
Assessment of Training Progression on a Surgical Simulator Using
Machine Learning and Explainable Artificial Intelligence Techniques
Constantinos Loukas
a
and Konstantina Prevezanou
b
Medical Physics Lab, Medical School, National and Kapodistrian University of Athens,
Mikras Asias 75 str., Athens, Greece
Keywords: Surgery, Virtual Reality, Skills Assessment, Machine Learning, Explainable AI (XAI).
Abstract: Surgical training on VR simulators provides an efficient education paradigm in laparoscopic surgery. Most
methods for skills assessment focus on the analysis of video and kinematic data for self-proclaimed skill
classification and technical score prediction. In this paper we evaluate a machine learning (ML) framework
for classifying the trainee’s performance with respect to the phase of training progression (beginning vs. end
of training and beginning vs. middle vs. end of training). In addition, we leverage techniques from the field
of Explainable Artificial Intelligence (XAI) to obtain interpretations on the employed black-box ML
classifiers. Three surgical training tasks with significant educational value were selected from a training
curriculum followed by 23 medical students. Five machine learning algorithms and two model-agnostic XAI
methods were evaluated using performance metrics generated by the simulator during task performance. For
all surgical tasks, the accuracy was >84% and >86% in the 2- and 3-class classification experiments,
respectively. The XAI methods seem to agree on the relative impact of each performance metric. Features
related to hand-eye coordination and bimanual dexterity (e.g. economy of movements, instrument pathlength
and number of movements), play the most important role in explaining the classification results.
1 INTRODUCTION
Virtual reality (VR) simulators have been
increasingly recognized as valuable tools for training
and assessment of surgical skills. Especially for
laparoscopic surgery, where surgeons are faced with
additional challenges compared to open surgery (such
as reduced depth perception, working with elongated
instruments and minimal force feedback), VR
simulation offers an efficient education paradigm
compared to traditional training on bench top models
and inanimate video trainer boxes (Guedes et al.,
2019). Specifically, VR systems include a plethora of
photorealistic scenarios ranging from basic to
procedural skills (Matzke et al., 2017) and advanced
surgical scenarios (Ikonen et al., 2012). With the aid
of dummy instruments trainees are able not only to
realistically interact with primitive virtual objects
(such as pegboard, suture, needle, etc.), but also to
perform demanding surgical tasks (e.g. bowel
suturing, gallbladder dissection), and entire surgical
a
https://orcid.org/0000-0001-7879-7329
b
https://orcid.org/0000-0002-3091-7413
procedures (e.g. cholecystectomy, appendectomy,
hernia repair surgery, etc.).
In addition to the safe and flexible training
environment, another significant advantage of VR
simulators lies on their ability to capture the hand
kinematics and interaction events with the virtual
world via motion tracking sensors embedded into the
mechanical interface of the dummy surgical tools
(Dosis et al., 2005). Upon task completion the
simulator generates an assessment report that
includes key metrics of task performance with respect
to time (e.g. task and activity completion time),
technical competency (instrument pathlength,
number of movements, etc.), safety (involuntary
errors such as tissue injuries, misplaced clips, suture
damage, etc.), and dexterity (% of adhesions
removed, number of knots locked, alternating throws,
etc.). However, the underlying relation and
educational interpretation of these parameters with
respect to the level of surgical competency that
Loukas, C. and Prevezanou, K.
Assessment of Training Progression on a Surgical Simulator Using Machine Learning and Explainable Artificial Intelligence Techniques.
DOI: 10.5220/0013109500003905
In Proceedings of the 14th International Conference on Pattern Recognition Applications and Methods (ICPRAM 2025), pages 465-474
ISBN: 978-989-758-730-6; ISSN: 2184-4313
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
465

trainees aim to achieve is still under investigation
(Varras et al., 2020).
Objective computer-aided technical skill
evaluation (OCASE-T) has received an increasing
amount of attention over the past few years for several
reasons (Vedula, Ishii and Hager, 2017). In addition
to saving time and money, it allows novice surgeons
to train effectively and with greater flexibility until
they reach an adequate level of competency by
receiving constructive feedback in the absence of
human supervision. Moreover, the assessment output
includes quantitative measures of performance that
allow trainees to evaluate their dexterity level with
respect to that achieved by expert surgeons. Over the
last decade, several studies supported the
effectiveness of VR simulators by demonstrating
their construct validity for laparoscopic skills
assessment (Larsen et al., 2006), comparing the
learning curves after training on a VR curriculum
with traditionally trained groups (Aggarwal et al.,
2007), proposing assessment methodologies based on
quantitative analysis of key laparoscopic skills
(Loukas et al., 2011), and highlighting skill retention
following laparoscopic simulator training (Stefanidis
et al., 2005).
Early approaches to OCASE-T focused on hidden
Markov models (HMMs), which consider the
multidimensional hand motion signal as an
unobserved state sequence relating to a set of
primitive gestures (Rosen et al., 2006). After training
a model for a respective skill-level based on signals
from the same class (e.g. novice, intermediate,
expert), a statistical distance is employed to compare
the likelihood of a new performance to those in the
training set and hence return the corresponding class.
Later works adopted approaches that extract
features, or descriptive metrics, from kinematic
signals in order to determine the skill level. For
example, data from an armband device (e.g.
acceleration, orientation, etc.), was employed in
(Kowalewski et al., 2019) for gesture detection and
skill assessment in laparoscopic suturing. In (Fard et
al., 2018) features such as instrument pathlength and
smoothness are extracted to train various machine
learning (ML) algorithms to classify experts vs.
novices. Other works employ entropy, texture and
frequency features, for self-proclaimed skill
classification and performance score prediction using
ML regression models (Zia et al., 2018). Alternative
sources such as electroencephalogram (EEG) and
electromyogram (EMG) have also been proposed for
laparoscopic expertise evaluation, but the reported
accuracy and applicability in a real-surgical
environment is limited compared to the kinematic
signals (Shafiei et al., 2021), (Fogelson et al., 2004),
(Soto Rodriguez et al., 2023).
