
HealthAIDE: Developing an Audit Framework for AI-Generated
Online Health Information
Tahir Hameed
a
Girard School of Business, Merrimack College, North Andover, MA 01845, U.S.A.
Keywords: Online Health Information, Large Language Models, Generative AI, AI Auditing, Responsible AI.
Abstract: Online health information (OHI) encompasses a wide range of public-facing content, such as information on
symptoms, diseases, medications, and treatments, while online medical information (OMI) involves more
specialized and regulated content, including clinical trial data, surgical procedures, and medical research. OMI
generation and dissemination is held to stringent standards for accuracy, transparency, and explainability,
whereas OHI often requires information-seekers to independently evaluate credibility and relevance of the
information. The rise of generative AI or large language models (LLMs) has exacerbated this disparity, as
LLMs are primarily applied to public-domain OHI without sufficient safeguards, leaving users vulnerable to
misinformation, bias, and non-transparent outputs. This paper presents a systematic literature survey on the
usage of AI and LLMs in OHI, highlighting focus areas and critical gaps in developing a robust framework
for auditing AI-generated health information. The proposed HealthAIDE Framework defines four key pillars
for oversight: reliability and accuracy, trust and acceptance, security and safety, and equity and fairness. A
short but systematic review of AI-driven health information literature reveals areas of stronger focus, such as
accuracy and trust, and weaker focus areas, such as misuse prevention and transparency. Addressing these
gaps through comprehensive audits will enable responsible evolution of AI-driven health information systems.
1 INTRODUCTION
Online Health Information (OHI) searches have
become a primary resource for individuals seeking to
check symptoms, explore treatment options and their
efficacy, and locate healthcare providers or clinics
(Hameed, 2018). With the rise of pre-trained large
language models (LLMs), OHI seeking, its use, and
corresponding health behavior are undergoing a
transformation (Clark et al., 2024; Yan et al.,2024).
Traditionally, users conducting OHI searches on
general-purpose or specialized healthcare search
engines faced issues such as information overload,
difficulty in distinguishing credible sources, and a
lack of personalization (Swar et al.,2017; Freeman et
al., 2020). They were less confident about the
information received and therefore conscientious
when using it. While generative-AI platforms address
some of these issues by offering personalized,
dynamic, and conversational interfaces, they also
introduce new complications while amplifying some
existing problems. For instance, misinformation
a
https://orcid.org/0000-0002-6824-6803
generated by AI hallucinations in definitive tones can
lead to misuse of OHI or undesirable behavior (Jin et
al., 2023, Shen et al., 2024). User trust also suffers
due to a lack of transparency about the sources of
information, making it difficult for users to verify its
accuracy. Additionally, the risks of potential misuse
of sensitive user data increase as open queries are
made on the internet rather than secure electronic
health records or clinical databases, raising concerns
about privacy and ethical use. These issues not only
magnify pre-existing concerns but also raise further
dilemmas around consent, privacy, and the accuracy
of recommendations (Shi et al.,2024).
AI audits assess AI systems to ensure their
reliability, ethical integrity, and compliance with
regulations and standards. These audits aim to
identify and address potential risks associated with
AI, such as bias, security vulnerabilities, privacy
concerns, and transparency issues. By analyzing an
AI system's data, algorithms, and outputs, auditors
can uncover risks, assess the impact of the systems,
and recommend improvements to enhance
Hameed, T.
HealthAIDE: Developing an Audit Framework for AI-Generated Online Health Information.
DOI: 10.5220/0013187100003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 173-183
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
173

trustworthiness and accountability (Falco et al., 2021;
Li et al., 2024, Mökander, 2023).
AI audits are essential for fostering trust in AI
systems and ensuring compliance with governmental
regulations such as the General Data Protection
Regulation (GDPR) in the EU, the Health Insurance
Portability and Accountability Act (HIPAA), and the
California Consumer Privacy Act (CCPA) in the US
(Forcier et al., 2019; Mulgund et al., 2021). However,
the rapid development of generative-AI systems has
complicated the definition and scope of assessments
in an ever-evolving information landscape. Proposed
initiatives, such as the Algorithmic Accountability
Act and the AI Bill of Rights in the US, along with
the EU AI Act, represent significant efforts to guide
the design, use, and deployment of AI systems,
focusing on protecting citizens' rights (Blumenthal-
Barby, 2023; Veale & Zuiderveen, 2021). These
regulations aim to pre-emptively identify potential
ethical, legal, and operational risks prior to
deployment and ensure ongoing monitoring of AI
systems post-implementation.
Even though OHI seeking is one of the fastest-
developing areas leveraging generative AI and LLM-
driven platforms, it also has the potential to cause
significant harm through the dissemination of
misinformation. Despite this, AI audits are not yet
fully adopted or deeply considered in this domain.
While substantial efforts are underway to support the
curation, auditing, and sharing of Online Medical
Information (OMI)—including biomedical content,
medical databases, and repositories used by
professionals—similar mechanisms are notably
absent in the OHI domain for patients and caregivers
(Li and Goel, 2024)
This paper introduces Health-AIDE, a
preliminary framework designed to audit AI-
generated OHI. Section 2 begins by exploring the
rapidly changing landscape of OHI, followed by a
scoping review of existing AI auditing literature to
identify the critical components of an AI audit
framework. Section 3 provides a systematic literature
review of peer-reviewed studies on generative AI in
the OHI domain. It evaluates the strengths and
weaknesses of the current AI-driven OHI systems and
applications against the proposed HEALTH-AIDE
framework. Finally, Section 4 draws conclusions and
discusses future directions for improving OHI
auditing practices.
As one of the earlier papers in this area, this work
aims to provide a foundation for developing Health-
AIDE into a comprehensive, scalable AI Auditing
framework also including the soft side of appropraite
communication with the patients and their caregivers.
By addressing the pressing need for AI audits in the
OHI domain, we hope to pave the way for safer, more
reliable, and ethically governed generative AI-driven
health information systems.
