
Development of a Real-Time Adaptable Virtual Reality-Scenario
Training for Anaesthesiology Education, a User-Centered Design
Krista Hoek
1a
, Christina Jaschinski
2
b
, Monique van Velzen
1c
and Elise Sarton
1d
1
Department of Anaesthesiology, LUMC, Albinusdreef 2, 2333ZA, Leiden, The Netherlands
2
Saxion University of Applied Sciences, M. H. Tromplaan 28, 7513AB, Enschede, The Netherlands
Keywords: VR-Simulation, Immersive Learning, Immersive VR, Proteus Effect, Medical Education, Crisis Resource
Management, User-Centered Design.
Abstract: Simulation training in medical settings has become pivotal in clinical education. Virtual reality (VR) presents
a novel approach to simulation, offering numerous advantages for both trainers and trainees by facilitating
high-fidelity practice in situational awareness, decision-making, and multitiered response systems within a
safe yet stressful environment. This paper outlines the development of a multiplayer VR simulation prototype
tailored for anaesthesiologist-intensivists, with input from a multidisciplinary expert team throughout the
process. Trainers can dynamically adjust patient physiological parameters, enabling training in crisis resource
management under pressure. Following a user-centered design (UCD) methodology, iterative design cycles
involve experts adapting a Failure Modes and Effects Analysis (FMEA) to prioritize trainee and trainer needs.
User feedback, gathered through various qualitative and quantitative UCD techniques such as interviews,
focus groups, and prototype testing, informs each iteration. Three simulation prototype versions underwent
evaluation, incorporating simulation settings, debriefing sessions, and FMEA analysis. Feedback informed
iterative design improvements until thematic saturation was reached, culminating in the creation of an initial
prototype. This paper aims to detail the development process of a VR scenario training program, geared
towards immersive simulation learning.
1 INTRODUCTION
One of the cornerstones of medical training is clinical
scenario training using an environment to learn
effectively (Anthony, 1996; Yunoki & Sakai, 2018).
Simulation based learning provides a safe learning
space where healthcare providers can gain experience
on medical emergencies or rare complications in a
controlled setting without putting real patients at risk.
Especially for anaesthesiologists/ intensivists,
management of a patient who is acutely deteriorating
requires excellent technical and non-technical skills
in a highly stressful and chaotic environment.
Technical skills may include tracheal intubation,
difficult airway management, vascular catheter
placement and regional anaesthesia. Also, sufficient
medical knowledge of differential diagnoses, drug
a
https://orcid.org/0000-0003-1984-3182
b
https://orcid.org/0000-0002-7940-7684
c
https://orcid.org/0000-0002-0289-6432
d
https://orcid.org/0009-0007-4403-3815
dosages, triages of possible actions, and crisis
resource management are crucial and may be
lifesaving. Situation awareness, decision making,
teamwork, communication and leadership are
indispensable skills in clinical practice outlining the
importance of human factors (Institute of Medicine
Committee on Quality of Health Care in, 2000).
Improvement in patient outcome may come from
multitiered rapid response systems.
Knowledge is constructed in social contexts and
students need to be active learners rather than passive
recipients of knowledge (Anthony, 1996). Although
several studies have shown the effectiveness of
simulation-based training over the last decade
(Dorozhkin et al., 2017), increasing pressure son
budget and logistic limitations, needs for alternative
methods of simulation have emerged. Also, current
simulation programs may not have scenarios with
Hoek, K., Jaschinski, C., van Velzen, M. and Sarton, E.
Development of a Real-Time Adaptable Virtual Reality-Scenario Training for Anaesthesiology Education, a User-Centered Design.
DOI: 10.5220/0012755600003693
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 16th International Conference on Computer Supported Education (CSEDU 2024) - Volume 1, pages 751-757
ISBN: 978-989-758-697-2; ISSN: 2184-5026
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
751

real-time adaptation possibilities which are seemed to
be required in order to create an immersive
environment with unlimited training possibilities for
personalization of the scenario (Bracq et al., 2019;
Tursø-Finnich et al., 2023; Yunoki & Sakai, 2018).
Immersive Virtual Reality uses a Head-Mounted-
Display (HMD) project in front of the eyes allowing
users to focus on display without interaction of the
outside world. It offers novel capabilities providing
new qualitative support for educators and trainees as
it can be used independent of geography, time and
space, and it is cost-effective (Pottle, 2019).
