
Development of a Patient-Embodied Experience, How and Why?
Krista Hoek
a
, Monique van Velzen
b
and Elise Sarton
c
Department of Anaesthesiology, LUMC, Albinusdreef 2, 2333ZA, Leiden, The Netherlands
Keywords: VR, Therapeutic Language and Communication, Ethnographic Phenomenology, Health Care Education,
Patient-Embodied Experience, Proteus-Effect.
Abstract: Introduction: The rise of immersive technologies, particularly virtual reality (VR), has significantly impacted
medical education. In patient-embodied VR, through VR headsets, learners can embody patient's perspective,
offering a secure and immersive learning encounter. This communication outlines a framework for crafting
patient-embodied experiences, drawing from our VR endeavours aimed at enhancing therapeutic
communication skills in medical education. Methods: Our framework includes a development process with
consideration of user experience, technical implementation, content creation and validation. Central to content
creation is the collaborative construction of a patient journey, involving the involved parties via storyboards
and scripts distinguishing direct and indirect actions. Results: For our patient-embodied experience, the
cooperative development of the patient journey, script and storyboard included an initial version created by
the main researcher after study of landmark articles on therapeutic communication and fieldwork. Validation
was achieved through two group sessions with healthcare providers who consented to participate.
Conclusions and practice implications: The findings and insights presented can contribute to the growing
knowledge in the field of educational VR development. They demonstrate the feasibility and potential of
leveraging immersive technologies to create engaging and impactful virtual experiences. Hitherto, further
validation may evaluate how they influence believes and attitudes of healthcare providers towards therapeutic
communication.
1 INTRODUCTION
Medical education has been incorporating elements
of experiential learning for several decades, and the
specific use of immersive technologies has gained
more prominence in recent years. In particular,
learning with virtual reality (VR), or immersive
virtual environments (IVEs) aligns with the
Constructivist Theory, which suggests that learners
actively construct their knowledge and understanding
of the world by building upon their existing mental
frameworks. In an immersive learning environment,
learners are given the opportunity to explore,
discover, and make meaning from their experiences
(Whitman, 1993)
In virtual reality (VR), immersive learning
incorporates various sensory modalities to enhance
multisensory engagement enabling embodiment.
a
https://orcid.org/0000-0003-1984-3182
b
https://orcid.org/0000-0002-0289-6432
c
https://orcid.org/0009-0007-4403-3815
Embodiment is the possibility in VR to visually
substitute a person's real body by a life-sized virtual
one, seen from the person's own first-person
perspective. In other words, when we place a VR
headset on, our virtual bodies momentarily substitute
our real bodies, a phenomenon known as the Proteus
effect (Fox et al., 2013). Multisensory and motor
systems interconnect during cognitive processing.
During VR, embodiment can increase users’
engagement and provide emotional fidelity invoking
a sense of presence creating realistic emotional and
neurocognitive responses (Bem, 1972; Navarro et al.,
2022).
When using VR as educational tool, learners have
the ability to experience a full 360-degree view,
providing them with unrestricted access and freedom
to explore their surroundings. This contrasts to
traditional video experiences, where the audience's
perspective is limited to a fixed viewpoint as depicted
758
Hoek, K., van Velzen, M. and Sarton, E.
Development of a Patient-Embodied Experience, How and Why?.
DOI: 10.5220/0012755800003693
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 16th International Conference on Computer Supported Education (CSEDU 2024) - Volume 1, pages 758-764
ISBN: 978-989-758-697-2; ISSN: 2184-5026
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
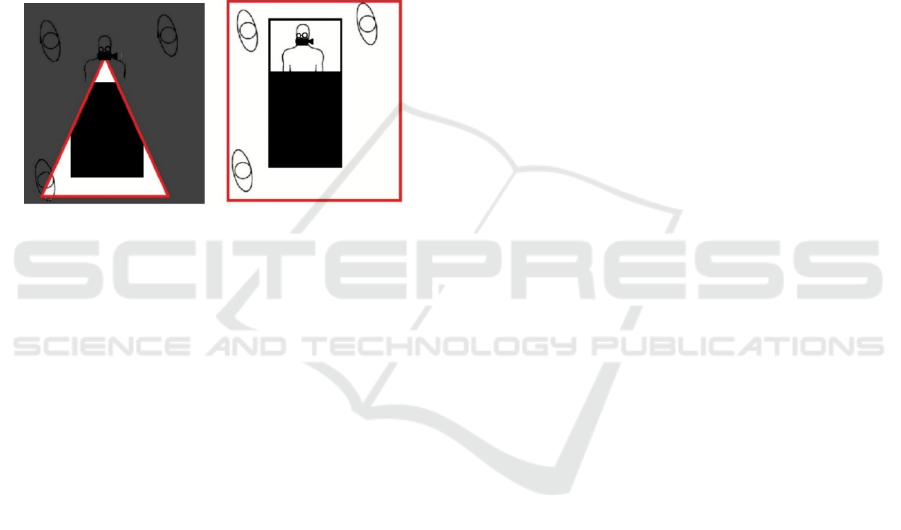
in Figure 1. The distinctive aspect of VR lies in its
participatory nature. In VR, writers, directors, and
producers, referred to as builders, do not have the
ability to dictate how learners engage with the story.