2 BACKGROUND & SCOPE OF
AI AUDITING IN ONLINE
HEALTH INFORMATION
2.1 Emergence of LLM and Generative
AI OHI Platforms
LLMs such as OpenAI's GPT series, Meta’s LLama
and Google's Bard have transformed OHI platforms
by enabling conversational, personalized, and
context-aware responses to user queries. These
models utilize huge datasets of medical literature and
publicly available information, to generate detailed
responses tailored to individual needs. (Shen et al.,
2024; Yan et al., 2024). Unlike traditional search
engines, LLMs excel in synthesizing information
from multiple sources and providing it in user-
friendly formats. No wonder, generative AI based
OHI platforms offers significant benefits, including
improved accessibility, efficiency, and interactivity.
Users can ask complex health-related questions and
receive coherent explanations, making it easier to
understand medical concepts. These tools have also
shown promise in underserved regions, where limited
access to healthcare professionals makes reliable
online information crucial. Despite these advantages,
the adoption of LLM-driven platforms has raised
ethical concerns about data privacy and the
trustworthiness of AI-generated advice, such as
diagnostics and treatment recommendations (Cocci et
al., 2024). Therefore, like all other sectors, there is a
strong need to ensure LLM-based OHI platforms
operate responsibly under the oversight of robust
regulatory frameworks (Mesko and Topol, 2023).
2.2 Auditing Generative AI and
LLM-Based Information and
Systems, Towards a Framework
Auditing has long been a critical governance
mechanism to ensure that information systems and
data are managed in compliance with technical, legal,
and ethical requirements established by
manufacturers, industry organizations, and
governments. Information systems auditing has
matured as a professional discipline with established
procedures and records (Champlain, 2003). However,
HEALTHINF 2025 - 18th International Conference on Health Informatics
174

the rapid evolution of generative AI and LLMs in
recent years has outpaced the development of
appropriate governance measures, leaving gaps in
defining and implementing effective management
practices.
Weidinger et al.’s (2022) taxonomy of LLM risks
highlights several critical issues, including the
perpetuation of discrimination and biases, inadvertent
information hazards such as data leaks, malicious use
such as fraudulent scams, and environmental harms
caused by excessive computing power requirements,
among others. However, the two most prevalent
hazards they identify in generative AI are distorted
human-machine interactions and misinformation
hazards. The former pertains to users overestimating
the capabilities of LLMs, leading to their unsafe or
inappropriate use. The latter poses significant risks as
less-informed users may consume misleading
information, resulting in harm and potentially eroding
public trust in AI-generated content.
Mökander et al. (2023) proposed a three-layered
approach to auditing the outputs of LLM-based
systems, aiming to ensure their effectiveness from
technical, social, and legal perspectives. Their
framework emphasizes equal attention to mitigating
social and ethical risks associated with AI systems.
The authors recommend three types of audits:
governance audits for LLM providers, model audits
conducted before the release of pre-trained LLMs,
and application audits for specific scenarios where
LLMs are deployed. This comprehensive approach
suggests that AI system audits should evolve to
address not only technological and procedural aspects
but also complementary areas that ensure the
responsible use and long-term impact of AI systems
on users, societies, and the natural environment
(Mökander et al., 2023).
We discuss most critical aspects of AI oversight
to develop a basic framework for auditing AI in
healthcare sector. At first, ensuring the accuracy and
correctness of generated content is a critical factor in
the reliability of any AI system. Techniques such as
prompt engineering, querying, and probing serve as
robust methods for generating content and comparing
it against established benchmarks. However, content
must also be assessed on qualitative and semantic
aspects, including fluency, coherence, and relevance,
which significantly contribute to overall user
satisfaction. (Davis et al., 2023). Reliability of AI
systems outputs involves their broader applicability
i.e. scalability as well as continuous learning to stay
on top of current knowledge. These aspects of
reliability, accuracy and access are primarily
addressed through technology and algorithmic audits,
which have consistently been the most prevalent and
central mechanism for evaluating AI systems.
AI systems often rely on vast amounts of sensitive
and personal data. Ensuring that this data is protected
from unauthorized access, breaches, or cyberattacks
is fundamental to maintaining the integrity of AI
systems and safeguarding user privacy (Bala et al.,
2024). Robust data security measures prevent data
leaks, tampering, or misuse throughout the data
lifecycle— from collection and storage to processing
and deployment. These measures include encryption,
access controls, regular security testing, and secure
data handling practices. Security audits help identify
vulnerabilities, ensure compliance with data
protection regulations, and verify that AI systems are
equipped with the necessary safeguards to protect
sensitive data (Nankya et al., 2024).
Similarly, harm prevention and misuse prevention
are essential components in ensuring that AI-
generated content does not lead to negative
consequences for individuals or society (Ellaham et
al., 2020). AI systems must be designed to avoid
producing outputs that could cause physical,
psychological, or social harm, such as promoting
harmful behaviors, spreading misinformation, or
enabling discrimination. Harm prevention strategies
include incorporating ethical guidelines into the AI’s
design, continuously monitoring outputs for
unintended negative effects, and ensuring that AI
models are trained to recognize and mitigate harmful
content. Misuse prevention focuses on safeguarding
against malicious or unethical use of AI systems, such
as using AI for fraud, manipulation, or the creation of
harmful content like deepfakes. To effectively
manage these risks, safety audits are required to
assess how well AI systems prevent harm and misuse.
These audits ensure that safeguards are in place, that
ethical considerations are followed, and that AI
systems are used responsibly, reducing the risk of
harm to individuals and society (Shneiderman, 2020).
Equity and fairness in AI systems rely heavily on
systematically evaluating the technical and
organizational practices surrounding their
development and deployment. This requires
mechanisms to identify, mitigate, and monitor biases
in datasets, models, and outputs while adhering to
ethical principles, regulatory requirements, and
industry standards that promote fairness and prevent
discrimination (Rajkomar, 2018, Ueda et al., 2024).
