
Evaluating Healthcare Automation: A Multi-Case Study on the
Utilization of Automation Initiatives in Healthcare Operations
Jani Kaitosalmi
a
and Milla Ratia
b
Department of Industrial Engineering and Management, Aalto University, Otakaari 1B, Espoo, Finland
Keywords: Healthcare Automation, Impact Assessment, Robotic Process Automation, Intelligent Automation.
Abstract: Automation technologies such as robotic process automation (RPA) and intelligent automation (IA) are
essential for managing rising healthcare costs and ensuring sustainable health services. Although these
solutions have been implemented in several Finnish healthcare organizations, their overall impact has not
been systematically evaluated. This research investigates the impact and evaluation of healthcare automation
through a multi-case study conducted in two Finnish healthcare organizations. While automation has
improved resource utilization, process efficiency, and standardization across units, the findings highlight the
need for a more comprehensive evaluation and continuous monitoring of automation benefits. Future research
should focus on developing a specific evaluation framework tailored to healthcare automation technologies.
The adoption of holistic evaluation methods could allow healthcare organizations to better understand the
impact of automation and further enhance operational efficiency and patient care.
1 INTRODUCTION
Mestres (2017) posits that healthcare faces three key
challenges: rising costs, a decrease in available
physicians, and an increase in patients. Similar trends
are noted in Finland, with increasing healthcare costs
and declining availability of personnel (Kirkonpelto,
Mäntyranta, et al., 2023). Digitalization offers
solutions by improving productivity, transforming
care delivery, and simplifying administration (Sony,
Antony & Tortorella, 2023). Although digitalization
can help healthcare organizations meet their
objectives, the outcomes of digital interventions often
take time to materialize and can be challenging to
measure (Cresswell, 2023).
This paper focuses on one specific avenue of
digitalization in healthcare – the impact of automating
digital workflows. Automation initiatives can deliver
a wide range of benefits to healthcare organizations
through cost savings, standardized and always-
available processes, and freeing employees from
repetitive manual tasks (Kedziora and Smolander,
2022; Ratia et al., 2021; Kedziora and Kiviranta,
2018).
Although automation solutions are recognized for
their potential, it remains unclear how these back-
a
https://orcid.org/0009-0009-1800-5137
b
https://orcid.org/0000-0002-3360-9555
office solutions generate value in the public
healthcare sector (Ratia et al., 2021). In particular,
there is a lack of relevant research on the impact
assessment of automation (Meironke and Kuehnel,
2022), with discussions being "ad-hoc and scattered,
with minimal empirical and theoretical support"
(Denagama Vitharanage et al., 2020). The research on
automation solutions often focuses on the technical
dimensions, giving less emphasis on the benefits and
value creation (Ratia et al., 2021). Various patient-
centric attempts have been made to create an overall
impact assessment framework for digitalization
efforts (e.g. WHO, 2016; Lillrank et al., 2019;
Parviainen et al., 2017; Karunasena & Deng, 2012).
However, research on automated back-office
solutions that do not directly affect patient outcomes
has been more limited. Especially in the Finnish
public sector, systematic evaluations of automation
technologies are limited (Kääriäinen et al., 2018).
This research aims to examine the outcomes of
automation solutions in healthcare and provide
information on how their impact can be measured.
The study focuses on two methods: robotic process
automation (RPA) and intelligent automation (IA),
applied within two Finnish public healthcare districts:
The Wellbeing Services County of Pirkanmaa
246
Kaitosalmi, J. and Ratia, M.
Evaluating Healthcare Automation: A Multi-Case Study on the Utilization of Automation Initiatives in Healthcare Operations.
DOI: 10.5220/0012947100003838
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 16th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2024) - Volume 3: KMIS, pages 246-255
ISBN: 978-989-758-716-0; ISSN: 2184-3228
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.

(PIRHA) and the Helsinki and Uusimaa Hospital
District (HUS). Although both healthcare
organizations had implemented various automation
tools, they had not fully assessed the overall impact
of these solutions. The objective of this paper is two-
fold: to identify key automation benefits and potential
risks and to provide information on what should be
considered when evaluating automation outcomes.
The research questions are the following:
RQ1. What are the benefits and risks of
utilizing automation solutions in healthcare?
RQ2. What should be considered when
evaluating automation in healthcare?
2 BACKGROUND LITERATURE
2.1 Utilizing Automation to Enhance
Healthcare Operational Processes
Workflow automation, which involves identifying
sequences of tasks that can be streamlined with digital
tools, provides opportunities to address process
inefficiencies in healthcare (Zayas-Cabán, Okubo, &
Posnack, 2023). Automating simple workflows is
needed in healthcare, where professionals are
burdened by repetitive administrative duties like data
entry, documentation, and scheduling – tasks that
often distract from patient care. Automation
technologies can take over these routine tasks,
allowing healthcare providers to dedicate more time
to meaningful patient interactions. (Mohamed &
Frank, 2022.)
Often automating business processes require the
use of application programming interfaces (API) to
connect with legacy systems (Herm et al., 2023; Syed
et al., 2020). However, such solutions are not always
feasible in healthcare due to technical constraints,
legacy systems, or vendor limitations. In these cases,
lightweight and non-invasive automation solutions,
such as RPA and IA, can present an opportunity to
improve operational processes across care delivery
and administration (Ferris, Ackers & Borhani, 2022;
Zayas-Caban, Okubo & Posnack, 2023).
RPA automates repetitive digital tasks typically
performed by humans (Ivančić, Suša Vugec, and
Bosilj Vukšić, 2019; Kääriäinen et al., 2018;
Willcocks, Lacity, and Craig, 2015; Ratia et al.,
2021). These robots mimic human actions on system
interfaces (Herm et al., 2023). Due to its low cost,
quick implementation, and minimal system changes,
RPA is attractive for healthcare providers struggling
with system integration (Ratia et al., 2021;
Osmundsen et al., 2019; Kedziora & Kiviranta,
2018).
