
A Multiple Source Data Collection and Integration Paradigm for the
Creation of a Dynamic COPD Data Mart
Giulio Pagliari
1a
, Agni Delvinioti
1b
, Nicoletta Di Giorgi
1c
, Maria Vittoria De Girolamo
1d
,
Angela Nervoso
2e
, Francesco Macagno
2f
, Carlotta Masciocchi
1g
,
Stefano Patarnello
1h
and Alice Luraschi
1i
1
Gemelli Generator RWD R&D, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Largo Agostino Gemelli 8,
00168 Rome, Italy
2
CEMAR, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Largo Agostino Gemelli 8, 00168 Rome, Italy
Keywords: Digital Health, Medical Informatics, COPD, Data Collection, Heterogeneous Data Sources, Real World Data.
Abstract: The creation of dynamic data marts in a hospital environment is challenging due to the number of different
data sources, the heterogeneity of data formats and the availability of structured datasets. Other than
identifying the relevant pathology and related information, the interaction with the Hospital Information
System requires dedicated personnel and an in-depth knowledge of the IT architecture of the Hospital. In this
paper, we show an ad-hoc solution for the RE-SAMPLE project in Fondazione Policlinico Universitario
Agostino Gemelli IRCCS, where the Chronic Obstructive Pulmonary Disease (COPD) is studied and a
framework for managing that pathology is proposed. The final aim of this work is to provide a description of
the tailored procedures of data extraction, integration and harmonization, and the final creation of a dedicated
COPD data mart for research purposes that has been implemented in the hospital premises by Gemelli
Generator RWD R&D.
1 INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a
common lung pathology, considered as the third
leading cause of death worldwide (WHO, 2023). Due
to symptoms as chronic cough or breathing difficulty,
this condition has a great impact on patients’ daily
life. COPD is considered as non-curable and is often
accompanied by other comorbidities, such as chronic
heart failure, anxiety and depression, and other
adverse conditions that require attention and specific
care for patients. For these reasons, patients often
need to perform follow-up visits and to stay in touch
with clinicians to report any event or exacerbation.
a
https://orcid.org/0000-0001-8481-1529
b
https://orcid.org/0000-0002-2402-9444
c
https://orcid.org/0000-0002-8033-5411
d
https://orcid.org/0009-0003-4046-6454
e
https://orcid.org/0009-0005-4976-9691
f
https://orcid.org/0000-0001-9603-9660
g
https://orcid.org/0000-0001-6415-7267
h
https://orcid.org/0009-0008-2765-5935
i
https://orcid.org/0000-0001-7400-7182
The RE-SAMPLE project (accessible at
https://www.re-sample.eu/) has the objective of
creating a digital framework to support patients in
managing their complex chronic conditions deriving
from the concurrent presence of COPD and other
comorbidities. With the use of a mobile application
and a clinical dashboard, patients can be monitored
remotely and can receive tailored suggestions to
manage their health condition. Leveraging on AI
models, risk profiles can be delivered to health care
professionals (HCPs) and, together with the clinical
and self-reported data of each single patient, can be
used as an additional source of information for
predicting symptom worsening and quality of life.
Pagliari, G., Delvinioti, A., Di Giorgi, N., Vittoria De Girolamo, M., Nervoso, A., Macagno, F., Masciocchi, C., Patarnello, S. and Luraschi, A.
A Multiple Source Data Collection and Integration Paradigm for the Creation of a Dynamic COPD Data Mart.
DOI: 10.5220/0013150100003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 507-514
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
507

Through the use of the project tools, the patient can
in fact easily report any exacerbation or event,
moving their usual care from the hospital to their
home and potentially minimizing the number of
hospitalizations adverse events day-by-day.
In this paper, we detail the methodology, and the
framework developed for the identification and the
integration of multiple data sources in the hospital
with the final release of a daily updating data mart
compliant to the common project data model and
specific data quality standards. The data mart serves
as a data source for the ingestion of patient data to a
Fast Healthcare Interoperability Resources (HL7
FHIR) based data repository for further federated
learning and data visualization tasks. Details on the
technical requirements and the implementation of the
RE-SAMPLE platform are beyond the scope of this
work.
The last years, there is growing interest in
exploring the benefits from the re-utilization and the
integration of Electronic Health Records (EHR) in
clinical trials (Kalankesh, 2024) (Nordo, 2019). At
the same time, digital tools are introduced to facilitate
clinical trial management especially during patient
screening and enrolment tasks (Kasahara, 2024). In
this work, we explore both EHR integration for data
collection along with data validation from multiple
sources and dedicated screening and enrolment
applications as a part of the RE-SAMPLE
infrastructure.
