
An Android App for Training New Doctors in Mechanical Ventilation
Andrea Bombarda
1 a
, Sara Noto Millefiori
1
, Michela Penzo
1
, Luca Novelli
2 b
and Angelo Gargantini
1 c
1
Department of Management, Information and Production Engineering, University of Bergamo, Bergamo, Italy
2
Pulmonary medicine Unit, ASST Papa Giovanni XXIII, Bergamo, Italy
{s.notomillefiori, m.penzo1}@studenti.unibg.it
Keywords:
Mobile Application, Mechanical Ventilation, Application Prototype, Training.
Abstract:
Mechanical ventilation is essential for critically ill patients, as recently demonstrated by the COVID-19 pan-
demic. The experience of physicians in correctly selecting ventilation parameters and values plays a crucial
role in ensuring the best possible outcome. In order to aid physicians in setting up a mechanical ventilator,
several brands have implemented in their products an adaptive ventilation mode called Adaptive Support Venti-
lation (ASV). This mode automatically selects pressure and respiratory rate to require the patient the minimum
breathing effort possible. However, physicians are generally skeptical about adopting this ventilation mode, as
they prefer to have all parameters under their control. Nevertheless, we believe that comprehending how ASV
works is paramount important, to understanding the patterns used, and possibly exploiting them while manu-
ally setting mechanical ventilators. For this reason, in this paper, we present Ventilation App, an Android
app for training new physicians in mechanical ventilation. It allows the simulation of a ventilation process
for a patient unable to breathe and gives feedback to the user by exploiting the same operating principles of
the ASV mode. Thanks to the feedback received by a collaborating physician, we believe that our app can be
useful for allowing physicians-in-training to acquire proficiency in mechanical ventilation.
1 INTRODUCTION
Mechanical ventilation plays a crucial role in the
treatment of critically ill patients, and the proficiency
of physicians in this area is vital to provide optimal
patient care. However, acquiring the necessary skills
and knowledge in mechanical ventilation can be a
challenging task, as it requires a deep understand-
ing of complex respiratory physiology and the abil-
ity to interpret and adjust ventilation parameters ef-
fectively. To solve this issue, automatic ventilation
strategies such as the Adaptive Support Ventilation
(ASV) modes have been proposed. In this way, the
mechanical ventilator automatically defines the ven-
tilation parameters and values based on the patient’s
respiratory mechanics, and by computing them by us-
ing the Otis’ curve (Fern
´
andez et al., 2013). However,
the complexity of ASV can give rise to concerns and
skepticism among healthcare professionals. Physi-
cians may question its efficacy and reliability, espe-
a
https://orcid.org/0000-0003-4244-9319
b
https://orcid.org/0000-0002-2705-248X
c
https://orcid.org/0000-0002-4035-0131
cially when compared to traditional modes of venti-
lation that they are more familiar with and that allow
them to manually manage the ventilation parameters.
Additionally, most clinicians may be hesitant to fully
embrace ASV due to a lack of comprehensive train-
ing or limited exposure to its implementation in real-
world clinical settings.
To bridge this gap and facilitate the learning pro-
cess for aspiring physicians, in this paper, we in-
troduce an Android application aimed at enhancing
training in mechanical ventilation by taking advan-
tage of the mechanisms used by the ASV strategy,
used by ventilators when automatically deciding the
ventilation strategy. It is based on the principle of
learning by doing, i.e., it lets the user manually set
the ventilation parameters after having decided on the
physiological and mechanical characteristics of the
patient. Then, the app simulates the mechanical ven-
tilation and gives feedback to the user by using the
measured effort and its distance from the optimal, i.e.,
the minimum one computed using the Otis equation
as automatically done by mechanical ventilators em-
ploying the ASV mode. In this way, physicians-in-
362
Bombarda, A., Millefiori, S., Penzo, M., Novelli, L. and Gargantini, A.
An Android App for Training New Doctors in Mechanical Ventilation.
DOI: 10.5220/0012323900003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 362-369
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.

training can understand the ventilation patterns used
by the ASV mode and, possibly, exploit them while
manually setting mechanical ventilators.
With this paper, our contribution is twofold. On
the one hand, we contribute our Android app allowing
physicians to train with mechanical ventilation. On
the other hand, we apply the paradigm of learning-
by-doing in the context of healthcare, especially de-
voted to increasing the understanding of physicians
in automatic procedures that are normally avoided for
lack of confidence. This approach can be generalized
to other fields, beyond mechanical ventilation, where
simulators are available.
The remainder of the paper is structured as fol-
lows. Sect. 2 presents the background on mechanical
ventilation, including operating principles and modes.
Moreover, it includes a brief analysis of existing An-
droid apps for training new physicians in terms of me-
chanical ventilation. In Sect. 3, we report the require-
ments and the architecture of the application we pro-
pose in this paper. Sect. 4 presents the implemented
app and explains its functioning. Finally, Sect. 5 re-
ports related work on apps for training physicians in
different fields, while Sect. 6 reports future work di-
rections and concludes the paper.
2 BACKGROUND
In this section, we report some background on the ba-
sis of mechanical ventilation, together with an analy-
sis of already existing apps for training physicians in
using mechanical ventilators.