RPA is effective in automating routine processes,
such as physician credentialing, patient scheduling,
and billing (Jain and Bhatnagar, 2019). For example,
during COVID-19, RPA accelerated diagnoses,
distributed targeted health information, and updated
quarantine data (Doğuç, 2021). In Finland, RPA was
used to process up to 2,000 COVID-19 vaccinations
daily, a task previously done by 10-15 employees
(Adolfsson, 2021). Similarly, in HUS, RPA saved
over 13,000 workdays in 2021, equivalent to the work
of 65 full-time employees (HUS, 2021).
While RPA is a powerful tool, its applications are
primarily limited to tasks that are highly rule-based,
structured, standardized, and supported by well-
documented decision logic (Ng, 2021). IA enhances
RPA with AI features such as machine learning and
natural language processing to replicate human
cognitive skills (Kedziora and Hyrynsalmi, 2023;
Coombs et al., 2020). With these capabilities, IA can
handle unstructured data, make real-time decisions,
and perform content-aware computing, overcoming
many limitations of RPA (Ng et al., 2021).
IA can assist in complex scheduling, capacity
management, and process optimization in operating
rooms and emergency departments by managing
patient movement between diagnostics and wards
(Garcia et al., 2020). Additionally, IA can coordinate
patient information, issue health risk alerts, predict
health outcomes, and optimize logistics processes
(Secinaro et al., 2021). However, IA research is still
in its early stages with challenges and potential
applications yet to be fully explored (Ng, 2021).
2.2 Impact Evaluation of Automation
Initiatives
Porter (2013) defines healthcare value as
“maximizing value for patients,” meaning achieving
the best outcomes at the lowest cost. In other words,
healthcare value = patient outcomes / total costs.
Specifically, Porter (2014) argues that while process
measurement and improvements are valuable tactics,
they cannot replace the importance of measuring the
results of care. Thus, healthcare value is the result of
care, not the volume of services delivered. What is
then the impact of back-office automation solutions
that do not directly affect patient outcomes?
To measure the overall healthcare outcomes, the
primary metric used is effectiveness, which refers to
the impact of treatment on the health conditions of a
population under routine conditions (Ikonen, 2019;
Pitkänen et al., 2018). From effectiveness, several
Evaluating Healthcare Automation: A Multi-Case Study on the Utilization of Automation Initiatives in Healthcare Operations
247

other important metrics are derived, such as cost-
effectiveness, which evaluates the ratio of
effectiveness to costs, and productivity, which is the
ratio of output (the result of an operation) to input (the
resources or costs used to achieve that output)
(Sintonen et al., 2021). Productivity can be enhanced
by either reducing costs while keeping the output
constant or by increasing output while maintaining
the same costs. Consequently, improving
productivity also enhances the cost-effectiveness of
healthcare processes (Sintonen et al., 2021).
Automation is often implemented to improve
cost-effectiveness by enhancing productivity.
Automation benefits can be tangible, like reduced
costs and faster processing, or intangible, such as
better customer satisfaction and employee
motivation. Evaluating both types separately is
crucial since not all benefits, like financial gains, are
easily measurable (Axmann and Harmoko, 2021).
While the automation benefits are recognized,
their impact assessment is still lacking (Meironke &
Kuehnel, 2022; Kääriäinen et al., 2018). According to
Kääriäinen et al. (2018), organizations tend to assess
automation mainly using a narrow set of criteria, with
a focus on internal savings. Many of the assessment
frameworks focus on the requirements, feasibility,
and readiness of a company to implement new
technology, such as the 5D digital technology
assessment (Axmann and Harmoko, 2021), RPA
selection indicators by Kim (2023), or the method for
RPA process selection proposed by Wanner et al.
(2019). However, they do not consider how to
conduct continuous monitoring and evaluate the
impact after the implementation.
Moreover, Meironke and Kuehnel (2022)
identified 62 unique metrics in the literature to
evaluate the benefits of automation. Most of these
metrics focus on efficiency and costs, emphasizing
the number of transactions, work hours saved, and
process time. Accuracy or error rates are also
commonly used to measure quality and compliance
benefits. On the other hand, metrics related to
implementation effort, employee and customer
satisfaction, availability, and interoperability are less
commonly found. Thus, the authors conclude that the
assessment of automation benefits “shows a
tendency” to prioritize quantifiable economic metrics
over qualitative and non-economic ones. (Meironke
and Kuehnel, 2022.)
3 METHODOLOGY
This research aims to provide insights into evaluating
automation outcomes. To address the research
questions, the study has focused on the benefits, risks,
and evaluation challenges of automation in two
Finnish healthcare districts: PIRHA and HUS.
The research was conducted as a multi-case
qualitative study. This study employed a qualitative
design to explore a relatively novel topic, which is
ideal for gaining an in-depth understanding of
phenomena within specific contexts when little is
known about a topic (Saunders et al., 2019; Antwi &
Hamza, 2015). Moreover, the research employed an
embedded multi-case study design; it contained more
than one sub-unit of analysis to conduct an in-depth
examination of a current phenomenon (the ‘case’)
within its real-life setting (Yin, 2018). The method
allowed to investigate stakeholders' experiences with
various automation implementations across multiple
units. The two case organizations were ideal for the
study due to their size and previous experience with
multiple automation projects. Furthermore, while
both healthcare organizations had implemented
various automation solutions, they had not fully
assessed their overall impact.
3.1 Data Collection
The empirical data was gathered through 32 semi-
structured interviews with employees, administrative
staff, and stakeholders in PIRHA and HUS
experienced with RPA and IA. Participants included
department secretaries, nurses, doctors, pharmacists,
digitalization experts, and head physicians. External
IT companies providing automation solutions were
also interviewed to capture their perspectives. Table
1 lists all participants.
The interview data was gathered in two phases:
from PIRHA in Spring 2023 and HUS in Autumn
2023. PIRHA interviews focused on RPA solutions,
while HUS interviews covered IA processes.
Purposive sampling was used, meaning the
participants were selected based on characteristics
that matched the research objectives (Andrade, 2021;
Etikan et al., 2016). Specifically, participants had
prior experience with automation and represented a
diverse set of roles. The research team provided
preferences for roles and units but had limited control
over participant selection. Due to the policies of both
organizations, the final participant selection was
made within a tight timeframe by a designated contact
person. Consequently, convenience and availability
also played a significant role in recruitment.