Main challenges in data collection in a real-world
setting, such as the hospital environment, are the
heterogeneity of data sources – which need to be
identified and mapped within the hospital, along with
data availability. A description of this problem has
been addressed in other works including (Kwok,
2022) and (Kerkri, 2001), and a description of
different solutions were reported in (Mate, 2015),
where an ontology-based solution is presented, or
(Jayaratne, 2019), where the authors introduce an
open data integration platform across different
sources. The creation of research datasets in such
context remains a challenging problem and often
leads to ad-hoc solutions that are tailored on the
specific Hospital. In COPD research domain, most
works focus on data modelling and disease
characterization problems while few ones focus on
systematic data collection such as the collaborative
approach for the definition of a COPD dataset in a
Healthcare System reported in (Lam, 2023).
To tackle these challenges in RE-SAMPLE
project, a core facility of Fondazione Policlinico
Universitario Agostino Gemelli IRCCS (FPG) named
Gemelli Generator RWD R&D (Damiani et al., 2021)
has developed a dedicated pipeline for data extraction
and data collection with the aim of retrieving all
required information from the different data sources
that are present in the hospital, including internal
tools that support HCPs in managing the prospective
study. The group has a relevant track record in the
creation of research data marts for other pathologies,
such as breast cancer (Marazzi, 2021), heart failure
(D’Amario, 2023), dyslipidemia (Capece, 2024) or
Covid-19 (Murri, 2022). FPG team actively
participated in the definition of both clinical and
technical requirements of the RE-SAMPLE platform.
To this end, a crucial task was the definition of a
common data model (Acebes et al., 2022), that
includes all the clinically relevant variables for
characterizing the health profile of COPD patients. In
fact, several variables are required to capture the
health condition of COPD patients with chronic
complex conditions. Functional scores based on
spirometry measurements, blood samples, along with
six-minute walking tests and Patient-Reported
Outcomes (PROs) on life habits (e.g. smoking) and
symptoms are needed for providing to Health Care
Professionals (HCPs) a complete overview of the
actual health status of the patient.
Data collection in the hospital requires a shared
effort between clinicians and a dedicated technical
team not only for the conduction of regular outpatient
visits but also for the development of data extraction
procedures from the Hospital Information System
(HIS) or the EHR that make hospital data available
for further visualization and modeling tasks.
In the following sections, a description of the
implementation of an ad-hoc solution for the creation
of the RE-SAMPLE data mart in FPG is reported,
along with the results of the deployment and use of
the defined procedures.
2 METHODS
As shown in Figure 1, the creation of the RE-
SAMPLE data mart stems from the need of collecting
clinical and secondary data for all the patients
included in the project. As a first step, screening is
required before asking a patient to join the study. This
step is made via a web-based recruitment app, where
all the inclusion and exclusion criteria are
standardized. Interacting with this tool, HCPs can
understand whether a patient is eligible for the
participation in the study and consequently being
enrolled.
HEALTHINF 2025 - 18th International Conference on Health Informatics
508
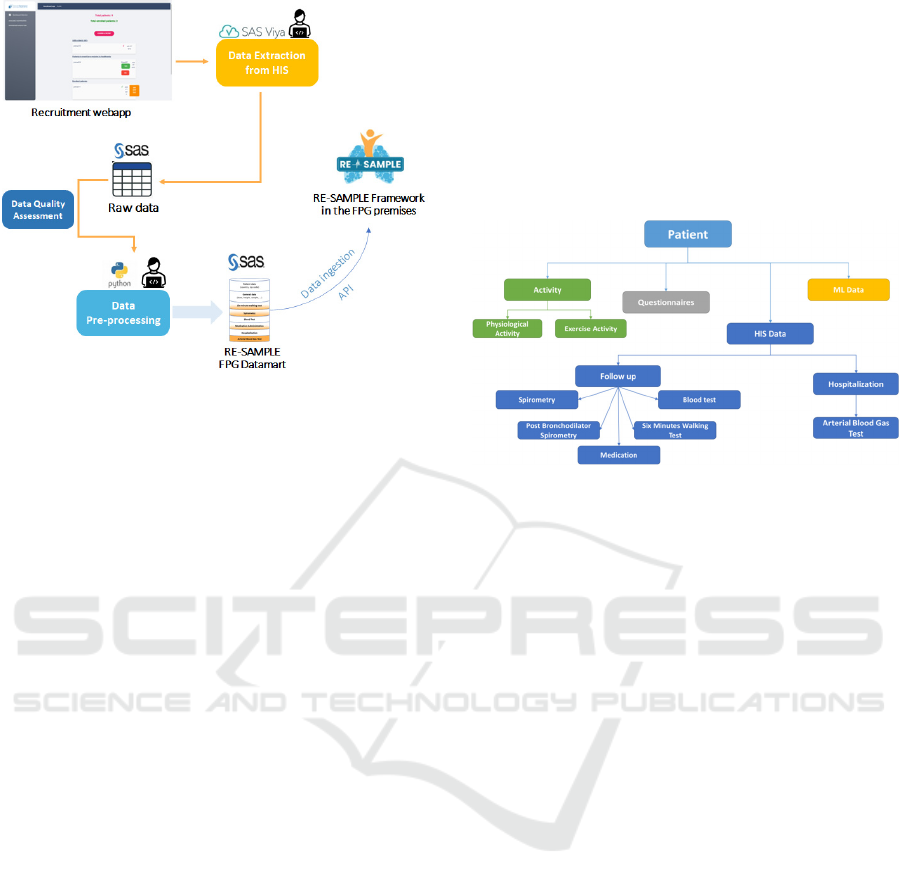
Figure 1: Data pipeline from patient screening to enrolment
and creation of the data mart, including the interaction with
the RE-SAMPLE framework in the FPG premises, hosted
in a dedicated Virtual Machine.
