
Vitamin D Levels Among Breast Cancer Patients in a Tertiary
Hospital in Lampung, Indonesia
Indri Windarti
1a
, Bintang Abadi Siregar
2
, Rizki Hanriko
1b
, Aditya Kusumaningtyas
2
and
Bayu Putra Danan Jaya
1c
1
Department of Anatomical Pathology, Faculty of Medicine, University of Lampung, Lampung, Indonesia
2
Department of Surgical, Faculty of Medicine, University of Lampung/Dr. H. Abdul Moeloek Hospital, Lampung, Indonesia
Keywords: Breast Cancer, Comorbidity, Vitamin D Level.
Abstract: Introduction: Vitamin D levels can vary among populations due to geographical location and sun exposure,
dietary habits, lifestyle, and genetic factors. People living in Indonesia may have a higher potential for sun
exposure, which can lead to adequate vitamin D synthesis in the skin. Several studies have suggested a
potential protective role of vitamin D against breast cancer. Preclinical studies have shown that vitamin D
may inhibit the growth and spread of breast cancer cells, induce cell death, and inhibit angiogenesis. Some
studies have found an inverse association, suggesting that higher vitamin D levels may be associated with a
reduced risk of breast cancer. This study was conducted to obtain the most recent information about the
vitamin D levels of breast cancer patients of Indonesian women, especially in Lampung. Methods: We
performed an observational analysis in an ongoing prospective cohort study of breast cancer patients at Dr.
H. Abdul Moeloek Hospital, Bandar Lampung, Indonesia. Sixty-eight subjects were collected from the main
study. Information on subjects, sociodemographic characteristics, clinical status, and tumor profile was
assessed. Vitamin D level was measured using ELISA methods. The association between sociodemographic
and clinical profiles with vitamin D levels was tested using Chi-square. Results: Breast cancer patients' mean
vitamin D level was low (19.7 ± 6.4 ng/ml). There was no correlation between sun exposure,
sociodemographic, and clinical status to Vitamin D levels of breast cancer patients. Patients with comorbidity
tend to have a low vitamin D level, primarily type 2 diabetes. Conclusion: Low vitamin D levels are frequently
found in our population. Further information about vitamin D levels and their association with the survival of
breast cancer patients is still challenging to become research questions.
1 INTRODUCTION
Breast cancer continues to evoke fear among the
majority of women. It is one of the prevalent
malignancies affecting women and the primary
contributor to global cancer-related fatalities.
Approximately 2.3 million new cases of breast cancer
are diagnosed each year (Mattiuzzi & Lippi, 2019;
Sung et al., 2021). The current approach to breast
cancer treatment involves surgical procedures,
chemotherapy, radiotherapy, and hormonal therapy.
However, these diverse treatments still have adverse
effects on patients. Optimal treatment with minimal
side effects has yet to be discovered. Particular
natural compounds are purported to enhance
a
https://orcid.org/0000-0001-8594-7137
b
https://orcid.org/0000-0003-3865-9364
c
https://orcid.org/0000-0009-5795-0022
treatment efficacy and act as a preventive against
breast cancer (Buja et al., 2020; Choudhury et al.,
2020; Ren et al., 2020). One such compound is
vitamin D (Bernhardt et al., 2021; Grabiec et al.,
2013).
Vitamin D, classified as a fat-soluble vitamin, is
essential in many biological processes. Operating as
a prohormone, it is crucial to managing calcium,
phosphorus, and skeletal muscle metabolism.
Moreover, vitamin D contributes to cardiovascular
and reproductive functions and is involved in various
physiological processes, including cell
differentiation, apoptosis, inflammation, and insulin
sensitivity (Chen & Zhi, 2020; Cosentino et al., 2021;
Janoušek et al., 2022). Interestingly, vitamin D is
130
Windarti, I., Siregar, B. A., Hanriko, R., Kusumaningtyas, A. and Jaya, B. P. D.
Vitamin D Levels Among Breast Cancer Patients in a Tertiary Hospital in Lampung, Indonesia.
DOI: 10.5220/0012901800004564
In Proceedings of the 5th International Conference on Social Determinants of Health (ICSDH 2023), pages 130-137
ISBN: 978-989-758-727-6; ISSN: 2975-8297
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)

recognized in preventing various cancer types, such
as colorectal, prostate, ovarian, lung, skin, and breast
cancers (Giovannucci, 2009; Kazemi et al., 2022). In
preclinical investigations, vitamin D has
demonstrated its ability to inhibit the proliferation of
cancer cells (Lopes et al., 2012; Zheng et al., 2017),
trigger apoptosis (Vanoirbeek et al., 2011), and
suppress angiogenesis (Susanti et al., 2018).
While vitamin D can be sourced from dietary
consumption, its primary source stems from the
synthesis of 7-dehydrocholesterol by epidermal cells
upon exposure to UV-B rays from the sun (Chen &
Zhi, 2020). Consequently, regions with limited sun
exposure necessitate supplementary vitamin D intake
to address the body's requirements. As a tropical
nation, Indonesia enjoys abundant sunshine
throughout the year, theoretically providing ample
sun exposure for its population and enabling adequate
synthesis of vitamin D in the skin to fulfill bodily
needs. However, several studies have revealed a
pronounced incidence of vitamin D deficiency,
particularly prevalent among the female population in
Indonesia (Green et al., 2008; Setiati, 2008). A recent
study has revealed a surprising prevalence of 63% in
vitamin D deficiency among pregnant women in
Indonesia (Octavius et al., 2023).
Vitamin D deficiency is associated with an
increased risk of developing several health
conditions, including rickets, osteoporosis, type 2
diabetes, cardiovascular disease, and autoimmune
disorders (Forouhi et al., 2012; Giovannucci, 2009).
