
Implementation of Health Information Systems at Health Centres
and Health Offices in Ciamis District
Wawan Ridwan
*
, Lukman Hakim, Gurendro Putro, Ristrini Ristrini, Rustika Rustika
and Dede Anwar Musadad
National Research and Innovation Agency, Bogor, Indonesia
Keywords: Community Health Centres, Health Information System, HIS Implementation.
Abstract: The Indonesian Ministry of Health recently introduced the health information system (HIS) to record and
report health programs, including at community health centres (CHCs) and the district health office.
Therefore, this study aimed to examine the implementation of HIS in CHCs and the Ciamis District Health
Office. This was a descriptive quantitative study with a secondary data analysis approach. The data used were
obtained from Risfaskes results, HIS implementation documents, and HIS staff information. Subsequently,
analysis was carried out using Wallace Foundation guidelines in Workbook B; Secondary Data Analysis. The
analysis showed that HIS had been implemented in 37 CHCs and the Ciamis District Health Office. However,
some CHCs had not consistently implemented all HIS applications as intended. The flow of data and
information between CHCs and the district health office and from the district health office to higher levels
lacked a one-data and one-door system due to variations in the implementation across different programs and
fields. The implementer of HIS was the personnel assigned to each health program that used the system. Some
CHCs had not implemented the use of HIS in the Ciamis District. Furthermore, the existence of this HIS had
not been able to facilitate the work and burden of CHCs.
1 INTRODUCTION
The health sector has rapidly implemented and
developed information and communication
technology (ICT), as evidenced by the widespread
adoption of e-health in various countries. WHO
defines e-health as the cost-effective and secure use
of information and communications technologies in
support of health and health-related fields, including
healthcare services, health surveillance, health
literature, and health education, knowledge and
research. Furthermore, e-health is characterized by
the utilization of ICT to enhance the flow of
information through electronic channels, thereby
strengthening health services and the management of
healthcare systems. This concept is not only related
to the technical aspects but also encompasses
attitudes and mindsets that extend beyond the
purview of local and national healthcare services,
such as regional and world interests (Union 2012).
In Indonesia, the adoption of e-health is marked
by the establishment of a health information system
(HIS). This concept is defined as an intricate
arrangement that encompasses data, information,
indicators, procedures, devices, technology, and
human resources (HR). The components are
intricately linked and managed using an integrated
approach to guide actions or decisions geared towards
supporting health development (Menkes RI 2014)
HIS is a pivotal component of the healthcare
infrastructure of a country and it affects the prevailing
government system. Furthermore, HIS serves as the
backbone of e-Health, as it involves systematic and
integrated management of health data and
information at all levels of government to improve
healthcare services provided to the community
(Soemitro 2016). Information systems can be defined
as organizational frameworks that incorporate a blend
of people, facilities, technology, media, procedures,
and controls. These elements work together to
establish communication channels, process routine
transactions, ensure signal management, manage
internal and external events, and provide a foundation
of information for intelligent decision-making
(Vondewi, R 2010). The development process
involves the creation of a new system to completely
replace the old variants or improve the existing
56
Ridwan, W., Hakim, L., Putro, G., Ristrini, , Rustika, and Musadad, D. A.
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District.
DOI: 10.5220/0012898800004564
In Proceedings of the 5th International Conference on Social Determinants of Health (ICSDH 2023), pages 56-69
ISBN: 978-989-758-727-6; ISSN: 2975-8297
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)

variants (Kinasih 2011). Several reports have shown
that the implementation of HIS still faces various
problems, including unintegrated and uncoordinated
data and information management activities. These
conditions often lead to overlapping data collection
and processing activities, both at the centre and in the
regions (Rondo, Pelealu, and Maramis 2013).
The development of the Ministry of Health's HIS
began in 1982 with the establishment of the Data
Collection and Processing Division within the
Planning Bureau (now the Data and Information
Center) (Soemitro 2016). At this time, there were 3
(three) managerial models, namely (1) manual
management by recording and reporting using
register books, cards, and forms, (2) offline
computerized management, which was mainly
carried out with computer devices, either by using
management information system (SIM) applications
or ordinary electronic office applications. However, it
lacked support from online internet networks
connecting the district/city and the provincial health
office, as well as national health data banks, (3) online
computerized HIS management, which was mostly or
entirely carried out with computer devices, using SIM
applications. It was connected online through the
internet network to the district and the provincial
health office, and national health data banks, to
facilitate communication and data synchronization
(Menkes RI 2012).
One of the healthcare facilities that has embraced
e-Health is CHCs (Puskesmas), leading to the
implementation of the Puskesmas Management
Information System (SIMPUS) at this level. SIMPUS
is designed to provide information that aids the
decision-making process in carrying out Puskesmas
management and achieving its target activities.
Furthermore, it takes the form of web-based software
that is connected to the system in the health
department (Perwira 2012). The use of SIMPUS by
employing ICT holds the potential to significantly
enhance the operational capabilities of community
health centres (CHCs). The system empowers
puskesmas to efficiently coordinate both public
health efforts (UKM) and individual health efforts
(UKP) by prioritizing promotive and preventive
initiatives, to elevate the level of public health
(Menkes RI 2014).
The use of manual systems within certain CHCs
has led to the occurrence of various problems. In the
handling of patient data, there has been a notable
prevalence of errors during processing (registration
data, examination data, referral data, and laboratory
data). Moreover, the patient service process has been
hindered by slow data retrieval within the registers.
These challenges can be addressed through the use of
SIMPUS, which leverages computer technology in
processing data. The advantages of this system
include expediting services, enhancing information
accuracy, swift data searches, quicker report
generation, and uniformity of information system,
leading to improved healthcare service (Wibisono
and Munawaroh 2012). SIMPUS incorporates a
standardized data structure for reporting across health
centres at the district/city level. This standardized
approach offers the dual benefits of swiftness and
precision in data and information processing (Wijaya,
Ifada, and Jauhari 2009).
Apart from SIMPUS, other HISs have also been
implemented at CHCs, including (1) health centre
records consisting of 4 items, (2) primary care
(Pcare), (3) health facilities information system
(HFIS), (4) BPJS non-capitation claims, and (5)
Puskesmas report, consisting of 7 items
(Balitbangkes, 2019). Several studies have shown
that the comprehensive adoption of SIMPUS remains
uneven across different CHCs due to challenges
encountered in various regions. Consequently,
various puskesmas still opt for the traditional
approach of data reporting, using manual procedures.
A review of the implementation of the computer-
based SIMPUS showed that its application yielded
considerable benefits. These include enhanced
performance, and accuracy, as well as time and
energy efficiency but some individuals considered its
implementation an additional workload for officers
(Putri 2013). This challenge can be addressed by
assigning special personnel with appropriate
expertise, namely information technology to manage
the application (Abdul 2003). The existing personnel
at Puskesmas conform to the stipulation of Law No.
36 of 2014 concerning Health Workers, which consist
of health workers and assistants, as well as non-health
workers who perform administrative duties.
The achievement of health program objectives,
which encompass indicators of life expectancy,
mortality, morbidity, and nutritional status of the
community, hinges on the establishment and
development of District ICIS, tailored to align with
the principle of centralization or regional autonomy
in the healthcare domain. The implementation of
district HIS holds immense significance, as it serves
as a mechanism for furnishing indicators that measure
the realization of a healthy district, while also serving
as a fundamental framework for health-oriented
regional development. Anticipated outcomes from
the data and information produced by the HIS include
bolstering the formulation of regional development
plans, providing analytical insight to support budget
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
57
allocation, aiding resource development, and guiding
policymakers during decision-making.
The management of HIS at the Ciamis District
Health Office is carried out by the Planning
Subdivision of the Information Program and Public
Relations Subdivision. One of their key
responsibilities is to collect, process, and present data,
information, programs, and activities within the
Health sector. HIS activities are also carried out by
program implementers in certain regions. Meanwhile,
HIS management at CHCs is entrusted to the
discretion of the head of each Puskesmas (Dinas
Kesehatan Kabupaten Ciamis 2019).
The mandatory adoption of HIS in Indonesia
commenced with the Regulation of the Minister of
Health Republic of Indonesia Number 18 of 2022
concerning the implementation of one health sector
data through HIS (Kemenkes RI 2022). The World
Health Organization (WHO) defines e-health as the
cost-effective and secure use of ICT to support
health-related fields, including health services,
surveillance, literature, education, knowledge, and
study. Clear evidence exists on the growing impact of
e-Health on the delivery of healthcare services across
the work in terms of improved delivery, effectiveness,
and responsiveness to the needs and expectations of
the community (WHO Eastern Mediterranean 2023).
