
Prediction of Response to Intra-Articular Injections of
Hyaluronic Acid for Knee Osteoarthritis
Eva K. Lee
1,2,3 a
, Fan Yuan
2
, Barton J. Mann
4
and Marlene DeMaio
4,5
1
Center for Operations Research in Medicine and Healthcare, The Data and Analytics Innovation Institute, Atlanta, U.S.A.
2
Georgia Institute of Technology, Atlanta, U.S.A.
3
AccuHealth Technologies, Atlanta, Georgia, U.S.A.
4
The American Orthopedic Society for Sports Medicine, Chicago, U.S.A.
5
Medical Corps, United States Navy, U.S.A.
Keywords: Knee Osteoarthritis, Injections of Hyaluronic Acid, Machine Learning for Evidence-Based Practice,
Branch-and-Bound, Particle Swarm Optimization.
Abstract: Osteoarthritis (OA) is a degenerative joint disease, with the knee the most frequently affected joint. Fifty
percent of knee OA patients eventually undergo surgical procedures such as knee replacement to address pain
and functional limitations. A significant number of these surgeries may be unnecessary, with intra-articular
injections of hyaluronic acid (HA) serving as a non-invasive, cost-effective alternative. Although research
studies have clearly demonstrated that HA improves knee function, the efficacy of this treatment remains
controversial. Many physicians have observed that effects depend on several patient characteristics such as
age, weight, gender, severity of the OA, and technical issues such as injection site and placement. In this study,
a multi-stage, multi-group machine learning model is utilized to uncover discriminatory features that can
predict the response status of knee OA patients to different types of HA treatment. The algorithm can identify
certain subgroups of knee OA patients who respond well to HA therapy. The baseline results, based on factors
such as patients’ weight, smoking status and frequency, identifies the patients most suitable for HA injection.
The model can achieve more than 89% blind prediction accuracy. The data derived from this study allows
physicians to administer HA products more selectively, resulting in a higher therapy success rate. Information
on the predicted responses could also be shared with patients beforehand to incorporate their values and
preferences into treatment selection. The model’s decision support tools also allow physicians to quickly
determine whether a patient is exhibiting at least the expected treatment response, and if not, to potentially
take corrective action. To the best of our knowledge, this work represents the first machine learning approach
that predicts patient responses to HA injections for knee osteoarthritis. The model is generalizable and can be
used to predict patient responses to other treatments and conditions.
1 INTRODUCTION
Osteoarthritis (OA) is a degenerative joint disease
that can affect the many tissues of the joint. It is one
of the most prevalent and costly chronic medical
conditions. affecting more than 32.5 million adults in
the United States (United States Bone and Joint
Initiative 2018). During 2019–2021, 21.2% of U.S.
adults (53.2 million) reported an arthritis diagnosis.
(Elgaddal, et al., 2022; Fallon, et. al., 2023) and by
2040, it is projected to increase to 78.4 million
Americans.
a
https://orcid.org/0000-0003-0415-4640
Arthritis increasingly is reported as the main
cause of disability among U.S. adults (Theis, K.A. et
al., 2019). Annual direct medical care expenditures
for osteoarthritis in the U.S. is estimated to exceed
$495.5 billion (United States Bone and Joint Initiative,
2019; Lo, et al., 2020). Worldwide, about 528 million
people were living with osteoarthritis in 2019 (WHO
2023, GBD 2019). It is estimated that those with OA
pain lost 31% of productive time at work due to
presenteeism and 8% due to absenteeism, compared
to 16% and 4%, respectively, for those who did not
report OA pain (Leifer et al., 2022).
Lee, E., Yuan, F., Mann, B. and DeMaio, M.
Prediction of Response to Intra-Articular Injections of Hyaluronic Acid for Knee Osteoarthritis.
DOI: 10.5220/0013071800003838
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 16th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2024) - Volume 1: KDIR, pages 497-508
ISBN: 978-989-758-716-0; ISSN: 2184-3228
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
497

There is no known cure for OA. Instead,
treatments aim to reduce pain, maintain or improve
joint mobility, and limit functional impairment.
Treatments are usually non-operative, such as
physical therapy, rest, modification of daily activities,
analgesics, and anti-inflammatory medication. For
individuals who desire or require a high level of
physical activity, rest and activity reduction are not
viable treatment options. Oral non-steroidal anti-
inflammatory drugs (NSAIDs) are often
recommended, although frequent and serious adverse
effects of NSAIDs have been reported (Zhang et al.,
2010, Salis and Sainsbury, 2024). Over the past 25
years, intra-articular injection of hyaluronic acid (and
similar hyaluronan preparations) has emerged as an
additional tool for managing the symptoms of OA for
patients who fail to respond to other conservative
treatments. However, controversies exist regarding
its safety and efficacy, the number of injections and
courses, type of preparation, duration of its effects,
and combining it with other drugs or molecules
(Chavda et al., 2022). Other factors include patient
characteristics such as age, weight, gender, and
severity of the OA.
Knee OA happens when the cartilage in the knee
joint breaks down, enabling the bones to rub together.
The friction makes the knees hurt, become stiff, and
sometimes swell. Knee OA is a leading cause of
arthritis disability (Cui et al., 2020). Of significance
for sport medicine, heavy physical activity,
participation in high intensity contact sports,
participation in certain elite level sports, and knee
injury have all been linked to the development of knee
OA (Chan, et al., 2020; Driban, et al., 2017;
Lohmander, et al., 2007; McAlindon et al., 1999;
Sharma, 2001; Spector et al., 1996; Turner, et al.,
2000). Although it cannot be cured, treatments are
available to slow its progression and ease the
symptoms. Knee OA alone results in the loss of an
average of 13 days of work per year (versus 3 days
for those without Knee OA (Ayis & Dieppe, 2009).
Knee osteoarthritis affects more than 14 million
Americans, and its symptoms often lead to physical
inabilities, disabilities, and all sorts of inconveniences
for patients. It is estimated that knee osteoarthritis is
associated with approximately $27 billion in total
healthcare costs every year, with about 800,000 knee
surgeries performed annually. Specifically, 99% of
these knee replacements are done to address pain and
functional limitations (Barbour et al., 2017).
In a
multicenter longitudinal cohort study, it was reported
that about one-third of knee replacements may be
unnecessary (Riddle et al., 2014).
The management of knee pain depends on the
diagnosis, inciting activity, underlying medical
conditions, body mass, and chronicity. In general,
non-operative management is the mainstay of initial
treatment and includes rehabilitation, activity
modification, weight loss when indicated, shoe
orthoses, local modalities, and medication. The oral
medication often prescribed is an analgesic, usually
with anti-inflammatory properties. Supplements,
such as chondroitin sulfate and glucosamine, have
been shown to have a role. Since 1997, the regimen
has expanded to include viscosupplementation.
These agents are preparations of hyaluronic acid or
their derivatives (HA) which are sterilely injected into
the knee. Although research studies have clearly
demonstrated that HA improves knee function, the
efficacy of this treatment remains controversial.
Many physicians have observed that effects seem to
depend on several patient characteristics, such as age,
weight, gender, severity of the OA and technical
issues such as injection site and placement (Mora et
al., 2018).
This study aims to answer an important question:
whether different types of patients may respond
differently to HA treatment. Is it possible to identify
certain subgroups of knee OA patients who respond
well (or those who don’t) to HA therapy? Further, we
question whether it is possible prior to treatment to
predict a patient’s response to HA injections based on
patient and treatment characteristics. Physicians
could then make empirically informed decisions
about whether to treat a particular patient with HA
and perhaps which type of HA preparation is most
likely to produce the best treatment response for that
individual patient.
The goal of this study is to evaluate which patient
population, or patient characteristics, would benefit
most from HA injection. Since at least 18% of out-
patient visits to military treatment facilities by active-
duty personnel are attributed to painful knee disorders,
our study focuses on these patients. The study uses a
prospective, double-blinded clinical trial. A multi-
stage, multi-group machine learning model (Lee et al.,
2016b; Lee, 2017; Lee & Egan, 2022; Lee et al., 2021,
2023a, 2023b) described in Section 2.3 is used to
uncover discriminatory patterns that can predict
suitability of treatment and outcomes. The resulting
predictive rule can be implemented as part of a
clinical practice guideline for evidence-based
intervention. The model enables physicians to
administer HA products more selectively and
effectively to the targeted population to maximize
cost effectiveness and the percentage of patients who
experience a successful HA injection.