It is also linked to an increased risk of developing
breast cancer. Women with sufficient vitamin D
levels have a lower risk of developing breast cancer
than women with deficient vitamin D levels (Atoum
& Alzoughool, 2017; Shaukat et al., 2017). This risk
applies to pre- and postmenopausal women (Bidgoli
& Azarshab, 2014; Kim et al., 2014). Interestingly, in
parallel with the prevalence of vitamin D deficiency
among women in Indonesia, breast cancer has
progressively risen, coupled with lower life
expectancies relative to other nations in the regions
(Susanti et al., 2018). This trend suggests a possible
association between vitamin D deficiency and breast
cancer in the Indonesian female population.
Vitamin D levels within the body can vary,
influenced by various factors, including geographic
location, ethnicity, medical conditions, lifestyle, and
genetics (Mazahery & Von Hurst, 2015). Despite
much evidence establishing a connection between
elevated vitamin D levels and a decreased risk of
breast cancer, there has been limited study exploring
the pattern of vitamin D levels among Indonesian
women diagnosed with breast cancer. Therefore, this
study was conducted to acquire current insights into
the vitamin D levels among breast cancer patients
within the female population of Indonesia, with a
particular emphasis on Lampung Province, and to
explore the association between vitamin D levels and
the sociodemographic and clinical characteristics of
the affected individuals.
2 METHODS
This study used an observational analytic approach
within an ongoing prospective cohort study involving
breast cancer patients at RSUD Dr. H. Abdul
Moeloek in Bandar Lampung, Indonesia. The study's
target population comprises breast cancer patients
currently undergoing treatment at Dr. H. Abdul
Moeloek Bandar Lampung who met the
predetermined inclusion and exclusion criteria. The
inclusion criteria encompass patients diagnosed with
breast cancer through histopathological and
mammographic assessments between 2021 and 2022,
possessing comprehensive medical record
data, and demonstrating a willingness to partake by
signing an informed consent. Conversely, exclusion
criteria pertain to breast cancer patients who have
undergone chemotherapy or radiotherapy, are
currently pregnant, or have declined participation in
the study. The final sample size consistent with the
inclusion and exclusion criteria comprised 68 breast
cancer patients. Ethical clearance for this research has
been obtained from the Ethics Committee for Health
Research, Faculty of Medicine, University of
Lampung, with EC number
2762/UN.26.18/PP.05.02.00/2022.
The data collected in this study included
