
Comparative Analysis of Machine Learning Models for Stroke Risk
Prediction
Ziqian Gao
Faculty of Arts and Science, University of Toronto, 100 St. George Street, Toronto, ON M5S 3G3, Canada
Keywords: Stroke Prediction, Machine Learning, Predictive Modelling.
Abstract: As the volume of medical data continues to grow rapidly, machine learning technologies have shown great
promise in predicting the risk of stroke. Stroke remains a leading cause of disability and death worldwide,
highlighting the importance of early and accurate risk prediction for effective prevention and management.
This study aims to enhance stroke risk prediction by systematically evaluating the performance of various
machine learning models, including Logistic Regression, Decision Trees, Random Forest, Gradient Boosting
Classifier, and Support Vector Machines. The study systematically compares these models based on metrics
such as accuracy, precision, recall, F1-score, and ROC-AUC values obtained from a well-preprocessed
dataset. The results show that the Random Forest model outperformed the others, demonstrating higher
accuracy and robustness, indicating its potential usefulness in clinical settings for early prediction of stroke
risk. Future studies could explore more advanced data analysis techniques and consider incorporating newer
models like neural networks to further enhance predictive performance.
1 INTRODUCTION
Stroke, a major contributor to serious long-term
disability and the second leading cause of mortality
globally represents a critical challenge in public
health. Defined by the World Health Organization
(WHO) as a major cause of mortality, stroke's impact
on individuals and healthcare systems worldwide is
profound (World Health Organization, 2022). This
condition, characterized by the sudden loss of brain
function due to disturbances in blood supply,
necessitates a nuanced understanding of its
multifactorial etiology to develop effective predictive
and preventive strategies. The complexity of stroke,
with its myriad risk factors ranging from genetic,
lifestyle, and environmental to socio-economic and
behavioral elements, calls for an integrated approach
in research and healthcare practices (Spence JD,
2020).
The urgency of enhancing stroke prediction
methodologies cannot be overstated, given its
devastating impact on populations worldwide. Recent
advancements in machine learning and data analysis
have significantly influenced research in stroke
prediction, offering new methodologies to assess risk
factors and their interactions more comprehensively.
The integration of big data analytics into medical
research allows for a more profound analysis of risk
factors, improving the predictive accuracy of stroke
occurrences. Despite these technological
advancements, the field continues to grapple with
significant challenges. One of the foremost
challenges is accurately capturing and integrating the
complex interactions among genetic, environmental,
and lifestyle factors that contribute to stroke risk.
Additionally, there is the issue of class imbalance in
datasets, which can skew predictive accuracy and
model performance. This study specifically addresses
these challenges by employing a variety of advanced
machine learning techniques, such as SMOTE for
handling class imbalance and ensemble methods like
Random Forests and Gradient Boosting Classifier for
capturing complex patterns in data. By systematically
evaluating these models across multiple performance
metrics, this research aims to enhance the robustness
and accuracy of stroke prediction models, ultimately
improving clinical decision-making and patient
outcomes.
This study advances the field of stroke risk
prediction through several key contributions. Firstly,
it introduces a systematic evaluation of diverse
machine learning models, such as logistic regression,
decision trees, random forests, gradient boosting
classifiers, and support vector machines, tailored
Gao, Z.
Comparative Analysis of Machine Learning Models for Stroke Risk Prediction.
DOI: 10.5220/0012998400004601
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Innovations in Applied Mathematics, Physics and Astronomy (IAMPA 2024), pages 93-101
ISBN: 978-989-758-722-1
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
93

specifically for stroke prediction. This evaluation
provides a detailed comparison of model performance
across multiple metrics—accuracy, precision, recall,
and F1-score—offering a nuanced understanding of
their practical applications in clinical settings.
Secondly, the study employs advanced techniques
like SMOTE to effectively address class imbalance,
enhancing the reliability of predictions in minority
classes. Additionally, the research underscores the
importance of integrating various demographic,
lifestyle, and medical attributes into predictive
models, demonstrating a comprehensive approach to
data preprocessing and feature engineering. These
contributions collectively enhance the robustness,
accuracy, and clinical relevance of stroke prediction
models, paving the way for future research to
incorporate even more sophisticated methods, such as
neural networks, to achieve superior predictive
performance and improved patient outcomes.