KMIS 2024 - 16th International Conference on Knowledge Management and Information Systems
248
All interviews followed a similar structure and
were conducted remotely via Microsoft Teams.
Participants discussed automation benefits and risks
from the perspectives of employees, patients, costs,
and processes and shared their views on impact
assessment. The interviews were recorded,
transcribed, and pseudonymized with participants'
permission before analysis.
While the interviewees discussed several
automated processes, the primary focus was on two
processes: referral handling and medical dosage
building. Both organizations had implemented a
referral sorter to shift manual work from nurses and
department secretaries. “Before automation or the
electronic patient record system's XDS archive, the
paper referrals arriving at the unit were placed on the
doctor’s desk,” as one secretary from HUS describes
it (Ahlskog, 2022). Now, the robot continuously
processes new doctors' referral texts in a virtual
referral center. It categorizes them into the correct
queues, where doctors can access and review the
referrals for further evaluation. In PIRHA, the RPA-
based solution uses predefined logic to automate
repetitive referral handling. However, if the robot
misplaces a referral, an employee must correct it.
Moreover, HUS has enhanced the referral sorter with
AI, using machine learning to interpret symptoms and
diagnoses from referral texts.
HUS has also an automation solution for filling
patients' dosage information in the electronic health
record system, Apotti. This medical dosage builder,
used by nurses and pharmacists, transforms free-text
medication info into the required structured format. It
provides code suggestions, reducing the need for
manual entry of the patient’s medication list. The
structured medical information is standardized data
that is used to generate dosage instructions with a
similar structure for all patients, reducing the need for
manual input and minimizing errors.
3.2 Data Analysis
Data analysis was conducted using qualitative content
analysis with the QDA software ATLAS.ti. The study
followed a directed content analysis approach
presented by Hsieh and Shannon (2005), starting with
relevant research findings and preliminary theory-
based categories for automation benefits and risks.
The empirical data consisted of two datasets, one for
each case, with data collection divided among the
researchers. Consequently, none of the researchers
participated in all interviews, resulting in a final
dataset that was a mix of primary and secondary data
for all researchers.
Given the mix of primary and secondary data, the
study employed tactics for an abductive content
analysis as outlined by Vila-Henninger et al. (2024).
Firstly, a deductive theory-based codebook was
created and expanded with inductive codes. For
instance, in this step, the benefit dimensions provided
by Meironke and Kuehnel (2022) were utilized to
categorize the benefits. The “AI coding” feature of
ATLAS.ti was also used for exploratory coding.
Secondly, to reduce data volume, codes were
combined into broader categories. Here, the ‘Query
Tool’ was used to sort codes based on the four
perspectives that were investigated. Finally, a
detailed manual qualitative analysis was performed to
identify emerging themes and compare differences
between the two cases.
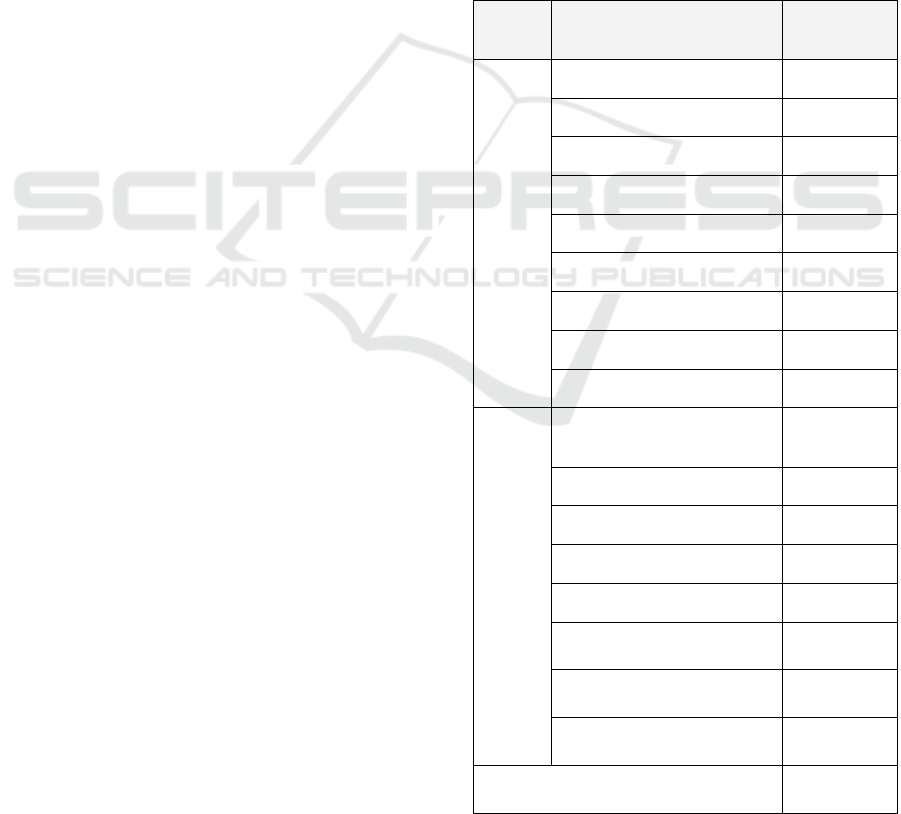
Table 1: Participant list from PIRHA and HUS.
Region Role
Number of
p
artici
p
ants
PIRHA
Department Secretar
y
5
Nurse 2
Chief Physician / Directo
r
2
Medical Docto
r
2
Digitalization Specialist 2
Head / De
p
ut
y
Head Nurse 2
Product Owner (External) 1
Midwife 1
Service Provider (External) 1
HUS
Pharmacist / Senior
Pharmacist
5
Di
g
italization S
p
ecialist 2
Department Secretar
y
2
Nurse 1
Product Owne
r
1
Deputy Chief Physician 1
Product Owner (External) 1
Data Scientist (External) 1
Total 32
Evaluating Healthcare Automation: A Multi-Case Study on the Utilization of Automation Initiatives in Healthcare Operations
249

4 FINDINGS
4.1 Perceived Benefits
The thematic interviews in both healthcare counties
expressed that the overall perception of automation
has been positive. The most mentioned direct benefits
were related to process efficiency, improved resource
utilization, and availability of services.
