
Systematic Review: Drug Interactions in the Treatment of
Hypertension with Diabetes Mellitus
Sofia Ngarso and Diana Laila Ramatillah
Faculty Pharmacy, University 17 August 1945 Jakarta, Jl. Sunter Permai Raya, Jakarta 14350, Indonesia
Keywords: Diabetes Mellitus, Drug, Hypertension, Interactions.
Abstract: Hypertension and diabetes are degenerative diseases that can cause a decrease in the body's physiological
functions. Regular monitoring of blood pressure and blood sugar levels, along with consistent treatment, can
help reduce physical complaints. However, it is important to be aware of potential drug interactions that may
affect the effectiveness of treatment and cause unwanted side effects. The objective of this study was to
evaluate drug interactions in the treatment of hypertension and diabetes mellitus. A systematic review was
conducted following the PRISMA (Preferred Reporting Items for Systematic Review) guidelines. Relevant
published articles were searched for to investigate the use and interactions of drugs in patients with
hypertension and diabetes. The literature search was conducted between July and August 2023 using Google
Scholar, National Library of Medicine, and Public Health Reviews. The results show that commonly used
treatments for hypertensive patients with diabetes mellitus include Amlodipine-Metformin, Furosemide-
Metformin, Captopril-Glimepiride, and Captopril-Metformin. It is important to note that the interaction of
various drugs can increase the risk of health problems and drug-drug interactions. The literature review's
conclusion highlights the significance of evaluating drug interactions in treating hypertension and diabetes
mellitus to ensure effective and appropriate treatment.
1
INTRODUCTION
Diabetes mellitus and hypertension are degenerative
diseases caused by various factors, such as age,
oxidative stress, and lifestyle, that lead to a decrease
in the body's physiological functions (Madania et al.,
2022). The prevalence of hypertension or high blood
pressure accompanied by complications of diabetes
mellitus, often referred to as the 'Silent Killer,'
continues to increase every year (Rosyadi, 2022).
The World Health Organization (WHO) reports
that 1.28 billion adults aged 30 to 79 worldwide suffer
from hypertension, with two-thirds of them residing
in low or middle income countries (WHO, 2023). The
number of people affected by hypertension continues
to rise annually across the globe. By 2025, it is
projected that 1.5 billion people will suffer from
hypertension, and 9.4 million people will die from
hypertension-related complications each year (Ganga
et al., 2022). In 2019, Paraguay, Dominican Republic,
Dominica, Argentina, Grenada, Jamaica, Saint Kitts
and Nevis, and Brazil had the highest prevalence of
hypertension, with rates exceeding 45% (PAHO,
2023). In 2018, Indonesia joined the list of Southeast
Asian countries with the highest incidence of
hypertension, affecting 34.1% of the population
(Pulungan et al., 2022).Hypertension is the
occurrence of increased blood pressure which is
characterized by systolic blood pressure >140 mmHg
and diastolic blood pressure >90 mmHg, where
symptoms can vary for each individual.
The most common symptoms of hypertension
include headache or heaviness in the nape of the neck,
vertigo, heart palpitations, fatigue, blurred vision,
tinnitus, and nosebleeds (Nurlinda et al., 2022).
Hypertension can lead to comorbidities, such as
diabetes mellitus, due to shared trigger factors like
diet, lack of physical activity, and impaired insulin
production in diabetes sufferers, which directly affect
blood pressure (Wati et al., 2021). Hypertension in
diabetes patients is caused by high blood glucose
levels, which lead to intravascular fluid resistance and
an increase in body fluid volume. Additionally,
damage to the vascular system increases peripheral
arterial resistance, resulting in hypertension
(Rasdianah & Pakaya, 2023).
Regular control of blood pressure and blood sugar
is necessary to reduce physical complaints, and
Ngarso, S. and Ramatillah, D.
Systematic Review: Dr ug Interactions in the Treatment of Hypertension with Diabetes Mellitus.
DOI: 10.5220/0012643000003821
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 4th International Seminar and Call for Paper (ISCP UTA ’45 JAKARTA 2023), pages 257-264
ISBN: 978-989-758-691-0; ISSN: 2828-853X
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
257
patients should undergo regular treatment
(Simanjuntak & Amazihono, 2023). The treatment
options for oral diabetes and hypertension include
Amlodipine-Metformin, Furosemide-Metformin,
Captopril-Glimepiride, and Captopril-Metformin
(Retnowati & Renha Lestari, 2022). It is important to
note that drug interactions can lead to unsuccessful
treatment of diabetes mellitus and increased blood
pressure. When patients take multiple medications,
treatment failure is a common problem that can lead
to increased toxicity or decreased efficacy of
concurrent medications (Abdulkadir et al., 2023).
Additionally, the use of multiple drugs increases the
risk of health problems and drug-drug interactions
(DDIs) (Madania et al., 2022). Drug interactions can
be a significant issue that affects patient clinical
outcomes. With the complexity of drugs used in
current treatments and the tendency for
polypharmacy to occur, the possibility of drug
interactions is increasing (Susanti, 2021).