Once the study cohort is identified, and patients
are mapped within the HIS, for all the different
patients primary and secondary data should be
retrieved through dedicated queries and pipelines. In
the schema shown in Figure 1, raw data from the
Hospital Data Warehouse are collected and processed
to create the final project dataset.
In the following sections, we present how the data
model was defined and how data sources were
mapped and integrated within FPG, towards the
creation of the final RE-SAMPLE data mart.
2.1
HIS Dataset
The Hospital Information System (HIS) dataset as
defined in RE-SAMPLE project (Acebes et al, 2022)
includes several data categories organized in distinct
time reference points. Namely, variables get collected
during enrolment and a required baseline visit, during
follow-up visits with a six-month frequency and
during in-patient hospital visits. As demonstrated in
Figure 2, in every time reference point named
encounter, specific data is captured. Finally,
additional data during different encounters such as
inpatient and emergency visits are also included.
During enrolment, the clinical team consisted of
pulmonologists and research nurses report general
patient information including zip code and biometric
data such as body mass index. A spirometry test is
performed to evaluate COPD diagnosis using the
Global Initiative for Chronic Obstructive Lung
Disease (GOLD) classification (Agustí et al, 2023).
Eligible patients are requested to perform a six-
minute walking test and blood exams. Moreover, the
clinical team captures information related to clinical
history including exacerbations, hospitalizations,
smoking, and medication plan and complete together
with the patient different questionnaires related to
general health, COPD and comorbidity symptoms
and mental state. Similar data gets collected
successively during follow-up visits apart from some
questionnaires.
Figure 2: HIS Dataset as a subset of RE-SAMPLE data
model. For simplicity we consider also baseline visits as a
type of follow-up visit. Adapted from (Acebes et al, 2022).
Regarding hospitalization instead, the dataset
includes additional variables related to arterial blood
gas tests typically performed during inpatient visits,
oxygen use, mechanical ventilation procedures, and
pneumonia.
2.2 Data Sources
The different data categories required for the RE-
SAMPLE project tasks, get effectively stored in
different data sources in the hospital and in different
formats. This requires the creation of a procedure that
retrieves data from multiple systems and creates an
integrated and harmonized project data mart. In this
section, a description of the different data sources is
provided.
2.2.1 Electronic Health Records (EHRs)
In clinical practice, all data reported by medical
personnel during hospital visits, inpatient, or
outpatient, gets collected in dedicated hospital
systems and stored within the hospital data warehouse
(DWH). Part of these sources contain information
stored in a structured format, while e.g. in clinical
notes and discharge letters are typically available in
an unstructured text format containing a summary of
the details collected during visits or medical
procedures.
