
Using Data Mining Techniques to Understand Patterns of Suicide and
Reattempt Rates in Southern Brazil
Caibe A. Pereira
1a
, Rômulo C. R. Peixoto
2b
, Manuella P. Kaster
1c
, Mateus Grellert
3d
and Jônata T. Carvalho
2e
1
Biochemistry Department, Federal University of Santa Catarina, Florianopolis, Brazil
2
Informatics and Statistics Department, Federal University of Santa Catarina, Florianopolis, Brazil
3
Institute of Informatics, Federal University of Rio Grande do Sul, Porto Alegre, Brazil
Keywords: SUS, Health Infrastructure, Machine Learning.
Abstract: Suicide is a multifactorial, complex condition and one of the leading global causes of death, with suicide
attempt as the main risk factor. To this day, studies have shown relevant indicators that help identify people
with risk of committing suicide, but the literature still lacks comprehensive studies that evaluate how different
risk factors interact and ultimately affects the suicide risk. In this paper, we aimed to identify patterns in data
from the Brazilian Unified Health System – SUS, from 2009 to 2020, of individual reports of suicide attempts
and suicide deaths in the Brazilian Southern States, integrating those with a database of the healthcare
infrastructure. We framed the problem as a classification task for each micro-region to predict suicide and
reattempt rate as low, moderate, or high. We developed a pipeline for integrating, cleaning, and selecting the
data, and trained and compared three machine learning models: Decision Tree, Random Forest, and XGBoost,
with approximately 97% accuracy. The most important features for predicting suicide rates were the number
of mental health units and clinics, and for both suicide and reattempts were the number of physicians and
nurses available. This novel result brings valuable knowledge on possible directions for governmental
investments in order to reduce suicide rates.
1 INTRODUCTION
Suicide is one of the leading causes of death, with
approximately 700,000 deaths annually. Suicides are
preventable, and prevention programs can mediate
this problem. To be more effective, the programs
must be directed to the risk populations (WHO,
2014). Suicide attempts are one of the main risk
factors, and each additional attempt increases the risk.
Moreover, detecting the risk of suicide is an open
challenge in mental health research (Gao et al., 2015).
The stress-diathesis model for suicidal behavior
associates biological and psychiatric traits with
environmental stressors (van Heeringen & Mann,
2014), increasing the complexity of this condition.
The environment has a significant contribution to
a
https://orcid.org/0000-0002-9719-2832
b
https://orcid.org/0000-0001-6319-9668
c
https://orcid.org/0000-0003-0258-6204
d
https://orcid.org/0000-0003-0600-7054
e
https://orcid.org/0000-0001-9020-2076
suicidal behavior during the spectrum from suicide
ideation to completion (Turecki et al., 2019).
Environmental factors, such as biological (e.g., noise
and pollution) and social stressors (e.g., crime and
harassment fear) and infrastructure (e.g., green areas,
traffic) influence mental health (Johnson et al., 2023).
The studies that analyze suicide behavior or
deaths usually use sociodemographic or clinical
features, and not the environment context of the
individual. Thus, in this study, we propose a data
mining and machine learning workflow to identify
patterns of healthcare infrastructure to predict suicide
reattempt rate (SAR) and suicide rate (SR). We used
aggregated data from individuals who attempted or
committed suicide and healthcare infrastructure in the
Southern region of Brazil to predict rates.
Pereira, C., Peixoto, R., Kaster, M., Grellert, M. and Carvalho, J.
Using Data Mining Techniques to Understand Patterns of Suicide and Reattempt Rates in Southern Brazil.
DOI: 10.5220/0012350500003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 385-392
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
385

Data were collected from the Brazilian Mortality
Information System (SIM) and Notifiable Diseases
Information System (SINAN), part of the Unified
Health System platform (DATASUS). In this paper,
we selected a case study in the southern states of
Brazil: Paraná (PR), Santa Catarina (SC), and Rio
Grande do Sul (RS). The SIM form is performed post-
mortem; thus, it is more prone to missing values,
especially if the deceased relatives are not present.
This paper is organized as follows: Section 2
presents an overview of suicide, with a focus on
Brazilian data and machine learning studies of
suicide. Section 3 and 4 specifies the data collection,
treatment, and analysis for this study, and the
machine learning models used. Section 5 presents a
discussion of the results and concludes the study. To
the best of our knowledge, this is the first work that
proposes a learning-based solution for suicide or
attempted suicide in Brazil using large-scale public
health data. We show here how important nurses’ and
physicians’ availability and basic and mental health
facilities are to classify suicide risk.
2 BACKGROUND
In Brazil, suicide attempt is a compulsory notification
and every attempt is registered in the SINAN. The
notification started to be compulsory in 2011, but in a
gradual manner; thus, we chose more recent years to
analyze. Suicide attempt notification occurs in the
healthcare unit where the victim was admitted.