2
METHODS
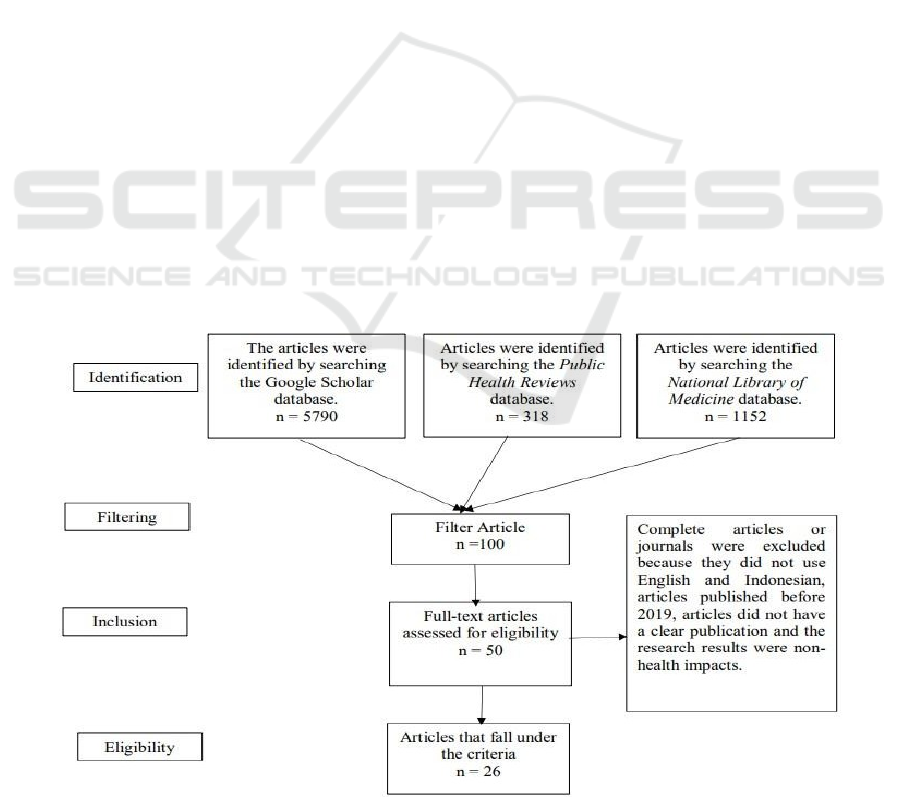
A systematic review was conducted to search for
published articles on drug use and drug interactions
in the treatment of hypertension and diabetes
mellitus. The search strategy involved using online
database facilities such as Google Scholar, National
Library of Medicine, and Public Health Reviews. The
search was limited to the years 2019 to 2023 and
included Public Health Reviews and the National
Library of Medicine. Researchers searched
international and national journals using the
keywords 'Drug Interactions in the Treatment of
Hypertension with Diabetes Mellitus' and 'Drug Use
and Drug Interactions in the Treatment of
Hypertension with Diabetes Mellitus' respectively. to
2023. English or Indonesian articles were selected
based on their relevance to the inclusion and
exclusion criteria. The inclusion criteria were limited
to articles published between 2019 and 2023 that
discuss treatment and treatment interactions, as well
as patient socio-demographics. The exclusion criteria
for this study are as follows: articles that are
incomplete or not written in English or Indonesian,
articles published before 2019, and articles that do not
have clear publications or research results that have
non-health impacts. The author employed a
systematic review method following the PRISMA
(Preferred Reporting Items for Systematic Review)
stages, which include identification, screening,
inclusion, and analysis of relevant article findings. To
record treatment and drug interactions, we reviewed
articles that met the inclusion criteria. The study
recorded and presented all identified risk factors,
along with a narrative explanation. Conclusions were
drawn based on the collected data on treatment and
drug interactions related to hypertension and diabetes
mellitus. A literature search was conducted using
Public Health Reviews, National Library of
Medicine, and Google Scholar, resulting in 7260
articles. However, only 26 articles met the inclusion
criteria and were included in the study.
Figure 1: Article collection using the PRISMA method.
ISCP UTA ’45 JAKARTA 2023 - THE INTERNATIONAL SEMINAR AND CALL FOR PAPER (ISCP) UTA ’45 JAKARTA
258

3
RESULTS AND DISCUSSION
The systematic review analysed several articles and
found evidence of drug use and interactions between
hypertension and diabetes mellitus treatments.
Respondent characteristics, such as age, gender,
antidiabetic treatment, and antihypertensive
treatment, were also studied. According to Susanti
(2021), the majority of patients diagnosed with
hypertension complicated by diabetes mellitus were
female (76%). Hormonal changes resulting from a
higher body mass index, premenstrual syndrome, and
menopause can cause fat to accumulate more easily
in the body. In women, the hormone estrogen is
unable to produce High Density Lipoprotein (HDL),
which can lead to increased blood pressure due to
atherosclerosis. According to research by Apristina et
al. (2023), the majority of respondents in the elderly
category (93.7%) exhibited these characteristics. As
age increases, changes occur that can make a person
more susceptible to various diseases, including
hypertension and diabetes mellitus.
