
Predicting Postpartum Depression in Maternal Health Using Machine
Learning
Maria Alejandra Terreros-Lozano
1
, Diana Lopez-Soto
2
, Samuel Nucamendi-Guillén
1
and María Alejandra López-Ceballos
1
1
Universidad Panamericana, Facultad de Ingeniería, Álvaro del Portillo 49, Zapopan, Jal, 45010, Mexico
2
Department of Industrial and Manufacturing Engineering, North Dakota State University, Fargo, ND, 58108, U.S.A.
Keywords: Postpartum Depression, Machine Learning, Maternal Health, Predictive Modelling, Random Forest, PRAMs
Data.
Abstract: Postpartum depression (PPD) is a severe mental health condition affecting mothers after childbirth,
characterized by prolonged sadness, anxiety, and fatigue. Unlike the transient "baby blues," PPD's symptoms
can last months, impacting a mother's ability to care for herself and her baby. In the U.S., PPD affects about
1 in 7 women, with a significant rise in prevalence from 13.8% to 19.8% in recent years. This condition leads
to adverse effects on maternal and infant health. Early diagnosis and treatment of PPD can help prevent long-
term depression and minimize the emotional and financial burden associated with the condition. This research
aims to evaluate machine learning models to predict PPD risk. Critical factors were identified, and an accuracy
of 96.57% and a precision of 99.88% were obtained. This predictive model enables early, personalized
interventions, aiming to improve maternal health outcomes and reduce the societal burden of PPD.
1 INTRODUCTION
Maternal health encompasses the well-being of
women throughout pregnancy, childbirth, and the
postnatal period. Health care should strive to ensure
that every phase is a positive experience, ensuring
that both women and their babies achieve their
highest potential for health and wellness.
The World Health Organization (WHO) reports
that about 140 million births occur annually, with the
percentage attended by skilled health personnel rising
from 58% in 1990 to 81% in 2019. This increase is
primarily attributed to more births in health facilities
with trained midwives and doctors (Maternal health
n.d.). From 2000 to 2020, the rise in the specialization
of maternal health care contributed to a decrease of
34% (from 339 deaths to 223 deaths per 100,000) in
deaths due to complications during pregnancy,
childbirth, and the postnatal period. However, with an
average annual reduction of just under 2.1%, the rate
of progress remains insufficient (Maternal mortality
rates and statistics n.d.). Furthermore, the U.S. has a
mortality rate far outstrips that of the other
industrialized nations, with a rate of 22.3 deaths per
100,000 live births (Hoyert 2024).
Various complications during pregnancy can lead
to the death of the mother. Some common
complications of pregnancy are high blood pressure,
gestational diabetes, infections, miscarriage, and
others. Moreover, women may also suffer
complications after giving birth, such as postpartum
depression (PPD). PPD is a medical condition related
to strong feelings of sadness, anxiety, and tiredness.
It is estimated that in the U.S., between 13.8% and
19.8% of women experience some type of PPD
(Bermúdez Serrano 2024), and of those, 50% are not
diagnosed by a health professional (Postpartum
Depression Statistics | Research and Data On PPD
(2024) 2024). PPD is a factor in 20% of all maternal
deaths (Hagatulah et al. 2024). Therefore, it is crucial
to address this issue to improve maternal health
outcomes. The goal of this research is to identify the
factors that increase women’s risk of developing
postpartum depression.
2 PROBLEM DESCRIPTION
Postpartum depression is often confused with Baby
Blues, but the main difference is the intensity and
duration of the symptoms. During the first two weeks
Terreros-Lozano, M. A., Lopez-Soto, D., Nucamendi-Guillén, S. and López-Ceballos, M. A.
Predicting Postpartum Depression in Maternal Health Using Machine Learning.
DOI: 10.5220/0013155700003893
In Proceedings of the 14th International Conference on Operations Research and Enterprise Systems (ICORES 2025), pages 255-263
ISBN: 978-989-758-732-0; ISSN: 2184-4372
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
255

after childbirth, mothers experience hormonal
changes that can cause anxiety, crying, and
restlessness, and 85% of mothers experience this,
which is expected given the abrupt change in life
having to take care of a newborn; these first two
weeks are known as the baby blues (Baby Blues and
Postpartum Depression 2024). Postpartum depression
usually appears two to eight weeks after giving birth
but can happen up to years. The symptoms to be
aware of include feeling overwhelmed, constant
crying, difficulty bonding with your baby, and
doubting your ability to care for yourself and your
baby (What is postpartum depression? n.d.).