Immersive VR can produce a visceral feeling of being
in a simulated world, a form of spatial immersion
called Presence (Fuhrt, 2008; Pottle, 2019)Also, in
virtual interactions, participant’s avatars can affect
their attitude, perception and behaviour in a conscious
or unconscious matter known as the Protheus Effect
(Bian et al., 2015; Navarro et al., 2022). However,
there are also potential drawbacks such as limited
haptic (tactile) feedback (Ruthenbeck & Reynolds,
2015) and the absence of non-verbal cues in the
trainees’ digital avatars (Pottle, 2019).
The main objective of this study is to develop a
prototype of a VR-scenario training program for
anaesthesiologists-intensivists. The VR-scenario
training program is tailored to the needs and
experience of the trainees and simulation trainers with
a multidisciplinary expert team involved throughout
the development process and guide all design
decisions. This paper will describe the development
phase of our prototype.
2 METHODS
2.1 Study Design
We’ve adapted a user centered design as it employs
scientifically proven methodologies of human
sciences to optimize designs of human-technology
interface improving its proficiency and performance
and is easy to use (Walden et al., 2020).
During the development phase, three simulation
prototype iterations were made, each evaluated with
a simulation setting, debriefing and Failure Modes
and Effects Analysis (FMEA) (Davis et al., 2008).
After every simulation, feedback was provided to the
development team responsible for the VR
environment. This feedback loop encompassed
evaluation of the simulation setting, debriefing
sessions, and analysis through FMEA. The VR
developers then utilized this feedback to iteratively
enhance the VR simulation. Subsequently, design
iterations were made, and the modified prototype
underwent testing and adaptation until thematic
saturation was achieved. We adapted FMEA as it
identifies possible system failures and vulnerabilities
in complex processes to make a system more robust
before an adverse event or problem occurs (Davis et
al., 2008). It is a method to identify parts of the
process most in the need of change. A
multidisciplinary expert team for the FMEA process
was selected including 5 steps: (1) team selection, (2)
process identification, (3) process flow diagram
preparation, (4) failure mode identification, and (5)
determination of an action plan.
For the evaluation phase which is beyond the
scope of this article, we will assess content validity
through qualitative and quantitative measures in an
exploratory sequential design.
2.2 Participants and Setting
The protocol was approved by the Institutional
Science Committee of the Anaesthesiology science
department and obtained a waiver from the
Institutional Review Board (NWMO-LUMC).
Informed consent was obtained prior to inclusion,
participation was voluntary and privacy rights were in
alignment with the Declaration of Helsinki and
GDPR guidelines. The multidisciplinary expert team
for the FMEA process was designed to include
anaesthesiologists-intensivists, trainers, human factor
specialists and software VR design technical experts.
Participation was voluntary. Exclusion criteria
included physical incapacity to use VR which was not
encountered during the study. Participants did not
receive a financial compensation.
2.3 Sample Characteristics
Three healthcare providers participated of whom one
the project manager. Two were anaesthesiologists-
intensivists, one was a resident. Together with two
developers and one experienced researcher they
assembled as the multidisciplinary expert team for the
FMEA process.
2.4 Conceptual Framework
Commonly, simulation consists of three components:
an initial briefing with explanation of the upcoming
scenario, the simulation experience and a debriefing
where learners are provided with a crucially
important opportunity to reflect on themselves and
their team in order to improve future practice
(Pacheco Granda & Salik, 2023).
ERSeGEL 2024 - Workshop on Extended Reality and Serious Games for Education and Learning
752
Today’s VR simulation programs often use preset
scenarios put into practice (Bracq et al., 2019;
Brammer et al., 2022; Macnamara et al., 2021).
Standardized patients (SPs) or standardized scenarios
have been utilized for procedural skills assessment
and non-technical skills development.
According to the principles of Cognitive Load
Theory (CLT) (Reedy, 2015), there is a limit on how
much information one can process simultaneously,
impacting the information storage and retrieval. A
trainer may not know beforehand how the trainees
will perform during the scenario; hence he/she may
not know beforehand how they want the scenario to
evolve. This outlines the importance of the
adaptability of a scenario, enabling a more effective
and valuable learning experience.
We’ve hypothesized our real-time adaptable VR-
training program could fill in this gap as we wanted
to create a program where a trainer could change the
scenario in real-time.