Ensuring accountability structures within AI providers
is essential to integrating equity and fairness
considerations into decision-making processes at all
levels. Transparency in algorithmic design, inclusivity
of training data, and representativeness of stakeholder
HealthAIDE: Developing an Audit Framework for AI-Generated Online Health Information
175
engagement efforts are critical aspects that must be
prioritized. Furthermore, effective monitoring post-
deployment is necessary to detect and address
unintended biases or inequities. To comprehensively
address these requirements, process and governance
audits emerge as a vital need, providing a structured
approach to evaluate and reinforce the equitable design
and implementation of AI systems, ensuring positive
outcomes for all users and communities.
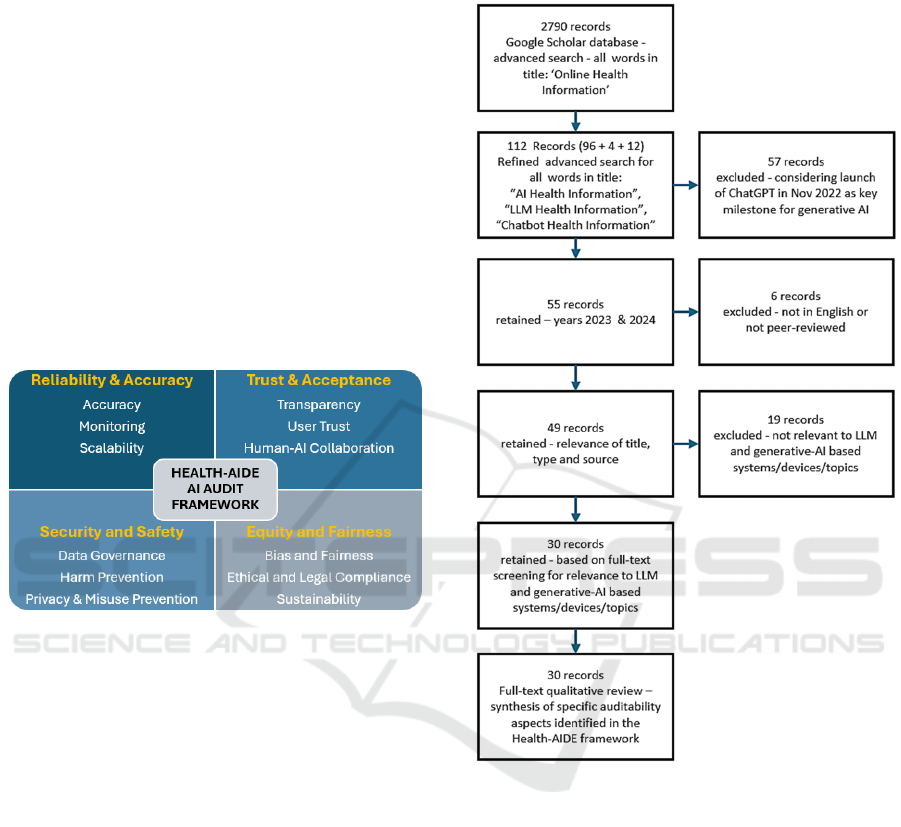
The AI auditing literature can clearly be organized
into the following major aspects that must be
monitored and assessed to develop and deploy
reliable, trustworthy, secure, and inclusive AI
systems. A well-structured Figure 1 outlines the
proposed framework for AI audits, specifically
tailored for the online health information sector,
while remaining broadly applicable to any
information domain.
Figure 1: Health-AIDE; A preliminary framework for
Auditing AI-generated health information.
3 A SYSTEMATIC REVIEW
OF OHI DRIVEN BY
GENERATIVE AI
ChatGPT was launched on November 30, 2022. While
research on transformer models and preliminary
applications existed prior, the release of ChatGPT
marked a significant turning point, driving public
access to advanced LLMs and generative AI systems.
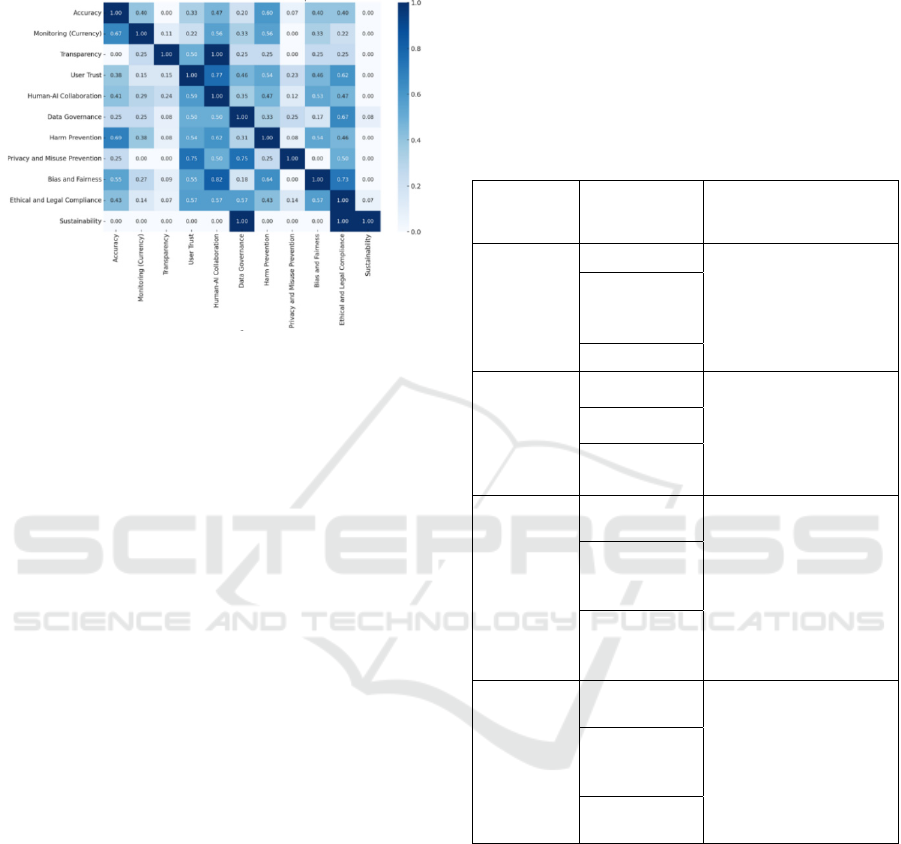
Recognizing this milestone, we conducted a systematic
literature review of articles published on the use of
LLMs and generative AI in the domain of OHI. The
aim was to evaluate the recorded advancements and
align them with the core dimensions of the proposed
Health-Aide framework, assessing the implications
and gaps in AI-driven OHI systems.