Instead, they can only invite participation, allowing
learners to choose where to direct their attention and
which aspects of the story to focus on (O’Sullivan et
al., 2018). This stands in contrast to conventional
storytelling, where a storyteller transmits the
narrative to listeners. Traditional videos typically
provide viewers a fixed perspective. The screen acts
as a window into the world of the video, and viewers
can only observe the events and scenes from the
specific viewpoint chosen by the director as shown in
Figure 1.
Figure 1: Red outlines show the extent of what a camera can
film in 90 vs 360 degrees of freedom. Left: 90 degrees of
freedom of traditional film, Right: 360 degrees of freedom
of VR.
In healthcare, a growing emphasis on patient-
centered care, and consumerism in medicine has
exemplified the importance of effective physician-
patient communication (Santana et al., 2018) and the
use of IVEs as an educational tool in this context
(“The Effects of Viewing an Uplifting 360-Degree
Video on Emotional Well-Being Among Elderly
Adults and College Students Under Immersive
Virtual Reality and Smartphone Conditions,” 2020;
Tang et al., 2022). We will refer to patient-embodied
VR as the specific VR application where a learner
who puts on the VR headset virtually becomes the
patient. Given that this immersive transformation has
the capacity to affect self-perception, attitudes,
convictions, and conduct in both implicit and explicit
ways (Bian et al., 2015; Fox et al., 2013; Navarro et
al., 2022), our hypothesis posits that it holds
substantial promise as an exceedingly effective and
innovative pedagogical approach in education on
communication skills.
An example of the use of patient-embodied VR
can be found in our work published recently (Hoek et
al., 2023a, 2023b). We developed two patient-
embodied experiences to create a possibility for
healthcare providers to feel what it is like to become
a patient. In these VR experiences, the learner
experiences the sequential stages of a patient
undergoing elective general anesthesia and surgery,
with nuanced shifts in language and interactions. We
will describe how we have developed these
experiences, and what important lessons we have
learned that can be used by researchers aiming to
develop-embodied VR experiences.
2 METHODS
This prospective exploratory research was carried out
at the Leiden University Medical Center (LUMC,
Leiden, the Netherlands), a large tertiary academic
teaching hospital. The protocol was approved by the
Institutional Science Committee and obtained a
waiver from the Institutional Review Board
(NWMO-LUMC).
Informed consent was obtained prior to
inclusion, participation was voluntary and privacy
rights were in alignment with the Declaration of
Helsinki and GDPR guidelines. Data was collected
and recorded between February 2019 to December
2020. Participants received no financial
compensation.
