
Knowledge Modelling for Automated Risk Assessment of
Cybersecurity and Indirect Patient Harms in Medical Contexts
Samuel M. Senior
1a
, Laura Carmichael
1b
, Steve Taylor
1c
, Mike Surridge
1d
and Xavier Vilalta
2
1
IT Innovation Centre, University of Southampton, Southampton, U.K.
2
Debiotech SA, Lausanne, Switzerland
Keywords: Automated Risk Assessment, Connected Medical Devices and In Vitro Diagnostic Devices, Cybersecurity,
Indirect Patient Harms, Knowledge Modelling.
Abstract: The use of connected medical and in vitro diagnostic devices (CMD&IVD) as part of individual care and self-
care practices is growing. Significant attention is needed to ensure that CMD&IVD remain safe and secure
throughout their lifecycles — as if a cybersecurity incident were to occur involving these devices, it is possible
that in some cases harm may be brought to the person using them. For the effective safety management of
these devices, risk assessment is needed that covers both the cybersecurity and patient safety domains. To this
end, we present knowledge modelling of indirect patient harms (e.g., misdiagnosis, delayed treatment etc.)
resulting from cybersecurity compromises, along with a methodology for encoding these into a previously
developed automated cybersecurity risk assessment tool, to begin to bridge the gap between automated risk
assessment related to cybersecurity and patient safety.
1 INTRODUCTION
It is increasingly common for connected medical
devices and in vitro diagnostic devices (CMD&IVD)
to be used as part of individual care and self-care
practices — e.g., for remote monitoring by clinicians,
for individuals to manage their conditions through
health apps (e.g., National Health Service [NHS]
England, 2023). Special attention is needed to ensure
that CMD&IVD remain safe and secure throughout
their lifecycles — especially given that CMD&IVD
cyberattacks “may put at severe risk the health and
safety of patients” (Biasin & Kamenjasevic, 2022).
To understand potential harms to patients from
such devices, risk management is necessitated,
particularly at patient safety, cybersecurity, and
privacy and data protection levels, so that the risks of
cybersecurity incidents can be understood in terms of
the potential patient harms that may result. In other
words, there is a need for cybersecurity risk
assessment for CMD&IVD to “explicitly consider the
health care outcomes, systems and processes for
a
https://orcid.org/0000-0002-3428-9215
b
https://orcid.org/0000-0001-9391-1310
c
https://orcid.org/0000-0002-9937-1762
d
https://orcid.org/0000-0003-1485-7024
which that information is used” (Piggin, 2017).
Additionally, risk-benefit analysis is also of
importance as tensions between the level of
cybersecurity controls on a device and its treatment
or diagnostic effectiveness may need to be
considered. As highlighted in the Medical Device Co-
ordination Group (MDCG, 2019) guidance on
cybersecurity where issues may be caused by “weak
security” — referring to security measures that are
inadequate in the given circumstances — and
“restrictive security” — relating to those security
measures that offer “a high level of protection may
have a safety impact”.
This paper describes knowledge extensions to an
existing knowledge-based expert system and
automated risk simulator of cyber-physical systems
called Spyderisk (Phillips et al., 2024) that follows
ISO/IEC 27005: 2022 “Information security,
cybersecurity and privacy — Guidance on manging
information security risks” (ISO, 2022) and ISO/IEC
27000: 2018 “Information technology — Security
Senior, S. M., Carmichael, L., Taylor, S., Surridge, M. and Vilalta, X.
Knowledge Modelling for Automated Risk Assessment of Cybersecurity and Indirect Patient Harms in Medical Contexts.
DOI: 10.5220/0013166900003899
In Proceedings of the 11th International Conference on Information Systems Security and Privacy (ICISSP 2025) - Volume 1, pages 263-274
ISBN: 978-989-758-735-1; ISSN: 2184-4356
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
263
techniques — Information security management
systems — Overview and vocabulary” (ISO, 2018).
The Knowledge Base of this expert system
contains pre-existing information about threats and
risks related to cyber-physical systems. As part of our
recent work for the Horizon Europe NEMECYS
project, we have begun to explore how this
Knowledge Base can be extended for use in the
specific domain of cybersecurity for CMD&IVD
systems so that automated risk assessment can be
performed for it. For example, ISO/TR 24971: 2020
(ISO, 2020) provides guidance on risk assessment for
medical devices and so starts to bridge this gap
between the relationship between domain-specific
risk management for medical devices with risk
management for cybersecurity.
The core extension to Spyderisk described in this
paper is domain model extensions corresponding to
indirect patient harms resulting from
cybersecurity compromises. For the purposes of this
paper, indirect patient harms are described as harms
that arise “as a consequence of the medical decision
or action taken/not taken on the basis of information
or result(s) provided by a device” (MDCG, 2023).
Indirect patient harms resulting from cybersecurity
compromises are translated into the terminology and
structure of this Knowledge Base, and mapped to
cybersecurity risks and threats already present within
it. Then, this new information and mapping is
encoded into the Knowledge Base, thus starting to
bridge and link between the domains of cybersecurity
and indirect patient harms for the automated risk
assessment and management of CMD&IVD. An
illustrative workflow guiding the extensions to our
tool for treatment-based indirect patient harms is
given. An equivalent workflow for diagnosis-based
indirect patient harms can also be formed through
following the same methodology, and both have been
successfully implemented in our tool (Spyderisk,
2024). Our work is driven by four use cases, focusing
on different types of connected medical and IVD
devices (NEMECYS, 2023).
2 BACKGROUND AND RISK
MANAGEMENT CONTEXT
ISO 27000 (ISO, 2022) and ISO 27005 (ISO, 2018)
have guided the development of the Spyderisk risk
modelling approach and continue to do so for the
extensions outlined here. In this section, we provide
an overview of how cybersecurity risk concepts from
these two standards have been interpreted for the
Spyderisk. We then outline our approach to extending
its Knowledge Base with domain-specific
information for the cybersecurity of CMD&IVD.
