
Raising the Confidence of Mothers in Preterm Birth Care:
Exploring the Secondary Role of the Internet
Jamale S. El-Eid
1a
, Nabil Georges Badr
1b
, Salim M. Adib
1c
and Bernard Gerbaka
2d
1
Higher Institute of Public Health - Faculty of Medicine, Saint Joseph University of Beirut, Beirut, Lebanon
2
Department of Epidemiology and Population Studies, American University of Beirut, Lebanon
Keywords: Preterm Birth, NICU Training, Knowledge Acquisition, Role of Internet.
Abstract: Adequate family education and knowledge regarding basic preterm baby care is essential to enhance parents’
experience and alleviate the quality of life with preterm babies. Our study looks at the extent to which
knowledge affects the confidence of new mothers. It explores other potential factors, sources of knowledge,
and the role of technology and online content. The research model for our empirical investigation takes the
foundations of the knowledge, attitudes, and practices (KAP) theory as the central survey framework of the
theory of planned behaviour. The study results showed that NICU training has a significant impact on mothers'
knowledge levels regarding the care of preterm babies after their discharge from the NICU. Findings revealed
a prevalent reliance on unofficial online sources such as Google, social media, and other informal websites,
rather than official resources like the WHO, CDC, or similar trusted platforms. Knowledge level emerged as
a significant predictor of the dependent variable, maternal confidence, with a predictability score of 43.6%.
This suggests that improved knowledge fosters greater confidence, particularly among first-time mothers who
often rely on secondary internet sources to bridge their knowledge gaps and boost their confidence. These
findings highlight opportunities for healthcare providers and health authorities to improve information
generation and dissemination and foster support systems for parents.
1 INTRODUCTION
Every year more than 15 million tiny creatures are
born prematurely or earlier than their expected
arrival. Pre-term birth or Premature birth (PB) refers
to births that occur earlier than 37 weeks or equivalent
to 259 days of gestation. It accounts for more than one
million neonatal deaths per year at the global level
1
And presents a major challenge to perinatal health as
it significantly contributes to various morbidities that
may extend to adulthood (Pinto F.a, 2019). PB may
drastically affect the little bundles of joy, their
mothers, and family members caring for them
(O'Donovan & Nixon, 2019).
Adequate family education and knowledge
regarding the basic preterm baby care is essential to
enhance parents’ experience and alleviate the quality
of life with the preemie (Sedigheh Khanjari, 2022).
This is when parents become the primary caregivers
a
https://orcid.org/0000-0003-2698-5269
b
https://orcid.org/0000-0001-7110-3718
c
https://orcid.org/0000-0001-8831-2954
who provide the basic and sometimes more
complicated care that may require a certain level of
training and monitoring (José Granero-Molina,
2019). Understanding parents’ challenges and the
support they need would help achieve optimal
outcomes for babies (Ma RH, 2021; Amorim, 2018).
In 2012, the prevalence of preterm births in
Lebanon was around 9.6% as per the National
Collaborative Perinatal Neonatal Network (NCPNN)
which analysed 35% of the national birth data. This
accounts for around 8656 neonates per year of the
total 90,167 births reported by the Ministry of Public
Health.
We are interested to learn about the extent to
which knowledge affects the confidence of the new
mothers attitude and explore the relevant indicators
for that. We aim to explore the sources of knowledge
parents seek for care of their preterm babies in a
context of a Low-or Middle-Income Country (LMIC)
d
https://orcid.org/0009-0002-5755-6862
1
https://www.who.int/news-room/fact-sheets/detail/
preterm-birth
372
Badr, N. G., El-Eid, J. S., Adib, S. M., Gerbaka and B.
Raising the Confidence of Mothers in Preterm Birth Care: Exploring the Secondary Role of the Internet.
DOI: 10.5220/0013099300003911
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 372-381
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
like Lebanon, where resources are scarce and
research is limited. Furthermore, as Information and
Communication Technology (ICT) modalities, also
known as digital tools, are becoming more popular,
employing them to educate and support parents of
preterm babies would be a way forward to address
those needs. Preterm birth disproportionately affects
minority and low-income groups and is associated
with high infant morbidity and mortality rates. In the
neonatal intensive care unit and elsewhere in the
postpartum period, healthcare teams can use digital
solutions to fulfil the needs of mothers and infants
(Jani, et al, 2021). Solutions like e-health,
telemedicine, and digital education can also be
substantial to secure support to health centres and
patients in rural areas and maybe less developed
countries who have little access to advanced facilities
(Ruxwana NL, 2010). Our research question explores
the extent that new mothers rely on the use of
information and communication technology ICT,
digital resources, and how they are combined with
direct training of parents caring for their preterm
babies after they are discharged from the NICU.
2 BACKGROUND
We are interested to explore the extent to which
knowledge affects attitude and explore the relevant
indicators for that. We set the stage for our empirical
investigation through a research model that takes the
foundations of the theory of knowledge, attitudes, and
practices (KAP) theory as the central survey
framework of the theory of planned behaviour
(Ajzen, I. 2011), Fig 1.
Figure 1: KAP Conceptual Model from Ajzen, I. (2011).
The theory postulates that knowledge acquisition
modifies human health-related behaviors in preterm
postnatal care (Herzog-Petropaki et al, 2022; Parker
et al, 2020; McMillan et al, 2009). We follow the
example of other research in this context to
understand mother’s confidence and competency in
preterm infant care (Kusumaningrum et al, 2019;
Bajoulvand et al, 2019; Hwang et al, 2023). Our
choice of KAP theory and model offers a deeper dive
into antecedents of knowledge and attitudes and
investigate knowledge levels acquired from online
information sources, NICU training and other factors
would influence the confidence of preterm infants’
mothers, especially testing for the impact of the ICT
use and online information sources that these new
mothers find relevant.