2.1 Mechanical Ventilation
Artificial mechanical ventilation replaces (or inte-
grates) the activity of the inspiratory muscles to en-
sure a sufficient supply of gas to the lungs. It is a nec-
essary tool in every modern intensive care unit (ICU).
The type and intensity of ventilation support required
by a patient vary over the course of treatment. Modern
mechanical ventilators are versatile and adapt to pa-
tient needs. They support patients who cannot breathe
or those who can still trigger a mechanical cycle by a
spontaneous inspiratory effort. Present-day mechan-
ical ventilators are complex machines, consisting of
many specialized components and featuring several
ventilation modes, which have to be set depending
on the conditions of the patients. There are numer-
ous conditions in which it is necessary to resort to
mechanical ventilation, for example in all those con-
ditions in which spontaneous natural breathing is not
possible (e.g., in the case of acute respiratory distress
syndrome - ARDS - or chronic obstructive pulmonary
disease - COPD).
Ventilation Modes. Depending on the patient and
the type of ventilator available, several ventilation
modes (i.e., specific combinations of breathing pat-
terns, control types, and operational algorithms) are
available in the products on the market, and the most
common are those based on pressure or volume con-
trol. Most of them operate in an open-loop way.
For what concerns volume-control ventilation
modes, the two most common modes are Mandatory
Minute Ventilation (MMV) and Controlled Manda-
tory Ventilation (CMV). With the former, the ventila-
tor provides a predetermined minute ventilation (i.e.,
a pre-defined volume of air) when the patient’s spon-
taneous breathing effort becomes inadequate (e.g., be-
cause of an apnea). When this occurs, the manda-
tory frequency is increased automatically to compen-
sate for the decrease in minute ventilation caused by
the apnea and to ensure the desired minute venti-
lation. With the latter, the ventilator controls both
the patient’s tidal volume (i.e., the volume of air in-
spired/expired in each breath) and respiratory rate. In
practice, the ventilator controls the patient’s minute
volume. This means that a patient cannot change the
ventilator frequency or breathe spontaneously.
Instead, the two main pressure-control ventilation
modes are Pressure Controlled Ventilation (PCV) and
Pressure Support Ventilation (PSV). In PCV mode,
the ventilator controls the timing of the breathing cy-
cle and regulates the pressure applied to the patient.
PCV mode is used in the acute phase of the disease
when patients are deeply sedated or paralyzed, and
cannot breathe themselves. On the other hand, PSV is
an assisted ventilatory mode that is patient-triggered,
pressure-limited, and flow-cycled. The main use of
this mode is for the weaning of the patient from me-
chanical ventilation because it gradually unloads the
work of breathing.
Ventilation Parameters. Depending on the venti-
lation mode, different parameters have to be set by
the physicians. In the following, a brief explanation
of the main ventilation parameters we exploit in the
work presented in this paper is given.
The respiratory rate (RR) indicates the number of
breaths per minute the patient has to take. For each
breath, the ratio between the inspiratory and expira-
tory times is set through the parameter I:E. During
the inspiration phase, the ventilator reaches the maxi-
mum pressure P
max
, which has to be set accurately in
order not to damage the patient’s lung with too high
pressure. On the other hand, during the expiration
An Android App for Training New Doctors in Mechanical Ventilation
363
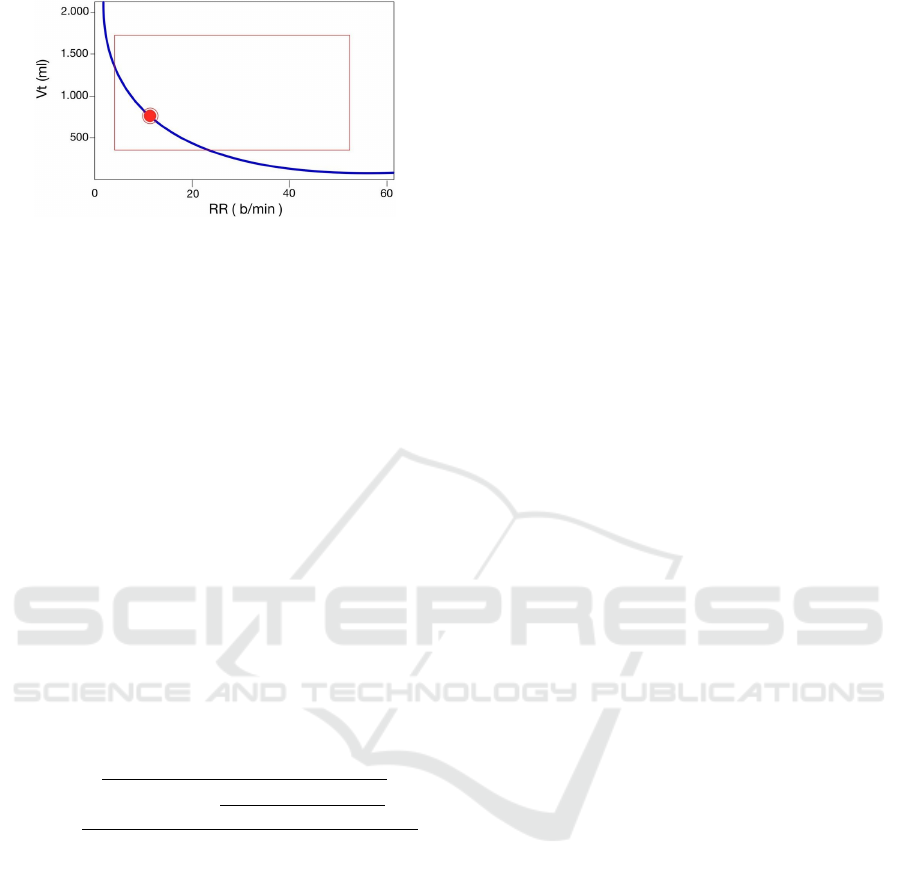
Figure 1: Example of the Otis curve for the minimal WOB.
