
A Fuzzy Decision Support System with Semantic Knowledge Graph for
Personalized Asthma Monitoring: A Conceptual Modeling
Ayan Chatterjee
a
Dept. of Digital Technology, STIFTELSEN NILU, 2007 Kjeller, Norway
Keywords:
Fuzzy Ontology, Decision Support System, Asthma Monitoring, Knowledge Representation.
Abstract:
Asthma, a complex chronic respiratory condition, poses significant management challenges, necessitating
personalized monitoring for optimal treatment outcomes and individual well-being. This study introduces a
Fuzzy Decision Support System (FDSS) for personalized asthma monitoring, leveraging semantic reasoning
techniques and SPARQL querying to enhance decision-making accuracy and provide individualized assess-
ments of asthma control and exacerbation risk. By utilizing semantic reasoning, the FDSS captures intricate
relationships among asthma parameters, health data, triggers, and treatment outcomes, enabling precise man-
agement decisions. Development involves creating an ontology to encapsulate asthma domain knowledge,
representing fuzzy logic, integrating crisp and fuzzy clinical variables, and executing SPARQL queries for
fuzzy inference. The proposed FDSS demonstrates the feasibility of integrating these techniques for person-
alized asthma management, offering flexibility and adaptability to improve treatment outcomes and quality of
life. Further research is needed to validate its efficacy in real-world healthcare settings.
1 INTRODUCTION
Asthma is a significant global health issue, preva-
lent across all ages, particularly affecting children
(WHO, 2019). This chronic lung disease causes air-
way inflammation and hyper-responsiveness, lead-
ing to wheezing, breathlessness, chest tightness, and
coughing (Gibson, 2000). Effective asthma manage-
ment requires regular symptom tracking, lung func-
tion assessment, trigger identification, and therapeutic
adjustments (Kang, 2024). In 2019, asthma affected
262 million people worldwide, resulting in 455,000
deaths (WHO, 2019). In the U.S., over 25 million
individuals have asthma, including more than 5 mil-
lion children (Cleveland Clinic, 2023). Proper moni-
toring can control symptoms and allow individuals to
lead active lives, while avoiding triggers is crucial for
symptom relief (WHO, 2019). The high asthma mor-
tality in lower-income nations underscores the need
for better diagnostic and treatment strategies. The
World Health Organization aims to reduce the bur-
den of asthma and progress towards universal health
coverage. Asthma is classified into allergic and non-
allergic types, triggered by factors such as allergens,
air pollution, weather conditions, tobacco smoke, and
a
https://orcid.org/0000-0002-1051-2814
food allergens (Ajami, 2022). Symptoms vary widely
in frequency and severity, with each individual react-
ing differently. Traditional asthma monitoring meth-
ods often use simplistic decision systems and static
protocols, failing to account for the disease’s com-
plexity. These methods typically categorize patients
as controlled or uncontrolled based on fixed crite-
ria for symptom severity, lung function, or medica-
tion use, which can lead to suboptimal management
(Pinnock, 2015). There is a pressing need for ad-
vanced decision support systems that integrate vari-
ability among patients, environmental factors, and
treatment nuances. A promising approach is combin-
ing logic, semantics, reasoning, rules, and querying
to create a robust framework for personalized asthma
care. Semantic reasoning can capture and interpret
complex relationships between asthma types, symp-
toms, triggers, and treatment outcomes, enhancing
decision-making and management effectiveness.
The integration of Clinical Decision Support Sys-
tems (CDSS) in digital health is crucial for remote
monitoring and decision-making, particularly for
asthma management, leading to improved outcomes
(Dramburg et al., 2020). Key CDSS components
include monitoring, digital technology, decision-
making, and remote communication. Successful
CDSS requires context awareness and personaliza-
Chatterjee, A.
A Fuzzy Decision Support System with Semantic Knowledge Graph for Personalized Asthma Monitoring: A Conceptual Modeling.
DOI: 10.5220/0012910500003838
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 16th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2024) - Volume 2: KEOD, pages 143-150
ISBN: 978-989-758-716-0; ISSN: 2184-3228
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
143

tion, adapting to individual circumstances and spe-
cific needs. Al-Dowaihi et al. (Al-Dowaihi, 2013)
developed a prototype for asthma self-management in
high pollution environments, which also alerts health-
care providers. Anantharam et al. (Anantharam,
2015) created kHealth, which uses sensor data to help
physicians determine asthma severity and improve pa-
tient quality of life. Ra et al. (Ra, 2016) introduced
AsthmaGuide, a cloud-based system that uses smart-
phones for real-time data collection and patient em-
powerment. Dieffenderfer et al. (Dieffenderfer, 2016)
developed a wearable sensor system to study the im-
pact of environmental factors on asthma. Quinde et
al. (Quinde, 2018) proposed context-aware systems to
enhance personalized asthma management, while Gy-
rard et al. (Gyrard, 2018) combined multiple knowl-
edge sources to personalize chronic disease manage-
ment. Galante et al. (Galante, 2022) developed
a context-based asthma control method and demon-
strated a self-monitoring approach, though lacking
dynamism. Ajami et al. (Ajami, 2022) created an
ontology-driven model for personalized asthma risk
detection and exacerbation prediction. Vatsal et al.
