
Contextualizing Syntactic Interoperability Data Standards for Health
Information Exchange in Uganda's Public Healthcare System
Bagyendera Moses
1,*
, Nabende Peter
1
, Godman Brian
2,3,*
and Nabukenya Josephine
1
1
Department of Information Systems, Makerere University, Kampala PO Box 7062, Uganda
2
Strathclyde Institute of Pharmacy and Biomedical Sciences, Strathclyde University, Glasgow G4 0RE, U.K.
3
School of Pharmacy, Sefako Makgatho Health Sciences University, Ga-Rankuwa, Pretoria 0208, South Africa
Keywords: Data Use, eHealth, Electronic Health Records, Syntactic Interoperability Standards, Hospitals, Uganda.
Abstract: Syntactic interoperability data standards are crucial for effective collaboration in modern health systems,
enabling seamless exchange of healthcare information. This paper aims to develop contextualized standards
to support digital healthcare in Uganda within the WHO global strategic framework 2020-2025. The standards
ensure patient data is collected, processed, shared, and stored in formats that facilitate interoperability.
Validation was done by the Health Information Innovation Research and Evaluation Technical Working
Group (HIIRETWG). A case study approach gathered primary data through questionnaires from Uganda's
healthcare experts. Derived from landscape studies, these standards underwent expert verification and testing.
Results show strong support (96%) for the developed standards, with 68% participation from digital health
experts. These standards are poised to strengthen Uganda's digital health system and inform decision-making
processes at various levels. The study underscores the importance of tailored standards to enhance healthcare
information exchange in resource-limited settings.
1 INTRODUCTION
The World Health Organization (WHO) recognizes
the crucial role of interoperability in health systems,
promoting equitable access to quality health data and
services globally (World Health Organization, 2020,
2021). This extends to various standards, including
Semantic/Terminology,Syntactic/Content, Transport,
Infrastructure, and Security/Privacy. This paper
focuses on Syntactic interoperability data standards,
emphasizing their significance in ensuring consistent
data structure and formatting for seamless
information exchange within healthcare systems.
Globally, three commonly used syntactic
interoperability data standards are Health Level
Seven (HL7), Fast Healthcare Interoperability
Resources (FHIR), and Digital Imaging and
Communications in Medicine (DICOM). These
standards provide a common language for healthcare
data exchange, facilitating electronic sharing to
enhance future patient care (Lin et al., 2010;
Umberfield et al., 2023).
*
*
Authors of correspondence
In Sub-Saharan Africa, limited interoperability
within health systems impedes effective data
collection and use (Verbeke et al., 2015). While some
countries like Rwanda, South Africa, and Kenya have
implemented standards to support seamless
integration and patient information flow, there's a
dearth of appropriate syntactic interoperability
standards continent-wide. This challenge is not
unique to Africa, as even European healthcare
systems face difficulties in capturing uniform patient
data (Pisana et al., 2022).
The barriers to interoperability and data utilization
in public healthcare systems include limited
knowledge of data analysis, poor attitudes toward
data reporting, and cultural challenges (Jawhari et al.,
2016; Kiberu et al., 2017; Kiwanuka & Nabukenya,
2023; Matovu & Ngo’ng’ Ocholla, 2009; Okungu et
al., 2019).
In Uganda, the Ministry of Health (MoH) has yet
to officially adopt inteoperability datae standards for
electronic data sharing, despite some health facilities
implementing these standards independently
(Kiwanuka et al., 2021; Wamema et al., 2023). The
Moses, B., Peter, N., Brian, G. and Josephine, N.
Contextualizing Syntactic Interoperability Data Standards for Health Information Exchange in Uganda’s Public Healthcare System.
DOI: 10.5220/0012711100003699
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2024), pages 267-275
ISBN: 978-989-758-700-9; ISSN: 2184-4984
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
267

lack of comprehensive guidelines for sharing
electronic patient data is a major barrier, hampering
the realization of the WHO global strategic
framework (Adeleke & Lawal, 2015; Ishijima et al.,
2015; Kiberu et al., 2017; Kiwanuka et al., 2021). The
existing Health Management Information System
(HMIS) in Uganda, initiated in 1985 and evolved into
DHIS 2 in 2012, aims to collect and manage
epidemiological and administrative information at the
district level.
Unfortunately, these systems lack customized
syntactic interoperability standards, hindering
reliable, timely, and integrated electronic health data
sharing.
The study seeks to validate requirements and
syntactic interoperability data standards for Uganda's
healthcare system, aligning with the WHO Global
Framework, 2020-2025, to provide guidance for
future healthcare improvements (World Health
Organization, 2021). As a result, provide guidance to
all key stakeholders in Uganda to help improve the
healthcare of its citizens in the future.
2 METHODOLOGY
2.1 Study Design
The study was conducted in three phases. First, a
requirements analysis was undertaken, which is a
descriptive cross-sectional survey to identify the
requirements of interoperability data standards for
HIE in Uganda (Peddireddy & Nidamanuri, 2021;
Shah et al., 2014) . The requirement analysis is seen
as an important and key stage in Design Science
Research (DSR) and artifact (Baskerville et al., 2018;
Peffers et al., 2007). This analysis is typically
performed using brainstorming, a systems review,
and a literature review (Achampong & Dzidonu,
2017). This approach identifies the requirements of
the various actors and users of a system yet to be built.
