
Developing a Structural Standard for Smart Contract Electronic Health
Records Based on the HL7 Fast Healthcare Interoperability Resources
Christian Pulmano
a
and Proceso Fernandez
b
Department of Information Systems and Computer Science, Ateneo de Manila University, Quezon City, Philippines
Keywords:
Electronic Health Records, HL7 FHIR, Blockchain, Smart Contracts, Solidity.
Abstract:
Electronic health records (EHRs) are becoming more essential to patient care, as they provide information
that is usually valuable for health and medical decision-making. Each EHR typically comprises validated data
provided by medical professionals during patient care and personal health data recorded by the individual
patient. Existing implementations of EHRs, however, are often siloed and managed by disparate organiza-
tions. Health information exchanges, which aim to interoperate EHRs by different health organizations, are
also primarily centralized and can be vulnerable to attacks such as distributed denial of service (DDoS) and
data breaches. Blockchain is a potential solution to solving some of the current issues in health information
exchange implementations. Smart contracts deployed on blockchain networks can help enforce appropriate
health and medical record-keeping and sharing standards. This study aims to create a blockchain-based im-
plementation that allows decentralized EHRs. Smart contracts were developed based on the Health Level 7
Fast Healthcare Interoperability Resource (HL7 FHIR). Experiments were designed and simulated on a local
Ethereum blockchain network where 10,000 (generated) patients’ records were processed for evaluation. The
results show that a structural standard can be applied to EHR smart contracts, but while blockchain solutions
for EHR systems may be expected to be less vulnerable than centralized systems, the gas costs in Ethereum
are potentially prohibitive and should be carefully considered.
1 INTRODUCTION
Electronic Health Records (EHRs) are important in
healthcare. An EHR is a collection of an individ-
ual’s health records gathered from various sources, in-
cluding data encoded by medical professionals during
consultations (Mahajan et al., 2023) and health and
wellness data gathered from personal health tracking.
They contain information vital to health and medi-
cal decision-making (Arbabi et al., 2022). There-
fore, aside from storing EHRs, it is also important to
consider the standards and format for which they are
shared with relevant decision-makers.
Unfortunately, EHRs are often managed by dis-
parate service providers and stored across multi-
ple facilities in unstandardized formats (Cerchione
et al., 2023). Data sharing can be challenging with-
out proper standards, making data inaccessible when
needed (Chelladurai and Pandian, 2022). Structural
standards define a structure by which data, including
the data fields and formats, can be shared across dis-
a
https://orcid.org/0000-0001-7870-8197
b
https://orcid.org/0000-0001-5370-4544
parate health organizations. One standard that can be
considered is the Health Level 7 Fast Healthcare Inter-
operability Resources (HL7 FHIR), a set of resources
that provides health data standards for storing and
exchanging health and health-related data (HL7.org,
2023a).
Even if such standards for data storage and ex-
change are followed, however, there are still other
important issues related to EHRs that have to be ad-
dressed. For example, typical implementations of
EHRs use centralized technologies and are vulnera-
ble to attacks such as distributed denial of service
(DDoS), malware, and hacking. If not properly im-
plemented, centralized technologies can also be prone
to data tampering. Blockchain, an emerging tech-
nology whose strengths include decentralization, im-
mutability, and security, presents a promising solution
to some of the current issues in centralized EHR im-
plementations.
A blockchain is a distributed ledger composed of a
growing list of connected blocks arranged in chrono-
logical order and securely linked together using cryp-
tographic hashes, where a block contains a set of
Pulmano, C. and Fernandez, P.
Developing a Structural Standard for Smart Contract Electronic Health Records Based on the HL7 Fast Healthcare Interoperability Resources.
DOI: 10.5220/0012624100003699
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2024), pages 169-175
ISBN: 978-989-758-700-9; ISSN: 2184-4984
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
169

confirmed transactions (Arbabi et al., 2022; Villar-
real et al., 2023). In the healthcare context, trans-
actions can refer to activities like creating a medical
record, diagnosing a patient, prescribing a medicine,
etc. The ability of blockchain systems to maintain an
immutable data ledger can benefit EHRs in terms of
data integrity and reliability. Furthermore, smart con-
tracts in a blockchain can enable individuals to man-
age their EHRs without going through their service
providers.
