
Deep Learning Characterization of Volatile Organic Compounds with
Spectrometer-on-Card
Ander Cejudo
1,2 a
, Markel Arrojo
1 b
, Miriam Guti
´
errez
1,3 c
, Karen L
´
opez-Linares
1,4 d
,
Hossam Haick
5 e
, Iv
´
an Mac
´
ıa
1,4,6 f
and Cristina Mart
´
ın
1,2,4 g
1
Fundaci
´
on Vicomtech, Basque Research and Technology Alliance (BRTA), Mikeletegi 57,
20009 Donostia-San Sebasti
´
an, Spain
2
Faculty of Engineering, University of Deusto, Avda. Universidades, 24, Bilbao 48007, Spain
3
Universidad Rey Juan Carlos, Cam. del Molino, 5, 28942 Fuenlabrada, Spain
4
BioGipuzkoa Health Research Institute (Bioengineering Area), eHealth Group, 20014 Donostia-San Sebasti
´
an, Spain
5
Department of Chemical Engineering and the Russell Berrie Nanotechnology Institute, Technion,
Israel Institute of Technology, Haifa 3200003, Israel
6
Computational Intelligence Group, Computer Science Faculty, University of the Basque Country, UPV/EHU, Spain
Keywords:
Exposome, Volatile Organic Compounds, Environment Characterization, Artificial Intelligence, Deep
Learning, Recurrent Neural Networks.
Abstract:
The exposome encompasses all environmental exposures that affect internal biological processes throughout
a person’s life, influencing health outcomes. Among these exposures, volatile organic compounds (VOCs)
are particularly significant, as they are closely related to respiratory issues, cardiovascular diseases, cancer,
and other health conditions. Detecting some of them is therefore critical for assessing environmental impacts
on health. In this study, we use a low-cost, highly portable SPectrometer-On-Card (SPOC) device designed
to characterize complex mixtures by separating VOCs through its layers. The device was previously tested
to detect VOCs in controlled laboratory conditions. Hereby, we explore artificial intelligence algorithms to
identify patterns in the signals captured by the SPOC in closer to real-word conditions. Specifically, we focus
on two different use cases including direct exposure to a VOC source and indoors versus outdoors signal
recognition. Our top-performing model, a recurrent neural network, achieves accuracies of 92,4% and 97,2%
for each use case, respectively, effectively identifying exposures in the first case and correctly classifying
87,5% of exposures in the second. These results demonstrate the potential of our methodology applied to
SPOC data for broader health-related applications, such as detecting incomplete combustions, identifying
diseases like cancer through exhaled breath, and detecting leaks from industrial plants.
1 INTRODUCTION
The concept of exposome is essential for understand-
ing health, as it encompasses the totality of environ-
mental exposures and their effects on internal biolog-
ical processes (Vermeulen et al., 2020). This holis-
tic perspective shows how diverse exposures (rang-
ing from chemicals to lifestyle factors) interact with
genetic predispositions to influence health outcomes
a
https://orcid.org/0000-0001-7944-2706
b
https://orcid.org/0009-0005-1099-7814
c
https://orcid.org/0000-0002-6692-9934
d
https://orcid.org/0000-0002-4800-6052
e
https://orcid.org/0000-0002-2370-4073
f
https://orcid.org/0000-0003-0448-7840
g
https://orcid.org/0000-0002-3919-2738
(Erzin and G
¨
ul
¨
oks
¨
uz, 2021; Danieli et al., 2024).
Among these chemicals, the study of volatile organic
compounds (VOCs) is particularly significant, given
their prevalence in both natural and anthropogenic en-
vironments and their implications for public health
(Li et al., 2020; Zhang et al., 2024).
VOCs are produced by both natural sources (e.g.
vegetation) (Katsouyanni, 2003) and human activity.
Burning fossil fuels, solvents in industrial processes
like petroleum distribution and storage, and motor
vehicle fumes (particularly in cities with heavy traf-
fic) are the main human-caused sources of VOCs (El-
bir et al., 2007; Wang and Zhao, 2008). Their pres-
ence in the air poses significant health risks, as expo-
sure to VOCs has been linked to various adverse ef-
fects. These include allergies, respiratory issues like
asthma, chronic obstructive pulmonary disease, and
Cejudo, A., Arrojo, M., Gutiérrez, M., López-Linares, K., Haick, H., Macía, I. and Martín, C.