Therefore, this study aims to develop policy
recommendations for the implementation of HIS to
support electronic recording and policy reporting at
CHCs and the Ciamis District Health Office..
2 METHOD
This was a descriptive quantitative study, with a
secondary data analysis approach. The data used were
obtained from Health Facility Research (Risfaskes),
HIS implementation documents, and a dataset on HIS
staff. Furthermore, the secondary data consisted of
the results of the 2019 Risfaskes in Ciamis District,
documents on the implementation of HIS and the
types of HIS that had been implemented, personnel
implementing HIS, and personnel with educational
background or information technology training.
Confirmation was carried out on the implementation
of HIS at several CHCs and the Ciamis District
Health Office. This process was expected to provide
information on the operation of HIS, including the
data flow system from the Puskesmas to the health
office.
Analysis was carried out using the Wallace
Foundation guidelines in Workbook B; Secondary
Data Analysis, and the results were presented in a
tabular form.
3 RESULTS
3.1 General Data of Ciamis District
Ciamis was one of the districts in West Java Province,
consisting of 27 sub-districts, 258 villages, and 7
villages. Furthermore, its geographical position was
at the coordinates of 1080 20' to 1080 40' East
Longitude and 70 40' 20" to 70 41' 20" South Latitude
(BPS Ciamis, 2019).
Table 1. General Description of Ciamis District.
Indicators Numbers/Values
Total Area
1.434 Km
2
Number of Subdistrict
27 Sub-distric
t
Number of Villages
265 Villa
g
es
Total Population
1.418.301 Peoples
Number of Households
496.893
Households
Average Souls/Households
2,9 Souls/
Households
Population Density per km
2
989,1 Soul/K
m
2
Dependent Load Ratio
45,6 Per 100
productive
p
opulation
Sex Ratio
100,7
Population 15 Years Old
1.156.401 Peoples
Population 15 years old
with no primary school
certificate
263.875 Peoples
Ciamis district had a land area of 1,433.10 km
2
with a total population of 1,418,301 people from
406,893 households in 2019 (DHO Kab Ciamis,
2020). This indicated that the population density was
989.1 people per km2, with a household density of 2.9
people per household. Among 1,156,401 individuals
aged >15 years, a total of 263,875 (22.82%) did not
have a primary school certificate, while 991,107
people (77.18%) had a certificate. The highest level
of education possessed by individuals aged >15 years
was elementary/middle school education, namely
597,117 people (60.25%), with the least being a
master's or doctoral degree among 1,747 people
(0.18%). The results showed that there was no data on
vocational high school graduates, as shown in Table
1.
ICSDH 2023 - The International Conference on Social Determinants of Health
58
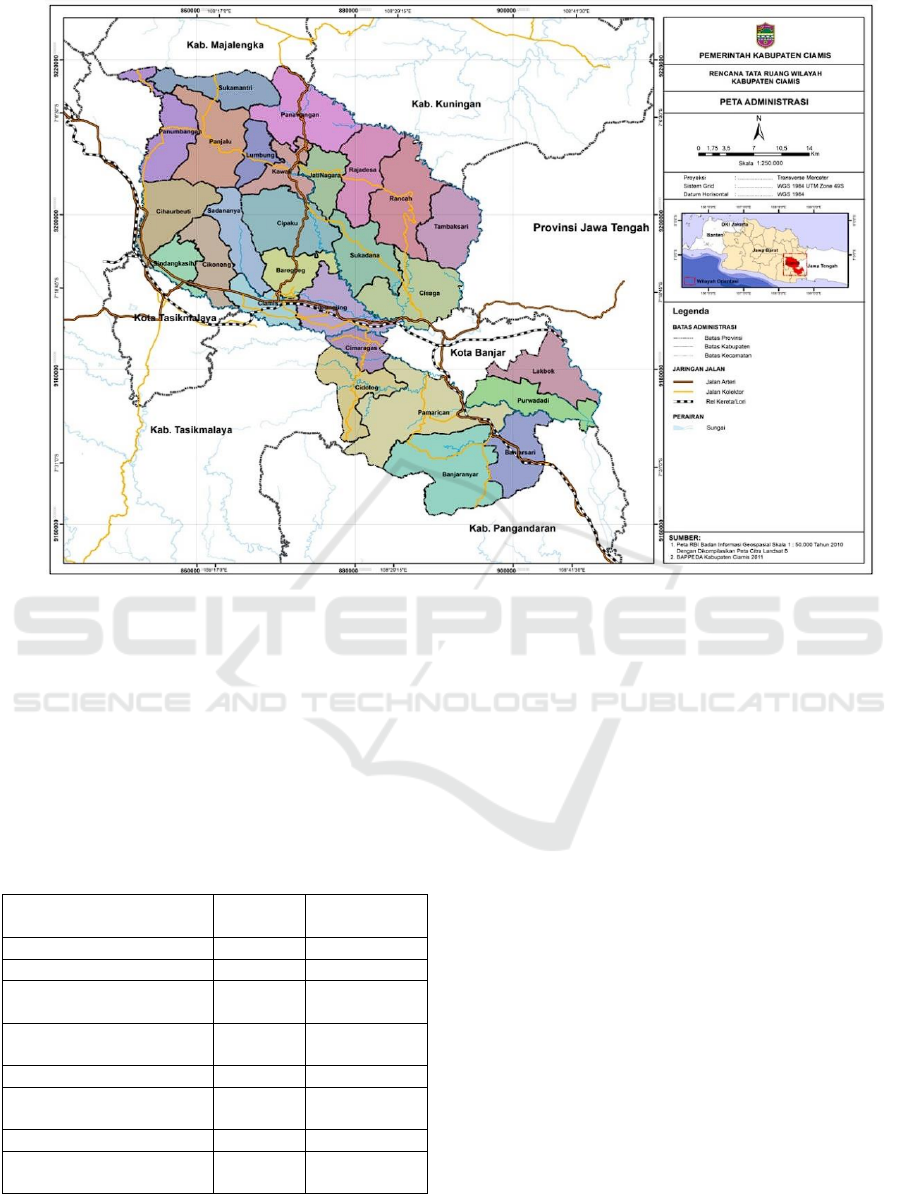
Figure 1. Administrative Map of Ciamis District.
3.2 Health Care Facilities
Health service facilities in Ciamis District in 2019
consisted of 7 types, namely General Hospitals,
Inpatient Puskesmas, Non-Inpatient Puskesmas,
Mobile Puskesmas, Puskesmas Pembantu,
Pharmacies, and Village Health Posts (Poskesdes),
while there were no Special Hospitals, as shown in
Table 2.
Table 2. Health Service Facilities in Ciamis District.
Indicators
Numbers/
Values
Unit
General Hos
p
ital 4 Hos
p
ital
S
p
ecialized Hos
p
ital 0 Hos
p
ital
Inpatient Community
Health Centre
29 CHCs
Non-Inpatient Health
Centre
17 CHCs
Mobile Health Centre 75 Mobile-CHCs
Sub-Community Health
Centre
85 Sub-CHCs
Pharmac
y
135 Pharmac
y
Village Health Post
(
VHP
)
139 VHP
Based on Government Regulation No. 47/2016 on
health service facilities, a health service facility was
a tool and/or place used to organize healthcare efforts,
including promotive, preventive, curative, and
rehabilitative. These efforts were often carried out by
the central and regional governments, and/or
community.
3.3 Human Resources (HR)
The number of health HR in CHCs, hospitals, UPTD
Pharmacy, Labkesda, and health offices in Ciamis
District in 2019 was 1,837 people, which were
classified into 12 groups. Furthermore, there were 25
specialist doctors, 78 general practitioners, 13
dentists, 1 specialist dentist, 827 nurses, 461
midwives, 90 public health workers, 38
environmental health workers, 45 nutritionists, 32
medical laboratory experts, 70 other biomedical
techniques, 11 physical therapists, 88 medical
technicians, and 58 pharmaceutical workers, as
shown in Table 3.
The ratio of HR at the 37 CHCs in the region was
highest for the midwife at 26.09 people per 100,000,
followed by nurses at 20.59 people per 100,000. The
smallest ratios were observed in physical therapists at
0.35 people per 100,000 and dentists at 0.71 people
per 100,000, as shown in Table 4.