2.1 Risk Assessment Schema
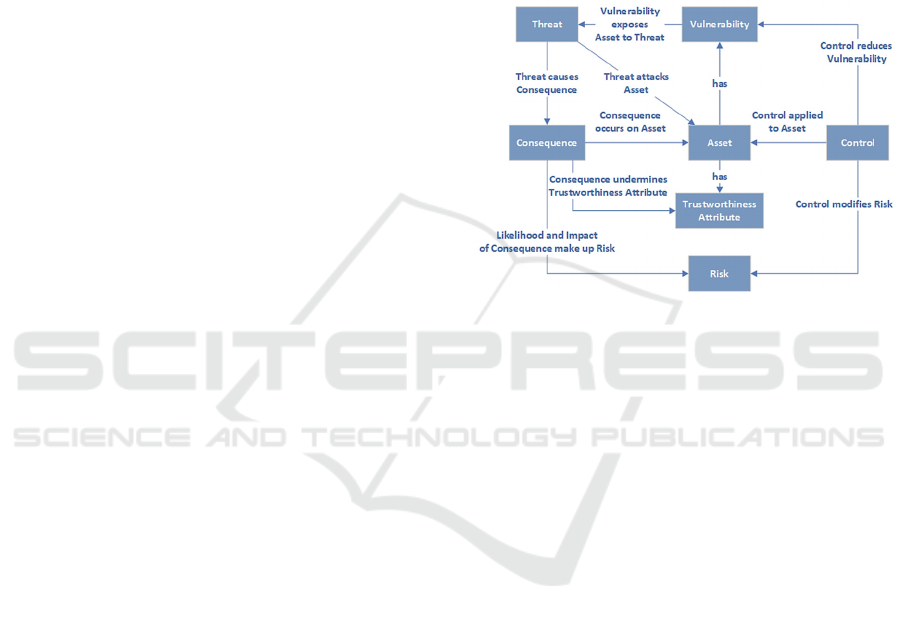
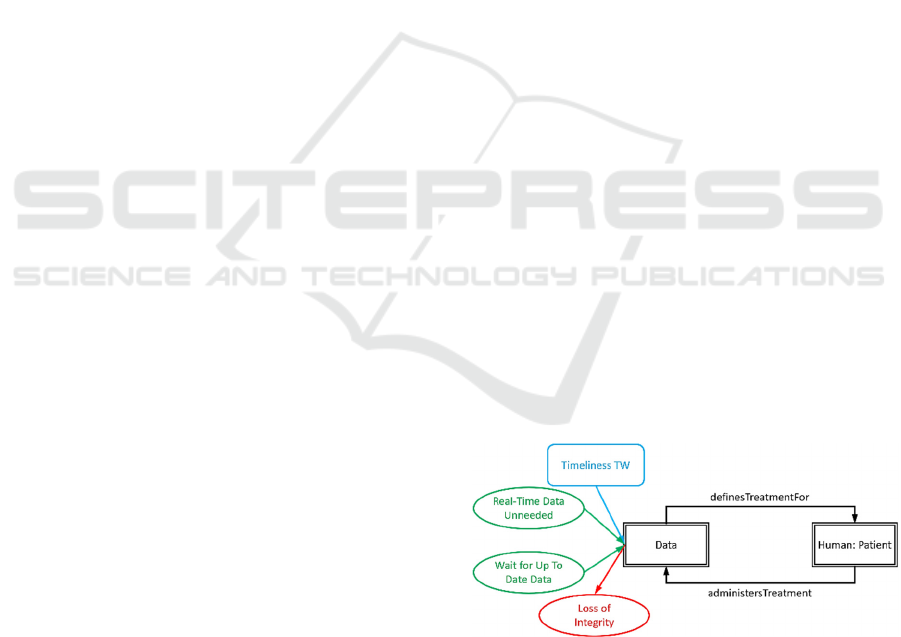
Figure 1 shows a risk assessment schema derived
from ISO 27000 (IS0, 2018) and adapted for the
trustworthiness-based approach of Spyderisk. It
shows relationships between the different elements
involved in ISO 27000-based risk assessment.
Figure 1: Risk assessment schema. Adapted from (Taylor,
2024).
Here, assets are entities of value within the modelled
system and can have vulnerabilities, which enable
threats. A successful threat acts on an asset to cause
a consequence, which is typically adverse. Risk is
the impact of a consequence combined with the
likelihood of the causing threat. Controls modify risk
by modifying the likelihood of the threat through
mitigative or preventative means. Trustworthiness
Attributes (TWAs) “model the expected behaviour
of an Asset, are (generally) desirable properties and
are closely related to the Consequences: each
Trustworthiness Attribute is undermined by a
Consequence.” (Phillips et al., 2024).
Spyderisk contains a Knowledge Base of Assets,
Consequences, TWAs, Controls and Threats for
cybersecurity and cyber-physical systems. The Asset
types include data, IT hosts, software processes,
networks, stakeholders, and physical spaces, amongst
others. TWAs include cybersecurity concepts like
confidentiality, integrity, and availability for data
assets, reliability for software processes and privacy
for humans. Consequences include (typically)
adverse behaviours affecting assets and also the
undermining of TWAs at assets, such as “loss of
confidentiality” on a data asset. Consequences in turn
can cause other threats.
ICISSP 2025 - 11th International Conference on Information Systems Security and Privacy
264
The operator of the Spyderisk creates a “System
Model” containing a configuration of assets and
relationships describing the system to evaluate, and
the Knowledge Base automatically determines the
threats and risks present, along with their likelihood.
2.2 Domain Modelling
The knowledge extensions to Spyderisk follow a
process known as domain modelling, which involves
the capture and encoding of knowledge relevant to
risk assessment for a given domain to integrate it with
the existing knowledge and thus to extend it. Here, an
essential part of domain modelling is to acquire
knowledge relevant to the cybersecurity of
CMD&IVD — such as, by working together with
cross-domain experts as part of project use cases and
examining existing requirements and best practice
related to risk assessment for CMD&IVD with
principal focus on the EU regulatory framework. For
instance, Annexes 1 of the Medical Device
Regulation (MDR) (Regulation 2017/745) and the In
Vitro Diagnostic Devices Regulation (IVDR)
(Regulation 2017/746) contain cybersecurity
requirements for CMD&IVD, and the MDCG
provides guidance on the cybersecurity for medical
devices (2019). Further, international standards on
risk management for medical devices are also used to
guide the developments — i.e., ISO 14971:2019
“Medical devices — Application of risk management
to medical devices” (ISO, 2019) “specifies
terminology, principles and a process for risk
management of medical devices, including software
as a medical device and in vitro diagnostic medical
devices” (ISO, 2019); and ISO 24971 (ISO, 2020) as
previously mentioned. A brief overview of the
domain modelling process is now described.
In the Knowledge Base, threats are modelled
using: (i) Matching Patterns and (ii) Threat
Patterns. “Broadly, a Matching Pattern describes a
set of connected Assets to be looked for in the System
Model: particular Asset types connected by specific
Relation types” (Phillips et al., 2024). “Threat
Patterns are matching parts of the System Model
where there could be an unwanted incident (of any
kind) […] [and] describes how the Nodes in the
pattern relate to its causes” (Phillips et al., 2024).
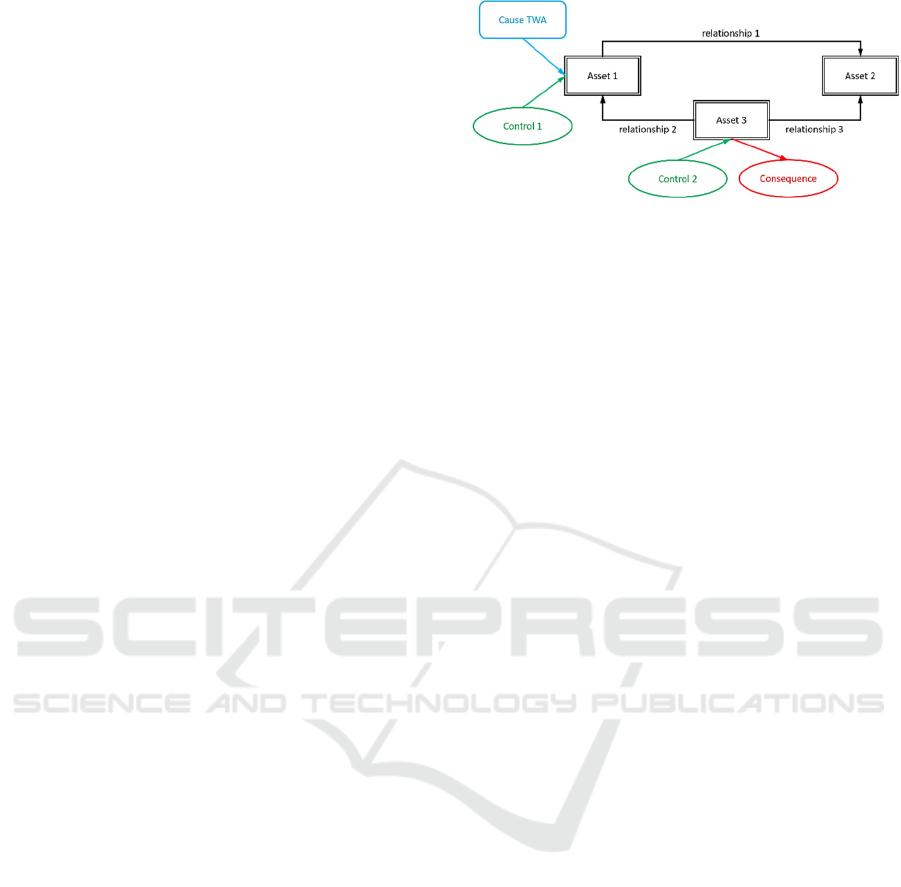
An example threat pattern is given in Figure 2. It
is based on a matching pattern with an additional
cause TWA that enables the threat (blue rounded
rectangle), two controls that block the threat (green
ovals), and a consequence that results from the threat
being successful (red oval).