PPD can be experienced in different ways by
different mothers. One of them is postpartum anxiety,
and the symptoms to identify it include far more
anxious behaviors than primarily depressed behavior,
like persistent fears and worries, high tension and
stress, and inability to relax (Postpartum Depression
Types - Pyschosis, OCD, PTSD, Anxiety and Panic
2023). There’s also postpartum obsessive-
compulsive disorder (OCD), which affects 3% to 5%
of new mothers. Symptoms of postpartum OCD
involve intrusive and persistent thoughts, often
centered around harming or even killing the baby
(Postpartum Depression Types - Pyschosis, OCD,
PTSD, Anxiety and Panic 2023). Postpartum panic
disorder occurs in up to 10% of postpartum women;
they experience intense anxiety and recurrent panic
attacks (Postpartum Depression Types - Pyschosis,
OCD, PTSD, Anxiety and Panic 2023). Postpartum
post-traumatic stress disorder (PTSD) takes place in
a mother's life when they experience a traumatic
experience before, during, or shortly after giving
birth; it results in a chronic mental health issue that
creates anxiety or panic-like symptoms. Postpartum
PTSD and PPD can co-occur, creating a complex case
and treatment challenge (Postpartum Depression
Types - Pyschosis, OCD, PTSD, Anxiety and Panic
2023).
Bermudez Serrano (Bermúdez Serrano 2024)
explains that if mothers are not monitored and given
the necessary care, they may develop postpartum
psychosis, which occurs in 1 in 1000 women. The
likelihood of experiencing such episodes is higher in
women who had mental health issues before
pregnancy. Those affected by postpartum psychosis
may experience hallucinations and suicidal or
infanticidal thoughts, making the early detection of
symptoms crucial for prompt treatment.
Although PPD is one of the most important causes
of maternal mortality, it is not the only repercussion.
Untreated PPD appears to have adverse effects on
both infants and mothers. Nonsystematic reviews
suggest that children of untreated depressed mothers,
compared to those of mothers without PPD, face risks
such as poor cognitive development, behavioral
inhibition, emotional issues, violent behavior,
externalizing disorders, and psychiatric and medical
problems during adolescence (Slomian et al. 2019).
Other reviews, both nonsystematic and systematic,
have identified specific maternal risks associated with
untreated PPD, including weight issues, alcohol and
drug use, social relationship difficulties,
breastfeeding challenges, and persistent depression,
compared to women who received treatment
(Slomian et al. 2019).
According to recent studies in the American
Journal of Public Health, the cost of untreated
perinatal mood and anxiety disorder (PMADs) for
2017 is a total of USD 14.2 billion (Health 2020).
This study is intended to support the early diagnosis
of PPD, and therefore, decision-makers can act
proactively and reduce risks to mother and child, as
well as costs.
3 RELATED RESEARCH
Machine learning (ML) techniques have been
effectively employed to forecast the persistence,
chronicity, severity of major depressive disorder, and
response to treatment (Kessler et al. 2016). Various
studies on depression prediction have primarily
utilized supervised ML algorithms: support vector
machines (SVM) and random forests (Jin 2015)
(Natarajan et al. 2017). There was a study that used a
multi-part survey consisting of demographic
questions, known PPD risk factors, and potential
symptoms of PPD. They implemented regression
trees and gradient-boosting methods to answer
whether PPD can be predicted from non-clinical data
and whether ML is viable for PPD prediction. With
the help of ML techniques, they ensure that PPD
occurs in mothers who have a terrible relationship
with their partners or do not receive assistance from
them. They aimed to develop a self-diagnosis tool and
treatment plan for new mothers (Natarajan et al.
2017).
Amit et al. (Amit et al. 2021) also worked on
predicting PPD risk using machine learning applied
to electronic health records (EHR). A gradient tree-
boosting algorithm was used to analyze data from
266,544 women. Their model obtained an accuracy of
0.805, but when combined with the Edinburgh
Postanal Depression Scale (EPDS), it significantly
improved to 0.844.
ICORES 2025 - 14th International Conference on Operations Research and Enterprise Systems
256

There’s also a related study by Bjertrup et al.
(Bjertrup, Væver, and Miskowiak 2023), where an
online neurocognitive risk screening tool was
developed to predict PPD. In their method, they used
emotional reactivity and evaluation of infant distress,
analyzed through statistical models, to predict PPD
risk in pregnant women. The results obtained showed
that negative reactivity to infant distress was a strong
predictor of PPD onset. The study concluded that
neurocognitive bias during pregnancy could serve as
a biomarker for PPD.
Other research has implemented nine different
supervised ML algorithms, including random forest
(RF), stochastic gradient boosting, support vector
machines (SVM), recursive partitioning and
regression trees, naïve Bayes, k-nearest neighbor
(kNN), logistic regression, and neural network, to
evaluate models with only demographic and lifestyle
variables to predict PPD (Shin et al. 2020). They
found that women with PPD were more likely to have
less education and had depression before pregnancy.