3 RESEARCH MODEL
3.1 Antecedents and Hypotheses
3.1.1 Confidence/ Attitude
The confidence of new mothers in caring for their
preterm baby has a significant impact on their ability
to handle their preemie at home. Maternal confidence
alleviates self-empowerment and capability in
handling the caretaking tasks with less stress and
anxiety (Premji, 2018). Mothers’ attitude and
confidence in taking control over caring for their
preterm baby at home is highly affected by the level
of knowledge and education they have (Parhiz Z,
2016). As such, mothers of preterm infants rather feel
unprepared to assume the full responsibility for their
babies after their discharge from the NICU because
they lack the proper education and confidence
(Kadiroğlu, 2021). Hence, inadequate knowledge of
mothers about caring for their preterm babies would
in turn associate with post-discharge complications
and sometimes readmission (Aldirawi, 2019). Our
inquiry into the confidence level of the new mothers
is modelled after Rinehimer, M. A. (2017), we
attempt to detect the new mother’s comfort
interacting with their infant at home, their reliance on
the information received and their understanding of
the baby’s developmental milestones.
We build a model (Fig. 2) where Confidence is the
dependent variable (CONF 4.1 – 4.10).
Figure 2: Our Model.
We consider the following variables as latent
independent variables:
(KNOW_LVL) - Scored knowledge level as
reported by the survey instrument (See Appendix)
(NICU_T1 – T10) - Represents the training
provided by NICU staff to preterm mothers
(INFO_SOURCE) – designates the source of
information on caring for preterm infant and whether
Raising the Confidence of Mothers in Preterm Birth Care: Exploring the Secondary Role of the Internet
373

it is official online sources/websites like the World
Health Organization, Center for Disease Control, and
other scientific societies (ONLINE_1); or unofficial
online sources like Google and other websites and
mobile applications (ONLINE_2) and finally (F&F) -
Family and friends.
(ICT_USE) is the variable that represents the use
of electronic platforms or mobile applications by new
mothers to get care information. Finally,
(EXT_FACTORS), include factors such as Maternal
age (AGE); Education level (EDU); length of the
infant stays in the NICU (NICU_DAYS) and whether
this was the mother’s first pregnancy (1ST_PREG).
3.1.2 NICU Training
Patient and family education is a core practice in
health care to improve health outcomes and foster
self-efficacy and confidence. When empowered with
knowledge about their health situation, treatment and
preventive alternatives, patients and their families
become more engaged in their care plan, which
positively affects their adherence (Paterick TE,
2017). Structured family-centred education of the
mothers and fathers not only improves the health
outcomes of the baby but also enhances the quality of
life of parents (Sedigheh Khanjari, 2022). Patient and
Family Education in general, and care for babies on
specific is highly recognized as a basic requirement
in Lebanon's Hospital national accreditation
standards under the Patient and Family Rights
domain. Hospitals are required to establish policies,
procedures, and mechanisms to realize this
requirement and put in place measures to assess its
effectiveness. Discharge education for NICU
graduates constitutes fundamental care aspects like
basic care, feeding, follow-up care among others
(Sedigheh Khanjari E. F., 2022). Our first (H1)
hypothesis states that NICU training, as a
fundamental knowledge base, is an important
antecedent to increasing the knowledge level of new
mothers in the care of their preterm infant.
3.1.3 Sources of Information
Upon the transition of the preterm baby home after
spending days or weeks in the NICU, parents
experience a significant level of anxiety and stress to
face the responsibility of being the primary caregivers
to the baby (Abiuty Omwenga Omweri, 2024). After
being passive recipients of information while at the
NICU, they become active seekers of various types of
information as they move home. Parents explore a
wide range of information from various sources
including computer-based or digital resources to fulfil
their needs in caring for the preterm baby at home
(Brazy, 2001). For instance, social media platforms,
like Google Search (Dol et al, 2019) and Facebook,
are reported as frequently utilized resources to look
out medical information and seek advice (Taylor K,
2023; Erika Frey, 2022). We are also interested in
exploring the interest in information available from
official health authority websites like the World
Health Organization (WHO), Centre for Disease
Control (CDC), National Health Authorities, Medical
Societies, which might be seen as a triangulated
source that might have a certain degree of reliability
and usefulness.
For our model, we therefore hypothesize (H2),
that, information sources on caring for preterm
infants are antecedents to increasing the knowledge
level of new mothers in the care of their preterm
infant. These sources could be either official online
sources/websites like the World Health Organization,
Center for Disease Control, and other scientific
societies, or unofficial online sources like Google and
other websites and mobile applications. They also
could be information offered by friends and family
members.
3.1.4 Knowledge Acquisition
For the third hypothesis, H3, we postulate the
knowledge level of new mothers is an important
antecedent to their confidence level in caring for their
preterm infants.
Parents of preterm babies need a wide range of
support services, among which education and
information prevail. The results of a systematic
review published in 2011 by Brett et al reflected that
parents of preterm babies need accessible,
individualized, and up-to-date education programs to
help them cater to their baby’s needs and support their
development (Brett J, 2011). Traditional education
and training programs that include physical presence
and face-to-face meetings may help parents to some
extent however, they also incur several logistical
challenges that affect the level of attendance and
response (Valérie Lebel, 2021). In addition,
educational resources that include verbal education
and/or printed pamphlets may not account for the
factors of interaction, individualization, and parents’
stress and well-being (Valérie Lebel, 2021).