2.1 Participants and Procedures
Healthcare providers working in the OR were invited
to participate in the development of the patient-
embodied VR experiences. They were recruited
between January 2019 and May 2019. The procedure
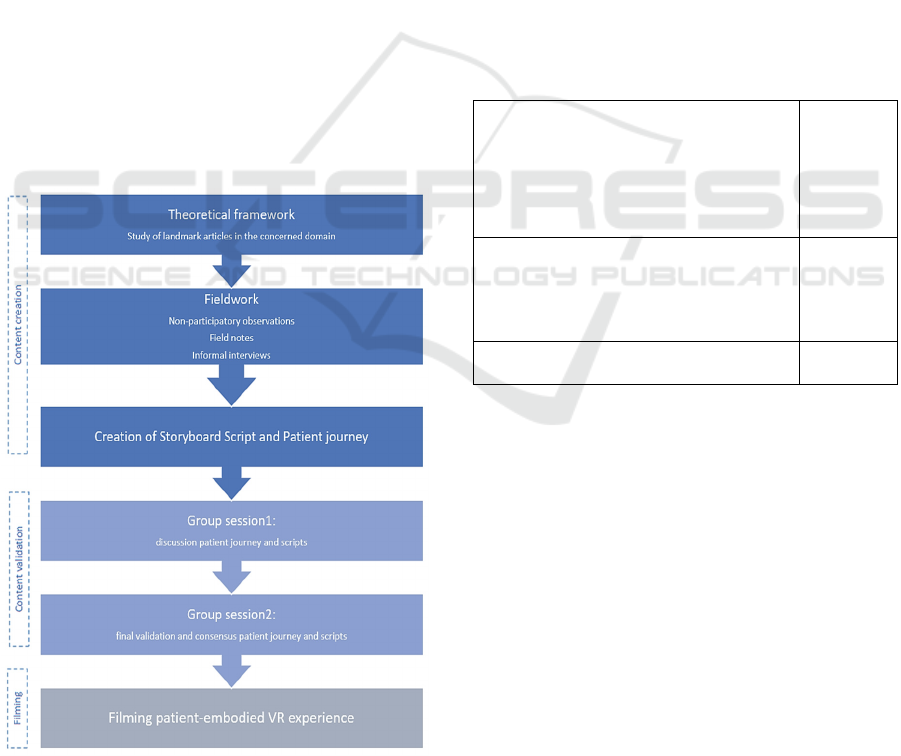
encompassed content creation, content validation,
and filming and editing of the VR experiences as
shown in Figure 2.
2.2 Content Creation
To create the storyboard and script of the patient
journey, a theoretical framework needed to consider
the study of landmark articles in the concerned
domain. In our case, Landmark patient-centered
studies were used to include important aspects of
lived patient experiences in preoperative settings
(Ben-Amitay et al., 2006; Butt, 2021; Derksen et al.,
2013; Kain et al., 2004; Kain et al., 2006; Lang et al.,
2005; Maranets & Kain, 1999; Smith & Mishra, 2010;
Swayden et al., 2012).
Secondly, fieldwork of the researcher (KH)
included informal interviews with healthcare
providers and patients, along with observations to
gather data was used to create an initial script for the
patient journeys as shown in Figure 2.
Development of a Patient-Embodied Experience, How and Why?
759
2.3 Content Validation
Group sessions are an adapted tool to validate the
storyboard and script (Stewart et al., 2007). In our
study, a first group session was held to discuss and
adapt the scripts.
Group input such as photographs, focused and
selective observation notes, reflective notes and
commentaries were used to write a second version of
the patient journeys. A second group session implied
a final validation where the scripts were discussed
and adapted until consensus was reached; that is until
the final script was consented by all group members
(Briggs et al., 2005) as shown in Figure 2.
The specific linguistic features were further
validated by an independent hypnotherapist based on
validated and relevant research (Boselli et al., 2018;
Lang, 2019; Lang & Berbaum, 1997; Lang et al.,
2005; Swayden et al., 2012; Watzlawick, 1978; Zech
et al., 2014).
2.4 Filming and Editing
Asking healthcare providers to play their own role has
several advantages as its economical, and the actors
may identify themselves very easily with their own
Figure 2 structure of the study participation.
professional role. We asked the developers to play
their own professional role, e.g. a surgeon would play
the surgeon. An anaesthetic nurse volunteered to play
the patient, as she had been a surgical patient several
times before.
3 RESULTS
3.1 Case Study Description
Nine healthcare providers participated in the
development of the patient-embodied VR
experiences. Six were OR nurses , one was a surgeon
and two were anaesthesiologist-hypnotherapists. One
hypnotherapist who was not affiliated with our
hospital did not participate in the filming of the
experiences. The majority was female (82%).
Demographics are shown in Table 1.
Table 1: Demographic characteristics of the VR
development team and study participants.
Clinical role
Anaesthesiologist-hypnotherapist
CRNA (Nurse anaesthetist)
Preoperative holding area nurse
Operating room nurse
Surgeon
2
2
3
1
1
Years of practice
<1year
1-5years
5-10years
>10years
1
3
1
4
Sex
Male/Female
2/7
3.2 Development of the
Patient-Embodied VR Experiences
Between February 2019 and December 2019 two
scripts and storyboards were created: the positive and
negative patient-embodied VR experience.