Recently, deep learning techniques, for example
1D convolutional neural networks (CNN) and time-
series models (such as long short-term memory
(LSTM) and temporally convolutional networks),
have been employed to capture and process sequential
information from the kinematic signals. In (Wang and
Majewicz Fey, 2018) various CNN models are
proposed to assess surgical performance by extracting
patterns in the surgeon’s maneuvers in robotic
surgery tasks. In (Benmansour, Malti and Jannin,
2023) a CNN+BiLSTM architecture that takes
advantage of both temporal and spatial features of
kinematic data was proposed for performance score
prediction in robotic surgery tasks. Moglia et al.
utilized data from a robotic surgery VR simulator to
develop an ensemble deep neural network (DNN) for
predicting the number of attempts and training time
required to attain proficiency (Moglia et al., 2022).
Most methods for surgical skills assessment focus
on the analysis of kinematic data. However, obtaining
this data requires access to the application
programming interface of the VR device, which is not
always feasible due to permission constraints from
the owner company. Another approach is to employ a
separate tracking system with motion sensors
attached to the surgeon’s hand, or the dummy
laparoscopic tools, which introduces additional
complexity and data management issues in the overall
training process. Moreover, most works provide
limited information about the trainee’s progress while
training on the VR simulator and they focus on
classification in predefined skill classes (e.g. novices,
intermediates, experts). Being able to provide
immediate constructive feedback to the trainees about
their training progress using the performance metrics
generated by the simulator can alleviate many of
these constraints.
In this paper we propose an ML approach for
classifying the trainee’s performance with respect to
the phase of training progression on a laparoscopic
VR simulator (beginning vs. end of training and
beginning vs. middle vs. end of training). In addition,
we leverage techniques from the field of Explainable
Artificial Intelligence (XAI) to obtain not only
interpretations on the employed black-box ML
classifiers, but also better understanding about the
most valuable metrics of surgical performance.
Specifically, we utilize two well-known XAI
techniques: Permutation feature importance (PFI)
(Fisher, Rudin and Dominici, 2019) and a more
advanced one based on SHapley Additive exPlanation
(SHAP) (Lundberg, Allen and Lee, 2017). Both
ICPRAM 2025 - 14th International Conference on Pattern Recognition Applications and Methods
466
methods are applied to derive model-agnostic, post-
hoc interpretations on five ML classifiers: Support
Vector Machine, Linear Discriminant Analysis,
Random Forest, Linear Regression and Gaussian
Naïve Bayes. In addition to providing results on skills
classification in three surgical tasks performed by
trainees following a structured VR simulation
training curriculum, we compare XAI techniques
based on the ranking of feature importances.
Additionally, we utilize visualization tools (summary
plots) to rank the performance metrics and investigate
their effect on model decisions.
2 METHODS
2.1 Dataset
The study included 23 medical students with no
experience in laparoscopy. The participants followed
a structured training curriculum on a laparoscopic VR
simulator (LapMentor
TM
, Surgical Science Sweden
AB). In particular, the participants performed 9
sequential laparoscopic tasks selected from the ‘Basic
Skills’ module of the simulator. The training goal was
to reach for 3 consecutive times the performance of
an expert, defined by quantitative thresholds on
predefined performance metrics, separately for each
surgical task. Upon reaching these thresholds the
student was allowed to advance to the next task. In
this study we focused on three training tasks with
significant educational value according to the
evaluation of our surgical education board (Figure 1):
Clipping and Grasping (Task 5), Two-Handed
Maneuvers (Task 6) and Cutting (Task 7).
Figure 1: Screen shots of the three surgical training tasks
performed on the VR simulator: (a) Clipping and Grasping
(Task 5), Two-Handed Maneuvers (Task 6) and Cutting
(Task 7).
For Task 5 the aim was to grasp and clip leaking
ducts within specific segments. Red segments appear
on the ducts at the beginning of the trial whereas the
segment turns green only when grasped properly.
After grasping the leaking duct, the trainee had to use
the clipper to place a clip within the green segment
only to stop the leakage. The task needs to be
completed before the pool overflows. For Task 6 the
goal was to use 2 grasping tools to locate a jelly mass
and move part of the jelly aside to expose a ball.
While holding the jelly aside, the trainee had to use
the other tool to grasp the exposed ball and place it in
the Endobag near the jelly. The aim of Task 7 was to
apply traction and cut safely and accurately a circular
tissue-like form using a grasper and scissors. The
grasper is used to retract the form and expose a safe
cutting area while the scissors are used for cutting the
form. In terms of educational objectives, the tasks aim
to provide training on key technical skills such as
hand-eye coordination, bimanual dexterity, tissue
handling and laparoscopic orientation.
Table 1: Features employed per surgical task. ‘I’ denotes
instrument and ‘+’ or ‘‒’ denote whether the metric is
available in the corresponding task or not, respectively.