For our inquiry, we conducted a desktop review
of available guidelines and resources for the basic
care information that parents should know about
caring for their preterm baby after discharge from the
NICU. We compiled references of publications by
(Furtak, 2021; WHO, 2022), and triangulated our
HEALTHINF 2025 - 18th International Conference on Health Informatics
374

information by articles of the American Academy of
Paediatrics parenting website
2
, Canadian Paediatric
Society, Foetus and Newborn Committee, Alberta
Health Services
3
, and the Center for Disease
Prevention and Control
4
. We use these references to
build a questionnaire that would explicitly assess the
level of knowledge parents acquire on basic preterm
baby care. We run our questionnaire by 30 preterm
babies’ parents and neonatal care practitioners to
obtain a relative validation or the relevance of the
questions (Appendix).
3.1.5 Use of Technology Tools
Digital tools may offer comfort, adaptability and
autonomy in providing care and the effectiveness of
care. The literature advocates including parents or
primary caregivers of infants requiring care in a
neonatal intensive care unit, when assessing the
relevance of exploiting technology in the circle of
care (Dol et al, 2017; Gibson, 2020). These
technologies include means of education (e.g. web-
based platforms, mobile applications);
communication (e.g. videos, SMS or text messaging),
or a combination of both.
The design and implementation of perinatal
eHealth programs are emerging as the availability of
new eHealth systems (i.e. applications and machine
learning-based tailored feedback), and ubiquitous
devices (i.e. smartphones and wearables) increases
(Auxier et al, 2023). Parents are open to using
technology as part of their neonatal intensive care;
videoconferencing for instance, is sought after
discharge as a means of providing post-departure
family assistance. We then propose the hypothesis
(H4), that the use of electronic platforms or mobile
applications by the new mothers to get care
information is an important antecedent to their
confidence level in caring for their preterm infants.
3.1.6 External Factors
Our last latent variable summarizes potential external
factors of determinants of health, namely age and
education that may have an influence on the
confidence of mothers to care for caring for a preterm
baby after discharge from the hospital (Taraban and
Shaw, 2018). The length of the NICU stay would
affect the parents' confidence given the exposure that
the parents get while shadowing the health care
practitioners in the NICU and whether the preterm
baby is their first-born (Pinar & Erbaba, 2020). That
2
HealthyChildren.org, 2023
3
www.albertahealthservices.ca/scns/page10303.aspx
said, our last hypothesis (H5) is that external factors
such as maternal age, education, length of the infant
stay in the NICU and whether this was the mother’s
first pregnancy are important antecedents to their
confidence level in caring for their preterm infants.
3.2 Approach and Study Design
We follow a convenience sampling using data on 26
public and private hospitals that offered NICU
services in two of the largest districts in Lebanon,
Mount Lebanon (suburb to the capital) and Beirut.
The target population included Lebanese parents with
preterm babies born earlier 37 weeks of gestation.
After securing the required ethical approvals, we
conducted the study between December 2023 and
September 2024. We approached all mothers who fit
the inclusion criteria in coordination with the NICU
health doctors or nurses within the discharge week.
We enrolled preterm mothers immediately after
delivery and contacted again 6-8 weeks after
discharge to partake the survey.
Our survey instrument comprises seven sections
(Appendix). In the first section, we collect 37 answers
to questions and summarize the score into three
knowledge levels as preliminary level (scores of
<50%), average (Scores 50% - 75%) and advanced
(scoring 75% - 100%). Upon data collection we
normalize our answers to produce our KNOW_LVL
variable values of (0, 1, and 2) respectively (Peterson
and & Cavanaugh, 2020). Section 2 explores the pre-
discharge training that parents were offered in the
Neonatal Intensive Care Unit (NICU). Section 3 asks
the participants to identify the sources they found
helpful to preterm baby care. Next, section 4
investigates new mothers’ attitudes and confidence
level regarding caring for preterm baby. Participants
were able to report whether they use electronic
platforms or mobile applications to get information
about caring for their baby in section 5. Finally,
sections six and seven attempt to capture external
factors such as maternal age, education, whether it
was a case of first pregnancy and the length of stay of
preterm baby in the NICU.
4 STATISTICAL ANALYSIS
The participants were mothers fitting the below
profile (Table 1). In an interestingly symmetrical
normal distribution, our sample show that mothers
4
www.cdc.gov/maternal-infant-health/about/index.html
Raising the Confidence of Mothers in Preterm Birth Care: Exploring the Secondary Role of the Internet
375
(N=78) with an average age of 32, 68% on their first
pregnancy, gave birth to their preterm baby within the
first 2 weeks of gestation.
Table 1: Sample Profile.
N=78 Avera
g
e Median Mode
Maternal a
g
e in
y
ears 32 32 32
Gestational age
(completed weeks) 31 32 33
First Pre
g
nanc
y
68%
4.1 Measurement Model Analysis
We loaded our model in SmartPLS3.0 and ran the
PLS algorithm. We then reduced the indicator
variables in order to reach convergent validity and
reliability. We accepted only the indicators with
loadings ≥ 0.708 as significant (Hair et al, 2019).