SINAN form is used for this purpose. It is an
individual form divided into ten domains, comprising
sociodemographic data about the individual with
details about the attempt (Ministry of Health, 2021).
All Brazilian healthcare-related infrastructure is
sent to the National Registry of Healthcare
Establishments (CNES) database, with different
categories. CNES is monthly updated and we
collected data from the southern states between 2009
and 2020. We gathered information on types of
establishments, professional specialization, mental
health services.
2.1 Suicide Data in Brazil
Brazil is a continental country divided into five
macro-regions (North, Northeast, Central-West,
Southeast, and South). SR and SAR differ between
regions, with the highest rates in the southern region.
Suicide in Brazil follow global trends, such as sex
ratio or methods (Ministry of Health, 2021). Registry
of suicide deaths in Brazil is compulsory and
classified according to the International
Classification of Diseases (ICD)-10 since 1996. Data
are publicly available in the DATASUS. The system
provides information on the death circumstance,
location, and personal information.
2.2 Related Work
2.2.1 Brazilian Studies
The studies that evaluated Brazilian SR and SAR data
were exploratory, analyzing the profile of the
individuals but with no predictive power. For SR,
data was collected from DATASUS; SAR data was
collected from different databases. In the Ministry of
Health (2021) report, from 2010 to 2019 SR showed
an increase of 42% in Brazil. The Southern was the
region with the highest SR. Moreover, attempt at
younger ages was more prevalent and mainly
occurred at home by self-poisoning.
Other studies focus on different aspects of suicide
in Brazil. From 2000 to 2017, Brazilian SR increased
significantly but differently by sex: male SR
increased by 75% and female by 85% (Palma et al.,
2021). Male-to-female ratio is even higher in older
people, reaching 8.2-fold more male deaths (Martini
et al., 2019). In adolescents, SR also increased over
the years and was associated with social inequality
and unemployment (Jaen-Varas et al., 2019).
In SC, a comparison between suicide attempters
and non-suicidal self-injured adolescents and adults
from 2014 to 2018 shows common traits between
groups, such as the majority of females, White
people, people with psychiatric disorders, and
poisoning as the method used. Comparing the
recurrence of the attempt, adults attempt more than
adolescents and with a higher percentage of alcohol
intoxication during the attempt (Pinheiro et al., 2021).
2.2.2 Machine Learning and Suicide
Electronic records were used to assess medical
databases and predict suicide attempts from self-
injured patients. The prediction was performed at
different time points using the Random Forest (RF)
model, with prediction accuracy decreasing with time
(Walsh et al., 2017). RF was used to predict attempts
in males and females with cocaine abuse; for females,
psychiatric issues showed more importance, whereas
for males, it was drug use (Roglio et al., 2020).
Different machine learning tests were used to
predict suicide in patients with depressive disorder.
Attempt, ideation, race, religion, and depressive
severity were the main factors for an attempt (Nordin
HEALTHINF 2024 - 17th International Conference on Health Informatics
386

et al., 2021). In addition, socioeconomic variables
(e.g., income, age, drinking, education) were the main
variables to predict suicide attempt and ideation by
XGBoost (XGB), support vector machine, or logistic
regression models (Choi et al., 2021).
Men and women differed regarding risk factors
with physical health more important for men. For
both sexes, psychiatric disorders and medication, 48
months previous to death, were important risk factors
(Gradus et al., 2020). Deep neural networks were
used to stratify the risk of suicide attempt with clinical
and demographic indicators. The model was able to
separate the sample into four categories, from low to
very high risk of attempt (Zheng et al., 2020).
McCullough et al. (2023) constructed an interaction
network of patients admitted to the hospital for
suicide or self-harm risk, indicating the trajectories
that led to referral to the emergency department.
Different types of data (sociodemographic,
clinical) and populations (countries/cultures or
diagnoses), can affect suicide; thus, analyzing data
from various conditions can increase our knowledge
about the risk factors and assist preventive measures.
Table 1 presents the studies that analyzed suicide
data. The studies focused on demographic or clinical
data. Our work uses demographic data to profile the
individuals attempting and committing suicide and
we aimed to identify patterns within the city's
healthcare infrastructure data to predict suicide and
suicide reattempt rates in Southern Brazil.
3 METHODS
The next sections describe the methods for data
collection, the analysis of the suicide rates dataset,
features and the models used for the predictions, and
our results. Figure 1 shows the workflow of the study.