A Multiple Source Data Collection and Integration Paradigm for the Creation of a Dynamic COPD Data Mart
509
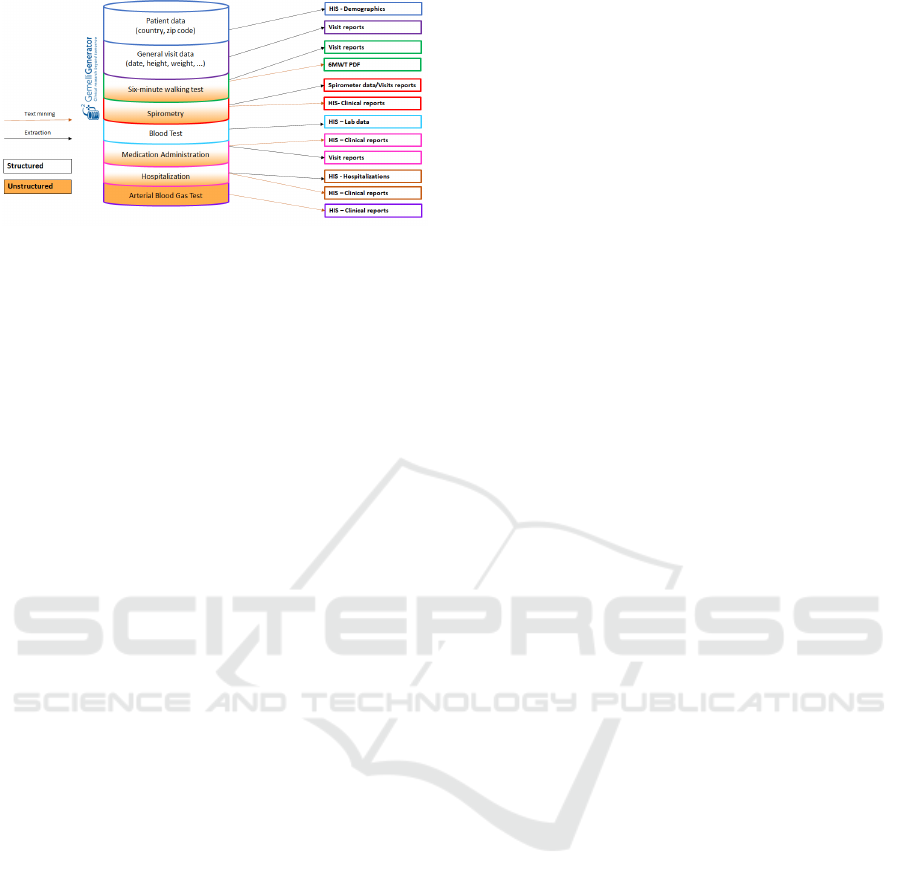
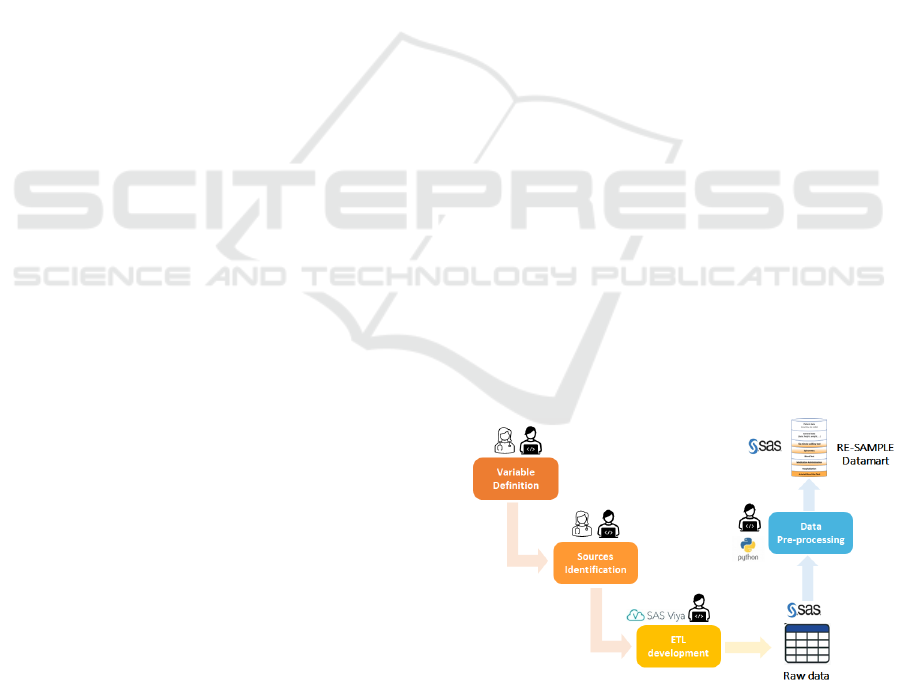
Figure 3: Data categories mapped into data sources.
Figure 3 reports a schematic view of the final RE-
SAMPLE data mart in FPG, i.e. a curated patient-
centered data repository that includes a subset of all
the available data related to the project within the
hospital’s IT system and data warehouse.
Administrative visit data and laboratory related data
are instead stored in a structured format. Medications
and arterial blood gas test data get extracted from
clinical notes and discharge letters. All this data is
accessible in the FPG data warehouse in a centralized
manner.
2.2.2 Medical Devices
Spirometry and six-minute walking test data is stored
locally in medical device dedicated application
storages. During functional tests, a dedicated
application accompanies each medical device and
produces reports in pdf files that include all
measurements performed during the tests. Typically,
this data is not integrated in the hospital data
warehouse and its extraction requires additional effort
and dedicated extraction pipelines: in our case, data is
retrieved from the devices and saved in the HIS or in
the dedicated platform described in §2.3.1 by the
HCP that performs the visit.