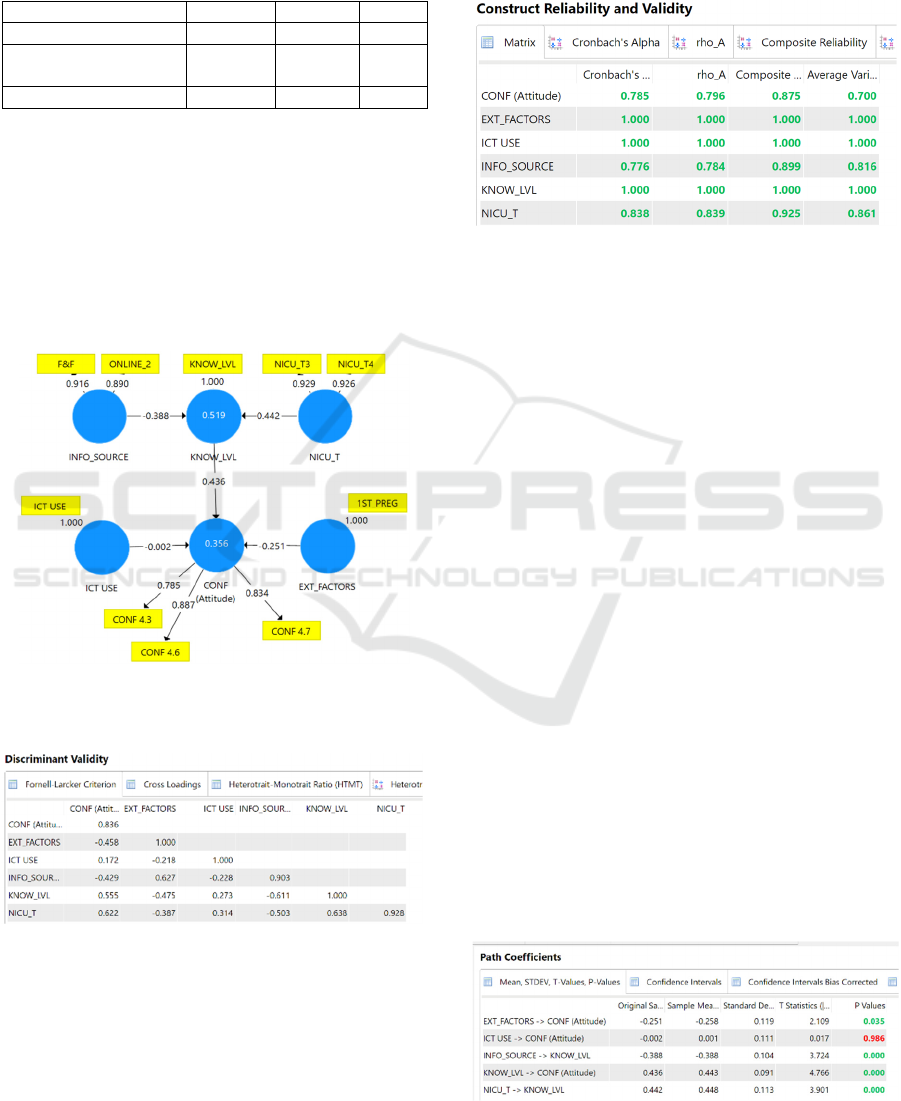
Figure 3 shows our valid model - with outer loading
factors.
Figure 3: Valid Model - with outer loading factors.
Table 2: Discriminant Validity.
The model is of a reflective construct; therefore,
construct validation can be obtained through
Confirmatory Factor Analysis (CFA) (i.e. convergent
and discriminant validity) and reliability testing (i.e.
Cronbach's Alpha) (Hair et al, 2019). We find that the
model has good discriminant validity since the AVE
squared value of each exogenous construct (the value
on the diagonal) exceeds the correlation between this
construct and other constructs - see Fornell-Larcker
Criterion Values in Table 2 (values below the
diagonal).
Table 3: Construct Reliability and Validity.
Subsequently, following Hair et al (2019), we
perform a convergent validity test by looking at the
loading factor value of each indicator against the
construct. We accept the indicators with loadings of
≥ 0.708 as significant with an AVE value for each
construct > 0.5. Subsequently, we assess the construct
reliability. The reliability test results in table 3 show
that all constructs have composite reliability and
Cronbach's alpha values greater than 0.7 (Hair et al,
2019). In conclusion, all constructs have met the
required validity and reliability.
Further, our model produced R2 values of .519
and .356 for Knowledge level and Confidence. These
moderate to substantial values reinforce the value of
our study and the findings (Hair et al, 2019). They
indicate that 51.9% of the variability in the outcome
in Knowledge Level and 35.6 % of the variability in
the confidence latent variable may be explained by
this study.
4.2 Supported Hypotheses
We found that two significant indicators inform the
NICU Training latent variable in our model. These
indicators relate to training on how to interact with
the preterm baby (NICU_T4) and how to position the
preterm baby in bed (NICU_T3). NICU training as a
fundamental knowledge base is an important
Table 4: Bootstrapping results.
HEALTHINF 2025 - 18th International Conference on Health Informatics
376

antecedent to increasing the knowledge level of new
mothers in the care of their preterm infant (H1).
Table 4 provides evidence of the statistical
findings to support hypothesis H1, H2, H3 and H5.
Information sources on caring for preterm infants
are antecedents to increasing the knowledge level of
new mothers in the care of their preterm infant (H2).
Mothers of preterm babies found information on
caring for their preterm baby from unofficial online
sources like Google and other websites and mobile
applications. Some have received information from
family and friends. What is interesting is that
information sources from official bodies such as
WHO or CDC did not seem as relevant.