In HUS, one external expert describes that the
referral processing time has decreased significantly,
from 32-35 hours to approximately 3-4 hours.
However, while quicker referral handling provides
information to patients faster, it doesn't necessarily
lead to faster treatment. More precisely, participants
describe that the referral sorter has merely moved the
bottleneck from the referral handling to the next step
of the patient journey. Thus, speeding up one part of
the process does not necessarily reduce overall
treatment time. However, faster referral handling can
be impactful for urgent patients. Participants describe
how automation robots process urgent cases faster
and thus increase the accessibility to treatment: “For
urgent referrals that take 1-7 days, it makes a
significant difference if they can be processed in 2-4
hours instead of five working days.”
While interviewees often mention time savings,
they struggle to pinpoint where the extra time goes.
Nurses and pharmacists note a slight increase in
patient care time, which enhances the overall quality
of the patient experience. However, these time
savings per patient inquiry are deemed small and hard
to measure. In HUS, doctors have faced additional
workload from the referral sorter, as incorrect
referrals have been directed to them. On the contrary,
in PIRHA, the effect has been more moderate. For
secretaries, the possible benefits seem most direct, as
they have more time for more challenging
administrative tasks, such as appointment scheduling
and other phone-related work.
Moreover, participants in HUS described that IA
solutions has created standardization across the
organization. Before automation, there were large
variations in how medication lists were written. As
automation requires rule-based inputs, it has
standardized the medical information, leading to
consistent interpretations across the organization.
“The fact that information is the same for all users.
Perhaps that’s the best benefit here. It also guides us
in standardizing practices across different areas of
healthcare,” describes one pharmacist. “This is a
massive organization, and with automation, we have
achieved greater unity across specialties,”
summarizes another participant.
Other process-related benefits were related to
compliance and interoperability. The solutions have
helped to meet reporting requirements and facilitated
data and system linkage. “The smoother we can make
reporting, the better,” describes one participant.
“From the perspective of organizational
development, it supports knowledge management,”
continues another interviewee. Moreover, while
automation robots act fast, they also handle
information without biases, positively impacting
equal access to treatment. “It’s not affected by
whether someone is in a bad mood, had a rough
morning, or is running late for work. Automation is
consistent; it doesn’t get tired or have biases.”
Automation solutions have also created indirect
benefits in both organizations, such as enhanced
employee and patient experience. The participants
describe that automation can help “find meaningful
job roles” and provide time for “brain-intensive work
that professionals are trained for.”
While cost savings are discussed, the perception
of it varies across units and roles. The digitalization
experts highlight the fast payback time and scalability
of automation solutions. “The time savings
accumulate when creating such easily scalable
processes. There are no additional costs with
expansion,” describes one digitalization expert. On
the contrary, nurses and secretaries find it hard to
evaluate cost savings, one reason being that some of
the potential saved time goes to monitoring and
correcting the results: “Any freed-up time currently
goes into fixing and monitoring the results. However,
in the long term, when hopefully everything is running
smoothly, I would see cost savings occurring,”
Lastly, participants note that patients likely don't
notice automation since it works in the background.
However, automation has positively impacted
patients in various ways, such as delivering treatment
information faster and allowing doctors more time for
patient care.
4.2 Recognized Risks
In both cases, the two main recognized potential risks
of automation were additional work created by
technical errors and decreased process quality. The
risk of additional work appears to be significantly
higher during what participants describe as the
“infancy stage,” meaning the early stages of
development. PIRHA reported significantly more
issues with its early-stage RPA solutions than HUS,
which had both more experience and more advanced
automation solutions implemented.
KMIS 2024 - 16th International Conference on Knowledge Management and Information Systems
250
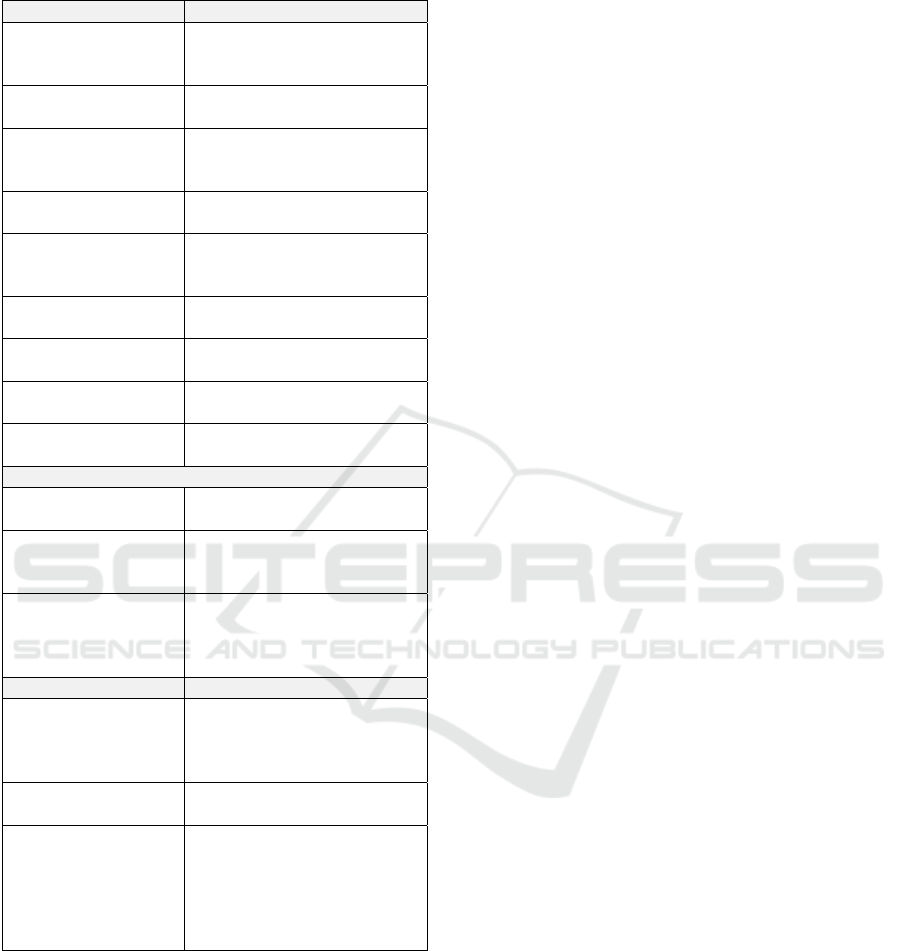
Table 2: An overview of the perceived main benefits and
risks in HUS and PIRHA.