The red dot indicates the optimal target ventilation point.
phase, the ventilator sets its pressure to the positive
end-expiratory pressure (PEEP), which is greater than
zero to prevent the collapse of the airway.
2.2 Adaptive Support Ventilation
Adaptive support ventilation (ASV) is a mechanical
ventilation mode that operates in a closed-loop sys-
tem, adjusting the ventilator’s output for each breath.
It utilizes the patient’s measured mechanical charac-
teristics (e.g., airway resistance and compliance) and
breathing effort to determine the appropriate level of
ventilatory support. The primary objective of ASV is
to deliver a predetermined level of alveolar ventila-
tion while minimizing the combined work of breath-
ing (WOB) for both the patient and the ventilator.
ASV can provide complete or partial ventilatory sup-
port and is applicable during mechanical ventilation’s
initiation, maintenance, or weaning stages. The venti-
lation pattern is automatically decided by the ventila-
tor for reducing the WOB based on the Otis equation
RR(t) =
r
1 +2 · a · RC
e
·
V
min
− RR(t − 1) ·V
D
V
D
− 1
a · RC
e
where RC
e
is the expiratory time constant (defined
through the resistance R and compliance C of the pa-
tient’s airway), V
min
is the target minute ventilation,
V
D
represents the dead space volume (computed as
2.2 · IBW , where IBW is the ideal body weight), a is
a factor depending on the flow waveform (e.g., it is
0.329 for sinusoidal flows), and RR is the respiratory
rate, i.e., the number of breaths per minute. Based
on Otis’s observations, if the ventilation pattern (res-
piratory rate and tidal volume) satisfies the proposed
equation, then the effort requested to the patient for
breathing is reduced to the minimum.
The ASV mode uses the Otis equation and con-
siders the curve in Fig. 1 for automatically adapt-
ing the respiratory rate (RR) and the tidal volume
(V
t
=
V
min
/RR), i.e., the volume inspired or expired dur-
ing a single respiratory cycle. Based on this curve,
every ventilation pattern that guarantees to stay on the
blue line is optimal and lowers the patient’s effort to
the minimum possible.
Note that the Otis curve identifies some safety lim-
its (see the red rectangle in Fig. 1), which are used by
ventilators when working in the ASV mode in order
to raise alarms and avoid dangerous conditions. In
terms of respiratory rate (x-axis in Fig. 1), the lower
limit is 5 respiratory cycles per minute, while the up-
per bound is computed as
20
/(R ·C) and, in any case, the
respiratory rate cannot exceed 60 breaths per minute.
On the other hand, in terms of tidal volume V
t
(y-
axis in Fig. 1), the safety limits depend on the pa-
tient’s IBW. Indeed, the minimum tidal volume can be
4.4
ml
/kg · IBW , while the maximum is 22
ml
/kg · IBW
and, in any case, the pressure applied by the ventilator
in order to achieve the intended tidal volume has to be
lower than 45cmH
2
O.
Despite being automatic, the ASV mode is nor-
mally avoided by physicians who prefer to manually
set ventilation parameters in order to keep them under
control. However, we believe that it is essential for
every doctor to understand how ASV works. In this
way, physicians can learn some of the patterns that are
normally used by ASV and integrate them into their
manually defined settings. This is the rationale behind
the application we propose in this paper.
2.3 Existing Apps for Training in
Mechanical Ventilation
Before starting the design of our app, we analyzed
existing applications related to training in mechanical
ventilation. With this analysis, we found four apps. In
the following, we give a brief overview of their fea-
tures and the differences between them and the appli-
cation we propose in this paper.
TruVent App (TruCorp, 2023) is a training appli-
cation in which the trainer and the physician interact.
The former sets patient characteristics, while the lat-
ter monitors and performs actions based on patient
status, which the trainer can continuously modify by
simulating different clinical conditions. However, the
TruVent App is not based on ASV nor uses the Otis
curve to give users feedback, as we do in our app.
Similarly, Ventsim (Ventsim, 2023) simulates interac-
tions between a patient and a ventilator and generates
waveforms. Different modes of ventilation are imple-
mented, and clinical scenarios can be tested by chang-
ing the ventilator and patient settings. However, as
TruVent App, it does not offer a way for the physician
to understand whether the settings are those leading
to the minimum breathing effort for the patient.