The codes for the methods and results are deposited
in the following Github repository:
https://github.com/anonimo-SBBD/SuicideRates.git
3.1 Data Collection and Pre-Processing
DATASUS provides curated data for SIM, SINAN,
and CNES data sets. To access the data from
DATASUS, we used the 'download' function of the
PySUS library (Coelho et al., 2021). We downloaded
the data from the SIM from 2009 to 2020. For
SINAN, we used data from 2016 to 2020. The files
were filtered according to the southern states and the
cause of death (as suicide) for SIM. For SINAN, we
filtered the observations in which the ‘self-inflicted’
and the type of violence ‘other’ columns
corresponded to ‘yes’ (Pinheiro et al., 2021). We
filtered the data based on the ‘violence specification’
column, using different string values that indicated
suicide attempt (“suic/ts/t.s/intox/enve/enfor”
referring to Portuguese spellings).
We chose the southern region as a case study
because the region has the highest SR and SAR and
similar socioeconomic and cultural aspects between
states. We performed an initial separated analysis of
the three states but observed that the analyses were
similar and decided on a single, unified analysis to
increase sample size.
We removed columns not relevant, redundant,
with more than 30% of missing values, or with an
unidentifiable meaning. The following variables
remained: age, sex, race/color, marital status,
schooling, city, and date of occurrence for suicide
completion plus the presence of disabilities or
disorders and the method used in the attempt. We
excluded columns with specific values or columns
with values equivalent to the outcome.
We add new variables based on the date and age:
month, year, season, day of the week, and range of
age (in 10 years, starting with 10 years old). Some
variables with missing data were converted to
"ignored value" (i.e., a value was not imputed while
filling the form) because this an available option in
SIM and SINAN forms. The entries with missing
values in the "age" or "date" variables were excluded.
We used these data sets in the exploratory analysis. In
the CNES data set, we use the columns for public
professional, category of the professional (43
categories), type of health establishment (33 types),
and mental health specialization.
Since in SIM, SINAN, and CNES data sets
variables were mostly categorical, we separated each
category using the One-hot encoding method. Date
and city code were used to group and add the values
with information on the number of entries for each
category presented and merged SIM or SINAN to
CNES data sets into a single dataframe (DF). For the
machine learning predictions, we calculated the SR of
each city, in the respective year and month, by
100,000 inhabitants and added a column with a
classification of the SR rate based on WHO
recommendation: low SR ≤ 5; 5 ≤ moderate SR ≤ 10;
high SR > 10 (WHO, 2014). For SAR, we classified
based on the percentage of reattempt rate: low SAR ≤
33%; 33% < moderate SAR ≤ 66%; high SAR > 66%
of reattempt considering all the attempts. We also add
a column with the city's estimated population and
demographic density for the models not to compute
the rates based on the population number.