The arrangement for subsequent papers is as
follows. Chapter 2 Review recent literature on stroke
prediction. Chapter 3 provides a detailed process for
constructing machine learning models. Chapter 4
analyzes the advantages and disadvantages,
performance differences, clinical significance, and
limitations of different methods from multiple
indicators. Finally, a summary was provided for the
entire article.
2 RELATED WORKS
In recent times, the intersection of machine learning
and stroke prediction has seen remarkable
advancements, as demonstrated by a variety of
studies employing diverse data sources and analytical
approaches to improve prediction models and patient
outcomes.
One notable area of innovation involves the use of
ensemble learning methods, such as Gradient
Boosting Machine (GBM) and Extreme Gradient
Boosting (XGB), explored by Xie et al. (2019). They
specifically utilized these models to integrate clinical,
demographic, and imaging data, achieving notable
prediction accuracies. This method reflects a growing
trend in leveraging complex datasets to refine
predictive accuracy in acute medical settings.
Further advancing the field, Islam et al. (2022)
introduced the use of EEG data in stroke prediction,
applying explainable AI (XAI) frameworks to
enhance transparency in AI decision-making
processes. This study not only improved prediction
accuracy but also provided insights into the model’s
reasoning, crucial for clinical acceptance. This
approach aligns with the broader movement towards
interpretability in machine learning, as seen in the
work of Bhatt et al. (2023), who integrated federated
learning within healthcare IoT frameworks to address
data privacy and scalability challenges effectively.
On a different note, Grimaud et al. (2019) focused
on the epidemiological aspects of stroke, analyzing
how geographical and socio-demographic factors
influence stroke outcomes. This study complements
clinical and technical approaches by highlighting the
importance of environmental and lifestyle factors,
also evident in the work of Andersen and Olsen
(2018) who examined how social determinants like
marital status impact stroke risk. Similarly, another
study by Shah et al. (2010) on the direct impact of
smoking on stroke incidence reveals how lifestyle
choices play a critical role in stroke risk, suggesting
that predictive models should integrate these factors
for a holistic risk assessment.
Moreover, the comprehensive reviews by Stephan
et al. (2017) and Han et al. (2019) provide a broader
context by discussing the implications of cognitive
impairments and atrial fibrillation in stroke
prediction. These studies underscore the necessity of
incorporating a wide range of clinical indicators to
enhance the specificity and reliability of predictive
models.
Collectively, these studies illustrate a shift
towards integrating diverse data types—from clinical
and demographic data to personal health monitoring
and lifestyle factors—into ML models. This
integration aims not only to enhance predictive
accuracy but also to tailor stroke management
strategies to individual patient profiles, thereby
advancing personalized medicine in neurology.
Each of these contributions supports a facet of
stroke research, from enhancing model accuracy and
transparency to incorporating broad epidemiological
data, thus paving the way for a more integrated and
nuanced approach to stroke prediction and
management. The relationship among these studies
underscores a comprehensive, multi-disciplinary
approach to tackling stroke prediction, which is
increasingly recognized as crucial for advancing
patient care and outcomes in the field of neurology.
Using the stroke dataset from Kaggle, this essay
aims to synthesize these diverse methodologies and
data integrations, emphasizing how they collectively
enhance the predictive accuracy of stroke outcomes.
It seeks to demonstrate how the convergence of
machine learning techniques, from the predictive
models by Xie et al. (2019) and Islam et al. (2022) to
the federated learning approaches by Bhatt et al.
(2023), contributes to a more robust understanding of
IAMPA 2024 - International Conference on Innovations in Applied Mathematics, Physics and Astronomy
94
stroke risks and outcomes, paving the way for
advancements in personalized medicine in neurology.
However, despite these advancements, significant
challenges remain. Current studies often focus on
specific datasets or a limited range of features, which
may not fully capture the complex interactions among
genetic, environmental, and lifestyle factors
contributing to stroke risk. This study addresses these
gaps by employing a variety of advanced machine
learning techniques to refine stroke prediction models
using a comprehensive dataset that includes a wide
range of features. By systematically evaluating the
performance of different models, including Logistic
Regression, Decision Trees, Random Forest,
Gradient Boosting Classifier, and Support Vector
Machines, this research aims to identify the most
effective methods for early stroke risk prediction in
clinical settings. The findings from this study are
intended to provide a robust foundation for future
research, potentially incorporating newer models like
neural networks to further enhance predictive
performance.