Guidelines of several digital platforms were used
(Newton, 2016; O’Sullivan et al., 2018). Filming was
performed using a GoPro
®
camera, editing was
performed using Movavi
®
enabling the experiences
to be available on most common VR headsets. Also,
an online Youtube version was uploaded making it
possible to view the experience online.
The final durations of the experiences were 12
minutes and 19 seconds for the negative experience,
and 10 minutes and 36 seconds for the positive
experience.
ERSeGEL 2024 - Workshop on Extended Reality and Serious Games for Education and Learning
760
The story-world needed to be as consistent with
reality as possible, using objects, personas, and
actions to stimulate the sense of immersive presence.
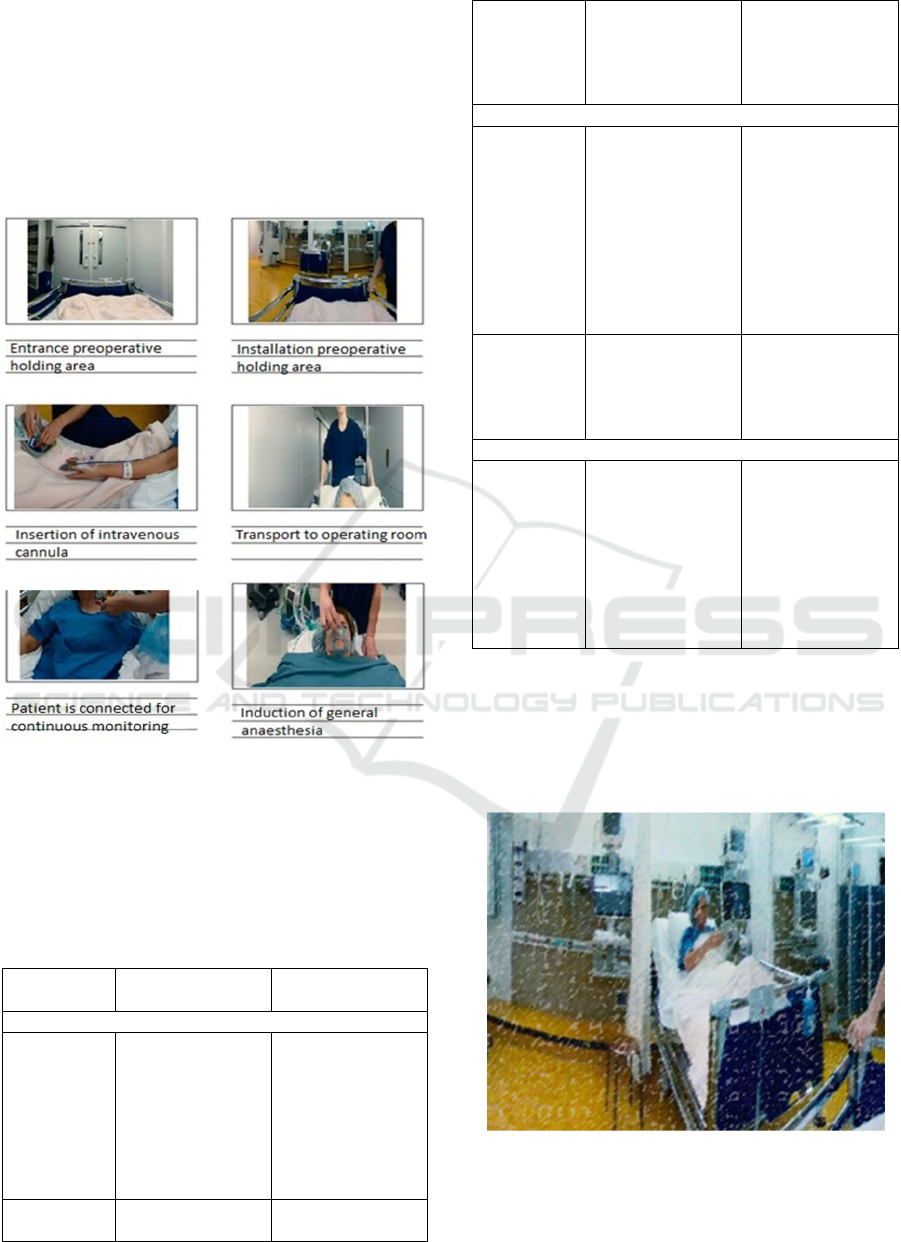
3.2.1 Storyboard and Script
We developed a storyboard with the main scenes as
shown in Figure 3 including all direct interactions
with the patient.