(Vatsal, 2024) developed an AI ensemble model for
asthma exacerbation forecasting, showing potential
for enhanced prediction accuracy and individualized
treatment. Molfino et al. (Molfino, 2024) reviewed AI
advancements in asthma management, while Wiec-
zorek et al. (Wieczorek, 2024) evaluated automated
acoustic analysis for asthma diagnosis and monitor-
ing. These studies address heterogeneity in system
modeling, rule-based, or AI-driven decision-making,
but often neglect comprehensive context representa-
tion and unified knowledge models.
To enhance decision-making accuracy and adapt-
ability, this study introduces a Fuzzy Decision Sup-
port System (FDSS) for personalized asthma moni-
toring, incorporating semantic reasoning techniques.
Fuzzy logic (Wikstr
¨
om, 2014) offers a flexible ap-
proach for handling uncertain and imprecise data,
enabling more precise and context-sensitive deci-
sions. Semantic reasoning, including OWL-based
knowledge representation (Chatterjee, 2021) and
SPARQL querying (Chatterjee, 2022b), further re-
fines decision-making by capturing intricate data pat-
terns. By integrating fuzzy logic with semantic rea-
soning, this FDSS addresses conventional asthma
monitoring limitations and provides clinicians with
personalized, actionable insights for improved asthma
management. The identified research questions for
this study are − a. How does a semantic knowledge
graph enhance the development of a FDSS for person-
alized asthma monitoring? b. What are the challenges
and considerations in representing fuzzy knowledge
in FDSS? and c. How does knowledge base, crisp val-
ues and their fuzzy representations, facilitate person-
alized assessments and rule-based decision-making in
asthma management using the FDSS?
This is strictly a technical proof-of-concept study;
rather than a clinical study, and focuses on the con-
ceptual modeling and its theoretical verification. The
future study will focus more on technical validation
using robust datasets. The paper is structured as fol-
lows. Section 2 elaborates the proposed FDSS and
associated approaches for system modeling. Section
3 describes the implementation, answers the research
questions, and elaborates study limitations and future
scope. Moreover, the paper is concluded in Section 4.
2 PROPOSED WORK
The design and development of the proposed FDSS
involve following key aspects.
2.1 System Architecture
The proposed FDSS architecture (see Fig. 1) includes
the following layers − Data Acquisition Layer: Col-
lects patient data from sources such as electronic
health records (EHRs), clinical assessments, wearable
devices, and patient-reported data, including context
like asthma attack triggers and factors. Data Prepro-
cessing Layer: Ensures data quality, consistency, and
compatibility through cleaning, normalization, fea-
ture extraction, and transformation. Ontology Con-
struction Layer : Constructs an OWL ontology rep-
resenting asthma monitoring knowledge with classes,
properties, relationships, individuals, logical opera-
tors (AND, OR, NOT), inference rules (TBox and
ABox), and axioms. It integrates relevant ontolo-
gies (Ajami, 2022), such as Asthma from BioPor-
tal, weather from COPDology, food allergens from
FoodOn, and symptoms from SNOMED-CT. Fuzzy
Knowledge Representation Layer: Encodes fuzzy
knowledge in the ontology using linguistic variables,
membership functions, and fuzzy rules, storing both
crisp values and fuzzy representations of clinical vari-
ables. Fuzzy Inference Engine Layer: Uses SPARQL
queries to perform fuzzy inference on patient data for
personalized asthma control and exacerbation risk as-
sessments. Decision Support Layer: Combines fuzzy
inference results with clinical guidelines to provide
actionable recommendations for asthma management.