3 METHODOLOGY
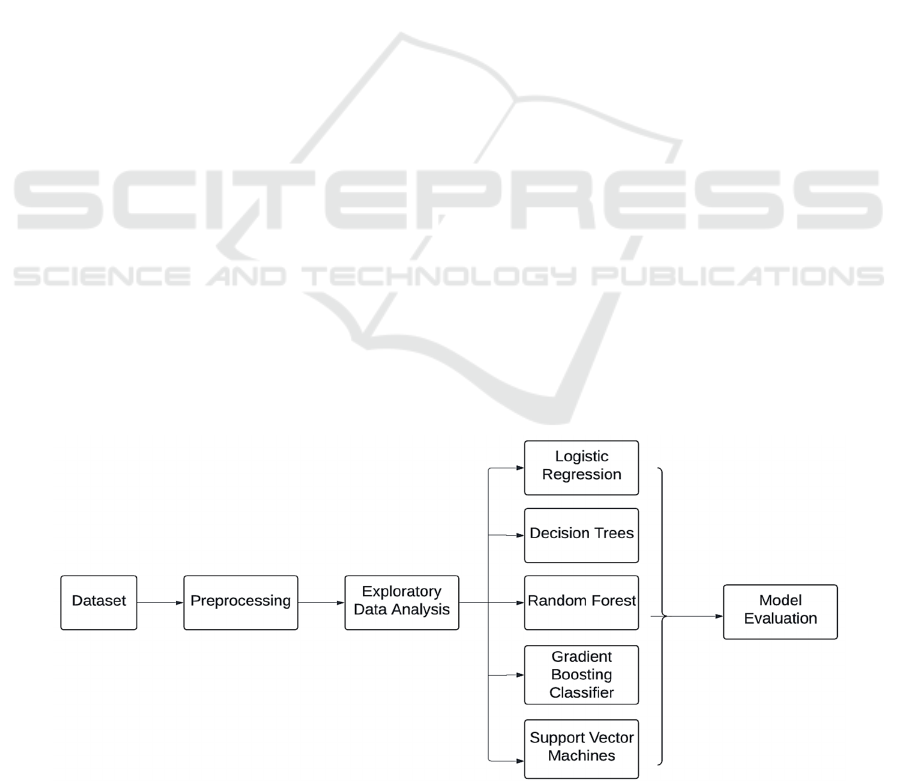
The methodology deployed in this study includes a
comprehensive strategy for predicting stroke risk
based on a range of demographic, lifestyle, and
medical attributes. It integrates several advanced
machine learning techniques to construct and
evaluate models capable of effectively identifying
individuals at higher risk of stroke. The research
presented herein delineates a multifaceted approach
to the development of a predictive model for stroke
risk, utilizing an array of machine learning
techniques. The methodology is segmented into four
distinct but interconnected stages: data preprocessing,
exploratory data analysis (EDA), model
development, and evaluation (Figure 1). This
structured approach ensures that each phase builds
upon the findings of the previous, culminating in the
generation of a reliable predictive tool.
3.1 Data Preprocessing
Data preprocessing is a critical initial step in the
analytical pipeline, focused on converting raw data
into an appropriate format that improves the
performance of machine learning models. The
process began with the importation and cleaning of
data, where missing values and inconsistencies were
addressed. Specifically, the dataset revealed 201
missing values for the 'BMI' attribute, which were
then addressed by median imputation to neutralize the
effect of outliers.
Categorical variables such as 'Gender', 'Residence
Type', 'Marital Status', and 'Smoking Status'
underwent encoding to convert them into numerical
formats suitable for machine learning algorithms.
This encoding involved replacing categories with
designated numerical values, enhancing the dataset's
uniformity and suitability for subsequent analysis.
Continuous variables were standardized using a
StandardScaler to ensure that the model inputs had
consistent scales and distributions, thereby
preventing any variable from dominating the model's
behavior due to its scale.
Figure 1: Workflow (Picture credit: Original).
Comparative Analysis of Machine Learning Models for Stroke Risk Prediction
95
To address the significant class imbalance observed
in the stroke dataset, the Synthetic Minority Over-
sampling Technique (SMOTE) was employed. This
method produces synthetic samples from the minority
class, thus balancing the class distribution effectively.
