohort and Fall Status
Table 2 presents demographic and clinical data about
participants included in the study, labeled as fallers
and non-fallers.
Table 2: Cohort characteristics for 12-month prospective
falls.
Non-Fallers
[NFs]
(N=142)
Fallers [Fs]
(N=29)
Combined
(N=171)
Gender
(
M/F
)
73/69 11/18 84/87
Age
(years)
79.4 ± 6.7 81.1 ± 5.5 79.7 ± 6.5
Height
(cm)
159.8 ± 9.1 159 ± 9.5 159.6 ± 9.1
Weight
(
k
g)
70.7 ± 13.1 70.2 ± 14.4 70.6 ± 13.3
MMSE 27.3 ± 1.9 27.1 ± 1.8 27.3 ± 1.8
Turns Characterization
A total number of 1,063,810 and 942,845 turns were
detected from the dataset with El-Gohary and Pham
algorithms, respectively (Figure 1).
Figure 1: Turns identified during real-world monitoring.
The average across days was computed for each
participant. “El-Gohary and Pham algorithms showed
very high agreement on TPH ( 𝑅
=0.97), high
agreement on DUR, ANG, and SPARC (𝑅
between
0.74 and 0.82) and moderate agreement on PV and
MV (𝑅
0.51-0.61) (Figures 2-3, Table 3).
Figure 2: Turn quantity correlation identified by turn
algorithms.
Table 3 summarizes descriptive characteristics for
turn quantity and quality parameters. Computed
DUR, ANG, and SPARC revealed high agreement
between quality turn characteristics identified by both
algorithms. MV and PV showed moderate correlation
among the computed parameters.
While not reported in the present manuscript,
outliers were identified in MV and PV, which may be
responsible for the lower agreement.
BIOSIGNALS 2023 - 16th International Conference on Bio-inspired Systems and Signal Processing
296
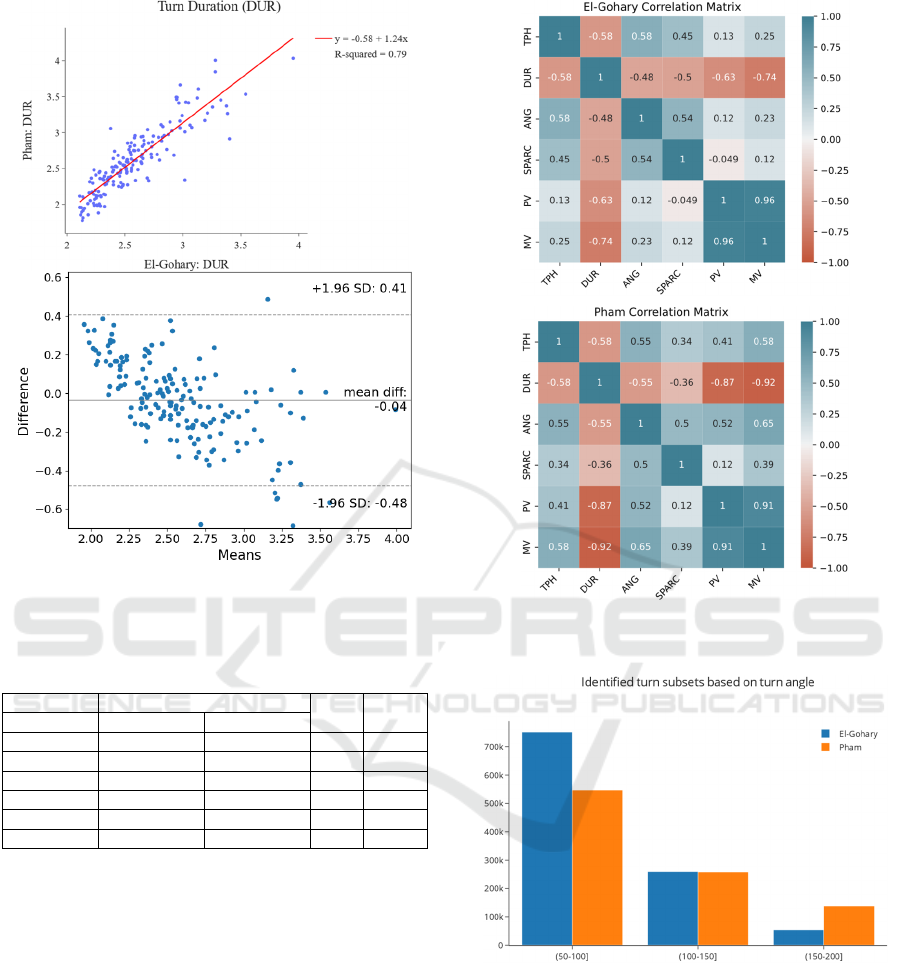
Figure 3: Correlation (upper) and Bland-Altman plot
(bottom) for turn duration (s).
