
Advanced VR Calibration for Upper Limb Rehabilitation: Making
Immersive Environments Accessible
Vanesa Herrera
1 a
, Ana Reyes-Guzm
´
an
2 b
, David Vallejo
1 c
, Jos
´
e Castro-Schez
1 d
,
Dorothy N. Monekosso
3 e
, Gonz
´
alez-Morcillo Carlos
1 f
and Javier Albusac
1 g
1
School of Computer Science, University of Castilla-La Mancha, Ciudad Real, Spain
2
Hospital Nacional de Parapl
´
ejicos de Toledo, Toledo, Spain
3
Department of Computer Science, University of Durham, Durham, County Durham, GB, U.K.
Keywords:
Upper Limb Rehabilitation, Virtual Reality, Dynamic Environment Adaptation, Free-Hand Calibration,
Immersive Gamification.
Abstract:
The creation of accessible spaces is essential for patients with motor injuries to conduct therapy safely and
effectively. Disruptive technologies such as Virtual Reality (VR) are increasingly being used as a complement
to traditional therapy, with excellent results. VR allows, among other things, the realistic recreation of physical
spaces, so much so that it is relatively easy to run the risk of transferring physical barriers into the virtual
space. This article proposes an innovative method of calibration in virtual environments that assesses the
motor limitations of patients with cervical spinal cord injuries, doing so individually for each upper limb. The
result is the dynamic adaptation of virtual environments to make them accessible and safe for rehabilitative
therapy practices. This method has been integrated into the Rehab-Immersive platform, which hosts a series
of serious games aimed at rehabilitating upper limbs, using immersive gamification techniques.
1 INTRODUCTION
In recent years, the use of Virtual Reality (VR) has
spread to a variety of fields, including physical and
psychological rehabilitation (Zhang et al., 2020; Cha
et al., 2021). The application of VR in rehabilitation
process has shown important benefits such as an im-
provement in mobility, balance and cognitive function
(Park et al., 2020), as well as reducing the percep-
tion of pain in patients (Goudman et al., 2022; Mal-
lari et al., 2019). Furthermore, the use of VR devices
in rehabilitation programs improves treatment adher-
ence and increases motivation (Dias et al., 2019), both
important qualities for a successful rehabilitation pro-
cess (Teo et al., 2022).
In particular, the technological advances that im-
a
https://orcid.org/0000-0002-6187-4794
b
https://orcid.org/0000-0003-2905-2405
c
https://orcid.org/0000-0002-6001-7192
d
https://orcid.org/0000-0002-0201-7653
e
https://orcid.org/0000-0001-7322-5911
f
https://orcid.org/0000-0002-8568-9542
g
https://orcid.org/0000-0003-1889-3065
mersive VR devices have undergone in recent years
have led to a new field in upper limb rehabilitation.
Wearable devices, such as head-mounted displays
(HMDs), provide users with immersive experiences
in virtual environments through a viewer and con-
trollers. More recently, this type of system has begun
to offer hand tracking through the existing inside-out
cameras in the headset (Khundam and N
¨
oel, 2021).
As a result, existing applications are being adapted or
new ones are being developed. These applications al-
low the user to interact with the virtual world using
his or her own hands, without the need for controllers
or joysticks. This new form of interaction with vir-
tual environments makes it more intuitive, natural and
simple. In line with this, recent studies demonstrate
the preference for this mechanism of interaction over
controllers (Juan et al., 2023). Moreover, it opens
new opportunities for people with reduced mobility in
their upper limbs who, until now, have been unable to
use these types of devices due to the need for fine mo-
tor skills to hold the controller and press the buttons.
This technological progress has generated new possi-
bilities in the development of applications for upper
limb rehabilitation. In this context, it is essential for
378
Herrera, V., Reyes-Guzmán, A., Vallejo, D., Castro-Schez, J., Monekosso, D., Carlos, G. and Albusac, J.
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible.
DOI: 10.5220/0012624600003690
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 26th International Conference on Enterprise Information Systems (ICEIS 2024) - Volume 2, pages 378-389
ISBN: 978-989-758-692-7; ISSN: 2184-4992
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.

patients to use their hands naturally, replicating tradi-
tional rehabilitation movements and grips.
Although hands-free interaction and accurate
hand tracking is an important advance in the acces-
sibility of immersive environments for people with
motor impairments, it is still not sufficient for the
proper development of rehabilitation therapies. The
challenge of developing VR environments that are
accessible and adapted to the different needs of end
users and the specific characteristics of each applica-
tion. VR makes it possible to simulate worlds and
situations that are difficult to reproduce in real envi-
ronments, which is a significant advantage, especially
given the diversity of environments and the mobility
constraints of certain users. This capability highlights
the need for virtual environments to be accessible and
adaptable to both user needs and application-specific
requirements.
For users with special needs or disabilities, the
creation of adapted, accessible, and inclusive VR en-
vironments is crucial (Soomal et al., 2020; Creed
et al., 2023). This involves tailoring the type of in-
teraction and the placement of interactive elements
to suit each user’s abilities. This is particularly im-
portant for patients with cervical spinal cord injuries
(cSCI), who require exercises to be performed while
seated, considering their upper limb mobility and
gripping capabilities. Proper positioning of interac-
tive elements in the VR environment is key to ensur-
ing safety, prevent overexertion or unwanted compen-
satory movement. These compensatory movements,
which are movement patterns adopted to overcome
motor restrictions (Luo et al., 2023), while facilitating
task performance, can sometimes lead to additional
problems that negatively affect the rehabilitation pro-
cess (see Figure 1).
One solution to address these challenges lies in the
ability of VR systems themselves to capture and store
relevant data. This includes data related to the kine-
matics of the body parts undergoing therapy, as well
as the position of elements in the virtual scene and
historical tracking of the patient’s progress. In addi-
tion, the capture and storage of kinematic data is es-
sential in the rehabilitation process. This practice pro-
vides healthcare professionals with a more objective
and quantitative view of the patient’s progress. This is
exemplified in the study by Onitsuka et al. (Onitsuka
et al., 2023), which highlights the significance of such
data in monitoring and enhancing rehabilitation out-
comes. This information is useful for adjusting and
optimising rehabilitation programmes, ensuring their
maximum effectiveness for the specific needs of each
patient. Furthermore, the capture and analysis of this
data not only facilitates the identification of the effec-
tiveness of the exercises but also allows for the detec-
tion of possible unwanted compensatory movements.
In this context, leveraging VR capabilities, a
practical solution for enhancing the accessibility and
adaptation of virtual rehabilitation environments in-
volves a calibration process before exercise execu-
tion. This calibration should focus on the specific mo-
tor conditions of the patient, taking into account their
particular characteristics and limitations. This assess-
ment allows for precise modifications to the position-
ing of the interactive elements within the virtual en-
vironment. Such an approach ensures that the virtual
environment is not only accessible but also highly per-
sonalized, adapting to both the physical capabilities of
the patient and their specific stage in the rehabilitation
process.