Smart contracts are computer programs that can
be deployed to blockchain networks and are consid-
ered digital counterparts of traditional paper-based
contracts (Arbabi et al., 2022). A key property of
a smart contract is that it is self-executing and thus
can automate the actions required in an agreement or
contract. Vitalik Buterin first published a white paper
for Ethereum in 2014, proposing a blockchain with a
built-in Turing-complete programming language for
developing smart contracts (Buterin et al., 2014). So-
lidity (Solidity Team, 2023a) is one of the program-
ming languages that can be used to write smart con-
tracts in an Ethereum blockchain. This allows devel-
opers to build applications that support different func-
tions, including healthcare, and deploy contracts to
the Ethereum blockchain.
Smart contract functions on Ethereum
blockchains are executed on the (blockchain)
miners’ Ethereum Virtual Machine (EVM), thus
requiring Transaction initiators to pay the miners
what is referred to as gas fees as compensation for
the used computing resources. These miners are
responsible for validating the transactions, creating
new blocks and cryptographically linking a newly
created block to the blockchain. Miners essentially
secure the blockchain network and promote decen-
tralization, and they are incentivized to do so by
earning ETH, which is the token for value exchange
in the Ethereum network.
The gas fees required for deploying or invoking
transactions in smart contracts can also depend on the
code design (Li et al., 2023). Thus, software develop-
ers have to carefully design the smart contract imple-
mentation if they wish to minimize the gas fees per
transaction.
In this paper, we partially implemented, as
proof of concept, a proposed structural standard for
blockchain-based EHRs using smart contracts based
on the Health Level 7 Fast Healthcare Interoperabil-
ity Resource (HL7 FHIR). The smart contract is en-
visioned to become the technical standard for imple-
menting EHRs in blockchain. Our implementation,
written in Solidity, enabled us to estimate average
gas fees. Other considerations, such as privacy and
authentication, were excluded in this iteration of the
study,
The remaining sections of this paper are as fol-
lows: Section 2 provides a brief overview of related
works, Section 3 outlines the methodology for the
study, Section 4 presents the results and discussions,
and Section 5 concludes the study.
2 RELATED WORKS
This section provides an overview of related works
about blockchain for EHRs and the evaluation of gas
costs based on smart contract coding patterns.
2.1 Blockchain for Electronic Health
Records
Many efforts have already been made to implement
blockchain for EHRs. Blockchain is the underlying
technology for Bitcoin, and since its conception, it has
been applied to different domains, including health
(Frizzo-Barker et al., 2020). One study reviewed a
good number of published works from 2016 to 2020
to determine the extent of applying blockchain tech-
nology for managing EHRs (Al Mamun et al., 2022).
The study chose several publications based on pri-
vacy, security, storage scalability, accessibility, and
cost analysis. It found that much research was still in
the conceptual stage or at most early prototype, and
only a small chunk was already in the implementa-
tion stage. However, multiple studies were able to
consider implementing health standards such as FHIR
and HL7 in their design (Zhang et al., 2018; Roehrs
et al., 2017; Donawa et al., 2019). More recent publi-
cations are also available where smart contracts and
artificial intelligence with blockchain are proposed
(Mahajan et al., 2023; Haddad et al., 2022), and func-
tionalities for access-based controls are implemented
(De Oliveira et al., 2022).
2.2 Evaluating Smart Contract Gas
Costs
Multiple studies (Di Sorbo et al., 2022; Li et al., 2023;
Zhao et al., 2023) focused on identifying expensive
gas patterns in Solidity smart contract source codes.
In one study, the researchers identified 19 common
gas-expensive patterns or code smells and proposed
code recommendations to reduce gas costs. They
also developed GasMet, which defines a suite of met-
rics that can help evaluate the relationships of code
patterns to their gas consumption (Di Sorbo et al.,
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
170
2022). Another study identified gas-expensive pat-
terns and categorized them into storage-related pat-
terns, judgment-related patterns, and loop-related pat-
terns. They proposed GaSaver, a tool that auto-
matically detects gas-expensive patterns in a Solidity
smart contract (Zhao et al., 2023).
