
3D Virtual Model Simulation: Applications for Dento-Facial
Deformities
Yassir Sabri
1
, Zaoui Fatima
2
, Boudi El Mostapha
3
and Benyahia Hicham
2
1
PhD Student CEDOC SVS, Faculty of Dentistry, Mohammed V University in Rabat, Morocco
2
Department of Orthodontics, Faculty of Dentistry, Mohammed V University in Rabat, Morocco
3
Department of Mechanical Engineering, Mohammadia School of Engineering, Mohammed V University in Rabat,
Morocco
Keywords: Biomechanical FEM Simulation, DICOM, 3D Modelling, Orthodontic Tooth Movement, Biomechanics.
Abstract: Nowadays, virtual treatment planning allows clinicians to create detailed, patient-specific workflows through
digital simulations. This improves the accuracy of treatment plans and leads to an efficient, and patient-centric
care. In dentistry, Computer-Aided Design and Computer-Aided Manufacturing CAD/CAM systems enable
digital design and fabrication of a all kind of oral devices like surgical guides for implant placement, or
orthodontic clear aligners. In the present paper, a 3D model will be created in order to be used to understand
orthodontic loadings effects on tooth movement and adjacent structures. Material and method: Cranio-facial
imaging data (Dicom) was used to creat a 3D model of a partial dento-alveolar model. All materials (teeth,
PDL and alveolar bone) were considered having isotropic linear elastic properties. Results: the 3 D model
will be used to realize a simulation by finite element method using more than 77158 second-order Lagrangian
tetrahedral elements. Discussion & Conclusion: The application of 3D virtual model in the context of dento-
facial deformities offers numerous advantages for diagnosis, treatment planning, and patient communication,
clinicians may be able to develop more effective and mechanically sound treatments with the use of numerical
simulation.
1 INTRODUCTION
In recent years, the integration of digital technologies
in the medical field has revolutionized patient care.
Advanced digital tools provide healthcare
professionals with a powerful means to simulate and
address various medical situations (J. S. Shinbane and
L. A. Saxon, 2018), (P. Riutord-Sbert et al., 2023).
In dentistry, there are many applications based on
digital technologies, in particular virtual treatment
planning, meaning the ability for dental clinicians to
create detailed, patient-specific workflows. This not
only improves the accuracy of treatment plans but
also allows for a more personalized approach, and for
efficient, and patient-centric care (J. S. Shinbane and
L. A. Saxon, 2018), (“Aplicación del metaverso como
técnica de aprendizaje en el grado de odontología.
Estudio preliminar”), (L. Camardella et al., 2016).
Digital radiography, including intraoral and
extraoral X-rays in particular: Cone Beam Computed
Tomography (CBCT), provides three-dimensional
images of oral structures, enabling detailed
assessment for treatment planning in areas like
implant placement, oral surgery, and orthodontics (R.
Urban et al., 2023), (H. W. Moon et al., 2020).
Computer-Aided Design and Computer-Aided
Manufacturing CAD/CAM systems enable the digital
design and fabrication of classical dental restorations
such as crowns, bridges, and veneers, as well as a new
array of oral devices like surgical guides for implant
placement, or orthodontic clear aligners (A.
Skorulska et al., 2021).
The application of 3D virtual model in the context
of dento-facial deformities offers numerous
advantages for diagnosis, treatment planning, and
patient communication. Surgeons and orthodontists
can use 3D virtual model for digital simulations based
on High-resolution imaging providing detailed
representations of teeth and craniofacial structures to
create patient-specific treatment plans.
The aim of our study is to generate a dento-
alveolar virtual model from acurate imaging data
(Dicom).
Sabri, Y., Fatima, Z., El Mostapha, B. and Hicham, B.
3D Virtual Model Simulation: Applications for Dento-Facial Deformities.
DOI: 10.5220/0012866300003854
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International e-Health Forum (IeHF 2023), pages 25-28
ISBN: 978-989-758-711-5
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
25

Figure 1: Different applications of digital technologies in
Dentistry.
2 MATERIAL AND METHODS
2.1 DICOM Data
A maxilla cone beam CT file (in DICOM format) was
selected from imaging database of orthodontic
department (CCTD CHIS Rabat), respecting several
criteria: no previous orthodontic or orthopedic
treatment histories, no craniofacial anomalies, no
previously reported or observed dental treatment or
anatomical defects on the canine incisors segment.
Table 1: Mechanical Proprieties of Materials.
Anatomic element
Young’s
module
(MPa)
Poisson’s
coefficient
Thickness
(mm)
Bone
2000
0.30
Periodontal ligament
0,68
048
0.2
Tooth
20000
0.15
Material of bracket
200000
0.3
The conebeam selected belong to a 13-year-old
girl, who was treated for maxillary bilateral second
premolars impaction (Conebeam equipment:
resolution of approximately 150-300m/pixel. Myray
Hyperion X9 3d, NNT viewer was utilised to process
the CT images).