Both investigations based their analysis on
demographic data. In this research, we included
health pre-pregnancy, health during pregnancy,
prenatal care, factors giving birth, health postpartum,
use of drugs or smoking before and during pregnancy,
if abused, and information on the infant data.
4 METHODOLOGY
The Pregnancy Risk Assessment Monitoring System
(PRAMS) data set from 2016–2021 from the Centers
for Disease Control and Prevention (CDC) was
analyzed for this study. PRAMS gathers state-
specific, population-based information on maternal
characteristics and experiences in the United States
before, during, and after pregnancy. A sample of
women who recently gave birth to live infants was
chosen from state birth certificate registries, and these
women were invited to participate in the PRAMS
survey (CDC 2024). The PRAMS questionnaire
consists of three sections: a core set of questions used
by all sites, a collection of standardized optional
questions that sites can choose from, and site-specific
questions typically utilized only by the site that
created them (CDC 2024). The PRAMS data from
2016 to 2021 included a total of 221,382 participants.
After cleaning the database (eliminating records with
inconsistencies and missing information), 8,103
records containing complete patient information were
selected.
There were over 500 variables. First, the data was
cleaned by classifying the information into nine
sections: demographics, pre-pregnancy, health during
pregnancy, prenatal care, factors giving birth, health
postpartum, use of drugs or smoking before and
during pregnancy, if abused, and information about
the infant. Then, observations with missing
information were discarded for further analysis to
find the variables that had the strongest relationship
with whether the mother had PPD or not. After doing
this, and with the help of contingency tables, a result
of 42 variables was achieved.
To facilitate practitioners' implementation of this
model, a second selection of variables was developed
using ‘feature importances’, based on the Decision
Tree Classifier algorithm (Matsumura et al. 2025).
This selection aimed to compare the accuracy
achieved after reducing the number of variables. This
evaluates whether the reduction in variables is
justified by an acceptable loss of accuracy in the
model. Fifteen variables were selected, which
resulted in the following.
Both sets of selected variables were assessed
using six classification algorithms: k-Nearest
Neighbor (kNN), classification tree analysis (CTA),
Random Forest (RF), Artificial Neural Network
(ANN), Extreme Gradient Boosting (XGboost),
Extremely Randomized Trees Classifier (Extra Trees
Classifier). Four different sample sizes were used for
each classification algorithm, and ten different
samples were run for each size, thus obtaining the
averages presented in the following section. To
develop and implement these algorithms, reference
the codes published on the website: https://scikit-
learn.org/stable/.
As a result, our database shows that there are
1,134 records with PPD, which corresponds to 14%
of the database, and 6,969 records without it. These
records are independent of each other. There is no
correlation between the results.
All experiments were performed using a PC Intel
Core i7 @2.40 GHz with 16 GB of RAM Memory
under Windows 11 OS.
5 RESULTS
In order to determine whether the number and types
of variables selected affect the performance of the
selected methods, we compared both scenarios: the
one taking 42 variables, which include demographics,
health pre-pregnancy, health during pregnancy,
prenatal care, factors giving birth, health postpartum,
use of drugs or smoking before and during pregnancy,
if abused, and information of the infant data, and the
other considering only the 15 variables selected.