User Interface Layer: Offers a user-friendly inter-
face with dashboards and visualization tools for clini-
cians to input data, view recommendations, and track
patient progress. Integration Layer: Ensures FDSS
KEOD 2024 - 16th International Conference on Knowledge Engineering and Ontology Development
144
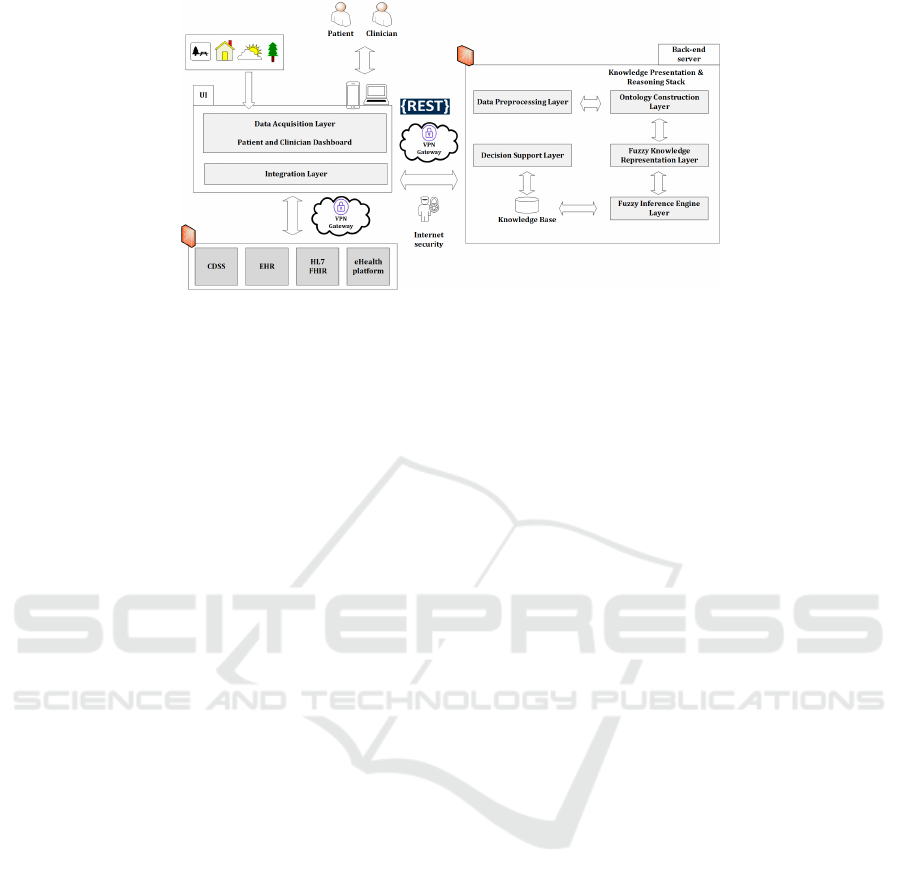
Figure 1: The architecture of the proposed Fuzzy Decision Support System (FDSS).
integration with EHR systems, CDSS, telemedicine
platforms, and Fast Healthcare Interoperability Re-
sources (FHIR), adhering to HL7 standards (Chatter-
jee, 2022a) for interoperability and data exchange.
2.2 Nature of Data
Asthma monitoring involves collecting diverse data
from sensors, questionnaires, and medical surveil-
lance (Merchant, 2018). Personal data includes de-
mographics (age, gender, location, occupation, smok-
ing status), asthma severity (severe, mild, moder-
ate), and physiological metrics (BMI, SpO2, heart
rate, body temperature). Age distinctions are cru-
cial, differentiating between Adult-onset (age < 18)
and Pediatric (age < 5) asthma. Asthma types in-
clude Exercise-induced, Occupational, and Asthma-
COPD overlap syndrome, with causes such as al-
lergies, chemicals, genetics, and infections. Symp-
toms range from intermittent to persistent, includ-
ing chest tightness, coughing, shortness of breath,
and wheezing, with severe attacks showing anxiety,
pain, nasal congestion, and cyanosis. Sensors de-
tect air pollutants like temperature, humidity, and par-
ticulate matter, aiding in trigger identification. Sen-
sor data, often continuous, falls into physiological
or environmental categories. Effective asthma man-
agement requires frequent monitoring and personal-
ized decision-making (Chakraborty, 2023), which an
FDSS can support, potentially reducing hospitaliza-
tions and costs. Analyzing both general and sensor
data enables informed treatment adjustments and pre-
ventive measures.
2.3 Ontology and Reasoning
Designing and developing an ontology and reasoning
involves defining formal representations of concepts,
relationships, and inference rules within the ontology.
Proposed ontology can be mathematically represented
as:
O = {C, P, I, φ, R}
where: C = set of classes representing key concepts
in asthma monitoring (e.g., Patient, Symptom, Per-
sonal Information, Medication, TreatmentPlan), P =
set of properties representing relationships between
classes (e.g., hasSymptom, hasMedication, hasTreat-
mentPlan), I = set of individuals or instances of
classes, φ = Set of logical formulas representing ax-
ioms and constraints (e.g., a patient can have multi-
ple symptoms, but only one treatment plan at a time),
and R = set of inference rules for deriving new knowl-
edge from existing data and ontology axioms (e.g., If
a patient has a specific combination of symptoms, rec-
ommend a personalized treatment plan based on his-
torical data, if a patient’s environmental exposure data
indicates high levels of allergens, suggest adjustments
to the treatment plan to account for potential exacer-
bation). The same can be represented mathematically
as follows − C = {C
1
,C
2
, . . . ,C
n
}, P = {(C
i
,C
j
)},
where (C
i
,C
j
) denotes a property between classes C
i
and C
j
, and
I = {i
1
, i
2
, ..., i
m
},
where i
j
is an instance of class C
k
.