The outcome measures of the requirement analysis
process are the purpose, scope, and objectives of any
proposed solution.
In the second phase, the Syntactic Interoperability
data standards were generated based on the
ascertained requirements from the first phase.
Syntactic interoperability Data standards encompass
regulations for exchanging and sharing data within a
standardized framework. A number of standards
should be applied to ensure that the patient (health)
data collected as well as the information processed,
shared, and stored, are in formats that support
syntactic interoperability. These include; Patient
Identification, Health Information Exchange
Registries, Compliance, Management and
Communication of Medical Imaging Data, Health
Information Systems, Digitization of Health
Information, Security and Privacy for Data and
Training and capacity building Standards.
In the final phase, the standards were face-
validated through technical expert opinion selected
by ministry of health digital health technical working
group. Candidate standards were passed through the
process which helped to filter suitable standards for
possible adaption or contextualization for the
Ugandan health system. The process helped to
eliminate candidate standards that were not relevant
to the needs of the environment. Only standards that
survived this elimination stage were subsequently
considered for adaption/contextualization.
2.2 Study Population and Sample
Expert opinion was obtained from the 17 respondents.
The selection criteria for inclusion of the respondents
required that they had been actively involved in the
digital health sphere of Uganda for at least 5 years
and/or had participated in the stakeholder validation
workshop to understand the challenges of digital
health in Uganda. The stakeholder validation meeting
enabled respondents to have a background of the
derived requirements and validate them from an
informed perspective, with the respondents chosen to
represent the full spectrum of digital health
stakeholders in Uganda to increase the heterogeneity
of the study findings.
2.3 Data Collection
Data for both phases were collected using an
interviewer-administered questionnaire that was
subsequently adapted to requirement validation
techniques (Peddireddy & Nidamanuri, 2021). The
questionnaire included standards contextualization
development syntactic interoperability data standards
criteria. These were the syntactic interoperability data
standards development process, standards
implementation, M&E, and the interoperability data
standard determination process.
Respondents used a 5-point Likert scale of either
Yes (agreed) or No (disagreed) regarding the
suitability of the Syntactic Interoperability data
standards validated based on five evaluation metrics,
i.e., completeness, clarity, applicability, usefulness,
and efficacy. The rating statements used a scale of 1
to 5, where 1 = strongly agree, 2 = agree, 3 = neutral,
4 = disagree and 5 = strongly disagree (Altillo et al.,
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
268
2021; Dackus et al., 2012; Gupta et al., 2019;
Mbonane et al., 2023).
Regarding the requirements for syntactic
interoperability data standards development,
respondents selected either Yes, No, or Not
applicable to the proposed contextualized standards
well-specified.
2.4 Data Management and Analysis
The collected quantitative data was analyzed using
MS Excel. This included data on current challenges
in light of the various challenges to the
standardization of digital health in Uganda’s health
system (Alunyu et al., 2021; Kiwanuka et al., 2021).
We subsequently derived and validated
requirements to guide the development of the
syntactic interoperability data standards for Uganda.
These requirements were also informed by the
literature and success stories in other countries
(Ameller et al., 2012; Tun & Madanian, 2023) .
The interoperability data and the standards were
adapted and subsequently presented to Digital Health
stakeholders in Uganda for their consultation and
validation. The Ministry of Health Information ,
Innovation and Research Technical Working Group
(HIIRETWG) developed a validation tool/set of
criteria for validating the standards. Standards
validation and testing focused on completeness,
usability, applicability, and perceived usefulness.
This led to consensus building that resulted in the
approval of documented standards.
2.5 Ethics
The ethical clearance to conduct this research was
approved by both the Makerere University School of
Public Health Research ethics committee (REC) and
the Ministry of Health.
3 RESULTS
3.1 Characteristics of Respondents
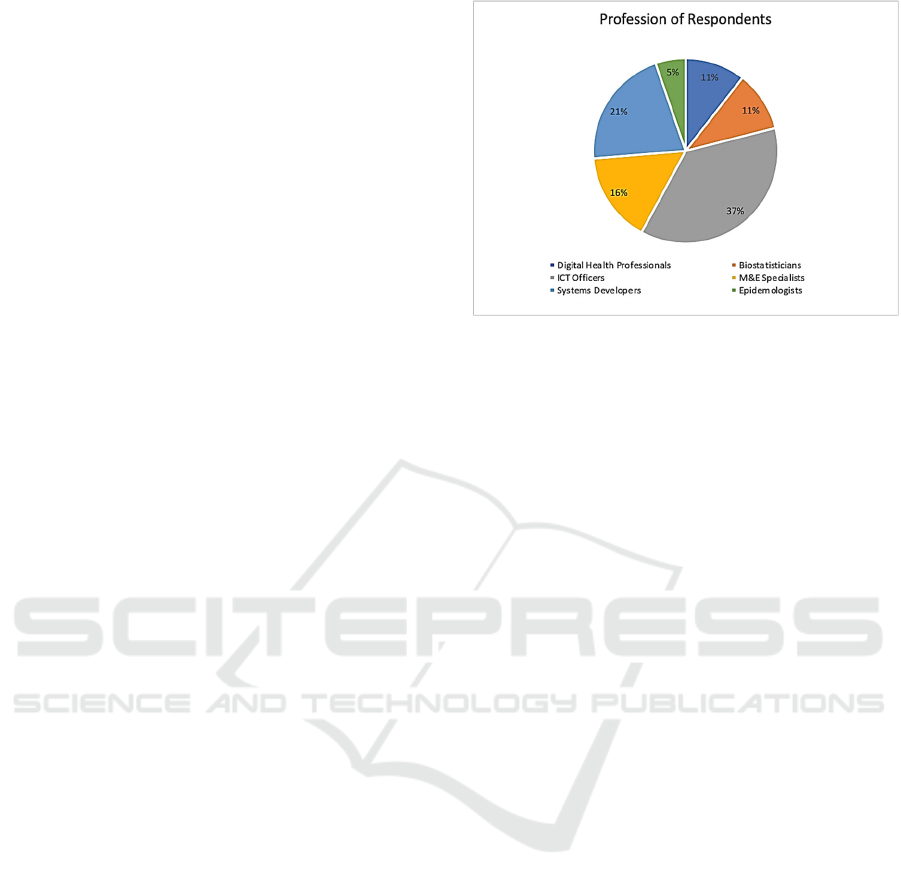
A total of 17 respondents were recruited giving a
response rate of 68% (n=17/25). Respondents
included, Digital Health professionals, ICT officers,
Systems Developers, Biostatisticians, Monitoring and
Evaluation specialists, and epidemiologists (Figure 1).