VentilO (IUCPQ, 2023) aims at training physi-
HEALTHINF 2024 - 17th International Conference on Health Informatics
364

cians in reasoning on how different values for the ven-
tilation parameters may influence the patient’s condi-
tion. Nevertheless, VentilO only implements volume-
based ventilation modes and, thus, the pressure-
controlled ones we want to deal with are not sup-
ported, nor training for users is given in those cases.
Finally, OpenPediatrics (OpenPediatrics, 2023)
provides a ventilator simulator embedding the most
recent pediatric and adult ventilation guidelines, as
well as COVID-19 information and COVID-19 pa-
tient cases. As for the TruVent app, the ventilator
simulator provided by OpenPediatrics is not based on
ASV nor uses the Otis curve to give users feedback,
as we do in our proposed app.
We can conclude that, to the best of our knowl-
edge, no Android app with the same operating princi-
ples as those we embed in Ventilation App exists.
3 APP DESIGN
At the beginning of the development process, we held
several meetings with physicians and experts to have
a deep understanding of how mechanical ventilation
works, especially in the context of the ASV mode,
and of the most perceived difficulties by physicians-
in-training when approaching this ventilation strat-
egy. Then, together with physicians and experts, and
thanks to the experience gained in the past by groups
working on the development of mechanical ventila-
tors (e.g., for treating patients affected by COVID-19
in ICUs) (Abba et al., 2021; Bombarda et al., 2021;
Bombarda et al., 2022; Pearce, 2020), we defined the
functional requirements of the Android app for train-
ing new doctors in mechanical ventilation. In this
way, we have been able to identify critical features
and isolate those that were not of interest for the sce-
nario we wanted to deal with, i.e., that of the ASV
mode. Then, the app architecture has been defined
according to the identified requirements.
3.1 Functional Requirements
During the process of the development of our An-
droid app, we started by individuating the require-
ments, which were then formalized in the Software
Requirements Specification document. For each re-
quirement, we have identified a description (some-
times with a rationale, when it was provided by the
experts we contacted) and an ID. In the Software Re-
quirements Specification, we have identified 4 differ-
ent modes, and, for each of them, we have defined
the set of needed requirements. In the following, we
describe each mode in detail.
Startup Mode: In startup mode, the Android app
shows the logo and offers the user the possibility to
start using the app (see Settings mode) or to view in-
formation on its operating principles (see Info mode).
Info Mode: In the info mode, the Android app
reports a message explaining its operating principle,
including the thresholds used for defining when the
breathing effort is low, medium, or high.
Settings Mode: In the settings mode, the user is
requested to set all the required parameters for the
simulation, i.e., both those of the patient and those of
the ventilator. For what concerns the patient, the app
asks the user to insert the gender, age, weight, height
(used to calculate the IBW), airway resistance, and
compliance. Then, for what concerns the ventilator,
the user must insert the basic ventilation parameters,
i.e., the PEEP value, the P
max
, the I:E fraction, and the
respiratory rate. When in this mode, the user may save
the data previously set into an embedded database, in
order to load them in another simulation, or load the
data from those previously saved. When all the pa-
rameters are set, the user may proceed by starting the
Simulation mode or by closing the app.
Simulation Mode: The simulation mode is the
core mode of the Android application. By using all
the data provided by the user during the Patient pa-
rameters set mode, it simulates the patient’s breath-
ing when the mechanical ventilator works in PCV
mode, i.e., when the patient is not able to breathe
autonomously. During the simulation, two plots are
shown: one that reports the pressure over time, and
one showing the flow over time. In order to allow
users to understand the effect and level of correctness
of the settings, during simulation mode, a semaphore
is shown: the green light is highlighted when the mea-
sured effort is equal to the minimum possible (see
the Otis’ equation in Sect. 2.2) with a tolerance of
±150, the yellow light is highlighted when the mea-
sured effort is distant from the optimal one from ±150
to ±300, otherwise, the red light is shown. These
threshold values have been discussed and approved
by physicians and have been derived from the exam-
ples given in the operator’s manual of the Hamilton
Galileo ventilator
1
, which embeds the ASV mode.
As previously explained in Sect. 2.2, safety lim-
its are identified by the ASV mode. The red light
is shown even if the chosen ventilation pattern does
not imply a high effort for the patient, but it is out-
side those safety limits. When in simulation mode,
the user may change some configuration parameters
(see Settings mode), freeze the simulation (see Freeze
mode), or stop the simulation and close the app.
1
https://bit.ly/3Zh4PIy
An Android App for Training New Doctors in Mechanical Ventilation
365
Exit
Click
Start
Simulation
Settings
Click
Freeze
Freeze
Simulation
after insp.