By doing so, SMOTE enhances the models' ability to
detect and predict minority class outcomes, crucial
for diseases like stroke where early detection is vital.
This approach not only prevents the models from
being biased towards the majority class but also
improves the sensitivity and specificity of the
predictive models used in the study.
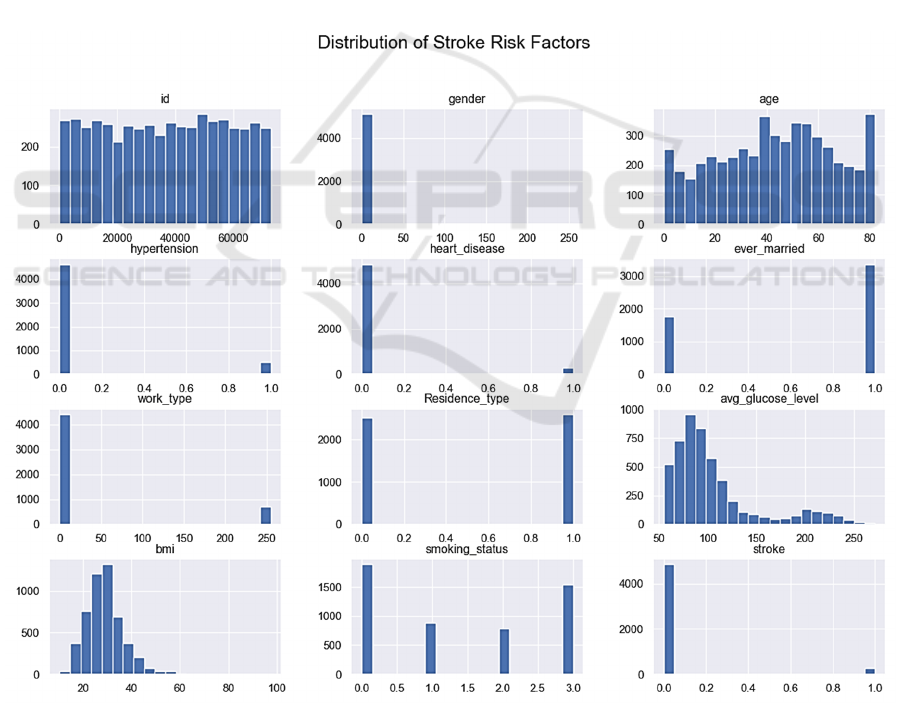
3.2 Exploratory Data Analysis (EDA)
Exploratory data analysis was performed to unearth
underlying structures and detect any anomalies.
Histograms for all numerical features were plotted to
understand distributional characteristics, which are
crucial for the selection of appropriate statistical
models and transformation techniques. The age
distribution illustrated a fairly uniform distribution
with slight right-skewness, indicating a wide range of
participants in different age brackets (Figure 2).
A correlation matrix was utilized to identify
potential multicollinearity and observe inter-variable
relationships (Figure 3). Strong correlations between
'age' and 'ever_married', and between 'hypertension'
and 'heart_disease', were noted. These findings were
visually corroborated through a heatmap, reinforcing
the necessity for careful feature selection to avoid
multicollinearity in the predictive models.
Figure 2: Distribution of Stroke Risk Factors (Picture credit: Original).