Figure 1: Distribution of respondents by category.
3.2 Challenges Facing Standardization
of Interoperability of Health Data
and Requirements for
Interoperability Data
Standardization
Table 1 contains details of the challenges facing the
standardization of Health Information Exchange in
Uganda based on Phase 1 of the research project.
Table 2 contains the derived and validated
requirements to guide the development of the
syntactic interoperability data standards for
Uganda
based on the identified challenges facing the
standardization of Health Information Exchange in
Uganda (Table 1).
3.3 Syntactic Interoperability Data
Standards
Table 3 contains details of the Syntactic
Interoperability data standards generated from the
designated requirements. These include data
exchange and sharing standards. The contextualized
syntactic interoperability data standards should be
applied to ensure that the patient (health) data
collected, information processed, shared, and stored
are in formats that support syntactic interoperability.
Contextualizing Syntactic Interoperability Data Standards for Health Information Exchange in Uganda’s Public Healthcare System
269

Table 1: Challenges facing standardization of Health Information Exchange.
Theme Sub-themes Challenge
Limited
guidelines for
standardization
Policy
development
Limited guidelines for collecting, storing, sharing, and exchanging electronic
patient data to inform decision-making and efficient service delivery.
Policy adoption Despite some health facilities implementing or having adopted electronic sharing
and exchange of patient data guidelines, the Ministry of Health is yet to officially
adopt them.
Inadequate
capacity
Monitor
compliance
There is an inadequate capacity to monitor compliance with Interoperability Data
Standards and or guidelines for data use and management across the Health sector
Interoperate
ima
g
es
Lack of reliable mechanism for managing health images information/data
collection, stora
g
e, and sharin
g
amon
g
health
p
roviders
Coordination Uncoordinated process guidelines for capturing paper-based patient records into
digital formats suitable for Electronic Medical Records (EMR), Electronic Health
R
ecords (EHR), and Personal health records (PHR).
Training Healthcare workers have inadequate training, and experience in data management
skills including; data collection, analysis, reporting, and use to inform the decision-
making process at different levels of the continuum of care.
Data safety Data privac
y
Data Security and Privacy Standards have not been officially adopted.
Security Health facilities do implement and/or use insufficient security and privacy
measures for electronic health data; which may compromise/put at risk the privacy
and con
f
identialit
y
o
f
p
atients’ data.
Table 2: Requirements for interoperability data standardization.
Theme Sub-theme Challen
g
e addresse
d
Interoperation
data
framework
Procedure Develop data interoperability standards/ SOPs/Guidelines for collecting, storing,
s
harin
g
, and exchan
g
in
g
electronic
p
atient data.
International
benchmarks
These should be based on the international standards for Health Information
Exchange (syntactic) - HL7, FHIR, DICOM, and the Uganda Data Protection and
Privacy Act, 2019.
An adoption mechanism should be put in place for data interoperability standards
f
or the electronic sharin
g
and exchan
g
e o
f
p
atient data across the health secto
r
Security The MoH should develop guidelines to support the core data security elements of
confidentiality, integrity, and availability across the health sector to roll out data
Interoperability Data Security Standards/guidelines for health information
mana
g
ement.
Images and media Develop Data Standards for Images, Multimedia, Waveform, and documents for
exchanging images across the continuum of patient care based on the international
standards for Health Image Information Exchange (DICOM), and the Uganda Data
Protection and Privacy
A
ct, 2019).
Migration of paper
data to electronic
forms
Formulate a strategy to migrate paper-based health records into electronic formats
to enhance data sharing and use.
Compliance
mechanism
Enforcement The MoH should enhance the compliance mechanism of all users to adhere to
Interoperability Data standards.
Privacy and
securit
y
Deploy security and privacy measures that protect the privacy and confidentiality
o
f
electronic
p
atient data at all levels.
Capacity
building
Monitor process MoH should build the capacity of data custodians and owners to monitor the
implementation and compliance of data management including data cleaning and
adherence to standards at all levels of the continuum of care.
Awareness /
Advocacy
The MoH should create data use and utilization awareness campaigns to monitor
compliance requirements and structures for health Information/data management.