While previous works have already suggested
the feasibility of using blockchain for EHRs, with
some of these also providing strategies for integrat-
ing health data standards like HL7 FHIR, often these
studies combined on-chain and off-chain approaches.
On-chain means that data is stored in a node (ma-
chine) that is part of the blockchain network, where
data is regularly verified since data is replicated across
multiple nodes in the blockchain network. On the
other hand, off-chain means that data is stored in a
machine outside the blockchain network and is not
included in block confirmation and verification (Miy-
achi and Mackey, 2021). Off-chain implementations
are meant to increase the scalability of blockchain so-
lutions, but they are more vulnerable to attacks, unlike
on-chain implementations (Al Mamun et al., 2022).
Our study investigates the feasibility of a structural
standard for (full) on-chain EHR smart contract im-
plementations on the Ethereum blockchain and pro-
vides insights on gas cost implications for such im-
plementations.
3 METHODOLOGY
The study’s main objectives are mainly two-fold: (1)
develop a smart contract that supports a (full) on-
chain EHR implementation based on HL7 FHIR and
(2) evaluate its feasibility in terms of gas costs. This
section outlines the methodology used to achieve the
objective.
3.1 Dataset Generation
A synthetic dataset containing 10,000 patients’ per-
sonal information records was generated using the
Python Faker (Ethicalads, 2023) package. This pack-
age has tools that help generate names, birth dates, ad-
dresses, and contact data. The number of records was
decided based on the amount that could be processed
given time limitations but could still provide good
record variations for estimating averages later on. A
Python script was written to generate data based on
the data dictionary of the FHIR Patient resource. The