2.5 Data Collection and Analysis
User feedback was collected through various
qualitative and quantitative UCD techniques
including contextual inquiry, interviews, focus
groups, observations, questionnaires, walk-throughs
and prototype testing.
3 RESULTS
Three simulation prototypes underwent evaluation by
the multidisciplinary expert team encompassing
FMEA sessions. An example of a FMEA session can
be found in Table 1.
3.1 VR-Simulation Requirements
The VR- simulation was designed to be a fully
immersive reality system, with auditory, visual, and
tactile feedback, in real time adaptable by the trainer.
This implies scenario’s to be adaptable online, during
the simulation. Patients’ clinical presentation (skin
color and rash, pupil dilation etc.), and paraclinical
presentation (arterial tension, pulse oximetry,
bispectral index measurements etc.) were available on
the trainer’s dashboard enabling a fully adaptable
simulation training.
With an initial analytic phase of the UCD design,
the multidisciplinary expert team produced a list of
basic requirements divided in five major themes as
shown in Table 2. The use of the MoSCoW
prioritisation technique further classified these
requirements (Miranda, 2022).
Table 1: Failure mode simulation session two.
Concern
Severity
category
Potential
Active
Failure
Action plan
Latency Perfor-
mance
impact
Participant
experience
Potential
Active
Failure
Purchase
powerful
server.
Bumping
into each
other
Perfor-
mance
impact
Dizziness IT
adaptations
within the
VR.
Telepor-
tation
Participant
experience
Failure to
immerse
Testing of
different
standalone
HMD with
limited
s
p
ace.
Onboard-
ing
Perfor-
mance
impact
Physical Use of
standalone
HMD
without
teleportation
o
p
tion,
Onboading Participant
safety
Failure to
immerse
Virtual
onboard area
with tutorial
Table 2: Basic requirements.
Visuals patients
Patient morphology, age sex
Anatomic details (facial hair,
neck size, chin size, intra-oral
anatom
y)
Visuals avatars Automated avatars
Hand and e
y
e movement
Visuals surgery Laparoscopy
Laparotom
y
Equipment OR OR table
OR lights
Respiratory machine
Anesthesiologic equipment
Surgical equipment
Multi
p
la
y
e
r
1-5
p
la
y
ers
Trainer dashboard Adaptability of medical
conditioning
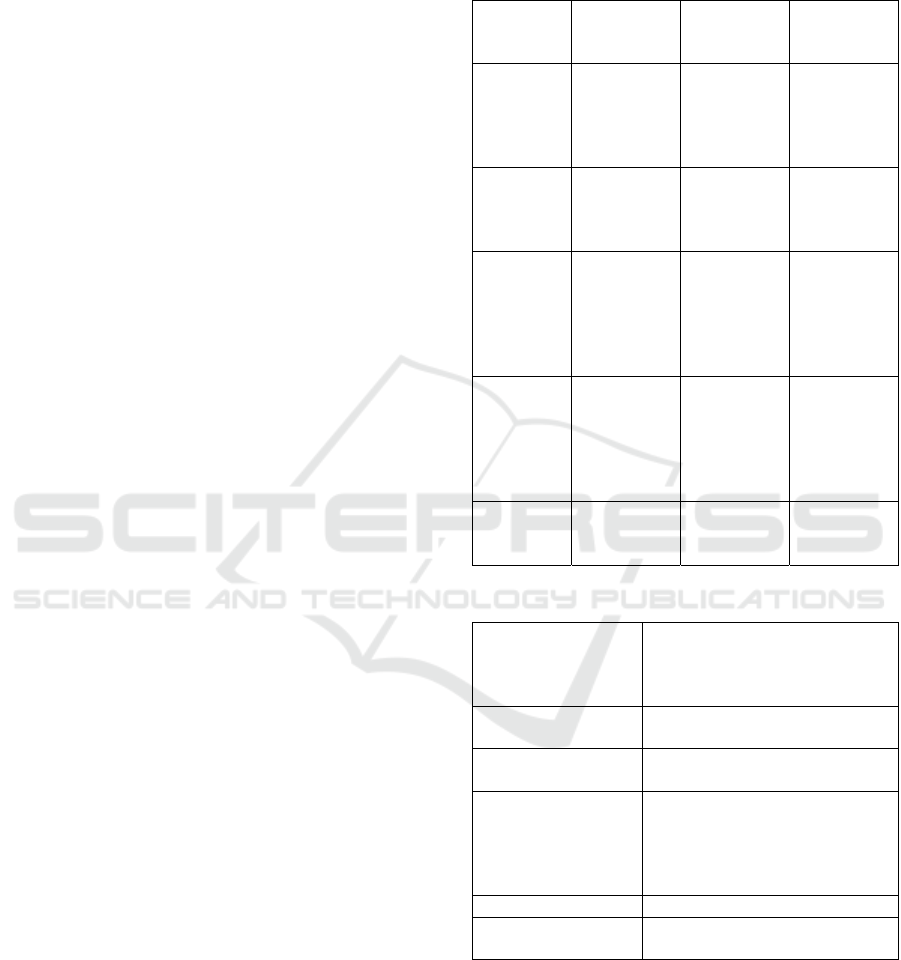
The static requirements consisted of materials
including airway devices, medication, and infusion
equipment, as well as operating room equipment such
as the operating table, lighting, and anaesthesiologic
and surgical instruments used for procedures such as
laparoscopy and laparotomy as shown in Figure 1.