Figure 2: Example threat pattern.
3 MODELLING INDIRECT
PATIENT HARMS AS RISKS
Indirect patient harms resulting from cybersecurity
compromises of CMD&IVD can occur due to one or
more cybersecurity-related incidents causing errors in
diagnosis and / or treatment. This work utilises types
of indirect harm determined by the MDCG, namely
“absence of diagnosis”, “delayed diagnosis”,
“misdiagnosis”, “absence of treatment”, “delayed
treatment”, and “inappropriate treatment” (MDCG,
2023). These are modelled as Consequences of
Threats that are adverse behaviours affecting
patients (considered as “Assets” in ISO 27000
nomenclature).
Typical treatment and diagnosis processes
utilising CMD&IVD have been used to derive patient
harm-related Consequences and how different
cybersecurity incidents lead to them. For this, four
key types of purpose for CMD&IVD devices are
outlined and explored. Additionally, a generic
workflow based on these is presented, which provides
a high-level illustrative view of how sensor data
generated via these devices, and the resulting
examination results they provide, are used to inform
treatment decisions actions taken / not taken. This is
then used to map elements of the workflow phases to
elements of the Knowledge Base so that cybersecurity
threats at the different stages can be considered in
how they result in indirect patient harms.
The domain modelling activities here have been
driven by the discussed standards as well as use cases
involving consultation with domain experts and
practitioners, with one such use case used as an
illustrative example in Section 6.
3.1 Purpose of Use of Medical Devices
A wide variety of decisions are made by individuals,
patients, and clinicians (decision-makers) as part of
individual care and self-care — some of which may
Knowledge Modelling for Automated Risk Assessment of Cybersecurity and Indirect Patient Harms in Medical Contexts
265

be informed by data generated and collected via
assorted types of CMD&IVD. A CMD or IVD device
will have an “intended purpose” — i.e., “the use for
which a device is intended according to the data
supplied by the manufacturer on the label, in the
instructions for use or in promotional or sales
materials or statements and as specified by the
manufacturer in the clinical evaluation”, as defined
in Article 2(12) of the MDR (Regulation 2017/745).
Types of “specific medical purposes” for medical
devices are outlined by Article 2(1) of the MDR as
follows:
• “[…] diagnosis, prevention, monitoring,
prediction, prognosis, treatment or
alleviation of disease,
• diagnosis, monitoring, treatment,
alleviation of, or compensation for, an
injury or disability,
• investigation, replacement or modification
of the anatomy or of a physiological or
pathological process or state,
• providing information by means of in vitro
examination of specimens derived from the
human body, including organ, blood and
tissue donations […]”
In this work, the focus is on the specific purposes
for medical devices that align with the key types of
intended purposes for CMD&IVD as identified
through the use cases. In particular, how medical
devices may be used for the following purposes:
• Diagnosis — some MDCG-based indirect
harms (MDCG, 2023) explicitly concern
diagnosis (e.g., ‘delayed diagnosis’,
‘misdiagnosis’).
• Treatment — some MDCG-based indirect
harms (MDCG, 2023) regard treatment (e.g.,
‘absence of treatment’, ‘delayed treatment’,
‘inappropriate treatment’).
• Monitoring — CMD&IVD can be used for
the purpose of monitoring.
• Providing information by means of in vitro
examination of specimens derived from the
human body — as there are instances of
CMD&IVD being used for the purpose of
providing such information.
How these four key types of purpose are modelled
is given in Section 4.
3.2 Generic Workflow: Monitoring and
Treatment for non-Emergency
Individual Care and Self-Care
Diagnosis, monitoring, treatment and providing IVD
information are complex activities. For instance,
diagnosis has been described as “a complex, patient-
centered, collaborative activity that involves
information gathering and clinical reasoning with the
goal of determining a patient's health problem. This
process occurs over time, within the context of a
larger health care work system that influences the
diagnostic process” (Balogh et. al., 2015). The aim
here is to identify key aspects and abstractions that
are required for understanding the risks in these
processes to enable their risk modelling and
simulation. This is important as medical devices may
be used as part of distinct clinical workflows and at
different stages of a care pathway. For instance, what
data is being collected, gathered or generated by the
CMD&IVD, and for what use, needs to be
considered. Each stage of the workflow represents
data, a process, or a consequence — concepts used
within our Knowledge Base.
The generic workflow is presented in Figure 3 and
focuses on CMD&IVD used for the purpose of
monitoring and treatment as part of individual care
(e.g., “intended for use by clinicians at point-of-
care” (ISO, 2020) or self-care (e.g., intended to be
used by individuals). It should be noted the IVDR
makes a distinction between IVD medical devices
used for “self-testing”, “near-patient testing”, and
testing inside a “laboratory environment”, see
Article 2(5) and (6) of the IVDR (Regulation
2017/746).
The workflow is organised into phases containing
processes, which are operations performing an
activity; data, which are generated by the processes
and link one process with another; and consequences,
which result from incidents occurring at the data and
processes. It illustrates how different types of sensor
data are generated, interpreted, and acted on for the
monitoring and treatment as part of non-emergency
individual care and self-care practices when those
decision-making processes rely on high quality
examination results derived from data generated and
collected via CMD&IVD.
This workflow is based on the specific medical
purposes for medical devices as well as our
interpretation of the informative guidance for in vitro
diagnostic medical devices given by Annex H of
ISO/TR 24971 (ISO, 2020) and the diagnostic
process outlined by the Committee on Diagnostic
Error in Health Care (Balogh, 2015).