Φ = {∀x(C(x) → P(x)), ∃x(C(x) ∧ Q(x))}
where C(x) and P(x) are predicates representing class
membership and property relationships, respectively.
A simplified example using first-order logic is as fol-
lows, −
P(x) represent the predicate “x is a patient”.
O(x, y) represent the predicate “x has observation y”.
S(x, y) represent the predicate “x has symptom y”.
T (x, y) represent the predicate “x has treatment plan
y”.
A Fuzzy Decision Support System with Semantic Knowledge Graph for Personalized Asthma Monitoring: A Conceptual Modeling
145

Axioms:
∃p ∈ P : There exists at least one patient in the
ontology
∀x∃y : P(x ) → O(x, y) : Patient has observation plans
∀x∃y : P(x ) → T (x, y) : Patient has a treatment plan
∀x∀y : T (x, y) → R(x, y) : Every treatment plan is
recommended for the patient
Inference Rules:
∀x∀y : P(x ) ∧ S(x,y
1
) ∧ S(x, y
2
) ∧ . . .
→ T (x, z) : If a patient exhibits specific symptoms,
recommend a personalized treatment plan
In description logics (DL), a TBox (T ) represents
the terminology or schema of the ontology, an ABox
represents the assertion or instance data, and an RBox
(R ) represents the relationship between classes and
properties; the same has been incorporated into the
mathematical model for ontology and reasoning in the
context of personalized asthma monitoring. As an ex-
ample, the concepts can be represented as:
T : {∀x(AP(x) → P(x)), x(HS(x, y) → S(x) ∧ P(y))},
A = {AP(a), S(s), HS(a, s)},
where a is an instance of AsthmaPatient class, s is an
instance of Symptom class, and (a, s) asserts the re-
lationship HasSymptom between AsthmaPatient and
Symptom, and
R = {F(HS ), I(HS, SO)},
where F(HS) specifies that the property HasSymp-
tom is functional, and I(HS, SO) indicates the inverse
relationship between HasSymptom and SymptomOf.
Inference rules have been applied to the TBox and
ABox to derive new knowledge from existing asser-
tions and schema definitions.
Let n be the number of classes, m be the number
of properties, and k be the knowledge base size. The
time complexity for building the ontology model is
O(n + m + k). Consistency checks and completeness
verification involve traversing the ontology structure
and logical evaluations. Overall complexity is influ-
enced by the ontology size, inference rules complex-
ity, ontology refinement extent, and test data size.
2.4 Fuzzy Knowledge Representation
Integrating fuzzy knowledge into the personalized
asthma monitoring ontology enhances adaptability
and depth by accommodating uncertainty and vague-
ness in healthcare data. Fuzzy ontology improves
modeling of imprecise concepts, relationships, and
membership degrees, addressing challenges in sub-
jective symptom categorization. Unlike conventional
ontologies that struggle with subjective evaluations
like ”mild,” ”moderate,” or ”severe,” fuzzy ontology
captures these assessments accurately, enabling pre-
cise reasoning and decision-making in asthma care.
Fuzzy sets and membership functions represent lin-
guistic variables and their degrees of membership.
Let’s consider, X: Universe of discourse (set of all
possible values), µ
A
(x): Membership function repre-
senting the degree of membership of an element x in
the fuzzy set A, and A: Fuzzy set defined over uni-
verse X . Each patient p is associated with fuzzy sets
representing observational variables:
Observations(p) = {(A
1
, µ
A1
), (A
2
, µ
A2
), . . . , (A
n
, µ
An
)}
where A
i
represents a linguistic variable and µ
Ai
repre-
sents its corresponding membership function. There-
fore, fuzzy logic system (FLS) can be mathematically
represented as:
FLS = (X, {A
1
, A
2
, . . . , A
n
}, {µ
A
1
, µ
A
2
, . . . , µ
A
n
}, Rules)
µ
A
i
(x) represents the degree of membership of
of crisp value x in linguistic variable A
i
.
The fuzzy sets in the ontology modifies the TBox
(a set of logical formulas defining fuzzy classes, prop-
erties, and relationships), ABox (a set of assertions or
instance data with fuzzy degrees of membership), and
RBox (a set of logical formulas defining fuzzy prop-
erties and their characteristics).
T Box = {∀x(A(x) → µA(x)), ∀x(B(x) → µB(x)),
R(A, B), . . .}
Here, ∀x(A(x) → µA(x)) represents the first part of
T Box, ∀x(B(x) → µB(x)) represents the second part,
R(A, B) represents the relation between A and B.