Using Data Mining Techniques to Understand Patterns of Suicide and Reattempt Rates in Southern Brazil
387
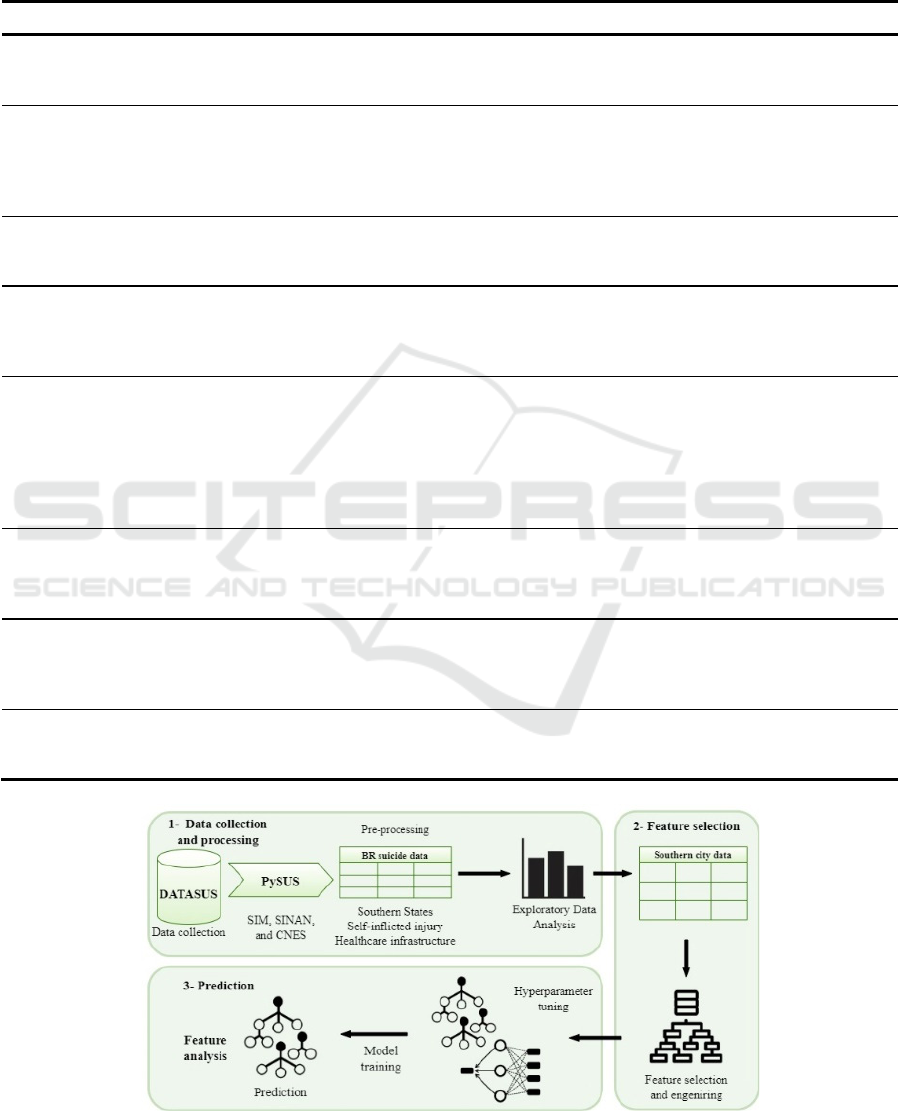
Table 1: Comparison between studies analyzing suicide data with machine learning approaches. Model results show the
representative of the best model the study performed (if more than one model). AUC, area under the curve; Acc, accuracy;
Sens, sensitivity; Spec, specificity; PPV, positive predictive value; NPV, negative predictive value; SIM, Mortality
Information System; SINAN, Notification of Interpersonal and Self-Inflicted Violence; CNES, National Registry of
Healthcare Establishments.
Study Database Time range Analysis Strategy Models results Country
McCullough
et al., 2023
Clinical interactions of
patients in the Hospital
Emergency Department
-
Classify the interaction
that led to referral to the
Emergency Department
Bernoulli naive Bayes
classifier
Acc.= 0.82
Australia
Gradus et
al., 2019
Clinical and
demographic data
1995 - 2015
Suicide prediction and
risk factor analysis
Random Forest
Men – AUC=0.80,
Spec.=0.97
Women – AUC=0.88,
Spec.=0.96
Denmark
Zheng et al.,
2020
Clinical and
demographic records
2015 - 2017
Attempt prediction and
risk factor analysis
Deep neural network
AUC=0.77, PPV=0.10,
relative risk=59.02
United
States of
America
Walsh et al.,
2017
Synthetic derivative -
Clinical and
demographic data of
p
revious attem
p
t
1 week to 2
years
Recurrence prediction
and risk factor analysis
Random Forests
AUC=0.84, precision=0.79,
recall=0.95
United
States of
America
Roglio et
al., 2020
Clinical and
demographic hospital
data - cocaine abuse
patients
2012 - 2018
Attempt prediction and
risk factor analysis
Random Forest
Men - AUC=0.68,
Acc.=0.66, Sens.=0.82,
Spec.=0.50, PPV=0.47,
NPV=0.84
Women - AUC=0.73,
other=0.71
Brazil
Nordin et
al., 2021
Clinical and
demographic hospital
data - depressive
disorder patients
-
Attempt prediction and
risk factor analysis
Bagging Decision tree
AUC=0.87, Acc.=0.92,
Sens.=0.92, Spec.=0.53,
PPV=0.89, NPV=0.76
Malasya
Choi et al.,
2021
KNHANES dataset -
suicide attempts and
ideation
2007 - 2019
Attempt prediction and
risk factor analysis
XGBoost
AUC=0.99, Acc.=0,99,
precision=0.98, recall=0.99,
F1-score=0.98
South Korea
This study
Demographic and
healthcare
infrastructure
2009 - 2020
Recurrence attempt rate
and suicide rate
prediction
XGBoost
Acc.=0.98, precision=0.97,
Sens./Spec.=0.94
Brazil
Figure 1: Workflow from data collection to outcome classification.
HEALTHINF 2024 - 17th International Conference on Health Informatics
388

3.2 Machine Learning Models and
Training Process
To classify SR or SAR, we used the SIM/CNES and
SINAN/CNES merged DF. We divided the DF into
two: train set (80%, SR - 17,007, SAR - 8,292 entries)
and test set (20%); we set the same random state and
divided the main outcome (SR or SAR). The models
were tested with 10-fold cross-validation.
We tested three tree-based machine learning
models: Decision Tree (DT), RF, and XGB. The
models were chosen based on simplicity to execute,
and analyze the results, do not require many data
treatments, such as scaling, and perform well with
categorical and numerical data. Feature importance
was computed with the mean accumulation of
impurity decrease within each tree.