2.2.3 Self-Reported Data
As mentioned before, during baseline and follow-up
visits, patients complete several questionnaires with
the assistance of the clinical team. Some of these
questionnaires are filled in on paper and later reported
in the clinical notes, while most of them are filled in,
in a tailored version of a mobile application named
Healthentia (iSprint, 2021). The HIS dataset includes
only information extracted from centralized hospital
systems or locally from medical device storages.
External data collected through the patient
application during the study are out of scope of this
manuscript.
2.3 Data Collection and Data
Integration Framework
Data collection is performed in every phase of a
prospective clinical study, from the screening of the
patients to enrol until the follow-up visits. While
during hospital visits data is collected by procedure in
hospital systems, this is not the case during screening
and enrolment phase. Furthermore, in the specific
RE-SAMPLE project use case, in the beginning of the
study the patient needs to be evaluated for enrolment.
Successively, he or she also needs to be registered in
an external mobile application for being monitored
and fill in self-reported questionnaires.
To cover such need during enrolment, we
developed a dedicated patient enrolment application
that facilitates screening but also allows for
registering new patients in the mobile application in
an automated way. During enrolment, the internal
hospital unique identifier gets mapped to the subject
ID unique identifier assigned to the patient in the
mobile application for the specific study. Such a
requirement is crucial to make possible the
integration of the various data from the different data
domains; in hospital and external that are kept
carefully separated in the entire RE-SAMPLE
platform following a privacy preserving by design
principle. Overall, all this heterogenous data coming
from multiple data sources needs to be integrated in a
unique data storage following the RE-SAMPLE data
model and daily updated with new encounter data for
further visualization and modelling tasks.
2.3.1 RE-SAMPLE Enrolment and
Screening Applications
As previously mentioned, a custom enrolment web
application has been developed within Gemelli
Generator RWD R&D services to standardize and
streamline patient screening and enrolment processes.
The RE-SAMPLE enrolment application, based on a
Django v. 3.2.16 and Python v3.11 framework,
centralizes diverse features useful for clinicians in the
preliminary phase of patient assessment. Patient
characteristics are evaluated in a structured way,
selecting different alternatives through drop-down
menus. Once patient inclusion and exclusion criteria
are assessed, they get automatically integrated to
define patient eligibility. Eligible patients who agree
to participate, get enrolled in the clinical study and a
unique in-study identifier is systemically assigned to
each of the one. Pre-registration in Healthentia is
integrated by a simple click in the enrolment
application workflow. An overview page allows
HEALTHINF 2025 - 18th International Conference on Health Informatics
510
clinicians to observe enrolled and drop-out patients,
due and effective follow-up visit dates, and to monitor
enrolled patient number over time. Patients table is
daily recovered from the application SQLite database
and stored in a SAS data repository included in
dedicated storage areas (SAS Viya 3.5 Caslibs). RE-
SAMPLE cohort definition is thus carried out to
further extract patient information from HIS.
Additionally, the application has been designed to
collect specific clinical reports hard to retrieve from
HIS with standard procedures (e.g. six-minutes
walking test reports). The RE-SAMPLE enrolment
app is accessible only in intranet from hospital's
internal systems and through specific authentication
using accounts reserved for clinical team members.
The inclusion and exclusion criteria integration
algorithm, implemented within the enrolment
application on the basis of the study protocol, has
been further used in the development of a supporting
tool for the identification of patients who might
benefit from the RE-SAMPLE prospective study out
of the FPG Hospital. Indeed, a completely
anonymized version of the algorithm has been
integrated in a screening application. The RE-
SAMPLE screening application is developed to
provide general practitioners (GPs) with a simple and
straightforward tool for assessing RE-SAMPLE
eligibility criteria, to shorten the communication
pathway and facilitate collaboration between GP and
FPG specialist. The screening application is
externally accessible, and no patient data is collected
or exposed. GPs can easily perform a screening for
inclusion and exclusion criteria while a notification is
generated to inform FPG clinical staff when a GP
performs a positive screening. When a patient is
eligible to participate to the study, it remains GP's
responsibility to contact an FPG specialist to
introduce the patient in the study.
2.3.2 Visit Template
Clinical notes include an overview of the data
reported during hospital visits by procedure in clinical
practice. Nonetheless, the unstructured format of the
textual data remains a bottleneck for further data
availability and exploitation. The FPG technical team
introduced a visit template to be used by the clinical
team during visits and to facilitate data extraction
procedures from text stored in electronic health
records.