On this basis, the article presents an advanced au-
tomatic calibration system adapted to upper limb re-
habilitation in patients with cSCI. This system takes
into account the physical characteristics of the patient
and the specific requirements of the exercises to be
performed. Thanks to this pre-calibration, it is pos-
sible to adapt the position of the elements in the vir-
tual environment according to the specific character-
istics of the exercise. For this reason, the range of
movement is taken into account separately for each of
the upper limbs, since the exercises can be performed
with one or two hands. In addition to the optimal po-
sition, it is taken into account that the patients perform
the exercises in a seated position, thus avoiding possi-
ble undesirable compensatory movements. It should
be noted that the calibration is based on hand posi-
tions, without the need for external elements such as
joysticks or controllers. As a result, patients perform
the exercises in a more natural and ergonomic way,
potentially improving the effectiveness of rehabilita-
tion.
The calibration system, aimed at improving up-
per limb rehabilitation of cSCI patients, has been
integrated into the Rehab-Immersive platform (Her-
rera et al., 2023). This integration facilitates design,
implementation and testing. The Rehab-Immersive
platform is currently developing a series of serious
games. These games are adapted to specific thera-
pies for the rehabilitation of upper limbs of ICSc pa-
tients. The collaboration with the Hospital Nacional
de Parapl
´
ejicos de Toledo has been key in this de-
velopment. This hospital is recognised as a refer-
ence centre for patients with SCI. The main objective
of Rehab-Immersive is to create an environment that
favours effective rehabilitation
The rest of the paper is structured as follows. Sec-
tion 2 reviews related works. Section 3 provides con-
text and background information. Section 4 describes
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible
379

Figure 1: On the left, a patient performs compensatory movements, with trunk inclination and grasping the wheelchair with
the left hand to achieve balance. On the right, due to a correct distribution of virtual elements, compensatory movements are
not necessary.
the automatic calibration system. Section 5 presents
the evaluation and the results obtained. Section 6 dis-
cusses the limitations and future work. Finally, the
paper concludes with Section 7, which presents the
conclusions.
2 RELATED WORKS
2.1 VR Rehabilitation for Upper Limbs
Several studies have focused on the rehabilitation of
upper limbs using VR techniques. These works can
be classified according to the degree of immersion and
the main way of interaction. Depending on the degree
of immersion, there are non-immersive and immer-
sive applications and, the use of devices such as con-
trollers or the user’s own hands (hand tracking) can
be considered.
Non-immersive and hand tracking upper limb VR
rehabilitation studies include the work of Shahmoradi
et al. (Shahmoradi et al., 2021), who used the Kinect
sensor to rehabilitate the upper limb in stroke patients
through a set of games. The results of the study indi-
cated improvements in participants’ range of motion
in terms of horizontal shoulder abduction and adduc-
tion, elbow flexion, and wrist supination and flexion.
The study by Reyes-Guzm
´
an et al. (de Los Reyes-
Guzm
´
an et al., 2021) also uses non-immersive VR
and hand tracking by means of a Leap Motion Con-
troller (LMC), and focused on SCI patients. The con-
clusions of the study indicate that the LMC is suitable
for a given sample of cervical patients for rehabilita-
tion purposes.
Regarding studies with immersive VR and the use
of controllers, the following can be found the study
by Lim et al. (Lim et al., 2020) which investigated
the use of VR in combination with conventional re-
habilitation for upper limb rehabilitation in patients
with SCI. The conclusion of the study is that VR train-
ing for upper limb function after SCI may be an ac-
ceptable adjunctive rehabilitation method without sig-
nificant adverse effects. With this degree of immer-
sion and type of interaction, the study by Everard et
al. developed an immersive VR version of the Box
and Block Test (BBT-VR) to assess manual dexterity
in stroke patients and healthy participants. The aim
was to evaluate the concurrent validity of the BBT-
VR, highlighting the need for regular follow-up and
kinematic assessments to objectively measure motor
recovery after stroke. The study by Lee et al. demon-
strates that a fully immersive VR rehabilitation pro-
gramme with an HMD and controllers is feasible for
upper limb rehabilitation in chronic stroke patients,
without serious adverse effects.
In the field of upper limb rehabilitation using im-
mersive VR systems and direct interaction with the
patient’s hands, is the study by AlMousa et al. (Al-
Mousa et al., 2020). This study presents the develop-
ment of a game designed for stroke patients requiring
upper limb rehabilitation at home. The game uses the
Oculus Rift HMD and the LMC hand tracker for a
fully immersive virtual reality experience.
In the latter group, the combination of immer-
sive virtual reality (VR) and hand tracking has proven
to be most effective for upper limb rehabilitation.
ICEIS 2024 - 26th International Conference on Enterprise Information Systems
380

This approach provides a more natural interaction,
which is crucial for patients with motor limitations
(AlMousa et al., 2020; Juan et al., 2023). In ad-
dition, non-immersive systems can limit depth per-
ception due to their design for flat monitors, which
negatively affects the user experience (Everard et al.,
2022).
2.2 Adaptation of VR Environments for
Rehabilitation
Adaptation in VR environments is essential to ensure
accessibility and effectiveness in rehabilitation. Sev-
eral studies have highlighted the accessibility chal-
lenges associated with these technologies, particu-
larly for people with physical disabilities. Mott et
al. (Mott et al., 2019) identify five key elements for
the accessibility of VR content: accessibility of inter-
action, accessibility of devices, inclusive representa-
tions and diversity of applications. In addition, in a
separate study conducted in 2020, (Mott et al., 2020)
identified seven specific barriers for people with re-
duced mobility, one of which related to the prepara-
tion of VR peripherals and the definition of VR game
boundaries.
The need to adapt virtual environments to the ca-
pabilities of rehabilitation patients is a topic widely
supported in the scientific literature. One example is
the study by Lagos Rodriguez et al. (Lagos Rodr
´
ıguez
et al., 2022) which highlights the importance of per-
sonalisation in VR environments, focusing on the spe-
cific needs of each patient. On the other hand, the
study by Carrington et al. (Pei et al., 2023), allows
wheelchair users to assess the accessibility of unfa-
miliar places remotely by exploring detailed digital
replicas. The study introduces a VR technique called
‘Embodied Exploration’, which allows wheelchair
users to explore high-fidelity digital replicas of phys-
ical environments. However, a limitation of the study
is the need for users to provide accurate measure-
ments of their biometrics.
3 BACKGROUND
Focused on the need to create patient-centred virtual
environments for upper limb rehabilitation in patients
with cSCI, the Rehab-Immersive (Herrera et al., 2023)
project arises, coordinated with the Hospital Nacional
de Parapl
´
ejicos (Toledo, Spain). In this project, a set
of serious games is being developed to improve the
mobility and manipulative skills of patients. Serious
games in the context of Rehab-Immersive take advan-
tage of the benefits of VR, such as motivation and re-
inforcement of the patient’s commitment, as well as
accurate monitoring and evaluation of the evolution
of the treatment by the specialist.