ICISSP 2025 - 11th International Conference on Information Systems Security and Privacy
266
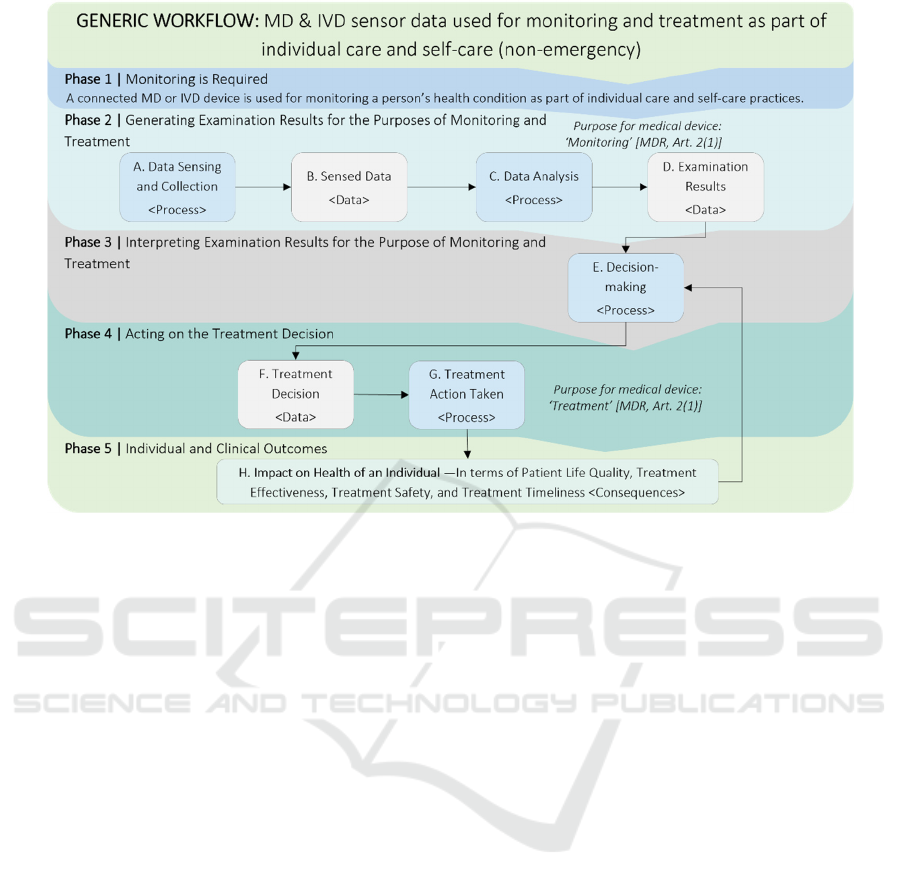
Figure 3: Generic workflow: MD & IVD used for monitoring and treatment in non-emergency individual care and self-care.
The different workflow phases are discussed below.
As assumption-making is a key aspect of threat
modelling since such underlying assumptions are
used to “postulate system properties of relevance, the
implications of which are relied upon during threat
documentation, prioritization and mitigation” (Van
Landuyt and Joosen, 2022), key domain modelling
assumptions are also described below.
3.3.1 Phase 1: Monitoring Is Required
This phase establishes an individual is undergoing
care or self-care where CMD&IVD are used to
monitor their condition. The workflow is initiated
where a CMD&IVD is used for monitoring a person’s
health condition, that requires ongoing treatment, as
part of individual care and/or self-care practices.
It is assumed this workflow concerns situations
where an individual has already received a diagnosis.
Further, to consider the indirect patient harms rather
than direct patient harms, non-emergency situations
are specifically concentrated on, where on-going
monitoring and treatment of a health condition may
be happening e.g., remotely, within a clinical context.
3.3.2 Phase 2: Generating Examination
Results
This phase of the workflow uses the sensors of the
CMD&IVD to generate the monitoring data that are
then processed to generate the Examination Results
Data. This follows three of the key purposes for
medical devices given in Article 2(1) of the MDR
(Regulation 2017 745), which are for “monitoring”
and “treatment” of “disease”, “an injury or
disability” as well as “providing information by
means of in vitro examination”.
It is assumed Examination Results Data are
derived from Sensed Data and used for monitoring
and treatment by clinicians and patients, and is crucial
to monitoring a health condition and making
necessary treatment decisions. The processes and data
for this phase of the workflow are:
• A. Data Sensing and Collection
<Process>. Data is sensed by an MD or IVD
medical device. (Other metadata may also be
collected here, such as time-stamp data.)
• B. Sensed Data <Data>. The sensed raw
data are an input to the data analysis process.
• C. Data Analysis <Process>. Raw data is
transformed into “meaningful, actionable
knowledge” (ISO, n.d.) data (i.e.,
Examination Results).
• D. Examination Results <Data>. Output
Examination Results provide meaningful,
actionable knowledge, interpreted and used
as an input to the decision-making process.
Knowledge Modelling for Automated Risk Assessment of Cybersecurity and Indirect Patient Harms in Medical Contexts
267

Cybersecurity incidents arising in any of the data or
processes at this phase impact the decision-making
process of the next phase, by either causing incorrect
input into it or causing a lack of input to it.
3.3.3 Phase 3: Interpreting Examination
Results
In the third phase, Examination Results are processed
and interpreted so appropriate treatment decisions can
be made by the individual or clinician.
It is assumed Examination Results are not
communicated to another medical device that
immediately administer treatment (ISO, 2020) and
instead, in Phase 4, one or more persons review the
Examination Results data before deciding whether to
act on it. Additionally, the Examination Results data
is viewed as a critical input to the decision-making
process. The process for this phase is:
• E. Decision-Making <Process>. Examina-
tion Results are processed and interpreted to
inform patient / clinician treatment decisions.
Cybersecurity incidents arising at this decision-
making process cause the output of it to either be
incorrect or absent. Additionally, incidents in the
prior phase can also result in this.
3.3.4 Phase 4: Acting on Treatment Decision
In Phase 4, treatment decisions are made and actions
taken. Treatment actions are taken as part of wider
individual care and / or self-care practices and will
contribute to realising “the best possible outcomes for
the individual” (Mukoro, 2011). The process and data
for this are:
• F. Treatment Decision <Data>. As an
output of the decision-making process, a
treatment decision is made.
• G. Treatment Action Taken <Process>.
Treatment decision is acted on by the patient
and/or clinician(s) responsible for their care.
For both the data and process of this phase, if
there are cybersecurity incidents then the actions
taken will either be incorrect or absent, impacting the
final phase by causing indirect patient harms.
3.3.5 Phase 5: Individual and Clinical
Outcomes
In this final phase, the effectiveness of the treatment
actions is evaluated in terms of the impact on the
health of the individual. This phase of the workflow
impacts patient harm consequences relating to the
outcomes of their treatment actions, described by:
• H. Impact on the Health of an Individual
<Consequences>. Patient harm consequen-
ces related to a lack treatment or lack of
necessary treatment. These result from
cybersecurity-related incidents in the prior
phases.
In summary, patient harm consequences that have
been identified. The next section describes how these
are caused by cybersecurity threats.
4 MAPPING CYBERSECURITY
CAUSES TO INDIRECT
PATIENT HARMS
To link cybersecurity threats to the non-emergency
indirect patient harms, the workflow is used to make
connections with pre-existing information about
threats and risks related to cyber-physical systems in
the Knowledge Base. The focus is about how the
security risk factors related to the generic workflow
can be mapped to indirect patient harms. The
workflow is concerned with processes, data, and
consequences that are indirect patient harms resulting
from threats. This process-data-consequence
approach can be represented as a threat-consequence
state mapping diagram, shown and described below.
4.1 Threat-Consequence State
Mapping Diagram
Threat-consequence state mapping diagrams are
concerned with the consequences of prior threats
leading to further threats and further consequences.