sociodemographic characteristics (age, education,
occupation, and duration of sun exposure), clinical
information (metastases, types of breast cancer, and
comorbidities), and serum vitamin D levels.
Sociodemographic data were collected through direct
interviews employing a structured questionnaire.
Clinical data were collected from medical record
data. Serum 25-OH vitamin D levels were measured
using the CMIA method by the ARCHITECT
i2000SR immunoassay analyzer at the Prodia Clinical
Laboratory, Jakarta. Vitamin D levels are expressed
in units of ng/mL, where patients are classified as
deficient if their levels fall below 20 ng/mL.
The association between sociodemographic and
clinical characteristics of patients with serum vitamin
D levels was assessed through the Chi-Square test.
Differences in mean serum vitamin D levels in
various comorbid groups were assessed using the
Vitamin D Levels Among Breast Cancer Patients in a Tertiary Hospital in Lampung, Indonesia
131
unpaired t-test and one-way analysis of variance
(ANOVA). All statistical tests were conducted at a
significance level of 95%.
3 RESULTS
3.1 Sample Characteristics
This study included 68 breast cancer patients as a
sample. The average age of the participants was 52.04
years, and 73.5% were over 45 years old.
Predominantly, the sample consisted of homemakers
(38.2%) with a high school education level (32.4%).
Exposure to sunlight was infrequent among most
participants (60.3%), and a significant proportion
reported having no comorbidities (77.9%). Among
the 68 participants, 94.1% were diagnosed with
invasive ductal carcinoma (IDC). Lung metastases
were the most frequent distant metastases (7.4%). The
average vitamin D level among breast cancer patients
was notably low, at 19.6 ng/mL, with the majority
exhibiting either vitamin D deficiency or
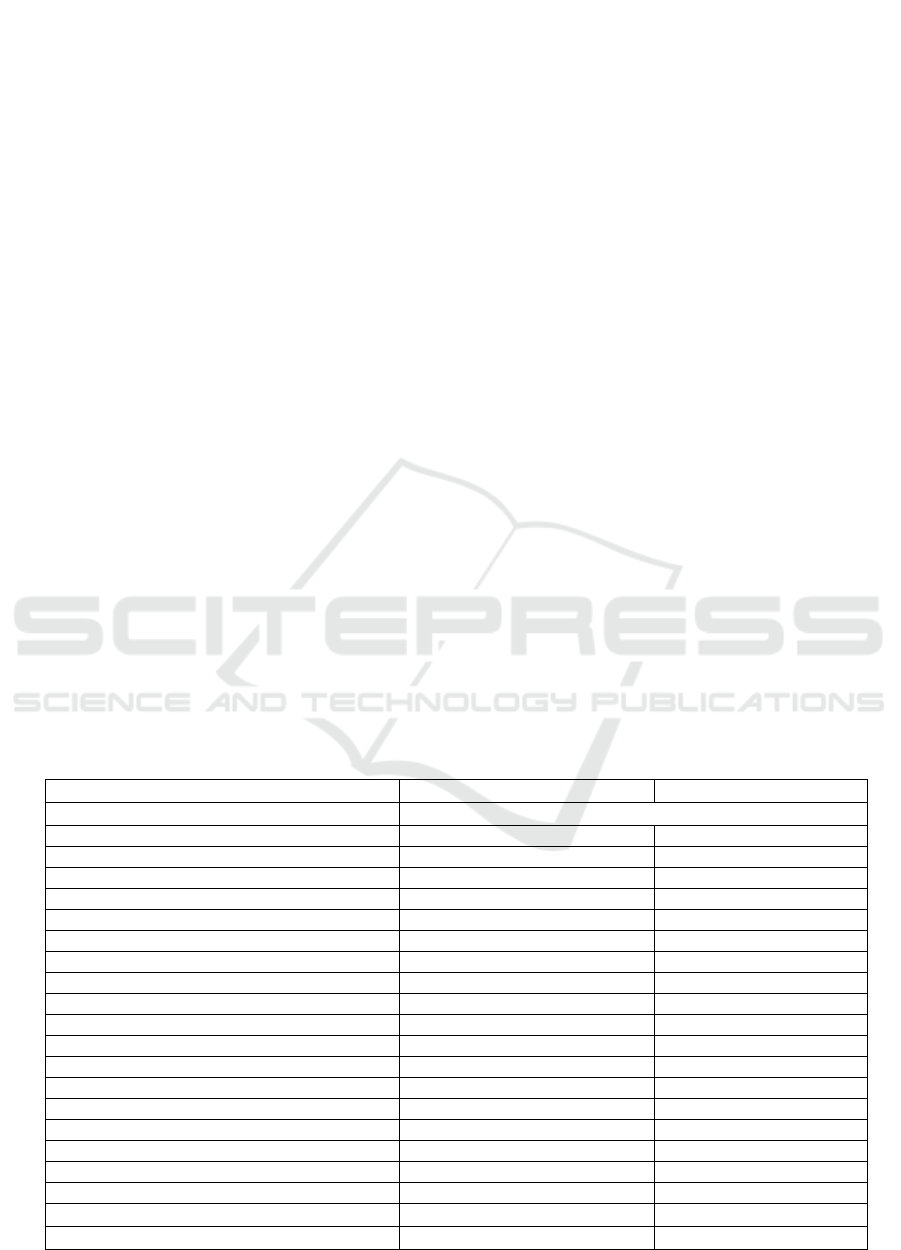
insufficiency, as illustrated in Table 1.
3.2 Association between
Sociodemography Characteristics
and Vitamin D Levels
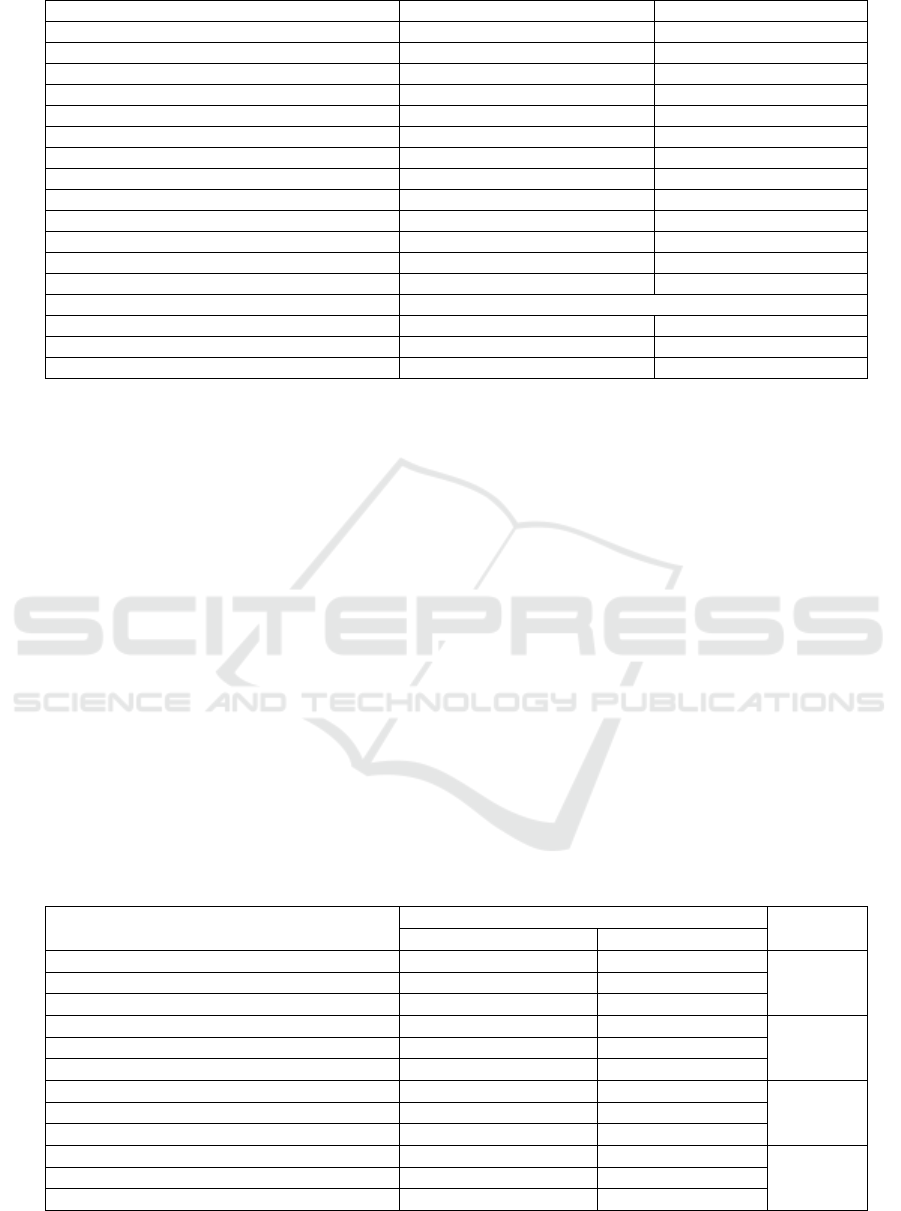
This study's sociodemographic characteristics
included age, education level, occupation, and sun
exposure. Age was categorized into two categories,
namely ≤ 45 years and > 45 years. Education level is
categorized into education up to senior high school
(unschooled, elementary, junior, and senior high
school) and higher education (diploma and bachelor).
Occupational variables are categorized into not-
workers and workers, while sun exposure variables
are categorized into high and low exposure. The Chi-
Square test results found no significant relationship
between these four variables and vitamin D levels
(Table 2).