Deep Learning Characterization of Volatile Organic Compounds with Spectrometer-on-Card.
DOI: 10.5220/0013210300003938
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2025), pages 197-207
ISBN: 978-989-758-743-6; ISSN: 2184-4984
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
197

irritation of the airways as a result of tropospheric
ozone generation (Tanaka et al., 2000). More severe
health issues like cancer, leukemia, and even mortal-
ity have been related to VOC exposure (Dutta et al.,
2018; Sun et al., 2016). The negative effects of VOCs
on human health depend on both the concentration
and the duration of the exposure (Soni et al., 2018).
The gold standard for VOC detection is gas
chromatography-mass spectrometry (GC–MS)
(Langford et al., 2014). This technique allows the
differentiation, identification, and quantification of
different VOCs in a sample. The sample is introduced
into the gas chromatograph, where the VOCs are
separated. A detector measures the quantity of each
ion, and the resulting spectrum is compared with a
reference library to identify the VOCs (Dincer et al.,
2006). However, this technology requires a labora-
tory, which is not always available or affordable. The
standard methodology for VOC detection is expen-
sive, energy-inefficient, and slow, requiring around
20 to 40 minutes for analysis completion (Fialkov
et al., 2020). To bring the compound samples to the
laboratory, adsorption tubes are required (Ho et al.,
2018; Li et al., 2004). These tubes adsorb compounds
onto an adsorbent material for transport. During
this process, the compounds can undergo changes
due to humidity, oxidant exposure, or incomplete
desorption, which may alter the sample (Kumar
and V
´
ıden, 2007; Woolfenden, 2010). Then, the
contents of the tubes are released for analysis using a
technique called thermal desorption. Therefore, there
is a need to develop strategies to analyze VOCs in
situ, providing fast and high-resolution results.
For on-site VOC analysis, two main approaches
can be distinguished: individual VOC identification
and non-target characterization. Devices designed for
the former approach require calibration for detect-
ing specific VOCs, which increases costs and limits
their ability to identify diverse compound mixtures
or a broader set of VOCs. In contrast, non-target
characterization devices, such as electronic noses (e-
noses) are more suited for detection, where the spe-
cific VOCs or mixtures of compounds are unknown
(Rabehi et al., 2024). These devices are usually
equipped with an array of cross-reactive sensors that
generate unique responses when exposed to various
complex mixtures of chemicals. These responses are
used to extract different patterns from the signals,
usually using unsupervised learning algorithms, be-
ing able to differentiate between groups and allow-
ing for applications such as early screening of various
cancers (Machado et al., 2005), lung diseases such as
pneumonia and upper respiratory tract infections (Per-
saud, 2005), diabetes (Saasa et al., 2019) or identifi-
cation of bacterial pathogens (Lai et al., 2002). Al-
though e-noses are sensitive to VOCs mixture pres-
ence, they cannot identify specific VOCs within the
detected patterns (Smolander, 2003).
Recent advancements have led to the development
of a miniaturized spectrometer device (SPectrometer-
On-Card, SPOC) aimed at characterizing complex
mixtures containing unknown VOCs while also pro-
viding the ability to detect specific VOCs within these
mixtures. This is achieved through a multi-layer de-
sign, which separates VOCs as the air flows through
the layers. However, this device is still a prototype
and has only been used for mixture characterization
and specific VOC detection in a controlled laboratory
environment at Technion (Israel Institute of Technol-
ogy) facilities Maity et al. (2022); more complex mix-
ture characterization in open-air environments has not
yet been conducted with this device.
The main objective of this work is to analyze the
potential of artificial intelligence (AI) techniques to
differentiate signals captured by the SPOC in two,
closer to real-world, environments. The unique fea-
tures of the SPOC for non-target VOC detection, com-
bined with the proposed methodology for signal clas-
sification may allow to analyze diverse compound
mixtures without being limited to a specific set of
VOCs. The results will highlight the potential of
this technology, combined with a novel AI approach,
to analyze diverse compound mixtures without being
limited to a specific set of VOCs.
The structure of the paper is organized as fol-
lows. In section 2, we delve into the previous re-
search conducted on the analysis of volatile organic
compounds. Section 3, provides an explanation of
the device used for data captured, the use cases con-
sidered in this study and the deep learning approach
for environment characterization. Section 4 presents
and discusses the quantitative results obtained from
the experiments. Section 5 concludes the study by
summarizing the key findings.