Table 1: Interactions of hypertension and diabetes mellitus drugs.
Hypertension
Medicine
Diabetes
Mellitus
Medicine
Effect Severity
Level
Reference Author
Amlodipine Metformin Amlodipine reduces the effects of
metformin by pharmacodynamic
antagonism and can cause
h
yp
o
g
l
y
cemia
Moderate 1. Abdulkadir et al., (2023)
2. Rahmawaty & Pratiwi, (2022)
3. Murwati & Murtisiwi, (2021)
Ramipril Metformin Ramipril may increase the toxicity of
metformin by an undetermined
interaction mechanism that may
lea
d
to h
yp
o
g
l
y
cemia
Moderate 1. Agus & Permana, (2023)
2. Rahman & Octavia, (2019)
Captopril Metfotmin Captopril can increase the effects
of metformin, thereby increasing
the ris
k
of h
yp
o
g
l
y
cemia
Moderate 1. Rasdianah et al., (2021)
2. Ganga et al., (2022)
Furosemide Metformin Furosemide used with metformin
can cause an increase in metformin
levels in the blood, causing
hypoglycemia
Moderate 1. Muhammad Fajar et al., (2023)
2. Refdanita & Sukmaningsih, (2021)
3. Fitri et al., (2022)
4. (Susanti, 2021)
Captopril Glimepiride Captopril can increase the effects of
glimepiride, causing hypoglycemia
Moderate 1. Sa'adah et al., (2018)
2. Retnowati & Renha Lestari, (2022)
3. Risal et al., (2021)
Bisopropol Glimepiride Bisoporol used with glimepiride can
inhibit the ß-2 receptors in the
pancreas so that it can reduce the
effects of glimepiride and will
cause hyperglycemia.
Moderate 1. Iskandar et al., (2021)
2. Oktaverawati & Susanti, (2020)
3. Amellia & Sumiwi,
4. (2023)
Ramipril Candesartan This interaction has a
pharmacodynamic mechanism and
has a synergistic effect, so it will
potentiate each other's effects. Dual
inhibition of the renin- angiotensin
system may increase the risk of
hypotension, hyperkalemia and
renal impairment
Moderate 1. Oktianti et al., (2023)
2. Suri et al., (2022)
3. Effendi & Harimu, (2022)
4. Momuat & Annisaa', (2023)
Ciprofloxacin Glimepiride Ciprofloxacin increases the effect of
glimepiride synergistically so it is
necessary to monitor blood sugar
levels re
g
ularl
y
Major 1. Tanty et al., (2023)
Systematic Review: Drug Interactions in the Treatment of Hypertension with Diabetes Mellitus
259

Table 1: Interactions of hypertension and diabetes mellitus drugs (cont.).
Hypertension
Medicine
Diabetes
Mellitus
Medicine
Effect Severity
Level
Reference Author
Bisopropol Insulin
Lispro
The use of bisoprolol
(cardioselective beta blocker) with
insulin lispro can increase the risk
of hypoglycemia
Moderate 1. Timur et al., (2022)
2. Dungan et al., (2019)
Bisopropol Metformin Concomitant use of metformin and
b
iso
p
rolol can cause h
yp
o
g
l
y
cemia
Moderate 1. Sormin & Salmaa Qoonitah, (2021)
2.
(
Reskiani et al., 2023
)
1.
DDI Between Amlodipine and Metformin
Combination therapy using Angiotensin II receptor
blocker (ARB) and Calcium-channel blocker (CCB)
is more effective in achieving blood pressure targets.
This therapy can be administered as monotherapy or
in combination. CCBs can cause arterial widening
and are commonly used as antihypertensive drugs.
Additionally, it has been found that it can reduce
resistance in blood vessels, leading to a decrease in
blood pressure (Rahmawaty & Pratiwi, 2022).
According to Abdulkadir et al., the interaction
between metformin and calcium channel blocker
drugs, such as amlodipine, can reduce the
effectiveness of metformin. This is due to a
pharmacodynamic interaction mechanism, which can
cause hypoglycemic effects. To avoid hypoglycemia
and potential drug interactions, it is necessary to
check blood sugar levels before administering this
drug and adjust the insulin dose accordingly
(Abdulkadir et al., 2023).
2.
DDI Between Ramipril and Metformin
Metformin is an oral drug used to lower blood sugar
levels. Due to its cationic nature, it has a high
potential for drug interactions, which can occur via
organic cationic ion transporters in the kidney. When
used in combination with ramipril, metformin can
cause hypoglycemia due to an increase in its blood
sugar-lowering effect. The interaction mechanism
between ramipril and metformin is undetermined
(Agus & Permana, 2023). When administering both
drugs, it is necessary to monitor them closely to avoid
any potential adverse effects and maintain a safe
distance between them (Rahman & Octavia, 2019).