3.3 Association between Clinical
Characteristics and Vitamin D
Levels
In this study, no significant association was found
between the type of breast cancer, the presence of
metastases, and comorbidities with vitamin D levels
in breast cancer patients (p > 0.05) (Table 3).
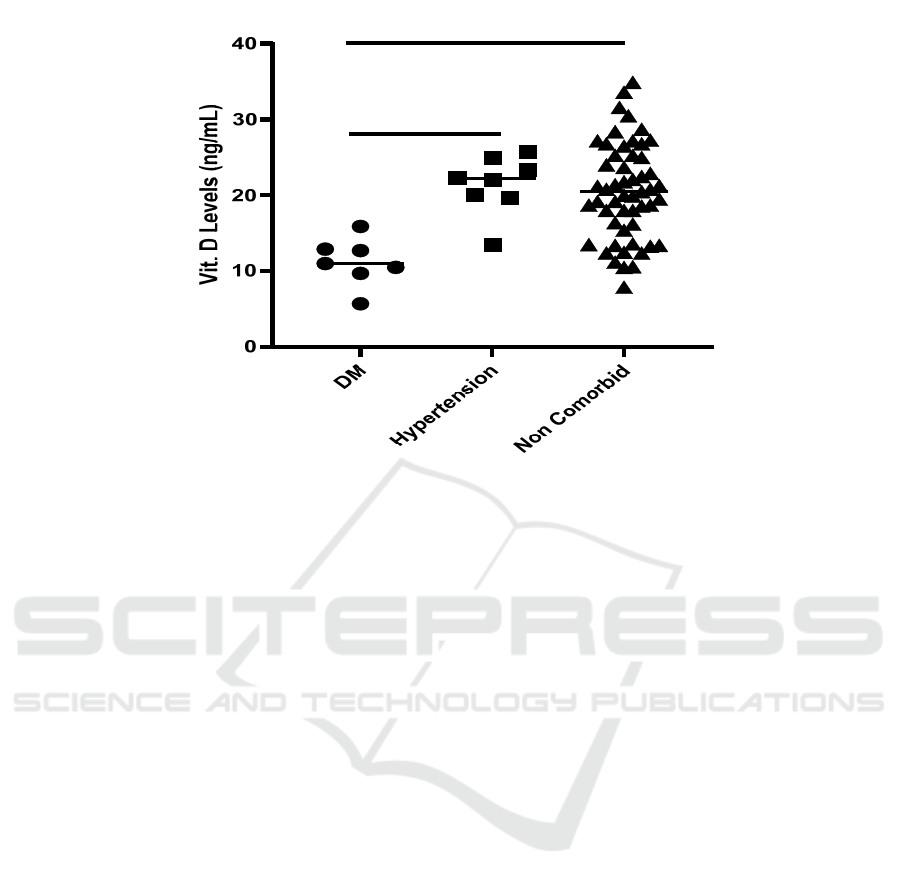
However, the presence of comorbidities appears to
affect vitamin D levels. Breast cancer patients with
comorbidities tend to have lower vitamin D levels
when compared to breast cancer patients without
comorbidities (Table 4). When examined further,
breast cancer patients with comorbid type 2 DM have
significantly lower vitamin D levels when compared
to breast cancer patients with comorbid hypertension
and no comorbid (Figure 1)
Table 1: Distribution of sociodemographic characteristics, tumor profile, and vitamin D levels.
Variable N %
Age, years (Min-Max) 52,04±8,88 (32-73)
-. ≤ 45 years 18 26,5
-. > 45 years 50 73,5
Education
-. Unschoole
d
8 11,8
-. Elementary School 9 13,2
-. Junior High School 9 13,2
-. Senior High School 22 32,4
-. Diploma 7 10,3
-. Bachelo
r
13 19,1
Occupation
-. Civil Servant 4 5,9
-. Private employees 4 5,9
-. Farme
r
15 22,1
-. Laboure
r
1 1,5
-. Housewife 26 38,2
-. Others 18 26,5
Sun Exposure
-. High 27 39,7
-. Low 41 60,3
Comorbid
ICSDH 2023 - The International Conference on Social Determinants of Health
132
-. DM 7 10,3
-. Hypertension 8 11,8
-. No Comorbidities 53 77,9
Type
-. IDC 64 94,1
-. Clear Cell Carcinoma 1 1,5
-. ILC 2 2,9
-. Mixe
d
1 1,5
Distant Metastases
-. Lungs 5 7,4
-. Mammae 1 1,5
-. Subclavicula
r
1 1,5
-. Brain 1 1,5
-. No Metastases 60 88,2
Vitamin D (ng/mL) 19,7±6,5
-. Deficienc
y
35 50,7
-. Insufficienc
y
29 42
-. Sufficienc
y
4 5,8
4 DISCUSSION
Vitamin D can be employed as an additional
supplement in treating breast cancer. Various studies
have proven the ability of this vitamin to induce
apoptosis, inhibit proliferation and angiogenesis, and
reduce the progression and risk of breast cancer
(Lopes et al., 2012; Vanhevel et al., 2022; Vanoirbeek
et al., 2011). Additional investigations have also
proven that high vitamin D levels can reduce the risk
of developing breast cancer (Estébanez et al., 2018;
Shamsi et al., 2020).
This study found that most newly diagnosed
breast cancer patients had vitamin D
deficiency/insufficiency, with an average vitamin D
level of 19.7 ng/mL. This value is lower when
compared to the established reference value for
sufficient vitamin D levels, set at 30 ng/mL (Amrein
et al., 2020). This result aligns with several previous
studies, which found similar results (Imtiaz &
Siddiqui, 2014; Narvaez et al., 2014; Shaukat et al.,
2017). Vitamin D deficiency in breast cancer patients
is recognized for its involvement in the proliferation
of primary tumors and metastases and cancer
aggressiveness (Al-Azhri et al., 2017; Williams et al.,
2016). This phenomenon can be attributed to the
disruption caused by the deficiency in regulating the
signaling of the vitamin D receptor and the metabolic
enzymes CYP27B1 and CYP24A1. These enzymes
facilitate the conversion of serum vitamin D into a
form capable of binding to vitamin D receptors. The
role of vitamin D receptors in suppressing tumor
growth is established; hence, the presence of these
imbalances can curtail their effectiveness in
restraining tumor progression (Voutsadakis, 2020).