The MoH should advocate for digital health courses including data analysis,
monitoring, and evaluation to be incorporated into health workers' training
curricula.
Access Data securit
y
g
uidelines should be well disseminated to all relevant stakeholders.
Capability The MoH should develop training guidelines for health workers on basic ICT Skills,
analysis, and data management
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
270
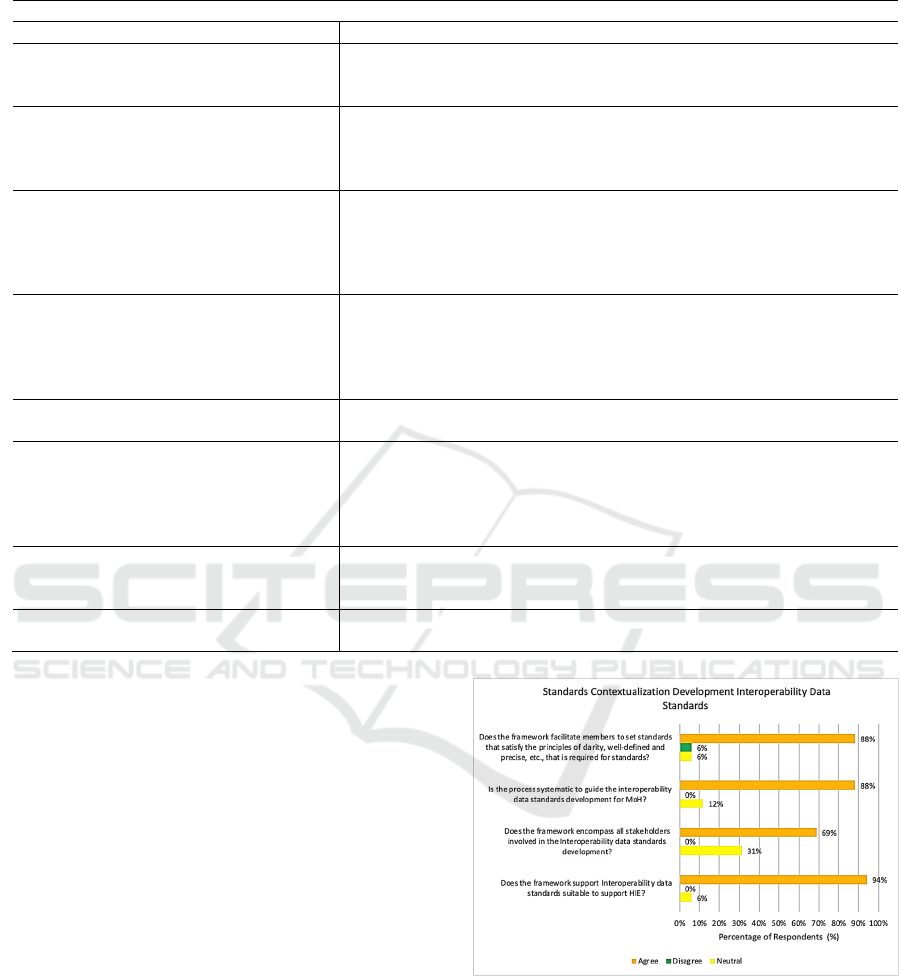
Table 3: Contextualized Syntactic Interoperability Data Standards.
S
y
ntactic Intero
p
erabilit
y
Data Standards
Standar
d
Statement
UG_DHS_DS01_P1: Patient
Identification
Establish a unique, standardized, comprehensive, and comprehensible
Electronic Medical Record (EMR), Electronic Health Records (EHR), and
Personal Health Record
(
PHR
)
UG_DHS_DS02. _ NHIE: Health
Information Exchange Registries Standard
Developing and maintaining comprehensive interoperable master lists of
health facilities, providers, and patients/clients is a necessary step toward
monitoring health infrastructure and services that form a core component
o
f
the National Health Mana
g
ement In
f
ormation S
y
stem
(
HMIS
)
.
UG_DHS_DS03. _CP: Compliance Establish an Intelligent and Integrated monitoring mechanism to ensure
compliance across the health sector. Generate data for observation and
clinically relevant events and encounters. This requires having a common
semantic and syntactic logical information model and structural
com
p
osition.
UG_DHS_DS4. -_MI: Management and
Communication of Medical Imaging Data
All health record management complies with the DCOM/ PACS Standards
in terms of imaging modalities including radiography, magnetic resonance
imaging (MRI), nuclear medicine, ultrasound, tomography,
echocardiography, X-ray, CT, and other modalities used in radiology,
cardiology, radiotherapy, ophthalmology, and dentistry.
UG_DHS_DS5_HIS: Health Information
S
y
stems Standard
Establish mechanisms for implementing and adhering to set guidelines for
all HIS solutions in the health secto
r
UG_DHS_DS6_DHI: Digitization of
Health Information Standard
Establish an ICT infrastructure that forms the foundations for electronic
communication and information/data sharing across geographical and
health-sector boundaries. This includes the computing infrastructure,
databases, directory services, network connectivity, and storage that
underpin a national eHealth environment.
UG_DHS_DS7_SP: Security and Privacy
for Data Standards
The Ministry of Health shall ensure adherence to the National Information
Security Policy and Strategy, the Uganda e-Government interoperability
f
ramework, and other relevant global standards.