3.
DDI Between Captopril and Metformin
Ganga et al. (2022) suggest that in hypertensive
patients with diabetes, ACEI monotherapy
(Captopril) is the preferred primary therapy due to its
long-term safety and lack of metabolic side effects.
Additionally, ACEI therapy is commonly used
because it provides kidney protection by causing
vasodilation in the renal efferent arterioles and
reducing proteinuria. The combination of metformin
and captopril can increase the risk or severity of lactic
acidosis and hypokalemia. Patients should monitor
their blood glucose levels and recognize early
symptoms of hypoglycemia. Rasdianah et al. (2021)
suggest this solution.
4.
DDI Between Furosemide and Metformin
Furosemide is an antihypertensive drug that can be
combined with metformin. However, this
combination can cause hypoglycemia as furosemide
can increase the plasma concentration of metformin
by 22%. Conversely, metformin can decrease the
concentration of furosemide and its elimination half-
life by 31% and 32%, respectively (Refdanita &
Sukmaningsih, 2021). Metformin belongs to the
biguanide class of drugs and is the first-line treatment
for diabetes. Furosemide, on the other hand, is a loop
diuretic. The two drugs have a minor interaction that
can increase metformin levels, although the
mechanism is not yet understood. It is important to
monitor patients to prevent loss of blood glucose
control. When discontinuing the drug in patients
taking metformin, it is important to monitor their
blood glucose levels to prevent hypoglycemia (Fitri
et al., 2022). To manage the interaction between these
two drugs, the dose should be adjusted and the patient
should be closely monitored for potential irregular
heartbeat issues (Fajar et al., 2023).
5.
DDI Between Captrpril and Glimepiride
The concurrent use of glimepiride and captropil may
have a moderate interaction effect, potentially leading
to changes in the patient's clinical status, additional
treatment, hospitalization, and/or prolonged length of
hospital stay. This is due to the potential for drug
interactions when using antidiabetic and
antihypertensive medications simultaneously, which
can be exacerbated by the patient's overall health
condition. Drug absorption requires monitoring
during use to anticipate unwanted reactions. When
ISCP UTA ’45 JAKARTA 2023 - THE INTERNATIONAL SEMINAR AND CALL FOR PAPER (ISCP) UTA ’45 JAKARTA
260

administering the drug captropil with glimepride, an
ACE inhibitor interaction mechanism can increase
glucose uptake by increasing capillary blood flow in
skeletal muscle. Therefore, the use of captopril can
enhance the effect of glimepiride (Sa'adah et al.,
2018). The combination of these two drugs does not
have a synergistic effect and instead produces a
combination effect that is lower than the effect of
each drug individually (Risal et al., 2021).
6.
DDI Between Bisoprolol and Glimepiride
Administration of beta blockers that selectively
inhibit β-1 is a better choice when given to
hypertensive patients with diabetes or peripheral
circulatory disorders. The use of carvedilol and
bisoprolol is beneficial and recommended for the
treatment of heart failure in combination with ACE
inhibitors, as stated in JNC VI and VII (Iskandar et
al., 2021). Glimepiride is a sulfonylurea drug, and
bisoprolol is a beta-blocker drug. These two drugs
interact through pharmacodynamic mechanisms. The
interaction between these two drugs can cause
hypoglycemia in patients. Beta blockers inhibit
insulin-induced glycogenesis in patients with
diabetes mellitus and delay the recovery of normal
blood glucose levels, leading to a decrease in insulin
secretion. To manage this interaction, it is
recommended to monitor the patient's glucose levels
or replace the antihypertensive with a different class
of drug (Oktaverawati & Susanti, 2020).
7.
DDI Between Candesartan and Ramipril
Suri et al. state that ACE inhibitor drugs and
angiotensin receptor blockers (ARB), including
candesartan and ramipril, have been shown to be
effective in treating hypertension in patients with
complications such as atherosclerosis and diabetes.
Monotherapy may be more effective than
combination therapy in improving blood pressure,
renal function, insulin resistance, and plasma
adipocytokine profile (Suri et al., 2022).
Additionally, the combination of ACEI/ARB with
potassium-sparing diuretics may increase blood
potassium levels and lead to hyperkalemia (Effendi &
Harimu, 2022).
8.
DDI Between Ciprofloxacin and Glimepiride
The combination of ciprofloxacin and glimepiride
can cause severe hypoglycemia, which may lead to
coma or death, particularly in elderly patients and
those with kidney problems. It is important to avoid
using Glimepiride with quinolone class antibiotics. If
therapy cannot be avoided, closely monitoring blood
sugar levels when starting therapy with quinolone
class drugs is necessary (Tanty et al., 2023).
9.
DDI Between Bisoprolol and Insulin Linspro
The moderate severity category suggests that the
effects may be moderate and could lead to organ
damage that requires additional therapy (Timur et al.,
2022). When using selective beta blockers with
insulin, the risk of hypoglycemia is higher than when
using non-selective beta blockers with insulin.