Table 2: Association between Sociodemography Characteristics and Vitamin D Levels.
Sociodemography Characteristics
Vitamin D Levels
p
Deficienc
y
Not deficienc
y
Age
0,197
-. > 45
y
ears 19
(
38,0%
)
31
(
62,0%
)
-. ≤ 45
y
ears 10
(
55,6%
)
8
(
44,4%
)
Education
0,429 -. Up to senior high school 19 (39,6%) 29 (60,4%)
-. Higher education 10 (50%) 10 (50%)
Occupation
0,583
-. Worke
r
19
(
45,2%
)
23
(
54,8%
)
-. Not-worke
r
10
(
38,5%
)
16
(
61,5%
)
Sun Ex
p
osure
0,448 -. High 10 (37,0%) 17 (63,0%)
-. Low 19 (46,3%) 22 (53,7%)
Vitamin D Levels Among Breast Cancer Patients in a Tertiary Hospital in Lampung, Indonesia
133
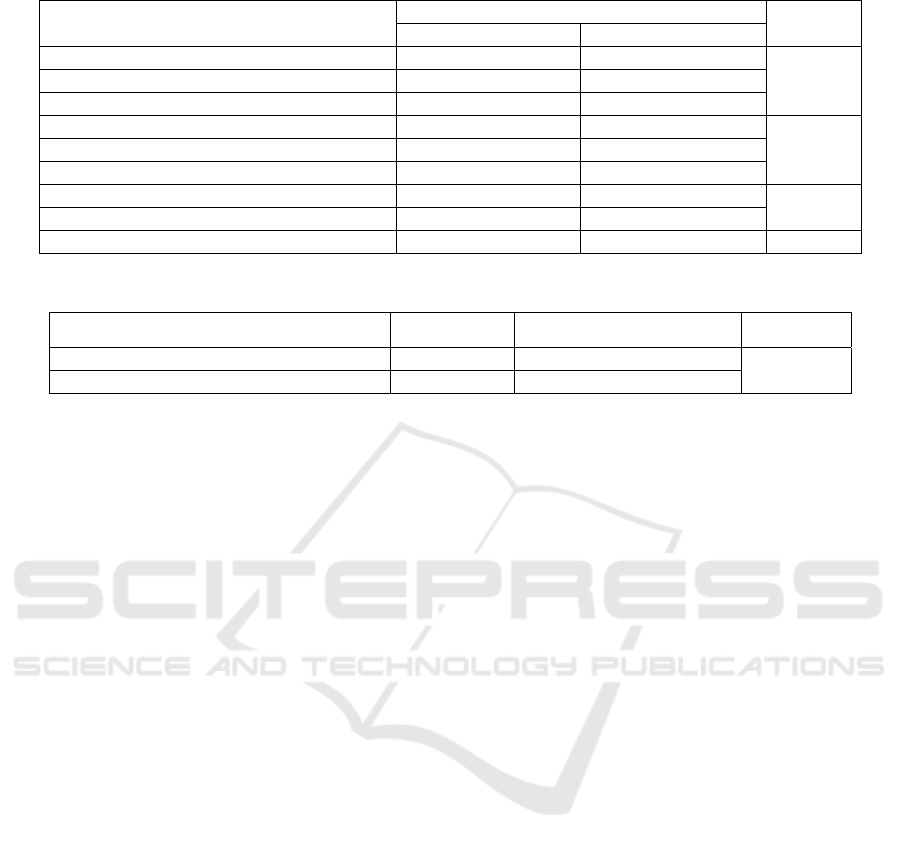
Table 3: Association between Clinical Characteristics and Vitamin D Levels.
Clinical Characteristic
Kadar Vitamin D
p
Deficiency Not deficiency
Metastases
0,715 -. Yes 4 (50%) 4 (50%)
-. No 25 (41,7%) 35 (58,3%)
Type
0,305 -. IDC 26 (40,6%) 38 (59,4%)
-. Non IDC 3 (75,0% 1 (25,0%)
Comorbid
0,343
-. Yes 8 (53,3%) 7 (46,7%)
-. No 21 (39,6%) 32 (60,4%)
Table 4: Difference in Vitamin D Levels between Comorbid and Non-comorbid.
Comorbid n Mean±SD (ng/mL) p
-. Yes 15 16,68±6,32 0,041*
-. No 53 20,54±6,31
Exp: * there is a significant relationship based on the unpaired t-test at α=5%.
This study also revealed that breast cancer
patients with comorbidities exhibited notably reduced
vitamin D levels compared to those without
comorbidities. Moreover, patients with both breast
cancer and type 2 diabetes mellitus (DM) displayed
particularly deficient vitamin D levels. Vitamin D's
interconnection with type 2 DM and hypertension has
been long recognized. The deficiency of vitamin D is
intricately linked to the onset of type 2 DM (Chagas
et al., 2012; Lim et al., 2013) and hypertension (Qi et
al., 2017; Zhang et al., 2017). Among patients with
type 2 DM, an inadequate supply of vitamin D is
responsible for instigating glucose intolerance and
interfering with insulin secretion. This disruption is
attributed to the activity of the vitamin D receptor, or
indirectly, via calcium hormones and inflammatory
processes (Chagas et al., 2012).
Vitamin D deficiency stems from several factors:
sun exposure duration, lifestyle, genetic
predisposition, age, and dietary vitamin D intake.