Figure 3: Storyboard patient-embodied VR experience.
We developed a script with ‘shadow actions’ visible
if the learner would look around. An overview of the
main differences in setting, direct interactions and
shadow actions can be found in Table 2.
Table 2: Overview of main difference in setting,
interactions and shadow actions.
Negative
experience
Positive experience
Setting
Preoperative
holding area
No (distraction)
activities for other
patients
No preventive
measures for
delirium prevention
Other patients use a
tablet or read a
magazine
Curtains opened,
visible clock,
noises of
monitoring
minimalized
Operation
room
Radio on Noises minimalized
Alarms and sounds
of continuous
monitoring on.
Surgical equipment
partially displayed
No visible surgical
equipment
Direct interactions
Contact with
preoperative
holding area
-Patient is ignored
when she requests
to go to the toilet
-Nurse does not ask
any personal
questions while she
places the IV
cannula
-Nurse sits next to
the patient
-Nurse uses
hypnotic distraction
methods during the
placement of the IV
cannula
-Nurse responds to
the concerns of the
patient.
Contact with
anaesthesio-
logist
Contact with
anaesthesiologist
with little rapport.
Anaesthesiologist
asks personal
questions before the
patient is taken into
the OR
Shadow interactions
Preoperative
holding area
OR nurse passes as
the patient is
brought to the
preoperative
holding area, he
tells his colleague
there is a bleeding
in the OR, and he
needs to hurry
OR nurse passes as
the patient is
brought to the
preoperative
holding area. He
holds something in
his arms, but is
discrete.
3.2.2 Setting
In the positive experience, another patient present is
able to read a magazine as shown in Figure 4. This is
a distraction method that may increase comfort while
the patients await their surgery (Pati & Nanda, 2011).
Figure 4: Positive experience: another patient reads a
magazine.
Development of a Patient-Embodied Experience, How and Why?
761
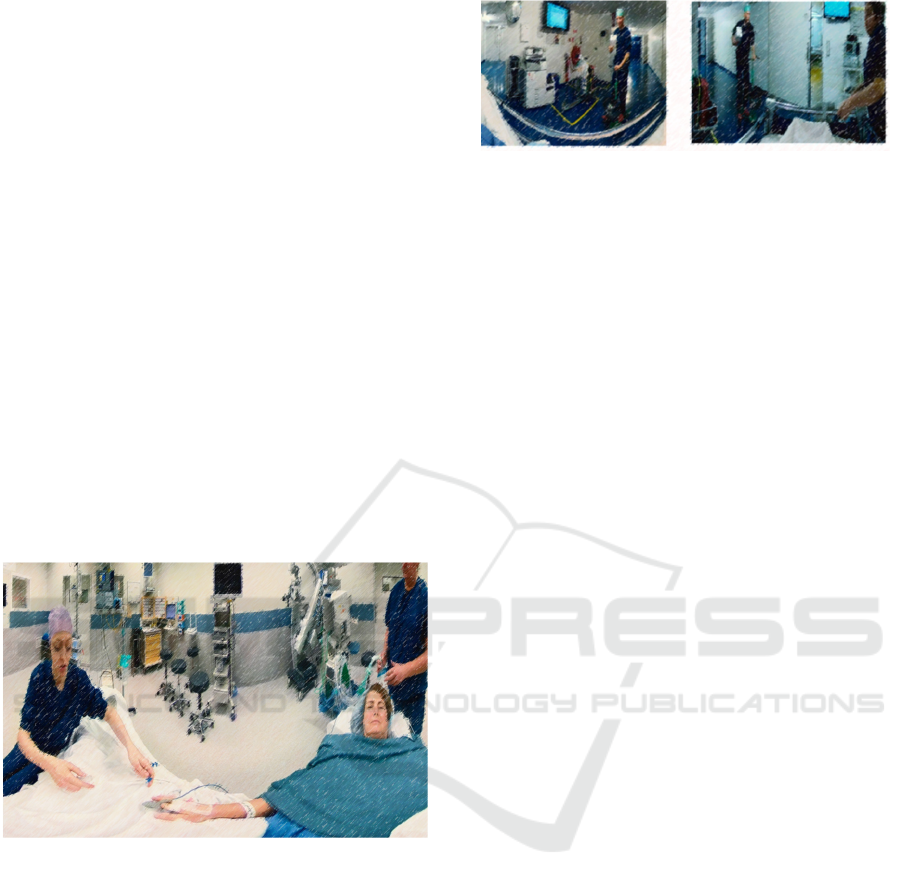
3.2.3 Direct Interactions
There are changes in attitude of the health care
providers with or without a direct therapeutic
relationship. One example is the communication style
of the anaesthesiologist just before the start of the
inductive phase of anaesthesia (patient is induced into
a state of unconsciousness and analgesia (pain relief)
before the start of the surgical procedure) as shown in
Figure 5.