duration
Inspiration
after expiration duration
Expiration
Click Stop
Simulation
Click Stop Simulation
Click
Resume
Adjust parameters
Open
App
Exit
Click Start
Startup
View Info
Click Info
Close
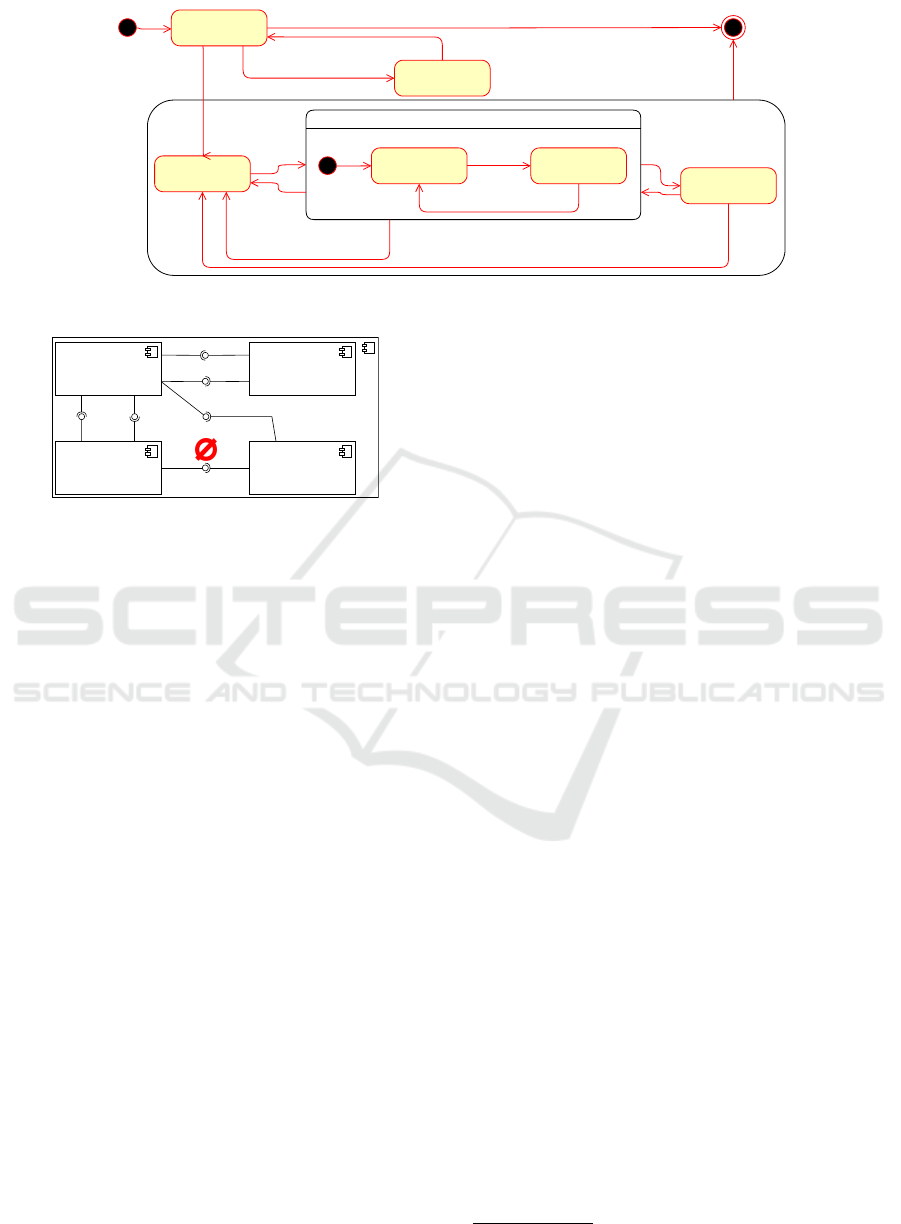
Figure 2: State machine.
«Component»
INSPIRE
«Database»
PatientDB
«Component»
GUI
«Component»
Ventilator
Figure 3: High-level software architecture.
Freeze Mode: The freeze mode can be activated
by the user during the simulation. When the freeze
mode is active, the simulation pauses and the user
can visualize the plot details in order to better under-
stand the patient’s condition. Users may exit from the
freeze mode by restarting the simulation (see Simula-
tion mode) or by stopping the simulation and setting
new patient parameters (see Settings mode).
A general overview of the transitions between the
application modes and the functionalities is given in
the state machine in Fig. 2, while a diagram showing
the interaction between actors and software artifacts
is available in our open-source repository at https://
github.com/foselab/VentilationApp.
3.2 App Architecture
The high-level architecture of the training app is re-
ported in Fig. 3. It is composed of 4 main compo-
nents. The INSPIRE component implements the pa-
tient simulation logic. It handles the electronic equiv-
alent of human lungs (van Diepen et al., 2021), com-
posed by the resistance R and compliance C set by
the user through the GUI, and when a defined pres-
sure is applied by the ventilator, it computes the cur-
rent flow and pressure in the patient’s airway. The
Ventilator component reads the ventilator’s param-
eters from the GUI and simulates a simple mechanical
ventilator working in PCV mode (see Sect. 2.1). It
sets the pressure (between the PEEP and P
max
val-
ues) and sends its value to the INSPIRE component,
through a ZeroMQ
2
communication channel, which
executes a single simulation step. The PatientDB
stores the patient and ventilator parameters saved by
the user in previous simulations. It is also used by the
GUI for loading previously saved data. Finally, the
GUI component shows the user all the Android app
screens, including the two plots and the semaphore
that signals the effort. Through the GUI, the user can
start/stop/freeze the simulation, set the configuration
parameters for the ventilator and those of the patient,
load them from the PatientDB, or decide to store the
data of the current simulation run into the database.
