
Innovation in Geriatric Care: An AI Assistant with LLM Integration
Based on Health Guidelines
Juliana Basulo-Ribeiro
1a,*
, Nádia C. G. Matos
2,3 b
, Sabrina Magalhães Araujo
2,3,4 c
,
Nuno Capela
2,3 d
, Francisco Bischoff
2,4,5 e
, Leonor Teixeira
1f
and Ricardo Cruz-Correia
2,4,5 g
1
Department of Economics, Management, Industrial Engineering and Tourism (DEGEIT),
Institute of Electronics and Informatics Engineering of Aveiro (IEETA), Intelligent Systems Associate Laboratory (LASI),
University of Aveiro, Aveiro, Portugal
2
Department of Community Medicine, Information and Health Decision Sciences (MEDCIDS), Faculty of Medicine,
University of Porto, Porto, Portugal
3
Health Data Science Ph.D. Program, Faculty of Medicine of the University of Porto, Porto, Portugal
4
CINTESIS - Center for Health Technology and Services Research, Faculty of Medicine, University of Porto, Porto,
Portugal
5
VirtualCare, Portugal
Keywords: Large Language Model, Artificial Intelligence, Healthcare, Geriatric Care.
Abstract: With the advance of artificial intelligence and natural language processing technology, a new tool is standing
out in the field of understanding and generating natural language in a sophisticated way: the Large Language
Model (LLM). According to several authors, LLMs can be used for various types of medical cases, providing
access to different sources of information, and have opened up countless opportunities in the healthcare sector.
This work aims to share the lessons learned during the process of developing an LLM-based assistant aimed
at specific pathologies that are more prevalent in the elderly in order to support caregivers, whether they are
private individuals, home care organizations, nursing homes or others. This study has a significant potential
impact on the community by providing access to detailed information on developing an LLM-based assistant.
1 INTRODUCTION
Language is vital for human communication and self-
expression, as well as being fundamental for
interaction between people and machines (Naveed et
al., 2023). With the advance of artificial intelligence
(AI) and natural language processing technology, a
new tool is coming to the fore in the field of
understanding and generating natural language in a
sophisticated way: the Large Language Model
(LLM). Language modeling is a long-standing
research topic, dating back to the 1950s, and today,
LLMs have evolved from statistical language models
a
https://orcid.org/0000-0002-3411-3519
b
https://orcid.org/0009-0007-7841-6574
c
https://orcid.org/0000-0003-1443-2106
d
https://orcid.org/0009-0007-7841-6574
e
https://orcid.org/0000-0002-5301-8672
f
https://orcid.org/0000-0002-7791-1932
g
https://orcid.org/0000-0002-3764-5158
to neural language models, pre-trained language
models and finally to large-scale LLMs (Minaee et
al., 2024). Examples of LLMs include OpenAI's GPT
(Generative Pre-trained Transformer), Google's T5
(Text-To-Text Transfer Transformer) and Google's
BERT (Bidirectional Encoder Representations from
Transformers) (Brown et al., 2020; Devlin et al.,
2018; Raffel et al., 2019).
Smith et al. (2024) points out 10 rules for using
LLMs in science, as these AI tools are set to change the
way we operate in many areas: (1) Recognize that
LLMs are powerful, but they can make mistakes; (2)
Confirm the information generated by the models with
Basulo-Ribeiro, J., Matos, N. C. G., Araujo, S. M., Capela, N., Bischoff, F., Teixeira, L. and Cruz-Correia, R.
Innovation in Geriatric Care: An AI Assistant with LLM Integration Based on Health Guidelines.
DOI: 10.5220/0013096100003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 361-371
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
361

reliable sources; (3) Train the model with reliable data
to ensure that it is representative and free of bias; (4)
Clearly specify the context so that the answers are more
accurate; (5) Be aware of the biases present in the data
used to train the model, and take steps to mitigate them;
(6) Collaborate and share knowledge, experiences and
challenges to achieve best practices for preparing
LLMs; (7) Maintain transparency by disclosing the
methodology, tools and limitations when presenting
work that incorporates LLMs; (8) Consider the ethical
implications of using language models; (9) Use models
as a support tool, but not as a substitute for critical
thinking and rigorous scientific methods; (10) Actively
collaborate to improve language models and promote
responsible and ethical AI practices.
Today, we can already imagine a future world
where health care is monitored not only by physicians
and nurses but also by solutions that integrate AI,
capable of understanding, interpreting, and even
predicting health needs. This is the world where
LLMs can play an extremely vital role in healthcare.
Behind the scenes of the digital revolution, these
models are shaping a new era of healthcare, where
communication between patients and healthcare
professionals reaches unprecedented levels of
personalization and efficiency. This is a topic
discussed in the literature, where Mehandru et al.
(2024) mention in their study that: "Recent
developments in large language models (LLMs) have
unlocked opportunities for healthcare, from
information synthesis to clinical decision support.".
LLM can help to improve patient care and medical
diagnosis (Nassiri & Akhloufi, 2024)
According to several authors, LLMs can be used
for various types of medical cases, giving access to
different sources of information and tools, including
clinical guidelines, databases with electronic health
records, among others, which shows the possibility
and importance of developing LLMs for health
based on guidelines (Mehandru et al., 2024; Park et
al., 2023; Yang et al., 2023). Smith et al. (2024)
point out that LLMs have the potential to transform
science, but they also present significant challenges
and risks. Thus, evaluating LLMs becomes crucial
in all contexts; however, it is in the medical context
that evaluation is most critical (Nassiri & Akhloufi,
2024). The accuracy, reliability and effectiveness of
LLMs are essential to ensure that the information
provided can be used safely and effectively in
healthcare, and in an environment where decisions
can have a significant impact on people's lives,
rigorous evaluation of LLMs becomes not only
necessary but indispensable (Mehandru et al., 2024;
Yang et al., 2023). Nassiri and Akhloufi (2024)
mention the importance of training the model using
specific health documents, all to reduce the risk of
producing incorrect information. A significant
ethical concern with the use of these models is the
risk of perpetuating biases and inaccuracies in
medical data and information, which can severely
impact patient care (Nassiri and Akhloufi, 2024). As
Nassiri and Akhloufi (2024) point out, there are
many "technical and ethical issues that need to be
resolved before LLMs can be used extensively in the
medical field".