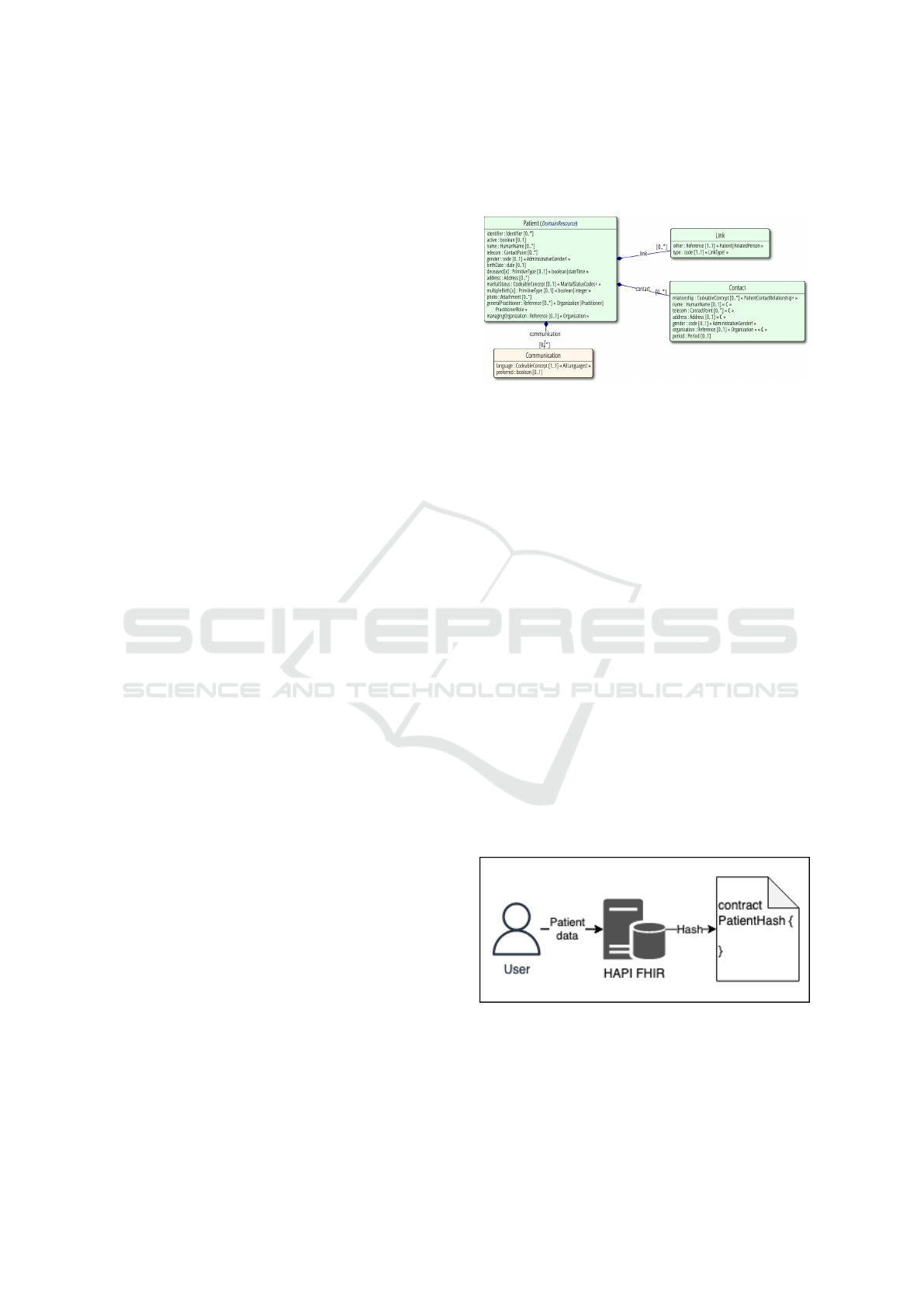
UML diagram in Figure 1 shows the data involved
under the resource. It should be noted that the gen-
erated dataset contained only general personal data
and excluded (generated) historical medical transac-
tion records for the time being since smart contracts
for other FHIR resources also need to be designed
based on their corresponding data fields.
Figure 1: UML diagram of the FHIR Patient Resource Con-
tent (HL7.org, 2023b).
3.2 Experiment Designs, Simulation,
and Evaluation
The experiments aimed to deploy, for evaluation,
some EHR systems that store patient personal records
based on the Patient (HL7.org, 2023b) resource of
HL7-FHIR. Two main models were designed and im-
plemented for the simulations. The first model im-
plements a hybrid off-chain and on-chain approach,
while the second model implements a full on-chain
approach. For both models, smart contracts were
developed using the Solidity (Solidity Team, 2023a)
programming language and deployed to a blockchain
network that was setup on a local server using
Ganache (Truffle, 2023). A summary of the available
functions for each smart contract is shown in Table
1. The models are also illustrated in Figures 2 and
3. The experiments are designed to help assess the
gas costs involved in digitalizing patient personal in-
formation records, which is one of the first steps in
creating patient EHRs, using smart contracts in the
Ethereum blockchain.
Figure 2: Illustration of model 1 components and workflow.
Following common implementations, a local
HAPI FHIR server (HAPI FHIR, 2023) was set up
for the first model to store the FHIR-based patient
records. HAPI-FHIR is an open-source project based
Developing a Structural Standard for Smart Contract Electronic Health Records Based on the HL7 Fast Healthcare Interoperability
Resources
171
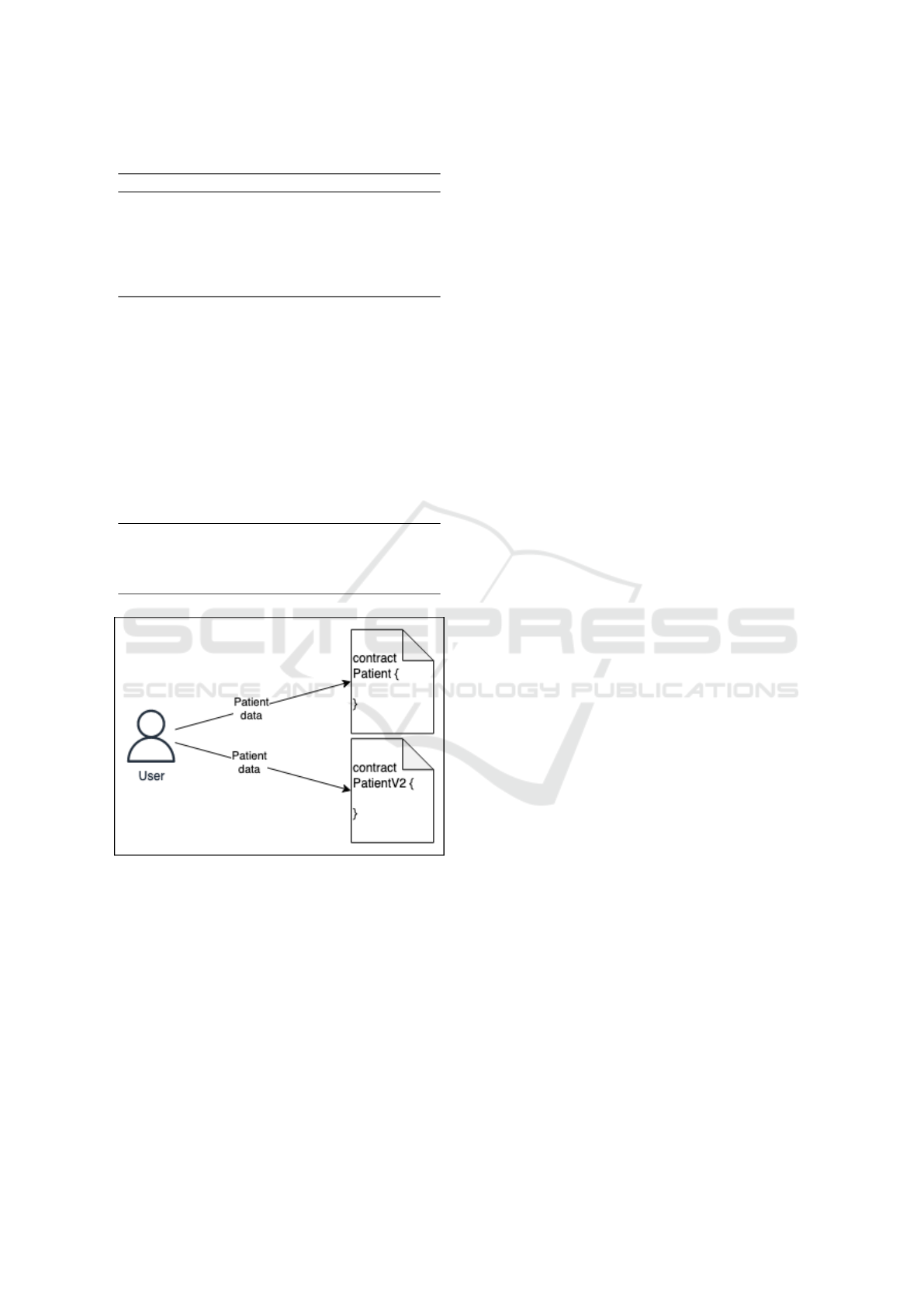
Table 1: Smart contract functions.