KDIR 2024 - 16th International Conference on Knowledge Discovery and Information Retrieval
498

2 METHODS AND STUDY
DESIGN
2.1 Patient Cohort, Treatment, and
Outcome Measures
2.1.1 Patient Data
Three group of patients (active-duty military
personnel, military retirees, and their families)
through the Department of Orthopaedics at the Naval
Medical Center Portsmouth were included. The
cohort includes those between 18 and 65 who sought
treatment for symptomatic osteoarthritis of the knee.
All patients were evaluated by a board-certified
orthopaedic surgeon. Each patient has had
radiographic evidence of knee OA with a minimum
Kellgren-Lawrence score of 1, has experienced
symptoms for more than three months, has failed a
minimum of three months of non-operative treatment,
including, but not limited to, analgesic and anti-
inflammatory medication, cortisone injection,
physical therapy, bracing, and/or heel wedge. The
cohort excludes patients with precautions or
contraindications for viscosupplementation, those
who had a cortisone injection within the past three
months, those who had prior HA injections at any
point, those with a history of deep knee infection,
those currently experiencing peripheral neuropathy,
chondrocalcinosis, or knee ligament instability, and
those who were candidates for knee surgery.
Patients were randomly assigned to receive either
Hylan G-F 20 (Synvisc®) [Sanofi Biosurgery,
Cambridge, MA, USA], a high molecular weight
(MW = 6000 kDa) cross-linked HA product derived
from an avian source, or EUFLEXXA®
[bioengineered 1% sodium hyaluronate (IA-BioHA);
Ferring Pharmaceuticals, Inc., Parsippany, NJ], a
medium weight (MW = 2400 - 2600 kDa) HA product
derived from bacterial fermentation.
Treatment allocations were randomly assigned by
the study pharmacist using the
RANDBETWEEN(0,1) function in Microsoft Excel.
Physicians, physicians performing the injections,
patients, and research personnel were blinded to
treatment assignment. To maintain blinding, the
pharmacy removed the original manufacturer's label
prior to dispensing and relabelled with the protocol
title, subject identifier and expiration date. The two
HA products had the same volume and color, so there
was no ability to discern one from the other at the time
of injection.
During a baseline evaluation before the first
injection, the following data were collected:
patient demographic data: age, sex, height,
weight, BMI (as calculated from height and
weight), and smoking history.
the Western Ontario and McMaster
Universities Osteoarthritis Index (WOMAC;
Bellamy, 2002) as a measure of knee OA
symptoms and functioning.
the RAND-36 (Hays et al., 1993) as a measure
of general health status.
the MARX Knee Activity Rating Scale (Marx
et al., 2001) to assess activity level (running,
deceleration, cutting (changing directions
while running) and pivoting.
patient-rated health conditions (a) using a
comorbidity questionnaire (Sangha et al.,
2003) and (b) quality of life as measured by the
EuroQOL EQ-5D (Brooks, 1996).
a patient-completed Arthritis Self-Efficacy
Scale (Lorig et al., 1989), an eight-item
instrument that assesses patient’s perceived
ability to manage arthritis symptoms.
Specific patient treatment expectations (e.g.,
“Improve ability to go up and down stairs”) and the
importance of these expectations were evaluated with
the scale developed by Mancuso (Mancuso et al.,
2001). Patients were also asked to rate their global
expectation for their response to the HA injections on
a seven-point scale ranging from “No improvement. I
don’t have much hope that this treatment will help my
symptoms at all” to “Excellent improvement. I expect
complete or nearly complete relief from knee
symptoms.” Patients with bilateral OA were
instructed to rate only the knee they perceived to be
more severe in terms of pain and functional
impairment on all instruments and to rate the same
knee at baseline and follow-ups.
Prior to the first injection, a physician assessed
quadriceps atrophy, presence of antalgic gait, knee
effusion, pain on palpation of the knee, range of
motion and alignment, and use of medication.
Patients also received four baseline radiographs.
These included (a) a standing anteroposterior (AP) of
the knee weight-bearing view; (b) weight-bearing
flexed view 400 posterior-anterior (PA) Rosenberg
view; (c) a lateral x-ray at 300; and (d) a Merchant
view. Digitized radiographs were evaluated for
osteoarthritis severity and for alignment by a board-
certified musculoskeletal radiologist and an
orthopaedic surgeon blinded to assigned treatment or
other patient characteristics. OA severity was rated
using the Kellgren-Lawrence Grading System which
incorporates joint space narrowing, osteophyte
formation, sclerosis and bony deformation observed
Prediction of Response to Intra-Articular Injections of Hyaluronic Acid for Knee Osteoarthritis
499

on x-rays. Scores range from 0 (no radiographic
features of OA) to 4 (large osteophytes, marked joint
space narrowing, severe sclerosis, and definite bony
deformity). Alignment was determined by measuring
the following angles from x-rays: (a) condylar-hip
angle of the femoral condylar tangent with respect to
the mechanical axis of the femur expressed as degrees
of deviation from 90°, negative for varus and positive
for valgus; (b) plateau-ankle angle between the tibial
margin tangent and the mechanical axis of the tibia
expressed as degrees of deviation from 90°, negative
for varus and positive for valgus; (c) condylar-plateau
angle between the femoral and tibial joint surface
tangents; and (d) hip-knee-ankle angle between a line
drawn from the center of the femoral head to the
midpoint of the tibial eminential spine and another
line from this midpoint to the center of the talus
surface of the ankle joint. The medial angle between
the lines is the HKA angle (varus < 180°).
2.1.2 HA Treatments
Patients received injections every seven days for a
total of three injections. Physicians received specific
instructions to standardize injection technique. All
injections were performed using an anteromedial
approach with a 21-gauge 1½” needle. Physicians
aspirated the knee joint prior to injection of the HA
product to ensure needle placement. Patients were
asked to flex and extend their knee a few times
following injection to maximize dispersal into the
joint. Patients were provided with written post
injection and standardized physical therapy
instructions. Patients were allowed full weight
bearing and full range of motion (active and passive)
after injections but were advised to avoid strenuous
activity (such as jogging, tennis, etc.) or prolonged
weight bearing for the first 48 hours after injection.
Patients were also instructed to use ice 30 minutes on
and 30 minutes off for 48 hours and take up to 4 gram
of acetaminophen per day as need for knee pain, but
not to take any 24 hours prior to each visit.
Patients were not offered a second course of HA
treatment within the first six months following the
final injection. Following the standard clinical
practice, those who received a second series of
injections after the first six months were not
considered treatment failures. Patients who had
surgery on the target knee to relieve arthritis
symptoms within the first six months following the
last HA injection were considered treatment failures.
The protocol was approved by the Institutional
Review Board at the data collection site and was
registered with ClinicalTrials.gov (identifier:
NCT01557868). A physician at the site served as the
medical monitor and an independent data and safety
board monitored the study.
2.1.3 Primary and Secondary Outcomes
The primary outcome was treatment responder status
defined a priori by improvement in the Western
Ontario and McMaster Universities Osteoarthritis
Index (WOMAC) Pain Scale (Hochberg et al., 1997;
Riddle & Perera, 2020) between baseline and 3-
month assessments. The WOMAC Pain Scale is
comprised of 5 items and the response format used in
this study was the 5-point rating scale. Scores were
calculated to range from 0 (worst) to 100 (best). The
reliability, validity and responsiveness of the
WOMAC Pain Scale have been supported in
numerous studies (Bellamy, et al., 2011; Burgers, et
al. 2015) and the WOMAC is one of the most widely
used outcome instruments in arthritis research.
Patients whose pain scores decreased by 20% or more
compared with their baseline scores were classified as
treatment responders and those whose scores did not
meet this criterion were classified as non-responders.
2.2 Machine Learning Predictive
Analysis
We apply a multi-stage machine learning approach to
analyze how different types of patients may respond
differently to HA treatment. The system will uncover
discriminatory features in the HA data that will reveal
patient and treatment characteristics that predict
optimal response to intra-articular injections of
hyaluronic acid for knee osteoarthritis. The model
determines which patient variables lead to the best
outcomes of HA.
Detail of the multi-stage multi-group discriminant
analysis via mixed-integer program (DAMIP) model
and computational framework is reported in Lee et al.
(Lee, 2017; Lee & Egan, 2022; Lee, Wang, et al.,
2016; Lee et al., 2021, 2023a, 2023b). Briefly we
include the DAMIP formulation below.