Description Code
name
Task
5
Task
6
Task
7
Trial numbe
r
TN + + +
Average speed of
left I (cm/sec)
Speed-L + + +
Average speed of
right I (cm/sec)
Speed-R + + +
Number of
movements-left I
#Move-
L
+ + +
Number of
movements-right
I
#Move-
R
+ + +
Total pathlength
of left I
(
cm
)
PL-L + + +
Total pathlength
of right I (cm)
PL-R + + +
Trial completion
time
Time + + +
Economy of
movement-left I
(%)
EOM-L + + ‒
Economy of
movement-right I
(
%
)
EOM-R + + ‒
# cli
pp
ed ducts #Cli
p
D+
‒
‒
Total # clipping
attempts
#ClipAtt + ‒ ‒
# exposed green
b
alls collecte
d
#GreenB ‒ + ‒
# lost balls which
miss the basket
#LostB ‒ + ‒
# cutting
maneuvers
#CuttM ‒ ‒ +
# cutting
maneuvers
without tissue
injur
y
#CuttM-
NoInj
‒ ‒ +
# retract.
o
p
erations
#React ‒ ‒ +
Assessment of Training Progression on a Surgical Simulator Using Machine Learning and Explainable Artificial Intelligence Techniques
467

The number of trials required to successfully
complete each task varied from 9-57 (median=23, 23
and 16 for Task 5, 6 and 7, respectively). Table 1
shows the performance metrics (i.e. features) that
were considered for further analysis. Overall, 12
features were utilized. Ten of these were common to
all or two of the tasks (TN, Speed-L, Speed-R,
#Move-L, #Move-R, PL-L, PL-R, Time, EOM-L,
EOM-R), while the other two were task specific
2.2 ML Framework
We employed an ML methodology to classify the
trainees’ trials into different phases of training
progression on the VR simulator. In particular, the
first experiment aimed to classify trials as being close
to the Beginning (BT) or the End (ET) of training on
a particular task. For this purpose, we included three
random trials before and after the median training
attempt (trial) of each subject. The second experiment
aimed to classify the students’ trials into three classes:
Beginning (BT), Middle (MT), and End (ET) of
training. For this purpose, the training trials of each
subject were first divided into three equal parts based
on their order in the training sequence, and then three
random trials from each part were selected. Given that
our study included 23 subjects, the total number of
samples (i.e. trials) for the first and second
experiment were n
1
=138 and n
2
=207, respectively.
Five ML algorithms that were previously applied
to similar classification tasks, such as self-proclaimed
skill classification (Mirchi et al., 2020), (Siyar et al.,
2020), (Winkler-Schwartz et al., 2019), were
employed in this study: Support Vector Machine
(SVM), Linear Discriminant Analysis (LDA),
Random Forest (RF), Linear Regression (LR) and
Gaussian Naïve Bayes (GNB). For SVM we
employed two variants, one with linear kernel (SVM-
Lin) and another one with a radial basis function
(SVM-RBF). For SVM, the regularization parameter
was set to C=1, the penalty term was set to L2 and the
kernel coefficient gamma=1/n
f
, where n
f
is the
number of features. For LR, the regularization
parameter was set to C=1, the penalty term was
squared L2, and the optimization solver was Limited-
memory BFGS. For LDA we employed the Singular
Value Decomposition (SVD) solver with no prior
class probabilities. For RF, the number of trees was
set to 100, the number of min samples required to split
an internal node was 2, the number of minimum
samples required to be at a leaf node was 1, and the
number of features to consider when looking for the
best split was set to
𝑛
. The GNB was based on a
Gaussian kernel without prior class probabilities
2.3 XAI Techniques
Recent advancements in XAI employ model-agnostic
interpretation methods to achieve explanations for
complex ML models. Unlike methods that are model-
specific, model-agnostic interpretations offer more
flexibility by decoupling the model from its
explanations (Ribeiro, Singh and Guestrin, 2016).
Hence, one may apply the same XAI technique to the
predictions of different ML models trained/tested on
the same dataset, allowing for comparison of
interpretation results. Model-agnostic interpretation
methods can be categorized into local and global
methods (Molnar, 2022). Local methods aim to
explain individual predictions whereas global
methods describe how features affect the prediction
on average. In this study we employed two commonly
used global explanation methods that provide
summary plots of feature importance: Permutation
Feature Importance (PFI) and SHapley Additive
exPlanations (SHAP).
PFI is based on the simple idea of measuring the
decrease in the prediction accuracy of the model
when the values of a feature are permuted, thereby
breaking the relationship between the feature and the
true outcome (Fisher, Rudin and Dominici, 2019). In
this work each feature was permuted 15 times and the
feature importance score for each feature was
computed as the average accuracy based on the
predictions of the permuted data in the test-set.
SHAP is based on the game theoretically optimal
Shapley values and aims to explain the prediction of
an instance by computing the contribution of each
feature to the prediction (Lundberg, Allen and Lee,
2017). Features with large absolute Shapley values
are important. Although the technique provides a
Shapley value φ
(i)
for any instance x
(i)
, the global
importance per feature (feature importance score)
can be obtained by averaging the absolute Shapley
values over all feature values (i.e. instances) in the
evaluated dataset, which in our case was the test-set.
3 EXPERIMENTAL RESULTS
For each experiment evaluated in this study (2-class
or 3-class classification), the dataset was randomly
split into a training set (70%) and a test set (30%),
ensuring that the class frequencies were preserved in
both sets. The ML models’ performance was
measured in terms of Accuracy (Acc), Precision (Pre)
and Recall (Rec).
For 2-class classification, the positive and
negative class was BT and ET, respectively. For 3-
ICPRAM 2025 - 14th International Conference on Pattern Recognition Applications and Methods
468
class classification Acc was calculated as the sum of
the diagonal elements of the confusion matrix (CM)
over the total number of test samples. For Pre and Rec
we adopted a 'macro' average approach by calculating
each metric individually for every label, which was
considered as the positive class, and subsequently
determining their unweighted mean.
3.1 Classification Results
Tables 2 and 3 show the results for the first (2-class
classification) and the second (3-class classification)
experiment, respectively. The results are shown
separately for each surgical task. Note also that for
these experiments we excluded the TN (trial number)
feature, so in total 11 out of 12 features were
considered (see Table 1). The reason for excluding
TN was to examine the potential for broader
applicability of the proposed methodology in
evaluating the students’ skills before entering the
training curriculum (see also Discussion). Overall,
the results in both experiments show better
performance for Task 5 and 6 compared to Task 7.