UG_DHS_DS8_TCB: Training and
ca
p
acit
y
buildin
g
Standar
d
Build health workforce skills in data management and use through training,
mentorshi
p
, and coachin
g
.
3.4 Validation of Syntactic
Interoperability Data Standards
Figure 2 depicts respondents' views regarding the
standards contextualization development of Syntactic
Interoperability Data Standards. 94% of participants
agreed that the framework supports interoperability
data standards suitable to support HIE, 68% agreed
that the framework encompasses all stakeholders
involved in the syntactic interoperability data
standards development, and 88% agreed that the
framework facilitates members to set standards that
satisfy the principles of clarity, well-defined and
precise, that is required for standards. In addition, 88
% of the respondents agreed that development
process was systematic enough to guide the
interoperability data standards development for the
MoH. However, 31% of respondents were neutral on
whether the framework encompasses all stakeholders
involved in the Syntactic Interoperability data
standards development.
Figure 2: Validation of Syntactic Interoperability Data
Standards.
4 DISCUSSION
We believe this is the first study in Uganda to assess
the requirements and validate the syntactic
interoperability data standards for Uganda following
initial activities. Our study found that the main
Contextualizing Syntactic Interoperability Data Standards for Health Information Exchange in Uganda’s Public Healthcare System
271

requirements for standardization should be explicit
about data sharing and exchange across the four
domains, i.e., business, data, applications, security,
and technology, and users should extract, analyze,
and use them. The main challenges were limited
guidelines for the standardization process, inadequate
capacity, and data safety. Encouragingly, the level of
validation by expert opinion was high regarding the
proposed framework.
As far as we know, we believe this is also the first
study in a resource-limited country to validate the
interoperability data standard for healthy ecosystems.
The study identified that the key challenges to the
implementation of interoperability standards for
health in Uganda is the current heterogeneity of
health information systems, with the heterogeneity of
health information systems posing a significant
challenge to the implementation of interoperability
standards for health in the country. Current health
information systems in Uganda differ in terms of their
data structure, data format, data definitions, and data
exchange protocols. This heterogeneity makes it
difficult to establish a common language for sharing
and exchanging health information.
Over the years, Uganda similar to other LMICs
has seen a general transformation of the Health
Information System and specifically, a rapid growth
in eHealth solutions (Ndabarora & Chipps, 2014).
The recognition of ICT as having great potential to
improve the delivery of healthcare services, and
therefore an aid to the delivery of public health
services to Ugandans, has resulted in the development
and execution of many eHealth interventions that
have mainly stayed at the pilot stage commonly
known as the “Uganda eHealth Pilotitis Disease”. In
other words, these initiatives have not been successful
in further scaling and implementation across the
entire country due to several impediments in four key
categories: governance, financial and human
resources, standards, and infrastructure
availability(Huang et al., 2017). Worse still, these
interventions address individual health programs and
are largely parallel and/or uncoordinated centrally by
the Ministry of Health. This has hindered seamless
health data flow across both the public and private
sectors in Uganda coupled with stretched human
resource to support data collection, transformation,
presentation, and archiving, among others
(Ndabarora & Chipps, 2014).
To address this challenge, Uganda needs to invest
in standardizing its health information systems. This
will involve developing a common data model for
health information, adopting common data standards,
and implementing interoperability standards
including FHIR (Fast Healthcare Interoperability
Resources), HL7 (Health Level Seven International),
and DICOM (Digital Imaging and Communications
in Medicine). In this regard, investment is required in
terms of standards-compliant systems development
and implementation. Alongside this, considerable
effort is required in terms of change management to
achieve interoperability. The investment required by
early standards adopters at the leading edge of new
initiatives is typically significantly higher and the
benefits are slower to accrue than that required by
implementing standards-based systems that are
already widely in use. The late adopter benefits from
the investment and efforts of early adopters in terms
of time and money needed to ensure any failures and
barriers to success are dealt with. This means that
vendors and providers in particular may be hesitant to
bear the cost of progressing with the implementation
of interoperability standards until Government takes
the lead in advocating and implementing
interoperability data standards (Brailer &
Blumenthal, 2010a).
As mentioned, one of the key challenges to the
implementation of interoperability
standards for
health in Uganda is the current heterogeneity
of
health information systems, similar to other countries
(Katehakis & A Kouroubali, 2019). Most large
hospitals will use many different ICT systems from
different suppliers, each supporting different
functions. There is no single health information
system that could facilitate all administrative,
clinical, technical, and, laboratory ICT requirements
of a large healthcare organization. In such a
fragmented environment, the requirement to achieve
interoperability is critical and the need for
interoperability standards becomes evident (Brailer &
Blumenthal, 2010a; Jama, 2016; Perlin et al., 2016).
This needs to be borne in mind by all key stakeholders
in Uganda going forward.
Another approach to overcoming this challenge is
to use data integration platforms that can harmonize
data from different systems, and convert them into a
common format. These platforms can help facilitate
the exchange of health information between different
health information systems.
In addition, capacity building and training
programs can be implemented to improve the skills
and knowledge of health practitioners on health
information systems and interoperability standards.