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
59
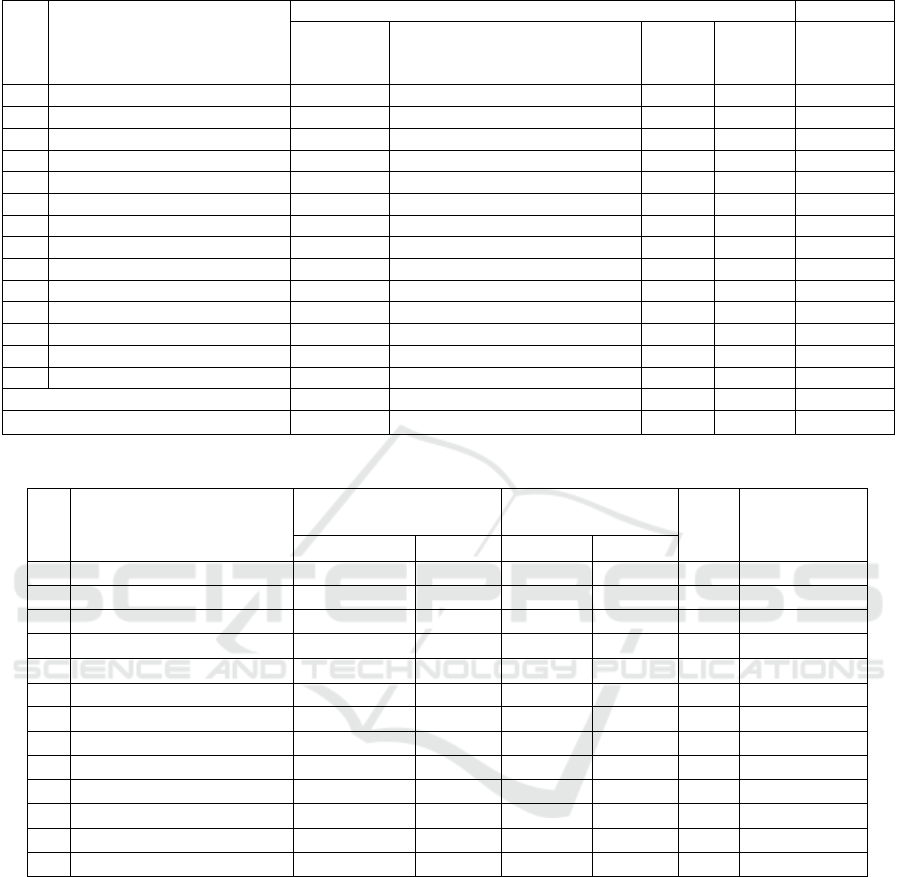
Table 3. Number of Health HR in Ciamis District.
No Type of Health Worker
T
yp
e
Hospital
Technical Implementation Unit
(UPTD) Pharmacy & Regional
Health Laborator
y
Head
Office
CHCs Total
1 S
p
ecialist Docto
r
25 0 0 0 25
2 General Practitione
r
29 1 4 44 78
3 Dentist 3 0 0 10 13
4 Specialist Dentist 1 0 0 0 1
5 Nurse 535 0 0 292 827
6 Midwife 91 0 0 370 461
7 Public Health 6 0 8 76 90
8 Environmental Health 3 0 2 33 38
9 Nutrition 10 0 2 33 45
10 Medical Laborator
y
Ex
p
ert 20 0 0 12 32
11 Biomedical En
g
ineerin
g
35 0 0 35 70
12 Ph
y
sical Thera
p
ist 6 0 0 5 11
13 Medical Technician 27 0 0 61 88
14 Pharmac
y
40 0 0 18 58
Total 831 1 16 989 1.837
Table 4. Number and Ratio of Medical Staff, Midwives, and Nurses to Population at Puskesmas in Ciamis District.
The number of HR assigned to 37 CHCs (20
treatment and 17 non-care Puskesmas) was 869
people, consisting of 13 sub-groups. The prevalent
types of HR were midwives, namely 370 individuals
or an average of 10 people per health centre, followed
by nurses, with 292 individuals or an average of 7.89
people per health centre. The last type of HR was
physical therapists, namely 5 people or an average of
0.14 people per health centre. Furthermore, the types
of HR whose average per Puskesmas was less than 1
were dentists (0.27), followed by environmental
health workers (0.89), nutritionists (0.89), medical
laboratory experts (0.32), biomedical engineering
experts (0.95), physical therapists (0.14), and
pharmacist (0.49).
The ratio of HR in 37 health centres in Ciamis
District was highest for midwives at 26.09 people per
100,000 population and nurses at 20.59 people per
100,000 population. Meanwhile, the smallest ratios
were physical therapists at 0.35 people per 100,000
population and dentists at 0.71 people per 100,000
population, as shown in Table 4.
Based on the results of confirmation at the Ciamis
District Health Office, the number of non-health HR
on duty in 2019 was 381 people, including 48 and 333
individuals at the health Office and CHCs,
respectively.
No Type of Health Worker
Inpatient Community
Health Centre
Non-Inpatient Health
Centre
Total Ratio
Total Average Total Average
1 General Practitioner
24 1,2 20 1,18 44 3,1
2 Dentist
6 0,3 4 0,24 10 0,71
3 Nurse
174 8,7 118 6,94 292 20,59
4 Midwife
181 9,05 189 11,12 370 26,09
5 Public Health
39 1,95 37 2,18 76 5,36
6 Environmental Health
18 0,9 15 0,88 33 2,33
7 Nutrition
19 0,95 14 0,82 33 2,33
8 Medical Laboratory Expert
7 0,35 5 0,29 12 0,85
9 Biomedical Engineering
22 1,1 13 0,76 35 2,47
10 Physical Therapist
5 0,25 0 0,00 5 0,35
11 Medical Technician
34 1,7 27 1,59 61 4,3
12 Pharmacy
7 0,35 11 0,65 18 1,27
536 - 453 - 989
ICSDH 2023 - The International Conference on Social Determinants of Health
60
In terms of the type of knowledge at the
undergraduate level, a total of 15.62% of the samples
were graduates in other fields, with an average of 1.41
people per Puskesmas. Furthermore, 6.97% were in
economics with an average of 0.62, 5.11% in
management with an average of 0.46, 3.00% were in
informatics with an average of 0.27, 2.40% were in
administration with an average of 0.22, 0.60% were
in law with an average of 0.05 people per Puskesmas,
and 0.30% were in education with an average of 0.03.
Based on the results, there were also non-health
HR who had attended informatics courses, namely
0.30% with an average of 0.03 people per Puskesmas.
The most common type of HR was elementary/junior
high/senior high school graduates, namely 65.77%
with an average of 5.92 people per health centre. This
condition was similar in the health office, where the
majority of the samples were other (47.92%),
economics (2.08%), management (6.25%), non-
informatics, administration (4.17%), law (2.08%),
and non-education graduates, as well as those who
attended informatics courses. The most common type
of HR in health offices was elementary/junior
high/senior high school graduates, namely 47.92%, as
shown in Table 5.
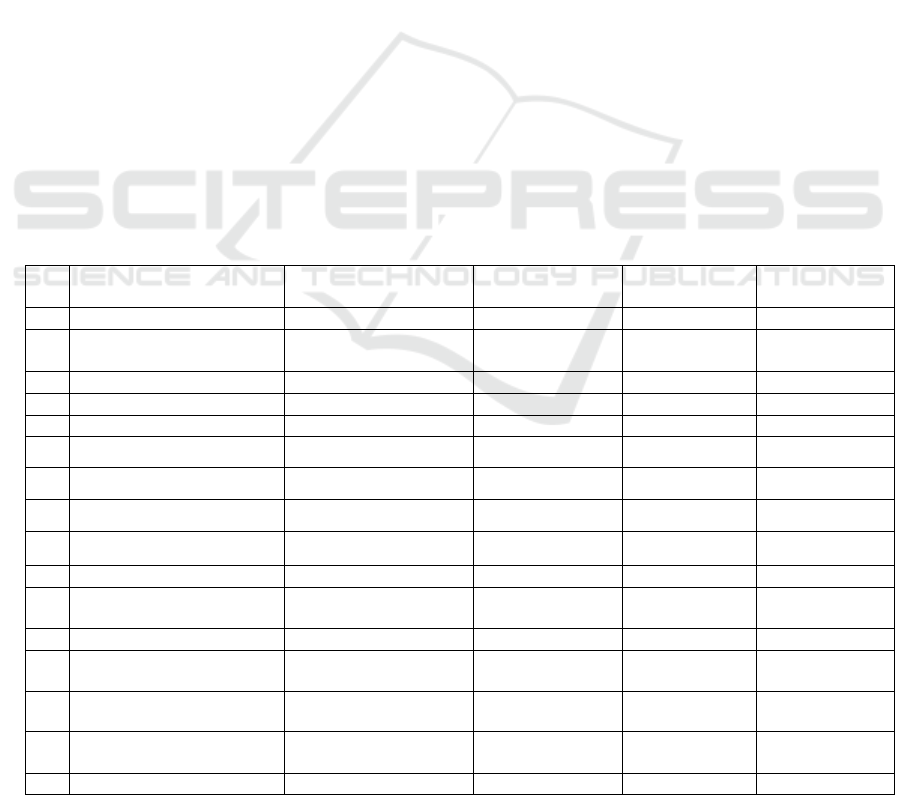
Table 5. Non-Health HR in Health Center and Health Office Ciamis District.