ABox = {(a, µ
A
(a)), (b, µ
B
(b)), (c, µ
C
(c)), . . .}
where µ
A
(a), µ
B
(b), µ
C
(c), etc., represent member-
ship functions.
RBox = {∀x (A(x)∧ B(x) → R
1
(x)), Functional(R
1
),
InverseOf(R
1
, R
2
), . . .}
Fuzzy inference rules apply fuzzy logic opera-
tions to fuzzy sets to derive new fuzzy knowledge.
If A is true with degree µ
A
(x) and B is true
with degree µ
B
(x), then C is true with degree
min(µ
A
(x), µ
B
(x)). As an example, let, Crisp value
Set − Symptom Severity: {Low, Medium, High} ∈
{1, 10}, Medication Adherence: {Low, Medium,
High} ∈ {1, 10}, and Environmental Sensitiv-
ity: {Low, Medium, High} ∈ {1, 10}, Predicate
KEOD 2024 - 16th International Conference on Knowledge Engineering and Ontology Development
146

logic statements − HighSymptomSeverity(x): Pa-
tient x or P(x) has high symptom severity level,
LowMedicationAdherence(x): P(x) has low medi-
cation adherence, HighEnvironmentalSensitivity(x):
P(x) has high environmental sensitivity,
UncontrolledAsthma(x): P(x) has uncontrolled
asthma, and HighExacerbationRisk(x): P(x) has
high exacerbation risk, and Fuzzy rules − Rule −
1: UncontrolledAsthma ← HighSymptomSeverity ∨
LowMedicationAdherence, and Rule − 2: HighEx-
acerbationRisk ← HighEnvironmentalSensitivity.
Let’s fuzzify the predicate logic statements
for Participant P(x) using linguistic variables
and membership functions − Symptom Severity:
High or HighSymptomSeverity(P(x)) (Mem-
bership: 0.8), Medication Adherence: Low or
LowMedicationAdherence(P(x)) (Membership:
0.5), and Environmental Sensitivity: High or
HighEnvironmentalSensitivity(P(x)) (Membership:
0.7). The centroid method (Chakraverty, 2019)
which has been used for defuzzification, calcu-
lates the center of gravity of the aggregated fuzzy
output to determine the crisp output value for
further decision-making with SPARQL in fuzzy
ontology. According to the fuzzy Rule − 1, the
membership degree of UncontrolledAsthma for
P(x): µ
UncontrolledAsthma
(P(x)) = max(0.8, 0.5) = 0.8,
and According to the fuzzy Rule − 2, the mem-
bership degree of HighExacerbationRisk for P(x):
µ
HighExacerbationRisk
(P(x)) = 0.7. Based on centroid
defuzzification method, the crisp output for Uncon-
trolledAsthma is 1 and for HighExacerbationRisk is
0.7.
Below are sample queries to retrieve the a. fuzzy
sets for different degrees of symptoms, asthma sever-
ity, and tiredness with their defuzzified membership
values, and b. the current degree of asthma severity
and frequency of symptoms for patients :
Query:1 - Retrieve Fuzzy Sets for Degree of asthma
severity, tiredness, and frequency of symptoms
SELECT ?severity ?tiredness ?frequency ?memvalue
WHERE {
?severity a :DegreeOfAsthmaSeverity ;
?tiredness a :Tiredness ;
?frequency a :FrequencyOfSymptoms ;
:hasMembershipValue ?memvalue .
}
Query:2 - Retrieve Asthma Severity and Symptom
Frequency for Patients
SELECT ?patient ?severity ?symptom ?frequency
WHERE
{
?patient a :Patient ;
:hasAsthmaSeverity ?severity .
?patient :hasSymptom ?symptom .
?symptom :hasFrequency ?frequency .
}
2.5 Proposed Algorithm
Algorithm 1 integrates asthma patient data and fuzzy
ontology for personalized care recommendations. It
evaluates fuzzy rules based on symptoms and demo-
graphics, optimizing care by considering their inter-
action and enhancing recommendation efficacy.
Algorithm 1: Personalized Asthma Monitoring and
Rule-based Decision-Making.
Require: • Patient data including symptoms and
demographic factors
• Fuzzy ontology with properties, linguistic
terms, membership functions, fuzzy rules,
and SPARQL queries.
Ensure: Personalized care recommendations based
on the patient’s symptom profile and demo-
graphic characteristics
1: Retrieve patient observable and measurable data
from Ontology
2: Execute SPARQL Queries to obtain fuzzy out-
comes for each symptom and demographic factor
3: Evaluate fuzzy rules using the fuzzy outcomes
4: Aggregate the fuzzy rule activations
5: Generate personalized care recommendations
based on the aggregated rule activations
6: return Personalized care recommendations
Goal: The algorithm aims to trigger logical rules
of the form (A IMPLIES B) or its equivalent (NOT(A)
OR B) for generating tailored recommendations af-
ter decision-making. If certain variables are inferred
as true, recommendations are provided based on the
originating semantic data. Time Complexity: Re-
trieving patient data has a complexity of O(1) or O(n)
if iterating over ’n’ patients. Executing SPARQL
queries has a complexity of O(m), where ’m’ is the
number of queries. Evaluating fuzzy rules has a com-
plexity of O(r), where ’r’ is the number of rules.