This may be due to the fact that by the time the
trainees start training on Task 7, they have already
mastered the skills required to achieve proficiency in
Table 2: Performance comparison for 2-class classification
without using the trial number feature (w/o TN). Best
results column-wise are shown in bold.
Method Acc (%) Pre (%) Rec (%)
Task 5 (w/o TN)
SVM-Lin 97.2 97.4 97.2
SVM-RBF 97.2 97.4 97.2
LDA 94.4 95.0 94.4
RF 97.2 97.4 97.2
LR 97.2 97.4 97.2
GNB 94.4 95.0 94.4
Task 6 (w/o TN)
SVM- Lin 94.7 94.7 94.7
SVM-RBF 92.1 92.2 92.1
LDA 86.8 86.9 86.8
RF 94.7 94.7 94.7
LR 84.2 84.6 84.2
GNB 86.8 87.7 86.8
Task 7 (w/o TN)
SVM- Lin 84.2 85.8 84.2
SVM-RBF 84.2 84.6 84.2
LDA 78.9 79.3 78.9
RF 81.6 81.7 81.6
LR 78.9 80.3 78.9
GNB 76.3 78.3 76.3
this task. Moreover, the results for 2-class
classification are much better than the results for 3-
class classification, as expected. Overall, the best
model is SVM. SVM-Lin shows the best performance
compared to all other algorithms as the Acc, Pre and
Rec were the highest in five out of the six
experimental runs (2 experiments for 3 surgical
tasks). In particular, with regard to the first
experiment (2 classes), Acc for Task 5, 6 and 7 was
close to 97%, 95% and ~84%, respectively. For the
second experiment (3-classes) Acc was lower, about
76%, 82% and 67%, for Task 5, 6 and 7, respectively.
No significant difference was found between the Pre
and Rec values in both experiments.
Table 3: Performance comparison for 3-class classification
without using the trial number feature (w/o TN). Best
results column-wise are shown in bold.
Method Acc (%)
Pre (%) Rec (%)
Task 5 (w/o TN)
SVM-Lin 75.9 77.8 75.9
SVM-RBF 74.1 74.2 74.1
LDA 64.8 67.8 64.8
RF 72.2 72.9 72.2
LR 66.7 67.0 66.7
GNB 70.4 70.3 70.4
Task 6 (w/o TN)
SVM- Lin 80.7 80.8 80.7
SVM-RBF 82.5 83.1 82.5
LDA 73.7 74.9 73.7
RF 75.4 75.5 75.4
LR 78.9 79.6 78.9
GNB 77.2 77.8 77.2
Task 7 (w/o TN)
SVM- Lin 67.3 70.0 67.6
SVM-RBF 63.5 63.6 63.7
LDA 59.6 63.2 59.7
RF 61.5 62.1 61.8
LR 63.5 63.2 63.7
GNB 59.6 59.0 59.8
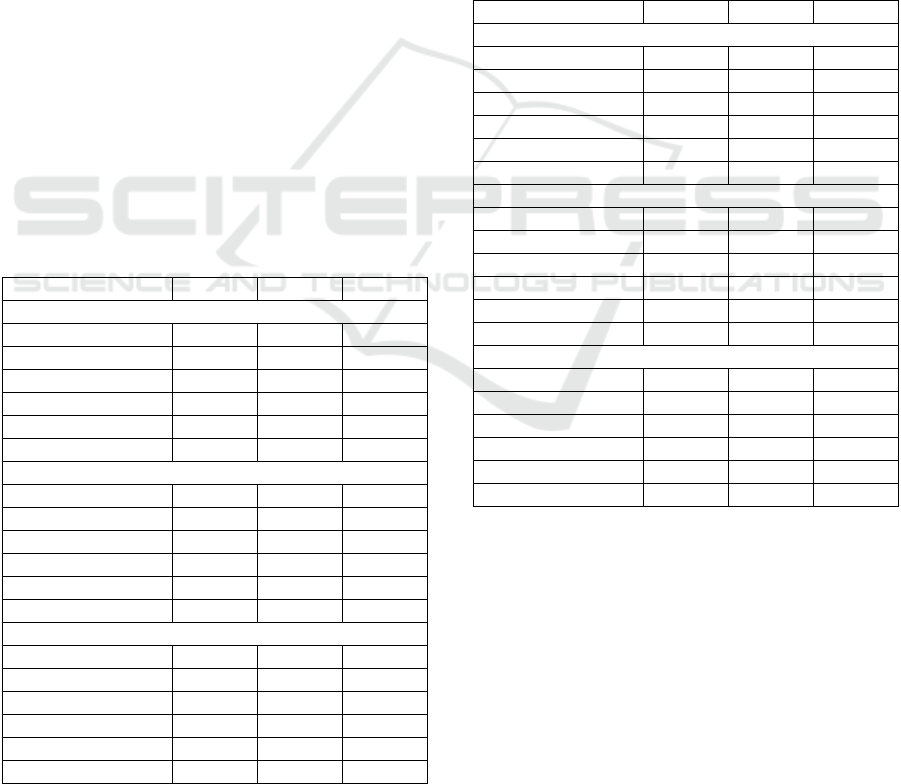
Figure 2 shows the CMs for SVM-Lin when using
11 features (i.e. without TN). For the 2-class
classification experiment, the performance is similar
for the two classes. For 3-class classification the best
performance is for the BT class and the second-best
for the ET class. Most of the confusion occurs
between MT and ET, especially when the ground-
truth is the MT class. This may be because trainees in
the middle of training have acquired much more skills
compared to the beginning, and thus are close to
achieving the required proficiency to complete the
task successfully.