Through various analyses and tests conducted
with patients and specialists, a key element has been
identified in VR environments for the rehabilitation of
cSCI patients: the significance of three-dimensional
(3D) positioning of elements within the space that pa-
tients interact with.
In order to solve this problem, a manual calibra-
tion of the elements with which the patient interacts
was implemented in two ways: with predefined posi-
tions (closer and further away) in the three axes, and
through manual positioning of the object in 3D space.
However, moving barriers were found in the man-
ual calibration. First, depending on the patient’s mo-
bility, it can be a tedious process. This is the case
when the elements with which the patient must in-
teract are positioned too far apart, leading to a sub-
optimal interaction location. Additionally, complex-
ity increases when there are numerous elements that
require individual configuration. Second, there are
patients who, given their conditions, cannot calibrate
the elements well due to grip difficulties. In the case
of predefined positions, these may not be adequately
adapted to the optimum. Thirdly, this calibration has
to be done for each element with which interactive
element and for each serious set, which is a slow pro-
cess.
Particularly in patients with limited or no func-
tional grip, this approach presents a significant prob-
lem, making it necessary for the specialist to intervene
by positioning the item. However, the specialist’s
view of the 3D space is not through the VR HMD, but
on a screen, which leads to a loss of depth sensation
and can lead to errors in calibration.
4 CALIBRATION SYSTEM
In response to the challenges mentioned above, the
calibration system proposed in this paper is tailored to
the specific needs of cSCI patients. This system is de-
signed to accommodate several factors to accomplish
effective rehabilitation. To achieve this, both the cali-
bration system and the BBT-VR have been developed
using Unity
1
and the Meta XR Interaction SDK
2
. First
of all, it takes into account the patient’s posture and
limited mobility, since the exercises are performed sit-
ting and without moving. This consideration includes
1
https://unity.com/
2
https://developer.oculus.com/documentation/unity/
unity-isdk-interaction-sdk-overview/
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible
381
(a) (b) (c)
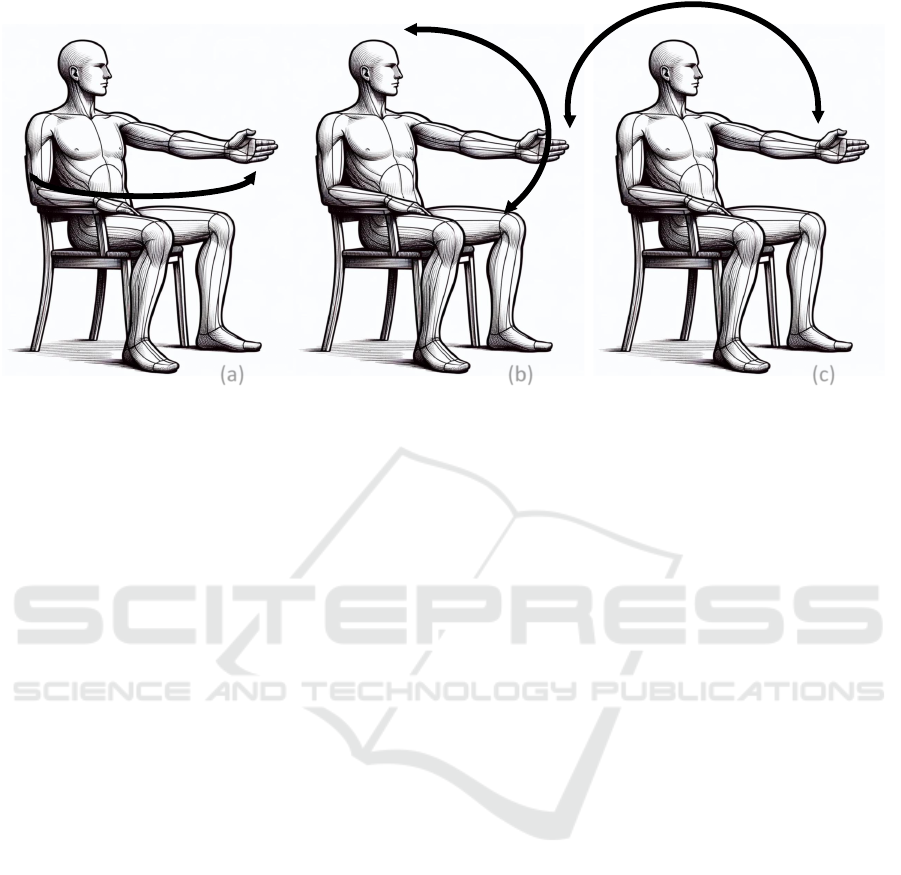
Figure 2: Movements to be reproduced for the calibration of the right and left arm in the three planes: (a) transverse plane,
(b) sagittal plane, and (c) frontal plane.
the height of the items and the position of the patient’s
legs.
The system also provides individual calibration
for each upper limb, adjusting the virtual environment
to respect the limitations and capabilities of each side
of the body.
In addition, the system is applicable to different
games and interactive elements. It incorporates cali-
bration data to adapt the interactive elements depend-
ing on the type of exercise, whether monomanual or
bimanual, and whether it involves gripping or not.
A key feature of this system is its automation and
customization capabilities. It automates the calibra-
tion process based on patient mobility and capacity
data, facilitating accurate and efficient customization
for each individual.
Thanks to this calibration, a safe VR environ-
ment is provided. Feature that helps prevent exces-
sive efforts and compensatory movements that could
be detrimental to the patient’s health.
Finally, the system improves ease of use, improv-
ing patient autonomy in the use of VR.
In summary, the proposed calibration system aims
to improve the patient’s experience and optimize re-
habilitation results, adjusting to the evolution of the
patient’s motor capacity and ensuring that the exer-
cises are performed safely and effectively.
Additionally, the calibration system will be tested
with one of the games implemented within Rehab-
Immersive, specifically the BBT-VR. The BBT, is a
manipulative dexterity test in which the patient must
move as many blocks as possible from one compart-
ment to another within a box, all within 60 seconds
(Mathiowetz et al., 1985).
The implemented calibration system is designed
to adapt the virtual workspace to fit the motor skills
of each cSCI patient. This calibration process takes
into account three aspects: i) head position, ii) elbow
flexion and, iii) shoulder movements.
The initial state of the HMD is captured to de-
termine the position and rotation of the head at rest.
On the other hand, elbow flexion, with the hands hip-
width apart, is used to determine the central area to
the patient and the position of the hands in this pose,
which is used for some therapeutic exercises. How-
ever, it is the analysis of the shoulder movements
that plays a central role in this process, following the
principles established by I. A. Kapandji (Kapandji,
1971). In this book, Kapandji details the complex
movements of the shoulder in the sagittal, frontal and
transveral planes, which include flexion and exten-
sion, abduction and adduction, and horizontal flexion
and extension, respectively.