3.4 HIS Implementation
Based on data from the Balitbangkes Data
Management Laboratory from the 2019 Rifaskes
results, activities at the Puskesmas supported by HIS
application could be divided into 6 groups, namely:
a. Puskesmas Management, consisting of 3
applications, namely the SIMPUS, SP2TP/SP3,
and e-Puskesmas.
b. HISDA application.
c. ASPAK.
d. Disease case/health status data, consisting of 10
applications, namely SITT, SIHA, SIHEPI, SI
PTM, SI PD3I, SISMAL, SI STBM, E-PPGBM,
KS, and SKDR.
e. Primary Care Application (Pcare).
f. HFIS application.
g. BPJS non-capitation claims, consisting of (1)
Pap smear/IVA claims, (2) Primary/promotive
screening, (3). First-level hospitalization (RITP),
(4) Obstetrics and neonates, (5) Ambulance
Claims, and (6) Other claims.
h. Puskesmas Report, consisting of:
(1) Monthly Report on Morbidity Data (LB1)
(2) Monthly Report on Drug Usage and Request
Sheet (LPLPO or LB2)
(3) Monthly Report on Nutrition, MCH,
Immunization, P2M (LB3)
(4) Monthly Report of Puskesmas Activity Data
(LB4)
(5) Annual Report of Basic Health Center Data
(LT1)
(6) Annual Report of Puskesmas Personnel
Data (LT2)
(7) Annual Report of Puskesmas Equipment
Data (LT3).
i. Medical record application.
No Types of Non-Health HR
CHCs Health Office Total
Total %
Average/
Health Cente
r
Total % Total %
1 Bachelor of Administration 8 2,40 0,22 2 4,17 10 2,62
2 Bachelor of Economics 23 6,91 0,62 1 2,08 24 6,30
3 Bachelor of Mana
g
ement 17 5,11 0,46 3 6,25 20 5,25
4 Bachelor of Informatics 10 3,00 0,27 0 0,00 10 2,62
5 Bachelor of Law 2 0,60 0,05 1 2,08 3 0,79
6 Bachelor of Education 1 0,30 0,03 0 0,00 1 0,26
7 Other Bachelo
r
52 15,62 1,41 18 37,50 70 18,37
8 Informatics Course 1 0,30 0,03 0 0,00 1 0,26
10 Elementar
y
/Secondar
y
/Hi
g
h School 219 65,77 5,92 23 47,92 242 63,52
Total 333 - - 48 - 381 -
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
61
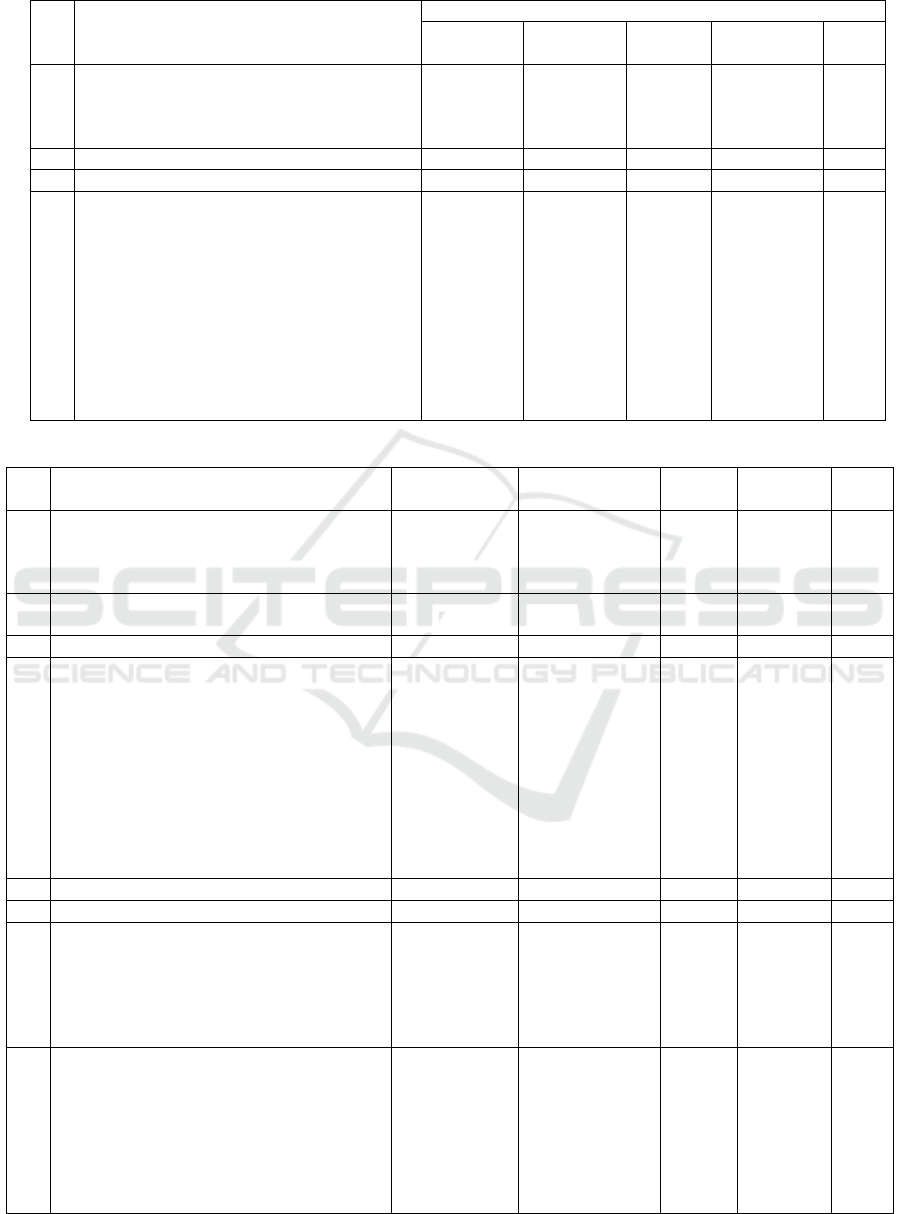
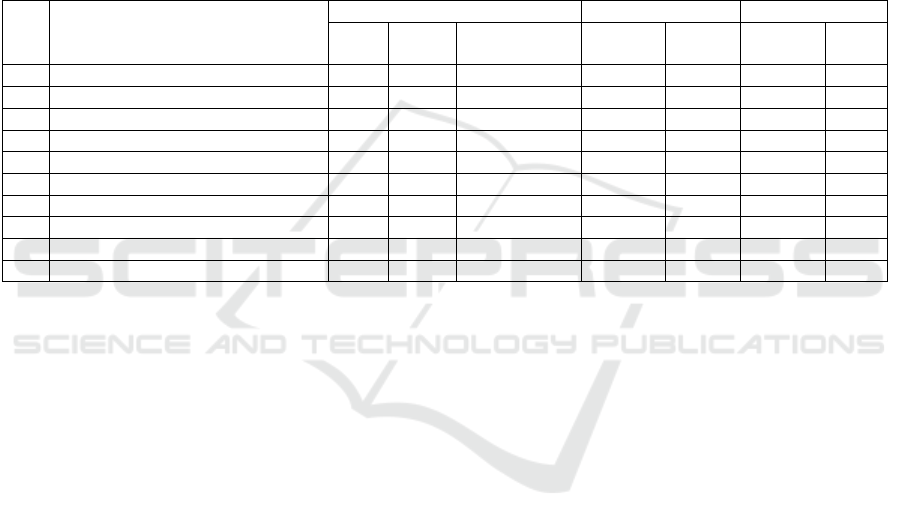
Table 6. Number of Health Centers Based on the Availability of HIS Ciamis District.