This can help ensure that the health workforce in
Uganda is equipped with the necessary skills to
effectively use and exchange health information
across different systems as they seek to improve the
care of patients including access to and the use of
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
272

medicines (Kiggundu et al., 2022). Based on our
findings in the study, implementation initiatives were
generated to solve the problems of fragmented
implementations of eHealth systems, a lack of
integrated data sharing, and a lack of reliable, timely,
and lack of integrated access to patient data
(GÅRDSTEDT et al., 2013; Huang et al., 2017).
Similar to other LMICs, Uganda needs to adopt,
contextualize interoperability data standards to
facilitate health Information Exchange in the Uganda
health system.
The validated requirements should lead to the
development or contextualization of syntactic
interoperability data standards for data use and aid the
decision-making processes, and offer an efficient
continuum of care, as stipulated by the WHO (World
Health Organisation, 2012). In addition, most
respondents agreed on all the requirements indicating
the need to fast-track standardization activity in
Uganda's healthcare system as previously suggested
by Alunyu et al. (2021)(Alunyu et al., 2021). Whereas
a few respondents had concerns that some of the
requirements are over-ambitious, others pointed out
that some of the standards were too prescriptive.
These few concerns could be solved by producing
detailed guidelines on the implementation of the
standards. The Ministry of Health and its partners
should also take advantage of these initiatives that
have not been successful in other countries when
developing and integrating syntactic interoperability
data standards. These include addressing four key
areas namely: governance, financial and human
resources, standards, and infrastructure availability.
These interventions should holistically address all
health programs coordinated centrally by the Ministry
of Health. This will enable seamless health data to
flow in the future across both the public and private
sectors in Uganda along with the necessary human
resource to support data collection, transformation
and reporting.
Cultural changes within the health sector are also
required to ensure independent healthcare
organizations are willing to share health information
beyond the confines of
their systems. Standardization
removes an element of local autonomy for providers
and the perception may exist that independent control
of health information systems by providers is
compromised (Kim, 2005; World Health
Organization, 2013). The changes required in
processes and operations at the local level also act as
a barrier to implementation as providers and local
ICT professionals must be educated about new
processes and methods of recording health
information with the introduction of standardized
terminologies (Umberfield et al., 2023). This will
change with developments in health data flow in
Uganda in the future.
Overall, whilst the benefits of interoperability in
healthcare are considerable, they may be difficult to
realize as the benefits are dispersed across many
stakeholders including vendors, providers,
policymakers, and the individual. Some vendors use
a lack of interoperability to their advantage as a
customer retention strategy by building systems that
can only interoperate with their own products (Brailer
& Blumenthal, 2010a). This also needs to be
addressed.
5 CONCLUSION
In conclusion, while the majority of respondents have
endorsed the derived interoperability data standards
artifact, it's important to recognize that selection
criteria may evolve over time to accommodate
changing needs. The successful implementation of
the validated syntactic interoperability data standards
promises to enhance service delivery, improve patient
outcomes, and ensure equity and safety in healthcare.
However, numerous barriers and challenges must be
addressed, including the availability of skilled
personnel, motivation, and adequate resources.
Continuous monitoring of the situation is imperative.
Therefore, significant investment is warranted in
the development and implementation of standards-
compliant systems. Additionally, substantial effort is
needed in terms of change management to achieve
seamless interoperability. Early adopters of
standards-based systems typically incur higher
investment costs and experience slower benefits
compared to those implementing established
standards. Late adopters benefit from the groundwork
laid by early adopters, saving time and resources
required to overcome obstacles and failures.
Consequently, vendors and providers may hesitate to
invest in interoperability standards until government-
led advocacy and implementation efforts gain
momentum (Brailer & Blumenthal, 2010b).
Funding: There was no funding for this paper.
Conflicts of Interest: The authors declare there are no
conflicts of interest.
Contextualizing Syntactic Interoperability Data Standards for Health Information Exchange in Uganda’s Public Healthcare System
273

REFERENCES
Achampong, E., & Dzidonu, C. (2017). Methodological
Framework for Artefact Design and Development in
Design Science Research. Researchgate.Net.
https://www.researchgate.net/profile/Emmanuel-
Achampong/publication/329775397_Methodological_F
ramework_for_Artefact_Design_and_Development_in_
Design_Science_Research/links/5c1a2297458515a4c7e
906fd/Methodological-Framework-for-Artefact-Design-
and-Development-in-Design-Science-Research.pdf
Adeleke, I., & Lawal, A. (2015). Information technology
skills and training needs of health information
management professionals in Nigeria: a nationwide
study. Journals.Sagepub.Com. https://journals.sagepub.
com/doi/pdf/10.1177/183335831504400104
Altillo, B. S. A., Gray, M., Avashia, S. B., Norwood, A.,
Nelson, E. A., Johnston, C., Bhavnani, D., Patel, H.,
Allen, C. H., Adeni, S., Phelps, N. D., & Mercer, T.
(2021). Global health on the front lines: an innovative
medical student elective combining education and
service during the COVID-19 pandemic. BMC Medical
Education, 21(1). https://doi.org/10.1186/S12909-021-
02616-9
Alunyu, A. E., Wamema, J., Kiwanuka, A., Bagyendera, M.,
Amiyo, M., Kambugu, A., & Nabukenya, J. (2021).