Development of a Real-Time Adaptable Virtual Reality-Scenario Training for Anaesthesiology Education, a User-Centered Design
753
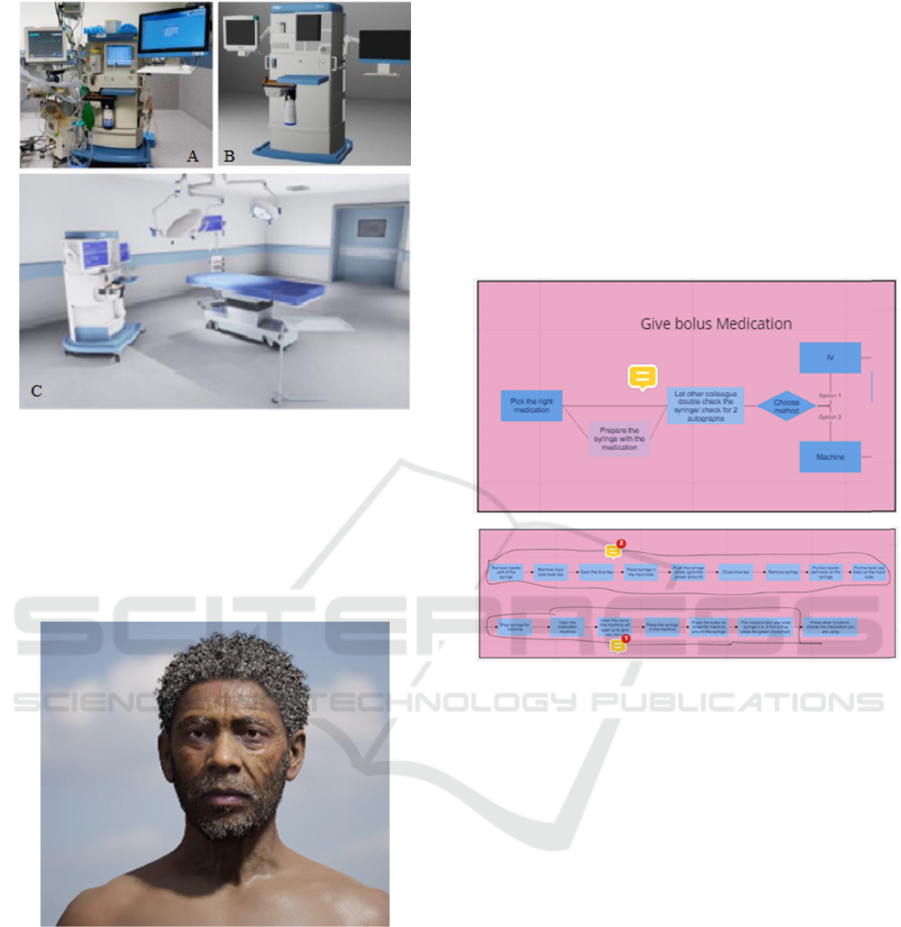
Figure 1: View of a photo (A), the digital design (B), and
the incorporation in the virtual OR environment (C).
Requirements of the visuals of the patients were
morphological features as shown in Figure 2.
Anatomic details such as facial hair, neck size, chin
size, intra-oral anatomy needed to be well designed to
enhance a high level of fidelity.