Therefore, monitoring of sugar levels is necessary.
Spacing between bisoprolol and insulin lispro can be
used to minimize the occurrence of hypoglycemia
(Dungan et al., 2019).
10.
DDI Between Metformin and Bisoprolol.
Concomitant use of metformin and bisoprolol may
lead to hypoglycemia. Therefore, it is necessary to
monitor glucose levels or adjust the antidiabetic dose
if required (Sormin & Salmaa Qoonitah, 2021).
Bisoprolol has a positive effect on the pathogenic
mechanisms of arterial hypertension and metabolic
syndrome. Similarly, metformin improves
carbohydrate and lipid metabolism. However, it may
also lower blood pressure and slow the heart rate,
which can cause dizziness (Reskiani et al., 2023).
Pharmacodynamic interactions can often be
extrapolated to other drugs in the same class because
drugs are classified based on their pharmacodynamic
effects. This means that the drug acts on the same
receptor, site of action, or physiological system with
additive, synergistic, or antagonistic effects without
changing plasma levels or other pharmacokinetic
profiles (Murwati & Murtisiwi, 2021). Osoro, Amir,
Vohra, and Sharma (2023) state that patient
compliance is the most significant factor influencing
drug-drug interactions. Monitoring is necessary as
moderate interaction effects can cause changes in
clinical conditions. Moderate interaction events can
occur at any age, but they are more likely to occur in
older patients due to age-related changes in
physiology, increased risk of chronic diseases, and
the use of multiple medications (Abdulkadir et al.,
2023). Regular and routine medication adherence is
crucial for maintaining stable blood pressure and
reducing or preventing physical symptoms,
ultimately improving the patient's quality of life.
Regular and routine medication adherence is crucial
for maintaining stable blood pressure and reducing or
preventing physical symptoms, ultimately improving
the patient's quality of life. It is important to note that
subjective evaluations have been excluded from this
text. Regular and routine medication adherence is
crucial for maintaining stable blood pressure and
reducing or preventing physical symptoms,
Systematic Review: Drug Interactions in the Treatment of Hypertension with Diabetes Mellitus
261

ultimately improving the patient's quality of life.
Tarigan et al. (2022) identified several factors that
influence treatment adherence, including knowledge,
attitudes, information from mass/electronic media,
and family support.
4
CONCLUSIONS
According to the results of a systematic review, the
treatments most commonly used for hypertensive
patients with diabetes mellitus are amlodipine
metformin, metformin ramipril, metformin
bisoprolol, metformin captopril, glimepiride
captopril, furosemide-metformin, bisoprolol-insulin
lispro, and ciprofloxacin glimepiride. Of these,
ciprofloxacin-glimepiride has the greatest potential
effect on hypoglycemia. Meanwhile, the combination
of glimepiride and bisoprolol may lead to
hyperglycemic effects.
To prevent this interaction, a time lag can be
provided when taking the medication. Drug
interactions can occur at any age, but are more likely
in old age due to changes in physiology, increased
risk of chronic diseases, and the need for multiple
medications. Follow the instructions closely to ensure
uniformity in the volume (Moore and Lopes, 1999).
ACKNOWLEDGEMENTS
I would like to express my gratitude to Professor for
their guidance and knowledge throughout this
research project. Their insights have been invaluable
in expanding my understanding and skills in this field.
I am fortunate to have had Professor as my advisor,
and their contributions have been instrumental in
guiding me towards achieving my academic goals.
Thank you for your dedication and patience
throughout this journey. I wish Professor continued
success and happiness in their academic and
professional pursuits.
REFERENCES
Abdulkadir, W. S., Djuwarno, E. N., Rasdianah, N., Akuba,
J., Fauziah Tahir, M., Farmasi, J., Olahraga, F., &
Kesehatan, D. (2023). Potensi Interaksi Obat
Antidiabetes Melitus Tipe-2 dengan Obat
Antihipertensi. Journal Syifa Sciences and Clinical
Research (JSSCR), 5(2), 245–252.
Agus, D., & Permana, S. (2023). Kajian Interaksi Obat
Diabetes Mellitus Tipe II dengan Penyakit Penyerta
Hipertensi di UPTD Puskesmas Cilacap “ X .” Jurnal
Kesehatan Qamarul Huda, 11(1), 335–342.
https://doi.org/10.37824/jkqh.v11i1.2023.483
Amellia, & Sumiwi, S. adi. (2023). Kajian Interaksi Obat
Pada Peresepan Pasien Diabetes Melitus Di Salah Satu
Rumah Sakit Di Kota Bandung. Journal of
Pharmaceutical and Sciences, 6(2), 445–450.
https://www.journal-jps.com
Apristina, A., Nurinda, E., Kusumawardani, N.,
Yugistyowati, A., & Dwinta, E. (2023). Analisis
Hubungan Tingkat Kepatuhan Penggunaan Obat
terhadap Luaran Klinis Pasien PROLANIS Diabetes
Melitus dengan Hipertensi di Puskesmas Minggir pada
Masa Pandemi Covid-19. Pharmaceutical Journal Of
Indonesia, 8(2), 149–155.