Predicting Postpartum Depression in Maternal Health Using Machine Learning
257

ICORES 2025 - 14th International Conference on Operations Research and Enterprise Systems
258

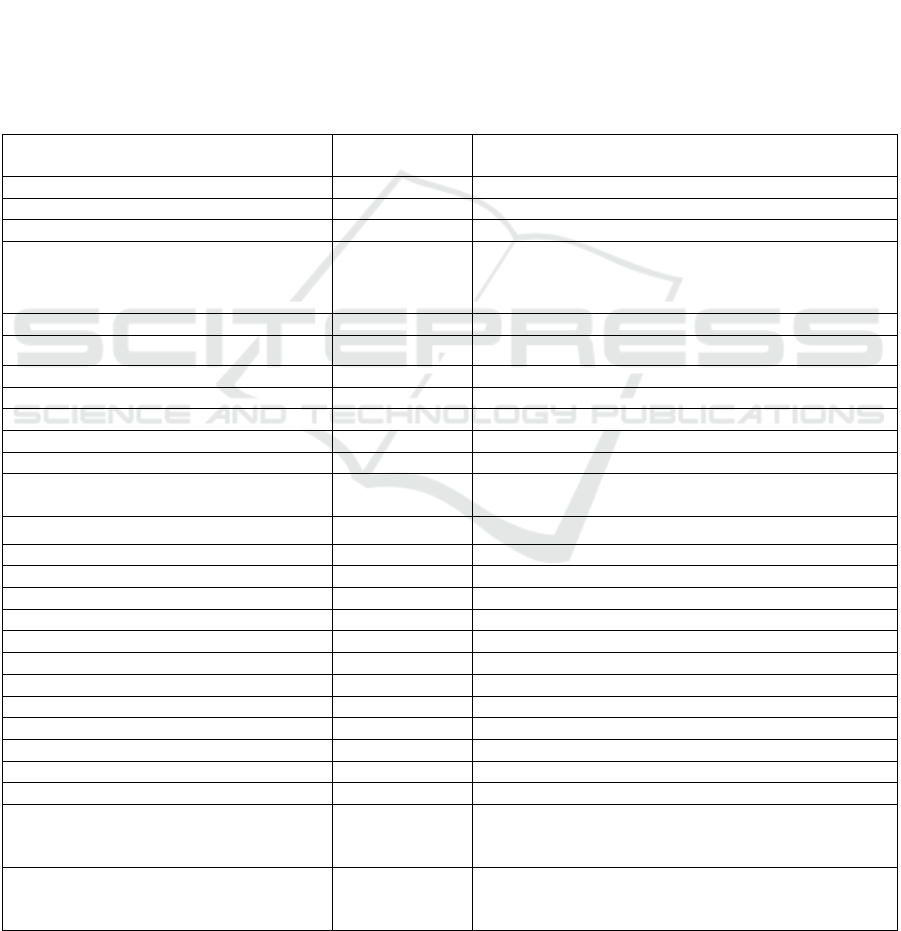
Table 1: Description of the variables selected.
Variable
Scale
Measurement
Levels of measurement
Mothers age Categorical
1= 17-20 YEARS OLD, 2= 21-25 YEARS OLD, 3= 26-30 YEARS
OLD, 4= 31-35 YEARS OLD, 5= 36-40 YEARS OLD, 6= 41-45
YEARS OLD
Mothers’ education level Categorical
0= UNKNOWN, 1=<= 8TH GRADE, 2=9-12 GRADE,NO
DIPLOMA, 3=HIGH SCHOOL GRAD/GED, 4=SOME
COLLEGE, NO DEG/ASSOCIATE DEG,
5=BACHELORS/MASTERS/DOCTORATE/PROF
Mother income Categorical
1 = LOWER CLASS (=<$28,007), 2=LOWER MIDDLE CLASS
($28,008 to $55,000), 3= MIDDLE CLASS ($55,001 to $89,744)
Pregnant intention Categorical
1=LATER, 2=SOONER, 3=THEN
4=DID NOT WANT THEN OR ANY TIME, 5=WAS NOT SURE
No. of previous live births Categorical 0=0, 1=1, 2=2, 3=3-5, 4=6+
No. of previous pregnancy
outcomes
Discrete
quantitative
1, 2, 3, 4, 5, 6, 7
Vitamin intake per week
during pregnancy
Categorical
1=DIDNT TAKE VITAMIN, 2=1-3 TIMES/WEEK, 3=4-6
TIMES/WEEK, 4=EVERY DAY/WEEK
Depression during pregnancy Binary YES = 1, NO = 0
Mom BMI (Body Mass Index) Categorical
1=UNDERWT ( < 18.5), 2=NORMAL (18.5-24.9), 3=OVERWT
(25.0-29.9), 4=OBESE (30.0 + )
Kotelchuck index Categorical
1=INADEQUATE, 2=INTERMEDIATE, 3=ADEQUATE,
4=ADEQUATE PLUS
Attendant at birth Categorical
1=PHYSICIAN (MD), 2=OSTEOPATH (DO), 3=CERT. NURSE
MIDWIFE/CM, 4=OTHER MIDWIFE, 5=OTHER,
6=UNKNOWN
No. of weeks breastfeeding. Categorical
1= 1-5 WEEKS, 2= 6-11 WEEKS, 3= 12-17 WEEKS, 4= 18-23
WEEKS, 5= 24-29 WEEKS, 6= 30-35 WEEKS, 7= 36-40 WEEKS,
8= <1 WEEKS, 9= Didn’t breastfeed
No interest in the baby since
birth
Categorical
1=ALWAYS, 2=OFTEN/ALMOST ALWAYS, 3=SOMETIMES,
4=RARELY, 5=NEVER
Infant age Categorical
0= 0-10 WEEKS, 1= 11-15 WEEKS, 2= 16-20 WEEKS, 3= 21-25
WEEKS, 4= 26-30 WEEKS, 5= 31-35 WEEKS, 6= 35-40 WEEKS
Using birth control
postpartum
Binary YES = 1, NO = 0
Postpartum Depression
Indicator (output variable)
Bernoulli
distribution
YES = 1, NO = 0
Predicting Postpartum Depression in Maternal Health Using Machine Learning
259

Table 2: Obtained results from scenario 1 (42 variables).