4 RESULTS
4.1 Exploratory Data Analysis
4.1.1 Suicide Attempt
The mean age of the attempters was 30.7 years, and
the absolute values decreased with the increase of age
(27% from 10 to 19 decreasing to 4% from
individuals over 60 years, approximately). For
schooling, middle and high school education (26.5%
and 32.0%) were the most represented (25.30% of the
data were missing). More than 1/3 of the attempters
had a disorder or disability (37.4%), and the most
common were psychiatric (23.6%) and mood (12.9%)
disorders. The main methods chosen for the attempt
were intoxication (67.8%), cutting/stabbing (9.5%),
and hanging (7.8%). Moreover, 18% of males and 8%
of females were intoxicated with alcohol during the
attempt. Interestingly, 38.5% of the individuals had
already attempted suicide, whereas 41.7% were first-
time attempters (19.8% of data was missing).
4.1.2 Suicide Completion
The three states had a cumulative rate of 6.02 (PR),
8.31 (SC), and 10.32 (RS) per 100,000 inhabitants.
From 2009 to 2020 SR increased: PR 41.00%, SC
51%, and RS 27.67%. Males died 3.85-fold more than
females and the mean age was 45 years old; most
deaths occurred between ages 20 to 59 years, and
most were White (87.38%). Schooling was divided by
years studied: from four to seven years corresponded
to 26.76%, and from eight to eleven years
corresponded to 24.20% (24.42% of the data was
missing). Most deaths occurred in the person's
residence (66.45%) and were distributed similarly
throughout the year.
4.2 Machine Learning Classification
Generalization of the models presented high
accuracy, approximately 0.95. Table 2 presents the
best parameters of the models, the evaluation metrics,
and the variables most important to the models to
predict SR and SAR. Low, moderate, and high classes
were imbalanced: SR - 58,67%, 17,87%, and 23,46%;
SAR - 15,67%, 76,60%, and 7,73%.
5 DISCUSSION
Combat of suicide deaths is a challenge to countries
around the globe. Low- and middle-income countries
are at particular risk, with almost 80% of global
deaths. In some of those countries, death rate has been
increasing in the past years, such as Brazil (WHO,
2021). Suicide deaths are preventable, and the World
Health Organization general guidelines suggest
restricting means (firearm and medications control)
and increasing awareness for mental health (WHO,
2014). Moreover, understanding regional specificity
helps developing more effective public policies.
From an economic perspective, suicide deaths
may cost up to 3 million dollars to the government in
direct and indirect costs per death (Kinchin & Doran,
2018; Shepard et al., 2016). Moreover, in Brazil, the
average cost of a suicide attempt is approximately
US$ 7,000 (Sgobin et al., 2015). Many costs occur
after the attempt and include years lost due to trauma,
post-treatment, and impact on work and life of family
and acquaintances (Kinchin & Doran, 2018).
Observing that many attempts occur between ages
10 and 20, we recommend the development of more
programs of mental health and suicide prevention
presented during school years. Indeed, school-based
preventive programs targeted at children and
adolescents can be cost-effective (Ahern et al., 2018).
Our analysis of the profile of individuals
committing suicide corroborates previous findings,
suggesting that preventive programs must target
specific populations. Suicide attempts are the main
risk factors, and many suicide completers do not die
on the first attempt. Non-pharmacological approaches
after the attempt, such as active contact and follow-
up and cognitive behavioral therapy, may be used
along with prevention programs to increase cost-
effectiveness and decrease SR and SAR (Martínez-
Alés et al., 2021; Ross et al., 2021).
Using Data Mining Techniques to Understand Patterns of Suicide and Reattempt Rates in Southern Brazil
389
Table 2: Comparison between machine learning models results and most important features used by the models to classify
reattempt and suicide rates in Southern Brazil. Important features specific to reattempt (*) or completion (
#
) rates (features
are in no particular order).
Model Parameters Results Important Features
Decision Tree ccp alpha = 0.005
Accuracy = 0.95
Precision = 0.94
Sensitivity = 0.95
Specificity = 0.91
Number of physicians
Demographic density
Number of nurses
#
Number of psychosocial centers
#
Number of basic units*
Random Forest max_depth = 15
Accuracy = 0.96
Precision = 0.98
Sensitivity = 0.93
Specificity = 0.94
Demographic density
Number of physicians
Number of nurses
Number of clinics
#
Public professionals
#
Number of dentists*
XGBoost
learning rate = 0.1
n estimators = 3000
subsample = 0.5
colsample bytree= 0.5
Accuracy = 0.98
Precision = 0.97
Sensitivity = 0.94
Specificity = 0.94
Number of physicians
#
Number of nurses
#
Number of clinics
#
Public professionals
#
Number of neonatal units*
Number of short sta
y
hos
p
ital*
Infrastructure of the environment in which the
individual is inserted is also important. For example,
green areas within the pathways used by the
population and spatial inaccessibility to psychiatrists
or psychotherapists was shown to interfere in suicide
rates in the region (Shen & Lung, 2018; Tadmon &
Bearman, 2023). In addition, since a substantial
proportion of suicide completers use the healthcare
system the year before their death (Ahmedani et al.,
2014), we sought to understand the impact that the
city's healthcare infrastructure has on SR and SAR in
a case study of the Brazilian Southern region.