The objective of this calibration phase is to de-
termine the maximum reach that a user can achieve
with each hand in three planes. The kinematics of the
shoulder are critical in this process, as the maximum
reach is achieved with the arm and elbow fully ex-
tended. The use of ellipses, rather than circles, to de-
fine the workspace is adopted because of the potential
mobility restrictions that patients may have. Ellipses
offer greater flexibility to accommodate these limita-
tions. Since users are seated and cannot perform the
full circumduction movement, the workspace is ide-
ally limited to the front and side areas, rather than ex-
tending behind the patient. In an optimal scenario,
these ellipses will approximate to circles. Through
various tests, it has been proven that using ellipses to
ICEIS 2024 - 26th International Conference on Enterprise Information Systems
382
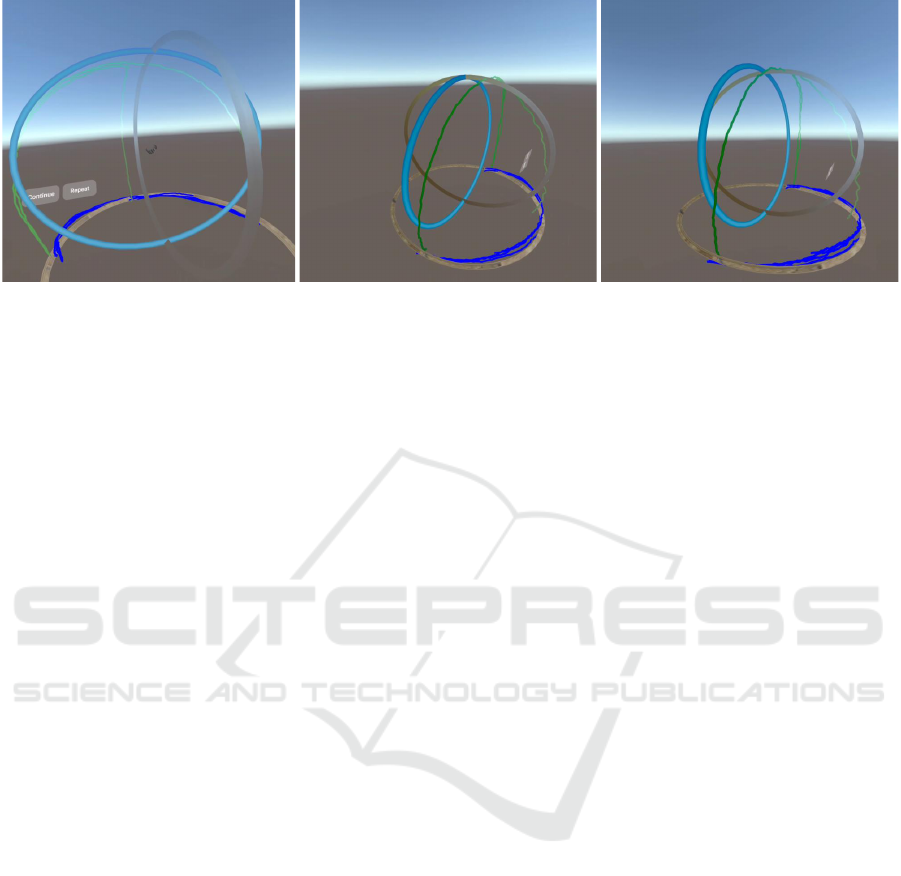
Figure 3: An example of sagittal, frontal, and transverse ellipses resulting from the calibration process. Images taken from
different perspectives and decorative elements have been removed for clearer visualization.
define the workspace results in greater accuracy than
using circles.
The calibration process has been designed in an
intuitive and detailed way. Each phase of calibration
is accompanied by an instructional video in which an
avatar demonstrates the specific movements that the
user must replicate. At the end of each instructional
video, the application emits a sound to indicate that
the user must begin to perform the movements or po-
sition themselves in the explained pose.
During the whole process, the user must keep his
back well supported and without twisting his trunk.
This requirement is essential in order to know the de-
gree of mobility of the upper limbs without the inter-
vention or influence of trunk movement.
In the first stage, the patient is instructed to look
forward for a few seconds. This first step captures
the position and rotation of the HMD, as its default
position is not always aligned with the zero position
on all three axes.
hmdInitialPosition = (x
hmd
,y
hmd
,z
hmd
),
hmdInitalRotation = (α
hmd
,β
hmd
,γ
hmd
),
where (α
hmd
,β
hmd
,γ
hmd
) are the Euler angles.
The second stage is for the patient to bend his
elbows 90 degrees while keeping his arms aligned
across the hip, making sure his hands are above the
knees. This position helps determine the central area
and ideal position for many virtual reality games.
An example of the importance of these positions is
the BBT-VR. This calibration ensures that the box is
placed in front of the patient at the correct height,
aligning with the elbows bent at 90 degrees.
centerPalmR = (x
r
,y
r
,z
r
),
centerPalmL = (x
l
,y
l
,z
l
),
During the third step, the calibration process is
further divided into two new phases. First, a detailed
calibration of the upper limbs movements in three di-
mensional planes is performed.
In this new first phase, the avatar asks the user to
fully extend the arm in the transversal plane and move
the arm from one end of the X-axis to the other, keep-
ing the arm above the knees (see Figure 2.a). This
stage is designed to calibrate the range of motion in
the horizontal plane and the patient’s ability to reach
laterally, thus capturing the range of possible move-
ments in this plane.
The second part of the calibration relates to the
frontal and sagittal planes. As in the previous stage,
the patient is asked to fully extend the arm. After the
avatar has shown the necessary movements, the cali-
bration begins. These movements consist of extend-
ing the arm from one end of the X-axis to the other
and moving it along the Y-axis (height) and Z-axis
(depth) (see Figure 2.b and c). The trajectory of these
movements simulates the drawing of a dome in the
air. This process is designed to assess and calibrate
the patient’s ability to perform both vertical and depth
movements. Figure 3 shows an example of ellipses
formed in the sagittal, frontal, and transverse planes,
outlining the patient’s movement scope. Next to the
ellipses, less firm traces, generated by the user during
the calibration process, are visible.
Simultaneously, and transparently to the user, the
system creates two lists of points during the calibra-
tion process. The first list, denoted as (P
R
XZ
), collects
the points traced by the patient’s arm in the X Z plane.
This list encapsulates all the trajectories performed in
the XZ plane.
The second list,P
R
XY/Y Z
, consists of the points gen-
erated during movements in the XY and Y Z planes.