It is crucial to emphasize the need for a
collaborative and multidisciplinary approach to this
type of AI-based technology, with interaction
between different specialists, such as: technology
professionals, healthcare professionals, and health
regulators. This collaboration not only promotes
innovation in healthcare but also ensures that these
technologies are implemented responsibly,
maximizing patient benefits and minimizing potential
risks. (Cascella et al., 2024; Piñeiro-Martín et al.,
2023; Thapa & Adhikari, 2023)
Population aging is one of the most significant
demographic phenomena of the 21st century, and as
the elderly population grows, so do the challenges
associated with managing health conditions specific
to this age group. Among these conditions, non-
oncological pathologies are particularly prevalent and
require special attention from both caregivers and
healthcare professionals. Often, a lack of knowledge
about these diseases and the best practices for
preventing or managing them results in complications
and a deterioration in the quality of life (Maresova et
al., 2019; Sun & Li, 2023; World Health
Organization, 2015, 2022).
This paper aims to present a project to develop an
assistant based on LLMs, which uses health
guidelines as a basis for supporting the care of the
elderly. This initiative follows the recommendations
proposed by Nassiri and Akhloufi (2024) in their
study, mentioned earlier in this section.
Consequently, this article is structured as follows:
section 2 describes the practical case carried out and
the discussion; and at the end, section 3 presents the
final remarks, which include the conclusion, the
contributions of this work, the limitations and future
work for the advancement of LLMs.
2 PRACTICAL STUDY
2.1 Goals and Methods
This article analyses the knowledge acquired
HEALTHINF 2025 - 18th International Conference on Health Informatics
362
during the development of an assistant designed to
deal with specific non-oncological pathologies that
commonly affect the elderly. The main objective is to
provide adequate support to carers, whether they are
private individuals, home care organisations, nursing
homes or others. In addition, this paper explores the
challenges encountered in developing a prototype of
a large language model (LLM) adapted to the care of
the elderly. It also seeks to understand how the
development process can reveal wider obstacles that
any research can face when working with scientific
documentation, including the specificities of LLMs
and the training techniques required for their effective
application.
To analyse the lessons learnt during the
development of the assistant, a qualitative method
was adopted, based on a documentary review and
critical reflection on the team's experiences
throughout the project.
The methodology was divided into three main
stages:
i. Data collection: Review of documents and
records related to the LLM development
project, including planning documents and
reports/documents of findings over time. In
addition, informal interviews were conducted
with team members involved in developing
the assistant to gain insights into the
challenges faced, strategies adopted, and
lessons learned.
ii. Data Analysis: Organization and
categorization of the data collected,
highlighting the main areas of learning
identified during the development process.
iii. Summary and Discussion: A summary of the
analysis results, highlighting the main lessons
learned throughout the development process.
In addition, a critical discussion was held on
the implications of these learnings for future
projects of this scope and practice in general.
Health professionals and technology developers were
involved in this process to promote this project's
effective and responsible development.
2.2 Results
2.2.1 Description of the Assistant
The work developed, an assistant based on an LLM,
is an innovative tool designed to support caregivers
of the elderly by providing detailed information on
prevalent diseases and medical guidelines. It uses
different datasets from the Transparency Portal and
INE Pordata, which can be updated every six months
and every year. The model acts as a conversational
assistant, able to answer questions and offer specific
educational material aimed at the most common
pathologies and care among the elderly. Among the
main beneficiaries are nursing homes, parish
councils, pharmacies, patient associations and home
care providers.
To guarantee the accuracy and relevance of the
information, this research was based on reliable
sources such as the World Health Organization
(WHO), PubMed and Elsevier, which ensures the
project's high technical feasibility. The tool's
innovation is evident, not only in the way it
transforms complex data into useful answers but also
in its ability to offer caregivers continuous support
24/7.
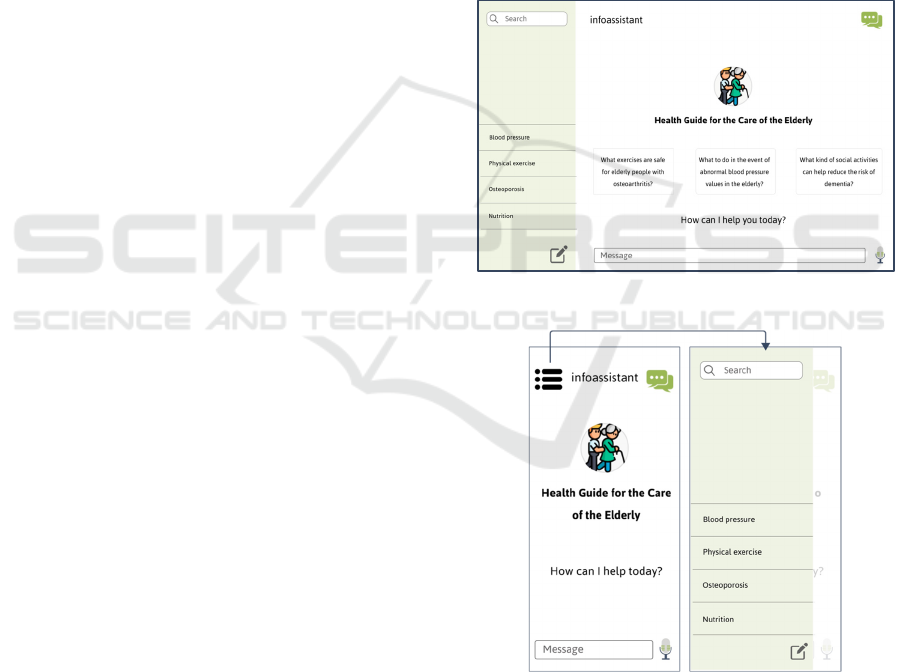
Figure 1: LLM "infoassistant" desktop mock-up.