3.3 Methods
To that end, our literature review followed a
structured and systematic process to ensure relevance
and depth in analysing AI-generated OHI.
Figure 2: Articles selection for systematic literature review.
Initially, a Google Advanced Search was
conducted using keywords like Online Health
Information, yielding 2,790 results. To refine the
focus, additional searches with terms such as AI
Health Information, LLM Health Information, and
Chatbot Health Information narrowed the results to
112. To ensure timeliness, only articles published
after the launch of ChatGPT in late 2022 were
considered, further reducing the scope to 55. After
reviewing article types and sources, only English
peer-reviewed journal articles and conference
proceedings were retained, resulting in 49 relevant
papers. Full-text reviews were then conducted,
focusing on AI auditing frameworks, ultimately
identifying 30 highly relevant sources for analysis.
The process is outlined in Figure 2.
HEALTHINF 2025 - 18th International Conference on Health Informatics
176

Each paper was reviewed thoroughly to analyze
the scope of the system or device capturing or
generating personal or clinical health information.
Features, opportunities, challenges, and issues
discussed in the articles were systematically mapped
to a table aligned with the dimensions of the Health-
Aide Framework. This mapping provided a
preliminary understanding of innovation trends,
highlighting where AI-driven OHI generation and
sharing are prioritized. The analysis offers insights
into key development areas, challenges, and gaps,
forming a foundation for refining the framework
further.
At this stage, the focus was on identifying
priorities and areas of emphasis without assigning
weights or conducting detailed comparisons. A more
rigorous analysis will be conducted in the next phase
using a systematic literature selection process through
the Web of Science database. This follow-up will
enable weighted assessments, deeper comparisons,
and a broader understanding of how these align with
the Health-AIDE Framework dimensions.
A table comprehensivley summarizing the
mapped observations is included in Appendix A (See
Table 3). This table highlights the features,
opportunities, and issues focused in each health
AI/LLM-based system or device with respect to the
Health-AIDE framework. It also provides a clear and
structured overview of the findings of the literature
review, offering a visual representation of current
innovation and research priorities in AI-based OHI
systems. It defintley serves as a valuable resource for
identifying trends and gaps for further exploration in
other research and future phases of this paper.
4 ANALYSIS, DISCUSSION &
CONCLUSIONS
Since this is a preliminary framework and an initial
attempt at identifying the current focus areas, we
began by calculating the frequencies of each auditable
aspect of health information. All the counts are
presented in Table 1.
Surprisingly, Human-AI Collaboration emerged
as the most emphasized focus area. This indicates that
both users and developers are deeply focused on
understanding and improving interactions with AI
systems in the health domain. Following this is
Accuracy, a critical priority for any information
system and particularly essential in healthcare, where
reliable and precise data is foundational.
Table 1: On-going innovation and research areas w.r.t
components of the AI/LLM-generated Online Health
Information Audit Framework - Health-AIDE.
Count of Discussions
(Implementations,
Opportunities or
Challenges)
Reliability
and
Accuracy
Accuracy 15
Currency/Updates
Monitoring
9
Scalability 5
Trust and
Acceptance
Transparency 4
User Trust 13
Human-AI
Collaboration
17
Security
and Safety
Data Governance 12
Safety and Harm
Prevention
13
Security and Misuse
Prevention
4
Equity and
Fairness
Bias and Fairness 11
Ethical and Legal
Compliance
4
Environmental
Sustainability
1
User Trust and Harm Prevention ranked next,
reflecting growing concerns about misinformation
and its potential dangers to individuals and society.
These aspects highlight the need to mitigate risks
associated with the dissemination of inaccurate or
harmful content in AI-driven systems.
At the lower end, aspects such as Sustainability,
Misuse Prevention, Ethical and Legal Compliance,
and Transparency received comparatively less
attention. This is somewhat unexpected, given that
Data Governance is reasonably well-addressed, yet
related areas like Security and Misuse Prevention
remain underexplored. This disparity underscores
potential gaps in the prioritization of critical aspects
in AI-driven health information systems development
that require further investigation and emphasis.
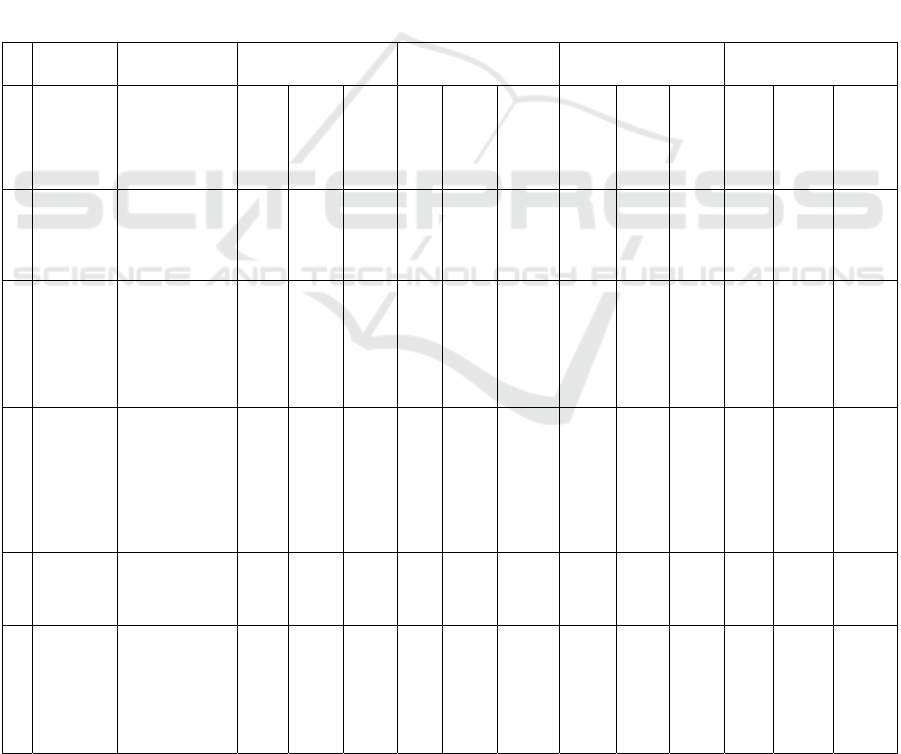
A co-occurrence map provides deeper insights
into how various aspects are interlinked in research,
innovation, and oversight. For instance, Human-AI
Collaboration strongly co-occurs with Bias and
Fairness, suggesting that as efforts progress to
improve human-AI interactions, there is a growing
recognition of the need for equity and fairness in
benefiting from health information systems.