No HIS Implementation System
Recordin
g
S
y
stem
Electronics
Electronics
& Manuals
Manuals Not in Use Total
1. Health center management
a) SIMPUS
b) SP2TP/SP3
c) e-Puskesmas
7
10
16
10
10
11
5
5
1
15
12
9
37
37
37
2. HISDA 5 7 1 24 37
3. ASPA
K
18 18 1 0 37
4. Disease Case Data/Health Status
a) SITT
b) SIHA
c) SIHEPI
d) SI PTM
e) SI PD3I
f) E-ISMAL
g) SI STBM
h) E-PPGBM
i) KS
h
)
SKDR
14
15
11
13
10
8
13
18
15
11
16
21
18
23
17
13
15
18
22
13
5
1
1
1
5
2
5
1
0
4
2
0
7
0
5
14
4
0
0
9
37
37
37
37
37
37
37
37
37
37
Table 7. Number of HIS Implementation Activities at Puskesmas Ciamis District.
No HIS Implementation System Activity Period
Number of
Activities/ CHCs
Total
CHCs
Number of
Activities
%
Health center management
a) SIMPUS
b) SP2TP/SP3
c) e-Puskesmas
Monthly
Monthly
Monthly
12 times
12 times
12 times
22
25
28
264
300
336
0.36
0.41
0.23
HISDA Monthly &
Incidental
13 times 13 169 0.60
ASPAK Incidental - 37 444 0.60
Disease Case Data/Health Status
a) SITT
b) SIHA
c) SIHEPI
d) SI PTM
e) SI PD3I
f) E-ISMAL
g) SI STBM
h) E-PPGBM
i) KS
j) SKDR
Monthly
Monthly
Monthly
Monthly
Monthly
Monthly
Monthly
Monthly
Incidental
Incidental
12 times
12 times
12 times
12 times
12 times
12 times
12 times
12 times
-
-
35
37
30
37
32
23
33
37
37
28
420
444
360
444
384
276
396
444
444
336
0.57
0.60
0.49
0.60
0.54
0.37
0.54
0.60
0.60
0.46
Pcare Monthly 12 times 37 444 0.60
HFIS Monthly 12 times 37 444 0.60
BPJS Non-Capitation Claims
a) Pap smear/IVA
b) RITP
c) Obstetrics and neonates
d) Ambulance Claims
e) Other Claims
Incidental
Incidental
Incidental
Incidental
Incidental
-
-
-
-
-
3
20
35
15
20
117
13,620
33,574
961
64,690
0.16
18.46
45.46
1.30
8.77
CHCs report
a) LB1
b) LPLPO or LB2
c) LB3
d) LB4
e) LT1
f) LT2
g) LT3
Monthly
Monthly
Monthly
Monthly
Yearly
Yearly
Yearly
12 times
12 times
12 times
12 times
1 time
1 time
1 time
37
37
37
37
37
37
37
444
444
444
444
37
37
37
0.60
0.60
0.60
0.60
0.05
0.05
0.05
ICSDH 2023 - The International Conference on Social Determinants of Health
62

No HIS Implementation System Activity Period
Number of
Activities/ CHCs
Total
CHCs
Number of
Activities
%
Medical records (electronic and combined) Dail
y
292 times 37 10,804 14.64
Total 132.002
The implementation of each HIS application did
not have the same operational period, where some
were daily. In the case of medical records, some of
them were monthly, annual, monthly and annual, and
incidental.
Due to various reasons, a proportion of health
centres in the Ciamis district have not implemented
all HIS applications. The results also showed that
some HISs were manual, electronic, and a mixture of
electronic and manual.
The least used application was HISDA, which was
used by 13 CHCs, accounting for 35.14% of the total
population. Among these Puskesmas, the availability
of data was carried out electronically by 5 of them
(13.51%), a mixture of electronic and manual by 7
(18.91%), and manually by 1 (2.70%).
The most widely used HIS applications were
ASPAK, SIHA, SI PTM, E-PPGBM, and KS, which
were used by all CHCs (100%). Among HIS
applications, none of them were carried out
electronically.
The most highly used electronic applications were
ASPAK and E-PPGBM by 18 Puskesmas (48.65%).
Meanwhile, the least used was HISDA, namely 5
Puskesmas (13.51%).
In the implementation of HIS (Table 7), some
CHCs did not record all HIS applications. Among
those using the recording system, some of them were
online, offline, or a mixture of online and offline.
The application with the least online recording
system was ASPAK, which was used by 36
Puskesmas. The results showed that none of the
Puskesmas had an online recording system is online,
with 17 (47.22%) being offline and 19 (52.78%) not
using any system, as shown in Table 8.
In 2018, the types of HIS applications carried out
by 37 health centres in Ciamis District were recorded
at 30 items, with the total number or frequency of
activities being 132,002, as shown in Table 7.
Based on the number of activities, the 5 items of
HIS activity types with the highest number of
activities were (1) obstetric and neonate claims,
namely 33,574 times (45.50%) by 35 Puskesmas, (2)
RITP claims, namely 13,620 times (18.46%) by 20
Puskesmas, (3) Electronic and combined medical
records were 108,04 times (14.64%) by 37
Puskesmas, (4) BPJS non-capitation claims for other
claims were 6,469 times (8.77%), and (5) BPJS non-
capitation for ambulance claims were 961 times
(1.30%) by 15 Puskesmas.
In terms of groups, the 5 HIS items with the
highest number of activities were (1) BPJS non-
capitation claims, namely 112,962 times (85.58%) by
37 Puskesmas, (2) medical records, namely 10,804
times (8.18%) by 37 Puskesmas, (3). Disease Case
data was performed 3,948 times (2.99%) by 33 health
centres, (4) Health centre reports were carried out
1,887 times (8.18%) by 37 health centres, and (5)
health centre management was performed 900 times
(0.68%) by an average of 25 health centre, as shown
in Table 2.
The calculation of the number of medical record
activities using HIS was based on the assumption that
each working day was carried out 1 time per
Puskesmas. The working days in Ciamis District were
6 days per week, and in a year, it was 52 weeks x 6
days - 20 national holidays and public holidays, to
give 292 working days. The number of medical
record activities carried out in Ciamis District in 2019
was 10,804.
In providing services in the building, some CHCs
did not have an inter-room computer network. The
2019 Rifaskes results showed that 17 of them
(45.95%) had the networks, 15 (40.54%) experienced
a total absence, and 5(13.51%) did not use computers.
Patient medical records in 23 CHCs (62.16%)
were in the form of family folders, and the remaining
14 (37.84%) were in other forms. In inpatient
registration, a total of 10 (27.02%) were online, and
the remaining 27 (72.98%) did not apply for
registration, as shown in Table 8.
Table 8. Computer Network System in Providing Indoor Services and Online Patient Registration at Puskesmas Ciamis
District.
No Activities
Yes No
Total % Total %
1. Using computers in in-building services 32 CHCs 86.49 5 CHCs 13.51
2. Computer networks exist between rooms in the building 17 CHCs 45.95 15 CHCs 40.54
3. The online patient registration system 10 CHCs 27.02 27 CHCs 72.98
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
63
The results showed that 16 activity items must be
implemented at the district health office and
supported by the HIS application, namely HISda, data
communication (komdat), health office management
information system (SIM DHO), SIMPUS,
SP2TP/SP3, e-Puskesmas, ASPAK, SITT, SIHA,
SIHEPI, SI PTM, SIPD3I, SISMAL, SI-STBM,
EPPGBM, and SKDR. A total of HIS data on 10
items that had been implemented were available,
namely Komdat, e-Puskesmas, ASPAK, SITT, SIHA,
SIPTM, SISMAL, SI-STBM, and EPPGBM.
Furthermore, the results showed that 2 of them were
still manual (SIHEPI and SIPD3I), while HISDA,
SIM DHO, SIMPUS, and SP2TP/SP3 had no dataset.
Among the data available, only 1 HIS activity (10%)
was available electronically, namely, ASPAK and the
remaining 9 were a combination of electronic and
manual, as shown in Table 9.
In the 10 HIS items, 3 activities (30%) used online
recording systems, namely ASPAK, SISMAL, and
SI-STBM, and the remaining 7 used a combination of
online and offline recording.
System developers were 70% MOH, 20% health
office, and 10% private developers, while the data
storage was 99% MOH servers and 10% non-
government servers, as shown in Table 9.
Based on the confirmation results at the 4 CHCs
and the Ciamis District Health Office, until 2020,
there were no issued regional policies from the local
government or health office regarding the
implementation of HIS in healthcare programs.
Therefore, the use of the program was considered the
main tasks and functions (tusi) of the implementation
unit and the duties of each officer. For example, if the
HIS application was related to nutrition, then the
person in charge of the EPPGBM also had the
responsibility of monitoring the nutrition program.