Aggregating fuzzy rule activations and generating
recommendations both have a complexity of O(1).
Therefore, the overall time complexity is O(m + r).
A Fuzzy Decision Support System with Semantic Knowledge Graph for Personalized Asthma Monitoring: A Conceptual Modeling
147

Figure 2: Key classes of the proposed ontology using OWLViz in Prot
´
eg
´
e.
Space Complexity: Storing patient data requires
O(n) space. The space required for the fuzzy ontol-
ogy is O(k + r), accounting for linguistic terms and
fuzzy rules. Thus, the overall space complexity is
O(k + r). The time and space complexities primarily
depend on the number of SPARQL queries executed
(m) and the number of fuzzy rules (r). Evaluation:
The concept is evaluated using the “Asthma Disease
Prediction Dataset” (Dataset, 2024), which includes
patient data, environmental factors, and medical his-
tory to predict asthma onset, severity, and treatment
outcomes.
2.6 Experimental Setup
Fuzzy OWL 2 in Prot
´
eg
´
e was used to design the on-
tology model, including classes, properties, relation-
ships, and individuals, while the Fuzzy DL reasoner
verified its consistency.
3 IMPLEMENTATION AND
DISCUSSION
The important classes of fuzzy ontology are depicted
in Fig. 2 (Axiom: 150, Logical axiom: 90, Declara-
tion axiom: 102, Class: 75, object property: 45, data
property: 63, and class axioms: 95). In Prot
´
eg
´
e, using
the Fuzzy DL reasoner, it achieved a reasoning time of
under 40.0 seconds without reporting any inconsisten-
cies. When loaded into the Jena workspace with the
“OWL MEM MICRO RULE INF” ontology specifi-
cation in TTL format (OWL full), the reading time
was approximately 4.0-4.5 seconds. Queries for on-
tology classes, ontologies, and statement elements
(predicate, subject, object) using Jena were executed
in under 3.0 seconds, 1.0 seconds, and 4.0 seconds
respectively. Each ontology model, representing a
complete RDF graph, is associated with a document
manager (default global document manager: “Ont-
DocumentManager”) to facilitate ontology document
processing. In the ontology API, all classes repre-
senting ontology values inherit from “OntResource”
with common attributes (versionInfo, comment, la-
bel, seeAlso, isDefinedBy, sameAs, differentFrom)
and methods (add, set, list, get, has, remove). This
paper presents a mathematical model for personal-
ized recommendation generation based on SPARQL
queries on top of a fuzzy ontology. The model uti-
lizes set theory to define patient attributes, filter func-
tions, and recommendation functions. It dynamically
generates tailored recommendations for asthma man-
agement based on patient characteristics and severity
of their asthma condition. The used dataset helps in
this regard for the proposed theoretical concept evalu-
ation. Let, P represent the set of patients in the fuzzy
ontology. Each patient p ∈ P has attributes such as
tiredness T (p), difficulty in breathing D(p), severity
S(p), and age A(p). Defined filter function F to select
patients, based on specific criteria:
F(p) =
(
1 if T (p) ≥ t
min
and D(p) ≥ d
min
and A(p) ≥ a
min
0 otherwise
Where:
t
min
is the minimum threshold for tiredness,
d
min
is the minimum threshold for difficulty
in breathing,
a
min
is the minimum age threshold.
Next, let R denote the set of recommendations.
For each patient p selected by F, the generated
personalized recommendations r are based on their
severity S(p) using fuzzy logic rules. The recommen-
dation function G is defined as:
G(p) =
“Administer emergency treatment” if S(p) = “Severe”
“Increase medication dosage” otherwise
KEOD 2024 - 16th International Conference on Knowledge Engineering and Ontology Development
148

Finally, a SPARQL query has been executed on the
fuzzy ontology to filter patients based on F, and for
each selected patient, generate personalized recom-
mendations using G. The result is a set of patient-
recommendation pairs {(p
1
, r
1
), (p
2
, r
2
), . . .}, provid-
ing tailored asthma management recommendations
for each patient.