The Brazilian health care system is decentralized,
with more focus on primary care and outpatient
specialized services than in hospitalization. It has
private and public domains, and more than 70% of the
population relies on public services. The services are
distributed based on the demographical density and
economic indicators. Thus, smaller cities have
primary but may lack specialized services. Larger
cities usually work as an epicenter, providing
specialized health services (Paim et al., 2011).
We used three models to classify SR and SAR:
DT, RF, and XGB. The models had similar results,
with predictive values of approximately 95%. As the
data are unbalanced, other metrics are also important
to be analyzed, and as presented in Table 2, F1-score
averaged approximately 0.94. As expected, XGB,
having a correction of errors during training, had a
better performance, although all models showed
satisfactory results in classifying SR and SAR.
Understanding which factors are decisive may
help focus on specific targets to change or improve.
Our data shows that Psychosocial Care Centers
(CAPS), a type of healthcare facility focused on
treatment and improvement of psychiatric conditions
in the population, are one of the main features.
Additionally, since the majority of the Brazilian
population relies on the National Health System,
increasing the system with more clinicians and
nurses, especially in cities with high SR and SAR,
may help decrease the rates. Interestingly, some
models also considered the dental professionals,
showing that general well-being is important.
CAPS are divided into six classes and for people
suffering psychological conditions, and focused on
adults, or children and adolescents, or substance
abusers, and may be open 24 hours per day (with
hospital beds available). The simplest CAPS require
15,000 inhabitants, and the most completes up to
150,000 (Ministry of Health, 2023). Brazil has 5 565
cities, from which only 677 have more than 50 000
inhabitants. Thus, the majority of the cities only have
CAPS I available. Considering that psychiatric
conditions and substance abuse are some of the main
factors of suicide, and that children and adolescents
showed high rates of suicide attempt, rates would
probably decrease with more centers in more cities.
A limitation of our study is that in each question
of the SIM/SINAN forms, the evaluator may mark
‘ignored’. The correct filing of the form with answers
that have semantic values can increase the specificity
HEALTHINF 2024 - 17th International Conference on Health Informatics
390

of the analysis, and if the forms were more similar,
we could group the forms and analyze
simultaneously. Also, for the SINAN form, the
presence of an anonymous identifier would help
distinguish the profile of the individual after the first
attempt. In addition, we were not able to distinguish
the different specializations of the healthcare
professionals, such as psychiatrists from general
physicians, or the teams present at the different
facilities, which could improve the models'
performance and point to more direct improvements.
Lastly, underreporting plays a crucial role, especially
in smaller regions, where suicide is more stigmatized.
6 CONCLUSIONS AND
PERSPECTIVES
In this study, we focused on extracting and
interpreting patterns from suicide completion and
reattempt rates in Brazil. This is the first study using
the Brazilian healthcare infrastructure to classify
rates. Our models achieved a high predictive
performance of up to 97% accuracy in predicting
suicide death or reattempt. Compared to other studies,
we focused on the environment in which the
population is inserted, trying to use the model in a
descriptive manner, to identify and better understand
the patterns arising from models’ application. This
approach showed the importance of Psychosocial
Care Centers and the number of physicians and nurses
in impacting deaths and suicide reattempts. Future
studies could use a similar approach with other city
infrastructures, such as those related to
industrialization, employment, education, and
sanitation to decrease these preventable deaths.
ACKNOWLEDGEMENTS
We would like to thank CAPES and FAPESC for the
financial support.
REFERENCES
Ahern, S., Burke, L.-A., McElroy, B., Corcoran, P.,
McMahon, E. M., Keeley, H., Carli, V., Wasserman, C.,
Hoven, C. W., Sarchiapone, M., Apter, A., Balazs, J.,
Banzer, R., Bobes, J., Brunner, R., Cosman, D., Haring,
C., Kaess, M., Kahn, J.-P., … Wasserman, D. (2018).