Table 3: El-Gohary and Pham correlation and mean
difference.
Overall means + SD
𝑅
Mean
diff
El-Gohary Pham
TPH (/h) 74.87±34.8 66.44±31.71 0.97 8.43
DUR (s) 2.57±0.33 2.61±0.46 0.79 0.04
ANG (°) 86.77±3.88 99.08±4.47 0.74 12.31
MV (°/s) 43.76±7.02 44.8±4.9 0.61 1.04
PV (°/s) 96.04±16.16 92.07±8.4 0.51 3.97
SPARC -2.14±0.09 -2.04±0.07 0.82 0.1
Taking physical properties of body movement
into account, it is expected that some of the quality
parameters extracted from turns will be correlated
(angle, velocity, duration). Therefore, to avoid
collinearity problems in the following multivariate
analysis, we analyzed potential correlations between
parameters. Figure 4 shows the correlation matrix for
all parameters (turn quantity and quality).
To account for different motor planning strategies
individuals take when performing a turn, three
subsets based on turn angle (small (50–100°],
medium (100–150°], and large (150–200°]) were
analyzed. As shown in figure 5, despite a high
agreement in angle estimation of both algorithms, the
subtle differences in the estimation techniques lead to
considerable differences when differentiating turns
based on their angle ranges.
Figure 4: Correlation matrix for turn quantity and quality
parameters.
Figure 5: Turns’ subsets division based on turn angle.
Turns and Prospective Falls
To identify associations between turn parameters and
prospective falls, the fall incidence used in the
analysis was calculated after a 6-month (NFs: 157,
Fs: 14) and a 12-month period (NFs: 142, Fs: 29).
The odds ratios that quantify the univariate
associations between turn quantity and quality
parameters and fall status after 12 months are shown
in Figure 6. Z-scored was applied for better
Fall Risk Assessment Using Wearable-Based Turn Detection: Comparison of Different Algorithms During Real-World Monitoring
297

visualization of the forest plot. The parameters were
grouped by characteristics according to the algorithm
used for turn detection and angle-range subsets (the
prefix 50, 100, or 150 defines the type of subset
analyzed).
Turn measures were associated with prospective
fall status when analyzing all turns for both
algorithms. Despite some differences, both
algorithms identified the same parameters that were
strongly associated with future falls. More TPH,
longer DUR, and less smooth movements (SPARC)
were associated with the risk of falling (Figure 6). PV
and MV demonstrated similar trends to DUR, which
is in agreement with findings in the turns
characterization section (correlation matrix, figure 4).
Finally, specific angle-range subsets (e.g., (150–
200°] TPH) seemed to provide stronger evidence for
turn associations with prospective falls.
Figure 6: Forest plot of univariate analysis for turn
parameters associated with 12-month prospective falls, El-
Gohary (top), Pham (bottom).
For multivariate analysis, we then performed a
selection of parameters based on the univariate
analysis and previous results from the correlation
matrix analysis. Since PV and MV were moderately
and highly correlated with DUR in the El-Gohary and
Pham parameters, respectively, both parameters were
removed from the following multivariate analysis.