Figure 2: CT images captured in DICOM format and ROI.
2.2 3D Modelling
Region of interest (ROI): for this preliminary study,
we focused on left maxillary canine and incisors, a
segment of three teeth: 2.1., 2.2., 2.3 as shown in
fig.1. It’s a simple partial model to test orthodontic
load on a single tooth (2.2) and reaction effects on
adjacent ones.
The CT images were segmented on invesalus
software*, by defining thresholds separately for both
teeth and bone based on their respective Hounsfield
unit (HU). 2 masks (STL format) were then created
and further processed on Catia v5 (*), to create the 3D
solid model.
The process consists of several stages: including
surface refinement, mask filling, PDL modelling by
virtual reconstruction from the external radicular
surface of teeth, and orthodontic brackets design.
3 RESULTS
Figure 3: Decomposition of study system.
IeHF 2023 - International e-Health Forum
26
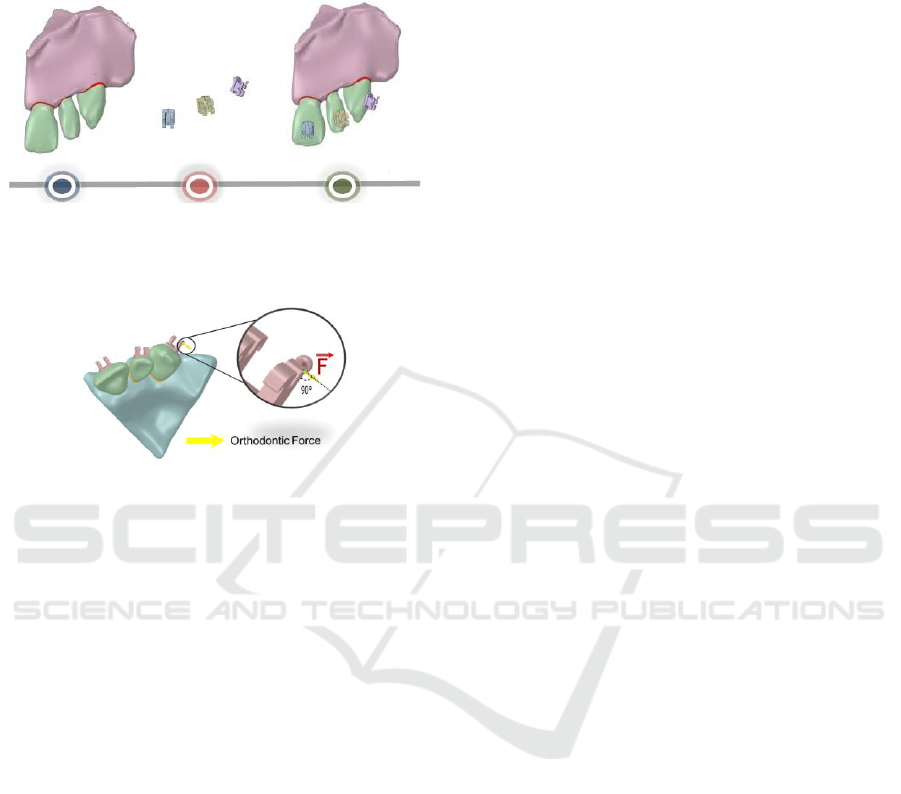
The 3D model will be used to realize a simulation
by finite element method using more than 77158
second-order Lagrangian tetrahedral elements.
Figure 4: Study model with bracket.
We will apply a force of 2N to study dentofacial
deformities.
Figure 5: Preliminary study: distal orthodontic force on
canine bracket.
4 CONCLUSIONS
The applications of 3D virtual model in order to
realize FE simulation will help us to study dento-
facial deformities for advancement in treatment
planning and patient care.
As technology continues to advance, the potential
for virtual simulations in medical and dental
treatment remains limitless, promising a future of
healthcare where innovation and precision converge
for the benefit of patients and practitioners.
REFERENCES
J. S. Shinbane and L. A. Saxon, “Virtual medicine:
Utilization of the advanced cardiac imaging patient
avatar for procedural planning and facilitation,”
Journal of Cardiovascular Computed Tomography,
vol. 12, no. 1. Elsevier Inc., pp. 16–27, Jan. 01, 2018.
doi: 10.1016/j.jcct.2017.11.004.
P. Riutord-Sbert et al., “Aplicación del metaverso como
técnica de aprendizaje en el grado de odontología.
Estudio preliminar,” Academic Journal, 2023, doi:
10.3306/AJHS.2023.38.02.43.