A cost-effectiveness analysis of school-based suicide
prevention programmes. European Child & Adolescent
Psychiatry, 27(10), 1295–1304. https://doi.org/
10.1007/s00787-018-1120-5
Ahmedani, B. K., Simon, G. E., Stewart, C., Beck, A.,
Waitzfelder, B. E., Rossom, R., Lynch, F., Owen-
Smith, A., Hunkeler, E. M., Whiteside, U., Operskalski,
B. H., Coffey, M. J., & Solberg, L. I. (2014). Health
care contacts in the year before suicide death. Journal
of General Internal Medicine, 29(6), 870–877.
https://doi.org/10.1007/s11606-014-2767-3
Choi, J., Cho, S., Ko, I., & Han, S. (2021). Identification of
risk factors for suicidal ideation and attempt based on
machine learning algorithms: a longitudinal survey in
Korea (2007–2019). International Journal of
Environmental Research and Public Health, 18(23),
12772. https://doi.org/10.3390/ijerph182312772
Coelho, F. C., Baron, B. C., de Castro Fonseca, G. M.,
Reck, P., & Palumbo, D. (2021). AlertaDengue/PySUS:
Vaccine. Zenodo. https://doi.org/10.5281/zenodo.488
3502
Gao, K., Wu, R., Wang, Z., Ren, M., Kemp, D. E., Chan, P.
K., Conroy, C. M., Serrano, M. B., Ganocy, S. J., &
Calabrese, J. R. (2015). Disagreement between self-
reported and clinician-ascertained suicidal ideation and
its correlation with depression and anxiety severity in
patients with major depressive disorder or bipolar
disorder. Journal of Psychiatric Research, 60, 117–
124. https://doi.org/10.1016/j.jpsychires.2014.09.011
Gradus, J. L., Rosellini, A. J., Horváth-Puhó, E., Street, A.
E., Galatzer-Levy, I., Jiang, T., Lash, T. L., & Sørensen,
H. T. (2020). Prediction of sex-specific suicide risk
using machine learning and single-payer health care
registry data from Denmark. JAMA Psychiatry, 77(1),
25. https://doi.org/10.1001/jamapsychiatry.2019.2905
Jaen-Varas, D., Mari, J. J., Asevedo, E., Borschmann, R.,
Diniz, E., Ziebold, C., & Gadelha, A. (2019). The
association between adolescent suicide rates and
socioeconomic indicators in Brazil: a 10-year
retrospective ecological study. Brazilian Journal of
Psychiatry, 41(5), 389–395. https://doi.org/10.1590/
1516-4446-2018-0223
Johnson, T., Kanjo, E., & Woodward, K. (2023).
DigitalExposome: quantifying impact of urban
environment on wellbeing using sensor fusion and deep
learning. Computational Urban Science, 3(1), 14.
https://doi.org/10.1007/s43762-023-00088-9
Kinchin, I., & Doran, C. (2018). The cost of youth suicide
in Australia. International Journal of Environmental
Research and Public Health, 15(4), 672.
https://doi.org/10.3390/ijerph15040672
Martínez-Alés, G., Cruz Rodríguez, J. B., Lázaro, P.,
Domingo-Relloso, A., Barrigón, M. L., Angora, R.,
Rodríguez-Vega, B., Jiménez-Sola, E., Sánchez-Castro,
P., Román-Mazuecos, E., Villoria, L., Ortega, A. J.,
Navío, M., Stanley, B., Rosenheck, R., Baca-García, E.,
& Bravo-Ortiz, M. F. (2021). Cost-effectiveness of a
contact intervention and a psychotherapeutic program
for post-discharge suicide prevention. The Canadian
Journal of Psychiatry, 66(8), 737–746. https://doi.org/
10.1177/0706743720980135
Using Data Mining Techniques to Understand Patterns of Suicide and Reattempt Rates in Southern Brazil
391

Martini, M., da Fonseca, R. C., de Sousa, M. H., de
Azambuja Farias, C., Cardoso, T. de A., Kunz, M.,
Longaray, V. K., & Magalhães, P. V. da S. (2019). Age
and sex trends for suicide in Brazil between 2000 and
2016. Social Psychiatry and Psychiatric Epidemiology,
54(7), 857–860. https://doi.org/10.1007/s00127-019-
01689-8
Mccullough, M. H., Small, M., Jayawardena, B., & Hood,
S. (2023). Mapping patient interactions in psychiatric
presentations to a tertiary emergency department.
MedRxiv Preprint, 1–23. https://doi.org/10.1101/
2023.05.17.23290083
Ministry of Health. (2021). Mortalidade por suicídio e
notificações de lesões autoprovocadas no Brasil.
Boletim Epidemiológico Secretaria de Vigilância Em
Saúde − Ministério Da Saúde, 52(33), 1–10.
https://www.gov.br/saude/pt-br/centrais-de-
conteudo/publicacoes/boletins/epidemiologicos/edicoe
s/2021/boletim_epidemiologico_svs_33_final.pdf
Ministry of Health. (2023). Centros de Atenção
Psicosocial. https://www.gov.br/saude/pt-br/composi
cao/saes/desme/raps/caps
Nordin, N., Zainol, Z., Mohd Noor, M. H., & Lai Fong, C.