IAMPA 2024 - International Conference on Innovations in Applied Mathematics, Physics and Astronomy
96
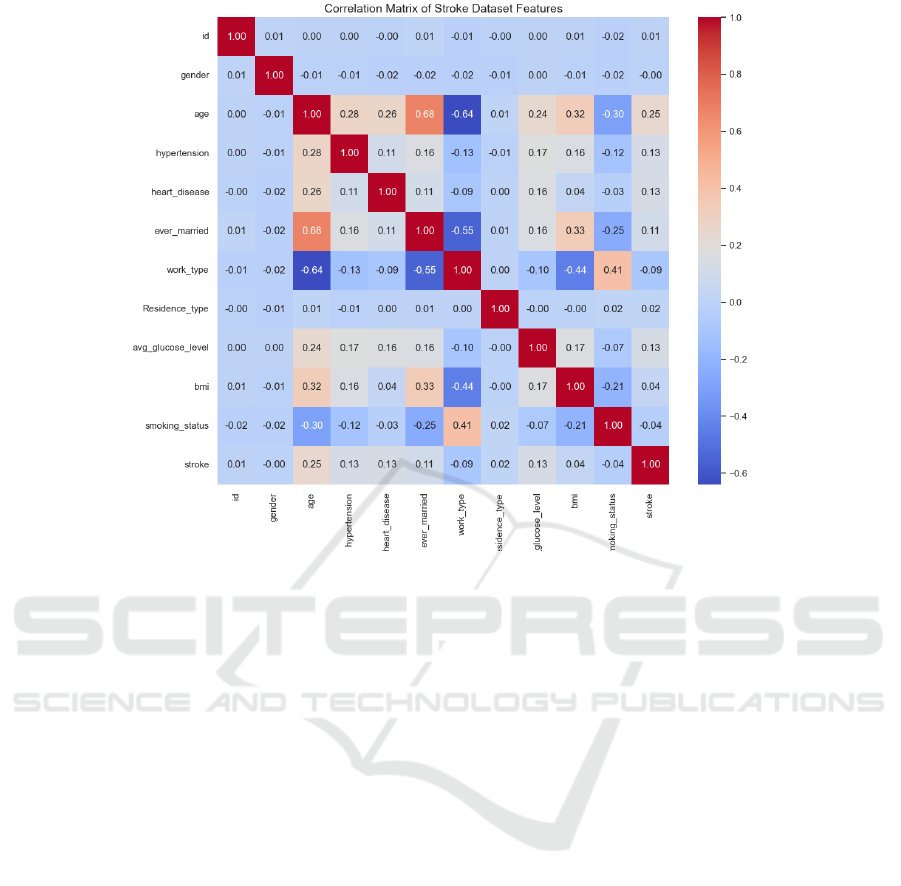
Figure 3: Correlation Matrix of Stroke Dataset Features (Picture credit: Original).
3.3 Model Development
The predictive modeling of stroke incidence requires
precise and robust machine learning techniques that
can effectively handle the intricacies of clinical data
characterized by imbalances and high dimensionality.
This study employs a suite of models, each chosen for
their specific strengths in addressing different aspects
of predictive accuracy and model interpretability in
medical diagnostics.
Logistic Regression is foundational to the study
due to its straightforward output of probability scores
that indicate the likelihood of stroke. This model
benefits clinical decision-making by providing clear,
interpretable results that medical professionals can
easily use to assess risk levels. The logistic model
excels in situations where the relationship between
the binary outcome and the independent variables can
be approximated linearly in the logit scale, making it
particularly suitable for initial risk assessments.
Decision Trees serve as an intuitive approach for
partitioning the data into subsets according to the
values of the explanatory variables, which in turn
makes the decision-making process transparent.
Trees inherently perform feature selection by
choosing the most predictive attributes at each node,
which simplifies the model by excluding non-
informative variables. However, single trees can be
prone to overfitting, especially with complex data,
which necessitates the use of techniques to prune the
trees or limit their growth.
Random Forests address the overfitting
tendencies of single decision trees by introducing
randomness in the selection of features and instances,
and by averaging multiple trees to improve the
generalization to new data. This method is highly
valued in clinical settings for its robust performance
across different types of data and its ability to handle
large feature spaces without significant loss of
accuracy.
Gradient Boosting Classifiers are included for
their capacity to sequentially focus on difficult cases
that previous models misclassified. This technique
gradually improves the model's performance by
combining weak learners into a strong learner,
optimizing a differentiable loss function. Gradient
boosting is particularly effective in enhancing
predictive accuracy, especially in unbalanced datasets
typical of medical outcomes like stroke, where
negative cases far outnumber positive ones.
SVM are utilized for their effectiveness in
classifying non-linearly separable data through the
use of kernel functions. This capability allows SVMs
to project data into higher-dimensional spaces where
a linear separator might exist, making it an excellent
tool for complex datasets with intricate patterns.
Comparative Analysis of Machine Learning Models for Stroke Risk Prediction
97

SVMs are favored for their high accuracy and the
flexibility offered by various kernel choices, such as
polynomial and radial basis function (RBF), which
can be tuned to the specific data characteristics of
stroke prediction.