Let 𝑢
represent the binary variable that
indicates whether observation i in group g is
classified to group h, ℎ∈
0
∪𝒢. Thus, 𝑢
=1
denotes a correct classification for observation i in
group g. The multi-group model with a reserved
judgement region is formulated as:
max 𝑢
∈𝒪
∈ 𝒢
(𝐃𝐀𝐌𝐈𝐏)
subject to
𝐿
= 𝜋
𝑓
𝒙
−
∑
𝜆
𝑓
𝒙
∈𝒢,
, ∀ ℎ,𝑔 ∈ 𝒢,𝑗 ∈ 𝒪
(1)
𝑦
−𝐿
≤𝑀1−𝑢
, ∀ ℎ, 𝑔 ∈ 𝒢, 𝑗 ∈ 𝒪
(2)
KDIR 2024 - 16th International Conference on Knowledge Discovery and Information Retrieval
500

𝑦
≤𝑀1−𝑢
, ∀ 𝑔 ∈ 𝒢, 𝑗 ∈ 𝒪
(3)
𝑦
−𝐿
≥𝜀1−𝑢
, ∀ ℎ, 𝑔 ∈ 𝒢, 𝑗 ∈ 𝒪
(4)
𝑦
≥𝜀 𝑢
,
∀ ℎ,𝑔 ∈ 𝒢, 𝑗 ∈ 𝒪
(5)
∑
𝑢
∈
∪𝒢
= 1, ∀ 𝑔 ∈ 𝒢, 𝑗 ∈ 𝒪
(6)
∑
𝑢
∈𝒪
≤𝛼
𝑛
, ∀ ℎ,𝑔 ∈ 𝒢,𝑔 ≠ ℎ (7)
𝑢
∈
0,1
∀ ℎ ∈
0
∪𝒢,𝑔∈𝒢,𝑗∈𝒪
(8)
𝑦
≥ 0, ∀ ℎ,𝑔 ∈ 𝒢, 𝑗 ∈ 𝒪
(9)
𝜆
≥ 0 ∀ ℎ, 𝑔 ∈ 𝒢,𝑔 ≠ ℎ (10)
Here, 𝜋
is the prior probability of group 𝑔 and
𝑓
(𝒙) is the conditional probability density function
of group 𝑔, 𝑔∈ 𝒢 for the data point 𝒙∈ℝ
. 𝒪
denote the set of observations in group g, and 𝑛
denote the number of observations in group g ∈𝒢.
𝛼
∈ (0, 1) , h, 𝑔∈𝒢, ℎ≠𝑔 represents the
predetermined limit on the inter-group
misclassification rate where the observations of group
𝑔 are misclassified to group h. The group assignment
decisions of observations that are classified into a
reserved judgment region are denoted by group g = 0.
Constraints (1) define the loss functions;
constraints (2)-(6) guarantee an observation is
uniquely assigned to the group with the maximum
value of 𝐿
(
𝒙
)
among all group, and constraints (7)
set the misclassification limits. With the reserved
judgment region in place, the mathematical system
ensures that a solution that satisfies the pre-set
misclassification rate always exists.
Theorem 1. Given prior probabilities 𝜋
and
conditional group density functions 𝑓
(𝒙), allocation
according to modified posterior probabilities defined
by the solution to (DAMIP) is a universally strongly
consistent method for classification.
Theorem 2. The DAMIP optimization problem is
𝒩𝒫 − 𝐶𝑜𝑚𝑝𝑙𝑒𝑡𝑒 when the number of groups is
greater than 2. The theoretical result holds for
DAMIP variants: (a) maximize the minimum value of
correct classification rates among all groups; (b)
maximize the minimum difference between correct
classification and misclassification; and (c) maximize
correct classification while constraining the
percentage of reserved judgment for each group.
The multi-stage classification approach utilizes
the reserved judgment region in DAMIP to improve
the classification performance, especially among
highly inseparable data. At each stage, DAMIP
partitions the observations into an ‘easy–to-classify’
subset that is classified to specific groups, and a
‘difficult-to-classify’ subset that is classified to a
reserved judgment region. The group assignment of
the difficult-to-classify observations are delayed, thus
allowing the DAMIP classifier to maintain a low
misclassification error. The observations in the
reserved judgment region are moved to the next stage
where a new feature set is selected and a new DAMIP
classifier is developed. In this way, the multi-stage
framework constructs a chain of successive classifiers
using different subsets of features. The classifier at
the ith stage, denoted by 𝑓
, can be represented by a
discriminant function 𝑓
(
𝒙
,𝝀
𝒊
)
, which is determined
by the feature subset 𝒙
, and the decision variables 𝝀
𝒊
in DAMIP.
At each stage, two models are performed: a
single-stage model that solves a DAMIP model
without a reserved judgment region and a multi-stage
model that solves a DAMIP model with a reserved
judgment region. The computational framework
selects the better of the two results. The algorithm
naturally terminates when there are no observations
in the reserved judgment region. To avoid overfitting
using too few observations for training, two
additional stopping criteria are used to terminate the
process: (a) the number of observations is less than a
preset minimum value, n, and (b) the maximum
allowed depth, d, is reached. The parameters n and d
are predetermined according to the number of
observations and the number of input features in the
given data.
Computationally, DAMIP classifier has some
distinct characteristics: (a) it is applicable for
classification of any number of groups; (b) there is
always a feasible solution to the model; (c) the
reserved judgement region facilitates successive
stage of classification to be performed; (d) DAMIP is
able to establish classification rules with good
predictive accuracy even when the training set is
relatively small; (e) DAMIP classifier can handle
imbalanced data; and (f) DAMIP classifier is totally
universally consistent.
Figure 1 shows the machine learning framework
where features are first selected via an exact branch-
and-bound algorithm (BB) and a fast heuristic particle
swarm optimization (PSO) (Lee et al., 2023a). The
resulting classification rule is subsequently
established via the DAMIP classifier. To quantify the
accuracy, ten-fold cross validation evaluation is
performed. If the results satisfy some pre-set accuracy
level, the classification rule is reported. Blind
prediction using this rule is then performed. We
contrast the BB-PSO/DAMIP results with eight
commonly used classifiers: Bernoulli Naïve Bayes,
Decision Tree, Gradient Boosting, K-nearest
neighbors, Logistic Regression, Neural Network,
Random Forest, and Support Vector Machine (SVM).
Prediction of Response to Intra-Articular Injections of Hyaluronic Acid for Knee Osteoarthritis
501
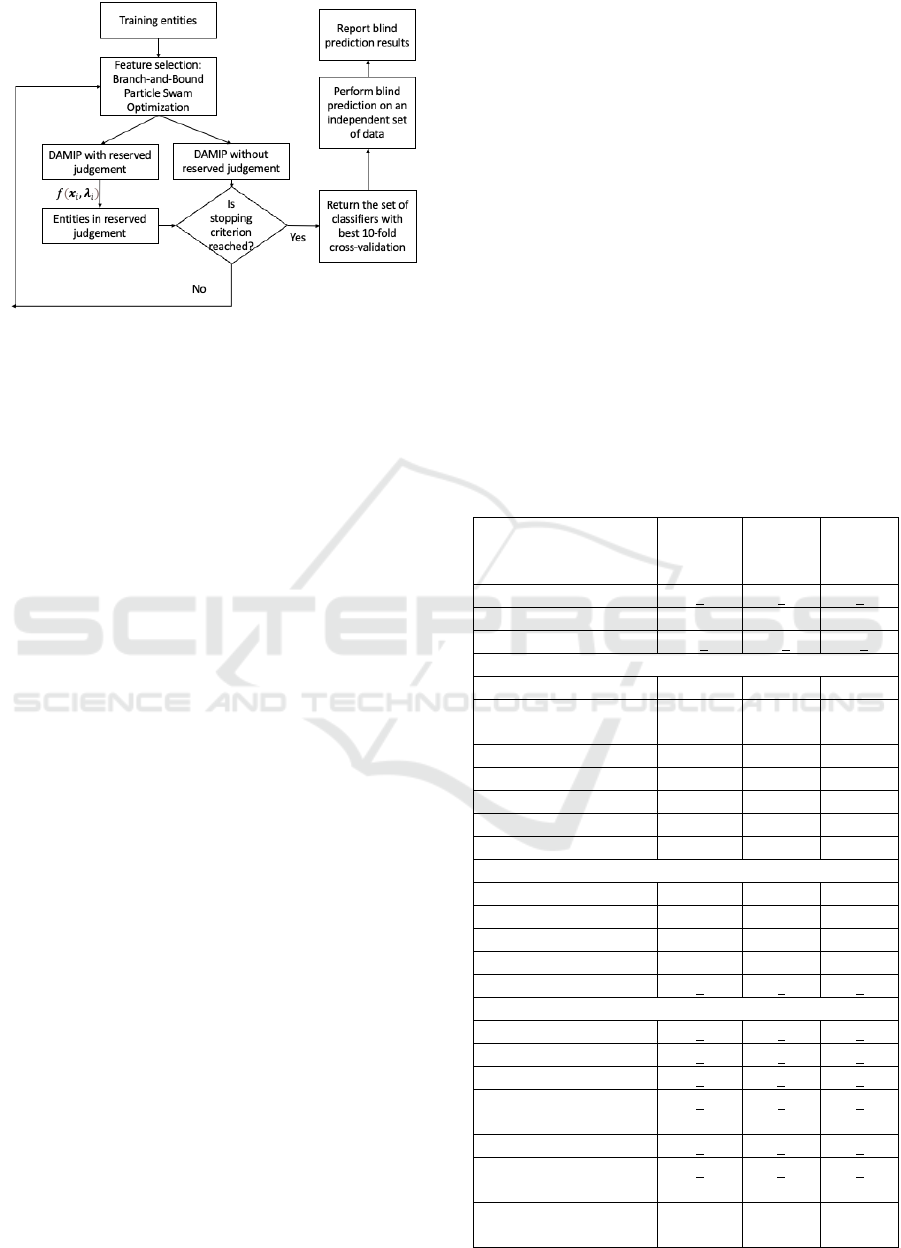
Figure 1: Multi-stage machine learning framework for HA
predictive analytics.