Investigating the Impediments to Accessing Reliable,
Timely and Integrated Electronic Patient Data in
Healthcare Sites in Uganda. {HEALTHINF} 2021 - 14th
International Conference on Health Informatics; Part of
the 14th International Joint Conference on Biomedical
Engineering Systems and Technologies, {BIOSTEC}
2021, Vol. 5 HEALT…(Vol. 5 HEALTHINF, ISBN 978-
989-758-490-9, pages 522-532), 1–7. https://doi.org/
10.5220/0010266705220532
Ameller, D., Ayala, C., & Cabot, J. (2012). How do software
architects consider non-functional requirements: An
exploratory study. Ieeexplore.Ieee.Org. https://ieee
xplore.ieee.org/abstract/document/6345838/
Baskerville, R. ;, Baiyere, A. ;, Gregor, S. ;, Hevner, A. ;, &
Rossi, M. (2018). Design science research contributions:
Finding a balance between artifact and theory.
Aisel.Aisnet.OrgR Baskerville, A Baiyere, S Gregor, A
Hevner, M RossiJournal of the Association for
Information Systems, 2018•aisel.Aisnet.Org, 19(5), 358–
376. https://doi.org/10.17705/1jais.00495
Brailer, D. J., & Blumenthal, D. (2010a). Guiding the health
information technology agenda. Interviewed by David J.
Brailer. Health Affairs (Project Hope), 29(4), 586–595.
https://doi.org/10.1377/HLTHAFF.2010.0274
Brailer, D. J., & Blumenthal, D. (2010b). Interview: Guiding
the health information technology agenda. Health
Affairs, 29(4), 586–595. https://doi.org/10.1377/HLTH
AFF.2010.0274
Dackus, G. H., Loffeld, S. M., & Loffeld, R. J. (2012). Use
of acid suppressive therapy more than 10 years after the
endoscopic diagnosis of reflux esophagitis with specific
emphasis to trademark and generic proton pump
inhibitors. Journal of Gastroenterology and Hepatology
(Australia), 27(2), 368–371. https://doi.org/10.1111/
J.1440-1746.2011.06855.X
GÅRDSTEDT, J., JULIN, N., & TÖRNQVIST, J. (2013). A
study of the preconditions for asustainable
implementation of a digitalhealth system in Uganda.
https://www.diva-
portal.org/smash/get/diva2:677241/FULLTEXT01.pdf
Gupta, M., Vohra, C., & and, P. R. (2019). Assessment of
knowledge, attitudes, and practices about antibiotic
resistance among medical students in India.
Ncbi.Nlm.Nih.Gov. https://www.ncbi.nlm.nih.gov/pmc/
articles/PMC6820394/
Huang, F., Blaschke, S., & Lucas, H. (2017a). Beyond
pilotitis: taking digital health interventions to the national
level in China and Uganda. Globalizationandhealth ….
https://globalizationandhealth.biomedcentral.com/article
s/10.1186/s12992-017-0275-z
Huang, F., Blaschke, S., & Lucas, H. (2017b). Beyond
pilotitis: Taking digital health interventions to the
national level in China and Uganda. Globalization and
Health, 13(1). https://doi.org/10.1186/S12992-017-
0275-Z
Ishijima, H., Mapunda, M., Mndeme, M., Sukums, F., &
Mlay, V. S. (2015). Challenges and opportunities for
effective adoption of HRH information systems in
developing countries: National rollout of HRHIS and
TIIS in Tanzania. Human Resources for Health, 13(1).
https://doi.org/10.1186/S12960-015-0043-1
Jama, J. P.-. (2016). Health information technology
interoperability and use for better care and evidence.
Jamanetwork.Com. https://jamanetwork.com/journals/ja
ma/article-abstract/2556001
Jawhari, B., Keenan, L., Zakus, D., & Ludwick, D. (2016).
Barriers and facilitators to Electronic Medical Record
(EMR) use in an urban slum. Elsevier. https://www.
sciencedirect.com/science/article/pii/S13865056163017
69
Katehakis, D., & A Kouroubali, A. (2019). A Framework for
the Consistent Management of eHealth Interoperability
in Greece. Pdfs.Semanticscholar.Org. https://doi.org/
10.5220/0007796906890695
Kiberu, V., Mars, M., Care, R. S.-A. J. of P. H., & 2017,
undefined. (2017). Barriers and opportunities to
implementation of sustainable e-Health programmes in
Uganda: A literature review. Journals.Co.ZaVM Kiberu,
M Mars, RE ScottAfrican Journal of Primary Health
Care and Family Medicine, 2017•journals.Co.Za, 9(1).
https://doi.org/10.4102/phcfm.v9i1.1277
Kiggundu, R., Wittenauer, R., Waswa, J. P., Nakambale, H.
N., Kitutu, F. E., Murungi, M., Okuna, N., Morries, S.,
Lieberman Lawry, L., Joshi, M. P., Stergachis, A., &
Konduri, N. (2022). Point prevalence survey of antibiotic
use across 13 hospitals in Uganda. Mdpi.Com, 11.
https://doi.org/10.3390/antibiotics11020199
Kim, K. (2005). Clinical data standards in health care: five
case studies. https://www.policyarchive.org/handle/
10207/7072
Kiwanuka, A., Bagyendera, M., Wamema, J., Egwar, A. A.,
Alunyu, A., Amiyo, M., Kambugu, A., & Nabukenya, J.