HealthAIDE: Developing an Audit Framework for AI-Generated Online Health Information
177
Addressing biases in design and implementation is
crucial to ensuring inclusivity and equitable access to
AI-driven health solutions.
Figure 3: Co-Occurrence map of auditability aspects of
AI/LLM-generated online health information.
Additionally, Data Governance and User Trust
strongly co-occur with Privacy and Misuse
Prevention, highlighting that privacy concerns and
potential data breaches are central to maintaining trust
in AI-based health information systems. Robust
privacy protections and safeguards against misuse are
essential for fostering confidence and reliability in
these systems.
Transparency and Human-AI Collaboration also
consistently co-occur, emphasizing the users' need to
understand the sources of information and the
explainability of how complex content is generated
and organized. Transparency is critical in fostering
trust, as it provides clear insights into how AI systems
work and ensures that outputs are explainable and
intuitive. In health information systems, this is
particularly important as decisions based on AI-
generated content can directly impact individual well-
being. Transparency is foundational for building trust
and enabling meaningful collaboration between
humans and AI.
In conclusion, these observations demonstrate
that existing and emerging laws, regulations,
technical guidelines, and process standards must be
complemented by interconnected and synergistic
requirements to ensure that information generated by
AI systems is trustworthy, safe, secure and equitable.
Addressing these aspects holistically is vital to
fostering user confidence and minimizing risks in AI-
driven health information systems.
A scan of existing or emerging industry standards,
audit toolkits, and national-level regulations reveals
an increasing emphasis on addressing the identified
auditability aspects for AI-driven software and
information systems in general (see Table 2).
However, compliance with these auditing standards
and regulations has yet to gain widespread acceptance
in the OHI sector,. This gap highlights the need for
greater efforts to enforce audit frameworks in OHI
domain for ensuring accountability, transparency,
and trust in AI-driven health information systems.
Table 2: AI standards, regulations and audit toolkits w.r.t to
OHI auditability aspects identified in HealthAIDE.
AI Standards,
Regulations and
Auditin
g
Toolkits
Reliability
and
Accuracy
Accuracy
ISO/IEC 23894:2023,
ISO/IEC 25010,
NIST AI RMF,
EU AI Act,
FDA SaMD
Currency/
Updates
Monitoring
Scalability
Trust and
Acceptance
Transparency
IEEE 7001-2021,
ISO/IEC TR 24028,
ANSI/CTA-2090,
NIH DISCERN,
Algorithmic
Accountability Act
User Trust
Human-AI
Collaboration
Security
and Safety
Data
Governance
GDPR,
EU AI Act,
HIPPA,
CCPA,
FedRAMP,
HL7, FHIR,
IEEE 7010-2020
Safety and
Harm
Prevention
Security and
Misuse
Prevention
Equity and
Fairness
Bias and
Fairness
WHO Ethics
Guidelines,
DoD
Ethical/Responsible AI
Guidelines,
Ada Toolkit,
ISO/IEC TR
24027:2021
Ethical and
Legal
Compliance
Environmental
Sustainability
This study represents a preliminary, smaller
survey and the development of an initial framework
for auditing AI-generated health information. Future
work aims to expand on this research by
incorporating a larger dataset of papers from the Web
of Science database and engaging expert reviews.
This expanded approach will address technical,
process, and interdisciplinary issues at a deeper level,
while also considering the details of above-noted and
emerging regulations, technical standards and
professional codes to create a more comprehensive
and robust framework.
HEALTHINF 2025 - 18th International Conference on Health Informatics
178

REFERENCES
Alhendawi, K. M. (2024). Task-technology fit model:
Modelling and assessing the nurses’ satisfaction with
health information system using AI prediction
models. International Journal of Healthcare
Management, 17(1), 12-24.
Alkhalaf, M., Yu, P., Yin, M., & Deng, C. (2024). Applying
generative AI with retrieval augmented generation to
summarize and extract key clinical information from
electronic health records. Journal of Biomedical
Informatics, 104662.
Amin, M. S., Johnson, V. L., Prybutok, V., & Koh, C. E.
(2024). An investigation into factors affecting the
willingness to disclose personal health information
when using AI-enabled caregiver robots. Industrial
Management & Data Systems, 124(4), 1677-1699.
Aparicio, E., Nguyen, Q., Doig, A. C., Gutierrez, F. X. M.,
Sah, S., Mane, H., ... & He, X. (2023, November).
Development of rosie the chatbot: A health information
intervention for pregnant and new mothers of color.
In APHA 2023 Annual Meeting and Expo. APHA.
Arda, S. (2024). Taxonomy to Regulation: A (Geo)
Political Taxonomy for AI Risks and Regulatory
Measures in the EU AI Act. arXiv preprint
arXiv:2404.11476.
Ascorbe, P., Campos, M. S., Domínguez, C., Heras, J., &
Reinares, A. R. T. (2023). prevenIA: a Chatbot for
Information and Prevention of Suicide and other Mental
Health Disorders. In SEPLN (Projects and
Demonstrations) (pp. 26-30).
Bala, I., Pindoo, I., Mijwil, M. M., Abotaleb, M., &
Yundong, W. (2024). Ensuring security and privacy in
Healthcare Systems: a Review Exploring challenges,
solutions, Future trends, and the practical applications
of Artificial Intelligence. Jordan Medical
Journal, 58(3).