These two lists, together provide a complete rep-
resentation of the patient’s arm movement capabili-
ties in all three axes. This separation into two lists
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible
383
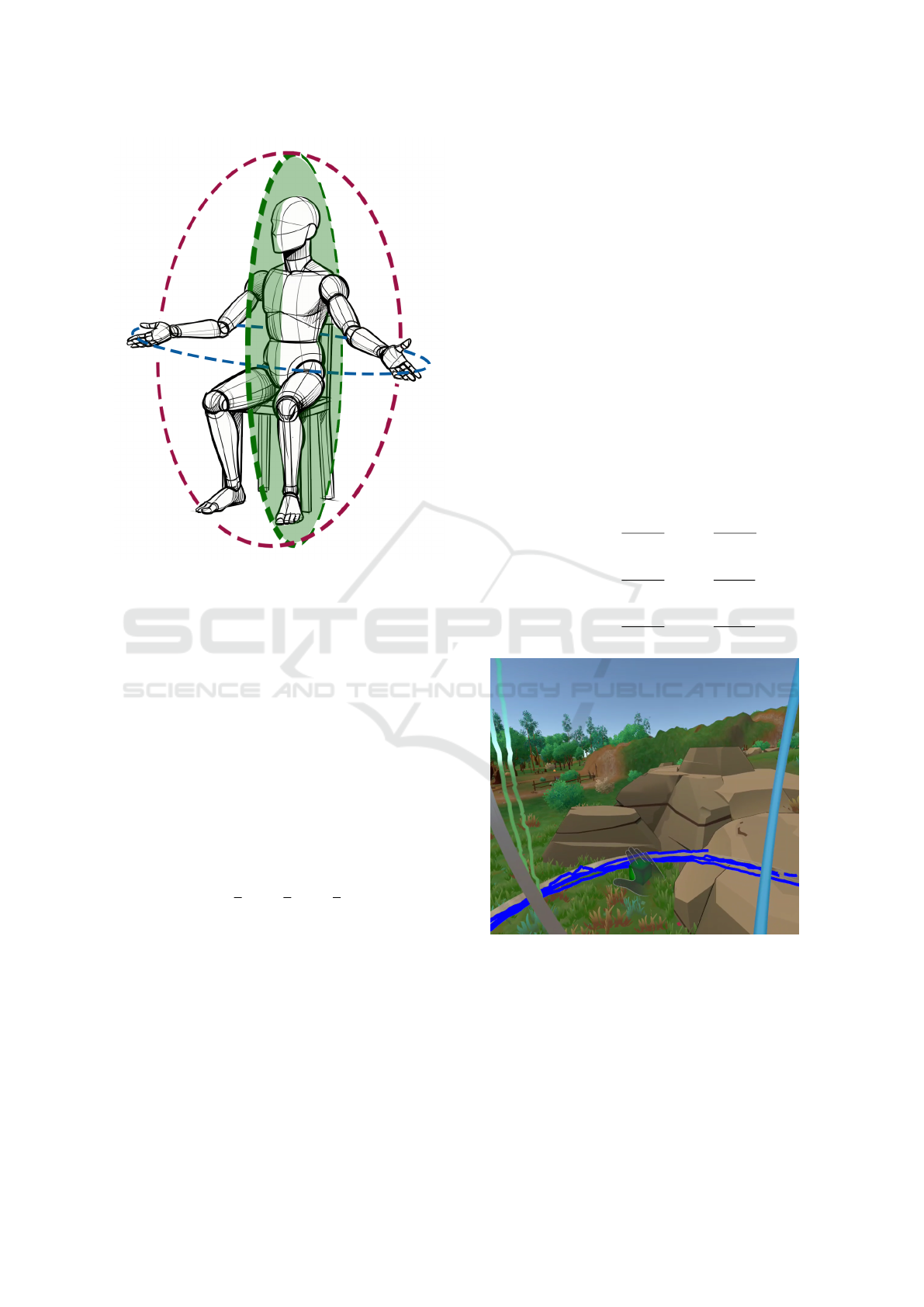
Figure 4: An example of sagittal, frontal, and transverse
ellipses resulting from the calibration process.
allows a more detailed and specific assessment of the
movement capabilities in different planes, facilitating
a more accurate calibration.
The fourth stage shows the calibration results. Af-
ter completing the calibration, the system draws three
ellipses. Each ellipse corresponds to the range of mo-
bility of the patient’s arm in different planes: XY , XZ,
and Y Z. These ellipses are calculated based on the
trajectory data (P
R
and P
L
) collected for each arm,
ensuring they represent the patient’s actual movement
capabilities. The ellipses are defined as follows:
1. The center of each ellipse, denoted as C, is com-
puted as the average position of the trajectory
points within each plane:
C =
1
n
n
∑
i=1
x
i
,
1
n
n
∑
i=1
y
i
,
1
n
n
∑
i=1
z
i
!
,
for (x
i
,y
i
,z
i
) ∈ P
R
or P
L
.
2. The radii of the ellipses are calculated based on
the maximum distances from the center point to
the points within each plane. For a set of points
{(x
i
,y
i
,z
i
)}, the radii in the X,Y , and Z directions
are calculated as:
r
x
= max
(x
i
,y
i
,z
i
)∈P
|x
i
− x
C
|,r
y
= max
(x
i
,y
i
,z
i
)∈P
|y
i
− y
C
|,
r
z
= max
(x
i
,y
i
,z
i
)∈P
|z
i
− z
C
|.
To test the accuracy of the calibration, a virtual
block is displayed at the center of the palm of the
patient’s hand (see Figure 5). The patient can move
their hand freely, with the block remaining attached
to the palm’s center. The color of the block provides
immediate feedback: it appears green if it is within
the defined ellipses, signifying that the hand is within
the calibrated workspace. If the block turns red, it in-
dicates that the hand has moved outside the defined
working area, surpassing the calibrated range of mo-
tion. To determine if a point is inside the calibrated
workspace, defined by ellipses in the XY , XZ, and Y Z
planes, the following mathematical condition is used:
Let O = (o
x
,o
y
,o
z
) represent the position of the
object (e.g., virtual block) in 3D space, and let C =
(c
x
,c
y
,c
z
) be the center of the ellipses with radii r
x
,
r
y
, and r
z
in the X ,Y , and Z dimensions, respectively.
The point O is considered to be inside the calibrated
workspace if the following conditions are met for
each plane:
Inside XY-plane:
o
x
− c
x
r
x
2
+
o
y
− c
y
r
y
2
≤ 1
Inside XZ-plane:
o
x
− c
x
r
x
2
+
o
z
− c
z
r
z
2
≤ 1
Inside YZ-plane:
o
y
− c
y
r
y
2
+
o
z
− c
z
r
z
2
≤ 1
Figure 5: Post-calibration environment with a cube attached
to the hand, indicating boundaries in green (within limits) or
red (outside limits).
Finally, the fifth stage involves the storage of the
calibration data. Once the calibration is completed
and verified for accuracy, the system stores the rele-
vant data in a historical record. This allows for the
calibration to be referenced or adjusted in future ses-
sions, ensuring a tailored and efficient VR experience
for each patient.