Model Contract Functions
1 HAPI
FHIR w/
Patien-
tHash
smart con-
tract
constructor
2a Patient
smart con-
tract
constructor, addI-
dentifier, setActive,
addName, addTelecom,
setGender, setBirth-
Date, setDeceased-
Info, addAddress,
setMaritalStatus,
setMultipleBirtht-
Info, addContact,
addCommunication,
setGeneralPractitioner,
setManagingOrganiza-
tion, addLink
2b PatientV2
smart con-
tract
constructor, addCon-
tact, setGeneralPracti-
tioner, setManagingOr-
ganization, addLink
Figure 3: Illustration of model 2 components and workflow.
on Java that developers can use to provide FHIR-
based API resources. In this study, a centralized
HAPI-FHIR server was deployed to convert personal
information records to the FHIR Patient resource data
format. The hash value of the Patient resource record
was then computed and submitted as a parameter
to the constructor function of the smart contract de-
ployed in a local Ethereum blockchain network. The
hash value of the record in the blockchain network
can be used to verify if the record has been tampered
with since altering the patient record should yield a
different hash value. The actual patient records are
stored in a centralized database system in this model.
For the second model, a fully on-chain approach
was developed. Under this approach, personal data is
directly submitted to a new smart contract deployed
on the local Ethereum blockchain network. The smart
contract accepts data such as name, birthdate, address,
contact information, and other needed information in
the HL7 FHIR Patient resource. Two versions were
developed and evaluated for this model. In the first
version, the constructor function does not accept any
parameters, and data can only be submitted using the
specific functions in the contract developed to handle
a particular piece of data input. The functions handle
data attributes defined in the Patient resource of HL7
FHIR.