“Aplicación del metaverso como técnica de aprendizaje en
el grado de odontología. Estudio preliminar”.
L. Camardella, E. Rothier, O. Vilella, E. Ongkosuwito, and
K. Breuning, “Virtual setup: application in orthodontic
practice.,” Journal of Orofacial
Orthopedics/Fortschritte der Kieferorthopadie, vol. 77,
no. 6, 2016.
(R. R. Urban et al., “AI-Assisted CBCT Data Management
in Modern Dental Practice: Benefits, Limitations and
Innovations,” Electronics (Switzerland), vol. 12, no. 7.
MDPI, Apr. 01, 2023. doi:
10.3390/electronics12071710.
H. W. Moon et al., “Molar inclination and surrounding
alveolar bone change relative to the design of bone-
borne maxillary expanders: A CBCT study,” Angle
Orthodontist, vol. 90, no. 1, pp. 13–22, 2020, doi:
10.2319/050619-316.1.
A. Skorulska, P. Piszko, Z. Rybak, M. Szymonowicz, and
M. Dobrzyński, “Review on polymer, ceramic and
composite materials for cad/cam indirect restorations in
dentistry—application, mechanical characteristics and
comparison,” Materials, vol. 14, no. 7. MDPI AG, Apr.
01, 2021. doi: 10.3390/ma14071592.
A. Geramy, K. Tanne, M. Moradi, H. Golshahi, and Y.
Farajzadeh Jalali, “Finite element analysis of the
convergence of the centers of resistance and rotation in
extreme moment-to-force ratios,” Int Orthod, vol. 14,
no. 2, pp. 161–170, 2016, doi:
10.1016/j.ortho.2016.04.001.
P. M. Cattaneo, M. Dalstra, and B. Melsen, “The finite
element method: A tool to study orthodontic tooth
movement,” J Dent Res, vol. 84, no. 5, pp. 428–433,
2005, doi: 10.1177/154405910508400506.
Y. Qian, Y. Fan, Z. Liu, and M. Zhang, “Numerical
simulation of tooth movement in a therapy period,”
Clinical Biomechanics, vol. 23, no. SUPLL.1, pp. 48–
52, 2008, doi: 10.1016/j.clinbiomech.2007.08.023.
A. Bouton, Y. Simon, F. Goussard, L. Teresi, and V.
Sansalone, “New finite element study protocol: Clinical
simulation of orthodontic tooth movement,” Int Orthod,
vol. 15, no. 2, pp. 165–179, 2017, doi:
10.1016/j.ortho.2017.03.001.
W. Ryniewicz et al., “Three-dimensional finite element
simulation of intrusion of the maxillary central incisor,”
Biocybern Biomed Eng, vol. 36, no. 2, pp. 385–390,
2016, doi: 10.1016/j.bbe.2016.02.003.
J. Chen, W. Li, M. V. Swain, M. Ali Darendeliler, and Q.
Li, “A periodontal ligament driven remodeling
algorithm for orthodontic tooth movement,” J Biomech,
vol. 47, no. 7, pp. 1689–1695, 2014, doi:
10.1016/j.jbiomech.2014.02.030.
A. Manmadhachary, Y. Ravi Kumar, and L. Krishnanand,
“Improve the accuracy, surface smoothing and material
adaption in STL file for RP medical models,” J Manuf
Process, vol. 21, pp. 46–55, 2016, doi:
10.1016/j.jmapro.2015.11.006.
J. H. Marangalou, F. Ghalichi, and B. Mirzakouchaki,
“Numerical simulation of orthodontic bone
remodeling,” Orthodontic Waves, vol. 68, no. 2, pp. 64–
71, 2009, doi: 10.1016/j.odw.2008.12.002.
3D Virtual Model Simulation: Applications for Dento-Facial Deformities
27

J. P. Gomez, F. M. Peña, V. Martínez, D. C. Giraldo, and
C. I. Cardona, “Initial force systems during bodily tooth
movement with plastic aligners and composite
attachments: A three-dimensional finite element
analysis,” Angle Orthodontist, vol. 85, no. 3, pp. 454–
460, 2015, doi: 10.2319/050714-330.1.
A. Hohmann et al., “Periodontal ligament hydrostatic
pressure with areas of root resorption after application
of a continuous torque moment: A study using identical
extracted maxillary human premolars,” Angle
Orthodontist, vol. 77, no. 4, pp. 653–659, 2007, doi:
10.2319/060806-234.
A. M. Schwarz, “Tissue changes incidental to orthodontic
tooth movement,” Kokubyo-Gakkai-Zasshi, vol. 6, no.
3, pp. 226–228, 2017, doi:
10.5357/koubyou1927.6.3_226.
IeHF 2023 - International e-Health Forum
28