Assessment of Training Progression on a Surgical Simulator Using Machine Learning and Explainable Artificial Intelligence Techniques
469
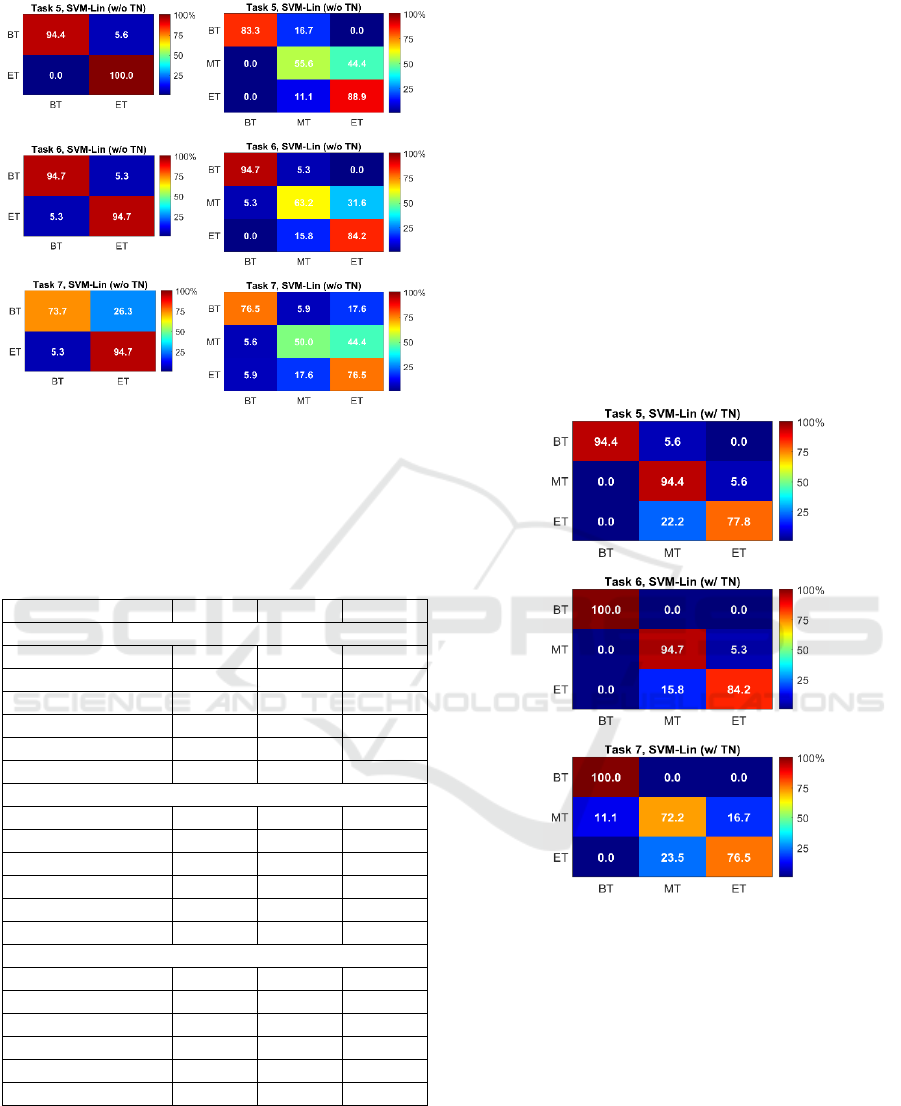
Figure 2: Color-coded confusion matrices for SVM-Lin
when using 11 features (i.e. without TN). The X and Y-axis
represent predicted and ground truth labels, respectively
(left/right CMs: 2-/3-class classification).
Table 4: Performance comparison for 3-class classification
when using all 12 features (i.e. including TN: w/ TN). Best
results column-wise are shown in bold.
Method
Acc (%) Pre (%) Rec (%)
Task 5 (w/ TN)
SVM-Lin 88.9 90.2 88.9
SVM-RBF 83.3 86.3 83.3
LDA 81.5 84.4 81.5
RF 87.0 88.0 87.0
LR 85.2 86.7 85.2
GNB 79.6 80.2 79.6
Task 6 (w/ TN)
SVM- Lin 93.0 93.3 93.0
SVM-RBF 94.7 95.5 94.7
LDA 87.7 89.3 87.7
RF 91.2 91.9 91.2
LR 93.0 93.3 93.0
GNB 86.0 86.5 86.0
Task 7 (w/ TN)
SVM- Lin 82.7 82.4 82.9
SVM-RBF 86.5 87.6 86.5
LDA 80.8 81.1 81.0
RF 82.7 83.3 83.0
LR 80.8 81.5 80.9
GNB 76.9 80.3 77.3
Table 4 presents the performance for 3-class
classification when using all available features (i.e. 12
features, including TN). Compared to the results
shown in Table 3, it may be seen that the performance
of all algorithms has been improved in all surgical
tasks by about 13% for Task 5 and 6 and close to 20%
for Task 7. SVM-RBF yields the best performance for
Tasks 6 and 7 with Acc close to 95% and 87%,
respectively. For Task 5 the best performance is
shown by SVM-Lin with Acc close to 90%, whereas
for Task 6 and 7 the best method is SVM-RBF.
Figure 3 shows the CMs for SVM-Lin when using
all available features (i.e. with TN). Compared to the
corresponding CMs shown in Figure 2, the best
performance is presented when the ground-truth
classes are BT and MT for Task 5 and 6 and ET for
Task 7, but only slightly compared to MT. Similarly
to the corresponding results in Figure 2, the greatest
confusion occurs between the MT and ET classes, but
now the misclassification is greater when the ground-
truth class is ET, probably because the TN values of
this class are more similar to those of MT compared
to the other features.