The knowledge level of mothers with preterm
infants emerged as a significant predictor of maternal
confidence, with a predictability score of 43.6%.
Improved knowledge fosters greater confidence,
particularly among first-time mothers who often rely
on secondary internet sources to bridge their
knowledge gaps and boost their confidence.
To that effect, the knowledge level of new
mothers is an important antecedent to their
confidence level in caring for their preterm infants
(H3). They believe that the information and
instructions they received from the NICU are
sufficient to meet their needs to care for their preterm
baby (CONF 4.3), the general knowledge they
acquired through the varied sources have increased
their understanding of their baby’s developmental
milestones (CONF 4.6). They are confident that they
know how to care for their newborn and the details of
follow-up assessments needed following discharge.
Our model analysis supports this hypothesis with a
predictability of 43.6 % (path coefficient = 0.436) and
high level of confidence (t= 4.766).
The maternal age, education, length of the infant
stay in the NICU, are not significant indicators.
However, the fact whether this was the mother’s first
pregnancy was important antecedent to their
confidence level in caring for their preterm infants
with a predictability of 25.1 % (path coefficient = -
0.255) and high level of confidence (t= 2.109).
Finally, there was no support for the hypothesis
that the use of electronic platforms or mobile
applications by the new mothers to get care
information is an important antecedent to their
confidence level in caring for their preterm infants.
5 RESULTS AND CONCLUSION
In summary, our effort identified support for four
hypotheses (H1, H2, H3 and H5) while H4, that states
the use of electronic platforms or mobile applications
by the new mothers to get care information is an
important antecedent to their confidence level in
caring for their preterm infants, was not supported.
We find our results surprising. Information sources
from official bodies, such as WHO or CDC were not
found as relevant. Additionally, using formal
electronic platforms was not an important factor
affecting new mothers’ confidence in caring for their
preterm infants. While, an essential source of
knowledge is still the support of friends and family,
mothers of preterm babies found information on
caring for their preterm baby from unofficial online
sources like Google and other websites and mobile
applications. Nevertheless, the study demonstrates
that NICU training has a significant impact on
mothers' knowledge levels regarding the care of
preterm babies after their discharge from the NICU.
This aligns with the knowledge, attitudes, and
practice (KAP) framework, where knowledge serves
as a critical foundation for shaping positive attitudes
and informed practices.
5.1 Emerging Crowdsourcing Platform
The internet promises to be an effective
crowdsourcing platform among preterm baby
mothers. By exploring the dynamics of how mothers
seek and utilize knowledge for the care of their
preterm baby(ies), the study provides valuable
insights into the complexities of knowledge
acquisition in terms of how mothers of preterm
infants acquire and use knowledge, particularly
highlighting the unexpected prominence of unofficial
online sources like google and social media. Mothers'
attitudes toward credible sources and the accessibility
or perceived relevance of the preference to seek non-
official information underscore the mothers'
information-navigation habits and the importance of
fostering effective management of crowdsourced
online information. Our findings highlight
opportunities for healthcare providers and health
authorities to improve information generation and
dissemination and eventually fostering support
systems for parents. One could propose forums and
open-source blogs that collect, disseminate, and
connect information from preterm baby mothers, and
help shape better support systems. Such a
sociotechnical approach could integrate unofficial
experiences, sourced from preterm mothers for the
support of their peers focused on the specific needs of
these parents.
What was not surprising, was the finding that
women on their first pregnancy have found a source
Raising the Confidence of Mothers in Preterm Birth Care: Exploring the Secondary Role of the Internet
377

of confidence boost in searching secondary sources
on the Internet. The internet is rich with informal sites
on neonatal care (Alderdice, et al, 2018). Albeit, the
quality of information in these sources may not be
verified, they seem to offer a confidence level boost
to mothers. For the setting of our study, we issue a
genuine invitation to the Lebanese National Health
Authority in collaboration with the health care
organizations to enhance their online presence and
support parents with the consistent information and
advice in terms of handling preterm babies after
discharge from the NICU.
5.2 Limitations and Further Research
The sample size used is narrow. Nonetheless, it is
effective in supporting our study. A retrospective
sample size verification using the minimum R
squared method showed that our sample size was
satisfactory (Kock, and Hadaya, 2018).
Still, the use of convenient sampling, in terms of
choosing two of the most populous districts among
the other districts of Lebanon to conduct the study,
may bring forth a form of bias. The study was
conducted in Beirut and Mount Lebanon only which
may not represent all regions of Lebanon, especially
the rural ones. However, Mount Lebanon, which is
the largest district, includes some rural areas,
especially in the mountain villages that are relatively
far from the capital cities. Nevertheless, our sampling
was inclusive to all hospitals who offer NICU
services in these two districts and were invited to take
part in the study and while exhaustive sampling was
used to reach out to every potential candidate who is
eligible to participate.
As such, our study captures insights from parents
of preterm babies residing in these rural areas.
Simultaneously, parents seeking neonatal services at
the referral hospitals in Beirut and Mount Lebanon
come from diverse regions in Lebanon including
areas outside these two big districts.
Acknowledging that the empirical part of this
effort was still in progress at the time of writing this
paper, we were motivated by interesting findings
from the questionnaire section of this study that
mothers' reliance on informal online sources to seek
information regarding their preterm babies, we
decided to disclose these findings early as they could
provide valuable insights and prompt timely
discussions on this critical aspect of information-
navigation or seeking behaviors.