Extension Points: The architecture has been cho-
sen to promote the future extensibility of the app.
New ventilatory strategies may be implemented by
simply modifying the Ventilator component. Sim-
ilarly, considering that the accuracy of the simulation
depends on the patient models, more complex and
realistic ones (including other parameters beyond R
and C) can be easily added in future releases, as the
INSPIRE component can simulate any kind of circuit
representing the respiratory system.
4 APP PROTOTYPE
In this section, we describe the prototype of our train-
ing Ventilation App, available and open source
at https://github.com/foselab/VentilationApp. It has
been developed for mobile devices, with a responsive
design, in order to make it suitable both for smart-
phones and tablets. Fig. 4 shows the Android applica-
tion screens, which we better explain in the following.
The app starts with the splash screen shown in
Fig. 4a, which contains two buttons, i.e., one for
accessing the info section and one for starting the
training. When the info button is clicked, the app
2
https://zeromq.org/
HEALTHINF 2024 - 17th International Conference on Health Informatics
366

(a) Splash screen. (b) Info screen. (c) Main window.
Figure 4: Startup and View Info mode in the First prototype in Android.
shows information about its purpose and functioning
(Fig. 4b). Instead, when the start button is clicked, the
app moves to the main window (shown in Fig. 4c).
The main window contains the core functionali-
ties of our Ventilation App. It contains real-time
charts reporting the simulation outcomes, namely the
airflow in the patient’s airways and the pressure mea-
sured at the patient’s mouth. This information is used
by physicians to understand potentially dangerous pa-
tient conditions, such as the auto-PEEP (i.e., when the
pressure in the patient’s airways increases breath after
breath, due to a too-short expiration time). In addi-
tion, two buttons allowing the setting of patient char-
acteristics and ventilation settings are present. For
what concerns the patient (Fig. 5a), the user is re-
quested to insert the gender, age, weight, height (used
to calculate the IBW), airway resistance, and com-
pliance. Then, in terms of ventilation parameters
(Fig. 5b), the user must set the value of the PEEP, the
P
max
, the I:E ratio, and the respiratory rate.
As introduced in Sect. 3, Ventilation App al-
lows the user to load both patient configurations and
ventilation parameters from an embedded database
(see Fig.3). In the case of patients it can be done by
clicking on the load button in Fig. 5a. In this way, the
list of patients (including age, gender, height, weight,
resistance, and compliance) is shown (Fig. 5c). The
user may then decide to load the desired patient by
clicking on the ”check” button or to delete one of the
patients by clicking on the trash bin icon. If a pa-
tient is chosen, all the fields in the patient configura-
tion (Fig. 5a) are automatically filled with the values
read from the DB. Similarly, as described for the pa-
tient parameters, the user can load the data related to
the ventilator configuration with a specific load button
(Fig. 5d). Therefore, a dedicated list is shown with
values of PEEP, PMax, I:E, and RR. Also in this case,
it is possible to select or delete the data with two dif-
ferent buttons (”check” or trash bin icon). When both
(a) Patient’s settings. (b) Ventilation set-
tings.
(c) Patient selection
from DB.
(d) Ventilation
params selection
from DB.
Figure 5: Settings mode in the first prototype in Android.
the patient’s parameters and the ventilator settings are
filled, the user can start the simulation by clicking the
play button in the main window (see Fig. 4c).
Thus, Ventilation App starts simulating a pa-
tient with the desired conditions who is undergoing
a mechanical ventilation procedure. During the sim-
ulation, at every breath, our app computes the WOB
for the patient and, based on it, lights up one of the
three semaphore lights, as explained in Sect. 3. If the
measured effort is low and near the target one, the
green light is shown, as in Fig. 6a. Instead, if the mea-
sured effort is higher but still acceptable, the yellow
An Android App for Training New Doctors in Mechanical Ventilation
367
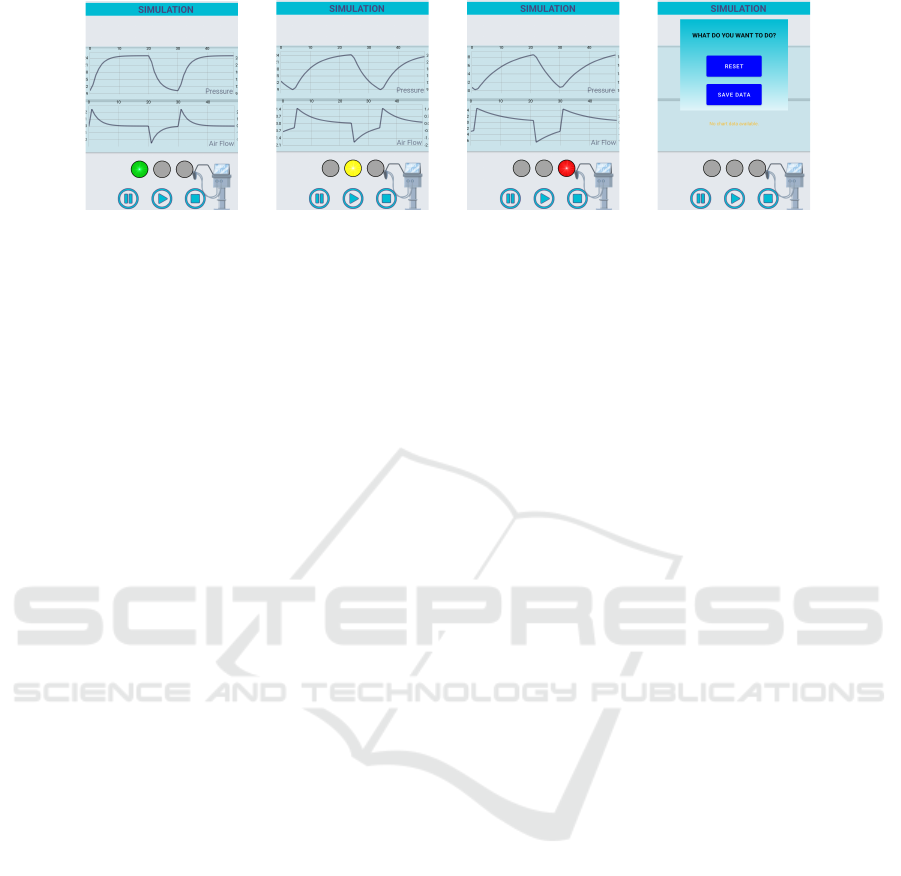
(a) Simulation with
optimal settings.