The second iteration of the second model is an
optimized version where the constructor function al-
ready accepts parameters and stores patient infor-
mation in the contract. Due to limitations in the
stack size of the EVM, not all data attributes were
included as parameters of the constructor function;
only data about the patients themselves were in-
cluded. Functions that process data external to the
patients, i.e., general practitioner, managing orga-
nization, and other links, were retained as separate
functions. Based on recommendations from previous
studies, the second version also uses bytes data type
instead of string for handling text data (Di Sorbo et al.,
2022; Li et al., 2023; Zhao et al., 2023).
A Python script was developed to simulate the
experiments for the two models where all models
used the same dataset. The Web3 package (Ethereum
Foundation, 2023) was used to invoke transactions
from the Python script to smart contracts in the
Ethereum blockchain network. All programs used for
the experiments were installed on a machine with a
macOS Sonoma 14.0 operating system, 8 GB mem-
ory, and an Apple M1 processor. The gas costs for
all invoked transactions were recorded during the ex-
periment runs. The gas costs for the different models
were then compared and evaluated.
4 RESULTS AND DISCUSSIONS
Table 2 summarizes the total gas cost and average
gas cost per record for the smart contracts. While
it is expected that the second model would require
higher gas costs than the first model, the purpose
of the experiments was to evaluate the magnitude of
the difference. As shown in Table 3, the total gas
cost to process 10,000 records for Model 1 is above
1.8 billion gas units. Model 2a incurred the high-
est gas cost at around 44.1 billion gas units, while
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
172

Table 2: Total gas costs and estimated gas fees for each model as of 2024-01-03T11:00:00Z.
Model 1 Model 2a Model 2b
HAPI FHIR w/ PatientHash Patient PatientV2
Records 10,000 10,000 10,000
Gas price (Gwei) 20 20 20
Gas price (USD) 0.000002367 0.000002367 0.000002367
Total gas cost 1,872,025,468 44,099,957,978 26,143,190,020
Gas cost/record 187,203 4,409,996 2,614,319
Gas fee/record (Gwei/record) 3,744,051 88,199,916 52,286,380
Gas fee/record (USD/record) 9 209 124
Table 3: Total gas costs for each smart contract function.
Model 1 Model 2a Model 2b
Function HAPI FHIR w/ PatientHash Patient PatientV2
Contract deployment 1,872,025,468 18,878,090,000 24,386,657,948
addIdentifier 2,077,611,622
setActive 338,402,376
addName 3,007,115,284
addTelecom 1,766,766,264
setGender 387,823,784
setBirthDate 451,550,000
setDeceasedInfo 475,833,369
addAddress 4,056,553,516
setMaritalStatus 450,645,024
setMultipleBirthInfo 543,069,056
addContact 9,098,202,123
addCommunication 809,973,488
setGeneralPractitioner 452,386,380 451,496,380
setManagingOrganization 451,947,088 451,277,088
addLink 853,988,604 853,758,604
Total 1,872,025,468 44,099,957,978 26,143,190,020
Table 4: Average gas costs and fees for each smart contract function.
Model 1 Model 2a Model 2b
Function HAPI FHIR w/ PatientHash Patient PatientV2
Contract deployment 187,203 1,887,809 2,438,666
addIdentifier 207,761
setActive 33,840
addName 300,712
addTelecom 176,677
setGender 38,782
setBirthDate 45,155
setDeceasedInfo 47,583
addAddress 405,655
setMaritalStatus 45,065
setMultipleBirthInfo 54,307
addContact 909,820
addCommunication 80,997
setGeneralPractitioner 45,239 45,150
setManagingOrganization 45,195 45,128
addLink 85,399 85,376
Total 187,203 4,409,996 2,614,319
Developing a Structural Standard for Smart Contract Electronic Health Records Based on the HL7 Fast Healthcare Interoperability
Resources
173

the updated smart contract for the second model (2b)
only required around 26.1 billion gas units. The gas
units required to process a patient record are approxi-
mately 187 thousand, 4.4 million, and 2.6 million for
models 1, 2a, and 2b, respectively. As of 2024-01-
03T11:00:00Z, the average gas price in the Ethereum
main net is 20 Gwei. Assuming the smart contracts
will be deployed in the main network, the gas fees per
record would be approximately 3.7 million Gwei (9
USD), 88.1 million Gwei (209 USD), and 52.3 mil-
lion Gwei (124 USD) for Models 1, 2a, and 2b, re-
spectively.