In 10-fold cross validation, the training set is
partitioned into 10 roughly equal subsets. In each run,
9-fold are selected to train and establish the rule, and
the remaining 1-fold is then tested, counting how
many of them are classified into which group.
Through 10 folds procedure (where each fold is being
validated exactly once), we obtain an unbiased
estimate of the classification accuracy.
Blind prediction is performed on patients that are
independent of the training set to gauge the predictive
power of the established rule. These patients have
never been used in the feature selection and the
machine learning analysis. We run each patient in the
blind set through the rule, which returns a group
status of the patient. The status is then checked
against the clinical status to confirm the accuracy.
The classifier response and outcome prediction
rules will culminate in a clinical decision algorithm
for the use of viscosupplementation in the treatment
of knee OA. For example, a physician determines that
HA is indicated for a particular patient. The physician
would then enter specific variables (those
discriminatory features identified by the classifier)
into a clinical computer program and a response set
would be generated for the potential outcome after
using hyaluronic acid injections. The optimal HA
agent(s) would be ranked. The physician would then
take this information into account as part of the
clinical decision process to select the HA agent for
the individual patient.
3 RESULTS
3.1 Patient Characteristics
Of the 273 patients assessed for eligibility, 45 did not
meet study criteria, 13 eligible patients declined to
participate, and 12 eligible patients could not
complete study participation due to anticipated
deployment or relocation. The other 203 eligible
patients were randomized to treatment: 107 assigned
to the Synvisc group and 96 to the Euflexxa group.
After randomization, 6 patients were non-compliant
with the study protocol, 9 received an excluded
intervention, 6 were reassigned, 10 were lost to
follow-up and 6 missed the follow-up appointment.
Consequently, these patients were not included in the
analyses, leaving a total of 166 (87 in the Synvisc
group and 79 in the Euflexxa group).
Table 1 summarizes the baseline characteristics of
the study participants. The Synvisc and the Euflexxa
groups did not differ on demographic or
anthropometric variables. The groups also did not
differ on co-morbid conditions with the exception that
a greater proportion of patients in the Euflexxa group
reported depression (21% vs. 10%, p = 0.02). The
baseline
scores from the patient report measures did
Table 1: Baseline Characteristics of the Study Participants.
Characteristic
Synvisc
(N = 107)
Euflexxa
(N = 96)
Combined
Sample
(N = 203)
Age – year 46+10 43+10 45+10
Female sex – no. (%) 44 (41) 36 (38) 80 (39)
Body mass index 30+5 29+5 30+5
Race
Asian 1 (1) 5 (5) 6 (3)
Black/African-
American
36 (34) 21 (22) 57 (28)
Hispanic 5 (5) 6 (6) 11 (5)
White 63 (59) 63 (66) 126 (62)
Other 2 (2) 1 (1) 3 (2)
Married – no. (%) 86 (80) 79 (82) 165 (81)
Current smoker – no. (%) 16 (15) 11(12) 27 (13)
Kellgren-Lawrence Score
Grade I – no. (%) 28 (26) 37 (39) 65 (32)
Grade II – no. (%) 44 (41) 33 (34) 77 (38)
Grade III – no. (%) 29 (27) 18 (19) 47 (23)
Grade IV–no. (%) 6 (6) 8 (8) 14 (7)
WOMAC Pain Scale 59+17 61+19 60+18
SF-36
Physical functioning 51+23 54+24 53+23
Mental health 79+15 74+18 77+17
Marx Activity Scale 5+5 5+5 5+5
EuroQOL EQ-5D Health
Rating
71+16 70+20 70+19
Arthritis Self-Efficacy Scale 6+2 6+2 6+2
Treatment response
expectation
5+1 5+1 5+1
Bilateral HA injections –
no. (%)
54 (51) 45 (47) 99 (49)
KDIR 2024 - 16th International Conference on Knowledge Discovery and Information Retrieval
502
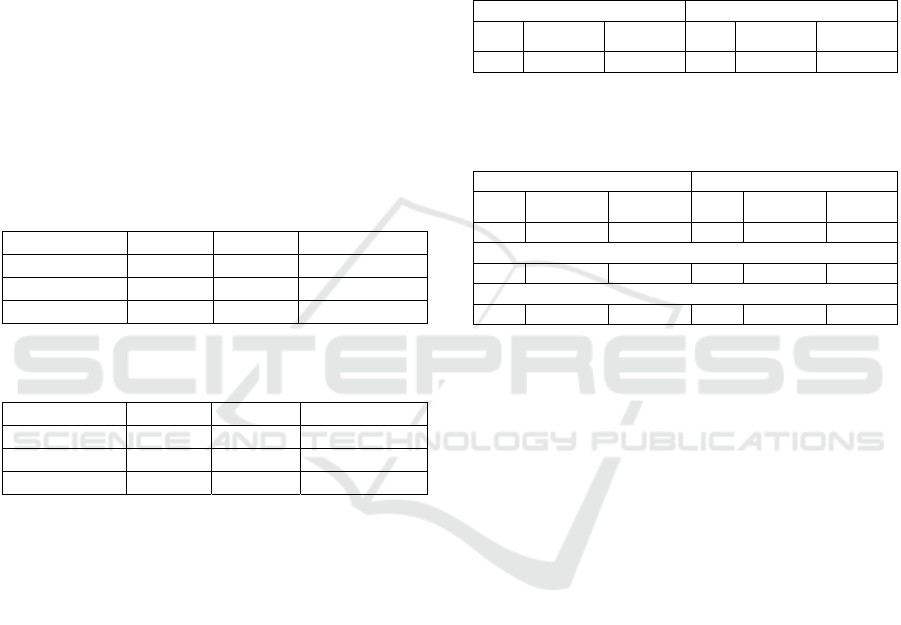
not significantly differ between the two treatment
groups either.
3.2 Primary End Points
Of the 166 patients who completed the 3-month
assessment, 84 (50.6%) were classified as treatment
responders. Within the Synvisc group, 57.5% were
responders compared to 43% of the Euflexxa group
(p = 0.04). This outcome, as well as those at the 2-
week and 6-month follow-ups, is shown in Table 2.
Table 3 displays the percentage of patients who were
classified as “recovered” based on both statistically
reliable improvement in WOMAC Pain Scale scores
and a follow-up score that fell within the range of age-
and sex-matched patients who reported having no
knee problems or any history of knee surgery (see
Mann, et al., 2012).
Table 2: Treatment Responders (20% Reduction in
WOMAC Pain) by Treatment Group.