Figure 2: View of a patient with high resolution facial
details.
Furthermore, dynamic requirements
encompassed procedures such as intubation, both
standard and alternative techniques, and the
placement of intracorporal catheters such as an
intravenous line, intra-arterial catheter, stomach
siphon, or central venous catheter.
Additional dynamic requirements included
patient positioning, administration intravenous (IV)
medication, and other related considerations. An
extensive overview of these items can be found in the
Appendix.
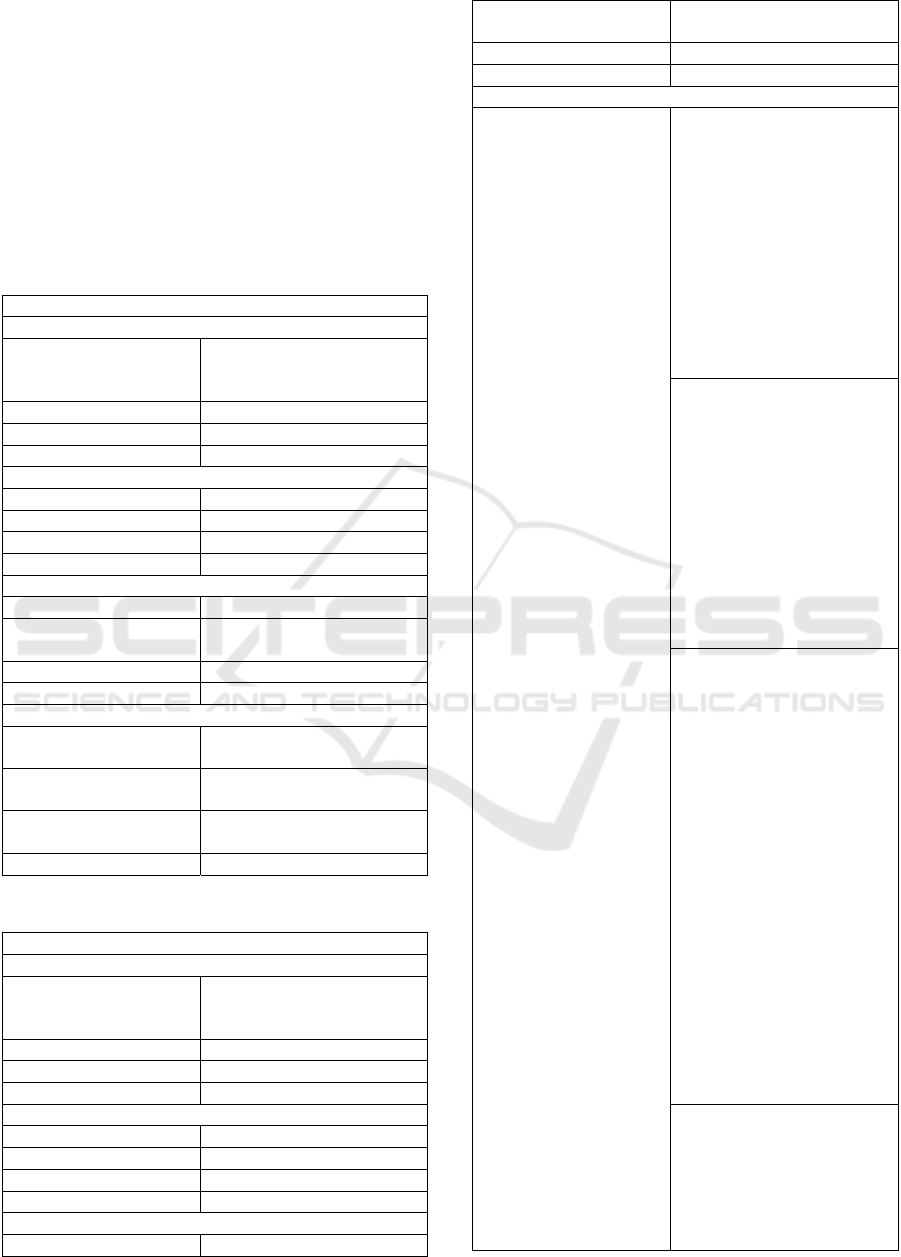
3.2 VR-Simulation Requirements
The multidisciplinary expert team employed a
collaborative approach to construct flow diagrams to
depict dynamic interactions of which an example is
depicted in Figure 3. This iterative process involved
the utilization of various media, such as videos
captured in the operating room, detailed descriptions,
and photographs, among others, to facilitate
communication between the different parties
involved.