Tables 3 and 4 show the total and average gas costs
per record for each function available in the smart
contracts. A contract deployed to the blockchain net-
work corresponds to one patient record. Model 1 re-
quired the lowest gas cost for deploying the smart
contracts for 10,000 records at 1.8 billion gas units
since it has minimal features and required inputs.
Model 2a required around 18.9 billion gas units for
contract deployment, which is lower than the value
for Model 2b at around 24.4 billion gas units. Model
2b has a higher value since its constructor already ac-
cepts multiple parameters, unlike Model 2a, which
doesn’t accept any parameter. It can also be observed
from the table that the more gas-expensive functions
are those requiring a struct (Solidity Team, 2023b)
type parameter such as addIdentifier(), addName(),
addAddress(), etc.
The results show that the first model is the least
gas-expensive strategy. However, there are also other
considerations to implementing a specific model. In
terms of decentralization, the EHRs in the first model
are still stored in a centralized HAPI FHIR server,
which is vulnerable to attacks and hacking. The hash
values recorded on-chain help with the verification of
the records, but additional safeguards must still be im-
plemented to ensure the centralized server’s security
and data integrity. In the second model, EHRs are
stored and validated by a decentralized network of
nodes.
The two versions in the second model show that
smart contract patterns should also be considered.
This is evident in the difference in gas cost values be-
tween the first and second versions. After reorganiz-
ing how data fields are encoded to the smart contract,
the total gas costs also changed significantly, despite
processing the same dataset.
It is also important to consider that a full on-
chain HL7 FHIR implementation will require includ-
ing other resources besides the Patient resource, in-
cluding Observations, Encounters, Procedures, etc.
The inclusion of other resources will also require ad-
ditional gas costs. Implementing the Patient resource
alone already incurred high values. Therefore, select-
ing only specific data points that benefit from the on-
chain implementation might be more appropriate.
5 CONCLUSIONS AND
RECOMMENDATIONS
The study provides insights into an on-chain im-
plementation of EHRs using smart contracts based
on the HL7 FHIR interoperability standard. Two
models were designed in the experiments, where a
hybrid off-chain-on-chain implementation was com-
pared against a full on-chain implementation. A syn-
thetic patient dataset was generated and processed for
evaluation.
The study concludes that gas costs for deploying
HL7 FHIR-based smart contacts should be consid-
ered. The high gas costs for implementing the Pa-
tient resource alone suggest that not all the data can be
implemented on-chain. Instead, HL7 FHIR resources
and data attributes that will benefit highly from on-
chain implementation should be carefully selected.
The design pattern at which smart contracts are devel-
oped is also relevant, considering that implementing
different patterns can also affect the gas requirements
of the contract.
Future work can look more closely into the gas
mechanics of the Ethereum blockchain to have more
insights into how gas costs are computed based on
smart contract patterns. Additional experiments can
also be conducted to evaluate the implementation in
other Layer 1 blockchains, or possibly even Layer
2 blockchain networks over the Ethereum or other
Layer 1 blockchains.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Depart-
ment of Information Systems and Computer Science
and the Ateneo de Manila University for their support
of the study.
REFERENCES
Al Mamun, A., Azam, S., and Gritti, C. (2022). Blockchain-
based electronic health records management: a com-
prehensive review and future research direction. IEEE
Access, 10:5768–5789.
Arbabi, M. S., Lal, C., Veeraragavan, N. R., Marijan, D.,
Nyg
˚
ard, J. F., and Vitenberg, R. (2022). A survey on
blockchain for healthcare: Challenges, benefits, and
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
174

future directions. IEEE Communications Surveys &
Tutorials.
Buterin, V. et al. (2014). A next-generation smart contract
and decentralized application platform. white paper,
3(37):2–1.