Follow-Up Synvisc Euflexxa P Value
2 weeks 56.3% 56.3% 0.55
3 months 57.5% 43.0% 0.04
6 months 51.3% 41.5% 0.31
Table 3: Return to Normal on WOMAC Pain Scale by
Treatment Group.
Follow-Up Synvisc Euflexxa P Value
2 weeks 36.5% 25.4% 0.20
3 months 38.0% 22.6% 0.06
6 months 33.9% 30.0% 0.31
3.3 Response and Outcome Prediction
We analyze the HA data to uncover patient and
treatment factors that predict optimal response to
intra-articular injections of hyaluronic acid for knee
osteoarthritis. The treatment responder status six
months after final injection is measured by
‘WOMACP20,” Treatment Responder Status Using
20% Reduction in WOMAC Pain Scale. Recovery
status is assessed via the KOOS Scale. The machine
learning model determines which patient variables
lead to the best outcomes of HA. We also perform the
prediction for each of the two HA products to gauge
their similarities and differences in treatment
outcome characteristics.
Table 4 shows the number of patients in the
training set and the blind prediction set for predicting
reinjection status. In this analysis, for every attribute
in which there is missing data, an associated binary
attribute is created to capture whether data is missing
or not for this field. The number of attributes at three
time-points: (a) baseline screening before first
injection; (b) prior to second injection (prefix: T0);
and (c) six months after final injection (prefix: T5) are
27, 483, and 1215 respectively. Table 5 shows the
training set and blind prediction statistics used for
predicting treatment responder status and recovery
status.
Table 4: Training set and blind prediction set characteristics
for predicting reinjection status.
Training set Blind Prediction Set
Total
No
reinjection
Reinjection Total
No
reinjection
Reinjection
150 111 39 53 40 13
Table 5: Training set and blind prediction set characteristics
for predicting treatment responder status and recovery
status.
Training set Blind Prediction Set
Total
Non-
Responder
Responder Total
Non-
Responder
Responde
r
71 34 37 70 41 29
Synvisc
40 18 22 36 19 17
Euflexxa
35 21 14 30 17 13
We summarize herein the best predictive rules for
each of the analyses. Table 6 shows the prediction
accuracy for no-reinjection versus re-injection using
attributes collected up to the three stated time-points.
For the baseline results, factors that appear to be
critical includes “Weight,” “Currently Smoke
Cigarettes,” and “Smoking: Number per day.”
Baseline prediction results are comparable to Pap
Smear test accuracy (~70%).
We can observe high accuracy in predicting
success for patients using screening and T0 attributes
alone (86% blind predictive accuracy). This is very
promising for identifying patients early (just after the
first injection) who should be targeted for HA
intervention (with an expected success outcome). The
discriminatory features selected includes the Marx
Activity Scale “T0MarxCuttingSymptomFree”,
“T0MarxCutting”, effectiveness of exercise
“T0ExerciseEffective”, confidence in the injector
“T0ConfidenceInjector”, and other medications
“T0MedicationXEffective.”
Including attributes until T5 significantly
increases the accuracy for predicting the reinjection
group (from 71% to 89%). Early attributes include
“T0PhysicalTherapyEffective”,
“T0MedicationXEffective,” and overall health
“T0EQRateHealth” continue to appear among the
selected features.
Prediction of Response to Intra-Articular Injections of Hyaluronic Acid for Knee Osteoarthritis
503
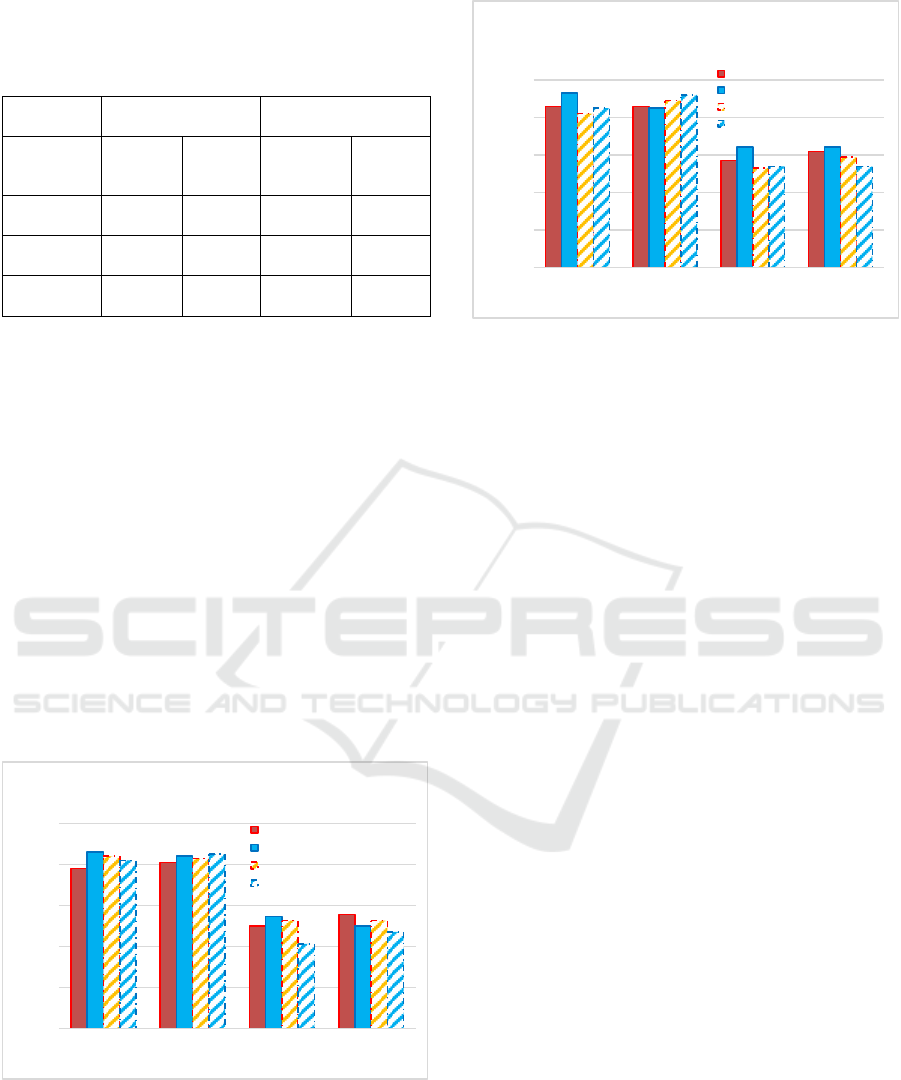
Table 6: Best predictive rule for re-injection status when
using attributes (a) baseline screening before first injection,
(b) prior to second injection, and (c) 6 months after final
injection.
Input
attributes
10-fold cross
validation
blind prediction
No-
reinjecti
on
Re-
injection
No-
reinjection
Re-
injection
Baseline
screening
71% 71% 72% 71%
Prior to 2
nd
injection
89% 74% 86% 71%
Input
attributes
84% 83% 81% 89%
Figure 2 show the 10-fold cross validation and
blind prediction accuracies for predicting treatment
responder status and recovery status for patients
injected with Synvisc and Euflexxa, respectively. For
each HA injection, four measurement frameworks are
graphed: PSO/DAMIP results for predicting
treatment responder and recovery respectively versus
the best results from the eight commonly used
classifiers, Random Forest. Our PSO/DAMIP
framework selected 3-8 discriminatory features
whereas Random Forest uses over 40 features with
poor results. Although the size of the two groups is
rather balanced, the challenge here is due to the
highly inseparable data that makes it difficult to
classify using traditional approaches. A multi-stage
approach allows the partitioning of patients from the
same group via different rules (associated with
different features).
Figure 2: Comparison of the best DAMIP classification
rules for predicting treatment responder status and recovery
status using Synvisc(top) and Euflexxa (bottom) against the
Random Forest approach.
Our study shows that early predictors can be used
to determine the group of patients who benefit the
most from HA injection. It also allows evidence-
based correction to be made during the course of
treatment. For example, after T0, the physician can
quit treatment based on results from the predictive
rule.