In the negative video, the anaesthesiologist
administers the medication, however, the
communication shows limited effort to establish
rapport (Butt, 2021; Hall et al., 1995; Hoek et al.,
2023a). Furthermore, the potential side effects of the
drugs are explicitly mentioned, thereby increasing the
likelihood of the patient experiencing these adverse
effects (Lang et al., 2005; Zech et al., 2014).
In the positive experience, the anaesthesiologist
uses hypnotic linguistic techniques to induce
relaxation (Boselli et al., 2018), enhance focus and
promote a smooth start of general anaesthesia. The
anaesthesiologist sits beside the patient (Swayden et
al., 2012).
Figure 5: Anaesthesiologist sits next to the patient, uses
suggestive language to induce relaxation.
3.2.4 Shadow Actions
An example of a suggestion used in the final script
was having an OR-nurse pass by to bring blood for
the transfusion of another patient to enhance
authenticity of the dynamics of the operating theatre.
Subtle changes between the experiences are shown in
Figure 6.
One portrays an OR-nurse that politely smiles to
the patients without showing any concerns. The other
portrays an OR-nurse that expresses a sense of
urgency. He seems bothered, and tells the
preoperative nurse he has to deliver blood. The
preoperative nurse seems worried.
Figure 6: Left: the operating room (OR) nurse remains
silent and smiles politely without showing his concerns.
Right: the OR nurse conveys a sense of urgency to bring
blood to another patient, and the preoperative nurse appears
annoyed and worried.
4 DISCUSSION AND
CONCLUSION
4.1 Discussion
This study describes the development of two patient-
embodied VR experiences. The specific linguistic
features were validated by an independent
hypnotherapist and were based on validated and
relevant research (Boselli et al., 2018; Lang, 2019;
Lang & Berbaum, 1997; Lang et al., 2005; Swayden
et al., 2012; Watzlawick, 1978; Zech et al., 2014).
Internal validity of the VR experiences was
confirmed given that healthcare providers
participated in the development of these experiences
themselves. Between the two experiences, small
changes in setting, interactions and shadow actions
would implicitly suggest a more or less welcoming
experience. Indeed, the development included
addition of these several elements enhancing
authenticity of the VR experiences.
This type of immersive storytelling with VR
offers for learners a possibility to create their own
story in 360°; as they were able to look around freely
in VR. Additionally, healthcare providers played their
own roles during the filming of the scenes.
4.2 Limitations
One of the limitations of the VR experiences lies in
the limited interaction within the VR-environment.
The learner had the ability to observe their
surroundings; however, due to the recorded nature of
the experiences, learners were not able to freely move
around as they would have in a virtual environment
utilizing computer-generated 3D video imagery.
We selected this setting based on the believe that
a patient typically finds themselves confined to a
hospital bed with limited mobility or free choices. We
contend that utilizing a genuine operating theatre and
ERSeGEL 2024 - Workshop on Extended Reality and Serious Games for Education and Learning
762

real actors enhances fidelity, thereby intensifying the
sense of immersion.
4.3 Innovation
The findings and insights presented in this study can
contribute to the growing knowledge in the field of
educational VR development. They demonstrate the
feasibility and potential of leveraging immersive
technologies to create engaging, authentic and
impactful virtual experiences (Hoek et al., 2023a)
4.4 Conclusion
By using immersive VR technology, one can create
an interactive and engaging virtual environment that
allows learners to experience a simulated reality, that
is the experience of being a patient.