Figure 3: Color-coded confusion matrices for SVM-Lin
when using all 12 features (i.e. with TN). The X and Y-axis
represent predicted and ground truth labels, respectively (3-
class classification CMs).
3.2 XAI Results
Figure 4 demonstrates the feature significance of
SVM-Lin for the two XAI methods (PFI and SHAP),
separately for each surgical task and classification
experiment (2- and 3-class classification with or
without the TN feature). To allow for better
comparison between PFI and SHAP, the feature
importance score was normalized by the score sum of
all features used in each corresponding experiment.
ICPRAM 2025 - 14th International Conference on Pattern Recognition Applications and Methods
470
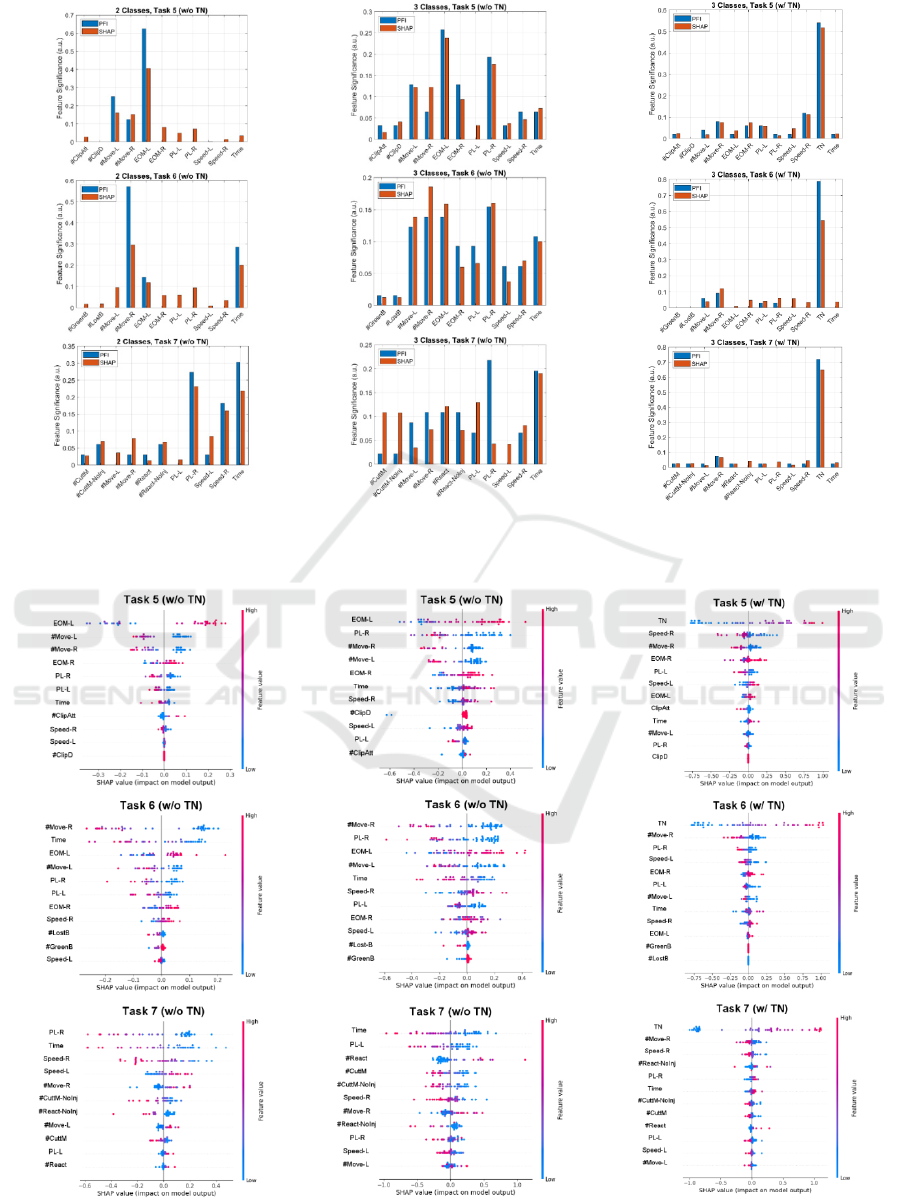
Figure 4: Normalized feature importance score (feature significance) of the two XAI methods for each classificatio
n
experiment and surgical task.
Figure 5: SHAP summary plots for SVM-Lin. Each plot corresponds to a different surgical task and classification experiment
.
Assessment of Training Progression on a Surgical Simulator Using Machine Learning and Explainable Artificial Intelligence Techniques
471

Overall, the two XAI methods seem to agree on
the relative impact of each feature. For example, for
2-class classification the two features with the
greatest impact are: EOM-L, #Move-L (Task 5),
#Move-R, Time (Task 6) and Time, PL-R (Task 7).
For 3-class classification without TN (w/o TN) the
two features with the greatest impact are: EOM-L,
PL-R (Task 5),
#Move-R, PL-R (Task 6) and Time, PL-R/PL-L
(Task 7). Thus, features related to technical skill and
bimanual dexterity (e.g. economy of movement, # of
movements and instrument pathlength) seem to play
the most important role, followed by the time
parameter that relates to how fast the trainee
completes the task. For 3-class classification with TN
(w/ TN), the TN feature has by far the greatest impact
among all features, having a relative score >50% for
Task 5, and >70% for Task 6 and Task 7.