The visit template includes all required
information for the study organized with keywords
and specific separator characters in separate lines. In
this way, all necessary information is always present
in text and in a specific format. At the same time,
unstructured information inserted in more data
sources serves for multiple source data validation and
completion such as in the case of six-minute walking
test data, where pdf report files must be manually
uploaded to the enrolment application by the clinical
team and further processed. Below, an example of the
data structure retrieved from such document:
#DATA_RESAMPLE#
#Comorbidities
DIABETES: YES/NO \n
CHF: YES/NO \n
[...]
OTHER_COMORBIDITY: YES/NO \n
#Other Sublist
var_1: value_1\n
var_2: value_2\n
[...]
var_n: value_n\n
2.3.3 Data Extraction and Data Integration
As demonstrated in Figure 3, an Extract Transform
Load (ETL) procedure runs daily on a SAS server and
creates a dedicated SAS data repository accessible in
SAS Viya 3.5 Caslibs. This initial SAS data
repository includes all structured data such as general
patient data, administrative visit data and blood tests
and clinical notes, using as a reference the patient
cohort stored by the enrolment application in a
dedicated table. Already in this level, a rule-based
text mining procedure extracts different variables: 1)
medication data and standardizes it using Anatomical
Therapeutic Chemical (ATC) Classification codes, 2)
visit template data by analysing fixed format
keywords and 3) hospitalization variables from
discharge letters.
Figure 4: RE-SAMPLE data mart creation pipeline
Successively, a scheduled job in Python v3.9.2,
running daily on a dedicated for the project virtual
machine (OS Debian 11, 32GB RAM, 4-core Xeon
A Multiple Source Data Collection and Integration Paradigm for the Creation of a Dynamic COPD Data Mart
511
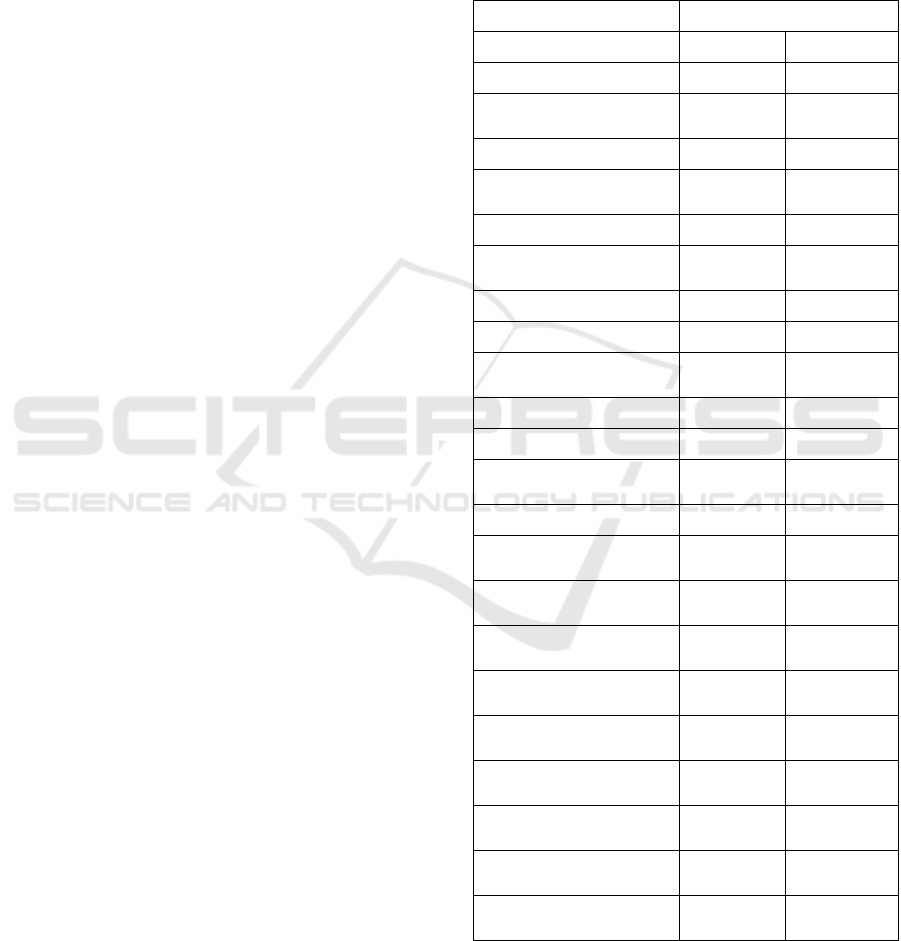
CPU) processes six-minute walking test reports
stored as pdf files in the enrolment application
database, processes and combines all different data
according to RE-SAMPLE data model into a final
SAS data repository, the RE-SAMPLE data mart.