One such diagram is given in Figure 3. They contain
controls and threats that are connected together to
show how chains of these form, leading from one to
the next. A Black Box is a type of Threat, a Red
Oval a type of Consequence, a Green Oval a type of
Control, a Red Arrow indicates a type of Threat
enabled by a Control, and a Green Arrow indicates
a type of Threat blocked by a Control. For the
threat-consequence diagram here, the Consequences,
Controls and Threats are grouped together between
black dashed lines. These groups are based on the
Assets at which the Consequences, Controls and
Threats occur.
Figure 4 maps security risk factors (including pre-
existing cybersecurity knowledge in the Knowledge
Base) associated with the generic workflow.
ICISSP 2025 - 11th International Conference on Information Systems Security and Privacy
268
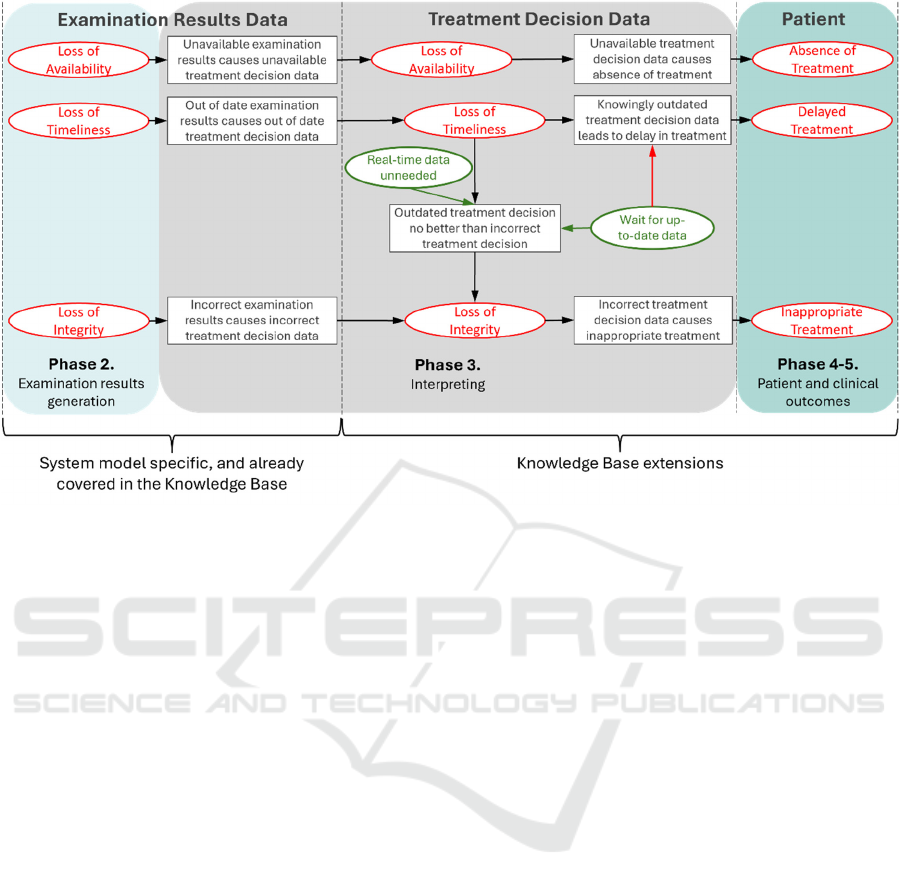
Figure 4: Threat-consequence mapping – Sensor data leading to undermined treatment.
The phases of the workflow are highlighted in the
diagram to show which phases of the workflow the
different consequences and threats occur in. The
processes of the workflow diagram are not explicitly
shown, but their actions are implicitly contained
within the threats. This then covers the indirect
patient harms that occur due to harmful medical
decisions for ongoing treatment.
4.2 Risk Modelling for Generic
Workflow
In Figure 4, the consequences in Phase 2 act on the
Examination Results Data, as an undermining of its
TWAs due to prior threats leading into the workflow.
The threats in Phase 3 represent flaws occurring in the
treatment decision-making process, resulting from
cybersecurity-related consequences and lead to
patient harm consequences in Phases 4-5 that affect
the patient. A key assumption is that the worst-case
scenarios are considered (Piggin, 2017).
Following through the diagram (Figure 4):
• If the Examination Results Data becomes
corrupted (loss of integrity) then through
the treatment decision-making processes
using this corrupted data the treatment
decision data will be corrupted and the
patient will receive an inappropriate
treatment.
• If the Examination Results Data becomes
unavailable (loss of availability) then there
is no input to the treatment decision-making
process so treatment cannot occur and
Treatment Decision Data will be
unavailable, leading to an absence of
treatment.
• If the Treatment Decision Data is out of
date and near real-time treatment
decision data is needed then the outdated
data is no better than being incorrect, leading
to a loss of integrity of the Treatment
Decision Data. If the Treatment Decision
Data does not need to be near real-time then
this threat path can be blocked with a control
specifying that. Additionally, if the data
does need to be up to date then it can be
blocked with a control specifying the
decision-making process will wait for up to
date data. Waiting for the data to be up-to-
data again, however, enables a threat
resulting in delayed treatment.
With the state mapping diagram defined, the
Threats, Controls, Consequences, and paths between
them can be encoded into the Knowledge Base. This
is discussed in the next section.
Knowledge Modelling for Automated Risk Assessment of Cybersecurity and Indirect Patient Harms in Medical Contexts
269
5 ENCODING DOMAIN
MODELLING EXTENSIONS
Three key types of domain modelling extensions have
been undertaken: (i) a review of existing Asset types
to determine what already exists in the domain model
that can be used towards modelling indirect patient
harms; (ii) new relationships between Assets have
been encoded; as have (iii) new matching patterns.
5.1 Use of Existing Asset Types
Some of the key assets identified for socio-technical
CMD&IVD sensor-based systems already exist in the
Knowledge Base and so can be modelled using these
existing Asset types. These are the Clinician being
modelled as the Adult asset type, the Individual /
Patient as a Human, Adult or Child, the CMD&IVD
Sensor as an IoT Sensor, the Data Sensing and
Collection process, Data Testing process as a Process
or Interactive Process, the Decision-making process
as an Interactive Process, and the Diagnostic
Decision, Examination Results, Treatment Decision
and Sensed Data as Health Data asset type.
5.2 New Relationships
To model the identified four key purposes of
CMD&IVD, new Relationship types between Assets
in the Knowledge Base are encoded for diagnosis and
treatment. Indicating a type of action from one asset
type to another, the new relationship types identified
and encoded are:
• administersTreatment: Relation between a
Human and Data indicating the Human is
administering treatment specified by Data.
• diagnoses: Relation between two Humans to
indicate one Human is a Clinician
diagnosing the other, who must be a Patient.
• diagnosisFor: Relation to indicate that
Health Data relating to a Patient is the
diagnosis, as determined by the Clinician.
• senses: Relation between a data asset and a
sensor, indicating the data is sensed output
of the sensor. This was pre-existing but not
user-assertable, and this has been changed.
• treats: Relation between two Humans
indicating one is a Clinician treating the
other, who must be a Patient.
• definesTreatmentFor: Relation to indicate
Health Data relating to a Patient is the
treatment instructions for them, which can
be carried out by the Clinician or Patient.