(2021). A comparative study of machine learning
techniques for suicide attempts predictive model.
Health Informatics Journal, 27(1), 146045822198939.
https://doi.org/10.1177/1460458221989395
Paim, J., Travassos, C., Almeida, C., Bahia, L., & Macinko,
J. (2011). The Brazilian health system: history,
advances, and challenges. The Lancet, 377(9779),
1778–1797. https://doi.org/10.1016/S0140-6736(11)
60054-8
Palma, D. C. de A., Oliveira, B. F. A. de, & Ignotti, E.
(2021). Suicide rates between men and women in
Brazil, 2000-2017. Cadernos de Saúde Pública, 37(12),
e00281020. https://doi.org/10.1590/0102-311x00281
020
Pinheiro, T. de P., Warmling, D., & Coelho, E. B. S. (2021).
Caracterização das tentativas de suicídio e
automutilações por adolescentes e adultos notificadas
em Santa Catarina, 2014-2018. Epidemiologia e
Serviços de Saúde, 30(4), e2021337.
https://doi.org/10.1590/s1679-49742021000400026
Roglio, V. S., Borges, E. N., Rabelo-da-Ponte, F. D.,
Ornell, F., Scherer, J. N., Schuch, J. B., Passos, I. C.,
Sanvicente-Vieira, B., Grassi-Oliveira, R., von
Diemen, L., Pechansky, F., & Kessler, F. H. P. (2020).
Prediction of attempted suicide in men and women with
crack-cocaine use disorder in Brazil. PLOS ONE, 15(5),
e0232242. https://doi.org/10.1371/journal.pone.0232242
Ross, E. L., Zuromski, K. L., Reis, B. Y., Nock, M. K.,
Kessler, R. C., & Smoller, J. W. (2021). Accuracy
requirements for cost-effective suicide risk prediction
among primary care patients in the US. JAMA
Psychiatry, 78(6), 642.
https://doi.org/10.1001/jamapsychiatry.2021.0089
Sgobin, S. M. T., Traballi, A. L. M., Botega, N. J., &
Coelho, O. R. (2015). Direct and indirect cost of
attempted suicide in a general hospital: cost-of-illness
study. Sao Paulo Medical Journal,
133(3), 218–226.
https://doi.org/10.1590/1516-3180.2014.8491808
Shen, Y.-S., & Lung, S.-C. C. (2018). Identifying critical
green structure characteristics for reducing the suicide
rate. Urban Forestry & Urban Greening, 34, 147–153.
https://doi.org/10.1016/j.ufug.2018.06.005
Shepard, D. S., Gurewich, D., Lwin, A. K., Reed, G. A., &
Silverman, M. M. (2016). Suicide and suicidal attempts
in the United States: costs and policy implications.
Suicide and Life-Threatening Behavior, 46(3), 352–
362. https://doi.org/10.1111/sltb.12225
Tadmon, D., & Bearman, P. S. (2023). Differential spatial-
social accessibility to mental health care and suicide.
Proceedings of the National Academy of Sciences,
120(19). https://doi.org/10.1073/pnas.2301304120
Turecki, G., Brent, D. A., Gunnell, D., O’Connor, R. C.,
Oquendo, M. A., Pirkis, J., & Stanley, B. H. (2019).
Suicide and suicide risk. Nature Reviews Disease
Primers, 5(1), 74. https://doi.org/10.1038/s41572-019-
0121-0
van Heeringen, K., & Mann, J. J. (2014). The neurobiology
of suicide. The Lancet Psychiatry, 1(1), 63–72.
https://doi.org/10.1016/S2215-0366(14)70220-2
Walsh, C. G., Ribeiro, J. D., & Franklin, J. C. (2017).
Predicting Risk of Suicide Attempts Over Time
Through Machine Learning. Clinical Psychological
Science, 5(3), 457–469. https://doi.org/10.1177/
2167702617691560
WHO (2014). Preventing suicide: A global imperative.
World Health Organization.
WHO (2021). Suicide worldwide in 2019: global health
estimates.
Zheng, L., Wang, O., Hao, S., Ye, C., Liu, M., Xia, M.,
Sabo, A. N., Markovic, L., Stearns, F., Kanov, L.,
Sylvester, K. G., Widen, E., McElhinney, D. B., Zhang,
W., Liao, J., & Ling, X. B. (2020). Development of an
early-warning system for high-risk patients for suicide
attempt using deep learning and electronic health
records. Translational Psychiatry, 10(1), 72.
https://doi.org/10.1038/s41398-020-0684-2
HEALTHINF 2024 - 17th International Conference on Health Informatics
392