We are proceeding with an extension of the
sample to other geographies of the country, while
adding a qualitative extension for the inquiry, to
deepen the understanding of the matter. Once
complete, we will share the expanded findings, as we
are positive, will shed more light on the complex
subject of preterm birth care.
REFERENCES
Abiuty Omwenga Omweri, M. L. (2024, January).
Caregivers’ Experiences in Providing Home Care for
Preterm Infants during the Initial Six Months Post-
Discharge from the Neonatal Care Unit. JCMA.
Ajzen, I. (2011). The theory of planned behaviour:
Reactions and reflections. Psychology & Health, 26(9),
1113–1127.
Alderdice, F., Gargan, P., McCall, E., & Franck, L. (2018).
Online information for parents caring for their
premature baby at home: a focus group study and
systematic web search. Health Expectations, 21(4),
741-751.
Aldirawi, A.,. -K. (2019). Mothers’ Knowledge of Health
Caring for Premature Infants after Discharge from
Neonatal Intensive Care Units in the Gaza Strip,
Palestine. Open Journal of Pediatrics, 9, 9(3), 239-252.
Amorim, M. S.-I. (2018). Quality of life among parents of
preterm infants: a scoping review. Qual Life Res, 1119–
1131.
Auxier, J., Savolainen, K. T., Bender, M., Rahmani, A. M.,
Sarhaddi, F., Azimi, I., & Axelin, A. M. (2023).
Exploring access as a process of adaptation in a self-
monitoring perinatal ehealth system: Mixed methods
study from a sociomaterial perspective. JMIR
Formative Research, 7, e44385.
Bajoulvand, R., González-Jiménez, E., Imani-Nasab, M.
H., & Ebrahimzadeh, F. (2019). Predicting exclusive
breastfeeding among Iranian mothers: application of
the theory of planned behavior using structural equation
modeling. IJNMR, 24(5), 323-329.
Brazy, J.,. (2001). How Parents of Premature Infants Gather
Information and Obtain Support. Neonatal Network,
20(2).
Brett J, S. S. (2011). A systematic mapping review of
effective interventions for communicating with,
supporting and providing information to parents of
preterm infants. BMJ Open.
Callander, E. A. (2021, July). The healthcare needs of
preterm and extremely premature babies in Australia—
assessing the long-term health service use and costs
with a data linkage cohort study. Eur J Pediatr, 2229–
223.
Dol J, R. B.-Y. (2019). Learning to parent from Google?
Evaluation of available online health evidence for
parents of preterm infants requiring neonatal intensive
care. Health Informatics Journal, 25(4), 1265-1277.
Erika Frey, C. B. (2022). Parents’ Use of Social Media as a
Health Information Source for Their Children: A
Scoping Review. Academic Pediatrics, 22(4), 526-539.
Furtak, S. L., Gay, C. L., Kriz, R. M., Bisgaard, R., Bolick,
S. C., Lothe, B., ... & Franck, L. S. (2021). What parents
HEALTHINF 2025 - 18th International Conference on Health Informatics
378

want to know about caring for their preterm infant: a
longitudinal descriptive study. Patient education and
counseling, 104(11), 2732-2739.
Gibson, C., Ross, K., Williams, M., & de Vries, N. (2021).
The experiences of mothers in a neonatal unit and their
use of the babble app. Sage Open, 11(2),
21582440211023170.
Guo, J. L., Wang, T. F., Liao, J. Y., & Huang, C. M. (2016).
Efficacy of the theory of planned behavior in predicting
breastfeeding: Meta-analysis and structural equation
modeling. Applied Nursing Research, 29, 37-42.
Hair, J. F., Risher, J. J., Sarstedt, M., & Ringle, C. M.
(2019). When to use and how to report the results of
PLS-SEM. European business review, 31(1), 2-24.
Herzog-Petropaki, N., Derksen, C., & Lippke, S. (2022).
Health behaviors and behavior change during
pregnancy: Theory-based investigation of predictors
and interrelations. Sexes, 3(3), 351-366.
Hwang, S. S., Parker, M. G., Colvin, B. N., Forbes, E. S.,
Brown, K., & Colson, E. R. (2021). Understanding the
barriers and facilitators to safe infant sleep for mothers
of preterm infants. J Perinatol., 41(8), 1992-1999.
Jani SG, Nguyen AD, Abraham Z, Scala M, Blumenfeld
YJ, Morton J, Nguyen M, Ma J, Hsing JC, Moiwa-
Grant M, Profit J, Wang CJ. PretermConnect:
Leveraging mobile technology to mitigate social
disadvantage in the NICU and beyond. Semin Perinatol.
2021 Jun; 45(4):151413.
José Granero-Molina, I. M.-S.-P. (2019). Experiences of
Mothers of Extremely Preterm Infants after Hospital
Discharge. Journal of Pediatric Nursing.
Kadiroğlu, T. G. (2021). Effect of Infant Care Training on
Maternal Bonding, Motherhood Self-Efficacy, and
Self-Confidence in Mothers of Preterm Newborns.
Matern Child Health J, 40(4), E18–E37.
Kock, N. & Hadaya, P. (2018). Minimum samples size
estimation in PLS-SEM: The inverse square root and
gamma exponential methods. Inf. Syst. J, 28(1), 227-261.
Kusumaningrum, T., Kurnia, I. D., & Doka, Y. P. (2019,
March). Factors Related to Mother’s Competency In
Caring For Low Birth Weight Baby Based on Theory
of Planned Behavior. In IOP Conference Series: Earth
and Environmental Science (Vol. 246, No. 1, p.