The person in charge of the SI-STBM application also
had the role of supervising the environmental health
program. These decisions depended on the policy of
the head of the Puskesmas, issued by the decision
letter.
Based on Rifaskes 2019 data, among 37 CHCs in
Ciamis District, a total of 24 (64.86%) had special
personnel, who were assigned to be responsible for
recording, while the remaining 13 (35.14%) did not
assign any personnel. The person in charge was only
saddled with an additional task but still had the main
responsibility of supervising the program
implemented by Puskesmas. Based on educational
background among 24 staff, 3 (12.5%) had an
education in medical records and health information
(RMIK) or health information (Infokes), while the
remaining 21 (87.5%) had a variety of backgrounds,
such as midwives, nurses, public health,
environmental health, and nutrition (Table 10).
Table 9. HIS Implemented by Health Office Ciamis District.
No
Health Information
Sistem Types
Availability
Recording
System
Developer
Data Storage
(Server)
1. HISDA - - - -
2. Data Communication
(Komdat) Application
Electronics & Manuals Online & Offline Health Ministry Health Ministry
3. SIM Health Office - - - -
4. SIMPUS - - - -
5. SP2TP/SP3 - - - -
6. e-Puskesmas Electronics & Manuals Online & Offline Private Non-Government
7. ASPAK Electronics Online Health Ministry Health Ministry
8. SITT Electronics & Manuals Online & Offline Health Office Health Ministry
9. SIHA Electronics & Manuals Online & Offline Health Ministry Health Ministry
10. SIHEPI Manuals - - -
11. SI PTM Electronics & Manuals Online & Offline Health Office Health Ministry
12. SIPD3I Manuals - - -
13. SISMAL Electronics & Manuals Online Health Ministry Health Ministry
14. SI-STBM Electronics & Manuals Online Health Ministry Health Ministry
15. EPPGBM Electronics & Manuals Online & Offline Health Ministry Health Ministry
16. SKDR Electronics & Manuals Online & Offline Health Ministr
y
Health Ministr
y
ICSDH 2023 - The International Conference on Social Determinants of Health
64
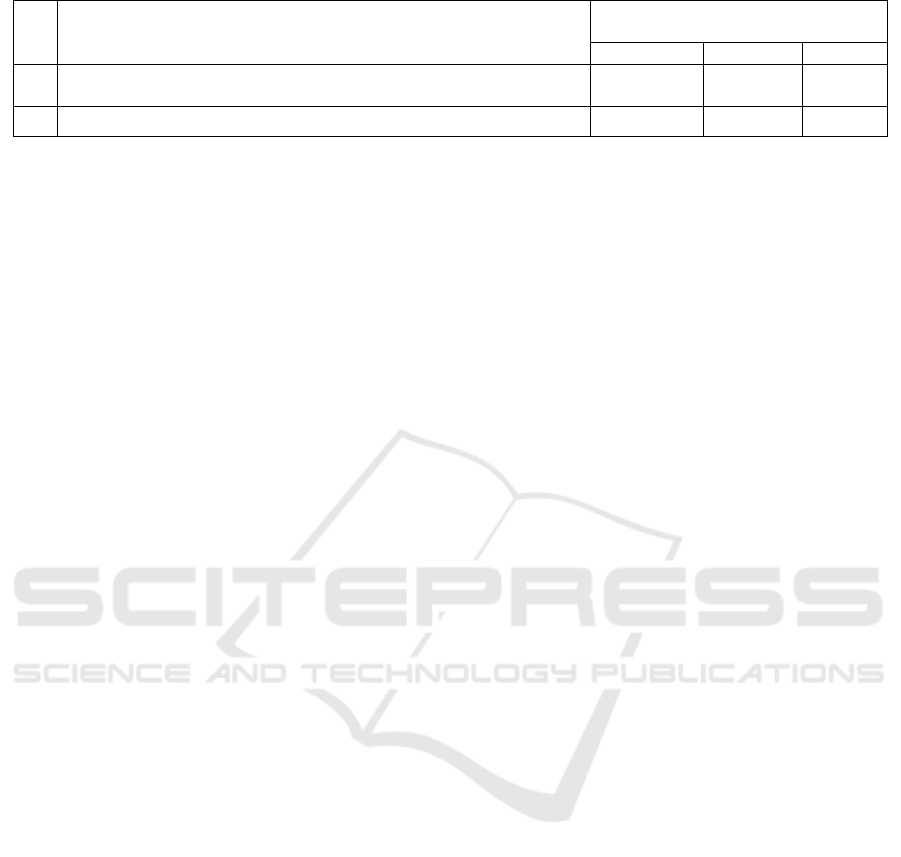
Table 10. Person in Charge of Recording and Reporting at Puskesmas Ciamis District.
No Person in Charge of Recording and Reporting at the Health Center
There is a Person in Charge of
Recording and Reporting
Yes No Total
1. Special personnel assigned to be responsible for recording and reporting
at CHCs
24 CHCs 13 CHCs 37 CHCs
2. Educated in RMIK or Infokes 3 CHCs 21 CHCs 24 CHCs
The flow of data and information in the
implementation of HIS in the Ciamis District was still
carried out partially, without the use of a single data
system tailored to the tasks of implementing each
program. Furthermore, data flow links were also
performed separately for each program. The flow of
a program at the Puskesmas was connected to the
same program at a higher level, and other programs
had different links.
4 DISCUSSIONS
In 2019, the overall HR at the Puskesmas in Ciamis
District, specifically medical personnel (general
practitioners and dentists), nurses, and midwives did
not meet the targets set 10 years ago (2010). The
targets were 30 general practitioners per 100,000
population, 11 dentists per 100,000 population, 75
midwives per 100,000 population, and 158 nurses per
100,000 population (BPPSDM, 2019). Based on the
results, the ratio of general practitioners, dentists,
nurses, and midwives was less than 26.9 per 100,000
population (less than 89.67%), 10.29 per 100,000
population (less than 93.55%), and 137.41 per
100,000 population (less than 86.97%), and 48.91 per
100,000 population (less than 65.21%).
Compared to the minimum standards of staffing
by the Annex of Permenkes No. 75 of 2014 (averaged
including the category of rural areas) in both
treatment and non-treatment Puskesmas, some health
HR had not met the requirement. The standards in the
treatment health centre were (1) 2 doctors or primary
doctors, (2) 1 dentist, (3) 8 nurses, (4) 7 midwives, (5)
1 community health worker, (6) 1 environmental
health worker, (7) 1 medical laboratory technologist,
(8) 2 nutrition workers, (9) 1 pharmaceutical worker,
(10) 2 administrative personnel, and 1 staff.
Meanwhile, the standards in the non-care health
centre were (1) 1 doctor or primary doctor, (2) 1
dentist, (3) 5 nurses, (4) 4 midwives, (5) 1 community
health worker, (6) 1 environmental health worker, (7)
1 medical laboratory technologist, (8) 1 nutritionist,
(9) 1 pharmaceutical worker, (10) 2 administrative
personnel, and 1 staff 1 person (Ministry of Health,
2014). These results indicated that in the treatment
health centre, general practitioners, dentists,
environmental health workers, medical laboratories
technologists, nutritionists, and pharmaceutical
workers were still lacking by 0.8, 0.7, 0.1, 0.65, 0.05,
and 0.65 persons per health centre, respectively. The
results also showed that nurses, midwives, and
community health workers had reached the minimum
standard of 0.7, 2.05, and 0.95 persons per health
centre, respectively. In non-care health centres,
general practitioners met the minimum standard of
0.18 per health centre, followed by nurses (1.97),
midwives (7.12), and community health workers
(1.18). Dentists, environmental health workers,
medical laboratory technologists, nutritionists, and
pharmaceutical workers were still lacking by 0.76,
0.12, 0.71, 0.18, and 0.35 people per health centre,
respectively.
Health workers at Puskesmas, specifically
doctors, midwives, and nurses were also given other
responsibilities as implementers of programs, which
were often related to their profession. This was
because Puskesmas was a health service facility used
to organize healthcare efforts, including promotive,
preventive, curative, and rehabilitative, with the
function of organizing public (UKM) and individual
(UKP) health efforts (Menteri Kesehatan 2014).
The implementation of all healthcare efforts
required coordination with all stakeholders in the
working area to prevent and reduce risks faced by
individuals, families, groups, and communities based
on the principles of the healthy paradigm. The
confirmation at the sample Puskesmas revealed that
most of these activities were carried out by medical
personnel, midwives, nurses, and management
personnel. Apart from health workers, the facility also
consisted of non-health staff who must support
administrative activities, financial administration,
information systems, and other operational activities
(Menteri Kesehatan 2014).