Monitoring is already covered in the Knowledge
Base so no new relationship need to be encoded for it.
5.3 New Matching and Threat Patterns
New types of Matching Pattern were encoded so that
the following sets of connected Assets and
Relationships can be found in modelled systems:
1. A clinician diagnosing a patient, as determined
through a Clinician-diagnoses-Patient
relationship in a wider matching pattern to
indicate the clinician creates and interacts with
the diagnosis data that is the patient diagnosis.
2. A clinician treating a patient, as determined
through a Clinician-treats-Patient relationship in
a wider matching pattern to indicate the clinician
creates and uses the treatment instructions data,
which forms the patient treatment actions.
3. A patient treating themselves via self-care
practices, as determined through a Data-
definesTreatmentFor-Patient relationship in a
wider matching pattern to indicate the patient is
interacting with an interactive application to
view and act on the treatment instructions data.
4. A sensor sensing user-asserted data, determined
through a Sensor-senses-Data relationship.
New Threat Patterns have been specified, which
are based on the first three Matching Patterns. These
encode the threats and their consequences identified
in the threat-consequence state mapping diagram.
One such threat pattern is given in Figure 5, where
timeliness of data being undermined results in a “loss
of integrity”, unless one of the two controls is active.
Figure 5: Threat pattern linking loss of timeliness to loss of
integrity.
Here the Data (treatment decision data) becomes
out of date (timeliness trustworthiness), causing a loss
of integrity of the Data, due to the starting assumption
that near real-time data is needed for the individual to
ICISSP 2025 - 11th International Conference on Information Systems Security and Privacy
270
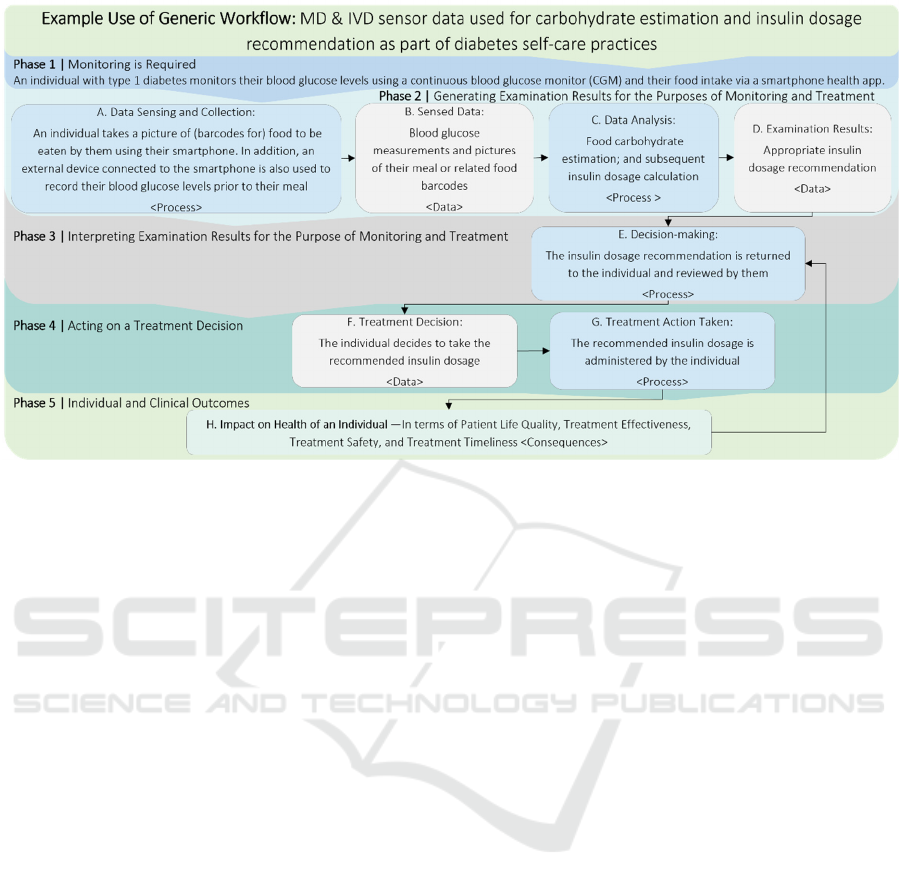
Figure 6: Use of Workflow: Use case example — IVD sensor data used for food calorie estimation and insulin dosage
recommendation in diabetes self-care practices.
correctly treat themselves. There are two controls that
block this threat from occurring. Firstly, it can be
asserted that near real-time data is not needed, and
secondly, the patient can wait for up-to-date data
before taking the treatment actions defined by it.
With the patient harms encoded, an illustrative
example is given next.
6 ILLUSTRATIVE EXAMPLE
Worked use cases with clinical and industrial
partners, as part of the NEMECYS project, have
guided the development of the indirect patient harms-
related extensions. Here one such use case is used as
an illustrative example for our approach. This
scenario was chosen as it builds on the examples in
Annex H of ISO/TR 24971 (pp. 62-85) (ISO 2020).
For this, the generic workflow of Figure 3 has
been specialised to illustrate the workflow and patient
harm domain modelling applied to the sensor data
being used in the self-care management of diabetes.
This specialised workflow is shown in Figure 6 and
describes a scenario where an individual with type 1
diabetes regularly monitors their blood glucose levels
and food intake to help manage their condition. The
individual monitors both their blood glucose levels
prior to a meal through using a continuous blood
glucose monitor (CGM) and their food intake by
taking pictures of their meal or the barcodes of the
food, that are then analysed in the cloud. This data is
collected via a “Software as a Medical Device”
(SaMD) app and uploaded to the cloud where food
carbohydrate levels are estimated and, with this and
the initial blood glucose levels, an appropriate insulin
dosage is calculated for the individual and their given
meal. This is communicated back to the individual so
they can administer the recommended insulin dosage.
The system model shown in Figure 7 models this
use case and focuses on the cybersecurity threats
involved in the data sensing, collection, processing
and communication, which then link to the newly
included indirect patient harms. There are two types
of sensed data within this use case: the pictures taken
by the individual of their food / barcodes; and their
initial blood glucose measurements. Within the
system model, these two data elements are given as a
single Data asset that achieves the same results.
The use case workflow above has steps identified
by letters A-H. Steps A-F (up to the treatment
decision) are covered within the system model:
• Health Sensor (A) senses User Phone Data
(B), which encapsulates both the blood
glucose data and food images / barcodes.
• User Phone Data (B) is stored locally on the
individual’s smartphone and also uploaded
to the cloud (C)
• In the cloud, User Phone Data is used to
update User Cloud Data (D).