Blumenthal-Barby, J. (2023). An AI bill of rights:
Implications for health care AI and machine learning—
A bioethics lens. The American Journal of
Bioethics, 23(1), 4-6.
Champlain, J. J. (2003). Auditing information systems. John
Wiley & Sons.
Chang, C. W., Hu, M., Ghavidel, B., Wynne, J. F., Qiu, R.
L. J., Washington, M., ... & Yang, X. (2024). An LLM-
Based Framework for Zero-Shot De-Identifying
Flexible Text Data in Protected Health Information
Enabling Potential Risk-Informed Patient Safety.
International Journal of Radiation Oncology, Biology,
Physics, 120(2), e518.
Clark, O., Reynolds, T. L., Ugwuabonyi, E. C., & Joshi, K.
P. (2024, June). Exploring the Impact of Increased
Health Information Accessibility in Cyberspace on
Trust and Self-care Practices. In Proceedings of the
2024 ACM Workshop on Secure and Trustworthy
Cyber-Physical Systems (pp. 61-70).
Cocci, A., Pezzoli, M., Lo Re, M., Russo, G. I., Asmundo,
M. G., Fode, M., ... & Durukan, E. (2024). Quality of
information and appropriateness of ChatGPT outputs
for urology patients. Prostate cancer and prostatic
diseases, 27(1), 103-108.
Davis, R., Eppler, M., Ayo-Ajibola, O., Loh-Doyle, J. C.,
Nabhani, J., Samplaski, M., ... & Cacciamani, G. E.
(2023). Evaluating the effectiveness of artificial
intelligence–powered large language models
application in disseminating appropriate and readable
health information in urology. The Journal of urology,
210(4), 688-694.
Ellaham, S., Ellahham, N., & Simsekler, M. C. E. (2020).
Application of artificial intelligence in the health care
safety context: opportunities and challenges. American
Journal of Medical Quality, 35(4), 341-348.
Falco, G., Shneiderman, B., Badger, J., Carrier, R.,
Dahbura, A., Danks, D., ... & Yeong, Z. K. (2021).
Governing AI safety through independent
audits. Nature Machine Intelligence, 3(7), 566-571.
Freeman, J. L., Caldwell, P. H., & Scott, K. M. (2020).
The role of trust when adolescents search for and
appraise online health information. The Journal of
Pediatrics, 221, 215-223.
Forcier, M. B., Gallois, H., Mullan, S., & Joly, Y. (2019).
Integrating artificial intelligence into health care
through data access: can the GDPR act as a beacon for
policymakers?. Journal of Law and the
Biosciences, 6(1), 317-335.
Hameed, T. (2018). Impact of Online Health Information
on Patient-physician Relationship and Adherence;
Extending Health-belief Model for Online Contexts.
In HEALTHINF (pp. 591-597).
Harrington, C. N., & Egede, L. (2023, April). Trust,
comfort and relatability: Understanding black older
adults’ perceptions of chatbot design for health
information seeking. In Proceedings of the 2023 CHI
Conference on Human Factors in Computing
Systems (pp. 1-18).
Hatamlah, H. (2024). Adolescents' online health
information seeking: Trust, e-health literacy, parental
influence, and AI-generated credibility. International
Journal of Data and Network Science, 8(2), 809-822.
Hong, S. J., & Cho, H. (2023). Privacy management and
health information sharing via contact tracing during
the COVID-19 pandemic: A hypothetical study on AI-
based technologies. Health Communication, 38(5),
913-924.
Jin, Q., Leaman, R., & Lu, Z. (2023). Retrieve, summarize,
and verify: how will ChatGPT affect information
seeking from the medical literature?. Journal of the
American Society of Nephrology, 34(8), 1302-1304.
Jin, E., & Eastin, M. (2024). Towards more trusted virtual
physicians: the combinative effects of healthcare
chatbot design cues and threat perception on health
information trust. Behaviour & Information
Technology, 1-14.
Kunlerd, A. (2024). Developing an Innovative Health
Information Service System: The Potential of Chatbot
Technology. Suan Sunandha Science and Technology
Journal, 11(2), 61-69.
Latt, P. M., Aung, E. T., Htaik, K., Soe, N. N., Lee, D.,
King, A. J., ... & Fairley, C. K. (2024). Real-World
HealthAIDE: Developing an Audit Framework for AI-Generated Online Health Information
179

Evaluation of Artificial Intelligence (AI) Chatbots for
Providing Sexual Health Information: A Consensus
Study Using Clinical Queries.
Li, S., Mou, Y., & Xu, J. (2024). Disclosing Personal
Health Information to Emotional Human Doctors or
Unemotional AI Doctors? Experimental Evidence
Based on Privacy Calculus Theory. International
Journal of Human–Computer Interaction, 1-13.
Li, Y., & Goel, S. (2024). Making it possible for the
auditing of AI: A systematic review of AI audits and AI
auditability. Information Systems Frontiers, 1-31.
Liew, T. W., Tan, S. M., Yoo, N. E., Gan, C. L., & Lee, Y.
Y. (2023). Let's talk about Sex!: AI and relational
factors in the adoption of a chatbot conveying sexual
and reproductive health information. Computers in
Human Behavior Reports, 11, 100323.
Link, E., & Beckmann, S. (2024). AI at everyone’s
fingertips? Identifying the predictors of health
information seeking intentions using AI. Communication
Research Reports, 1-11.
Liu, J., Wang, J., Huang, H., Zhang, R., Yang, M., & Zhao,
T. (2023, October). Improving LLM-Based Health
Information Extraction with In-Context Learning.
In China Health Information Processing
Conference (pp. 49-59). Singapore: Springer Nature
Singapore.
Ma, Y., Achiche, S., Pomey, M. P., Paquette, J., Adjtoutah,
N., Vicente, S., ... & MARVIN chatbots MARVIN
chatbots Patient Expert Committee. (2024). Adapting
and evaluating an AI-Based Chatbot through patient
and stakeholder engagement to provide information for
different health conditions: Master Protocol for an
Adaptive Platform Trial (the MARVIN Chatbots
Study). JMIR Research Protocols, 13(1), e54668.