ICEIS 2024 - 26th International Conference on Enterprise Information Systems
384

The stored historical data, used for game cali-
bration, also presents another value for medical spe-
cialists. By regularly repeating the calibration pro-
cess over time, changes in a patient’s mobility can
be closely monitored. This enables a more personal-
ized rehabilitation approach, tailored specifically ac-
cording to the evolving mobility data of each patient,
thereby optimizing the rehabilitation process.
4.1 Application of Calibration Data in
BBT-VR
In the specific case of the BBT-VR (see Figure 6),
which is a monomanual exercise, the precise position-
ing of the virtual box is essential. The calibrated data
is used to ensure that the box is placed in a comfort-
able position in front of the user, without requiring
excessive arm extension.
Additionally, the height of the virtual box is care-
fully adjusted to be suitable for the patient’s stature. It
is positioned to avoid being too high or too low, which
might interfere with the patient’s legs, considering the
seated position during the exercise.
Furthermore, the box is centered relative to the pa-
tient’s midline, ensuring that the exercises are sym-
metric and balanced, regardless of which hand is be-
ing used.
To facilitate these adjustments in BBT-VR, an op-
tion has been added to the configuration menu that
allows users to choose between automatic or man-
ual calibration. The manual option involves the user
physically grabbing the box and moving it to the ap-
propriate position. Additionally, while the box is ide-
ally positioned in front of the user, the option for lat-
eral positioning has been introduced. This lateral po-
sition will be to the right if the right hand is selected
as dominant, and to the left if the left hand is chosen.
Depending on the selected configuration, the
BBT-VR begins by placing the box either manually
or automatically, and in the selected position, either
central or lateral.
5 EVALUATION AND RESULTS
The evaluation was conducted with a diverse group
of participants, including both men and women, aged
between 20 and 43 years. All participants selected did
not have any mobility issues in their upper limbs. The
study was divided into two sessions: the first involved
6 participants, while the second included 9.
Initially, participants received a comprehensive
briefing about the test session’s procedures. The first
part of the session focused on testing an automatic
Figure 6: BBT implementation in VR.
calibration system (see Figure 7). Participants were
required to follow instructions provided by an avatar,
mimicking the indicated movements. To correctly
perform the calibration, participants were asked to
keep their backs against the backrest and ensure all
movements were made without twisting or shifting
their torso. After calibration, they were asked to ver-
ify if the defined area appropriately adapted to the ac-
cessible area for them, without the need for excessive
movements or trunk torsions.
Subsequently, the participants were introduced to
a BBT-VR application. In this part, they tested the
automatic calibration, both in central and lateral posi-
tioning, for the right and left hands.
Finally, participants completed a questionnaire to
gather their impressions and feedback on the experi-
ence. The questionnaire, which was explained to each
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible
385

participant before completion, comprised 10 ques-
tions. The initial set collected basic information, such
as the participant’s assigned identifier, age, height,
and hand dominance. Question 4 asked about previ-
ous experience with immersive virtual reality (HMD)
devices, asking: ’have you used immersive virtual re-
ality HMD devices before?’, with possible answers:
’Never (N)’, ’Occasionally (O)’ or ’Frequently (F)’.
The following questions examined their experiences
with the calibration system and the VR application,
using a Likert scale for responses:
• Q6: did you find the automatic calibration system
complex? Rate on a scale of 1 to 5, where 1 is not
complex at all and 5 is very complex.
• Q7: after calibration, do you feel that the work-
ing area defined by the three ellipses adequately
matches the range of motion limits of your upper
limb? Please rate on a scale of 1 to 5, where 1
means ’not at all’ and 5 means ’completely’.
• Q8: is the position of the box in the BBT-VR
application, with automatic calibration in normal
mode (centered to the user), correct for you?
• Q9: is the position of the box in the BBT-VR ap-
plication, with automatic calibration in right lat-
eral mode, correct for you?
• Q10: is the position of the box in the BBT-VR ap-
plication, with automatic calibration in left lateral
mode, correct for you?
For questions Q8, Q9, and Q10, participants rated
the appropriateness of the box’s position on a Likert
scale from 1 to 5, where 1 indicates the lowest score
(least appropriate) and 5 indicates the highest score
(most appropriate).
Also, to facilitate observation and verification of
the participants’ movements and actions during the
test, an external screen was used. This screen mir-
rored in real-time what the participants were seeing
through the Meta Quest 3.
Figure 7: Moments captured during evaluation, while par-
ticipants test the calibration method.
5.1 Results
The results obtained in the study were analyzed from
two complementary perspectives. The first, a quanti-
tative approach, focused on technical considerations
related to the elliptical volume defined by ellipses in
the XZ, XY , and ZX planes. For the central position
of the box, it was verified that the center of the box
was located within the elliptical volume, in relation to
both the right and left sides of the upper limbs. For
the lateral positions of the box, it was confirmed that
the center of the box was within the control area de-
fined by the corresponding elliptical volume (right or
left).
The second perspective, with a qualitative ap-
proach, focused on the patient’s viewpoint and per-
ception. This subjective evaluation sought to under-
stand the experiences and impressions of the partic-
ipants regarding the calibration process and their in-
teraction with the virtual environment. Analyzing the
results of the VR experience questionnaire, we identi-
fied several significant trends that reflect participants’
perceptions of the VR calibration system and its sub-
sequent use in the BBT-VR application.
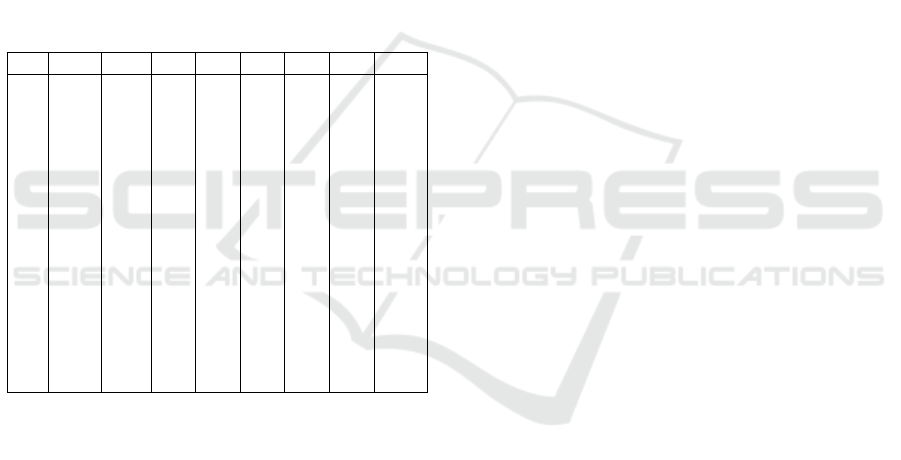
The data presented in Table 1 includes the re-
sponses to the questionnaire. To complete this
overview, it is worth mentioning that for question Q5,
all participants reported being right-handed. The ease
of use of the calibration system is highlighted, as ev-
idenced by the low average score of 1.07 in question
Q6, with a standard deviation of only 0.26. This indi-
cates that most participants found the system straight-
forward, with very little variation in their responses,
reinforcing the notion of an intuitive and easy-to-
manage design.