012029). IOP Publishing.
Ma RH, Z. Q. (2021, Nov). Transitional care experiences of
caregivers of preterm infants hospitalized in a neonatal
intensive care unit: A qualitative descriptive study.
Nurs Open, 8(6), 3484-3494.
McMillan, B., Conner, M., Green, J., Dyson, L., Renfrew,
M., & Woolridge, M. (2009). Using an extended theory
of planned behaviour to inform interventions aimed at
increasing breastfeeding uptake in primiparas
experiencing material deprivation. British Journal of
Health Psychology, 14(2), 379-403.
Parhiz, Z., Birjandi, M. H., Khazaie, T., & Sharifzadeh, G.
(2016). The effects of an empowerment program on the
knowledge, self-efficacy, self-esteem, and attitudes of
mothers of preterm neonates. Modern Care Journal,
13(3).
Parker, M. G., Hwang, S. S., Forbes, E. S., Colvin, B. N.,
Brown, K. R., & Colson, E. R. (2020). Use of the theory
of planned behavior framework to understand
breastfeeding decision-making among mothers of
preterm infants. Breastfeeding Medicine, 15(10), 608-
615.
Paterick TE, P. N. (2017). Improving health outcomes
through patient education and partnerships with patient.
Proc (Bayl Univ Med Cent, 30, pp. 112-113.
Peterson, R. A., & Cavanaugh, J. E. (2020). Ordered quantile
normalization: a semiparametric transformation built for
the cross-validation era. Journal of applied statistics.
Pinar & Erbaba, (2020). Experiences of new mothers with
premature babies in neonatal care units: A qualitative
study. J Nurs Pract, 3(1), 179-185.).
Pinto F.a, c. ·. (2019). Born Preterm: A Public Health Issue.
Portuguese Journal of Public Health.
Premji, S. S. (2018). Mother’s level of confidence in caring
for her late preterm infant: A mixed methods study.
Journal of Clinical Nursing, 27, e1120–e1133.
Rinehimer, M. A. (2017). Investigating the Needs of
Parents of Premature Infants’ Interaction in the
Neonatal Intensive Care Unit. Seton Hall University
Hall Dissertations and Thesis.
Ruxwana NL, H. M. (2010). ICT applications as e-health
solutions in rural healthcare in the Eastern Cape Province
of South Africa. Health Inf Manag, 39(1), 17-26.
Sedigheh Khanjari, E. F. (2022). The effect of family-
centered education on the quality of life of the parents
of premature infants. J Neonatal Nurs, 26(6), 407-412.
Taraban, L., & Shaw, D. S. (2018). Parenting in context:
Revisiting Belsky’s classic process of parenting model
in early childhood. Developmental Review, 48, 55-81.
Taylor K, H. J. (2023). Social Media as a Source of Medical
Information for Parents of Premature Infants: A
Content Analysis of Prematurity-Related Facebook
Groups. American Journal of Perinatology, 1629-1637.
Valérie Lebel, M. H. (2021). The development of a digital
educational program with parents of preterm infants
and neonatal nurses to meet parents educational needs.
Journal of Neonatal Nursing, 27(1), 52-57.
WHO (2022), Recommendations for Care of the Preterm or
Low Birth Weight Infant ISBN: 978-92-4-005826-2
Wong, K. K. K. (2013). Partial least squares structural
equation modeling (PLS-SEM) techniques using
SmartPLS. Marketing Bulletin, 24(1), 1-32.
Yang M, C. H.-A. (2023, May). Neonatal health care costs of
very preterm babies in England: a retrospective analysis
of a national birth cohort. BMJ Paediatr Open, 7(1).
APPENDIX
Section 1. Knowledge Level Score (KNOW_LVL):
Possible answers: Agree=1 Disagree=0
2.1- The preterm baby has a corrected age that
accounts for the weeks born earlier than 37 weeks.
Raising the Confidence of Mothers in Preterm Birth Care: Exploring the Secondary Role of the Internet
379

2.2- My preterm baby needs to visit his/her
doctor one to 2 weeks following discharge from the
NICU.
2.3- The mother’s milk is the recommended
feeding for preterm babies.
2.4- In case breast-feeding is not possible, the
preterm baby should be fed only formula milk for the
first 4 to 6 months.
2.5- The preterm baby should be fed at least
every three to four hours day and night.
2.6- Refrigerated milk must be placed on the
counter to warm to room temperature before being
given to the baby.
2.7- If the preterm baby is fed formula milk,
bottled water should be used to prepare the milk.
2.8- Adding more water to the bottle than
required might be dangerous to my preterm baby.
2.9- Extra milk that remains in the bottle can be
used for the next feed.
2.10-Prepared formula milk should be stored in
the refrigerator and used within 24-48 hours.
2.11-Milk bottles need to be cleaned with hot and
soapy water (or on the top rack of the dishwasher).
2.12-I know if my preterm baby is getting enough
breast milk or formula milk through the daily number
of wet.
2.13-Preterm babies do not need to be bathed
every day.
2.14-The preterm baby should be bathed either
before feeding or at least one hour after feeding.
2.15-A baby should always be transported in a
rear-facing infant-only car safety seat.
2.16-My preterm baby should have routine
monthly or bimonthly visits to the doctor up till the
age of 12 months.
2.17-My preterm baby needs to be assessed by a
pediatric neurologist.