(2021). Establishing the state of practice about data
ICT4AWE 2024 - 10th International Conference on Information and Communication Technologies for Ageing Well and e-Health
274

standards in monitoring healthcare interventions for HIV
in Uganda’s EMR-based health information systems.
https://doi.org/10.5220/0010264302000211
Kiwanuka, A., & Nabukenya, J. (2023). Requirements for
Implementing Digital Health Terminology Standards in
Uganda’s Electronic Medical Records-Based Health
Information Systems. Springer. https://link.springer.
com/chapter/10.1007/978-3-031-20664-1_11
Lin, C., Lin, I., Roan, J., systems, J. Y.-J. of medical, & 2012,
undefined. (2010). Critical factors influencing hospitals’
adoption of HL7 version 2 standards: An empirical
investigation. SpringerCH Lin, IC Lin, JS Roan, JS
YehJournal of Medical Systems, 2012•Springer, 36(3),
1183–1192. https://doi.org/10.1007/s10916-010-9580-2
Matovu, J., & Ngo’ng’ Ocholla, D. (2009). Aspects of the
status of management information systems and the
information needs for public administration in Uganda.
https://doi.org/10.1515/libr.2009.018
Mbonane, H., Sibanda, M., & Godman, B. (2023).
Knowledge, attitudes and practices of healthcare
professionals on the use of an electronic stock visibility
and management tool in a middle-income country.
Elsevier. https://www.sciencedirect.com/science/article/
pii/S2667276623000148
Ndabarora, E., & Chipps, J. (2014). Systematic review of
health data quality management and best practices at
community and district levels in LMIC.
Journals.Sagepub.Com. https://journals.sagepub.com/
doi/pdf/10.1177/0266666913477430
Okungu, V., Marshal, M., Health, M. J.-I. J. of, & 2019,
undefined. (2019). Sustainability, equity and
effectiveness in public financing for health in Uganda: an
assessment of maternal and child health services.
Dergipark.Org.TrV Okungu, M Marshal, M
JanineInternational Journal of Health Services Research
and Policy, 2019•dergipark.Org.Tr, 4(3), 233–246.
https://doi.org/10.23884/ijhsrp.2019.4.3.08
Peddireddy, S., & Nidamanuri, S. (2021). Requirements
Validation Techniques: Factors Influencing them.
https://www.diva-portal.org/smash/record.jsf?pid=diva
2:1533905
Peffers, K., Tuunanen, T., Rothenberger, M. A., &
Chatterjee, S. (2007). A design science research
methodology for information systems research. Journal
of Management Information Systems, 24(3), 45–77.
https://doi.org/10.2753/MIS0742-1222240302
Perlin, J., Baker, D., & Brailer, D. (2016). Information
technology interoperability and use for better care and
evidence: a vital direction for health and health care.
Nam.Edu. https://nam.edu/information-technology-
interoperability-and-use-for-better-care-and-evidence-a-
vital-direction-for-health-and-health-care/
Pisana, A., Wettermark, B., Kurdi, A., Tubic, B., Pontes, C.,
Zara, C., Van Ganse, E., Petrova, G., Mardare, I., Fürst,
J., Roig-Izquierdo, M., Melien, O., Bonanno, P. V.,
Banzi, R., Marković-Peković, V., Mitkova, Z., &
Godman, B. (2022). Challenges and Opportunities With
Routinely Collected Data on the Utilization of Cancer
Medicines. Perspectives From Health Authority
Personnel Across 18 European Countries. Frontiers in
Pharmacology, 13. https://doi.org/10.3389/FPHAR.20
22.873556/FULL
Shah, T., Applications, S. P.-I. J. of C., & 2014, undefined.
(2014). A review of requirement engineering issues and
challenges in various software development methods.
Researchgate.NetT Shah, SV PatelInternational Journal
of Computer Applications, 2014•researchgate.Net,
99(15), 975–8887. https://doi.org/10.5120/17451-8370
Tun, S. Y. Y., & Madanian, S. (2023). Clinical information
system (CIS) implementation in developing countries:
requirements, success factors, and recommendations.
Journal of the American Medical Informatics
Association. https://doi.org/10.1093/JAMIA/OCAD011
Umberfield, E. E., Staes, C. J., Morgan, T. P., Grout, R. W.,
Mamlin, B. W., & Dixon, B. E. (2023). Syntactic
interoperability and the role of syntactic standards in
health information exchange. In Health Information
Exchange (pp. 217–236). Elsevier. https://doi.org/
10.1016/B978-0-323-90802-3.00004-6
Verbeke, F., Karara, G., & Nyssen, M. (2015). Human
factors predicting failure and success in hospital
information system implementations in sub-Saharan
Africa. Ebooks.Iospress.Nl, 216, 482–486.
https://doi.org/10.3233/978-1-61499-564-7-482
Wamema, J., Alunyu, A., Amiyo, M., & Nabukenya, J.
(2023). Enterprise architecture requirements for
standardising digital health in Uganda’s health system.
Health Policy and Technology, 12(4), 100805.
https://doi.org/10.1016/J.HLPT.2023.100805
World Health Organisation. (2012). National eHealth
Strategy Toolkit. www.who.int
World Health Organization. (2013). eHealth standardization
and interoperability. EB132.R8. https://doi.org/10.5
World Health Organization. (2020). Global Strategy on
Digital Health 2020-2024.
World Health Organization. (2021). Global strategy on
digital health 2020-2025. http://apps.who.int/book
orders.
Contextualizing Syntactic Interoperability Data Standards for Health Information Exchange in Uganda’s Public Healthcare System
275