Dungan, K., Merrill, J., Long, C., & Binkley, P. (2019).
Effect of beta blocker use and type on hypoglycemia
risk among hospitalized insulin requiring patients.
Cardiovascular Diabetology, 18(163), 1–9.
https://doi.org/10.1186/s12933-019-0967-1
Effendi, F., & Harimu, H. B. (2022). Gambaran Potensi
Interaksi Obat Antihipertensi Oral (Golongan Ace
Inhibitor Dan Angiotensin Receptor Blocker) Pada
Pasien Poli Jantung Rsud Ciawi Bogor. Jurnal
Kesehatan Mahardika, 8(2), 1–9.
https://doi.org/10.54867/jkm.v8i2.59
Fitri, D. R. S., Intiyani, R., & Miyarso, C. (2022).
Gambaran Potensi Interaksi Obat Pada Pasien Diabetes
Melitus Tipe 2 Di Instalasi Rawat Jalan PKU
Muhammadiyah Sruweng. Jurnal Farmasi Klinik Dan
Sains, 2(2), 20–26.
Gangga, I. M. P., Wintariani, N. P., & Apsari, D. P. (2022).
Pola Penggunaan Obat Antihipertensi Pasien Hipertensi
Dan Hipertensi Dengan Diabetes Militus Di Puskesmas
Selemadeg Timur II Tabanan. Widya Kesehatan, 4(2),
20–27.
https://doi.org/10.32795/widyakesehatan.v4i2.3388
Iskandar, H., Adelia, D., & Muharomah, A. (2021).
Gambaran
Potensi Interaksi Obat Hipertensi di Instalasi Farmasi Rawat
Jalan Rumah Sakit Metropolitas Medical Centre
Periode Oktober - Desember 2018. Jurnal Farmasi
IKIFA, 1(1)(1), 1–9.
Madania, Rasdianah, N., Dalu, M. C., & Pakaya, M. (2022).
Potensi Interaksi Obat Pasien Hipertensi Dan Diabetes
Melitus Tipe 2 Di Instalasi Rawat Jalan Rsud Toto
Kabila. JMTS: Jurnal Mitra Teknik Sipil, 5(1), i.
https://doi.org/10.24912/jmts.v5i1.17649
Momuat, A. G. F., & Annisaa’, E. (2023). Evaluasi
Rasionalitas Penggunaan Antihipertensi Golongan
Angiotensin II Receptor Blocker (ARB) pada Pasien
Penyakit Ginjal Kronis. Generics: Journal of Research
in Pharmacy, 3(1), 55–64.
https://doi.org/10.14710/genres.v3i1.17210
Muhammad Fajar, Umi Yuniarni, & Ratu Choesrina.
(2023). Pola Penggunaan dan Interaksi Obat
Antidiabetes dan Antihipertensi pada Pasien Diabetes
Melitus Tipe 2 dengan Komplikasi Hipertensi di RSUD
Subang. Bandung Conference Series: Pharmacy, 327–
334. https://doi.org/10.29313/bcsp.v3i2.8753
ISCP UTA ’45 JAKARTA 2023 - THE INTERNATIONAL SEMINAR AND CALL FOR PAPER (ISCP) UTA ’45 JAKARTA
262

Murwati, I. S., & Murtisiwi, L. (2021). Identifikasi Potensi
Interaksi Obat pada Peresepan Pasien Rawat Jalan
Diabetes Melitus Tipe 2 dengan Hipertensi di RSUD dr.
Soediran Mangun Sumarso Wonogiri. Jurnal Farmasi
(Journal of Pharmacy), 10(1), 38–45.
https://doi.org/10.37013/jf.v10i1.119
Nurlinda, Diniarti, F., & Wulandar. (2022). Determinan
Kejadian Hipertensi Di Rumah Sakit Umum Daerah
Kabupaten Kaur Tahun 2021. Journal Hygea Public
Health, 1(1), 29–36.
Oktaverawati, M., & Susanti, E. (2020). Kajian Interaksi
Obat Pada Peresepan Pasien Diabetes Melitus Dengan
Komplikasi Hipertensi Di Apotek Rawat Jalan Jkn
Rumah Sakit Dr. Saiful Anwar Malang. Akademi
Farmasi Putra Indonesia Malang, Dm.
Oktianti, D., Septina Widyadewi, P. P., & Wati, D. R.
(2023). Identfikasi Potensi Interaksi Obat
Antihipertensi Pada Pasien Rawat Jalan Di Rs X
Denpasar Periode Oktober-Desember 2021.
INPHARNMED Journal (Indonesian Pharmacy and
Natural Medicine Journal), 6(2), 82.
https://doi.org/10.21927/inpharnmed.v6i2.2578
Osoro, I., Amir, M., Vohra, M., & Sharma, A. (2023).