(b) Simulation with
non-optimal settings.
(c) Simulation with
wrong settings.
(d) Stop screen.
Figure 6: Simulation mode and Stop screen in the first prototype in Android.
light is turned on, as in Fig. 6b. Finally, if the chosen
ventilation strategy is beyond the safety limits or the
measured effort is considered too high, the red light is
shown (see Fig. 6c). Indeed, from Fig. 6a to Fig. 6c
(where the chosen respiratory rate is too high and the
pressure cannot reach the set maximum value) we can
see that the pressure curve tends to become more flat,
hence implying higher effort for the patient.
Having received the feedback on the chosen set-
tings and analyzed the relevant patient’s data through
the pressure and flow curves, the user may decide
to freeze the ventilation (e.g., to take a screenshot)
with the pause button available in the main window
(Fig. 4c). Finally, when the simulation is completed,
the user may stop it by clicking on the stop button in
the main window (Fig. 4c). In that case, the pop-up
in Fig. 6d is shown. It lets the user choose whether to
stop and reset the simulation or to save the current set-
tings (both those of the patient and of the ventilator)
in order to load them for following simulations.
5 RELATED WORK
As reported in Sect. 2.3 no other Android apps offer-
ing the same functionalities we offer with our train-
ing app exist, to the best of our knowledge. However,
the effort spent by developers in designing and imple-
menting simulation apps for physicians demonstrates
the importance of such tools (Kunkler, 2006), espe-
cially in the most critical scenarios such as emergency
medicine (Reznek, 2002). A survey conducted by
the authors of (Wallace et al., 2012) reports that over
85% of the interviewed participants, including medi-
cal students and physicians, reported using a mobile-
computing device for their training. This is the reason
why we also decided to opt for a mobile app. Indeed,
especially due to the increasing complexity and pre-
ciseness of patient models, simulators can be useful
tools in determining a physician’s understanding and
use of best practices, management of patient compli-
cations, appropriate use of instruments and tools, and
overall competence in performing procedures. Also
in other medical domains beyond mechanical ventila-
tion, simulators have been used, for example, to train
doctors in the management of temporary pacemak-
ers (Crowe et al., 2013), in bedside cardiac examina-
tions (Takashina et al., 1997), in surgeries (Ph
´
e et al.,
2016), in chronic kidney disease treatments (Markos-
sian et al., 2021) and also during radiology proce-
dures (L. E. Wood, 2018; Toderis et al., 2022). Using
case-based simulation training software (as the app
we propose in this paper) has been shown to improve
physicians’ skills even more than simple textbook re-
views (Schwid, 2001; Couto et al., 2015).
6 CONCLUSIONS AND FUTURE
WORK
In this paper, we have shown the methodology
adopted to develop the first prototype of a mobile
application to make the training of new physicians
in mechanical ventilation easier and more effective.
It exploits the principles of the minimum WOB, de-
scribed by the Otis equation, and used by ventilators
implementing the ASV mode to give users feedback
not only on the correctness of the set ventilation pa-
rameters, but also on their optimality, to reduce the ef-
fort required to patients when under mechanical ven-
tilation. Starting from the discussion of the idea with
pneumologists and the analysis of the already exist-
ing apps, we have first defined the requirements and
the architecture, and then implemented the initial pro-
totype presented in this paper. This prototype is just
preliminary work that we have used to verify the fea-
sibility of the idea and to stimulate discussion with ex-
perts in mechanical ventilation. In the future, we may
conduct further analysis with physicians-in-training
in order to refine Ventilation App, and to investi-
HEALTHINF 2024 - 17th International Conference on Health Informatics
368

gate potential ethical and legal implications of using
it for medical education.