Cerchione, R., Centobelli, P., Riccio, E., Abbate, S., and
Oropallo, E. (2023). Blockchain’s coming to hospi-
tal to digitalize healthcare services: Designing a dis-
tributed electronic health record ecosystem. Techno-
vation, 120:102480.
Chelladurai, U. and Pandian, S. (2022). A novel blockchain
based electronic health record automation system for
healthcare. Journal of Ambient Intelligence and Hu-
manized Computing, pages 1–11.
De Oliveira, M. T., Reis, L. H. A., Verginadis, Y., Mattos,
D. M. F., and Olabarriaga, S. D. (2022). Smartac-
cess: Attribute-based access control system for med-
ical records based on smart contracts. IEEE Access,
10:117836–117854.
Di Sorbo, A., Laudanna, S., Vacca, A., Visaggio, C. A.,
and Canfora, G. (2022). Profiling gas consumption
in solidity smart contracts. Journal of Systems and
Software, 186:111193.
Donawa, A., Orukari, I., and Baker, C. E. (2019). Scaling
blockchains to support electronic health records for
hospital systems. In 2019 IEEE 10th Annual Ubiq-
uitous Computing, Electronics & Mobile Commu-
nication Conference (UEMCON), pages 0550–0556.
IEEE.
Ethereum Foundation (2023). gm — web3.py 6.11.4 docu-
mentation.
Ethicalads (2023). Welcome to faker’s documentation! —
faker 18.13.0 documentation.
Frizzo-Barker, J., Chow-White, P. A., Adams, P. R., Men-
tanko, J., Ha, D., and Green, S. (2020). Blockchain
as a disruptive technology for business: A systematic
review. International Journal of Information Manage-
ment, 51:102029.
Haddad, A., Habaebi, M. H., Islam, M. R., Hasbullah,
N. F., and Zabidi, S. A. (2022). Systematic review on
ai-blockchain based e-healthcare records management
systems. IEEE Access, 10:94583–94615.
HAPI FHIR (2023). hapifhir/hapi-fhir: Hapi fhir - java api
for hl7 fhir clients and servers.
HL7.org (2023a). Fhir v5.0.0.
HL7.org (2023b). Patient - fhir v5.0.0.
Li, J., Zhao, Z., Su, Z., and Meng, W. (2023). Gas-
expensive patterns detection to optimize smart con-
tracts. Applied Soft Computing, 145:110542.
Mahajan, H. B., Rashid, A. S., Junnarkar, A. A., Uke, N.,
Deshpande, S. D., Futane, P. R., Alkhayyat, A., and
Alhayani, B. (2023). Integration of healthcare 4.0 and
blockchain into secure cloud-based electronic health
records systems. Applied Nanoscience, 13(3):2329–
2342.
Miyachi, K. and Mackey, T. K. (2021). hocbs: A
privacy-preserving blockchain framework for health-
care data leveraging an on-chain and off-chain sys-
tem design. Information Processing & Management,
58(3):102535.
Roehrs, A., Da Costa, C. A., and da Rosa Righi, R. (2017).
Omniphr: A distributed architecture model to inte-
grate personal health records. Journal of biomedical
informatics, 71:70–81.
Solidity Team (2023a). Home — solidity programming lan-
guage.
Solidity Team (2023b). Types — solidity 0.8.24 documen-
tation.
Truffle (2023). Ganache - truffle suite.
Villarreal, E. R. D., Garc
´
ıa-Alonso, J., Moguel, E., and
Alegr
´
ıa, J. A. H. (2023). Blockchain for healthcare
management systems: A survey on interoperability
and security. IEEE Access, 11:5629–5652.
Zhang, P., White, J., Schmidt, D. C., Lenz, G., and Rosen-
bloom, S. T. (2018). Fhirchain: applying blockchain
to securely and scalably share clinical data. Computa-
tional and structural biotechnology journal, 16:267–
278.
Zhao, Z., Li, J., Su, Z., and Wang, Y. (2023). Gasaver: A
static analysis tool for saving gas. IEEE Transactions
on Sustainable Computing, 8(2):257–267.
Developing a Structural Standard for Smart Contract Electronic Health Records Based on the HL7 Fast Healthcare Interoperability
Resources
175