McMahon, E., Fetters, T., Jive, N. L., & Mpoyi, M. (2023).
Perils and promise providing information on sexual and
reproductive health via the Nurse Nisa WhatsApp
chatbot in the Democratic Republic of the Congo. Sexual
and Reproductive Health Matters, 31(4), 2235796.
Mendel, T., Nov, O., & Wiesenfeld, B. (2024). Advice from
a Doctor or AI? Understanding Willingness to Disclose
Information Through Remote Patient Monitoring to
Receive Health Advice. Proceedings of the ACM on
Human-Computer nteraction, 8(CSCW2), 1-34.
Meskó, B., & Topol, E. J. (2023). The imperative for
regulatory oversight of large language models (or
generative AI) in healthcare. NPJ digital medicine,
6(1), 120.
Mökander, J. (2023). Auditing of AI: Legal, ethical and
technical approaches. Digital Society, 2(3), 49.
Mökander, J., Schuett, J., Kirk, H. R., & Floridi, L. (2023).
Auditing large language models: a three-layered
approach. AI and Ethics, 1-31.
Mulgund, P., Mulgund, B. P., Sharman, R., & Singh, R.
(2021). The implications of the California Consumer
Privacy Act (CCPA) on healthcare organizations:
Lessons learned from early compliance
experiences. Health Policy and Technology, 10(3),
100543.
Nankya, M., Mugisa, A., Usman, Y., Upadhyay, A., &
Chataut, R. (2024). Security and Privacy in E-Health
Systems: A Review of AI and Machine Learning
Techniques. IEEE Access.
Nyarko, A. J. (2024). Exploring Ghanaian Tertiary
Students’ Perceptions Towards AI as a First-Hand
Source of Health Information for Diagnosis and Self-
Medication. Journal of Health Informatics in Africa,
11(1), 64-76.
Ono, G. N., Obi, E. C., Chiaghana, C., & Ezegwu, D.
(2024). Digital Divide and Access: Addressing
Disparities in Artificial Intelligence (Ai) Health
Information for Nigerian Rural Communities. Social
Science Research, 10(3).
Park, J., Singh, V., & Wisniewski, P. (2023). Supporting
youth mental and sexual health information seeking in
the era of artificial intelligence (ai) based
conversational agents: Current landscape and future
directions. Available at SSRN 4601555.
Rajkomar, A., Hardt, M., Howell, M. D., Corrado, G., &
Chin, M. H. (2018). Ensuring fairness in machine
learning to advance health equity. Annals of internal
medicine, 169(12), 866-872.
Raddatz, N., Kettinger, W. J., & Coyne, J. (2023). Giving
to Get Well: Patients’ Willingness to Manage
and Share Health Information on AI-Driven
Platforms. Communications of the Association for
Information Systems, 52(1), 1017-1049.
Rezaee, Z., Homayoun, S., Poursoleyman, E., & Rezaee, N.
J. (2023). Giving to Get Well: Patients’ Willingness to
Manage and Share Health Information on AI-Driven
Platforms. Global Finance Journal, 55.
Sakriwattana, K. (2024). Factor affecting intention to use
chatbot for health information. Procedia of
Multidisciplinary Research, 2(7), 5-5.
Shen, S. A., Perez-Heydrich, C. A., Xie, D. X., & Nellis, J.
C. (2024). ChatGPT vs. web search for patient questions:
what does ChatGPT do better?. European Archives of
Oto-Rhino-Laryngology, 281(6), 3219-3225.
Shi, X., Liu, J., Liu, Y., Cheng, Q., & Lu, W. (2024). Know
where to go: Make LLM a relevant, responsible, and
trustworthy searchers. Decision Support Systems,
114354.
Shneiderman, B. (2020). Bridging the gap between ethics
and practice: guidelines for reliable, safe, and
trustworthy human-centered AI systems. ACM
Transactions on Interactive Intelligent Systems
(TiiS), 10(4), 1-31.
Swar, B., Hameed, T., & Reychav, I. (2017). Information
overload, psychological ill-being, and behavioral
intention to continue online healthcare information
search. Computers in human behavior, 70, 416-425.
Ueda, D., Kakinuma, T., Fujita, S., Kamagata, K., Fushimi,
Y., Ito, R., ... & Naganawa, S. (2024). Fairness of
artificial intelligence in healthcare: review and
recommendations. Japanese Journal of
Radiology, 42(1), 3-15.
Vaira, L. A., Lechien, J. R., Abbate, V., Allevi, F., Audino,
G., Beltramini, G. A., ... & De Riu, G. (2024).
HEALTHINF 2025 - 18th International Conference on Health Informatics
180
Validation of the QAMAI tool to assess the quality of
health information provided by AI. medRxiv, 2024-01.
Veale, M., & Zuiderveen Borgesius, F. (2021).
Demystifying the Draft EU Artificial Intelligence
Act—Analysing the good, the bad, and the unclear
elements of the proposed approach. Computer Law
Review International, 22(4), 97-112.
Weidinger, L., Uesato, J., Rauh, M., Griffin, C., Huang, P.
S., Mellor, J., ... & Gabriel, I. (2022, June). Taxonomy
of risks posed by language models. In Proceedings of
the 2022 ACM Conference on Fairness, Accountability,
and Transparency (pp. 214-229).
Xiao, Z+3:50., Liao, Q. V., Zhou, M., Grandison, T., & Li,
Y. (2023, March). Powering an ai chatbot with expert
sourcing to support credible health information access.
In Proceedings of the 28th international conference on
intelligent user interfaces (pp. 2-18).
Yan, Y., Hou, Y., Xiao, Y., Zhang, R., & Wang, Q. (2024).
KNOWNET: Guided Health Information Seeking from
LLMs via Knowledge Graph Integration. IEEE
Transactions on Visualization and Computer Graphics.
Yiannakoulias, N. (2024). Spatial intelligence and
contextual relevance in AI-driven health information
retrieval. Applied Geography, 171, 103392.