4 CONCLUSIONS
In 2019, about 528 million people worldwide were
living with osteoarthritis, an increase of 113% since
1990. For 365 million, the knee was the most
frequently affected joint. On average, the total cost of
knee replacement surgery ranges from $30,000 to
$50,000. This includes the cost of the surgery itself,
the hospital stays, anesthesia and other associated
medical expenses. HA treatment, on the other hand,
costs about $900 to $3,000 for a full course (three to
five injections administered over several weeks). The
range reflects the variations due to the type of HA
product and the physician's fees. Although 50% of
knee osteoarthritis patients eventually receive
surgical procedures, almost one third of these
surgeries are unnecessary. Hence intra-articular
injections of hyaluronic acid can serve as a non-
invasive cost-effective alternative to surgery for knee
osteoarthritis.
Unlike surgical options, HA injections do not
require incisions or extensive recovery periods. HA is
a substance that naturally occurs in the synovial fluid
of the joints, which helps lubricate and cushion them.
In osteoarthritis, this fluid becomes less effective,
leading to pain and reduced mobility. Thus, HA
0%
20%
40%
60%
80%
100%
DAMIP /
WOMACP20
DAMIP /
KOOSRecovery
RandomForest /
WOMACP20
RandomForest /
KOOSRecovery
Percentage of accuracy
Name of classifier
10-fold cross validation (solid) and Blind
prediction (dotted) results for Synvisc
10-fold, Non-Responder
10-fold, Responder
Blind prediction, Non-Responder
Blind prediction, Responder
0%
20%
40%
60%
80%
100%
DAMIP /
WOMACP20
DAMIP /
KOOSRecovery
RandomForest /
WOMACP20
RandomForest /
KOOSRecovery
Percentage of accuracy
Name of classifier
10-fold cross validation (solid) and Blind
prediction (dotted) results for Euflexxa
10-fold, Non-Responder
10-fold, Responder
Blind prediction, Non-Responder
Blind prediction, Responder
KDIR 2024 - 16th International Conference on Knowledge Discovery and Information Retrieval
504

injected directly into the knee joint helps restore the
lubricating properties of the synovial fluid and reduce
inflammation. By restoring lubrication, HA injections
can help improve joint mobility and reduce stiffness.
The procedure is relatively low risk, with mild
potential side effects, such as temporary swelling or
discomfort.
However, the benefits of HA injections are not
permanent; they typically last for several months.
Repeated injections may be needed for ongoing relief.
More importantly, controversies exist regarding its
safety and efficacy, the number of injections and
courses, type of preparation, duration of its effects,
and combining it with other drugs or molecules. Other
factors include patient characteristics such as age,
weight, gender, and severity of the OA. The study
uses a prospective, double-blinded clinical trial. A
multi-stage, multi-group DAMIP-based machine
learning model is utilized to uncover discriminatory
features that can predict the response status of knee
OA patients to different types of HA treatment. The
algorithm can identify certain subgroups of knee OA
patients who respond well (or those who don’t) to HA
therapy. The study’s baseline result, including factors
such as patients’ weight, smoking status and smoking
frequency, gives physicians insight for patient
treatment recommendations by identifying those
most suitable for HA injection.
To the best of our knowledge, this work presents
the first machine learning approach that predicts
patient responses to HA injections for knee
osteoarthritis. Another uniqueness of this study is that
this is the first prospective clinical trial designed such
that in addition to clinical data, patient self-reporting
data is also carefully collected. The latter is
challenging since patients often refuse or bypass
questionnaires or miss filling in forms. Self-reported
answers may be exaggerated; respondents may be too
embarrassed to reveal private details; various biases
may affect the results, like social desirability bias.
However, knee pains, whether patients can move or
do certain activities are standard questions used by
physicians and are rather routine evaluation for
active-duty personnel and athletes, and hence their
self-reporting are rather reliable. Further, there has
been no study indicating that patients would
exaggerate their pain to receive treatment to their
knee pain.
Traditional data collection methods, primarily
focusing on clinical settings, limits our understanding
of drug efficacy and patient wellbeing. Patient self-
reporting data is crucial for machine learning in
healthcare because it provides a unique, subjective
perspective on a patient's health experience, including
their symptoms, quality of life, and perception of
treatment effectiveness, which can be vital for
accurate diagnosis, treatment planning, and overall
patient care, often not captured by solely objective
medical data like lab results or imaging scans. There
is growing interest and support for the utility and
importance of patient-reported outcome measures
(PROMs) (Kingsley & Patel, 2017; Verma, et al.,
2021). This is one of the strengths of our study since
it includes a broad spectrum of patient wellbeing data.
DAMIP classifier was chosen partly due to earlier
DAMIP models have produced good predictive
accuracy on blind data for numerous clinical studies
where the training patient size is relatively small (e.g.,
in early cancer detection to uncover genomic
signatures that predict CpG islands methylation
(Feltus, et al., 2003), vaccine immunogenicity
prediction that accelerates vaccine design and target
delivery (Lee, Nakaya, et al., 2016a; Nakaya, et al,
2011, 2015; Querec, et al., 2009;) in which DAMIP
results were instrumental in the eventual world-wide
clinical trial of the Malaria vaccines (Kazmin, et al.,
2017; Lee, Nakaya et al., 2016a)). DAMIP has also
been used for studies involving very large number
patient sets with equally consistent predictive
accuracy (Lee, Wang, et al., 2016b). Multi-stage is
performed herein to manage the highly inseparable
data.
With the established predictive rule, prior to
treatment physicians can predict a patient’s response
to HA injections based on patient and treatment
characteristics. Physicians can then make empirically
informed decisions about whether to treat a particular
patient with HA and perhaps which type of HA
preparation is most likely to produce the best
treatment response for that individual patient.
Predicting treatment response based on clinically
measured variables and patient-centered well-being
data will empower physicians with an evidence-based
decision-making tool to administer the most cost-
effective intervention for the patients.
The study's follow-up period is focused on six
months after the final injection. Since knee
osteoarthritis is incurable, treatment for patients
includes rehabilitation, activity modification, weight
loss when indicated, shoe orthoses, local modalities,
and medication. For more severe cases, either HA
injections or knee surgery is selected. And HA
injections are typically given as a series of 3-5
injections, spaced one week apart, with repeat
courses usually needed every six months, depending
on the individual's pain relief duration and the
severity of their arthritis; most people experience pain
relief for several months after a full course of
injections.
Prediction of Response to Intra-Articular Injections of Hyaluronic Acid for Knee Osteoarthritis
505

The data and model derived from this study
allows physicians to administer HA products more
selectively and effectively, which will increase the
percentage of patients who experience a successful
HA therapy. Information about predicted responses
could easily be shared with patients to incorporate
their values and preferences into treatment selection.
Specifically, the classification rule can be
implemented within the electronic health record
system as an Application Programming Interface
(API). In addition, this decision support tool would
allow physicians to quickly determine whether a
patient is exhibiting at least an expected treatment
response and if not, to potentially take corrective
action. Of note, this model can also be used to predict
patient responses to other forms of treatment and
conditions.
There is a clear demand for evidence-based
medical decision-making in addition to expert
opinion, clinical experience and case reports.
Additionally, there is an increased demand for
clinical studies of prospective, rather than
retrospective, treatment assessment options. While
each of these study types has a role, the value of
evidence-based, single studies or meta-analyses of
published reports is that clinical criterion or criteria
are analyzed globally with respect to outcome.
Quantified variables that are uncovered by predictive
models are evaluated and analyzed and can serve as
important decision variables to help physicians select
the best course of treatment for patients. Evidence-
based decision-making increases outcome success.
Trends, impressions and opinions are minimized and
objective, evidence-based, outcome-driven targeted
delivery is maximized.
ACKNOWLEDGEMENTS
A portion of the results from this project (the machine
learning advances) received the first runner-up prize
at the Caterpillar and INFORMS Innovative
Applications in Analytics Award. This work is
partially supported by grants from the National
Science Foundation (IIP-1361532), and the American
Orthopedic Society for Sports Medicine. Findings
and conclusions in this paper are those of the authors
and do not necessarily reflect the views of the
National Science Foundation and or the American
Orthopedic Society for Sports Medicine. The authors
extend their deepest respect and gratitude to the late
Dr. Barton J. Mann PhD, with whom we collaborated
on the knee osteoarthritis research, and to Dr. Captain
Marlene DeMaio (retired) from Medical Corps,
United States Navy, for her clinical guidance and
collaboration on the project. We thank the
anonymous reviewers for their insightful comments.