The proposed fuzzy ontology includes properties,
such as “Age Group”, “Degree of Asthma Sever-
ity”, “Frequency of Symptoms”, “Effectiveness of
Medication”, and “Recommendation”. Fuzzy rules
recommend treatment adjustments based on these
properties. Moreover, specific symptoms and de-
mographic factors are incorporated into the ontol-
ogy to personalize asthma monitoring and care. The
logical structure of the ontology is supported by
the features of the adopted dataset. The extended
structure of the fuzzy ontology includes properties
such as “Tiredness” (Tiredness(x), where x represents
the degree of tiredness experienced by the patient,
and membership functions: µ
Low
(x), µ
Medium
(x),
and µ
High
(x)), “Dry-Cough” (Dry-Cough, where
Dry-Cough(x) is true if the patient experiences a dry
cough and false otherwise), “Difficulty-in-Breathing”
(Difficulty-in-Breathing(x), where x represents the
severity of difficulty in breathing, and membership
functions: µ
Low
(x), µ
Medium
(x), µ
High
(x)), “Sore-
Throat” (Sore-Throat, where Sore-Throat(x) is true if
the patient experiences a sore throat and false other-
wise), “Severity” (Severity(x), where x represents the
severity levels, and membership function: µ
Mild
(x),
µ
Moderate
(x), µ
Severe
(x)), and Age with corresponding
linguistic terms and membership functions. Age has
been found as an important property in asthma moni-
toring and care. Thus, let, A
1
, A
2
, A
3
, and A
4
represent
the fuzzy sets for the following age categories: A
1
(x):
Less than 5 years, A
2
(x): 5-18 years, A
3
(x): 18-65,
and A
4
(x): Greater than 65 years.
For evaluation on the adopted dataset, two fuzzy
rules have been considered from the rule-base or
knowledge base (KB) for personalized recommen-
dation generation: Rule − 3: IF Tiredness is high
AND DifficultyInBreathing is moderate THEN In-
crease Medication Dosage (IMD), and Rule − 4:
IF Severity is severe THEN Administer Emergency
Treatment (AET). The defuzzified decision is ob-
tained through the centroid method after applying
fuzzy rules and obtaining fuzzy outputs.
An example SPARQL query for generating per-
sonalized asthma recommendations based on specific
criteria and fuzzy properties is:
SELECT ?recommendation
WHERE {
?patient :hasSymptom ?symptom .
?symptom :Tiredness ?tiredness .
?symptom :Difficulty-in-Breathing ?breathing .
?symptom :Severity ?severity .
?patient :hasDemograph ?demo .
?demo :hasAge ?age .
FILTER (?tiredness ≥ 0.7 && ?breathing ≥ 0.5
&& ?age ≥ 18)
BIND (IF(?severity = :Severe, “AET”,
“IMD”) AS ?recommendation)
}
Patient data, including tiredness, breathing diffi-
culty, and severity, is filtered to identify adults with
high tiredness and moderate breathing difficulty. Rec-
ommendations for increasing medication or adminis-
tering emergency treatment are made based on fuzzy
rules and severity. The aggregated fuzzy output is
defuzzified using the centroid method to provide a
clear recommendation. For example, if a patient has
tiredness = High (0.8), DifficultyInBreathing = Mod-
erate (0.6), and Severity = Moderate (0.4), the sys-
tem generates a recommendation to ”Increase Med-
ication Dosage” based on Rule 3. If the centroid
value exceeds a threshold (e.g., 0.5), the recommen-
dation is confirmed. The implementation addresses
the research questions as follows: First, the seman-
tic knowledge graph, shown in Fig. 2, underpins the
FDSS for personalized asthma monitoring, efficiently
handling reasoning tasks with quick processing in
Prot
´
eg
´
e and Jena environments. Second, although
representing fuzzy knowledge in the FDSS is com-
plex, the ontology integrates fuzzy rules effectively,
enabling tailored recommendations based on proper-
ties like tiredness and breathing difficulty. Third, the
synergy between the knowledge base, crisp values,
and their fuzzy representations supports personalized
monitoring and decision-making. SPARQL queries
use criteria such as tiredness and breathing difficulty
to generate tailored recommendations, with defuzzi-
fication providing clear insights for asthma manage-
ment. Overall, the algorithm integrates patient data,
rule-based logic, and fuzzy ontology via SPARQL
queries to deliver customized asthma monitoring rec-
ommendations. In this context, fuzzy ontology sur-
passes general ontology by effectively capturing and
representing uncertainty and imprecision in patient
data, thus enhancing decision-making accuracy. It im-
proves personalized asthma monitoring by handling
uncertainty, offering flexibility, and integrating with
A Fuzzy Decision Support System with Semantic Knowledge Graph for Personalized Asthma Monitoring: A Conceptual Modeling
149

semantic web technologies. Fuzzy ontology-based
SPARQL enhances interpretability and adaptability,
though scalability issues may arise with growing data
volumes. Future research could integrate machine
learning models to address these scalability concerns
and improve predictive power and automatic feature
learning in the FDSS for asthma management.