Pharmacist Interventions in Minimizing Drug Related
Problems in Diabetes With Co-Existing Hypertension:
A Five-Year Overview and Ground Report From India.
International Journal of Public Health, 68(April), 1–7.
https://doi.org/10.3389/ijph.2023.1605808
Pan American Health Organisation. (2023). Hypertension.
Pan American Health Organisation.
https://www.paho.org/en/enlace/hypertension
Pulungan, R. M., Helda, H., & Amar, M. I. (2022). Risk
Factors for Hypertension Incidence Among Women in
Indonesia. Malaysian Journal of Public Health
Medicine, 22(3), 310–
318.
https://doi.org/10.37268/MJPHM/VOL.22/NO.3/ART.
1688
Rahman, H., & Octavia, T. A. (2019). Kajian Interaksi Obat
Metformin pada Pasien Diabetes Mellitus. Jurnal
Farmasetis, 8(2), 55–58.
https://doi.org/10.32583/farmasetis.v8i2.592
Rahmawaty, A., & Pratiwi, Y. (2022). Kajian Drug Related
Problems (DRPs) Interaksi Obat dalam Peresepan
Polifarmasi pada Pasien Prolanis di Fasilitas Kesehatan
Dasar Dokter X Kabupaten Kudus. Cendekia Journal of
Pharmacy, 6(1), 13–25.
https://doi.org/10.31596/cjp.v6i1.158
Rasdianah, N., Hiola, F., Suryadi, A. M. A., & Gani, A. S.
W. (2021). Interaksi Obat Pada Pasien Diabetes Melitus Tipe
2 Dengan Penyakit Penyerta Di Rumah Sakit Otanaha
Kota Gorontalo. Indonesian Journal of Pharmaceutical
Education, 1(1), 40–46.
https://doi.org/10.37311/ijpe.v1i1.9953
Rasdianah, N., & Pakaya, M. (2023). Studi Interaksi Obat
Pasien Diabetes Melitus Tipe 2 dengan penyakit
penyerta : Studi Kasus Rumah Sakit X Gorontalo.
Journal Syifa Sciences and Clinical Research
, 5(1),
192–199.
https://ejurnal.ung.ac.id/index.php/jsscr/article/view/87
31/6333
Refdanita, & Sukmaningsih, V. (2021). Potensi Interaksi
Obat Pasien Diabetes Melitus Tipe-2 dengan Hipertensi
di Rumah Sakit “ X ” Periode 2019. Sainstech Farma,
14(1), 47–53.
Reskiani, M., Salam, M. R., & Idrus, I. (2023). Gambaran
Peresepan Obat Antihipertensi dan Interaksi Obat Pada
Pasien BPJS DI APotek Kimia Farma 479 Kendari.
Jurnal Pelita Sains Kesehatan, 3(3), 84–92.
https://ojs.pelitaibu.ac.id/index.php/jpasaik
Retnowati, E., & Renha Lestari, D. (2022). Hubungan
Kombinasi Oral Diabetes dan Hipertensi terhadap
Interaksi Obat pada Pasien Rawat Jalan Puskesmas
Kendung. URECOL, 458–468.
Risal, A., Khusna, K., & Pambudi, R. S. (2021). Interaksi
Obat Hipoglikemia Oral (OHO) dengan Obat Lain pada
Pasien Diabetes Mellitus Tipe II berdasarkan
Farmakokinetik dan Farmakodinamik di Puskesmas
Sangkrah. 1st E-Proceeding SENRIABDI 2021, 1(1),
979–990.
Rosyadi, A. (2022). Evaluasi Pola Peresepan Obat Pasien
Hipertensi Dengan Diabetes Mellitus Pada Pasien
Geriatri Pengguna JKN. Jurnal Bina Cipta Husada,
18(2), 45–58.
Sa’adah, F. Z., Lestari, F., & Yuniarni, U. (2018). Kajian
Probabilitas Interaksi Obat Antidiabetes Golongan
Sulfonilurea di Satu Rumah Sakit Swasta Kota
Bandung. Prosiding Farmasi, 2(2), 509–515.
Simanjuntak, E. Y., & Amazihono, E. (2023). Kepatuhan
Pengobatan Dengan Kualitas Hidup Pasien Hipertensi.
Jurnal Keperawatan, 6(3), 1–9.
Sormin, I. P., & Salmaa Qoonitah. (2021). Analisis
Interaksi Obat Pasien Diabetes Melitus Tipe-2 Dengan
Komplikasi Hipertensi Di Instalasi Rawat Jalan Rumah
Sakit “ X .” Social Clinical Pharmacy Indonesia
Journal, 46(100), 1– 10.
Suri, N., Mulyaningsih, D. W., & Melani, D. (2022).