Figure 2: LLM "infoassistant" mobile mock-up.
The tool's relevance to external entities is also
highlighted, as it facilitates the dissemination of
knowledge and good practices, contributing to
improving care provided to the elderly. This
combination of innovation, technical feasibility and
positive impact makes this project a valuable solution
Innovation in Geriatric Care: An AI Assistant with LLM Integration Based on Health Guidelines
363
in the field of geriatric care. Figure 1 and Figure 2
show a prototype of the natural language conversation
assistant that we intend to make available at the end
of the project in desktop and mobile versions,
respectively.
2.2.2 Approach to Preparing the Assistant
This subsection aims to present the action plan
conducted from the decision to develop this project to
its preparation and availability. The plan for this
project was divided into several work packages (WP)
to make it easier to manage and execute them,
allocating the different resources to each one.
WP1: Data Collection (Search and Download
of Guidelines) The first WP in the initial phase,
focused on searching for and downloading health
guidelines related to non-oncological pathologies
prevalent in the elderly population, using specialized
websites such as PubMed. These documents, which
are generally in PDF format, constitute the database
for the project. At a later stage, this task was
automated using Python technology, allowing
relevant documents to be identified, downloaded and
stored periodically. This systematic process, in line
with the requirements identified, reduces the
likelihood of errors and does not require human
intervention. The methodology involved creating
specific queries, processing the results, extracting
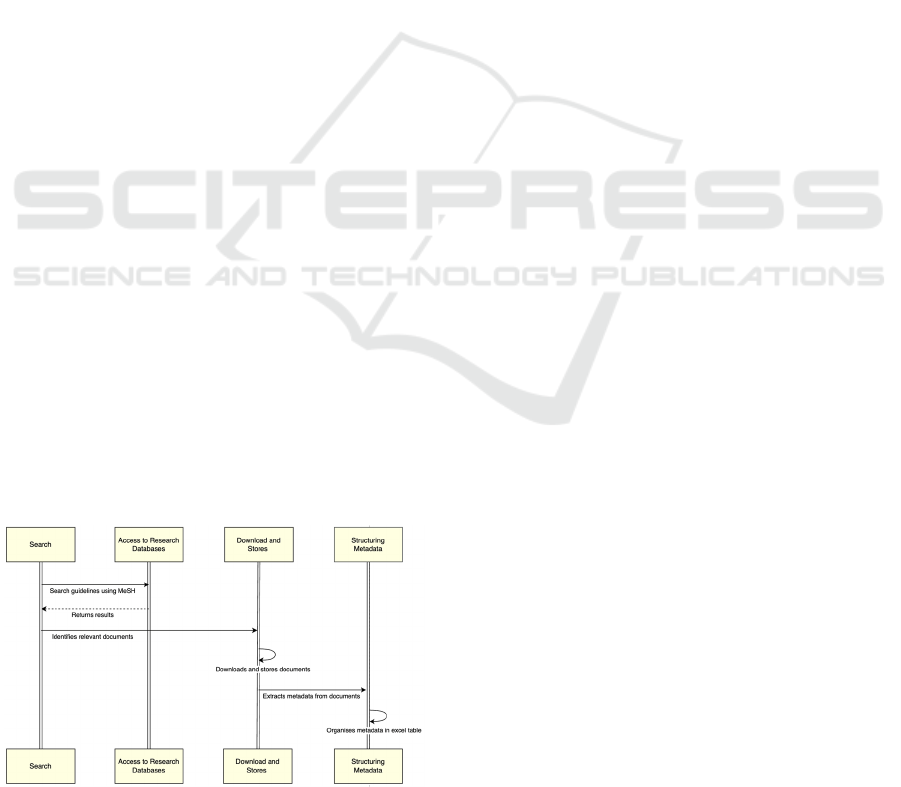
relevant data and storing the information. Figure 3
illustrates the workflow of this WP, with the 'Search'
stage representing the process of searching for
guidelines using MeSH (Medical Subject Headings)
terms; the 'Access to Research Databases' stage
returns the results of the previous task and identifies
the most relevant documents. The public API
(Application Programming Interface ) of the NCBI
Entrez system (https://www.ncbi.nlm.nih.gov/
books/NBK25501/ ) was utilized, providing access to
a wide range of Entrez databases, including PubMed,
PMC, Gene, Nuccore and Protein. The third stage,
Figure 3: Schematic representation of WP1.
'Download and Store', represents the process of
downloading and storing the guidelines, as well as
extracting their metadata. Finally, the ‘Structuring
Metadata’ stage aims to organize the metadata
according to the structure defined for the inputs of the
next work package, WP2.
WP2: Processing the Guidelines The second
WP aims to analyse and convert the PDF documents
collected (during the WP1 process) into text
(questions and answers) to extract specific
information from these documents. Group the
guidelines by disease, considering the International
Statistical Classification of Diseases and Related
Health Problems, 10th Revision (ICD-10) system and
for each disease coding, symptoms, signs, abnormal
findings, complaints, social circumstances and
external causes of injury or disease. With this set of
information, a range of questions and answers was
identified, which would serve as the basis for the
following WP.