Accuracy Precision
Sample Size
Method
10% 15% 20% 30% 10% 15% 20% 30%
kNN 0.8665 0.8469 0.8661 0.8655 0.6772 0.6292 0.5712 0.6061
CTA 0.9411 0.9423 0.9379 0.9399 0.8008 0.7958 0.7921 0.8039
ANN 0.9482 0.9461 0.9481 0.9490 0.8625 0.8517 0.8742 0.8526
XGboost 0.9587 0.9569 0.9558 0.9553 0.9323 0.9490 0.9232 0.9323
RF 0.9657 0.9647 0.9620 0.9616 0.9989 0.9970 0.9970 0.9972
Extra Tree Classifier 0.9639 0.9600 0.9587 0.9597 0.9847 0.9787 0.9821 0.9766
Table 3: Obtained results from scenario 2 (15 variables).
Accuracy Precision
Sample size
Method
10% 15% 20% 30% 10% 15% 20% 30%
kNN 0.8991 0.8949 0.8916 0.8864 0.7543 0.7949 0.7854 0.8075
CTA 0.9429 0.9413 0.9407 0.9440 0.8144 0.7920 0.8055 0.8235
ANN 0.9610 0.9575 0.9560 0.9575 0.9502 0.9346 0.9400 0.9328
XGboost 0.9543 0.9540 0.9582 0.9538 0.9108 0.9097 0.9244 0.9085
RF 0.9629 0.9595 0.9591 0.9601 0.9917 0.9895 0.9931 0.9949
Extra Tree Classifier 0.9571 0.9613 0.9603 0.9623 0.9830 0.9732 0.9831 0.9713
6 RESULTS
In order to determine whether the number and types
of variables selected affect the performance of the
selected methods, we compared both scenarios: the
one taking 42 variables, which include demographics,
health pre-pregnancy, health during pregnancy,
prenatal care, factors giving birth, health postpartum,
use of drugs or smoking before and during pregnancy,
if abused, and information of the infant data, and the
other considering only the 15 variables selected.
We reported the test dataset used to measure the
performance of each method mentioned before. We
considered the accuracy and precision metrics to
evaluate the performance of the selected approaches.
According to Evidently AI Team (Accuracy vs.
precision vs. recall in machine learning n.d.),
accuracy indicates the frequency with which a
classification machine learning model is generally
correct. Precision reflects the rate at which a machine
learning model accurately predicts the target class.
According to the results shown in Table 2, the
highest accuracy was found using Random Forest,
whereas the lowest accuracy was obtained using the
k-Nearest Neighbor with 42 variables (0.9657 and
0.8469, respectively). As for precision, we again got
the highest score using Random Forest and the lowest
using k-Nearest Neighbor with 42 variables (0.9989
and 0.5712, respectively).
On the other hand, we obtained (again) the best
accuracy and precision with random forest (0.9629
and 0.9949, respectively), as seen in Table 3. The
percentages shown in the tables represent the sample
size used in the algorithm after training. These
samples were run ten times to obtain the averages
shown in the table. Both the highest accuracy and
precision were found when a 10% sample size was
used, which indicates that the more training given to
the algorithm, the better the results. It is important to
note that the difference between the best accuracy
obtained from the model with 42 variables and that
from the model with 15 variables is less than 0.3%.
This means we could safely apply the model with 15
variables, which will require less time from
practitioners for follow-up and will not result in any
significant loss of accuracy in predictions.
Based on the chi-squared test of the contingency
tables (including 95% confidence intervals), we
obtained the results of the tendencies of each variable.
Younger mothers, particularly those aged between 18
and 25, are more likely to experience PPD (p-value =
ICORES 2025 - 14th International Conference on Operations Research and Enterprise Systems
260

0.0001). Although the likelihood of depression
decreases as maternal age increases, cases continue to
be observed in mothers up to 45 years of age (p-value:
0.0001).
Educational attainment also plays a crucial role.
Mothers with lower education levels (such as those
with 8th grade or less and 9th-12th grade without a
diploma) are more likely to experience PPD (p-value
= 0.0001). In contrast, higher levels of education are
associated with a lower likelihood of depression (p-
value = 0.0001).
The level of income that each mother has also
represents an association with presenting PPD.
Mothers with lower incomes are more likely to
present PPD (p-value = 0.0001), and mothers with
higher incomes may show it but at a lower percentage
(p-value = 0.0001).
Another significant factor is pregnancy intention.