The results of the ROC curve analysis using TPH,
DUR, ANG, and SPARC to classify fallers vs. non-
fallers over a 6-month and 12-month period are
shown in Figure 7. A different set of parameters (e.g.,
based on specific angle ranges) was also analyzed and
was found to only marginally improve the
performance of the classifier.
Figure 7: ROC curve for 6-month (top) and 12-month
(bottom) prospective falls.
4 CONCLUSIONS
In this study, we compared two wearable-based turn
detection algorithms and assessed their importance in
real-world fall risk assessment.
Although both algorithms are based on the same
“principle” (e.g., estimating turns based on the
rotation of the pelvis around the vertical axis),
different processing steps to identify turn events lead
to significant differences in the number of detected
turns and angles estimated by both algorithms. The
readings from the gyroscope (i.e., the angular speed)
are generally very accurate; however, drift might
occur when integrating gyroscope readings over
BIOSIGNALS 2023 - 16th International Conference on Bio-inspired Systems and Signal Processing
298

longer periods, such as in continuous monitoring
experiments. Future studies could apply available
techniques to avoid drifting, such as the integration of
data coming from the orientation sensor (magnetic
plus acceleration) and data coming from the
gyroscope. The use of additional sensors combined
with data fusion techniques could improve accuracy
in the identification of turns while increasing
computational and power costs.
Despite some differences and potential errors in
estimating some quantity and quality parameters,
both algorithms showed a moderately to very high
correlation. We hypothesize that the differences
among turn parameters at the single-subject level are
less of a concern when looking for associations with
prospective falls. In line with this discussion, we
could summarize a pipeline-process: turn detection,
calculation of turn parameters at the single-turn level,
and calculation of the average over turns of each
subject to extract turn parameters at the subject level.
The last two steps downstream (probably, the average
step in particular) attenuate the discrepancies, making
the two algorithms exchangeable. Initial evidence for
this statement is given by the similar performance of
the logistic regression model built on the identified
turning parameters with both algorithms.
All in all, the results and parameters presented
here are in line with previous research studies and
with current clinical standards tests. In fact, turning
ability is a fundamental aspect of several walking
tests, including the Timed Up and Go Test (TUG),
which is used to discriminate fallers from non-fallers.
Other cohorts could also be explored in prospective
longitudinal studies, it should be noted that the
percentage of fallers after 6 and 12 months in this
cohort was significantly lower than the global
statistics for falls in older adults.
Last but not least, a quick review of the literature
shows an exponential increase in reports related to
wearable-based monitoring for fall prevention.
However, despite several efforts to use this
technology for assessments of both healthy and
pathological movement patterns, the high level of
heterogeneity in the use of wearables (e.g., sensor
location and extracted gait parameters) makes it hard
to yield conclusive results. While some ongoing
initiatives aim to establish the clinical validity of
digital mobility biomarkers in different cohorts, some
real-world characteristics, such as turning, deserve
deeper analysis.
ACKNOWLEDGEMENT
This study was partially funded by the Innovative
Medicines Initiative 2 Joint Undertaking under grant
agreement No 820820 (Mobilise-D). This Joint
Undertaking receives support from the European
Union’s Horizon 2020 research and innovation
programme and EFPIA.
REFERENCES
Caby, B., Kieffer, S., de Saint Hubert, M., Cremer, G., &
Macq, B. (2011). Feature extraction and selection for
objective gait analysis and fall risk assessment by
accelerometry. BioMedical Engineering OnLine, 10(1),
1. https://doi.org/10.1186/1475-925X-10-1
El-Gohary, M., Pearson, S., McNames, J., Mancini, M.,
Horak, F., Mellone, S., & Chiari, L. (2013). Continuous
monitoring of turning in patients with movement
disability. Sensors (Basel), 14(1), 356–369.
Figueiredo, A. I., Balbinot, G., & Brauner, F. O. (2020).