REFERENCES
Ayis S, Dieppe P. (2009). The natural history of disability
and its determinants in adults with lower limb
musculoskeletal pain. J Rheumatol. 36:583–91. doi:
10.3899/jrheum.080455
Barbour, K. E., Helmick, C. G., Boring, M., & Brady, T. J.
(2017). Vital Signs: Prevalence of Doctor-Diagnosed
Arthritis and Arthritis-Attributable Activity Limitation
— United States, 2013–2015. MMWR. Morbidity and
Mortality Weekly Report, 66(9).
Bellamy, N. (2002). WOMAC osteoarthritis index user
guide. Version V. Brisbane, Australia.
Bellamy, N., Wilson, C., Hendrikz, J., Whitehouse, S. L.,
Patel, B., Dennison, S., & Davis, T. (2011).
Osteoarthritis Index delivered by mobile phone (m-
WOMAC) is valid, reliable, and responsive. Journal of
Clinical Epidemiology, 64(2).
Brooks, R., & De Charro, F. (1996). EuroQol: The current
state of play. Health Policy, 37(1).
https://doi.org/10.1016/0168-8510(96)00822-6
Burgers, P. T. P. W., Poolman, R. W., Van Bakel, T. M. J.,
Tuinebreijer, W. E., Zielinski, S. M., Bhandari, M.,
Patka, P., & Van Lieshout, E. M. M. (2015). Reliability,
validity, and responsiveness of the Western Ontario and
McMaster Universities osteoarthritis index for elderly
patients with a femoral neck fracture. Journal of Bone
and Joint Surgery - American Volume, 97(9).
Chan, L. L. Y., Wong, A. Y. L., & Wang, M. H. (2020).
Associations between sport participation and knee
symptoms: A cross-sectional study involving 3053
undergraduate students. BMC Sports Science,
Medicine and Rehabilitation, 12(1).
Chavda, S., Rabbani, S. A., & Wadhwa, T. (2022). Role and
Effectiveness of Intra-articular Injection of Hyaluronic
Acid in the Treatment of Knee Osteoarthritis: A
Systematic Review. Cureus.
https://doi.org/10.7759/cureus.24503
Cui, A., Li, H., Wang, D., Zhong, J., Chen, Y., & Lu, H.
(2020). Global, regional prevalence, incidence and risk
factors of knee osteoarthritis in population-based
studies. EClinicalMedicine, 29–30.
Driban, J. B., Hootman, J. M., Sitler, M. R., Harris, K. P.,
& Cattano, N. M. (2017). Is participation in certain
sports associated with knee osteoarthritis? A systematic
review. In Journal of Athletic Training (Vol. 52, Issue
6). https://doi.org/10.4085/1062-6050-50.2.08
Elgaddal N, Kramarow EA, Weeks JD, Reuben C. Arthritis
in adults age 18 and older: United States, 2022. NCHS
Data Brief, no 497. Hyattsville, MD: National Center
for Health Statistics. 2024.
Fallon, E. A., Boring, M. A., Foster, A. L., Stowe, E. W.,
Lites, T. D., Odom, E. L., & Seth, P. (2023). Prevalence
of Diagnosed Arthritis — United States, 2019–2021.
KDIR 2024 - 16th International Conference on Knowledge Discovery and Information Retrieval
506

MMWR. Morbidity and Mortality Weekly Report,
72(41). https://doi.org/10.15585/mmwr.mm7241a1
Feltus, F. A., Lee, E. K., Costello, J. F., Plass, C., &
Vertino, P. M. (2003). Predicting aberrant CpG island
methylation. Proceedings of the National Academy of
Sciences of the United States of America, 100(21).
GBD 2019: Global burden of 369 diseases and injuries in
204 countries and territories, 1990–2019: a systematic
analysis for the Global Burden of Disease Study 2019.
Hays, R. D., Sherbourne, C. D., & Mazel, R. M. (1993). The
rand 36‐item health survey 1.0. Health Economics,
2(3). https://doi.org/10.1002/hec.4730020305
Hochberg, M. C., Altman, R. D., Brandt, K. D., &
Moskowitz, R. W. (1997). Design and conduct of
clinical trials in osteoarthritis: Preliminary
recommendations from a Task Force of the
Osteoarthritis Research Society. Journal of
Rheumatology, 24(4).
Kazmin, D., Nakaya, H. I., Lee, E. K., Johnson, M. J., Van
Der Most, R., Van Den Berg, R. A., Ballou, W. R.,
Jongert, E., Wille-Reece, U., Ockenhouse, C., Aderem,
A., Zak, D. E., Sadoff, J., Hendriks, J., Wrammert, J.,
Ahmed, R., & Pulendran, B. (2017). Systems analysis
of protective immune responses to RTS,S malaria
vaccination in humans. Proceedings of the National
Academy of Sciences of the United States of America,
114(9). https://doi.org/10.1073/pnas.1621489114
Kingsley, C., & Patel, S. (2017). Patient-reported outcome
measures and patient-reported experience measures.
BJA Education, 17(4).
Lee, E. K. (2017). Innovation in big data analytics:
Applications of mathematical programming in
medicine and healthcare. Proceedings - 2017 IEEE
International Conference on Big Data, Big Data 2017,
2018-January.
Lee, E. K., & Egan, B. (2022). A Multi-stage Multi-group
Classification Model: Applications to Knowledge
Discovery for Evidence-based Patient-centered Care.
International Joint Conference on Knowledge
Discovery, Knowledge Engineering and Knowledge
Management, IC3K - Proceedings, 1.
Lee, E. K., Li, Z., Wang, Y., Hagen, M. S., Davis, R., &
Egan, B. M. (2021). Multi-Site Best Practice
Discovery: From Free Text to Standardized Concepts to
Clinical Decisions. 2021 IEEE International
Conference on Bioinformatics and Biomedicine
(BIBM), 2766–2773.
https://doi.org/10.1109/BIBM52615.2021.9669414
Lee, E. K., Nakaya, H. I., Yuan, F., Querec, T. D., Burel,
G., Pietz, F. H., Benecke, B. A., & Pulendran, B.
(2016a). Machine learning for predicting vaccine
immunogenicity. Interfaces, 46(5).
Lee, E. K., Wang, Y., Hagen, M. S., Wei, X., Davis, R. A.,
& Egan, B. M. (2016b). Machine learning: Multi-site
evidence-based best practice discovery. Lecture Notes
in Computer Science (Including Subseries Lecture
Notes in Artificial Intelligence and Lecture Notes in
Bioinformatics), 10122 LNCS.
Lee, E. K., Wang, Y., He, Y., & Egan, B. M. (2019). An
efficient, robust, and customizable information
extraction and pre-processing pipeline for electronic
health records. IC3K 2019 - Proceedings of the 11th
International Joint Conference on Knowledge
Discovery, Knowledge Engineering and Knowledge
Management, 1.
https://doi.org/10.5220/0008071303100321
Lee, E. K., Yuan, F., Man, B. J., & Egan, B. (2023a). A
General-Purpose Multi-stage Multi-group Machine
Learning Framework for Knowledge Discovery and
Decision Support. Communications in Computer and
Information Science, 1842 CCIS.
https://doi.org/10.1007/978-3-031-43471-6_4
Lee, E. K., Yuan, F., Mann, B. J., & Egan, B. (2023b).
Handling Imbalanced and Poorly Separated Data: a
Multi-Stage Multi-Group Machine Learning Approach.
Proceedings - 2023 2023 IEEE International
Conference on Bioinformatics and Biomedicine, BIBM
2023.
https://doi.org/10.1109/BIBM58861.2023.10386028
Leifer, V. P., Katz, J. N., & Losina, E. (2022). The burden
of OA-health services and economics. Osteoarthritis
and Cartilage, 30(1).
https://doi.org/10.1016/j.joca.2021.05.007
Lo, J., Chan, L., & Flynn, S. (2021). A Systematic Review
of the Incidence, Prevalence, Costs, and Activity and
Work Limitations of Amputation, Osteoarthritis,
Rheumatoid Arthritis, Back Pain, Multiple Sclerosis,
Spinal Cord Injury, Stroke, and Traumatic Brain Injury
in the United States: A 2019 Update. In Archives of
Physical Medicine and Rehabilitation (Vol. 102, Issue
1). https://doi.org/10.1016/j.apmr.2020.04.001
Lohmander, L. S., Englund, P. M., Dahl, L. L., & Roos, E.
M. (2007). The long-term consequence of anterior
cruciate ligament and meniscus injuries: Osteoarthritis.