Mothers who did not want the pregnancy or were
uncertain about it exhibited the highest rates of PPD
(p-value = 0.0001). On the other hand, those who
wished for the pregnancy, whether sooner or at the
time, report lower rates of depression (p-value =
0.0001).
First-time mothers are at a higher risk of PPD,
possibly due to the challenges and adjustments
associated with first-time parenthood (p-value =
0.0333). On the contrary, mothers with more previous
live births (mainly two or more) showed a
significantly lower risk of PPD (p-value = 0.0317).
It seems that mothers with cero previous
pregnancy outcomes are more likely to develop PPD
(p-value = 0.0374), and mothers with one or more
outcomes seem to experience less PPD (p-value =
0.0221). Some outcomes could be spontaneous or
induced losses or ectopic pregnancies. However,
since the groups with more terminations are smaller,
further statistical analysis might be necessary to
confirm these trends.
Mothers who did not take vitamins during
pregnancy are more likely to experience PPD
compared to those who did (p-value = 0.0082).
Regular vitamin intake, particularly daily, is
associated with a lower likelihood of depression,
indicating that prenatal care and nutrition may
contribute positively to postpartum mental health
outcomes (p-value = 0.0085).
For depression during pregnancy, it was presented
that 34.94% of mothers who experience it also report
PPD (p-value = 0.0001), compared to only 8% among
those who did not experience prenatal depression (p-
value = 0.0001). This substantial difference
underlines the importance of addressing mental
health issues during pregnancy to reduce the
likelihood of PPD.
In terms of maternal Body Mass Index (BMI),
underweight mothers (BMI < 18.5) are at the highest
risk of PPD, followed by obese mothers (BMI > 30)
(p-value = 0.0029). While overweight mothers (BMI
25 - 29.9) also show an elevated risk, it is lower than
that of underweight and obese mothers. These
findings suggest that extremes in maternal BMI—
whether too low or too high—can contribute to
postpartum mental health challenges.
The Kotelchuck Index, also known as the
Adequacy of Prenatal Care Utilization (APNCU)
index, measures the adequacy of prenatal care and is
classified into four categories. Inadequate, which is
associated with the highest risk of PPD (16.38%).
Intermediate and adequate, which presented lower
risks of PPD, which suggests that timely and
sufficient prenatal care helps (p-value = 0.0006); the
final category is adequate plus, it presented a
relatively high rate of PPD, indicating that additional
visits may not always equate to better mental health
outcomes (p-value = 0.0006).
The type of healthcare provider attending the
delivery also affects the likelihood of PPD. Mothers
attended by other midwives have the lowest risk of
PPD (3.70%), followed by certified nurse midwives
(10.74%). In contrast, mothers attended by physicians
and osteopaths exhibit the highest likelihood of PPD,
around 14% (p-value = 0.0219).
The amount of time a mother is able to breastfeed
her baby also has an impact on her mental health, with
women who did not breastfeed or breastfeed for a
short time (1-11 weeks) having the highest rates of
PPD (p-value = 0.0001), with more than 20%
experiencing it. Breastfeeding for 12-23 weeks
appears to be associated with the lowest risk of PPD,
with rates between 10-11% (p-value = 0.0001).
Mothers who consistently showed no interest
since birth are at the highest risk for PPD; the fact that
100% of these women were diagnosed with PPD
suggests that the lack of interest is a strong indicator
of postpartum mental health issues (p-value =
0.0001). Even though the mothers who only
experience that lack of interest sometimes have a
lower risk, there is still the presence of PPD.
Regarding the infant’s age, the mothers who
presented the highest rates of PPD were those with
babies aged less than or equal to 10 weeks (p-value =
0.0002); after the risk decreases, the lowest risk seen
in the 26-30 weeks range (p-value = 0.0002). This
suggests that the early postpartum period is the most
critical time for monitoring and addressing PPD.
Predicting Postpartum Depression in Maternal Health Using Machine Learning
261

Finally, the use of birth control postpartum is
associated with a lower likelihood of PPD. Mothers
not using birth control postpartum are more likely to
experience depression, with 16.27% reporting PPD
(p-value = 0.0009). In contrast, those who use birth
control have a lower rate of depression, with only
13.25% affected (p-value = 0.0007).
7 CONCLUSIONS
PPD is an issue that should have more attention in the
U.S. Now that we know the effects that it has on a
mother and child's life, this is why this research has
the goal to help predict this health issue so decision-
makers can make more informed decisions and be
prepared.
This research has demonstrated that the use of
machine learning techniques can be highly effective
in predicting the risk of postpartum depression (PPD)
in new mothers. Through the analysis of an extensive
and diverse dataset provided by PRAMS, significant
variables influencing the likelihood of developing
PPD were identified, including demographic, health-
related, and pregnancy and postpartum factors.