SPARC Metrics Provide Mobility Smoothness
Assessment in Oldest-Old With and Without a History
of Falls : A Case Control Study. 11(June), 1–11.
https://doi.org/10.3389/fphys.2020.00540
Glaister, B. C., Bernatz, G. C., Klute, G. K., & Orendurff,
M. S. (2007). Video task analysis of turning during
activities of daily living. 25, 289–294. https://
doi.org/10.1016/j.gaitpost.2006.04.003
Gulde, P., & Hermsdörfer, J. (2018). Smoothness Metrics
in Complex Movement Tasks. 9(September), 1–7.
https://doi.org/10.3389/fneur.2018.00615
Haertner, L., Elshehabi, M., Zaunbrecher, L., Pham, M. H.,
Maetzler, C., van Uem, J. M. T., Hobert, M. A., Hucker,
S., Nussbaum, S., Berg, D., Liepelt-Scarfone, I., &
Maetzler, W. (2018). Effect of fear of falling on turning
performance in Parkinson’s disease in the lab and at
home. Frontiers in Aging Neuroscience, 10(MAR), 1–
8. https://doi.org/10.3389/fnagi.2018.00078
Leach, J. M., Mellone, S., Palumbo, P., Bandinelli, S., &
Chiari, L. (2018). Natural turn measures predict
recurrent falls in community-dwelling older adults: a
longitudinal cohort study. Scientific Reports, 8(1),
4316. https://doi.org/10.1038/s41598-018-22492-6
Mancini, M., Schlueter, H., El-Gohary, M., Mattek, N.,
Duncan, C., Kaye, J., & Horak, F. B. (2016).
Continuous Monitoring of Turning Mobility and Its
Association to Falls and Cognitive Function: A Pilot
Study. The Journals of Gerontology Series A:
Biological Sciences and Medical Sciences, 71(8),
1102–1108. https://doi.org/10.1093/gerona/glw019
Marín, J., Blanco, T., de la Torre, J., & Marín, J. J. (2020).
Gait analysis in a box: A system based on
magnetometer-free IMUs or clusters of optical markers
with automatic event detection. Sensors (Switzerland),
20(12), 1–27. https://doi.org/10.3390/s20123338
Fall Risk Assessment Using Wearable-Based Turn Detection: Comparison of Different Algorithms During Real-World Monitoring
299

Pham, M. H., Elshehabi, M., Haertner, L., Heger, T.,
Hobert, M., Faber, G., & Maetzler, W. (2017).
Algorithm for Turning Detection and Analysis
Validated under Home-Like Conditions in Patients with
Parkinson ’ s Disease and Older Adults using a 6
Degree-of-Freedom Inertial Measurement Unit at the
Lower Back. 8(April), 1–8. https://doi.org/10.3389/
fneur.2017.00135
Roussos, G., Herrero, T. R., Hill, D. L., Dowling, A. V.,
Müller, M. L. T. M., Evers, L. J. W., Burton, J., Derungs,
A., Fisher, K., Kilambi, K. P., Mehrotra, N., Bhatnagar,
R., Sardar, S., Stephenson, D., Adams, J. L., Ray Dorsey,
E., & Cosman, J. (2022). Identifying and characterising
sources of variability in digital outcome measures in
Parkinson’s disease. Npj Digital Medicine, 5(1), 1–10.
https://doi.org/10.1038/s41746-022-00643-4
Thierfelder, A., Seemann, J., John, N., Harmuth, F., Giese,
M., Schüle, R., Schöls, L., Timmann, D., Synofzik, M.,
& Ilg, W. (2022). Real-Life Turning Movements
Capture Subtle Longitudinal and Preataxic Changes in
Cerebellar Ataxia. Movement Disorders, 37(5), 1047–
1058. https://doi.org/10.1002/mds.28930
Thigpen, M. T., Light, K. E., Creel, G. L., & Flynn, S. M.
(2000). Turning difficulty characteristics of adults aged
65 years or older. Physical Therapy, 80(12), 1174–
1187. https://doi.org/10.1093/ptj/80.12.1174
BIOSIGNALS 2023 - 16th International Conference on Bio-inspired Systems and Signal Processing
300