Direct benefits Description
Process efficiency
Increase in volumes and
decrease in throughput times
and delays.
24/7 availability
The robots are always
available to work.
Increased resource
utilization
Time savings enable
employees to complete more
complex tasks.
Standardization
Automation provides similar
out
p
uts across units.
Faster access to
treatment (urgent
cases)
Automation can prioritize
urgent cases.
Compliance
Helps to meet reporting
re
q
uirements.
Interoperability
Easier data and system
linkage.
Scalability
The solutions are fast and
cheap to scale across units.
Equal access to
treatment
Robots handle information
without biases.
Indirect benefits
Increased employee
ex
p
erience
Increased job satisfaction and
meanin
g
fulness of work.
Increased patient
experience
Provides information faster to
the patient and can speed up
treatment visits.
Cost-effectiveness
Increase in the value of time
gains (difference in cost of
process by a human vs
automation
)
Potential risks
Additional work
Automation solutions are not
error-free. The risk of
additional work is higher
durin
g
the "infanc
y
sta
g
e."
Decrease in quality
Humans perform tasks more
accurately than robots.
Risks in patient safety
Automation faces challenges
in interpreting complex data.
Outputs involving critical
patient information still need
to be reviewed by a
p
rofessional.
While additional work is a risk, it also matters to
whom and how much of it is created. In PIRHA, most
of the additional work was targeted to secretaries and
nurses, some of whom felt that “it has consumed work
hours and taken away time from patient care.” The
participants in PIRHA describe that the RPA robot
should be able to handle 50 percent of the referrals to
be beneficial. For example, one participant noted a
success rate of only 27 percent during a two-week test
period. Some other interviewed secretaries and nurses
share similar experiences of automation feeling like
an “additional burden.” “There is still a substantial
amount of manual checking required. In the last
report, more than 3/4 of cases had errors,” describes,
for example, another participant. In HUS, while the
intelligent referral sorter appears to be more effective
than the regular RPA solution in PIRHA, it has also
created some extra work for the doctors. However, on
the organizational level, the overall effect has been
positive: “The doctors don’t see the advantage yet in
the referral handling work. However, when I try to
consider it from the perspective of the clinic’s
operation, I see that it creates a positive impact”,
describes one participant in HUS.
While automation increases quantity, it does not
necessarily increase quality. Participants underline
that humans still perform tasks with higher accuracy
than robots. Thus, there appears to be a trade-off
between quality and efficiency: “I don’t believe it has
improved quality. But it has shifted mechanical work
away from humans,” concludes one doctor. “The
process is less precise; errors occur more frequently
than with a human. However, the robot performs
faster and around the clock. That’s the trade-off,”
continues one external expert.
Lastly, interpreting data with changing inputs
appears to be challenging. Several participants
described that the dosage builder struggles with
situations where the medication dosage changes
within a time period. “Often if there is a variable
dosage, like one tablet in the morning and two in the
evening… It cannot handle such situations properly,
so it just makes a guess,” describes one pharmacist.
Thus, to maintain patient safety, the outputs need to
be verified carefully by a professional. Moreover, the
referral sorter in both case organizations has had
issues interpreting complex data, for instance,
sending the patient to a clinic outside their regular
municipality.
4.3 Challenges Measuring the Impact
of Automation
Measuring the impact of automation initiatives is
perceived hard in both case organizations. The main
assessment challenges relate to a lack of holistic data,
baseline measurements, targets, and a regular
evaluation process.
Active evaluation and monitoring have been
missing from many implementations in both
organizations. “Not in any way, at least not in our
unit,” is how one participant describes the current
state. “I don’t know if there’s any monitoring at the
Evaluating Healthcare Automation: A Multi-Case Study on the Utilization of Automation Initiatives in Healthcare Operations
251

PIRHA level, but at the unit level, there isn’t,”
continues another employee.
The assessment has mainly focused on whether
the technology works as intended, not on how people
interact with it or how it improves outcomes: “We
have tried to gather genuine user feedback, but it has
not been very successful. Essentially, what we
document is the result of encountering bugs."
Evaluating the impact of automation is also
challenging because it's “just a small part of it all,”
making it unclear which outcomes are directly caused
by automation. Feedback has mostly been technical
error reports: “We get these cold reports that tell us
how many times the robot has run and how many
cases there are per month or week.”
Interviewees in both organizations note that
evaluating progress is difficult without a baseline for
comparison. “We didn’t do measurements before the
start of this referral processing, such as how much
time we spend now and how much we used to spend.
Therefore, it’s a bit challenging to assess time
savings,” describes one secretary. In some cases,
potential benefits have been calculated in advance
without collecting data afterward. We haven’t had
any active monitoring. It’s been more like we’ve
calculated in advance the potential benefit and how
quickly the process would pay for itself,” summarizes
one digitalization expert.
While participants acknowledge the time savings,
it seems unclear how the saved time is utilized. “What
would interest me is somehow measuring how the
saved work time is being used. Whether it means
being able to serve one more patient or making more
phone calls,” describes one digitalization expert.
Measuring time savings appears challenging because
automation replaces only small specific tasks, not
entire workflows. “Measuring how much time
various small tasks take is always challenging," as
one digitalization expert describes. Secondly,
assessment efforts would require an additional layer
of monitoring, which would be difficult both
technically and due to possible resistance: “Adding
extra monitoring to the busy daily work might not be
the most effective solution."