In this study, the ensemble methods, specifically
Random Forests and Gradient Boosting, are chosen
not only for their high accuracy but also for their
ability to provide insights into feature importance and
model uncertainties. These properties are crucial for
understanding the factors that drive predictions and
for refining the models based on domain-specific
knowledge in stroke research.
By integrating these diverse methodologies, the
research aims to construct a comprehensive
predictive model that leverages the unique strengths
of each method. The ensemble approaches enhance
model stability and accuracy, logistic regression
offers simplicity and interpretability, decision trees
provide a clear visualization of the decision paths,
gradient boosting focuses on improving predictions
iteratively, and SVMs offer robust classification
capabilities. This multifaceted approach ensures that
the predictive model is not only accurate but also
adaptable to the complexities and variabilities
inherent in medical data related to stroke.
4 EXPERIMENTAL SETUP AND
RESULTS
The purpose of this section is to delineate the
experimental setup utilized for model training and the
subsequent results, which were pivotal in ascertaining
the efficacy of various machine learning algorithms
for stroke prediction.
4.1 Experimental Setup
The experimental framework was meticulously
designed to provide an unbiased and rigorous
assessment of the models. The dataset was partitioned
into training and testing subsets using an 80:20 split,
ensuring adequate data for model training while
reserving a subset for assessment. Model training was
conducted on a controlled computational
environment to maintain consistency across
experiments.
Model hyperparameters were selected based on
preliminary tests and literature precedents to optimize
each algorithm's performance. Each model was
evaluated using cross-validation techniques on the
training set to tune the parameters and prevent
overfitting. The Python programming language,
along with libraries such as Scikit-learn and
imbalanced-learn, was employed to implement the
algorithms and handle data manipulation and analysis
tasks.
4.2 Model Training and Evaluation
Following model development, rigorous evaluation
metrics were applied to assess each model's
performance. Accuracy, a fundamental metric,
offered an initial estimation of model performance.
However, accuracy alone can be misleading,
particularly in the presence of class imbalance.
Therefore, confusion matrices were utilized to
provide a more nuanced assessment, offering insights
into the models' abilities to correctly predict each
class.
Classification reports provided a detailed account
of the precision, recall, and F1 scores for each model,
allowing for the evaluation of models beyond mere
accuracy. These scores are particularly critical in
medical diagnostics, where the costs of false
negatives and false positives can have significant
implications.
Finally, ROC curve analysis was conducted for an
aggregate evaluation of model performance across
various threshold levels. Each model's AUC score
was calculated, serving as a singular metric
encapsulating the model's capacity to differentiate
between classes. Models were ranked based on their
AUC scores, with higher scores indicating superior
performance in stroke prediction.
The evaluation process also considered the
practical implications of model implementation. The
complexity of the model, interpretability of results,
and computational efficiency were factored into the
selection of the most appropriate model for
deployment in a clinical setting.
4.3 Results and Analysis
The effectiveness of the models was assessed through
various metrics, including accuracy, precision, recall,
and the F1-score. Each metric provides insight into
different aspects of performance, crucial for a
nuanced understanding of each model's strengths and
limitations in the context of stroke prediction (Table
1 and figure 4).
IAMPA 2024 - International Conference on Innovations in Applied Mathematics, Physics and Astronomy
98

Table 1: Result of stroke prediction.
Metho
d
Accurac
y
Precision Recall F1-score
Logistic Regression 75.24% 93% 75% 82%
Decision Tree 87.08% 89% 87% 88%
Random Forest 92.27% 89% 92% 91%
Gradient Boostin
g
Classifie
r
89.63% 91% 90% 90%
SVM 73.68% 93% 74% 80%
Figure 4: Performance Comparison of Stroke Prediction Models (Picture credit: Original).
In terms of accuracy, Random Forest (92.27%) is the
highest-performing model due to its ensemble nature
that combines multiple decision processes to reduce
overfitting and biases. Decision Tree (87.08%) and
Gradient Boosting Classifier (89.63%) follow, with
the latter using a sequential corrective approach for
classification refinement. Logistic Regression
(75.24%) and SVM (73.68%) have lower accuracy,
possibly due to their linear nature struggling with
non-linearity or class imbalances in stroke data.
Precision measures a model's exactness in
positive predictions. Logistic Regression and SVM
score high in precision (93%), possibly from
conservative prediction strategies sacrificing recall.