WP3: Develop and Refine the AI Assistant
Considering that the assistant was designed to answer
questions about non-oncological pathologies
prevalent in the elderly population, based on the
guidelines collected and processed in the previous
work packages, this stage involved setting up a
workspace in the AnythingLLM (AnythingLLM,
2024) tool, a framework to facilitate designed to
facilitate interaction with natural language models,
delivering precise answers. Various approaches were
explored and combined during this stage, such as
fine-tuning, transfer learning, RAG (Retriever-
Augmented Generation), or even a combination of
these techniques. These methods, defined in detail
later in this document, allowed for the refinement and
adjustment of the assistant to ensure it could provide
useful and accurate answers to questions related to
non-oncological pathologies in the elderly population
based on the guidelines collected and processed. The
outcome of this WP is an assistant capable of
delivering relevant and precise responses. Another
output of this WP is an API that allows other systems
to access the developed assistant.
WP4: Making the Assistant Available The
last WP of the project involved developing an
interface that makes the assistant available, allowing
users to interact directly with it. This interface would
invoke the API developed in the previous WP to
allow the assistant to be incorporated into another
system, making it possible to clarify doubts, always
based on the health guidelines collected, thus
providing a useful tool for both caregivers,
professionals in the field and even the elderly
themselves.
HEALTHINF 2025 - 18th International Conference on Health Informatics
364
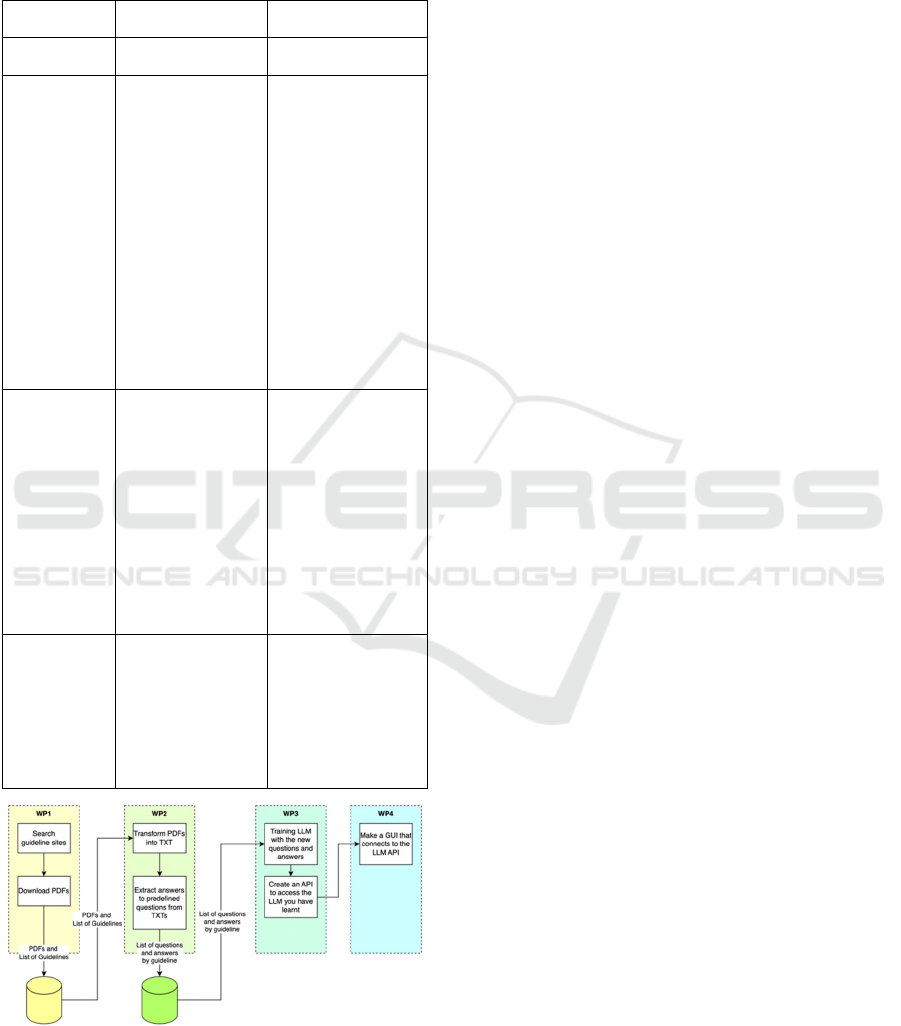
Table 1 summarizes this information, and Figure
4 illustrates it, considering the sequence of events
over the 4 WPs.
Table 1: Summary of each work package.
Work
Packages
Objective
Considerations/
Outputs
WP0: Project
Management
WP1: Search
and download
guidelines
i. find/identify the
guidelines;
ii. download the
guidelines;
iii. Put the guidelines
into a paste;
iv.Generate a list of
documents in the
folder with
information about
the guidelines;
v.Extra task:
Identify the main
illnesses and
needs of the
elderly within the
project's scope.
• Folder with
guidelines;
• List with
Timestamp, DOI,
Name, URL
• Various formats:
.pdf, .doc, .txt
WP2: Edit the
guidelines
i. Define the
variables to
extract;
ii. Extract the data
(the result is a
table);
iii. Translate the data
into a
question/answer
format (table).
• List of data by
guideline - 1st
phase in EN
• Context:
Population; gender,
ethnicity, age, etc...
• Decision
algorithm: what the
guideline proposes
as a solution
• Question/Answer
format - 1st phase
in EN
WP3:
Develop and
refine the AI
assistant
Use the WP2 data
and refine LLM with
the
questions/answers.
The output/result is a
service that, when
invoked, establishes
the dialog.
• API to send a
question and
receive a reply
• API for dialog
Figure 4: Schematic illustration of the LLM development
project.