4 CONCLUSION
The FDSS for personalized asthma monitoring lever-
ages semantic reasoning and fuzzy logic to enhance
asthma care. By using ontological representation,
fuzzy reasoning, and SPARQL queries, the FDSS of-
fers a flexible framework for personalized decision-
making, potentially improving treatment effective-
ness and patient quality of life. Future work should
focus on validating the FDSS’s effectiveness and
practicality in real-world healthcare settings.
REFERENCES
Ajami, H. (2022). First steps of asthma management
with a personalized ontology model. Future Internet,
14(7):190.
Al-Dowaihi, D. (2013). Mbreath: Asthma monitoring sys-
tem on the go. In 2013 International Conference on
Computer Medical Applications (ICCMA), pages 1–4.
IEEE.
Anantharam, P. (2015). Knowledge-driven personalized
contextual mhealth service for asthma management in
children. In 2015 IEEE international conference on
mobile services, pages 284–291. IEEE.
Chakraborty, A. (2023). Development of an iot-enabled
cost-effective asthma patient monitoring system: In-
tegrating health and indoor environment data with sta-
tistical analysis and data visualization. Internet of
Things, 24:100942.
Chakraverty, S. (2019). Defuzzification. Concepts of
Soft Computing: Fuzzy and ANN with Programming,
pages 117–127.
Chatterjee, A. (2021). An automatic ontology-based ap-
proach to support logical representation of observ-
able and measurable data for healthy lifestyle man-
agement: Proof-of-concept study. Journal of Medical
Internet Research, 23(4):e24656.
Chatterjee, A. (2022a). Hl7 fhir with snomed-ct to achieve
semantic and structural interoperability in personal
health data: a proof-of-concept study. Sensors,
22(10):3756.
Chatterjee, A. (2022b). Personalized recommendations
for physical activity e-coaching (ontorecomodel): on-
tological modeling. JMIR Medical Informatics,
10(6):e33847.
Cleveland Clinic (2023).
https://my.clevelandclinic.org/health/diseases/6424-
asthma.
Dataset (2024). https://www.kaggle.com/datasets/
deepayanthakur/asthma-disease-prediction.
Dieffenderfer, J. (2016). Low-power wearable systems for
continuous monitoring of environment and health for
chronic respiratory disease. IEEE journal of biomedi-
cal and health informatics, 20(5):1251–1264.
Dramburg, S., Marchante Fern
´
andez, M., Potapova, E., and
Matricardi, P. M. (2020). The potential of clinical de-
cision support systems for prevention, diagnosis, and
monitoring of allergic diseases. Frontiers in Immunol-
ogy, 11:575892.
Galante, C. M. (2022). Asthma management updates. Nurs-
ing2023, 52(2):25–34.
Gibson, P. G. (2000). Monitoring the patient with asthma:
an evidence-based approach. Journal of Allergy and
Clinical Immunology, 106(1):17–26.
Gyrard, A. (2018). Personalized health knowledge graph.
In CEUR workshop proceedings, volume 2317. NIH
Public Access.
Kang, H.-q. (2024). The experience of shared decision-
making for people with asthma: A systematic review
and metasynthesis of qualitative studies. Health Ex-
pectations, 27(2):e14039.
Merchant, R. (2018). Digital health intervention for asthma:
patient-reported value and usability. JMIR mHealth
and uHealth, 6(6):e7362.
Molfino, N. A. (2024). Machine learning approaches to pre-
dict asthma exacerbations: A narrative review. Ad-
vances in Therapy, 41(2):534–552.
Pinnock, H. (2015). Supported self-management for
asthma. Breathe, 11(2):98–109.
Quinde, M. (2018). Personalisation of context-aware so-
lutions supporting asthma management. In Comput-
ers Helping People with Special Needs: 16th Interna-
tional Conference, ICCHP 2018, Linz, Austria, July
11-13, 2018, Proceedings, Part II 16, pages 510–519.
Springer.
Ra, H.-K. (2016). Asthmaguide: an asthma monitoring
and advice ecosystem. In 2016 IEEE Wireless Health
(WH), pages 1–8. IEEE.
Vatsal, S. K. (2024). Advanced ensemble learning approach
for asthma prediction: Optimization and evaluation.
In 2024 International Conference on Automation and
Computation (AUTOCOM), pages 283–288. IEEE.
WHO (2019). https://www.who.int/news-room/fact-
sheets/detail/asthma.
Wieczorek, K. (2024). Acoustic biomarkers in asthma:
a systematic review. Journal of Asthma, (just-
accepted):1–18.
Wikstr
¨
om, R. (2014). Fuzzy ontology for knowledge mo-
bilisation and decision support. PhD thesis,
˚
Abo
Akademi-
˚
Abo Akademi University.
KEOD 2024 - 16th International Conference on Knowledge Engineering and Ontology Development
150