This development process involves careful
consideration of user experience, technical
implementation, content creation and validation. In
our opinion, key elements of the content creation
should be based on the cooperative development of a
patient journey, with participation of the involved
parties using a storyboard and script that distinguishes
between direct actions and indirect (shadow) actions.
4.5 Future Directions and Study
Validation
The findings of this study can contribute to further
research and healthcare education programs avid to
use experiential learning with patient-embodied VR.
We conclude with a call for further research to fully
unlock the potential and drawbacks of patient-
embodied VR as an educational tool and its
usefulness in medical training. Also, further research
may examine how patient-embodied VR might affect
patient reported outcomes like preoperative anxiety.
Initial validation of our patient-embodied
experience consisted of a qualitative study analyzing
the lived experience of anaesthesiologists (Hoek et
al., 2023a). Further validation may include evaluation
of the effects of the implementation of a training in
therapeutic communication with an integrated
patient-embodied VR experience.
ACKNOWLEDGEMENTS
We thank all healthcare providers participating in the
development of the VR experiences.
COMPETING INTERESTS
This research did not receive any specific grant from
funding agencies in the public, commercial, or not-
for-profit sectors.
REFERENCES
Bem, D. (1972). Self-perception theory (Vol. 6). Academic
Press.
Ben-Amitay, G., Kosov, I., Reiss, A., Toren, P., Yoran-
Hegesh, R., Kotler, M., & Mozes, T. (2006). Is elective
surgery traumatic for children and their parents? J
Paediatr Child Health, 42(10), 618-624.
https://doi.org/10.1111/j.1440-1754.2006.00938.x
Bian, Y., Zhou, C., Tian, Y., Wang, P., & Gao, F. (2015).
The Proteus Effect: Influence of Avatar Appearance on
Social Interaction in Virtual Environments. HCI,
Boselli, E., Musellec, H., Bernard, F., Guillou, N., Hugot,
P., Augris-Mathieu, C., Diot-Junique, N., Bouvet, L., &
Allaouchiche, B. (2018). Effects of conversational
hypnosis on relative parasympathic tone and patient
comfort during axillary brachial plexus blocks for
ambulatory upper limb surgery: A Quasiexperimental
Pilot Study. Int J Clin Exp Hypn, 66(2), 134-146.
https://doi.org/10.1080/00207144.2018.1421355
Briggs, R., Kolfschoten, G., & de Vreede, G.-J. (2005).
Toward a Theoretical Model of Consensus Building.
Butt, M. F. (2021). Approaches to building rapport with
patients. Clinical Medicine, 21(6), e662-e663.
https://doi.org/10.7861/clinmed.2021-0264
Derksen, F., Bensing, J., & Lagro-Janssen, A. (2013).
Effectiveness of empathy in general practice: a
systematic review. Br J Gen Pract, 63(606), e76-84.
https://doi.org/10.3399/bjgp13X660814
Fox, J., Bailenson, J., & Tricase, L. (2013). The
embodiment of sexualized virtual selves: The Proteus
effect and experiences of self-objectification via
avatars. Computers in Human Behavior, 29, 930–938.
https://doi.org/10.1016/j.chb.2012.12.027
Hall, J. A., Harrigan, J. A., & Rosenthal, R. (1995).
Nonverbal behavior in clinician—patient interaction.
Applied and Preventive Psychology, 4(1), 21-37.
https://doi.org/https://doi.org/10.1016/S0962-
1849(05)80049-6
Hoek, K., van Velzen, M., & Sarton, E. (2023a). Patient-
embodied virtual reality as a learning tool for
therapeutic communication skills among
anaesthesiologists: A phenomenological study. Patient
Education and Counseling, 114, 107789. https://doi.org/
https://doi.org/10.1016/j.pec.2023.107789
Hoek, K., van Velzen, M., & Sarton, E. (2023b). Response
to correspondance on patient-embodied virtual reality
as a learning tool for therapeutic communication skills
among anaesthesiologists: A phenomenological study.
Patient Educ Couns, 117, 107980. https://doi.org/
10.1016/j.pec.2023.107980
Development of a Patient-Embodied Experience, How and Why?