2.2.3 Lessons Learned
This section aims to share lessons learned throughout
the development process of this project. By 'lessons
learned,' we mean the challenges identified during the
execution of each WP of the project and the
methodologies that were applied to address them,
including both the strategies that proved effective in
solving the problem and those that did not achieve the
expected results.
WP1: Search and Download Guidelines
• Efficient Research
Creating specific queries using MeSH terms ensures
that all relevant documents are identified, but failure
to improve them can jeopardize the quality and
relevance of the results returned.
• Data Processing
The conversion of content in .pdf format to text (i.e.,
encoding, special characters), tables, flowcharts and
figures sometimes leads to a lack of precision in the
information extracted, which can be accentuated by
different document formats and structures. This lack
of precision, although not completely unknown, takes
on greater relevance when we talk about the health
sector since inaccurate information can lead to advice
and/or decision-making that jeopardizes the health
and safety of patients. To mitigate this situation, it is
important to develop efficient algorithms to extract
and organize the necessary metadata automatically,
minimizing human intervention and errors. In
addition, it is necessary to define an effective method
for segmenting the data, such as the Chunking method
(Dozza et al., 2013). The method must divide the
content in such a way as to maintain the connection
between data that shares the same context; for
example, when extracting information from a health
document, the algorithm must automatically identify
and group together sections relating to the same
patient, diagnosis or treatment, ensuring that the
information extracted is accurate and contextualized.
• Storage and Organization
Storing the guidelines as well as their metadata in an
organized and accessible way proved to be a major
challenge, due to the periodic updating of the data
without redundancies, maintaining the integrity and
timeliness of the information.
• Tokens
Another challenge faced was the fact that many
research databases use tokens in the process of
downloading guidelines, and access tokens usually
have a limited lifetime, expiring after a certain period.
Automating this flow becomes complicated as this
Innovation in Geriatric Care: An AI Assistant with LLM Integration Based on Health Guidelines
365

requires tokens to be obtained and renewed
frequently. In addition, there may also be usage
limitations, i.e., limitations on the number of requests
that can be made within a certain period, which
requires careful management to ensure that the
defined limits are not exceeded. Thus, automating
tasks that depend on tokens adds a layer of
complexity to the data collection process. Managing
the validity and security of tokens, automating
renewal and preparing the system for potential
changes to third-party systems are essential strategies
for mitigating these types of challenges.
WP2: Edit the Guidelines
• Additional Section in the Guidelines
Since health guidelines do not have a standard
structure, we propose adding a section with specific
fields to improve their usefulness and make them
easier for algorithms to understand. By incorporating
these additional fields, the models could more easily
interpret the health guidelines, allowing them to be
better trained. This would ensure access to reliable
information in a clear and effective way. These fields
could include:
o Summary: A summary of the main
recommendations and conclusions of the guideline,
allowing a quick understanding of its content.
o Content Overview: A more detailed description
of the topics covered in the guideline, highlighting the
areas of focus and the main information provided.
o Purpose and Usefulness: A clear explanation of
the objectives of the guideline and how it can be used
in clinical practice or even in the reformulation of
health policies.
o Who is it for: An identification of the health
professionals, managers, researchers or other
stakeholders for whom the guideline has been
developed, helping to ensure that it is aimed at the
right audience.
o Structure of the Guideline: A description of how
the guideline is organized, including main sections,
subsections and how to navigate through the
document.
o Frequently Asked Questions: A list of common
questions about the guideline and its answers,
addressing concerns that users may have when
implementing its recommendations.
• Versions in the Guidelines
In addition, these guidelines should have clearly
identified versions so that algorithms and models can
easily check whether they are using the latest version
in order to ensure maximum effectiveness and
relevance of the content provided. Including a
versioning system would help ensure that the
information and recommendations are always up to
date, reflecting the most up-to-date information. This
approach would also make it possible to verify
changes over time, making it easier to understand
evolutions and updates in the guidelines. To do this,
the guidelines could have a section or be
accompanied by a document where it is possible to
have a summary of what has been
added/changed/removed, a "release note". This would
not only make it easier to compare the different
versions but would also help answer questions about
changes in procedures.
WP3: Train the AI Assistant
• Versions of LLM Models and Software
Version management is crucial in software and LLM
models to maintain a clear timeline of its
development and the functionalities that make it up.
Each version should record changes in functionality,
performance and bugs fixed. This makes it possible to
compare different versions to assess performance
improvements directly. This practice helps maintain
and update systems, provides transparency for end
users, and facilitates the reproduction of results in
scientific research.
• Tool Used to Develop the Wizard
For the project's development, the AnythingLLM
(AnythingLLM, 2024) tool was chosen because it is
an open-source platform offering significant
flexibility for customization and integration into
several projects. This solution supports various
language models, including proprietary models, such
as GPT-4, and open-source models, such as Llama
and Mistral (https://useanything.com/). It includes a
graphical user interface that facilitates interaction
with the language model, integration with various
data sources used to train and refine the models, and
customization based on the specific needs of your
application, all easily and intuitively. With
AnythingLLM, there is no need to worry about
privacy issues, a relevant point given that we are in
the health sector, as it already implements measures
to ensure that user data is treated securely and
privately.
• Settings at AnythingLLM
Within the AnythingLLM tool, there are several
optional parameters that, while not mandatory, should
be adjusted or defined, such as the model to be used
(explained in the next few topics), to customize the
model's behavior based on the specific needs of each
project. Below are some of the settings available in
the desktop version that can impact the model's
HEALTHINF 2025 - 18th International Conference on Health Informatics
366

behavior. Figure 3 shows a screenshot of the
workspace settings.
o Chat Mode: The "Chat" option, when active,
sends the model the entire context of the
conversation, i.e., the history of the conversation
in the window. The "Query" option sends only
the question asked by the user. Although context
is important, it also contributes to performance
degradation, so evaluating the objective and
finding a balance is important.
o Chat History: This is the number of
questions/answers that will be sent as a history to
the model whenever we are in "Chat" mode.
o Prompt: Here, we should put relevant
information and the instructions, in order to
contribute to improving the performance of our
assistant. For example, give a summary of the
content of the documents that will serve as a
knowledge base for the model we are using.
o LLM Temperature: This parameter relates to the
creativity of the LLM. It is set to a value between
0 and 1. The higher the value, the more creative
the model's responses will be. By default, the
software uses a value of 0.7, which is
recommended by most models. In the test phase,
we used lower values since we are in the health
field. However, the answers provided by the
model were very literal, lacking the
personalization and naturalness of natural
language. For this reason, we opted to restore the
default value.