Interestingly, this study found no association between
vitamin D levels and duration of sun exposure,
lifestyle (education and occupation), and age. This
fact leads us to hypothesize that vitamin D deficiency
in breast cancer patients is more dominantly caused
by a lack of vitamin D intake from food. This
hypothesis gains empirical validation from the
findings of a pivotal study conducted by Alco et al.
(2014). Their investigation reveals that inadequate
vitamin D intake corresponds to a remarkable 28.7-
fold escalation in the risk of vitamin D deficiency or
insufficiency among breast cancer patients (Alco et
al., 2014).
Several studies have shown that vitamin D
supplementation to breast cancer patients can
increase serum vitamin D levels without inducing
toxic manifestations (Alco et al., 2014). While
animal-based experimental studies have
demonstrated a favorable impact of vitamin D
supplementation on breast cancer, clinical
investigations have not shown similar results (de La
Puente-Yagüe et al., 2018; Linowiecka et al., 2021).
Vitamin D supplementation has not shown significant
benefits in the effective treatment of breast cancer
patients (Zemlin et al., 2023). Nevertheless, the
potential benefits of vitamin D supplementation,
particularly in individuals with concurrent type 2
diabetes mellitus (DM) conditions, warrant careful
consideration, given the diminished vitamin D levels
observed in this subgroup. This deliberation is
motivated by the intent to avert other ailments linked
to vitamin D deficiency, such as rickets and
osteoporosis, which can potentially exacerbate the
health status of breast cancer patients.
ICSDH 2023 - The International Conference on Social Determinants of Health
134
✱
✱
Figure 1: Differences in mean vitamin D levels between comorbid groups.
5 CONCLUSIONS
Vitamin D deficiency is commonly observed among
breast cancer patients, especially those with type 2
DM comorbidities. The presence of vitamin D
deficiency in breast cancer patients does not exhibit
any association with sociodemographic attributes or
clinical status. Further information about vitamin D
levels and their association with the survival of breast
cancer patients is still challenging to become research
questions.
ACKNOWLEDGEMENTS
We thank the Higher Education for Technology and
Innovation Project (HETI Project) Universitas
Lampung for supporting this research through the
Innovation and Collaboration Grant 2022.
REFERENCES
Al-Azhri, J., Zhang, Y., Bshara, W., Zirpoli, G., McCann,
S. E., Khoury, T., Morrison, C. D., Edge, S. B.,
Ambrosone, C. B., & Yao, S. (2017). Tumor expression
of vitamin D receptor and breast cancer
histopathological characteristics and prognosis.
Clinical Cancer Research, 23(1), 97–103.
https://doi.org/10.1158/1078-0432.CCR-16-0075
Alco, G., Igdem, S., Dincer, M., Ozmen, V., Saglam, S.,
Selamoglu, D., Erdogan, Z., Ordu, C., Pilanci, K. N.,
Bozdogan, A., Yenice, S., Tecimer, C., Demir, G.,
Koksal, G., & Okkan, S. (2014). Vitamin D levels in
patients with breast cancer: Importance of dressing
style. Asian Pacific Journal of Cancer Prevention,
15(3), 1357–1362. https://doi.org/10.7314/APJCP.20
14.15.3.1357
Amrein, K., Scherkl, M., Hoffmann, M., Neuwersch-
Sommeregger, S., Köstenberger, M., Tmava Berisha,
A., Martucci, G., Pilz, S., & Malle, O. (2020). Vitamin
D deficiency 2.0: an update on the current status
worldwide. European Journal of Clinical Nutrition,
74(11), 1498–1513. https://doi.org/10.1038/s41430-
020-0558-y
Atoum, M., & Alzoughool, F. (2017). Vitamin D and Breast
Cancer: Latest Evidence and Future Steps. Breast
Cancer: Basic and Clinical Research, 11, 1–8.
https://doi.org/10.1177/1178223417749816
Bernhardt, S. M., Borges, V. F., & Schedin, P. (2021).
Vitamin D as a Potential Preventive Agent For Young
Women’s Breast Cancer. Cancer Prevention Research
(Philadelphia, Pa.), 14(9), 825–838.
https://doi.org/10.1158/1940-6207.CAPR-21-0114
Bidgoli, S. A., & Azarshab, H. (2014). Role of vitamin D
deficiency and lack of sun exposure in the incidence of
premenopausal breast cancer: a case control study in
Sabzevar, Iran. Asian Pacific Journal of Cancer
Prevention : APJCP, 15(8), 3391–3396. https://doi.o
rg/10.7314/APJCP.2014.15.8.3391
Buja, A., Pierbon, M., Lago, L., Grotto, G., & Baldo, V.
(2020). Breast Cancer Primary Prevention and Diet: An
Umbrella Review. International Journal of
Vitamin D Levels Among Breast Cancer Patients in a Tertiary Hospital in Lampung, Indonesia
135

Environmental Research and Public Health, 17(13), 1–
54. https://doi.org/10.3390/IJERPH17134731
Chagas, C. E. A., Borges, M. C., Martini, L. A., & Rogero,
M. M. (2012). Focus on Vitamin D, Inflammation and
Type 2 Diabetes. Nutrients, 4(1), 52. https://doi.org/
10.3390/NU4010052
Chen, Y., & Zhi, X. (2020). Vitamin D Status in Population
Functions of Vitamin D in the Reproductive System.
Endocrinology, 161(4), 1–12.
https://doi.org/10.1210/endocr/bqaa023
Choudhury, H., Pandey, M., Wen, L. P., Cien, L. K., Xin,
H., Yee, A. N. J., Lee, N. J., Gorain, B., Amin, M. C. I.