Figure 3: View flow diagram of a bolus gift medication.
4 DISCUSSION AND
CONCLUSION
This paper provides useful information on the
development of a prototype of VR-scenario training
program with the potency of experimental learning
with VR. It may contribute to further research and
healthcare educational programs avid to use
immersive simulation learning with VR. A real-time
adaptable program may fully optimize learning
processes and adds flexibility within the scenario’s.
Future research on the prototype, employing UCD
techniques, is crucial to further validate its
effectiveness through iterative cycles of evaluation,
utilizing Kirkpatrick's evaluation model (Cannon-
Bowers, 2008; Falletta, 1998; Smidt et al., 2009).
This evaluation model assesses the prototype's
potential impact on four levels: (a) participants'
reaction to the training, (b) participants' learning
outcomes from the training, (c) participants'
behavioral changes resulting from the training, and
ERSeGEL 2024 - Workshop on Extended Reality and Serious Games for Education and Learning
754

(d) the subsequent organizational impact stemming
from participants' changed behavior. Additionally, it
also considers (e) the economic benefits or overall
human welfare derived from the training (Cannon-
Bowers, 2008; Falletta, 1998; Smidt et al., 2009).
ACKNOWLEDGEMENT
This work was supported by the Tech For Future,
Centre of Expertise on research in High Tech Systems
and Materials.
REFERENCES
Anthony, G. (1996). Active Learning in a Constructivist
Framework. Educational Studies in Mathematics,
31(4), 349-369. http://www.jstor.org/stable/3482969
Bian, Y., Zhou, C., Tian, Y., Wang, P., & Gao, F. (2015).
The Proteus Effect: Influence of Avatar Appearance on
Social Interaction in Virtual Environments. HCI,
Bracq, M. S., Michinov, E., Arnaldi, B., Caillaud, B.,
Gibaud, B., Gouranton, V., & Jannin, P. (2019).
Learning procedural skills with a virtual reality
simulator: An acceptability study. Nurse Educ Today,
79, 153-160.
https://doi.org/10.1016/j.nedt.2019.05.026
Brammer, S. V., Regan, S. L., Collins, C. M., & Gillespie, G.
L. (2022). Developing Innovative Virtual Reality
Simulations to Increase Health Care Providers'
Understanding of Social Determinants of Health. Journal
of Continuing Education in the Health Professions,
42(1). https://journals.lww.com/jcehp/Fulltext/2022/
04210/Developing_Innovative_Virtual_Reality_Simulat
ions.11.aspx
Cannon-Bowers, J. A. (2008). Recent advances in scenario-
based training for medical education. Curr Opin
Anaesthesiol, 21(6), 784-789.
https://doi.org/10.1097/ACO.0b013e3283184435
Davis, S., Riley, W., Gurses, A. P., Miller, K., & Hansen, H.
(2008). Failure Modes and Effects Analysis Based on In
Situ Simulations: A Methodology to Improve
Understanding of Risks and Failures. In K. Henriksen, J.
B. Battles, M. A. Keyes, & M. L. Grady (Eds.), Advances
in Patient Safety: New Directions and Alternative
Approaches (Vol. 3: Performance and Tools).
https://www.ncbi.nlm.nih.gov/pubmed/21249922
Dorozhkin, D., Olasky, J., Jones, D. B., Schwaitzberg, S.
D., Jones, S. B., Cao, C. G. L., Molina, M., Henriques,
S., Wang, J., Flinn, J., & De, S. (2017). OR fire virtual
training simulator: design and face validity. Surg
Endosc, 31(9), 3527-3533.
https://doi.org/10.1007/s00464-016-5379-7
Falletta, S. V. (1998). Evaluating Training Programs: The
Four Levels: Donald L. Kirkpatrick, Berrett-Koehler
Publishers, San Francisco, CA, 1996, 229 pp. The
American Journal of Evaluation, 19(2), 259-261.
https://doi.org/https://doi.org/10.1016/S1098-
2140(99)80206-9
Fuhrt. (2008). Immersive Virtual Reality. In B. Furht (Ed.),
Encyclopedia of Multimedia (pp. 345-346). Springer
US. https://doi.org/10.1007/978-0-387-78414-4_85
Institute of Medicine Committee on Quality of Health Care
in, A. (2000). In L. T. Kohn, J. M. Corrigan, & M. S.