Figure 5: Workspace settings for the desktop version of
AnythingLLM.
• Testing the Different Existing Models
The ability to quickly test different LLM models is
essential for iterating and improving the quality of
proposed solutions. Tools such as LM Studio
(Element Labs, 2023) make it possible to conduct
these tests quickly and intuitively, offering user-
friendly interfaces and detailed analysis of model
performance locally (on the machine). These tools
can be configured to run a series of tests, such as
assessing language comprehension, generating text
and the ability to answer questions, which provides
important metrics on the usefulness and quality of
each model tested. All of this makes it possible to
make better choices about which model(s) to use,
depending on the purpose you want to achieve since
the models are built for specific purposes, which
makes them more accurate for the subjects they were
developed for.
Another issue with models is that you must bear
in mind that there are models that only perform well
and efficiently in a specific language (e.g., EN)
because they have been built and trained in that
language and are, therefore, not multilingual. That is
why it is important to test different models so that you
can choose based on your use case.
• Choosing a Model
At an early stage of the project, a document was
drawn up with the pros and cons of the different
models available, such as Falcon - Technology
Innovation Institute (TII) in Abu Dhabi; Ihama 2 -
Meta; Bloom; MPT-7B - MosaicML; Vicunha-13B -
LMSYS ORG; GPT-3 - OpenAI; BERT; among
others. However, after choosing the tool, an
exhaustive analysis was also carried out of all the
existing models in the Desktop version of
AnythingLLM up to the date of development (May
2024), such as: LLaMA3 (Uncensored); LLaMA2
13B; LLaMA 3; CodeLlama 7B; Mistral 7B; Mistral
8x7B; Gemma 2B; Gemma 7B; Phi-2; Orca-Mini;
Orca-Mini 7B; Orca-Mini 13B; among others.
When choosing the model to use in LLM to
generate answers based on health guidelines
regarding the care of the elderly and the most
common pathologies in that age group, several factors
need to be taken into account, such as: the size of the
model, the ability to handle domain-specific
information and whether or not the model has been
optimized for health applications, as they may not
have the controls or training necessary to handle
sensitive and accurate medical/health information. In
addition, it is important to ensure that any model used
complies with local and international health data
privacy regulations, such as GDPR and HIPAA,
where applicable. Given the information found, it was
decided to choose the Orca-Mini 13B model.
• Orchestrating the Solution
Orchestration in LLM solutions involves managing
and automating various tasks and services that
comprise the LLM infrastructure, such as model
training, testing, and model deployment. Using
orchestration software like Flowise (Flowise, 2024)
allows you to manage these tasks efficiently. In this
case, Flowise was used for this purpose. This type of
Innovation in Geriatric Care: An AI Assistant with LLM Integration Based on Health Guidelines
367

solution also allows different models to be used in the
same solution, with questions being directed to the
model with the best performance for the specific task.
This ensures that the solution takes full advantage of
the different capabilities of each model, maximizing
the accuracy and efficiency of the answers provided.
• Model Training
An unclear concept in this type of project is the issue
of model training. In the context of this project, the
term "training" will be used in a broad sense, referring
both to the adjustment of model parameters (as in
Fine-Tuning) and to the adaptation of the model
through other techniques and approaches, which will
be detailed later in this document. Since a pre-trained
model was used, it was necessary to understand which
techniques and/or approaches were used to adapt the
model to the dataset, the guidelines.
Fine-Tuning is a technique that can be applied in
these situations where pre-trained models are used. It
involves further training the model using a specific
dataset to adjust and optimize its performance for a
particular task. This is achieved by adjusting the
model's parameters with an additional specific
dataset, the guidelines. Fine-tuning the base model
with specific data from the collected health guidelines
ensures that the model understands and responds to
the nuances and specificities of these guidelines. To
implement this technique, machine learning
frameworks such as PyTorch or TensorFlow are
recommended for adjusting the model. Libraries such
as Hugging Face Transformers are also very helpful
in this process.
Another technique is Transfer Learning, where
the model pre-trained on a specific task is adapted to
another related task. Instead of training the model
from scratch, the knowledge gained during the initial
training is reused, saving time and computational
resources.
Retrieval-Augmented Generation (RAG),
although not a training technique in the traditional
sense, is a powerful approach to improving the quality
of answers generated by language models during
inference, especially in question-and-answer systems.
It combines information retrieval and text generation.
Rather than relying solely on the language model to
generate answers, this approach first retrieves
relevant documents from a database and then uses this
information to generate more accurate and
contextually relevant answers. This enhances the
accuracy and relevance of responses, as the model
does not just rely on its prior training but also uses up-
to-date, context-specific information, ensuring that
answers are always based on the most relevant
documents by retrieving these guidelines before
generating an answer. When combined with training
techniques such as Fine-Tuning and Transfer
Learning, RAG can contribute to a highly effective
and accurate assistant, capable of providing informed
and relevant answers based on specific guidelines.
It is therefore important to understand that
“training” an LLM in this project involves several key
considerations, and the choice of the appropriate
techniques and approaches depends on various
factors, including the project's objectives, available
resources and the type of data. Below is a table
summarizing the techniques and their applicability.