2.3.4 Data Quality
As detailed in previous sections, data collection
involves manual procedures performed by the clinical
team. Data collected through the enrolment
application is standardized and structured and thus of
high quality. On the contrary, data extracted from text
using the visit template are more liable to errors since
the data is standardized by procedure but still inserted
manually. To mitigate such errors, to estimate and to
improve the quality of the collected data, a scheduled
job in Pyttexthon v3.9.2 is running weekly on the
same virtual machine and generates detailed reports
that include missing rates and error tables per visit
type e.g. baseline, follow up stored on the initial SAS
data repository. There are two types of reports, one
referring to the complete dataset and another only to
newly inserted data in a week time. Both reports are
automatically sent via email to the technical and
clinical team for further and timely validation.
RE-SAMPLE prospective study requires a
significant effort level from the clinical team but also
particular training in the use of the various
applications and procedures to follow. We introduce
such data quality procedures as an effort to monitor
the quality of the collected data but also to support
clinicians to recover missing information whenever
possible.
2.3.5 Data Recovery
The data quality procedure generates error tables
organized per visit type. To make sure all available
text information gets exploited, an additional rule-
based text mining pipeline extracts relevant
information from clinical notes and completes the
collected visit data, where errors or missing values
occur. A scheduled job in Python v3.9.2 is running
daily after the RE-SAMPLE data mart update and
generates tables with missing rates and data recovery
rates per data category after the integration of text
mining results. All data quality and data recovery
results are stored in the initial SAS repository.
3 RESULTS
In this section, we present some use cases of the
introduced framework for data collection and data
integration.
Table 1: Missing rates before and after data quality and data
recovery procedures for baseline visits.
Baseline visits (n=85) Missing rate (%)
Variable Initial Final
General: weight 2 (2.4%) 0 (0.0%)
SixMinuteWalkingTest:
oxygenQuantity
44 (51.8%) 0 (0.0%)
General: bmi 2 (2.4%) 0 (0.0%)
SixMinuteWalkingTest:
stopWalking
35 (41.2%) 0 (0.0%)
General: height 2 (2.4%) 0 (0.0%)
SixMinuteWalkingTest:
stopWalking
35 (41.2%) 0 (0.0%)
General: mmseScore 6 (7.1%) 1 (1.2%)
General: smokingPackYears 27 (31.8%) 1 (1.2%)
General:
mmrcDyspneaScale
4 (4.7%) 1 (1.2%)
Spirometry: fev1 11 (12.9%) 10(11.8%)
Spirometry: fev1Fvc 11 (12.9%) 10 (11.8%)
Spirometry:
fev1PercentagePredicted
11 (12.9%) 10 (11.8%)
Spirometry: fvc 11 (12.9%) 10 (11.8%)
SixMinuteWalkingTest:
minimumOxygenSaturation
35 (41.2%) 19 (22.4%)
SixMinuteWalkingTest:
medication
37 (43.5%) 23 (27.1%)
SixMinuteWalkingTest:
percentTimeBelow85
35 (41.2%) 23 (27.1%)
SixMinuteWalkingTest:
diastolicPressure
35 (41.2%) 23 (27.1%)
SixMinuteWalkingTest:
walkingAid
38 (44.7%) 23 (27.1%)
SixMinuteWalkingTest:
systolicPressure
35 (41.2%) 23 (27.1%)
SixMinuteWalkingTest:
walkedDistance
38 (44.7%) 24 (28.2%)
SixMinuteWalkingTest:
oxygenUse
44 (51.8%) 24 (28.2%)
SixMinuteWalkingTest:
theoreticalWalkedDistance
38 (44.7%) 29 (34.1%)
3.1 RE-SAMPLE Enrolment Process
In Figure 5, we present a couple of screenshots of the
enrolment application. Here, the user has access to a
HEALTHINF 2025 - 18th International Conference on Health Informatics
512

Figure 5: Enrolment application; enrolled patients overview.
Figure 6: Enrolment application; patient data view.
comprehensive overview of all planned and
completed visits as required for the specific study.
The clinical team can easily spot upcoming follow-up
visits in red and drop-out patients in orange.
Additionally, a monthly trend plot provides a better
picture of enrolment progress over time.
Instead, as shown in Figure 6, the user can access
any moment the complete list of information
collected per screened or enrolled patient.
Additionally, in this view the user can tag the patient
as drop-out and can fill in information related to
conducted follow-up visits.
3.2 Data Quality and Data Recovery
In Table 1, we report the results of the data quality
and data recovery pipelines on a specific variable
group with respect to the missing rates. As clearly
demonstrated, the overall data integration pipeline
introduced in this work, contributes significantly to
the reduction of missing rates. Please note that
missing rates also include cases of data with wrong
format where the data is available but not as expected.