Figure 5 shows SHAP summary plots, based on
the SVM-Lin model, for each surgical task and
classification experiment (2- or 3-class classification
and with or without using the TN feature). This type
of plot can be used to visualize the relative impact of
all features over the entire dataset (in this case the
test-set). Features are sorted by the sum of their
SHAP value magnitudes across all samples. SHAP
values less than 0, equal to 0 and greater than 0 signify
negative contribution, no contribution and positive
contribution, respectively. For each instance, the
given explanation is represented by a single dot on
each feature row and the x position of the dot is
determined by its SHAP value. The vertical colorbar
to the right of the axes indicates the mapping of
feature values (from low to high). In essence, more
proficient technical skills, which are acquired towards
the end of training phase, are indicated by higher
values of EOM (economy of movement) and lower
values of pathlength (PL) or/and number of
movements (#Move), as expected.
4 CONCLUSIONS
In this paper we evaluate an ML framework for
classifying trainees’ performance with respect to the
phase of training progression on a VR laparoscopic
simulator using the output performance metrics
(features). SVM showed the best performance with
>84% accuracy in the 2-classification experiments
when using 11 features (i.e. w/o TN) and >86% in the
3-class classification experiment when using 12
features (i.e. w/ TN), in all three surgical tasks
evaluated. The reason for not using TN in the initial
experiments was to allow for broader application
potential of the proposed methodology. For example,
in addition to informing a trainee about the phase of
his/her training progression on the simulator, the
proposed framework could also be used to inform
trainees outside the training curriculum about their
skill level. In this case, the trainee could obtain
potentially useful information about the training
effort required to successfully complete a particular
surgical task.
With respect to the XAI experiments, the two XAI
methods (PFI and SHAP) seem to agree on the
relative impact of each performance metric. Features
related to technical skills and bimanual dexterity
seem to play the most important role both in the 2-
and 3-class classification experiments (e.g. EOM, PL
and #Move). Goal-oriented features with respect to
each task seem less important in explaining the
classification results. When used, the TN feature
seems to outperform all other features in the 3-class
classification experiments, probably due to the
similar number of trials performed in each phase of
training progression by all students.
Despite the study’s findings, some limitations
must be addressed. First, our dataset includes training
trials from 23 medical students and may not capture
the overall variability in surgical skill acquisition. In
future research we plan to increase the sample size by
including more trainees and expert surgeons. Second,
although the construct validity of VR surgical
simulators has been addressed by several studies in
the past (Aggarwal et al., 2007), (Aggarwal et al.,
2009), in the future we aim to examine the
educational value of our training curriculum by
evaluating it on real-world surgical tasks for groups
with and without VR training. Third, in this study we
examined the classification of training progress in
predefined classes. The classes were defined by hard
thresholds, which separated each subject's trials into
equal parts based on their order in the training
sequence. As future work we intend to develop a
framework that predicts the Objective Structured
Assessment of Technical Skill (OSATS) score and
thus obtain a grade of the training progress (Martin et
al., 1997). Furthermore, subsequent application of
XAI techniques could provide students with valuable
insight into the progression of their skills, thereby
enhancing the overall quality of surgical training.
ACKNOWLEDGEMENTS
The author thanks Special Account for Research
Grants and National and Kapodistrian University of
Athens for funding to attend the meeting.
ICPRAM 2025 - 14th International Conference on Pattern Recognition Applications and Methods
472

REFERENCES
Aggarwal, R., Ward, J., Balasundaram, I., Sains, P.,
Athanasiou, T., and Darzi, A. (2007). Proving the
effectiveness of virtual reality simulation for training in
laparoscopic surgery. Annals of Surgery, 246(5), 771–
779.
Aggarwal, R., Crochet, P., Dias, A., Misra, A., Ziprin, P.,
and Darzi, A. (2009). Development of a virtual reality
training curriculum for laparoscopic cholecystectomy.
British Journal of Surgery, 96(9), 1086–1093.
Benmansour, M., Malti, A., and Jannin, P. (2023). Deep
neural network architecture for automated soft surgical
skills evaluation using objective structured assessment
of technical skills criteria. International Journal of
Computer Assisted Radiology and Surgery, 18(5), 929–
937.
Dosis, A., Aggarwal, R., Bello, F., Moorthy, K., Munz, Y.,
Gillies, D., and Darzi, A. (2005). Synchronized video
and motion analysis for the assessment of procedures in
the operating theater. Archives of Surgery, 140(3), 293–
299.
Fard, M. J., Ameri, S., Darin Ellis, R., Chinnam, R. B.,
Pandya, A. K., and Klein, M. D. (2018). Automated
robot-assisted surgical skill evaluation: Predictive
analytics approach. International Journal of Medical
Robotics and Computer Assisted Surgery, 14(1), 1–10.
Fisher, A., Rudin, C., and Dominici, F. (2019). All models
are wrong, but many are useful: learning a variable’s
importance by studying an entire class of prediction
models simultaneously. Journal of Machine Learning
Research, 20, 177.
Fogelson, N., Loukas, C., Brown, J., and Brown, P. (2004).
A common N400 EEG component reflecting contextual
integration irrespective of symbolic form. Clinical
Neurophysiology, 115(6), 1349–1358.
Guedes, H. G., Câmara Costa Ferreira, Z. M., Ribeiro de
Sousa Leão, L., Souza Montero, E. F., Otoch, J. P., and
Luiz de Almeida Artifon, E. (2019). Virtual reality
simulator versus box-trainer to teach minimally
invasive procedures: A meta-analysis. International
Journal of Surgery, 61, 60–68.
Ikonen, T. S., Antikainen, T., Silvennoinen, M., Isojärvi, J.,
Mäkinen, E., and Scheinin, T. M. (2012). Virtual reality
simulator training of laparoscopic cholecystectomies-A
systematic review. Scandinavian Journal of Surgery,
101(1), 5–12.
Kowalewski, K. F., Garrow, C. R., Schmidt, M. W.,
Benner, L., Müller-Stich, B. P., and Nickel, F. (2019).