Regarding the accuracy of the working area (Q7),
the high average scores of 4.27, with a standard devi-
ation of 1.03, suggest that participants generally per-
ceived that the defined working area aligned well with
the movement limits of their upper limbs.
As for the appropriateness of the box’s position in
the BBT-VR application (Q8, Q9, Q10), the predomi-
nantly positive responses are reflected in the high av-
erage scores (4.73 for Q8, 4.33 for Q9 and Q10), with
relatively low standard deviations (0.46 for Q8, 0.62
for Q9, and 0.49 for Q10). These figures indicate a
generally favorable perception of the box calibration
in all modes. However, it is interesting to note the
trend of slightly higher scores for the box’s central
position (normal mode) compared to the lateral posi-
tions. This could suggest a perceived greater accuracy
or comfort in the central setup, although the variations
are not substantial.
To conclude, the study provides a comprehensive
ICEIS 2024 - 26th International Conference on Enterprise Information Systems
386
understanding of the VR upper limb calibration sys-
tem and its integration into the BBT-VR, using both
quantitative and qualitative approaches. From a tech-
nical perspective, the precise placement of the BBT-
VR box within the elliptical volume was validated in
both central and lateral positions, ensuring the cor-
rect execution of the exercises without excessive ef-
fort or compensatory movements. From a user per-
spective, the ease of use of the system and the posi-
tive perception of the accuracy of the workspace and
box placement in the application were highlighted.
These results underline the technical effectiveness of
the system and its positive reception by users, high-
lighting its potential in precision-oriented VR appli-
cations while ensuring user comfort.
Table 1: Table summarizing the responses collected from
the questionnaire on automatic calibration. The columns,
from left to right, represent the participant ID, age, height,
and responses to questions related to the automatic calibra-
tion system and the BBT-VR.
ID Age Ht Q4 Q6 Q7 Q8 Q9 Q10
1 21 178 N 1 5 4 3 5
2 27 160 F 1 4 5 4 4
3 24 174 F 1 4 5 5 5
4 21 191 N 2 5 5 4 4
5 21 165 N 1 4 5 5 4
6 21 180 O 1 5 5 5 5
7 40 166 F 1 4 5 4 5
8 42 172 F 1 4 4 5 4
9 38 179 O 1 5 5 4 4
10 30 165 O 1 4 5 5 4
11 37 166 F 1 5 4 4 4
12 41 178 N 1 5 5 4 4
13 29 175 O 1 4 5 4 4
14 27 173 F 1 1 5 5 5
15 43 177 F 1 5 4 4 4
6 LIMITATIONS AND FUTURE
WORK
Although the initial results of the calibration system
are promising, further validation is needed to confirm
its effectiveness. A larger study with a larger number
of participants, including people with cSCI, is needed
to confirm the preliminary results. Previous tests were
conducted exclusively with healthy individuals, as the
primary objective of this initial phase was to estab-
lish the system’s safety before extending the testing
to patients in subsequent phases. Additionally, storing
other variables like the maximum degree of wrist flex-
ion/abduction and arm rotation should be considered
to enhance the calibration accuracy and applicability.
Following the study, there is a need to automate
the implementation of the calibration system for each
set. In the current iteration, specific values of the cal-
ibration data were manually selected and applied to
correctly position elements in 3D space for the test
set. The aim for future development is to automate
this aspect so that the system can classify each set ac-
cording to a set of parameters and automatically apply
the calibration values in an efficient manner.
This will require a thorough study and ranking
of the relevant parameters. These parameters could
include factors such as whether the exercise is one-
handed or bimanual, involves lateral trunk displace-
ment or not, and requires centred positioning or posi-
tioning adapted to the range of motion of each arm. It
will also be important to consider the plane of move-
ment, whether vertical or horizontal. This second
phase of implementation of the VR upper limb reha-
bilitation calibration system aims to facilitate its im-
plementation in any game in a simple way.
7 CONCLUSIONS
This article presents an innovative calibration method
for immersive spaces used in upper limb rehabilita-
tion. The method particularly accounts for the mo-
tor limitations of patients with cervical spinal cord in-
juries who require rehabilitative therapy to regain mo-
bility. A key novelty of the method is its considera-
tion of the limitations of each limb individually, form-
ing three ovals in the sagittal, frontal, and transverse
planes. The set of generated ovals, along with the
proposed methods, are used to reconfigure the virtual
environment in which the patient exercises, ensuring
that all objects they interact with are within reach
based on the detected limitations. In other words, the
environment adapts to become an accessible, suitable,
and safe space for therapy.
The correct distribution of virtual components
with which the user interacts, taking their limitations
into account, also prevents more significant problems
such as body compensations that could endanger the
integrity of healthy parts.
Finally, the different calibrations performed by the
same patient at different times, along with the record-
ing of kinematics during exercise, provide therapists
with a valuable tool for objectively measuring a pa-
tient’s progress. In particular, comparing calibrations
allows for the measurement of improvements in mo-
bility.
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible
387

ACKNOWLEDGEMENTS
This work has been founded by the Spanish Ministry
of Science, Innovation and Universities under the Re-
search Project: Platform for Upper Extremity Reha-
bilitation based on Immersive Virtual Reality (Rehab-
Immersive), PID2020-117361RB-C21 and PID2020-
117361RB-C22.
REFERENCES
AlMousa, M., Al-Khalifa, H. S., and AlSobayel, H. (2020).
Move-IT: A Virtual Reality Game for Upper Limb
Stroke Rehabilitation Patients. In Computers Helping
People with Special Needs: 17th International Con-
ference, ICCHP 2020, Lecco, Italy, September 9–11,
2020, Proceedings, Part I, pages 184–195, Berlin,
Heidelberg. Springer-Verlag.
Cha, K., Wang, J., Li, Y., Shen, L., Chen, Z., and Long,
J. (2021). A novel upper-limb tracking system in a
virtual environment for stroke rehabilitation. Journal
of NeuroEngineering and Rehabilitation, 18(1):166.
Creed, C., Al-Kalbani, M., Theil, A., Sarcar, S., and
Williams, I. (2023). Inclusive AR/VR: accessibility
barriers for immersive technologies. Universal Access
in the Information Society.
de Los Reyes-Guzm
´
an, A., Lozano-Berrio, V., Alvarez-
Rodr
´
ıguez, M., L
´
opez-Dolado, E., Ceruelo-Abajo, S.,
Talavera-D
´
ıaz, F., and Gil-Agudo, A. (2021). Rehab-
Hand: Oriented-tasks serious games for upper limb
rehabilitation by using Leap Motion Controller and
target population in spinal cord injury. NeuroReha-
bilitation, 48(3):365–373.