In American Journal of Sports Medicine (Vol. 35, Issue
10). https://doi.org/10.1177/0363546507307396
Long, H., Liu, Q., Yin, H., Wang, K., Diao, N., Zhang, Y.,
Lin, J., & Guo, A. (2022). Prevalence Trends of Site-
Specific Osteoarthritis From 1990 to 2019: Findings
From the Global Burden of Disease Study 2019.
Arthritis and Rheumatology, 74(7).
https://doi.org/10.1002/art.42089
Lorig, K., Chastain, R. L., Ung, E., Shoor, S., & Holman,
H. R. (1989). Development and evaluation of a scale to
measure perceived self‐efficacy in people with arthritis.
Arthritis & Rheumatism, 32(1).
https://doi.org/10.1002/anr.1780320107
Mancuso, C. A., Sculco, T. P., Wickiewicz, T. L., Jones, E.
C., Robbins, L., Warren, R. F., & Williams-Russo, P.
(2001). Patients’ expectations of knee surgery. Journal
of Bone and Joint Surgery, 83(7).
https://doi.org/10.2106/00004623-200107000-00005
Mann, B. J., Gosens, T., & Lyman, S. (2012). Quantifying
clinically significant change: A brief review of methods
and presentation of a hybrid approach. In American
Journal of Sports Medicine (Vol. 40, Issue 10).
https://doi.org/10.1177/0363546512457346
Marx, R. G., Stump, T. J., Jones, E. C., Wickiewicz, T. L.,
& Warren, R. F. (2001). Development and evaluation
of an activity rating scale for disorders of the knee.
Prediction of Response to Intra-Articular Injections of Hyaluronic Acid for Knee Osteoarthritis
507

American Journal of Sports Medicine, 29(2).
https://doi.org/10.1177/03635465010290021601
McAlindon, T. E., Wilson, P. W. F., Aliabadi, P.,
Weissman, B., & Felson, D. T. (1999). Level of
physical activity and the risk of radiographic and
symptomatic knee osteoarthritis in the elderly: The
Framingham study. American Journal of Medicine,
106(2). https://doi.org/10.1016/S0002-9343(98)00413-
6
Mora, J. C., Przkora, R., & Cruz-Almeida, Y. (2018). Knee
osteoarthritis: Pathophysiology and current treatment
modalities. In Journal of Pain Research (Vol. 11).
https://doi.org/10.2147/JPR.S154002
Nakaya, H. I., Hagan, T., Duraisingham, S. S., Lee, E. K.,
Kwissa, M., Rouphael, N., Frasca, D., Gersten, M.,
Mehta, A. K., Gaujoux, R., Li, G. M., Gupta, S.,
Ahmed, R., Mulligan, M. J., Shen-Orr, S., Blomberg,
B. B., Subramaniam, S., & Pulendran, B. (2015).
Systems Analysis of Immunity to Influenza
Vaccination across Multiple Years and in Diverse
Populations Reveals Shared Molecular Signatures.
Immunity, 43(6).
https://doi.org/10.1016/j.immuni.2015.11.012
Nakaya, H. I., Wrammert, J., Lee, E. K., Racioppi, L.,
Marie-Kunze, S., Haining, W. N., Means, A. R.,
Kasturi, S. P., Khan, N., Li, G. M., McCausland, M.,
Kanchan, V., Kokko, K. E., Li, S., Elbein, R., Mehta,
A. K., Aderem, A., Subbarao, K., Ahmed, R., &
Pulendran, B. (2011). Systems biology of vaccination
for seasonal influenza in humans. Nature Immunology,
12(8). https://doi.org/10.1038/ni.2067
Querec, T. D., Akondy, R. S., Lee, E. K., Cao, W., Nakaya,
H. I., Teuwen, D., Pirani, A., Gernert, K., Deng, J.,
Marzolf, B., Kennedy, K., Wu, H., Bennouna, S.,
Oluoch, H., Miller, J., Vencio, R. Z., Mulligan, M.,
Aderem, A., Ahmed, R., & Pulendran, B. (2009).
Systems biology approach predicts immunogenicity of
the yellow fever vaccine in humans. Nature
Immunology, 10(1). https://doi.org/10.1038/ni.1688
Riddle, D. L., Jiranek, W. A., & Hayes, C. W. (2014). Use
of a validated algorithm to judge the appropriateness of
total knee arthroplasty in the United States: A
multicenter longitudinal cohort study. Arthritis and
Rheumatology, 66(8).
https://doi.org/10.1002/art.38685
Riddle, D. L., & Perera, R. A. (2020). The WOMAC pain
scale and crosstalk from co-occurring pain sites in
people with knee pain: A causal modeling study.
Physical Therapy, 100(10).
https://doi.org/10.1093/ptj/pzaa098
Salis, Z., & Sainsbury, A. (2024). Association of long-term
use of non-steroidal anti-inflammatory drugs with knee
osteoarthritis: a prospective multi-cohort study over 4-
to-5 years. Scientific Reports, 14(1).
https://doi.org/10.1038/s41598-024-56665-3
Sangha, O., Stucki, G., Liang, M. H., Fossel, A. H., & Katz,
J. N. (2003). The Self-Administered Comorbidity
Questionnaire: A new method to assess comorbidity for
clinical and health services research. Arthritis Care and
Research, 49(2). https://doi.org/10.1002/art.10993
Saxon, L., Finch, C., & Bass, S. (1999). Sports
participation, sports injuries and osteoarthritis
implications for prevention. In Sports Medicine (Vol.
28, Issue 2). https://doi.org/10.2165/00007256-
199928020-00005
Sharma, L., Song, J., Felson, D. T., Cahue, S., Shamiyeh,
E., & Dunlop, D. D. (2001). The role of knee alignment
in disease progression and functional decline in knee
osteoarthritis. JAMA, 286(2).
https://doi.org/10.1001/jama.286.2.188
Spector, T. D., Harris, P. A., Hart, D. J., Cicuttini, F. M.,
Nandra, D., Etherington, J., Wolman, R. L., & Doyle,
D. V. (1996). Risk of osteoarthritis associated with
long-term weight-bearing sports: A radiologic survey
of the hips and knees in female ex-athletes and
population controls. Arthritis and Rheumatism, 39(6).
https://doi.org/10.1002/art.1780390616
Theis, K. A., Steinweg, A., Helmick, C. G., Courtney-Long,
E., Bolen, J. A., & Lee, R. (2019). Which one? What
kind? How many? Types, causes, and prevalence of
disability among U.S. adults. Disability and Health
Journal, 12(3).
https://doi.org/10.1016/j.dhjo.2019.03.001
Turner, A. P., Barlow, J. H., & Heathcote-Elliot, C. (2000).
Long term health impact of playing professional
football in the United Kingdom. British Journal of
Sports Medicine, 34(5).
https://doi.org/10.1136/bjsm.34.5.332
United States Bone and Joint Initiative: The Burden of
Musculoskeletal Diseases in the United States (BMUS)
Fourth Edition. Forthcoming;
4th:http://www.boneandjointburden.org. Accessed
December 20, 2023.
United States Bone and Joint Initiative. The Burden of
Musculoskeletal Diseases in the United States (BMUS).
In: In. Fourth ed. Rosemont, IL. 2018: Available at
https://www.boneandjointburden.org/fourth-edition.
Accessed June 12, 2023
Verma, D., Bach, K., & Mork, P. J. (2021). Application of
machine learning methods on patient reported outcome
measurements for predicting outcomes: A literature
review. In Informatics (Vol. 8, Issue 3).
https://doi.org/10.3390/informatics8030056
World Health Organization. Osteoarthritis. 14 July 2023.
https://www.who.int/news-room/fact-
sheets/detail/osteoarthritis
Zhang, W., Nuki, G., Moskowitz, R. W., Abramson, S.,
Altman, R. D., Arden, N. K., Bierma-Zeinstra, S.,
Brandt, K. D., Croft, P., Doherty, M., Dougados, M.,
Hochberg, M., Hunter, D. J., Kwoh, K., Lohmander, L.
S., & Tugwell, P. (2010). OARSI recommendations for
the management of hip and knee osteoarthritis. Part III:
Changes in evidence following systematic cumulative
update of research published through January 2009.
Osteoarthritis and Cartilage, 18(4).
KDIR 2024 - 16th International Conference on Knowledge Discovery and Information Retrieval
508