In some units, monitoring is seen as a sensitive
issue. The work culture in these units seems to affect
how openly the benefits of automation are discussed:
“If you have a difficult work atmosphere, you don’t
go tell your boss you have more bandwidth. You enjoy
the fact that you have more space to do things. You
don’t report that you saved another 5 hours of work
time this week,” as one participant describes.
However, collecting impact data could help in
motivating employees to use the solutions: It would
likely turn even sceptical individuals towards a more
positive outlook.
4.4 Evaluation Metrics
Process metrics like time savings, throughput
volumes, and error rates are frequently mentioned,
especially those affecting treatment delivery, such as
handled referrals for urgent patients. At HUS, greater
emphasis is placed on qualitative metrics like worker
wellbeing and satisfaction, reflecting their more
mature solutions. In contrast, PIRHA focuses more on
technical aspects, as their solutions are in earlier
stages of development.
Back-office automation benefits patients
indirectly, such as faster referral processing or clearer
prescription instructions. Key metrics from the
patient’s perspective include patient safety,
satisfaction, treatment efficiency, and service
accessibility. Pharmacists and nurses using the
medical dosage builder particularly emphasize
patient safety as a crucial metric. Regarding the
referral sorter, the main patient risk is treatment
delays due to incorrect classification: “The biggest
risk we've identified is a delay in treatment due to
incorrect classification. However, the risk is very low,
and the consequences should not be significant.”
Measuring cost efficiency appears challenging,
particularly due to difficulties in quantifying time
savings. Cost savings may differ across units
depending on whose tasks are automated. For
instance, automating a doctor's tasks is more valuable
than a secretary's. However, organizations can
estimate time gains by "converting the saved time into
work hours and the hourly rate,” as one participant
summarizes. Additionally, automation enhances
organizational capabilities by increasing
standardization and simplifying scalability. This
organizational impact could be measured by metrics
like the number of standardized processes, speed of
implementation, and the number of employees
trained in automation.
5 DISCUSSION
The results emphasize the need for an impact
assessment model, as no proper "template or tool"
exists. Despite some used metrics, employees found
the value of implemented solutions unclear: “The
robot works well, but very few feel it’s needed in their
process.” In some cases, not seeing the benefits has
also caused resistance to adoption: “Some employees
KMIS 2024 - 16th International Conference on Knowledge Management and Information Systems
252

feel that they don’t want to adopt automation because
they perceive it as an additional burden.”
Based on both PIRHA and HUS interviews,
evaluation has been inadequate because a process has
not been built around it. Essentially, assessing digital
transformation should answer two questions: is the
project doing things right and is the project doing the
right things (Pritchett et al., 2013)
More concretely, impact assessment includes two
steps: monitoring implementation activities and
evaluating the monitored outcomes. Monitoring,
which refers to routine data collection, review, and
analysis, is the most time-consuming part of the
process (WHO, 2016). Evaluation, the systematic and
objective assessment of the implemented solutions, is
only the final step in determining whether objectives
have been met and the impact has been achieved
(WHO, 2016). In other words, evaluation aims to
determine whether changes in the monitored metrics
are the result of the digital intervention.
The findings from the two case organizations
emphasize six key steps in impact assessment: 1)
defining clear objectives, 2) choosing suitable
metrics, 3) setting baselines and targets, 4)
implementing monitoring mechanisms, 5) gathering
feedback, and 6) conducting regular evaluations.
Firstly, when setting goals, it is essential to
consider both the potential direct and indirect benefits
of automation. In HUS and PIRHA, the primary
advantages include operational efficiencies such as
time savings and productivity boosts, while indirect
benefits include reduced costs, improved
transparency, and enhanced experiences for patients
and employees. Automation outcomes that improve
the health system's effectiveness are mostly indirect
second-order effects, such as freeing up time for
patient interaction or more complex administrative
work.
The maturity of the solution should also be
considered for in the evaluation (WHO, 2016). In
other words, consider if the automation solution is
developed and evaluated for the first time or if it is
undergoing scale-up. For instance, PIRHA’s newer
RPA solutions had more errors than HUS's mature
systems, which requires evaluating them differently
depending on their development stage.
Moreover, not all metrics are relevant to every
context. More specifically, the impact can vary based
on the context in which they are implemented. Thus,
a full acknowledgment of the different perspectives
and boundaries is necessary (Williams 2015). More
precisely, organizations must broadly consider their
specific stakeholders’ perspectives: what goals are
relevant for whom and what is needed to measure.
Automation goals may not be achieved if
stakeholders are not engaged in setting the objectives
(Zayas-Caban et al., 2021).
Baseline measurements are essential for setting
realistic targets. Both PIRHA and HUS faced
challenges due to a lack of baseline data, as no initial
measurements were taken before implementation.
Inconsistent monitoring was also a major obstacle.
While technical data was collected, qualitative
insights have been lacking. Employees stressed the
need for gathering feedback to fully understand
automation's impact. Collecting feedback is
important, as unanswered quality or safety concerns
can undermine the long-term success of automation
initiatives (Zayas-Caban et al., 2021).
Lastly, evaluation should occur regularly and be
based on evidence collected at across multiple time
points (WHO, 2016). While interviews identified cost
efficiency and resource utilization as key factors for
evaluation, both organizations would benefit from
considering other dimensions. Similarly, Axmann
and Harmoko (2024) argue that traditional cost-
benefit analysis overlooks many automation benefits,
possibly leading to poor decisions. They propose a
balanced scorecard (BSC) framework to evaluate
RPA projects, categorizing benefits into four areas:
financial, process improvement, customer
satisfaction, and learning. With adjustments, the
model could potentially be applied to healthcare. The
BSC, originally developed by Kaplan and Norton
(1992), has already been used in healthcare, both with
original and modified perspectives (Amer et al., 2022;
Betto et al., 2022). Further research is needed to
determine whether BSC framework could effectively
evaluate healthcare automation outcomes.