Thanks to the feedback received by the experts we
collaborated with, we have identified some key future
work. The first future work direction will be focused
on having pre-defined scenarios in which the evolu-
tion of the patient status is described depending on
the actions taken by the physicians. For now, it can be
done only manually by saving into the database some
relevant patient data and, then, changing them on-the-
fly. Nevertheless, we believe that integrating some
formalism automatically describing the patient’s evo-
lution depending on environmental conditions and
ventilation choices, such as Markov Decision Pro-
cesses (Lakkaraju and Rudin, 2016), or including an
AI component, is feasible and worthwhile. Another
future work direction is related to the expandability
of the lung simulator on which our Android app is
based. Indeed, it would be very appreciated by physi-
cians to have different patient models, with different
granularities, and modeling patients having different
diseases. We believe that it can be easily done by ex-
ploiting the INSPIRE framework, which is on the ba-
sis of Ventilation App and supports the simulation
of complex circuits. Finally, more ventilation modes
beyond PCV can be implemented, in order to let new
physicians train under disparate patient conditions.
ACKNOWLEDGEMENTS
This work has been partially funded by
PNRR - ANTHEM (AdvaNced Technologies
for Human-centrEd Medicine) - Grant PNC0000003
– CUP: B53C22006700001 - Spoke 1 - Pilot 1.4.
We would like to thank Eleonora Vitali for the
preliminary work done for this project.
REFERENCES
Abba, A., Accorsi, C., et al. (2021). The novel mechan-
ical ventilator milano for the COVID-19 pandemic.
Physics of Fluids, 33(3):037122.
Bombarda, A., Bonfanti, S., Galbiati, C., Gargantini, A.,
Pelliccione, P., Riccobene, E., and Wada, M. (2021).
Lessons learned from the development of a mechani-
cal ventilator for COVID-19. In 2021 IEEE 32nd In-
ternational Symposium on Software Reliability Engi-
neering (ISSRE). IEEE.
Bombarda, A., Bonfanti, S., Galbiati, C., Gargantini, A.,
Pelliccione, P., Riccobene, E., and Wada, M. (2022).
Guidelines for the development of a critical software
under emergency. Information and Software Technol-
ogy, 152:107061.
Couto, T. B., Farhat, S. C., et al. (2015). High-fidelity
simulation versus case-based discussion for teaching
medical students in brazil about pediatric emergen-
cies. Clinics, 70(6):393–399.
Crowe, M. E., Hayes, C. T., and Hassan, Z.-U. (2013). Us-
ing software-based simulation for resident physician
training in the management of temporary pacemakers.
Simulation in Healthcare: The Journal of the Society
for Simulation in Healthcare, 8(2):109–113.
Fern
´
andez, J., Miguelena, D., Mulett, H., Godoy, J., and
Martin
´
on-Torres, F. (2013). Adaptive support ventila-
tion: State of the art review. Indian Journal of Critical
Care Medicine, 17(1):16–22.
IUCPQ (2023). VentilO Android App. https://play.google.
com/store/apps/details?id=ca.qc.iucpq.ventilo.
Kunkler, K. (2006). The role of medical simulation:
an overview. The International Journal of Medical
Robotics and Computer Assisted Surgery, 2(3).
L. E. Wood, M. M. Picard, M. K. (2018). App review: The
radiology assistant 2.0. Journal of Digital Imaging.
Lakkaraju, H. and Rudin, C. (2016). Learning cost-effective
treatment regimes using markov decision processes.
Markossian, T. W., Boyda, J., et al. (2021). A mobile
app to support self-management of chronic kidney
disease: Development study. JMIR Human Factors,
8(4):e29197.
OpenPediatrics (2023). Openpediatrics. https://www.
openpediatrics.org/simulators.
Pearce, J. M. (2020). A review of open source
ventilators for COVID-19 and future pandemics.
F1000Research, 9:218.
Ph
´
e, V., Cattarino, S., et al. (2016). Outcomes of a virtual-
reality simulator-training programme on basic surgi-
cal skills in robot-assisted laparoscopic surgery. The
International Journal of Medical Robotics and Com-
puter Assisted Surgery, 13(2):e1740.
Reznek, M. (2002). Virtual reality and simulation: Training
the future emergency physician. Academic Emergency
Medicine, 9(1):78–87.
Schwid, H. A. (2001). Components of an effective medical
simulation software solution. Simulation & Gaming,
32(2):240–249.
Takashina, T., Shimizu, M., and Katayama, H. (1997).
A new cardiology patient simulator. Cardiology,
88(5):408–413.
Toderis, L., Vo, A., et al. (2022). Development of a mobile
training app to assist radiographers’ diagnostic assess-
ments. Health Informatics Journal, 28(2).
TruCorp (2023). Truvent app. https://trucorp.com/product/
truvent-app/.
van Diepen, A., Bakkes, T. H. G. F., et al. (2021). A model-
based approach to generating annotated pressure sup-
port waveforms. Journal of Clinical Monitoring and
Computing.
Ventsim (2023). Ventsim. https://ventsim.cc/#/.
Wallace, S., Clark, M., and White, J. (2012). ‘it's on my
iPhone’: attitudes to the use of mobile computing de-
vices in medical education, a mixed-methods study.
BMJ Open, 2(4):e001099.
An Android App for Training New Doctors in Mechanical Ventilation
369