M., & Pichika, M. R. (2020). Folic Acid Conjugated
Nanocarriers for Efficient Targetability and Promising
Anticancer Efficacy for Treatment of Breast Cancer: A
Review of Recent Updates. Current Pharmaceutical
Design, 26(42), 5365–5379. https://doi.org/10
.2174/1381612826666200721000958
Cosentino, N., Campodonico, J., Milazzo, V., De Metrio,
M., Brambilla, M., Camera, M., Marenzi, G.,
Johansson, H., Serrano, D., Raimondi, S., Gnagnarella,
P., & Dominguez, L. J. (2021). Vitamin D and
Cardiovascular Disease: Current Evidence and Future
Perspectives. Nutrients 2021, Vol. 13, Page 3603,
13(10), 3603. https://doi.org/10.3390/NU13103603
de La Puente-Yagüe, M., Cuadrado-Cenzual, M. A.,
Ciudad-Cabañas, M. J., Hernández-Cabria, M., &
Collado-Yurrita, L. (2018). Vitamin D: And its role in
breast cancer. The Kaohsiung Journal of Medical
Sciences, 34(8), 423–427. https://doi.org/10.1016/J.
KJMS.2018.03.004
Estébanez, N., Gómez-Acebo, I., Palazuelos, C., Llorca, J.,
& Dierssen-Sotos, T. (2018). Vitamin D exposure and
Risk of Breast Cancer: a meta-analysis. Scientific
Reports, 8(1). https://doi.org/10.1038/S41598-018-
27297-1
Forouhi, N. G., Ye, Z., Rickard, A. P., Khaw, K. T., Luben,
R., Langenberg, C., & Wareham, N. J. (2012).
Circulating 25-hydroxyvitamin D concentration and the
risk of type 2 diabetes: results from the European
Prospective Investigation into Cancer (EPIC)-Norfolk
cohort and updated meta-analysis of prospective studies.
Diabetologia, 55(8), 2173–2182.
https://doi.org/10.1007/S00125-012-2544-Y
Giovannucci, E. (2009). Vitamin D and cancer incidence in
the Harvard cohorts. Annals of Epidemiology, 19(2), 84–
88.
https://doi.org/10.1016/J.ANNEPIDEM.2007.12.002
Grabiec, M., Walentowicz, P., Sadłecki, P., & Walentowicz-
Sadłecka, M. (2013). The role of vitamin D in the
carcinogenesis of breast and ovarian cancer. Polish
Gynaecology, 84(4). https://doi.org/10.17772/gp/1581
Green, T. J., Skeaff, C. M., Rockell, J. E. P., Venn, B. J.,
Lambert, A., Todd, J., Khor, G. L., Loh, S. P.,
Muslimatun, S., Agustina, R., & Whiting, S. J. (2008).
Vitamin D status and its association with parathyroid
hormone concentrations in women of child-bearing age
living in Jakarta and Kuala Lumpur. European Journal
of Clinical Nutrition, 62(3), 373–378.
https://doi.org/10.1038/SJ.EJCN.1602696
Imtiaz, S., & Siddiqui, N. (2014). Vitamin-D status at breast
cancer diagnosis: correlation with social and
environmental factors and dietary intake. Journal of
Ayub Medical College, Abbottabad : JAMC, 26(2), 186–
190.
Janoušek, J., Pilařová, V., Macáková, K., Nomura, A., Veiga-
Matos, J., Silva, D. D. da, Remião, F., Saso, L., Malá-
Ládová, K., Malý, J., Nováková, L., & Mladěnka, P.
(2022). Vitamin D: sources, physiological role,
biokinetics, deficiency, therapeutic use, toxicity, and
overview of analytical methods for detection of vitamin
D and its metabolites. Critical Reviews in Clinical
Laboratory Sciences, 59(8), 517–554.
https://doi.org/10.1080/10408363.2022.2070595
Kazemi, S. M., Esmaieli-bandboni, A., Veisi Malekshahi, Z.,
Shahbaz Sardood, M., Hashemi, M., Majidzadeh, K.,
Kadkhodazadeh, M., Esmaili, R., & Negahdari, B.
(2022). Vitamin D receptor gene polymorphisms and risk
of breast cancer in Iranian women. Annals of Medicine
and Surgery, 73(December 2021), 103150.
https://doi.org/10.1016/j.amsu.2021.103150
Kim, Y., Franke, A. A., Shvetsov, Y. B., Wilkens, L. R.,
Cooney, R. V., Lurie, G., Maskarinec, G., Hernandez, B.
Y., Le Marchand, L., Henderson, B. E., Kolonel, L. N.,
& Goodman, M. T. (2014). Plasma 25-hydroxyvitamin
D3 is associated with decreased risk of postmenopausal
breast cancer in whites: A nested case-control study in
the multiethnic cohort study. BMC Cancer, 14(1), 1–7.
https://doi.org/10.1186/1471-2407-14-29/COMMENTS
Lim, S., Kim, M. J., Choi, S. H., Shin, C. S., Park, K. S., Jang,
H. C., Billings, L. K., & Meigs, J. B. (2013). Association
of vitamin D deficiency with incidence of type 2 diabetes
in high-risk Asian subjects. The American Journal of
Clinical Nutrition, 97(3), 524.
https://doi.org/10.3945/AJCN.112.048496
Linowiecka, K., Wolnicka-Głubisz, A., & Brożyna, A. A.
(2021). Vitamin D endocrine system in breast cancer.
Acta Biochimica Polonica, 68(4), 489–497.
https://doi.org/10.18388/ABP.2020_5961
Lopes, N., Paredes, J., Costa, J. L., Ylstra, B., & Schmitt, F.
(2012). Vitamin D and the mammary gland: a review on
its role in normal development and breast cancer. Breast
Cancer Research : BCR, 14(3). https://doi.org/10.1186
/BCR3178
Mattiuzzi, C., & Lippi, G. (2019). Current Cancer
Epidemiology. Journal of Epidemiology and Global
Health, 9(4), 217–222. https://doi.org/10.2991/JEG
H.K.191008.001
Mazahery, H., & Von Hurst, P. R. (2015). Factors Affecting
25-Hydroxyvitamin D Concentration in Response to
Vitamin D Supplementation. Nutrients, pp. 7, 5111–
5142. https://doi.org/10.3390/nu7075111
Narvaez, C. J., Matthews, D., LaPorta, E., Simmons, K. M.,
Beaudin, S., & Welsh, J. E. (2014). The impact of
vitamin D in breast cancer: genomics, pathways,
metabolism. Frontiers in Physiology, p. 5.
https://doi.org/10.3389/FPHYS.2014.00213
Octavius, G. S., Daleni, V. A., Angeline, G., & Virliani, C.