Gradient Boosting Classifier (91%) and Random
Forest (89%) maintain high precision without
significant recall trade-off due to their complex
structures detecting subtle data patterns.
Recall is critical in medical diagnostics. Random
Forest leads with 92% recall, capturing a broad range
of positive cases. Gradient Boosting Classifier (90%)
focuses on prior errors to enhance sensitivity
iteratively. Decision Tree's recall (87%) may be due
to its unpruned nature capturing more positives at an
overfitting risk. Logistic Regression and SVM have
recall rates of 75% and 74%, needing additional
measures for class imbalances or complex
interactions.
The F1-score balances precision and recall, with
Gradient Boosting Classifier (90%) as the top
performer, followed by Random Forest (91%).
Logistic Regression and SVM have F1-scores of 82%
and 80%, indicating less effectiveness in identifying
true positives.
The ROC-AUC score, measuring a model's class
discrimination, is high for Logistic Regression and
SVM (0.85), followed by Random Forest and
Gradient Boosting Classifier (0.82 and 0.83).
Decision Tree lags with an AUC of 0.54 due to
simplicity and vulnerability to noise (Figure 5).
In summary, each model's performance is
influenced by dataset challenges like class imbalance
and feature dependencies. Ensemble methods excel in
integrating multiple decision processes, crucial in
stroke prediction, while simpler models may need
advanced techniques for improved performance.
Comparative Analysis of Machine Learning Models for Stroke Risk Prediction
99
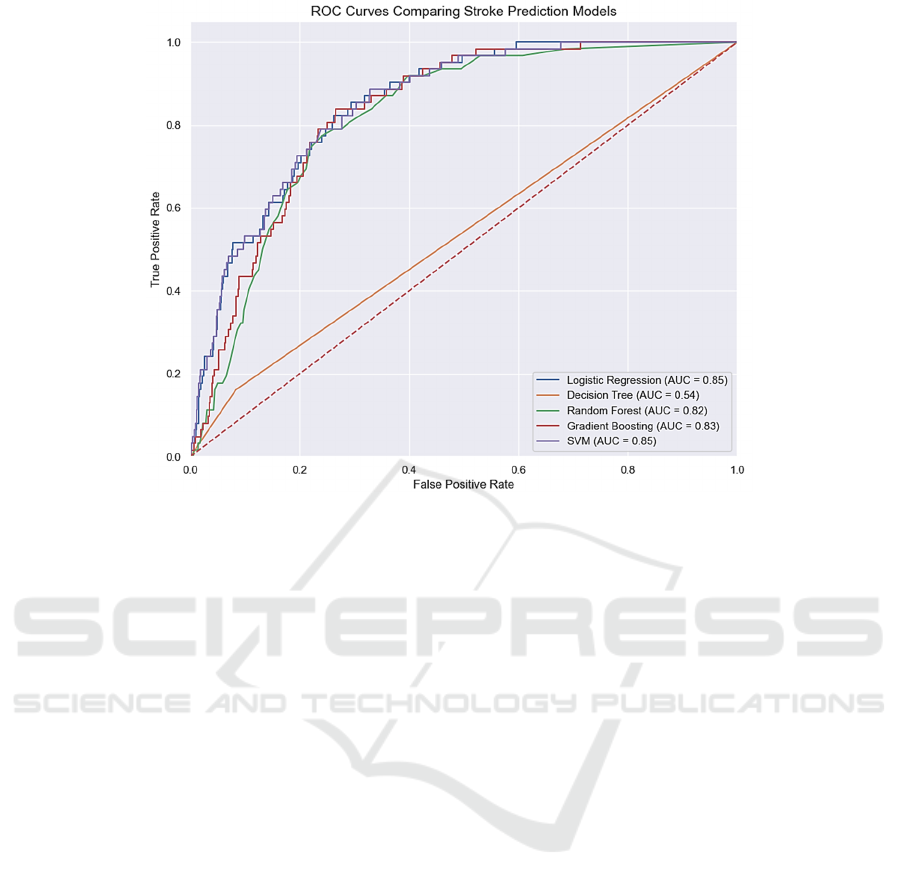
Figure 5: ROC Curves Comparing Stroke Prediction Models (Picture credit: Original).