Yin, R., & Neyens, D. M. (2024). Examining how
information presentation methods and a chatbot impact
the use and effectiveness of electronic health record
patient portals: An exploratory study. Patient
Education and Counseling, 119, 108055.
APPENDIX
Table 3: Systematic Literature Review – Mapping key features, opportunities, challenges and issues of AI systems in literature
onto Health-AIDE AI Auditing framework.
Reliability &
Accuracy
Trust and
Acceptance
Security and Safety
Equity
Reference AI Scope
Accu
racy
Monit
oring
(Curr
ency)
Scala
bility
Tran
spar
enc
y
User
Trust
Huma
n-AI
Collab
oratio
n
Data
Gover
nance
Harm
Preve
ntion
Privacy
and
Misuse
Preven
tion
Bias
and
Fairn
ess
Ethical
and
Legal
Compli
ance
Sustai
nability
1
Xiao, Z.
et al.,
(2023)
Expert-sourced
chatbot;
Design,
Evaluation,
OHI
X X X X X X X
2
Vaira et
al. (2024)
OHI, Quality
assessment of
medical
Artificial
Intelligence
(QAMAI) based
on mDISCERN
X X
3
Hatamla
h, H.
(2024)
Parental
oversight and
communicatio
n to ensure
reliable and
trustworthy
info and
behavior
X X X
4
Yiannak
oulias,
N.
(2024)
Spatial
dispersion and
OHI
X X X
5
Amin,
M. S., et
al.,
(2024).
Caregiver
robots
interaction,
Disclosing
personal
health info
(PHI)
X X X X X
HealthAIDE: Developing an Audit Framework for AI-Generated Online Health Information
181
Table 3: Systematic Literature Review – Mapping key features, opportunities, challenges and issues of AI systems in literature
onto Health-AIDE AI Auditing framework (cont.).
Reliability &
Accuracy
Trust and
Acceptance
Security and Safety
Equity
Reference AI Scope
Accu
racy
Monit
oring
(Curr
ency)
Scala
bility
Tran
spar
enc
y
User
Trust
Huma
n-AI
Collab
oratio
n
Data
Gover
nance
Harm
Preve
ntion
Privacy
and
Misuse
Preven
tion
Bias
and
Fairn
ess
Ethical
and
Legal
Compli
ance
Sustai
nability
6
Liew, T.
W., et
al.
(2023)
Chatbot, Youth
interactions on
sexual and
reproductive
health (SRH)
information,
X X X X X
7
Link, E., &
Beckman
n, S.
(2024).
OHI seeking
X
8
Li, S.et
al., (2023)
AI doctors,
disclosure of
PHI
X X X X X
9
Raddatz,
N.et al.
(2023)
Internet of
Medical
Things,
disclosure of
PHI
X X X X
10
Park, J. et
al. (2023)
Sexual and
reproductive
chatbots,
adolescents,
OHI
X X X X X X
11
Nyarko,
A. J.
(2024)
Engaging with
OHI for self-
care purposes,
Ghanian
students
X X X X
12
Ono, G.N.
et al.
2024
Digital gaps, AI
access,
Nigerian
students
X X
13
Alhenda
wi, K. M.
(2024).
Connected
medical
devices cloud
network,
Exchange of
health info
X X X X
14
Hong, S.
J.et al.
(2023)
Users
considering
adoption of
contact-
tracing app.,
COVID-19
X X
15
Mendel,
T. et
al.2024
Remote
patient
monitoring
devices, dis-
closure of PHI
X X X
16
Latt, P.
M.et al.
(2024)
Sexual health,
prompt-tuned
chatbots,
Australia
X X X X X
17
Rezaee,
Z.et al.
(2023)
ESG
disclosures by
firms, EU and
others
X X X
HEALTHINF 2025 - 18th International Conference on Health Informatics
182
Table 3: Systematic Literature Review – Mapping key features, opportunities, challenges and issues of AI systems in literature
onto Health-AIDE AI Auditing framework (cont.).
Reliability &
Accuracy
Trust and
Acceptance
Security and Safety
Equity
Reference AI Scope
Accu
racy
Monit
oring
(Curr
ency)
Scala
bility
Tran
spar
enc
y
User
Trust
Huma
n-AI
Collab
oratio
n
Data
Gover
nance
Harm
Preve
ntion
Privacy
and
Misuse
Preven
tion
Bias
and
Fairn
ess
Ethical
and
Legal
Compli
ance
Sustai
nability
18
Alkhalaf,
M.et al.
(2024)
Zero-shot
prompt
engineering,
RAG, EHRs, AI
Hallucinations
X X X
19
Ma, Y.et
al. (2024)
MARVIN
Chatbots,
Multiple
disease
diagnostics
and care
X X X X
20
Liu, J.et
al. (2023)
CHINA, Health
information
extraction, In-
context
learning
X X X
21
Chang, C.
W.et al.
(2024)
Zero-shot de
identification
of health data
X X X X
22
Nguyen,
V. C.et al.
(2024)
Mental health,
Misinformation
, Few-shot
X X
23
Jin, E.et
al. (2024)
Virtual
Doctors/
Physicians,
Chatbots
X X X X
24
Harringto
n, C. N. et
al. (2024)
Chatbots,
Gender and
race
associations
X X X X X
25
Yin, R., &
Neyens,
D. M.
(2024).
Design,
Chatbots,
EHRs, Patient
Portals
X X
26
Kunlerd,
A. (2024).
Line Chatbots,
Diet regimens,
Health
X X X X X X
27
Sakriwatt
ana, K.
(2024).
Chatbots,
Intergeneration
al differences,
Age gaps
X X X X
28
Aparicio,
E.et al.
(2023)
Chatbots, Pre-
natal care,
Post-partum
care, Mothers
of color
X X X X X X
29
McMahon
, E.et al.
(2023)
Congo, Sexual
and
Reproductive
Health, NISA
chatbot
X X X X X X
30
Ascorbe,
P.et al.
(2023)
Mental health,
Suicide
Preven-tion,
Chatbot,
WhatsApp,
Spain
X X X X X
HealthAIDE: Developing an Audit Framework for AI-Generated Online Health Information
183