Donaldson (Eds.), To Err is Human: Building a Safer
Health System. National Academies Press (US)
Copyright 2000 by the National Academy of Sciences.
All rights reserved. https://doi.org/10.17226/9728
Macnamara, A. F., Bird, K., Rigby, A., Sathyapalan, T., &
Hepburn, D. (2021). High-fidelity simulation and
virtual reality: an evaluation of medical students'
experiences. BMJ Simul Technol Enhanc Learn, 7(6),
528-535. https://doi.org/10.1136/bmjstel-2020-000625
Miranda, E. (2022, 2022//). Moscow Rules: A Quantitative
Exposé. Agile Processes in Software Engineering and
Extreme Programming, Cham.
Navarro, J., Peña, J., Cebolla, A., & Baños, R. (2022). Can
Avatar Appearance Influence Physical Activity? User-
Avatar Similarity and Proteus Effects on Cardiac
Frequency and Step Counts. Health Commun, 37(2),
222-229. https://doi.org/10.1080/10410236.2020.
1834194
Pacheco Granda, F. A., & Salik, I. (2023). Simulation
Training and Skill Assessment in Critical Care. In
StatPearls. StatPearls Publishing Copyright © 2023,
StatPearls Publishing LLC.
Pottle, J. (2019). Virtual reality and the transformation of
medical education. Future Healthc J, 6(3), 181-185.
https://doi.org/10.7861/fhj.2019-0036
Reedy, G. B. (2015). Using Cognitive Load Theory to Inform
Simulation Design and Practice. Clinical Simulation in
Nursing, 11(8), 355-360. https://doi.org/https://doi.org/
10.1016/j.ecns.2015.05.004
Ruthenbeck, G. S., & Reynolds, K. J. (2015). Virtual reality
for medical training: the state-of-the-art. Journal of
Simulation, 9(1), 16-26.
https://doi.org/10.1057/jos.2014.14
Smidt, A., Balandin, S., Sigafoos, J., & Reed, V. A. (2009).
The Kirkpatrick model: A useful tool for evaluating
training outcomes. J Intellect Dev Disabil, 34(3), 266-
274. https://doi.org/10.1080/13668250903093125
Tursø-Finnich, T., Jensen, R. O., Jensen, L. X., Konge, L.,
& Thinggaard, E. (2023). Virtual Reality Head-
Mounted Displays in Medical Education: A Systematic
Review. Simulation in Healthcare, 18(1), 42-50.
https://doi.org/10.1097/sih.0000000000000636
Walden, A., Garvin, L., Smerek, M., & Johnson, C. (2020).
User-centered design principles in the development of
clinical research tools. Clin Trials, 17(6), 703-711.
https://doi.org/10.1177/1740774520946314
Yunoki, K., & Sakai, T. (2018). The role of simulation
training in anesthesiology resident education. J Anesth,
32(3), 425-433. https://doi.org/10.1007/s00540-018-
2483-y
Development of a Real-Time Adaptable Virtual Reality-Scenario Training for Anaesthesiology Education, a User-Centered Design
755
APPENDIX
This appendix gives an extensive overview of the
static and dynamic requirements of the VR
simulation.
The requirements are annotated with the of the
MoSCoW prioritisation.
Static requirements included anaesthesia supplies,
airway supplies, operating room supplies, surgical
procedures.
Table 3.
STATIC
Anaesthesia su
pp
lies
Must
Intravenous infusion (IV) sets
in pink, green, blue, yellow,
and oran
g
e
Shoul
d
Subcutaneous needle
Coul
d
Tape
Will not have Intravenous deep cathete
r
Airway supplies
Must Size 6 oro
p
har
y
n
g
eal tube
Shoul
d
Size 7 oro
p
har
y
n
g
eal tube
Coul
d
Size 8 oro
p
har
y
n
g
eal tube
Will not have Size 3 laryngoscope
Operating room supplies
Must IV stan
d
Should
Infusion pump filled with
syringes
Coul
d
ECG electrodes
Will not have Blood
p
ressure cuff
Sur
g
ical
p
rocedures
Must
Laparotomy (in supine
p
osition): vertical incision
Should
Laparoscopy (in supine or
(anti)Trendelenburg)
Could
Laparotomy in pregnant
p
atients
(
horizontal incision
)
Will not have Limb surger
y
Table 4.