4.4 Discussion
The experimental results revealed that while some
models achieved high overall accuracy, their
application in a clinical setting requires careful
consideration of the trade-offs between various
performance metrics. High accuracy may not always
translate to clinical utility, particularly when the cost
of false negatives is substantial, as in the case of
stroke prediction. The ROC analysis provided a more
comprehensive understanding, suggesting that
Logistic Regression and SVM, despite their
limitations in precision for stroke cases, offered a
balanced discriminative ability across thresholds.
The ramifications of these results are significant.
In clinical practice, the ability to accurately predict
stroke cases could save lives and prevent long-term
disabilities. Therefore, the selection of the
appropriate model is not solely based on statistical
performance but also on the clinical context and the
consequences of predictive errors.
5 CONCLUSION
In summary, this study has successfully evaluated the
performance of multiple machine learning models for
stroke risk prediction, focusing on models including
Logistic Regression, Decision Trees, Random Forest,
Gradient Boosting Classifier, and Support Vector
Machines. Among these, the Random Forest model
stood out for its superior effectiveness, attributed to
its robust handling of complex and imbalanced
datasets crucial in medical diagnostics. The model's
ability to aggregate multiple decision trees helps
mitigate biases and overfitting, producing a more
reliable and generalizable prediction tool.
Moving forward, future research could explore
real-time data analytics and continuous monitoring of
physiological parameters to better capture the
temporal progression of risk factors. These
advancements may lead to the development of
dynamic prediction models that adjust predictions
based on new data, potentially enhancing accuracy
and clinical utility. By leveraging the findings of this
study and incorporating cutting-edge research, future
efforts can work towards transforming the landscape
of stroke prevention. This proactive and personalized
approach could significantly improve patient
outcomes by predicting and mitigating risks more
effectively.
REFERENCES
World Health Organization. Stroke, Cerebrovascular
accident. WHO EMRO; 2022. Available from:
https://www.emro.who.int/health-topics/stroke-
cerebrovascular-accident/index.html.
Spence JD. Stroke Prevention. Stroke. 2020;51(7):2255–
2262.
IAMPA 2024 - International Conference on Innovations in Applied Mathematics, Physics and Astronomy
100

Xie Y, Jiang B, Gong E, Li Y, Zhu G, Michel P,
Wintermark M, Zaharchuk G. Use of Gradient
Boosting Machine Learning to Predict Patient
Outcome in Acute Ischemic Stroke on the Basis of
Imaging, Demographic, and Clinical Information. AJR
Am J Roentgenol. 2019 Jan;212(1):44-51.
Islam MS, Hussain I, Rahman MM, Park SJ, Hossain MA.
Explainable Artificial Intelligence Model for
Stroke Prediction Using EEG Signal. Sensors (Basel).
2022;22(24):9859.
Bhatt H, et al. Artificial Neural Network‐Driven Federated
Learning for Heart Stroke Prediction in Healthcare
4.0 Underlying 5G. Concurrency and Computation:
Practice and Experience. 2023;36(3). doi:
10.1002/cpe.7911.
Grimaud O, Lachkhem Y, Gao F, Padilla C, Bertin M,
Nowak E, Timsit S. Stroke Incidence and Case
Fatality According to Rural or Urban Residence.
Stroke. 2019;50(10):2661–2667.
Andersen KK, Olsen TS. Married, unmarried, divorced, and
widowed and the risk of stroke. Acta Neuro
Scandinavica. 2018;138(1):41–46. .
Shah RS, Cole JW. Smoking and stroke: the more you
smoke the more you stroke. Expert Rev
Cardiovasc Ther. 2010;8(7):917–932.
Stephan BCM, Richardson K, Savva GM, Matthews FE,
Brayne C, Hachinski V. Potential Value of Impaired
Cognition in Stroke Prediction: A U.K. Population-
Based Study. J Am Geriatr Soc. 2017;65(8):1756–
1762.
Han L, Askari M, Altman RB, Schmitt SK, Fan J, Bentley
JP, Narayan SM, Turakhia MP. Atrial Fibrillation
Burden Signature and Near-Term Prediction of Stroke.
Circ Cardiovasc Qual Outcomes. 2019;12(10).
Stroke Prediction Dataset [Internet]. Kaggle. Available
from:https://www.kaggle.com/code/mennatallah77/str
oke-prediction-with-99-accuracy.
Comparative Analysis of Machine Learning Models for Stroke Risk Prediction
101