Sensor-based machine learning for workflow detection
and as key to detect expert level in laparoscopic
suturing and knot-tying. Surgical Endoscopy, 33(11),
3732–3740.
Larsen, C. R., Grantcharov, T., Aggarwal, R., Tully, A.,
Sørensen, J. L., Dalsgaard, T., and Ottesen, B. (2006).
Objective assessment of gynecologic laparoscopic
skills using the LapSimGyn virtual reality simulator.
Surgical Endoscopy and Other Interventional
Techniques, 20(9), 1460–1466.
Loukas, C., Nikiteas, N., Kanakis, M., and Georgiou, E.
(2011). The contribution of simulation training in
enhancing key components of laparoscopic
competence. The American Surgeon, 77(6), 708–715.
Lundberg, S. M., Allen, P. G., and Lee, S.-I. (2017). A
unified approach to interpreting model predictions.
Proceedings of the 31
st
International Conference on
Neural Information Processing Systems, 4768–4777.
Martin, J.A., Regehr, G., Reznick, R., Macrae, H.,
Murnaghan, J., Hutchison, C., Brown, M (1997).
Objective Structured Assessment of Technical Skill
(OSATS) for surgical residents. British Journal of
Surgery, 84(2), 273–278.
Matzke, J., Ziegler, C., Martin, K., Crawford, S., and
Sutton, E. (2017). Usefulness of virtual reality in
assessment of medical student laparoscopic skill.
Journal of Surgical Research, 211, 191–195.
Mirchi, N., Bissonnette, V., Yilmaz, R., Ledwos, N.,
Winkler-Schwartz, A., and Del Maestro, R. F. (2020).
The Virtual Operative Assistant: An explainable
artificial intelligence tool for simulation-based training
in surgery and medicine. PLoS ONE, 15(2), e0229596.
Moglia, A., Morelli, L., D’Ischia, R., Fatucchi, L. M.,
Pucci, V., Berchiolli, R., Ferrari, M., and Cuschieri, A.
(2022). Ensemble deep learning for the prediction of
proficiency at a virtual simulator for robot-assisted
surgery. Surgical Endoscopy, 36(9), 6473–6479.
Molnar, C. (2022). Interpretable machine learning: a guide
for making black box models explainable. Ebook.
https://christophm.github.io/interpretable-ml-book/.
Ribeiro, M. T., Singh, S., and Guestrin, C. (2016). Model-
agnostic interpretability of machine learning. arXiv
preprint. arXiv:1606.05386v1.
Rosen, J., Brown, J. D., Chang, L., Sinanan, M. N., and
Hannaford, B. (2006). Generalized approach for
modeling minimally invasive surgery as a stochastic
process using a discrete Markov model. IEEE
Transactions on Bio-Medical Engineering, 53(3), 399–
413.
Shafiei, S. B., Durrani, M., Jing, Z., Mostowy, M., Doherty,
P., Hussein, A. A., Elsayed, A. S., Iqbal, U., and Guru,
K. (2021). Surgical hand gesture recognition utilizing
electroencephalogram as input to the machine learning
and network neuroscience algorithms. Sensors, 21(5),
1733.
Siyar, S., Azarnoush, H., Rashidi, S., Winkler-Schwartz,
A., Bissonnette, V., Ponnudurai, N., and Del Maestro,
R. F. (2020). Machine learning distinguishes
neurosurgical skill levels in a virtual reality tumor
resection task. Medical and Biological Engineering and
Computing, 58(6), 1357–1367.
Soto Rodriguez, N. A., Arroyo Kuribreña, C., Porras
Hernández, J. D., Gutiérrez-Gnecchi, J. A., Pérez-
Escamirosa, F., Rigoberto, M. M., Minor-martinez, A.,
and Lorias-Espinoza, D. (2023). Objective evaluation
of laparoscopic experience based on muscle
electromyography and accelerometry performing
circular pattern cutting Tasks: a pilot study. Surgical
Innovation, 30(4), 493–500.
Assessment of Training Progression on a Surgical Simulator Using Machine Learning and Explainable Artificial Intelligence Techniques
473

Stefanidis, D., Korndorffer, J. R., Sierra, R., Touchard, C.,
Dunne, J. B., and Scott, D. J. (2005). Skill retention
following proficiency-based laparoscopic simulator
training. Surgery, 138(2), 165–170.
Varras, M., Nikiteas, N., Varra, V. K., Varra, F. N.,
Georgiou, E., and Loukas, C. (2020). Role of
laparoscopic simulators in the development and
assessment of laparoscopic surgical skills in
laparoscopic surgery and gynecology (Review). World
Academy of Sciences Journal, 2(2), 65–76.
Vedula, S. S., Ishii, M., and Hager, G. D. (2017). Objective
assessment of surgical technical skill and competency
in the operating room. Annual Review of Biomedical
Engineering, 19(1), 301–325.
Wang, Z., and Majewicz Fey, A. (2018). Deep learning
with convolutional neural network for objective skill
evaluation in robot-assisted surgery. International
Journal of Computer Assisted Radiology and Surgery,
13(12), 1959–1970.
Winkler-Schwartz, A., Yilmaz, R., Mirchi, N., Bissonnette,
V., Ledwos, N., Siyar, S., Azarnoush, H., Karlik, B.,
and Del Maestro, R. (2019). Machine learning
identification of surgical and operative factors
associated with surgical expertise in virtual reality
simulation. JAMA Network Open, 2(8), e198363.
Zia, A., Sharma, Y., Bettadapura, V., Sarin, E. L., and Essa,
I. (2018). Video and accelerometer-based motion
analysis for automated surgical skills assessment.
International Journal of Computer Assisted Radiology
and Surgery, 13(3), 443–455.
ICPRAM 2025 - 14th International Conference on Pattern Recognition Applications and Methods
474