4 CONCLUSIONS
In this work, we present an innovative paradigm for
collecting and integrating prospective study data from
multiple sources dynamically over time in a hospital
setting. Such methodology and framework
successfully serve RE-SAMPLE prospective study
purposes up until now, that is, the creation of a daily
updated COPD data mart available for data ingestion
into a comprehensive platform for further data
exploitation tasks.
A Multiple Source Data Collection and Integration Paradigm for the Creation of a Dynamic COPD Data Mart
513

Support applications for enrolment and screening
process significantly increase data quality and
facilitate study management. Nonetheless, clinicians
and non-technical personnel needs to be trained
properly and get progressively familiar with the
proposed tools.
Visit templates guarantee easier data integration
as all patient data remains in hospital data sources.
Additionally, clinicians do not need to use multiple
tools to insert patient data. However, they appear to
be more liable to human errors especially when the
study protocol to follow is complex and requires
significant amount of time per visit. Thus, structured
data based CRFs might be a better solution to
guarantee higher data quality with the cost of required
training and higher complexity for the clinical
personnel.
ACKNOWLEDGEMENTS
This work is supported by the RE-SAMPLE project
that has received funding from the European Union’s
Horizon 2020 research and innovation program under
grant agreement No 965315.
REFERENCES
Acebes A., et al. (2022, August 31). RE-SAMPLE D4.1:
Representation of Multi-Modal Data and Disease
Progression Monitoring Features. Available at
https://www.re-sample.eu/resources/deliverables/
(accessed October 2024)
Agustí, A., et al. (2023). Global initiative for chronic
obstructive lung disease 2023 report: GOLD executive
summary. American journal of respiratory and critical
care medicine, 207(7), 819-837.
Capece, U., et al. (2024). Real-world evidence evaluation
of LDL-C in hospitalized patients: a population-based
observational study in the timeframe 2021–2022. Lipids
in Health and Disease, 23(1), 224.
Damiani A., et al. (2021). Building an artificial intelligence
laboratory based on real world data: the experience of
gemelli generator. Frontiers in Computer Science, 3,
768266.
D’Amario, D., et al. (2023). GENERATOR HEART
FAILURE DataMart: An integrated framework for
heart failure research. Frontiers in cardiovascular
medicine, 10, 1104699.
Innovation Sprint (iSprint). (2021). Healthentia: Driving
Real World Evidence in Research & Patient Care.
Available at: https://innovationsprint.eu/healthentia
(accessed October 2024)
Jayaratne, M., et al. (2019). A data integration platform for
patient-centered e-healthcare and clinical decision
support. Future Generation Computer Systems 92 996-
1008.
Kalankesh, L. R., & Monaghesh, E. (2024). Utilization of
EHRs for clinical trials: a systematic review. BMC
medical research methodology, 24(1), 70.
Kasahara, A., et al. (2024). Digital technologies used in
clinical trial recruitment and enrollment including
application to trial diversity and inclusion: A systematic
review. Digital health, 10, 20552076241242390.
Kerkri, E. M., et al. (2001) An approach for integrating
heterogeneous information sources in a medical data
warehouse. Journal of Medical Systems 25, 167-176.
Kwok, C. S. et al. (2022). Data collection theory in
healthcare research: the minimum dataset in
quantitative studies. Clinics and practice, 12(6), 832-
844.
Lam, S.S.W., et al. (2023). Development of a real-world
database for asthma and COPD: The SingHealth-Duke-
NUS-GSK COPD and Asthma Real-World Evidence
(SDG-CARE) collaboration. BMC Med Inform Decis
Mak 23, 4
Marazzi, F., et al. (2021). Generator breast datamart—the
novel breast cancer data discovery system for research
and monitoring: Preliminary results and future
perspectives. Journal of Personalized Medicine, 11(2),
65.
Mate, S., et al. (2013) "Ontology-based data integration
between clinical and research systems." PloS one 10.1,
e0116656.
Murri, R., et al. (2022). A real-time integrated framework
to support clinical decision making for covid-19
patients. Computer Methods and Programs in
Biomedicine, 217, 106655.
Nordo, A. H., et al. (2019). Use of EHRs data for clinical
research: Historical progress and current applications.
Learning health systems, 3(1), e10076.
World Health Organization (WHO). (2023, March 16).
Chronic obstructive pulmonary disease (COPD).
Available at https://www.who.int/news-room/fact-
sheets/detail/chronic-obstructive-pulmonary-disease-
(copd) (accessed October 2024).
HEALTHINF 2025 - 18th International Conference on Health Informatics
514