The HIS was developed to support the seven
national healthcare subsystems, namely (1) health
efforts, (2) health study and development; (3) health
financing; (4) health HR; (5) pharmaceutical
preparations, medical devices, and food; (6) health
management and regulation; and (7) community
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
65

empowerment (Daryo Soemitro, 2016). The
implementation of this program was expected to
make the recording and reporting activities at the
Puskesmas become an interrelated unit. In its
application, the use of ICT was a necessity because
HIS increased along with efforts to improve the
quality, efficiency, and effectiveness of management
and implementation of health development.
At present, the frequency of ICT activities is very
high, including in Ciamis District. According to
Rifaskes 2019 data, the frequency of HIS
implementation at Puskesmas during 2018 in 9
activity items, namely Puskesmas management (25),
HISDA (13), ASPAK (37), disease case data (33),
Pcare (37), HFIS (37), BPJS non-capitation claims
(19), Puskesmas reports (37) and medical records
(33) was 132,002 times (Table 7.9) or 452 times per
working day. The confirmation from 4 Puskesmas
showed that the application of ICT could enhance
performance, increase accuracy, and reduce the time
required (time and energy efficiency). However, the
large amount of applications and the high frequency
of ICT activities increased the burden on employees,
including health workers. This was because there was
no officer specifically handling HIS and the
implementation process was complex.
One of the consequences of this situation was that
some CHCs in the Ciamis District could not
implement all SIMPUS items. Rifaskes 2019 data
showed that among 37 Puskesmas, 22 (54.46%)
implemented SIMPUS, and only 7 had electronic
information. The report also revealed that only 5 of
them used online recording systems. Several HIS
applications have been implemented by all facilities,
such as ASPAK, SIHA, SI PTM, E-PPGBM, and KS.
Meanwhile, HISDA had the lowest implementation,
namely 13 Puskesmas, accounting for 35.13% of the
total population. In the availability of information,
some of the facilities used electronic approaches, with
ASPAK and E-PPGBM being the most used
applications by 18 CHCs (48.65%). Based on the
results, HISDA had the lowest usage by only 5
facilities (13.51%). The most common use of the
online recording system was observed in KS by 17
samples (45.95%), and the least was HISDA with
only 3 samples (8.11%). ASPAK was not carried out
using online recording by any of the facilities.
HIS must be managed at the central and regional
levels (provincial and district/city), as well as in
health care facilities by their respective authorities.
This arrangement aimed to (1) ensure the availability,
quality, and access to health information, (2)
empower the participation of the community,
including professional organizations in the
implementation of HIS, and (3) achieve the
implementation of the HIS within the scope of the
national health system, specifically through
strengthening cooperation, coordination, integration,
and synchronization (Kemsekneg 2014).
The management of HIS in districts/cities was
carried out by structural or functional work units that
organized government affairs in the health sector. The
activities carried out included managing health data
and information at the district/city scale, in the form
of (1) requesting health data and information from
parties related to HIS management, (2) collecting
and/or combining routine and non-routine datasets
from sources, (3) processing health data, (4). storing,
maintaining, and providing health data and
information reserves, (5) providing feedback to
sources, (6) conducting data analysis as needed, (7)
disseminating health information using electronic
and/or non-electronic media, (8). sending health data
and information needed in the management of
provincial and national HIS, and (9) implementing
guidance and facilitating the development of HIS in
first-level facilities. Meanwhile, the management of
the program in health facilities was carried out by the
HIS manager in each health facility (Kemsekneg
2014). This regulation implied that the management
of HIS at the district level and health facilities must
be carried out by a special unit or team or officer who
performed these activities. The aim was to facilitate
the management of data and information, as well as
their flow to various levels. The approach was also
used to ensure that all components of the HIS were
implemented properly. Therefore, data and
information managed in the HIS application at the
health facility level were only issued and received by
the manager (one door), while the source of data was
from program implementers at the health facility.
Feedback from higher-level ICT managers
(district/city, provincial and central) was received by
other managers and then channelled to the relevant
people. The management of the HIS at the district/city
level must also be carried out by a special unit to
ensure that all data and information flow only entered
and were issued by the unit. Data from health
facilities were forwarded to the relevant field or
section, while data inputted for reporting and
feedback were obtained from the relevant field or
section. This type of ICT management helped to
ensure that there was only one data (one data) at the
health facility or district level because it was only
managed by one unit. Furthermore, this situation
facilitated data management, which could be used as
a basis for making decisions or policies as a follow-
up to information received.
ICSDH 2023 - The International Conference on Social Determinants of Health
66

One-stop HIS management by using ICT was the
national e-health strategy, which was a
comprehensive approach to planning, developing,
implementing, and evaluating the use of ICT in the
health sector. The aim was to provide a reference for
the government, professional/community
organizations, academics, practitioners, and other
stakeholders in carrying out e-health planning,
development, implementation, and evaluation
(Permenkes RI 2017). Furthermore, the optimal use
of ICT in the implementation of HIS was an aspect of
the application of the Electronic-Based Government
System (SPBE). The SPBE approach was defined as
the administration of government that used ICT to
provide services to users (Peraturan Presiden RI
2018).
In the strategic plan of the Ministry of Health
(Renstra) for the 2020-2024 period, HIS management
was one of the priority programs, intending to
stabilize (1) health information services that were
faster, valid, resource sharing, (2) integrated
electronic-based standard HIS, and (3) the
implementation of HIS in health service facilities.
Furthermore, data flow optimization was carried out,
which involved data reporting from districts/cities
through the Komdat application, reporting from all
source entities, and data bank development. The
fragmentation of the current HIS showed the need to
develop the ONE DATA initiative with a strategy
through the development of one standard, one
standardized metadata, and one portal. The aim was
to improve the integration, interoperability, and use
of government data whose use was not limited to
agencies, but also as a form of fulfilling public
information needs (Kemenkes 2020). In connection
with one data, a regulation had been issued, namely
Presidential Regulation Number 39 of 2019
concerning One Data Indonesia. In this regulation,
Satu Data Indonesia was defined as a government
policy to produce a dataset that was accurate, up-to-
date, integrated, and accountable, as well as easily
accessible and shared between central agencies and
regional agencies. This could be achieved through the
fulfilment of data standards, metadata, data
interoperability, and using reference codes and master
data (Pemerintah Republik Indonesia 2019).
The 2019 Ciamis District Health Profile showed
that the number of Health HR was still insufficient
when compared to the ratio of the population to be
served. This indicates that to prevent an increase in
the burden on HR, the management of HIS at the
Puskesmas was carried out by non-health HR or
others who did not provide direct services to patients
and the number had exceeded the minimum standard.
However, non-health HR with a background in
informatics and informatics courses were few sat
health office and Puskesmas, namely 11 individuals,
which was insufficient to manage HIS. The short-
term countermeasure was to provide courses or
training on informatics, including software,
hardware, network management, and ICT to existing
HR. These individuals were then given the
responsibility of managing the entire ICT by using the
principle of one data in their respective work units.
For the long term, recruitment of non-health HR with
a background in informatics was carried out, both
ASN recruitment and Government Employees with
Work Agreements (PPPK). The type of people
managing the program must be permanent
employees, namely ASN or PPPK. This was to ensure
that they had high responsibility due to employment
status, considering the importance of data and
information management in policy-making. The
approach was expected to help non-health HR support
administrative activities, financial administration,
information systems, and other operational activities
(Menkes RI 2014).
The implementation of data communication in the
HIS must be carried out in an integrated manner. The
aim was to 1) ensure the availability, quality, and
access to priority health data and other data content,
2) optimize the flow of health data from
districts/cities and/or provinces to the ministry or vice
versa, and 3) realize the implementation of an
integrated HIS (Menteri Kesehatan 2014). The MOH
regulation implied that the flow of data and
information from the health centre to the district
health office must be connected to the provincial
health office and the MOH in a network. To support
this policy, a national information system network
(HISNAS) was established, which was an integrated
data communication network infrastructure using a
wide area network (WAN). The WAN was a
telecommunications network that covered a large area
and was used to send information over long distances
between different local area networks (LANs), and
other local computer architectures (Menteri
Kesehatan 2014). The results of the 2017 HIS
evaluation showed that it was "present but
inadequate" for resources (47%), indicators (61%),
data sources (51%), data quality (55%), data use and
dissemination (57%) and "not adequate" for data
management (35%). Based on these results, the
overall HIS still needed to be improved (Menkes RI
2012). A similar situation also occurred at the
Puskesmas and the Ciamis District Health Office,
where the application was not yet interconnected with
the HISNAS Network. To improve the
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
67

implementation of HIS, the Indonesian Ministry of
Health developed a Roadmap for the Action Plan to
Strengthen the Indonesian HIS, which in one part
mentioned the national model, namely integrated
HIS. This national model was defined as an
information system that provided an interconnection
mechanism between information sub-systems in
various appropriate ways. Therefore, data from one
system could routinely flow to, go to, or be retrieved
by one or more other system. Integration included
both technical systems (systems that can
communicate with each other) and content (common
data sets). The physical form of integrated ICT was
an information system application that was linked to
other applications.