6 CONCLUSIONS
This research explored the impact of automation
solutions in two Finnish healthcare districts,
providing insights into the benefits, risks, and
evaluation of automation initiatives in healthcare.
However, several limitations must be acknowledged.
Firstly, this study focused only on two regions with
varying levels of automation maturity, which may
limit the generalizability of the findings to other
healthcare environments. Additionally, the research
primarily gathered insights from employees familiar
with automation without including patients. Although
participants were asked to reflect on the impact of
automation on patients, no direct feedback was
collected from patients themselves.
Evaluating Healthcare Automation: A Multi-Case Study on the Utilization of Automation Initiatives in Healthcare Operations
253

The findings contribute to future research on
developing an impact assessment framework that
could help healthcare organizations better understand
and enhance the use of automation. Future research
should explore whether successful evaluation
frameworks from other industries can be adapted for
the healthcare sector.
REFERENCES
Adolfsson, F. (2021). Västerbotten sparar 100 000 timmar
med RPA. Voister.
Ahlskog, B. (2022). Ohjelmistorobotit ja tekoäly
lähetekäsittelyn apuna. Husari, 4/2022.
Amer, F., Hammoud, S., Khatatbeh, H., Lohner, S., Boncz,
I., & Endrei, D. (2022). A systematic review: the
dimensions to evaluate health care performance and an
implication during the pandemic. BMC Health Services
Research, 22(1), 621.
Antwi, S. K., & Hamza, K. (2015). Qualitative and
quantitative research paradigms in business research: A
philosophical reflection. European journal of business
and management, 7(3), 217-225.
Andrade C. (2021). The Inconvenient Truth About
Convenience and Purposive Samples. Indian journal of
psychological medicine, 43(1), 86–88.
Axmann, B., & Harmoko, H. (2021). The five dimensions
of digital technology assessment with the focus on
robotic process automation (RPA). Tehnički glasnik,
15(2), 267-274.
Betto, F., Sardi, A., Garengo, P., & Sorano, E. (2022). The
evolution of balanced scorecard in healthcare: A
systematic review of its design, implementation, use,
and review. International Journal of Environmental
Research and Public Health, 19(16), 10291.
Coombs, C., Hislop, D., Taneva, S. K., & Barnard, S.
(2020). The strategic impacts of Intelligent Automation
for knowledge and service work: An interdisciplinary
review. The Journal of Strategic Information Systems,
29(4), 101600.
Cresswell, K., Anderson, S., Montgomery, C., Weir, C. J.,
Atter, M., & Williams, R. (2023). Evaluation of
Digitalisation in Healthcare and the Quantification of
the “Unmeasurable.” Journal of General Internal
Medicine, 38(16), 3610-3615.
Denagama, V., Manuraji, I., Bandara, W., Syed, R., &
Toman, D. (2020). An empirically supported
conceptualisation of robotic process automation (RPA)
benefits. Association for Information System,
Marrakech.
Doğuç, Özge (2021). “Robotic process automation (RPA)
applications in COVID-19”. In: Dincer, H. & Yüksel,
S. (Eds.) Management Strategies to Survive in a
Competitive Environment: How to Improve Company
Performance (pp. 233–247). Springer.
Etikan, I., Musa, S. A., & Alkassim, R. S. (2016).
Comparison of convenience sampling and purposive
sampling. American journal of theoretical and applied
statistics, 5(1), 1-4.
Ferris, T., Ackers, J., and Borhani, M. (2022). RPA in the
NHS: Guidance for designing, delivering and
sustaining RPA within the NHS. May. NHS.
Garcia, J.F, Spatharou, A., Hieronimus, S., Beck, J.P., and
Jenkins, J. (2020). Transforming healthcare with AI.
McKinsey & Company: Our Insights.
Herm, L. V., Janiesch, C., Helm, A., Imgrund, F., Hofmann,
A., & Winkelmann, A. (2023). A framework for
implementing robotic process automation
projects. Information Systems and e-Business
Management, 21(1), 1-35.
Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to
qualitative content analysis. Qualitative health
research, 15(9), 1277-1288.
HUS (2021). Tarkastuslautakunnan arviointikertomus 2021
Helsingin ja Uudenmaan sairaanhoitopiirin
valtuustolle. April. HUS.
Ikonen, T (2019). Asiakasryhmäkohtainen tieto laadusta ja
vaikuttavuudesta sosiaali- ja terveydenhuollon tiedolla
johtamisessa ja ohjauksessa. Sosiaali-ja
terveysministeriön raportteja ja muistioita, 70.
Ivančić, L., Suša Vugec, D., & Bosilj Vukšić, V. (2019).
Robotic process automation: systematic literature
review. In Business Process Management: Blockchain
and Central and Eastern Europe Forum: BPM 2019
Blockchain and CEE Forum, Vienna, Austria,
September 1–6, 2019, Proceedings 17 (pp. 280-295).
Springer International Publishing.
Jain, R and R Bhatnagar (2019). Robotic process
automation in healthcare- a review. International
Robotics & Automation Journal 5(1), 12–14.
Kääriäinen, J., Aihkisalo, T., Halén, M., Holmström, H.,
Jurmu, P., Matinmikko, T., Seppälä, T., Tihinen, M.,
and Tirronen, J., (2018). Ohjelmistorobotiikka ja
tekoäly–soveltamisen askelmerkkejä. Valtioneuvoston
selvitys- ja tutkimustoiminnan julkaisusarja, 65/2018.
Kaplan, R. S. (1992). The Balanced Scorecard-Measures
That Drive Performance. Harvard Business Review.
Karunasena, K., & Deng, H. (2012). Critical factors for
evaluating the public value of e-government in Sri
Lanka. Government information quarterly, 29(1), 76-
84.
Kedziora, D., and Smolander, K., 2022: Responding to
Healthcare Emergency Outbreak of COVID-19
Pandemic with Robotic Process Automation (RPA),
Proceedings of the 55th Hawaii International
Conference on System Sciences, 6207-6216
Kedziora, D., & Hyrynsalmi, S. (2023, May). Turning
robotic process automation onto intelligent automation
with machine learning. Proceedings of the 11th
International Conference on Communities and
Technologies, 1-5
Kedziora, D., & Kiviranta, H. (2018). Digital Business
Value Creation with Robotic Process Automation (rpa)
in Northern and Central Europe. Management
(18544223), 13(2), 64- 174.