Our results indicate that the Random Forest model
achieved the highest accuracy and precision at 96%
and 99%, respectively, utilizing a comprehensive set
of 42 variables. Between the two models tested, there
is no significant difference in accuracy and precision;
the difference is less than 0.3%. However, selecting
15 variables will make it easier for practitioners to
track them, and it won’t mean a risk.
Implementing machine learning models to predict
PPD risk can significantly impact the improvement of
maternal health by enabling early and personalized
preventive interventions. This approach can
contribute to reducing the economic and social
burden associated with PPD, enhancing the quality of
life for mothers and their families. Future research
could focus on integrating these models into
healthcare systems to maximize their applicability
and effectiveness.
REFERENCES
“Accuracy vs. Precision vs. Recall in Machine Learning:
What’s the Difference?” https://www.evidentlyai.
com/classification-metrics/accuracy-precision-recall
(October 9, 2024).
Amit, Guy, Irena Girshovitz, Karni Marcus, Yiye Zhang,
Jyotishman Pathak, Vered Bar, and Pinchas Akiva.
2021. “Estimation of Postpartum Depression Risk from
Electronic Health Records Using Machine Learning.”
BMC Pregnancy and Childbirth 21(1): 630.
doi:10.1186/s12884-021-04087-8.
“Baby Blues and Postpartum Depression: Mood Disorders
and Pregnancy.” 2024. https://www.hopkinsmedi
cine.org/health/wellness-and-prevention/post partum-
mood-disorders-what-new-moms-need-to-kn ow (June
12, 2024).
Bermúdez Serrano, Mercedes María. 2024. “Relación entre
la depresión postparto y la mala calidad del sueño
durante el embarazo y el postparto.” http://crea.uj
aen.es/jspui/handle/10953.1/23233 (July 16, 2024).
Bjertrup, Anne Juul, Mette Skovgaard Væver, and Kamilla
Woznica Miskowiak. 2023. “Prediction of Postpartum
Depression with an Online Neurocognitive Risk
Screening Tool for Pregnant Women.” European
Neuropsychopharmacology 73: 36–47. doi:10.1016/
j.euroneuro.2023.04.014.
CDC. 2024. “PRAMS Data.” Pregnancy Risk Assessment
Monitoring System (PRAMS). https://www.cdc.gov/
prams/php/data-research/index.html (July 17, 2024).
Hagatulah, Naela, Emma Bränn, Anna Sara Oberg, Unnur
A. Valdimarsdóttir, Qing Shen, and Donghao Lu. 2024.
“Perinatal Depression and Risk of Mortality:
Nationwide, Register Based Study in Sweden.” BMJ
384: e075462. doi:10.1136/bmj-2023-075462.
Health, MGH Center for Women’s Mental. 2020. “New
Study Estimates the Astonishing Cost of Neglected
Perinatal Mood and Anxiety Disorders in US Mothers -
MGH Center for Women’s Mental Health.”
https://womensmentalhealth.org/posts/cost-pmads/,
https://womensmentalhealth.org/posts/cost-pmads/
(July 16, 2024).
Hoyert, Donna L. 2024. “Maternal Mortality Rates in the
United States, 2022.”
Jin, Haomiao. 2015. “Development of a Clinical
Forecasting Model to Predict Comorbid Depression
Among Diabetes Patients and an Application in
Depression Screening Policy Making.” Preventing
Chronic Disease 12. doi:10.5888/pcd12.150047.
Kessler, R. C., H. M. van Loo, K. J. Wardenaar, R. M.
Bossarte, L. A. Brenner, T. Cai, D. D. Ebert, et al. 2016.
“Testing a Machine-Learning Algorithm to Predict the
Persistence and Severity of Major Depressive Disorder
from Baseline Self-Reports.” Molecular Psychiatry
21(10): 1366–71. doi:10.1038/mp.2015.198.
“Maternal Health.” https://www.who.int/health-topics/
maternal-health (July 16, 2024).
“Maternal Mortality Rates and Statistics.” UNICEF DATA.
https://data.unicef.org/topic/maternal-health/ maternal-
mortality/ (July 30, 2024).
Matsumura, Kenta, Kei Hamazaki, Haruka Kasamatsu,
Akiko Tsuchida, and Hidekuni Inadera. 2025.
“Decision Tree Learning for Predicting Chronic
Postpartum Depression in the Japan Environment and
Children’s Study.” Journal of Affective Disorders 369:
643–52. doi:10.1016/j.jad.2024.10.034.
Natarajan, Sriraam, Annu Prabhakar, Nandini Ramanan,
Anna Bagilone, Katie Siek, and Kay Connelly. 2017.