Dias, P., Silva, R., Amorim, P., La
´
ıns, J., Roque, E.,
Ser
ˆ
odio, I., Pereira, F., and Santos, B. S. (2019). Using
Virtual Reality to Increase Motivation in Poststroke
Rehabilitation. IEEE Computer Graphics and Appli-
cations, 39(1):64–70. Conference Name: IEEE Com-
puter Graphics and Applications.
Everard, G., Otmane-Tolba, Y., Rosselli, Z., Pellissier, T.,
Ajana, K., Dehem, S., Auvinet, E., Edwards, M. G.,
Lebleu, J., and Lejeune, T. (2022). Concurrent valid-
ity of an immersive virtual reality version of the Box
and Block Test to assess manual dexterity among pa-
tients with stroke. Journal of NeuroEngineering and
Rehabilitation, 19(1):7.
Goudman, L., Jansen, J., Billot, M., Vets, N., Smedt, A. D.,
Roulaud, M., Rigoard, P., and Moens, M. (2022). Vir-
tual Reality Applications in Chronic Pain Manage-
ment: Systematic Review and Meta-analysis. JMIR
Serious Games, 10(2):e34402.
Herrera, V., Vallejo, D., Castro-Schez, J. J., Monekosso,
D. N., de los Reyes, A., Glez-Morcillo, C., and Al-
busac, J. (2023). Rehab-Immersive: A framework to
support the development of virtual reality applications
in upper limb rehabilitation. SoftwareX, 23:101412.
Juan, M.-C., Elexpuru, J., Dias, P., Santos, B. S., and
Amorim, P. (2023). Immersive virtual reality for upper
limb rehabilitation: comparing hand and controller in-
teraction. Virtual Reality, 27(2):1157–1171.
Kapandji, I. (1971). The Physiology of the Joints, Volume I,
Upper Limb, volume 50. Churchill Livingstone.
Khundam, C. and N
¨
oel, F. (2021). A Study of Physical
Fitness and Enjoyment on Virtual Running for Ex-
ergames. International Journal of Computer Games
Technology, 2021:1–16.
Lagos Rodr
´
ıguez, M., Garc
´
ıa, A. G., Loureiro, J. P., and
Garc
´
ıa, T. P. (2022). Personalized Virtual Reality En-
vironments for Intervention with People with Disabil-
ity. Electronics, 11(10):1586. Number: 10 Publisher:
Multidisciplinary Digital Publishing Institute.
Lim, D. Y., Hwang, D. M., Cho, K. H., Moon, C. W., and
Ahn, S. Y. (2020). A Fully Immersive Virtual Reality
Method for Upper Limb Rehabilitation in Spinal Cord
Injury. Annals of Rehabilitation Medicine, 44(4):311–
319.
Luo, Z., Lim, A. E.-P., Durairaj, P., Tan, K. K., and Ve-
rawaty, V. (2023). Development of a compensation-
aware virtual rehabilitation system for upper extrem-
ity rehabilitation in community-dwelling older adults
with stroke. Journal of NeuroEngineering and Reha-
bilitation, 20(1):56.
Mallari, B., Spaeth, E. K., Goh, H., and Boyd, B. S. (2019).
Virtual reality as an analgesic for acute and chronic
pain in adults: a systematic review and meta-analysis.
Journal of Pain Research, 12:2053–2085.
Mathiowetz, V., Volland, G., Kashman, N., and Weber, K.
(1985). Adult norms for the box and block test of man-
ual dexterity. The American Journal of Occupational
Therapy, 39(6):386–391.
Mott, M., Cutrell, E., Gonzalez Franco, M., Holz, C., Ofek,
E., Stoakley, R., and Ringel Morris, M. (2019). Acces-
sible by Design: An Opportunity for Virtual Reality.
In 2019 IEEE International Symposium on Mixed and
Augmented Reality Adjunct (ISMAR-Adjunct), pages
451–454.
Mott, M., Tang, J., Kane, S., Cutrell, E., and Ringel Mor-
ris, M. (2020). “I just went into it assuming that I
wouldn’t be able to have the full experience”: Under-
standing the Accessibility of Virtual Reality for Peo-
ple with Limited Mobility. In The 22nd International
ACM SIGACCESS Conference on Computers and Ac-
cessibility, pages 1–13, Virtual Event Greece. ACM.
Onitsuka, K., Kubota, K., Yokoyama, M., Miyazawa, T.,
Hamaguchi, T., Taniguchi, H., Usuki, N., Miyamoto,
S., Okazaki, K., Murata, K., and Kanemura, N.
(2023). Clinical utility of markerless motion capture
for kinematic evaluation of sit-to-stand during 30 s-
CST at one year post total knee arthroplasty: a ret-
rospective study. BMC Musculoskeletal Disorders,
24(1):254.
Park, J.-S., Jung, Y.-J., and Lee, G. (2020). Vir-
tual Reality-Based Cognitive–Motor Rehabilitation
in Older Adults with Mild Cognitive Impairment:
A Randomized Controlled Study on Motivation and
Cognitive Function. Healthcare, 8(3):335. Number:
3 Publisher: Multidisciplinary Digital Publishing In-
stitute.
ICEIS 2024 - 26th International Conference on Enterprise Information Systems
388

Pei, S., Chen, A., Chen, C., Li, F. M., Fozzard, M., Chi, H.-
Y., Weibel, N., Carrington, P., and Zhang, Y. (2023).
Embodied Exploration: Facilitating Remote Accessi-
bility Assessment for Wheelchair Users with Virtual
Reality. In Proceedings of the 25th International ACM
SIGACCESS Conference on Computers and Accessi-
bility, ASSETS ’23, pages 1–17, New York, NY, USA.
Association for Computing Machinery.
Shahmoradi, L., Almasi, S., Ahmadi, H., Bashiri, A., Azadi,
T., Mirbagherie, A., Ansari, N. N., and Honarpishe,
R. (2021). Virtual reality games for rehabilitation of
upper extremities in stroke patients. Journal of Body-
work and Movement Therapies, 26:113–122.
Soomal, H. K., Poyade, M., Rea, P. M., and Paul, L. (2020).
Enabling More Accessible MS Rehabilitation Train-
ing Using Virtual Reality. Advances in Experimental
Medicine and Biology, 1262:95–114.
Teo, J. L., Zheng, Z., and Bird, S. R. (2022). Identifying
the factors affecting ‘patient engagement’ in exercise
rehabilitation. BMC Sports Science, Medicine and Re-
habilitation, 14:18.
Zhang, W., Paudel, D., Shi, R., Liang, J., Liu, J., Zeng, X.,
Zhou, Y., and Zhang, B. (2020). Virtual Reality Ex-
posure Therapy (VRET) for Anxiety Due to Fear of
COVID-19 Infection: A Case Series. Neuropsychi-
atric Disease and Treatment, 16:2669–2675.
Advanced VR Calibration for Upper Limb Rehabilitation: Making Immersive Environments Accessible
389