Table 2: Summary of training techniques and their
applicability.
Technique Description Application
Transfer
Learning
Use a pre-trained
model as a starting
point and adjust it for
the specific task.
• When you have a
limited set of
specific data.
• To save time and
computing resources
by using pre-trained
models.
Fine-Tuning
Further train a pre-
trained model with a
specific data set to
improve performance
on a specific task.
• When you have
domain-specific data
and want to adapt a
pre-trained model to
improve accuracy
and relevance.
Supervised
Learning
Training a model
with labeled data,
with the goal of
learning a function
for mapping inputs to
outputs.
• When you have a
large set of labeled
data.
• For tasks such as
text classification,
answering specific
questions, or
sentiment analysis.
Unsupervise
d Learning
Training a model
with unlabeled data
to find hidden
patterns or structures.
• When the data is not
labeled.
• For tasks such as
clustering or
dimensionality
reduction.
Semi-
Supervised
Learning
Combining labeled
and unlabeled data to
improve model
performance.
• When you have a
limited amount of
labeled data but a
large amount of
unlabeled data.
• To increase model
accuracy with less
labeling effort.
Reinforceme
nt Learning
Training a model
where they learn to
make decisions
through rewards and
punishments.
• For tasks that
involve a sequence
of decisions.
WP4: Make Assistant Available
• Summoning the Assistant
Considering the specific characteristics of the
AnythingLLM framework, it is important to note that
invoking the wizard is only possible when using the
HEALTHINF 2025 - 18th International Conference on Health Informatics
368

contained version of the tool. Generally, the desktop
version is used by a single user or in an individual
development environment, where there is no room for
the scalability and management of multiple instances
required in a productive environment. So, given that
the aim was to enable multi-user system execution
and to "publish" the workspace on websites or other
platforms, we decided to replicate the development
process described in WP3 with the Docker version of
the tool. Throughout the process, it was possible to
see some differences, both in terms of the settings
available and in terms of customization, with greater
flexibility without significant impacts in terms of
complexity for the user.
Another point is that the tool incorporates a chat
widget that allows the workspace and its built-in
knowledge base to be readily displayed on a website.
Figure 6: An example of a script tag embeds.
2.3 Discussions
This article aims to report on work in progress to
create a health assistant based on guidelines that
support an LLM. This effort corroborates the idea put
forward by several authors that it is possible to create
virtual health assistants based on reliable information
(Mehandru et al., 2024; Park et al., 2023; Yang et al.,
2023).
Advances in innovative LLM technology have
shown significant potential to transform medical
practice by providing quality and accessible care to
healthcare professionals and patients, as noted by
several authors in the literature (Mehandru et al.,
2024; Nassiri & Akhloufi, 2024). However, due to the
sensitive and critical nature of the healthcare sector in
which they operate, it is imperative that these
assistants are rigorously assessed at a clinical level. In
their study, Nassiri and Akhloufi (2024) highlight the
importance of this clinical assessment for any AI-
based healthcare tool. In line with this thinking, our
project recognizes the need to carry out this
assessment to validate the development of this
healthcare assistant.
Another relevant point to highlight is the need to
continually train the model with new data and
updated guidelines to maintain the assistant's
relevance and accuracy, a critical component for the
long-term success of any AI tool in healthcare.
Finally, it is worth noting the importance of
multidisciplinary collaboration between technology
developers, healthcare professionals and regulatory
authorities to ensure that the development and
implementation of LLM-based healthcare assistants
are carried out in a responsible manner, as mentioned
by several authors in the literature (Cascella et al.,
2024; Piñeiro-Martín et al., 2023; Thapa & Adhikari,
2023). This collaborative approach safeguards patient
safety and well-being.
3 FINAL REMARKS
3.1 Conclusion
Today, significant progress has been made in the field
of LLMs. This progress results from the growing
demand for innovative solutions to combat many
daily challenges. These advances aim not only to
improve the performance of LLMs in challenging
tasks but also to explore new possibilities for
previously unexplored applications, which will have
a transformative impact on various areas of
knowledge.
The final product resulting from this work, which
will be presented to users, is more like a movie than a
static image due to the dynamic nature of LLMs.
Unlike an image, which remains the same over time,
LLMs are designed to learn and adapt through use and
interaction with users. This allows for continuous
improvement of the responses it provides.
In developing the assistant presented in this study,
the processes were initially conducted manually,
reflecting a more exploratory initial phase. As the
project progressed, there was a natural evolution
towards automation. This "maturation" was
evidenced by the progressive implementation of
automated systems in each WPs. This transition made
it possible to: optimize efficiency, reduce the time and
effort required, and increase the accuracy and
consistency of the results achieved.
3.2 Contributions and Implications
This study has a significant potential impact on the
community by providing access to detailed
information on how to prepare an assistant based on
LLMs. This resource is extremely useful today, not
only in the health area but in all sectors of activity.
This LLM is an important tool to help people in their
Innovation in Geriatric Care: An AI Assistant with LLM Integration Based on Health Guidelines
369

daily lives, facilitating access to relevant health
information quickly and effectively.
3.3 Limitations and Future Work
One of the limitations of this study is that it has not
been clinically validated. Therefore, in future work,
we would like to evaluate LLM clinically. The current
stage of development serves as an opportunity to
conduct tests and consequent improvements, which
will guarantee the effectiveness of the assistant when
it is introduced to the market.
ACKNOWLEDGEMENTS
This work was supported by Portuguese funds
through the Institute of Electronics and Informatics
Engineering of Aveiro (IEETA) (UIDB/00127/2020)
funded by national funds through FCT - Foundation
for Science and Technology. This work has also been
done under the scope of – and funded by – the Health
Data Science Ph.D. Program of the Faculty of
Medicine of the University of Porto, Portugal –
heads.med.up.pt. The authors are thankful to the
Program and its faculty for investing in their students
and funding the open-access publication of their
research. Additionally, this article was developed
under the Mobilizing Agenda No. 41 - HfPT –
HEALTH FROM PORTUGAL, co-funded by the
PRR and the European Union through the Next
Generation EU mechanism.