763

Kain, Z. N., Caldwell-Andrews, A. A., Maranets, I.,
McClain, B., Gaal, D., Mayes, L. C., Feng, R., &
Zhang, H. (2004). Preoperative anxiety and emergence
delirium and postoperative maladaptive behaviors.
Anesth Analg, 99(6), 1648-1654. https://doi.org/10.12
13/01.Ane.0000136471.36680.97
Kain, Z. N., Mayes, L. C., Caldwell-Andrews, A. A., Karas,
D. E., & McClain, B. C. (2006). Preoperative anxiety,
postoperative pain, and behavioral recovery in young
children undergoing surgery. Pediatrics, 118(2), 651-
658. https://doi.org/10.1542/peds.2005-2920
Lang, E. (2019). Comfort Talk®: From the Waiting Room
to the Treatment Suite. Dtsch Z Zahnarztl Hypn, 25(1),
22-24.
Lang, E. V., & Berbaum, K. S. (1997). Educating
interventional radiology personnel in nonpharmaco-
logic analgesia: effect on patients' pain perception.
Acad Radiol, 4(11), 753-757. https://doi.org/10.1016/
s1076-6332(97)80079-7
Lang, E. V., Hatsiopoulou, O., Koch, T., Berbaum, K.,
Lutgendorf, S., Kettenmann, E., Logan, H., &
Kaptchuk, T. J. (2005). Can words hurt? Patient-
provider interactions during invasive procedures. Pain,
114(1-2), 303-309. https://doi.org/10.1016/j.pain.200
4.12.028
Maranets, I., & Kain, Z. N. (1999). Preoperative anxiety
and intraoperative anesthetic requirements. Anesth
Analg, 89(6), 1346-1351. https://doi.org/10.1097/
00000539-199912000-00003
Navarro, J., Peña, J., Cebolla, A., & Baños, R. (2022). Can
Avatar Appearance Influence Physical Activity? User-
Avatar Similarity and Proteus Effects on Cardiac
Frequency and Step Counts. Health Commun, 37(2),
222-229. https://doi.org/10.1080/10410236.2020.1834
194
Newton, K. (2016). The Storyteller’s Guide to the Virtual
Reality Audience. Stanford d.school. https://medium.
com/stanford-d-school/the-storyteller-s-guide-to-the-
virtual-reality-audience-19e92da57497
O’Sullivan, B., Alam, F., & Matava, C. (2018). Creating
Low-Cost 360-Degree Virtual Reality Videos for
Hospitals: A Technical Paper on the Dos and Don’ts
[Tutorial]. J Med Internet Res, 20(7), e239.
https://doi.org/10.2196/jmir.9596
Pati, D., & Nanda, U. (2011). Influence of positive
distractions on children in two clinic waiting areas.
Herd, 4(3), 124-140. https://doi.org/10.1177/19375
8671100400310
Santana, M. J., Manalili, K., Jolley, R. J., Zelinsky, S.,
Quan, H., & Lu, M. (2018). How to practice person-
centred care: A conceptual framework. Health Expect,
21
(2), 429-440. https://doi.org/10.1111/hex.12640
Smith, A. F., & Mishra, K. (2010). Interaction between
anaesthetists, their patients, and the anaesthesia team.
Br J Anaesth, 105(1), 60-68. https://doi.org/10.1093/
bja/aeq132
Stewart, D., Shamdasani, P., & Rook, D. (2007). Focus
Groups (2nd ed.) https://doi.org/10.4135/97814129
91841
Swayden, K. J., Anderson, K. K., Connelly, L. M., Moran,
J. S., McMahon, J. K., & Arnold, P. M. (2012). Effect
of sitting vs. standing on perception of provider time at
bedside: a pilot study. Patient Educ Couns, 86(2), 166-
171. https://doi.org/10.1016/j.pec.2011.05.024
Watzlawick, P. (1978). The language of change: Elements
of therapeutic communication. W W Norton & Co.
Whitman, N. (1993). A review of constructivism:
understanding and using a relatively new theory. Fam
Med, 25(8), 517-521.
Zech, N., Seemann, M., & Hansen, E. (2014). [Nocebo
effects and negative suggestion in anesthesia].
Anaesthesist, 63(11), 816-824. https://doi.org/10.1007/
s00101-014-2386-8
ERSeGEL 2024 - Workshop on Extended Reality and Serious Games for Education and Learning
764