(2023). A systematic review and meta-analysis of the
prevalence of vitamin D deficiency among Indonesian
ICSDH 2023 - The International Conference on Social Determinants of Health
136

pregnant women: a public health emergency. AJOG
Global Reports, 3(2), 100189. https://doi.org/10.101
6/j.xagr.2023.100189
Qi, D., Nie, X. L., Wu, S., & Cai, J. (2017). Vitamin D and
hypertension: Prospective study and meta-analysis.
PloS One, 12(3). https://doi.org/10.1371/JOURNAL.
PONE.0174298
Ren, X., Xu, P., Zhang, D., Liu, K., Song, D., Zheng, Y.,
Yang, S., Li, N., Hao, Q., Wu, Y., Zhai, Z., Kang, H.,
& Dai, Z. (2020). Association of folate intake and
plasma folate level with the risk of breast cancer: a
dose-response meta-analysis of observational studies.
Aging, 12(21), 21355–21375. https://doi.org/10.1863
2/AGING.103881
Setiati, S. (2008). Vitamin D status among Indonesian
elderly women living in institutionalized care units.
Acta Med Indonesia, 40(2), 78–83.
Shamsi, U., Khan, S., Azam, I., Khan, A. H., Maqbool, A.,
Hanif, M., Gill, T., Iqbal, R., & Callen, D. (2020). A
multicenter case control study of association of vitamin
D with breast cancer among women in Karachi,
Pakistan. PLOS ONE, 15(1), e0225402. https://doi.org/
10.1371/JOURNAL.PONE.0225402
Shaukat, N., Jaleel, F., Moosa, F. A., & Qureshi, N. A.
(2017). Association between Vitamin D deficiency and
Breast Cancer. Pakistan Journal of Medical Sciences,
33(3), 645–649. https://doi.org/10.12669/pjms.333.
11753
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M.,
Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global
Cancer Statistics 2020: GLOBOCAN Estimates of
Incidence and Mortality Worldwide for 36 Cancers in
185 Countries. CA: A Cancer Journal for Clinicians,
71(3), 209–249. https://doi.org/10.3322/CAAC.21660
Susanti, M., Widjaja, S. S., & Siregar, D. R. (2018).
Pengaruh Vitamin D terhadap Indeks Apoptosis pada
Penderita Kanker Payudara. Jurnal Kesehatan Andalas,
7(2), 182–186. https://doi.org/10.25077/JKA.V7I2.799
Vanhevel, J., Verlinden, L., Doms, S., Wildiers, H., &
Verstuyf, A. (2022). The role of vitamin D in breast
cancer risk and progression. Endocrine-Related
Cancer, 29(2), R33–R55. https://doi.org/10.1530/ERC-
21-0182
Vanoirbeek, E., Krishnan, A., Eelen, G., Verlinden, L.,
Bouillon, R., Feldman, D., & Verstuyf, A. (2011). The
Anticancer and Anti-Inflammatory Actions of
1,25(OH)2D3. Best Practice & Research. Clinical
Endocrinology & Metabolism, 25(4), 593.
https://doi.org/10.1016/J.BEEM.2011.05.001
Voutsadakis, I. A. (2020). Vitamin D receptor (VDR) and
metabolizing enzymes CYP27B1 and CYP24A1 in
breast cancer. Molecular Biology Reports
, 47(12),
9821–9830. https://doi.org/10.1007/S11033-020-
05780-1/METRICS
Williams, J. D., Aggarwal, A., Swami, S., Krishnan, A. V.,
Ji, L., Albertelli, M. A., & Feldman, B. J. (2016).
Tumor Autonomous Effects of Vitamin D Deficiency
Promote Breast Cancer Metastasis. Endocrinology,
157(4), 1341–1347. https://doi.org/10.1210/EN.2015-
2036
Zemlin, C., Altmayer, L., Stuhlert, C., Schleicher, J. T.,
Wörmann, C., Lang, M., Scherer, L. S., Thul, I. C.,
Spenner, L. S., Simon, J. A., Wind, A., Kaiser, E.,
Weber, R., Goedicke-Fritz, S., Wagenpfeil, G., Zemlin,
M., Solomayer, E. F., Reichrath, J., & Müller, C.
(2023). Prevalence and Relevance of Vitamin D
Deficiency in Newly Diagnosed Breast Cancer
Patients: A Pilot Study. Nutrients, 15(6), 1–12.
https://doi.org/10.3390/nu15061450
Zhang, R., Li, B., Gao, X., Tian, R., Pan, Y., Jiang, Y., Gu,
H., Wang, Y., Wang, Y., & Liu, G. (2017). Serum 25-
hydroxyvitamin D and the risk of cardiovascular
disease: dose-response meta-analysis of prospective
studies. The American Journal of Clinical Nutrition,
105(4), 810–819. https://doi.org/10.3945/AJCN
\.116.140392
Zheng, Y., Trivedi, T., Lin, R. C., Fong-Yee, C., Nolte, R.,
Manibo, J., Chen, Y., Hossain, M., Horas, K., Dunstan,
C., Zhou, H., & Seibel, M. J. (2017). Loss of the vitamin
D receptor in human breast and prostate cancers
strongly induces cell apoptosis through downregulation
of Wnt/β-catenin signaling. Bone Research, 5.
https://doi.org/10.1038/BONERES.2017.23
Vitamin D Levels Among Breast Cancer Patients in a Tertiary Hospital in Lampung, Indonesia
137