“Boosting for Postpartum Depression Prediction.” In
2017 IEEE/ACM International Conference on
Connected Health: Applications, Systems and
ICORES 2025 - 14th International Conference on Operations Research and Enterprise Systems
262
Engineering Technologies (CHASE), 232–40.
doi:10.1109/CHASE.2017.82.
“Postpartum Depression Statistics | Research and Data On
PPD (2024).” 2024. PostpartumDepression.org.
https://www.postpartumdepression.org/resources/statis
tics/ (July 30, 2024).
“Postpartum Depression Types - Pyschosis, OCD, PTSD,
Anxiety and Panic.” 2023. PostpartumDepression. org.
https://www.postpartumdepression.org/post partum-
depression/types/ (July 31, 2024).
Shin, Dayeon, Kyung Ju Lee, Temidayo Adeluwa, and
Junguk Hur. 2020. “Machine Learning-Based
Predictive Modeling of Postpartum Depression.”
Journal of Clinical Medicine 9(9): 2899. doi:10.3390/
jcm9092899.
Slomian, Justine, Germain Honvo, Patrick Emonts, Jean-
Yves Reginster, and Olivier Bruyère. 2019.
“Consequences of Maternal Postpartum Depression: A
Systematic Review of Maternal and Infant Outcomes.”
Women’s Health 15: 1745506519844 044. doi:10.1177/
1745506519844044.
“What Is Postpartum Depression? | UNICEF Parenting.”
https://www.unicef.org/parenting/mental-health/what-
postpartum-depression (July 16, 2024).
APPENDIX
Table 4 shows the remaining 27 variables considered in the original set of 42 variables for the analysis:
Table 4: Obtained results from scenario 1 (42 variables).
Variable
Scale
Measurement
Levels of measurement
His
p
anic ethnic
g
rou
p
Binar
y
YES = 1, NO = 0
Marital Status Cate
g
orical 1 = MARRIED, 2 = OTHER
Lan
g
ua
g
e Cate
g
orical 1=ENGLISH, 2=SPANISH, 3=CHINESE
Maternal race grouped Categorical
1=WHITE, 2=BLACK, 3=AM INDIAN, 4=AK
NATIVE, 5=ASIAN, 6=HAWAIIAN/OTH PAC
ISLNDR, 7=OTHER/MULTIPLE RACE
High blood pressure before pregnancy Binar
y
YES = 1, NO = 0
Depression before pregnancy Binary YES = 1, NO = 0
Asthma before pregnancy Binary YES = 1, NO = 0
Anxiety before pregnancy Binary YES = 1, NO = 0
Anemia before
p
re
g
nanc
y
Binar
y
YES = 1, NO = 0
Heart
p
roblems before
p
re
g
nanc
y
Binar
y
YES = 1, NO = 0
Infertility treatment Binary YES = 1, NO = 0
Number of prenatal care visits Categorical
1 = 1-10 visits, 2 = 11-20 visits, 3 = 21-30 visits, 4 = 31-
40 visits, 5 = 41-50 visits
Start PNC in 1
st
trimester Binary YES = 1, NO = 0
Mother get WIC food during pregnanc
y
Binary YES = 1, NO = 0
Hi
g
h blood
p
ressure durin
g
p
re
g
nanc
y
Binar
y
YES = 1, NO = 0
Vacuum deliver
y
Binar
y
YES = 1, NO = 0
Infant bein
g
breast-fe
d
Binar
y
YES = 1, NO = 0
Postpartum visits checkup Binary YES = 1, NO = 0
Breastfeed ever Binary YES = 1, NO = 0
Abused by husband during pregnancy Binary YES = 1, NO = 0
Abused b
y
ex-husband durin
g
p
re
g
nanc
y
Binar
y
YES = 1, NO = 0
If drinkin
g
alcohol Binar
y
YES = 1, NO = 0
If smoke three months before pregnancy Binary YES = 1, NO = 0
If smoke last three months of pregnancy Binary YES = 1, NO = 0
If smokes now Binary YES = 1, NO = 0
How often ecig used three months before
pregnant
Categorical
1=MORE THAN ONCE A DAY, 2=ONCE A DAY
3=2-6 DAYS A WEEK, 4=1 DAY A WEEK OR LESS,
5=NOT USE ELECTRONIC VAPOR PRODUCTS
How often ecig use the last three months Categorical
1=MORE THAN ONCE A DAY, 2=ONCE A DAY,
3=2-6 DAYS A WEEK, 4=1 DAY A WEEK OR LESS,
5=NOT USE ELECTRONIC VAPOR PRODUCTS
Predicting Postpartum Depression in Maternal Health Using Machine Learning
263