Knowledge Modelling for Automated Risk Assessment of Cybersecurity and Indirect Patient Harms in Medical Contexts
271
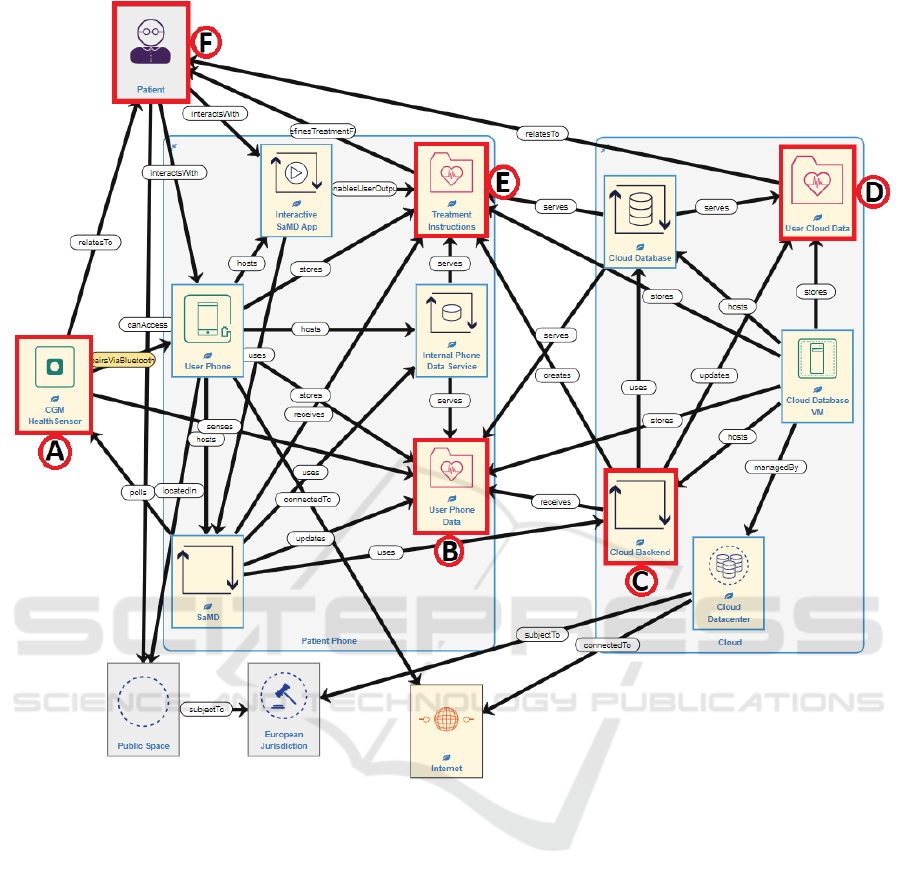
Figure 7: System model for self-managed type 1 diabetes use case.
• These are used to calculate the Treatment
Instructions Data (E), which is transmitted
back to the individual’s smartphone.
• The individual views Treatment Instructions
via the smartphone Interactive SaMD App
and actions the Treatment Instructions (F).
Figure 8 shows the risks present. Each row
corresponds to a risk, which is a Consequence
occurring at an Asset, with associated Impact and
Likelihood. To manage typical cybersecurity risks
like Loss of Confidentiality of the health data assets,
typical cybersecurity controls have been applied, like
the different health data assets being encrypted and
transmitted securely between the smartphone and
cloud. This reduces most risks to a medium risk level
or lower. However, Inappropriate Treatment of the
Patient and Loss of Authenticity of the User Phone
Data are still High risks.
Spyderisk is then used to trace between
Consequences and Threats to work backwards to the
Root Cause Threat. A Root Cause Threat is the very
first threat in a Threat Path, enabling the path to occur.
The root cause to Inappropriate Treatment of the
Patient and Loss of Authenticity of the User Phone
Data is that if the Health Sensor is spoofed when
paired with the patient smartphone, particularly if
pairing occurs in the Public Space, then the
“imposter” Health Sensor will have a Loss of
Authenticity and report incorrect blood glucose
levels to the SaMD. This leads to a Loss of
Reliability in that process, propagating to a Loss of
Reliability in the Cloud Backend, a Loss of
Authenticity in the User Cloud Data, and a Loss of
Authenticity and Integrity in the Treatment
ICISSP 2025 - 11th International Conference on Information Systems Security and Privacy
272
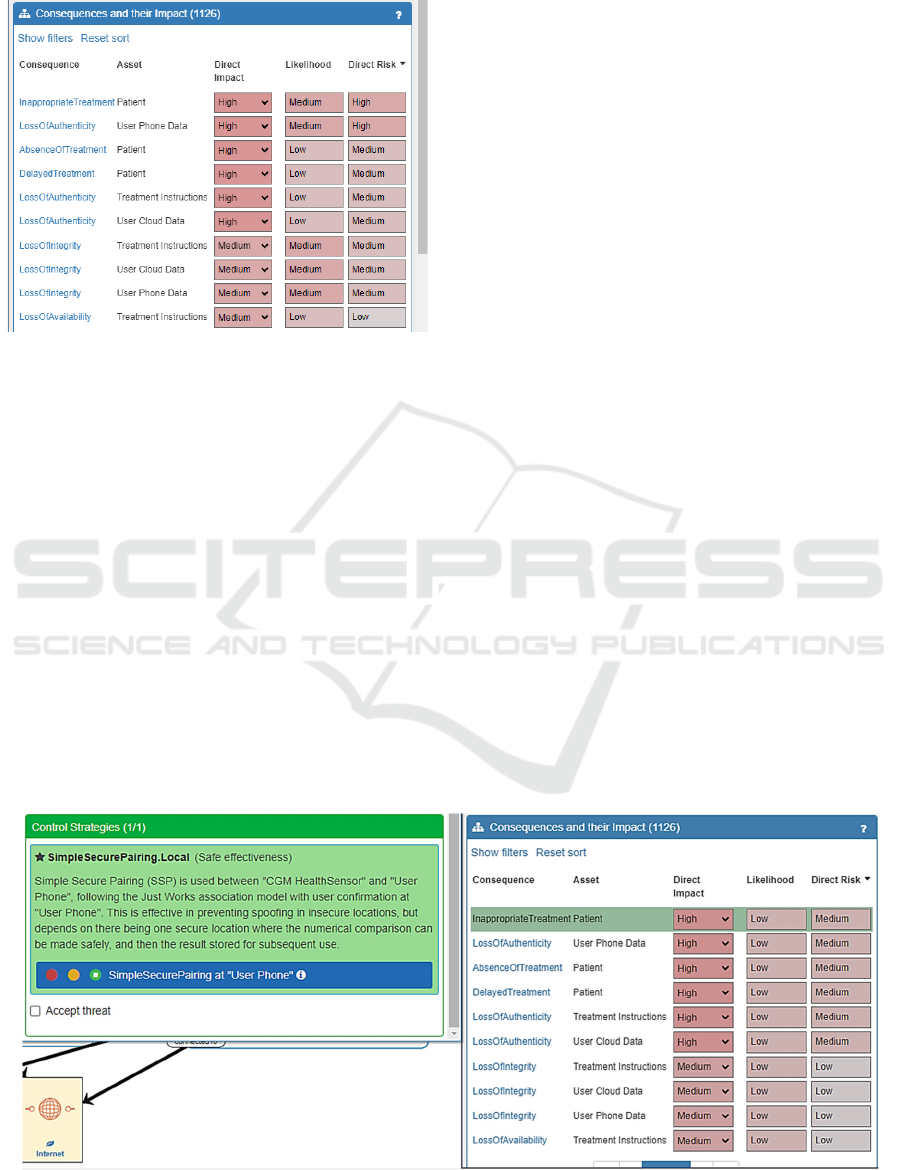
Instructions, finally resulting in Inappropriate
Treatment of the individual.
Figure 8: Initial system risks.
A Simple Secure Pairing control on the
smartphone so the correct Health Sensor pairs with it
blocks this threat path, and applied it reduces the
Inappropriate Treatment risk to Medium, shown in
Figure 9. The Medium risk level remains due to the
consequence impact being high as it involves correct
treatment of a patient, whereas the likelihood of it
occurring becomes Low, reduced from Medium.