To implement all ICT applications in Puskesmas
in Ciamis District, it was necessary to improve the
management of ICT at the local level. Improvements
were made to the management of HIS implementing
HR, work units, supporting hardware, data and
information flow system, internet networks,
financing, and regulations or policies on its
implementation issued by the Regent or Head of
SKPD and as well as the head of Fasyankes.
Furthermore, to strengthen the optimization of HIS
with one Puskesmas data and one Ciamis District
Health Office data connected in the HISNAS
Network, it was necessary to establish a one-door
system at the Ministry of Health. This had been stated
in the Roadmap of the Action Plan for Strengthening
the Indonesian HIS, that strengthening the HIS could
be carried out by developing a national model,
namely an integrated HIS. This model was an
information system that provided a mechanism for
interconnection between information sub-systems in
various appropriate ways. The physical form of an
integrated HIS is an information system application
that is linked to other applications. Therefore, data
from one system could routinely flow, go to, or be
retrieved by one or more other systems.
5 CONCLUSIONS
In conclusion, HIS has been implemented in 37 CHCs
and the Ciamis District Health Office, but some of the
CHCs have not routinely used all HIS applications.
The data and information flow from the Puskesmas to
the health office and from the district health office to
a higher level lacked a one-data and one-door system.
This was because each program or field employed its
unique approach, leading to fragmentation and a lack
of integration with the HISNAS Network.
HIS implementers at Puskesmas and the health
office were also in charge of executing health
programs involving HIS applications. Consequently,
for some certain individuals, the implementation of
HIS was considered an additional burden after
carrying out the primary duties and functions.
REFERENCES
Abdul, Kadir. 2003. Pengenalan Sistem Informasi. Penerbit
Andi, Yogyakarta. Vol. 1.
Dinas Kesehatan Kabupaten Ciamis. 2019. “Profil
Kesehatan Kabupaten Ciamis Tahun 2019.” Profil
Kesehatan Kabupaten Ciamis, 1–162.
Kemenkes. 2020. “Permenkes RI Nomor 21 Tahun 2020.”
Kementerian Kesehatan RI.
https://www.slideshare.net/maryamkazemi3/stability-
of-
colloids%0Ahttps://barnard.edu/sites/default/files/inlin
e/student_user_guide_for_spss.pdf%0Ahttp://www.ib
m.com/support%0Ahttp://www.spss.com/sites/dm-
book/legacy/ProgDataMgmt_SPSS17.pdf%0Ahttps://
www.n.
Kemenkes RI. 2022. Permenkes No. 18 Tahun 2022
Tentang Penyelenggaraan Satu Data Bidang
Kesehatan Melalui Sistem Informasi Kesehatan.
https://yankes.kemkes.go.id/unduhan/fileunduhan_166
2610931_564143.pdf.
Kemsekneg. 2014. PP No. 46 Tahun 2014 Tentang Sistem
Informasi Kesehatan. Peraturan Menteri Kesehatan
Republik Indonesia Nomor 46 Tahun 2014 Tentang
Sistem Informasi Kesehatan.
http://jdih.kkp.go.id/peraturan/pp-46-2014.pdf.
Kinasih, Renditya Sakti Ksatria. 2011. “SISTEM
INFORMASI PELAYANAN KESEHATAN PADA
PUSAT KESEHATAN MASYARAKAT
(PUSKESMAS) PURWANTORO II DIKABUPATEN
WONOGIRI JAWA TENGAH.” Universitas
AMIKOM Yogyakarta.
Menkes RI. 2012. “Keputusan Menteri Kesehatan Republik
Indonesia Nomor 192/Menkes/Sk/vi/2012 Tentang
Roadmap Rencana Aksi Penguatan Sistem Informasi
Kesehatan Indonesia” 2008: 4–72.
———. 2014. Permenkes RI No. 75 Tahun 2014.
http://hukor.kemkes.go.id/uploads/produk_hukum/PM
K No. 75 ttg Puskesmas.pdf.
Menteri Kesehatan. 2014. “Berita Negara Republik
Indonesia Nomor 1954 Tahun 2014.” Peraturan
Menteri Kesehatan Republik Indonesia Nomor 46
Tahun 2014 Tentang Sistem Informasi Kesehatan 1
(1954): 1–16. http://jdih.kkp.go.id/peraturan/pp-46-
2014.pdf.
Pemerintah Republik Indonesia. 2019. “Peraturan Presiden
Republik Indonesia No 39 Tahun 2019 Tentang Satu
Data Indonesia.” Peraturan Presiden.
https://peraturan.bpk.go.id/Home/Details/108813/perp
res-no-39-tahun-2019.
ICSDH 2023 - The International Conference on Social Determinants of Health
68

Peraturan Presiden RI. 2018. “Peraturan Presiden Nomor
95 Tahun 2018 Tentang Sistem Pemerintahan Berbasis
Elektronik.” Menteri Hukum Dan Hak Asasi Manusia
Republik Indonesia, 110.
Permenkes RI. 2017. “Peraturan Menteri Kesehatan
Republik Indonesia Nomor 46 Tahun 2017 Tentang
Strategi E-Kesehatan Nasional.” Menteri Kesehatan
Republik Indonesia, no. 1635: 1–47.
https://peraturan.bpk.go.id/Home/Details/139565/perm
enkes-no-46-tahun-2017.
Perwira, EAC. 2012. “SISTEM INFORMASI
MANAKEMEN PUSKESMAS ( STUDI KASUS:
PUSKESMAS NGAWEN DAN PUSKESMAS
JOGONALAN KABUPATEN KLATEN).” Journal of
Informatics and Technology 1 (3): 1–16.
https://ejournal3.undip.ac.id/index.php/joint/article/vie
w/6319.
Putri, Aisyiyah. 2013. “Analisis Sistem Pencatatan Dan
Pelaporan Puskesmas (Sp3) Dengan Penerapan Simpus
Di Puskesmas Karangmalang Semarang Tahun 2012 -
2013Analisis Sistem Pencatatan Dan Pelaporan
Puskesmas (Sp3) Dengan Penerapan Simpus Di
Puskesmas Karangmalang Semarang Tahun.” Fakultas
Kesehatan, Universitas Dian Nuswantoro Semarang
2013: 2012–14.
http://eprints.dinus.ac.id/6579/1/jurnal_12789.pdf.
Rondo, Tirzanny V M, F J O Pelealu, and Franckie R R
Maramis. 2013. “Analisis Pelaksanaan Sistem
Informasi Kesehatan Di Puskesmas Kabupaten
Minahasa Tenggara.” Fakultas Kesehatan Masyarakat
Universitas Sam Ratulangi Manado, 1–6.
https://fkm.unsrat.ac.id/wp-content/.../TIRZANY-
RONDO-091511076.pdf.
Soemitro, Daryo. 2016. “Tantangan E-Kesehatan Di
Indonesia.” Buletin Jendela Data Dan Informasi
Kesehatan 1.
Union, World Health Organization and International
Telecommunication. 2012. National EHealth Strategy
Toolkit.
https://www.who.int/publications/i/item/national-
ehealth-strategy-toolkit.
WHO Eastern Mediterranean. 2023. “EHealth.” 2023.
https://www.emro.who.int/health-topics/ehealth/.
Wibisono, Setyawan, and Siti Munawaroh. 2012. “Sistem
Informasi Manajemen Puskesmas (Simpuskesmas)
Berbasis Cloud Computing.” Jurnal Teknologi
Informasi DINAMIK 17 (2): 141–46.
https://www.unisbank.ac.id/ojs/index.php/fti1/article/v
iew/1661.
Wijaya, Roy Rendra, Noor Ifada, and Achmad Jauhari.
2009. “Perancangan & Pengembangan Sistem
Informasi Kesehatan ( Spt Simpus).” KUrsor Vol.5, No.
2 5 (2).
Implementation of Health Information Systems at Health Centres and Health Offices in Ciamis District
69