DYNAMIC
Anaesthesia su
pp
lies
Must have IV infusion sets in pink,
green, blue, yellow, and
oran
g
e
Should have Subcutaneous needle
Could have Tape
Will not have IV cathete
r
Airwa
y
su
pp
lies
Must have Size 6 oro
p
har
y
n
g
eal tube
Should have Size 7 oro
p
har
y
n
g
eal tube
Could have Size 8 oropharyngeal tube
Will not have Size 3 laryngoscope
Operating room supplies
Must have IV stan
d
Should have Infusion pump filled with
s
y
rin
g
es
Could have ECG electrodes
Will not have Blood
p
ressure cuff
Surgical procedures
Must have Placement of IV line
Applying a tourniquet
Finding a visible vein
(lightly tapping on vein,
asking patient to make a
fist)
Cleaning the skin
Opening IV packaging
Placing IV catheter
Securing the catheter with
tape
Connecting IV bag to IV
line
Administration of bolus
medication
Opening the cap or valve
and attaching the syringe
Pushing the plunger
Administration of
continuous medication -
Medication is in a pump
that is connected to the IV
line
Selecting "speed" and
"amount" of medication,
then confir
m
Placement of vital
monitoring
(after connecting to the
monitor, values are also
visible on the screen)
BIS
-Placing BIS stickers on
forehead
-Connecting to BIS
monitoring
ECG:
Placement of 5 electrodes
-Connection to ECG
monitoring
Blood pressure
-Placement of blood
pressure cuff
-Connection to monitoring
Pulse oximeter
-Placement of finger probe
-Connection to monitorin
g
Intubation
Preoxygenation with
placement of a mask on
patient's face
Induction of anesthesia:
starting medication that
causes patient to fall asleep
ERSeGEL 2024 - Workshop on Extended Reality and Serious Games for Education and Learning
756
Bag-valve mask ventilation
Intubation
-With laryngoscope
-With glidescope
-different views:
View grade 1, View grade
2, View grade 3, View
grade 4, View with vomit
grade 1/2
Positioning:
Table in Trendelenburg
position
Table in Anti-
Trendelenburg position
Placement of an additional
rolled-up blanket under the
neck
(changes intubation
conditions)
Placement of arms along the
sides
Placement of arms on
armrests
Placement of sterile drapes
with attachment to the
anesthesia
p
ole
Should Placement of arterial line
Palpate for pulses (inside
pulse for radial artery)
Sterilize the skin
Injection of local anesthesia
(2cc syringe with lidocaine,
subcutaneous needle)
Opening of arterial needle
from packaging
Placement of arterial needle
(placement is successful:
red blood returns from the
hub)
Withdrawal of needle
Advancement of catheter
Close the red cap
Cover with tegaderm
Connect arterial line
Zeroing arterial line
(
o
p
tional
)
Removal of arterial blood
Draw blood into arterial line
hub
Withdrawal of arterial blood
Backflush blood from the
arterial line hub
Flush arterial line
Warming
Placement of upper body or
lower bod
y
Administration of
pressure infusion
Place the infusion in a
p
ressure ba
g
Squeeze the air pump under
the
p
ressure ba
g
.
Could have Placement of gastric tube
Placement of gastric tube
through the nostril
Advancement of the tube up
to 55cm
Suctioning the gastric tube
will either show nothing
(tube is likely misplaced) or
green gastric contents (tube
is in the right place)
Ta
p
in
g
the tube in
p
lace
Will not have Defibrillation
Placement of defibrillator
pads (rhythm visible on
defibrillator)
Charging the defibrillator
with adjustable joules
Rhythm chec
k
Should Placement of temperature
probe
Placement of temperature
probe through the nostril
Connection to the monito
r
Will not have Placement of central line
Placement of urinary
catheter
Placement of ultrasound-
guided IV
Placement of ultrasound-
guided CVC
Placement of ear oximetry
Placement of TOF-CUF
Measurement of
neuromuscular blockade
Blood draw from peripheral
site
Cell-saver
Warming Connection to
bear-hugger
Activation of bea
r
-hu
gg
e
r
Development of a Real-Time Adaptable Virtual Reality-Scenario Training for Anaesthesiology Education, a User-Centered Design
757