Evaluasi Permasalahan Terkait Obat Pada Pasien Gagal
Ginjal Kronik Dengan Komplikasi Hipertensi Dan
Diabetes Melitus Tipe II Di Rumah Sakit Umum Daerah
Provinsi Lampung. Jurnal Ilmu Kedokteran Dan
Kesehatan, 9(3), 1063–1072.
https://doi.org/10.33024/jikk.v9i3.7909
Susanti, I. (2021). Evaluasi Interaksi Obat Pada Pasien
Geriatri dengan Diabetes Melitus dan Hipertensi. Jurnal
Media Komunikasi Ilmu Kesehatan, 13(02), 191–195.
Tanty, H. N., Charles, Meryta, A., & Zufitasari, A. (2023).
Potensi Interaksi Obat Pada Pasien Geriatri Penderita
Diabetes Melitus Di RS “X” Periode Januari-Maret
2022. Jurnal Farmasi IKIFA,
2(1), 31–41.
Tarigan, J. A., Ketaren, S. O., Tarigan, F. L., Nababan, D.,
Manurung, K., & Sitorus, M. E. J. (2022). Faktor yang
Berhubungan dengan Tingkat Kepatuhan Pasien
Dengan Penyakit Penyerta Diabetes Mellitus Dan
Hipertensi Terhadap Penerapan Protokol Kesehatan Di
UPT. Puskesmas PB. Selayang II. PREPOTIF Jurnal
Kesehatan Masyarakat, 6(2), 1639.
http://journal.universitaspahlawan.ac.id/index.php/prep
otif/article/view/5020%0Ahttp://journal.universitaspah
Systematic Review: Drug Interactions in the Treatment of Hypertension with Diabetes Mellitus
263

lawan.a
c.id/index.php/prepotif/article/download/5020/4305
Timur, W. W., Ussa, R. E., & Widyaningrum, N. (2022).
Kajian Interaksi Antar Obat Terhadap Profil Glikemik
Pada Pasien Diabetes Rawat Inap Rumah Sakit Islam
Sultan Agung Semarang. Pharmacon: Jurnal Farmasi
Indonesia, 19(2), 221–227.
https://doi.org/10.23917/pharmacon.v19i2.18583
Wati, F. R., Afiani, N., & Qodir, A. (2021).
Hubungan Kepatuhan Konsumsi Obat Terhadap
Kualitas Hidup Pasien Hipertensi Dengan Penyerta
Diabetes Mellitus. Media Husada Journal of Nursing
Science, 2(2), 28–34.
World Health Organisation (WHO). (2023).
Hypertension. World Health
Organisation (WHO).
https://www.who.int/news-room/fact-
sheets/detail/hypertension
Suri, N., Mulyaningsih, DW, & Melani, D. (2022).
Evaluation of Drug-Related Problems in Chronic
Kidney Failure Patients with Complications of
Hypertension and Type II Diabetes Mellitus at the
Regional General Hospital of Lampung Province.
Journal of Medicine and Health Sciences, 9(3), 1063–
1072. https://doi.org/10.33024/jikk.v9i3.7909
Susanti, I. (2021). Evaluation of Drug Interactions in
Geriatric Patients with Diabetes Mellitus and
Hypertension. Journal of Health Sciences
Communication Media, 13(02), 191–195.
Tanty, H.N., Charles, Meryta, A., & Zufitasari, A. (2023).
Potential Drug Interactions in Geriatric Patients
Suffering from Diabetes Mellitus at "X" Hospital for the
Period January-March 2022. IKIFA Pharmacy Journal,
2(1), 31–41.
Tarigan, JA, Ketaren, SO, Tarigan, FL, Nababan, D.,
Manurung, K., & Sitorus, MEJ (2022). Factors
Associated with the Level of Compliance of Patients
with Comorbidities Diabetes Mellitus and Hypertension
to the Implementation of Health Protocols at UPT. PB
Health Center. Selayang II. PREPOTIF Public Health
Journal, 6(2), 1639.
http://journal.universitaspahlawan.ac.id/index.php/pre
potif/article/view/5020%0Ahttp://journal.universitaspa
h lawan.ac.id/index.
php/prepotif/article/download/5020/4305
Timur, WW, Ussa, RE, & Widyaningrum, N. (2022). Study
of Interactions Between Drugs on Glycemic Profiles in
Inpatient Diabetes Patients at Sultan Agung Islamic
Hospital, Semarang. Pharmacon: Indonesian
Pharmaceutical Journal, 19(2), 221–227.
https://doi.org/10.23917/pharmacon.v19i2.18583
Wati, FR, Afiani, N., & Qodir, A. (2021). The Relationship
between Compliance with Medication Consumption
and Quality of Life in Hypertension Patients with
Diabetes Mellitus. Media Husada Journal of Nursing
Science, 2(2), 28–34.
World Health Organization (WHO). (2023). Hypertension.
World Health Organization (WHO).
https://www.who.int/news- room/fact-
sheets/detail/hypertension
ISCP UTA ’45 JAKARTA 2023 - THE INTERNATIONAL SEMINAR AND CALL FOR PAPER (ISCP) UTA ’45 JAKARTA
264