2.18-My preterm baby may need neuro-
developmental therapy like physical therapy,
psychomotor therapy, feeding therapy...
2.19-My preterm baby may need eye
screening/exam
2.20-Rectal temperature 38ₒC or above is an
alarming sign of illness that requires doctor
consultation.
2.21-The decreased activity is an alarming sign of
illness that requires doctor’s consultation.
2.22-At 1 to 2 months, taking less than 6 feeds of
milk per day is an alarming sign that requires doctor’s
consultation.
2.23-The absence of wet diapers for more than 6
hours is an alarming sign that requires doctor’s
consultation.
2.24-Diarrhea (more stools than the baby’s usual)
for more than one day is an alarming sign that requires
doctor’s consultation.
2.25-Unusual (more than the usual spitting)
vomiting is an alarming sign that requires doctor’s
consultation.
2.26-Yellowish eyes or skin is an alarming sign
that requires doctor’s consultation.
2.27-Fast or difficult breathing is an alarming sign
that requires doctor’s consultation.
2.28-Common cold can cause severe respiratory
illness in preterm babies.
2.29-Preterm babies are vulnerable and more
prone to infections.
2.30-Preterm babies’ vaccination schedule is
different from that of term babies.
2.31-Crowded places and visits increase preterm
babies’ exposure to infections.
2.32-The number of people who provide
care/interact with my preterm baby at home should be
limited.
2.33- Baby should be placed on the back and not
on the stomach while sleeping to avoid the risk of
sudden infant death syndrome (SIDS)
2.34-I should log my baby’ (temperature, milk
intake, daily wet diaper…) to share with the doctor
during the follow-up visits.
2.35-Mother and father skin-to-skin contact with
the preterm baby is beneficial for the baby’s well-
being and development.
2.36-Play has an important role in the
development of my preterm baby.
2.37-Tummy time is essential for the baby’s
development, provided that it is supervised.
Section 2. NICU training and post-discharge
services (NICU_T1-T10 ): Possible answers: 1: Yes
2: No 3: Not Applicable .
NICU_T1: 1.1-I was given instructions about
caring for my preterm baby at home by the NICU
team before discharge.
NICU_T2: 1.2-The NICU staff taught me how to
hold my preterm baby
NICU_T3: 1.3-The NICU staff taught me how to
position (place) my preterm baby in bed.
NICU_T4: 1.4- The NICU staff prepared me to
interact with my preterm baby
NICU_T5: 1.5- The NICU staff taught me how to
feed my preterm baby
NICU_T6: 1.6- The NICU staff taught me how to
identify early signs of illness in my preterm baby
NICU_T7: 1.7- The NICU staff taught me how to
identify signs of discomfort (like colic pain, hunger,
diaper rash) in my preterm baby
HEALTHINF 2025 - 18th International Conference on Health Informatics
380

NICU_T8: 1.8-The NICU team guided me to who
to call if I have questions after discharge
Section3. Source of Knowledge: Possible
answers: Never, 2: Rarely, 3: Sometimes, 4: Often, 5:
Always.
NICU_T9 3.1- I seek information on caring for
my preterm baby from the NICU nurses
NICU_T10 3.2- I seek information on caring
for my preterm baby from my baby’s doctor
ONLINE_1 3.3- I seek information on caring
for my preterm baby from official online
sources/websites like the World Health Organization
(WHO), Center for Disease Control (CDC), and other
scientific societies.
ONLINE_2 3.4- I seek information on caring
for my baby from online sources like Google and
other websites and mobile applications …
F&F 3.5- I seek information on caring for my
preterm baby from family and friends.
Section 4. Attitudes (Confidence) Possible
answers: 5 Point Likert Scale
Scale: 1: Strongly Disagree – 2: Disagree- 3:
Neither disagree nor agree - 4: Agree – 5: Strongly
Agree
CONF 4.1: 4.1- Given the information I received
from the NICU, I feel comfortable interacting with
my infant at home
CONF 4.2: 4.2- I understand the information that
healthcare professionals gave me about my baby’s
general health condition.
CONF 4.3: 4.3- I believe that the information and
instructions I received from the NICU are sufficient
for care for my preterm baby.
CONF 4.4 4.4- I believe I need additional
information to feel more comfortable
interacting/caring for my infant at home.
CONF 4.5 4.5- I am afraid to touch my baby
because I may hurt or upset the baby.
CONF 4.6 4.6- I am confident in my
understanding of my baby’s developmental
milestones.
CONF 4.7 4.7- I am confident that I know
the screening and follow-up assessments needed
following discharge.
CONF 4.8 4.8- I am confident that I know
about the early signs of illness when my baby needs
medical follow-up.
CONF 4.9 4.9- I am confident I know what
to do when I detect early signs of illness.
CONF 4.10 4.10- Overall, I am confident
handling and caring for my infant at home
Section 5. Technology Use. Possible answers:
Agree=1 Disagree=0
ICT_USE I use electronic platforms or mobile
applications to get information about caring for my
baby to help me care for my baby.
Section 6. External factors
AGE 6.1- Maternal age in years: ________
EDU 6.2- Highest education/degree: < Pre-
High School; High School+; Higher Education>
NICU_DAYS 6.4- How many days did your
preterm baby spend in the NICU? ------
1ST_PREG 6.5- Is this your first
pregnancy? 1: Yes – 2: No; if no, please go to
question 6.5.
Raising the Confidence of Mothers in Preterm Birth Care: Exploring the Secondary Role of the Internet
381