KMIS 2024 - 16th International Conference on Knowledge Management and Information Systems
254

Kim, S.H., (2023). Development of Evaluation Criteria for
Robotic Process Automation (RPA) Solution Selection.
Electronics 12(4), 986.
Lillrank, P., Tenhunen, H., Hörhammer, I., Halminen, O.,
Lyly, T., Linna, M., Silander, K., Laurila, R., Hiltunen,
A-M, Riikonen, E., Miettinen, S., Tanila, T., Chen, A.
& Vesinurm, M. (2019). Terveydenhuollon
digitaalisten ratkaisujen vaikuttavuuden osoittaminen.
HEMA-instituutti.
Meironke, A., & Kuehnel, S. (2022). How to measure
RPA’s benefits. A review on metrics, indicators, and
evaluation methods of RPA benefit assessment. 17th
International Conference on Wirtschaftsinformatik.
Mestres, J. C. (2017). State of the art of health care: The
cubism period. The digitization of healthcare: New
challenges and opportunities, 3-21.
Ng, K. K., Chen, C. H., Lee, C. K., Jiao, J. R., & Yang, Z.
X. (2021). A systematic literature review on intelligent
automation: Aligning concepts from theory, practice,
and future perspectives. Advanced Engineering
Informatics, 47 (101246).
Osmundsen, K., Iden, O. and Bygstad, B. (2019).
Organizing Robotic Process Automation: Balancing
Loose and Tight Coupling. Proceedings of the 52nd
Hawaii International Conference on System Sciences
2019. 6918-6926.
Parviainen, P., Kääriäinen, J., Honkatukia, J., and Federley,
M., (2017). Julkishallinnon digitalisaatio–tuottavuus ja
hyötyjen mittaaminen. Valtioneuvoston selvitysja
tutkimustoiminnan julkaisusarja, 3/2017.
Pitkänen, L., Haavisto, I., Vähäviita, P., Torkki, P., Leskelä,
L., & Komssi, V. (2018). Vaikuttavuus SOTE:ssa.
Suoritteista tuloksiin. Nordic Healthcare Group NHG.
Pritchett, L., Samji, S., & Hammer, J. S. (2013). It's all
about MeE: Using Structured Experiential Learning
('e') to crawl the design space. Center for Global
Development working paper, (322).
Ratia, M., Myllärniemi, J. and Helander, N. (2018). Robotic
process automation-creating value by digitalizing work
in the private healthcare? Proceedings of the 22nd
International Academic Mindtrek Conference, 222-227
Ratia, M., Myllärniemi, J. and Helander, N. (2021).
Intellectual Capital and Robotic Process Automation
(RPA)-a Capability Perspective. International Forum
on Knowledge Asset Dynamics, 1810-1824
Saunders, M., Lewis, P., Thornhill, A., and Bristow, A.,
(2019). “Research Methods for Business Students"
Chapter 4: Understanding research philosophy and
approaches to theory development”. In: Research
Methods for Business Students. Pearson Education, pp.
128–171.
Secinaro, S., Calandra, D., Secinaro, A., Muthurangu, V.,
& Biancone, P. (2021). The role of artificial intelligence
in healthcare: a structured literature review. BMC
medical informatics and decision making, 21, 1-23.
Sintonen, H., Blom, M., Roine, R. P., Räsänen, P., &
Ryynänen, O. P. (2021). Terveystaloustiede on tärkeää
lääkärille. Lääkärilehti, 76(39)
Sony, M., Antony, J., & Tortorella, G. L. (2023). Critical
success factors for successful implementation of
healthcare 4.0: A literature review and future research
agenda. International Journal of Environmental
Research and Public Health, 20(5), 4669.
Syed R, Suriadi S, Adams M, Bandara W, Leemans SJ,
Ouyang C., Hofstede AH, van de Weerd I, Wynn MT,
Reijers HA (2020). Robotic process automation:
contemporary themes and challenges. Computers in
Industry, 115, 103162.
Vila-Henninger, L., Dupuy, C., Van Ingelgom, V., Caprioli,
M., Teuber, F., Pennetreau, D., Bussi, M., & Le Gall,
C. (2024). Abductive coding: Theory building and
qualitative (re) analysis. Sociological Methods &
Research, 53(2), 968-1001.
Wanner, J., Hofmann, A., Fischer, M., Imgrund, F.,
Janiesch, C., & Geyer- Klingeberg, J. (2019). Process
selection in RPA projects-towards a quantifiable
method of decision making. 40th International
Conference on Information Systems, Munich.
WHO (2016). Monitoring and evaluating digital health
interventions: a practical guide to conducting research
and assessment. World Health Organization:
Publications.
Willcocks, L., Lacity, M. and Craig, A. (2015a). The IT
Function and Robotic Process Automation. The
Outsourcing Unit Working Research Paper Series.
15(05), 1-39.
Willcocks, L., Lacity, M. and Craig, A. (2015b). Robotic
Automation at Xchanging. The Outsourcing Unit
Working Research Paper Series, 15(03), 1-26.
Willcocks, L.P., Lacity, M.C., Craig, A. (2017). Robotic
Process Automation: Strategic Transformation Lever
for Global Business Services? Journal of Information
Technology Teaching Cases. 7, 17–28
Williams, Bob (2015). “Prosaic or profound? The adoption
of systems ideas by impact evaluation”. IDS Bulletin
46(1), 7–16.
Yin, R. K. (2018). Case study research and applications:
Design and Methods. (6
th
ed.). Sage Publication.
Zayas-Cabán, T., Okubo, T., and Posnack, S., (2023).
Priorities to accelerate workflow automation in health
care. Journal of the American Medical Informatics
Association 30(1), 195–201.
Evaluating Healthcare Automation: A Multi-Case Study on the Utilization of Automation Initiatives in Healthcare Operations
255