The control to wait for up-to-date data on the
Treatment Instructions has been applied, indicating
the patient will wait for up-to-date treatment
instructions before following them and taking their
insulin dosage. This blocks the threat paths for Loss
of Timeliness in the Treatment Instructions and
Inappropriate Treatment of the individual as they will
now not be following treatment instructions that are
based on outdated information. However, it enables a
threat path leading to Delayed Treatment, which
could affect the individual as they may require taking
the correct insulin dosage soon after having their
meal. This illustrates that there are different potential
control strategies and trade-offs that may need to be
considered. Spyderisk does not make the trade-off
decision, though it does provide decision support
information in terms of the possible consequences of
an intervention, which can be taken into consideration
when determining an appropriate course of action.
This demonstrates that non-emergency, indirect
patient harm risks related to cybersecurity incidents
are modelled in Spyderisk automated risk assessment
approach, and initial risk-benefit analyses can be
conducted to consider how some patient harm-related
controls can block certain threats and risks, but enable
others, and so need to be considered carefully.
7 CONCLUSIONS
Knowledge of non-emergency indirect patient harms
has been collected and translated into the terminology
of the Knowledge Base that is part of an existing
cybersecurity risk simulator called Spyderisk. This
knowledge has then been used to determine threat
paths linking cybersecurity incidents to indirect
patient harms and this has been encoded inside that
Knowledge Base. An illustrative example following
a guiding use case has also been presented.
We envision this work will continue by increasing
the link and modelling between these two domains,
and see this work as important since understanding,
preventing and mitigating cybersecurity risks that
result in patient harms is important as they can have
profound effects on the health and wellbeing of
individuals using CMD&IVD.
Figure 9: Effect of secure pairing controls on treatment.
Knowledge Modelling for Automated Risk Assessment of Cybersecurity and Indirect Patient Harms in Medical Contexts
273

ACKNOWLEDGEMENTS
Project Report. This conference paper has been
adapted from part of a NEMECYS project deliverable
report: D2.1 Risk Benefit Schemes (initial) (found at:
https://ec.europa.eu/research/participants/documents
/downloadPublic?documentIds=080166e50edeaf43
&appId=PPGMS).
Funding Statement. This work has been conducted
as part of the NEMECYS project, which is co-funded
by the European Union (101094323), by UK
Research and Innovation (10065802, 10050933 and
10061304), and by the Swiss State Secretariat for
Education, Research and Innovation.
We would like to give thanks to our project partners
for their involvement in risk modelling related use
case discussions. Please note that all views expressed
in this paper are those of the authors, and do not
necessarily represent those above.
REFERENCES
Balogh, E. P., Miller, B. T., Ball, J. R., Committee on
Diagnostic Error in Health Care, Board on Health Care
Services, Institute of Medicine, & The National
Academies of Sciences, Engineering, and Medicine
(Eds.). (2015). Improving Diagnosis in Health Care.
National Academies Press (US).
Biasin E, Kamenjasevic E. Cybersecurity of Medical
Devices: Regulatory Challenges in the European
Union. In: Cohen IG, Minssen T, Price II WN,
Robertson C, Shachar C, eds. The Future of Medical
Device Regulation: Innovation and Protection.
Cambridge University Press; 2022:51-62.
https://doi.org/10.1017/9781108975452.005.
International Organisation for Standardization (ISO). (n.d.).
An easy guide to understanding healthcare data analytics.
https://www.iso.org/healthcare/data-analytics
International Organisation for Standardization (ISO).
(2018). Information technology – Security techniques –
Information security risk management systems –
Overview and vocabulary (ISO Standard No.
27000:2018).
International Organisation for Standardization (ISO).
(2019). Medical devices — Application of risk
management to medical devices (ISO Standard No.
14971:2019).
International Organisation for Standardization (ISO).
(2020). Medical devices — Guidance on the application
of ISO 14971 (ISO Standard No. TR 24971:2020).
International Organisation for Standardization (ISO).
(2022). Information security, cybersecurity and privacy
protection – Guidance on managing information
security risks (ISO Standard No. 27005:2022).
Medical Device Coordination Group (MDCG) (2019).
MDCG 2019-16 Guidance on Cybersecurity for
medical devices. https://ec.europa.eu/docsroom/docu
ments/41863
Medical Device Coordination Group (MDCG) (2023).
MDCG 2023-3. Questions and Answers on vigilance
terms and concepts as outlined in the Regulation (EU)
2017/745 on medical devices. https://health.ec.euro
pa.eu/system/files/2023-02/mdcg_2023-3_en_0.pdf
Mukoro, F. (2011). Care Planning — Mini Topic Review.
NHS Kidney Care. https://www.england.nhs.uk/impro
vement-hub/wp-content/uploads/sites/44/2017/11/Car
e-Planning-Mini-Topic-Review.pdf
NEMECYS. (2023). NEMECYS Use Cases.
https://nemecys.eu/about-us/use-cases
Phillips, S. C., Taylor, S., Boniface, M., Modafferi, S.,
Surridge, M. (2024). Automated Knowledge-Based
Cybersecurity Risk Assessment of Cyber-Physical
Systems. IEEE Access, 12, 82482-82505. doi:
10.1109/ACCESS.2024.3404264
National Health Service [NHS] England. (2023). Medical
devices and digital tools. Version 1.2, 25 May 2023.
https://www.england.nhs.uk/long-read/medical-
devices-and-digital-tools/.
Piggin, R. (2017). Cybersecurity of connected medical
devices. BSI White Paper. Available at: https://www.
bsigroup.com/meddev/LocalFiles/en-US/Whitepapers/
bsi-md-whitepaper-cybersecurity.pdf (Accessed 18
October 2024).
Regulation 2017/745. Regulation (EU) 2017/745 of the
European Parliament and of the Council of 5 April
2017 on medical devices, amending Directive
2001/83/EC, Regulation (EC) No 178/2002 and
Regulation (EC) No 1223/2009 and repealing Council
Directives 90/385/EEC and 93/42/EEC (Text with EEA
relevance.). http://data.europa.eu/eli/reg/2017/745/oj
Regulation 2017/746. Regulation (EU) 2017/746 of the
European Parliament and of the Council of 5 April
2017 on in vitro diagnostic medical devices and
repealing Directive 98/79/EC and Commission
Decision 2010/227/EU (Text with EEA relevance.).
http://data.europa.eu/eli/reg/2017/746/oj
Spyderisk. (2024). Spyderisk Open Project.
https://github.com/Spyderisk
Taylor, S.; Jaatun, M.; Mc Gibney, A.; Seidl, R.;
Hrynchenko, P.; Prosvirin, D. and Mancilla, R. (2024).
A Framework Addressing Challenges in Cybersecurity
Testing of IoT Ecosystems and Components. In
Proceedings of the 9th International Conference on
Internet of Things, Big Data and Security, ISBN 978-
989-758-699-6, ISSN 2184-4976, pages 226-234.
Van Landuyt, D., Joosen, W. (2022). A descriptive study of
assumptions in STRIDE security threat modeling.
Softw Syst Model 21, 2311–2328
ICISSP 2025 - 11th International Conference on Information Systems Security and Privacy
274