REFERENCES
AnythingLLM. (2024). AnythingLLM.
Brown, T. B., Mann, B., Ryder, N., Subbiah, M., Kaplan,
J., Dhariwal, P., Neelakantan, A., Shyam, P., Sastry, G.,
Askell, A., Agarwal, S., Herbert-Voss, A., Krueger, G.,
Henighan, T., Child, R., Ramesh, A., Ziegler, D. M.,
Wu, J., Winter, C., … Amodei, D. (2020). Language
Models are Few-Shot Learners. http://arxiv.org/abs/
2005.14165
Cascella, M., Semeraro, F., Montomoli, J., Bellini, V.,
Piazza, O., & Bignami, E. (2024). The Breakthrough of
Large Language Models Release for Medical
Applications: 1-Year Timeline and Perspectives. In
Journal of Medical Systems (Vol. 48, Issue 1). Springer.
https://doi.org/10.1007/s10916-024-02045-3
Devlin, J., Chang, M.-W., Lee, K., & Toutanova, K. (2018).
BERT: Pre-training of Deep Bidirectional
Transformers for Language Understanding.
http://arxiv.org/abs/1810.04805
Dozza, M., Bärgman, J., & Lee, J. D. (2013). Chunking: A
procedure to improve naturalistic data analysis.
Accident Analysis and Prevention, 58, 309–317.
https://doi.org/10.1016/j.aap.2012.03.020
Element Labs, Inc. (2023). LM Studio (4).
Flowise. (2024). Flowise.
Maresova, P., Javanmardi, E., Barakovic, S., Barakovic
Husic, J., Tomsone, S., Krejcar, O., & Kuca, K. (2019).
Consequences of chronic diseases and other limitations
associated with old age - A scoping review. BMC
Public Health, 19(1). https://doi.org/10.1186/s12889-
019-7762-5
Mehandru, N., Miao, B. Y., Almaraz, E. R., Sushil, M.,
Butte, A. J., & Alaa, A. (2024). Evaluating large
language models as agents in the clinic. In npj Digital
Medicine (Vol. 7, Issue 1). Nature Research.
https://doi.org/10.1038/s41746-024-01083-y
Minaee, S., Mikolov, T., Nikzad, N., Chenaghlu, M.,
Socher, R., Amatriain, X., & Gao, J. (2024). Large
Language Models: A Survey. http://arxiv.org/
abs/2402.06196
Nassiri, K., & Akhloufi, M. A. (2024). Recent Advances in
Large Language Models for Healthcare.
BioMedInformatics, 4(2), 1097–1143. https://doi.org/
10.3390/biomedinformatics4020062
Naveed, H., Khan, A. U., Qiu, S., Saqib, M., Anwar, S.,
Usman, M., Akhtar, N., Barnes, N., & Mian, A. (2023).
A Comprehensive Overview of Large Language
Models. http://arxiv.org/abs/2307.06435
Park, J. S., O’Brien, J., Cai, C. J., Morris, M. R., Liang, P.,
& Bernstein, M. S. (2023, October 29). Generative
Agents: Interactive Simulacra of Human Behavior.
UIST 2023 - Proceedings of the 36th Annual ACM
Symposium on User Interface Software and
Technology. https://doi.org/10.1145/3586183.3606763
Piñeiro-Martín, A., García-Mateo, C., Docío-Fernández,
L., & López-Pérez, M. del C. (2023). Ethical
Challenges in the Development of Virtual Assistants
Powered by Large Language Models †. Electronics
(Switzerland), 12(14). https://doi.org/10.3390/
electronics12143170
Raffel, C., Shazeer, N., Roberts, A., Lee, K., Narang, S.,
Matena, M., Zhou, Y., Li, W., & Liu, P. J. (2019).
Exploring the Limits of Transfer Learning with a
Unified Text-to-Text Transformer
. http://arxiv.org/
abs/1910.10683
Smith, G. R., Bello, C., Bialic-Murphy, L., Clark, E.,
Delavaux, C. S., Lauriere, C. F. de, Hoogen, J. van den,
Lauber, T., Ma, H., Maynard, D. S., Mirman, M.,
Lidong, M., Rebindaine, D., Reek, J. E., Werden, L. K.,
Wu, Z., Yang, G., Zhao, Q., Zohner, C. M., &
Crowther, T. W. (2024). Ten simple rules for using
large language models in science, version 1.0. PLoS
Computational Biology, 20(1). https://doi.org/10.
1371/journal.pcbi.1011767
Sun, X., & Li, X. (2023). Editorial: Aging and chronic
disease: public health challenge and education reform.
Front Public Health, 16(2), 107–118.
https://doi.org/10.3389/fpubh.2023.1175898
HEALTHINF 2025 - 18th International Conference on Health Informatics
370

Thapa, S., & Adhikari, S. (2023). ChatGPT, Bard, and
Large Language Models for Biomedical Research:
Opportunities and Pitfalls. In Annals of Biomedical
Engineering (Vol. 51, Issue 12, pp. 2647–2651).
Springer. https://doi.org/10.1007/s10439-023-03284-0
World Health Organization. (2015). World report on
ageing and health.
World Health Organization. (2022). Ageing and health.
Yang, H., Yue, S., & He, Y. (2023). Auto-GPT for Online
Decision Making: Benchmarks and Additional
Opinions. http://arxiv.org/abs/2306.02224.
Innovation in Geriatric Care: An AI Assistant with LLM Integration Based on Health Guidelines
371