2 BACKGROUND
There are many studies that detect specific VOCs and
their concentrations for air quality assessment. Won
et al. (2021) analyzed the concentrations of 24 VOCs
that are measured in underground shopping districts
in Korea using a Thermal Desorption–Gas Chro-
matography Mass Spectrometry (TD–GCMS) device.
The results indicated higher VOC concentrations in-
doors, identifying six sources of air pollution. Simi-
larly, the authors of (Scheepers et al., 2017) studied
the indoor air quality of a university hospital. Air
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
198

samples were collected both indoors and outdoors us-
ing canisters and then these were analyzed with TD-
GCMS. The authors concluded that laboratory work
contributes substantially to indoor pollution, whereas
known outdoor sources do not significantly affect in-
door air quality. Another study (Pang et al., 2019)
used a portable photoionization detector to charac-
terize up to eight VOCs in a laboratory environment,
showing that the concentration response increases lin-
early with the chemical concentrations tested.
Several works can be found in the state-of-the-art
that aim at the non-target characterization of air based
on VOC detection. Many of these works make use
of e-noses, which are particularly popular for provid-
ing distinguishable patterns for different VOC expo-
sures. One of the first works that addressed the envi-
ronment characterization problem using e-noses was
conducted by Nicolas et al. (2000). They used the
response of a cross-reactive detector to monitor air
quality combined with principal components analy-
sis to classify different unknown air mixtures around
VOC emitting sources. Similar works use artificial
neural networks to identify patterns in data registered
from the pulp and paper industry (Deshmukh et al.,
2014). For example, Licen et al. (2020) used an e-
nose device to identify patterns with clustering and
self-organizing maps from different VOC mixtures in
the context of air quality. Furthermore, they validated
their findings by using ancillary data from a photoion-
ization detector that measures VOCs.
VOC characterization in air extends beyond air-
quality control and has proven valuable in other fields,
particularly in early-stage disease diagnosis, as ex-
haled air can provide valuable insights into metabolic
diseases (Li et al., 2023). For instance, Anzivino et al.
(2022) successfully used Principal Component Anal-
ysis (PCA) to cluster patients with head and neck can-
cer and rhinitis based on breath signals captured by an
e-nose device. Similarly, (Liu et al., 2021) proposed
a PCA-Singular Value Estimation ensemble learning
framework to cluster the 214 breath samples for early
lung cancer detection, achieving excellent results with
95,75% accuracy and 94,78% recall in their classifi-
cation task.
While the non-target characterization of air has
been extensively researched ((Nicolas et al., 2000; Li-
cen et al., 2020)) and the application of AI is common
in this field (Liu et al., 2023), to the best of our knowl-
edge, no prior studies have explored AI-enhanced
characterization using a portable, lightweight, and
cost-effective device capable of providing insights
into individual detection as well. Thereby, in this
work we aim to leverage a methodology based on
advanced signal processing and AI tools to disentan-
gle information coming from a multi-layered detector
that is able to characterize and differentiate complex
air mixtures.
3 MATERIALS AND METHODS
This section introduces the device used for data cap-
ture in two different use cases and the designed deep
learning-based pipeline for environment characteriza-
tion. Subsection 3.1 outlines the motivation behind
the SPOC device for VOC analysis, whereas subsec-
tion 3.2 details the two use cases selected for this
study. Finally, subsection 3.3 presents the methodol-
ogy for signal analysis using several machine learning
methods.
3.1 Spectrometer-on-Card
The SPectrometer-On-Card (SPOC) device, proto-
typed by Technion (Israel Institute of Technology),
is employed to detect and measure the presence
of VOCs in suspension. This innovative technol-
ogy utilizes a miniaturized, layer-based sensor ca-
pable of identifying complex molecular structures
through a hierarchically stacked geometrical config-
uration (HSGC). Each layer is composed of function-
alized graphene sensors printed on porous cellulose
sheets, with multiple layers stacked together (Maity
et al., 2022). This architecture could be thought of
as a miniaturized version of chromatography columns
(where the porosity of cellulose plays the main role)
and mass spectrometer (where the array of sensors is
responsible for identifying unknown compounds).
As a mixture of compounds flows from the first
to the last layer, molecules are differentiated through
two mechanisms: molecular size (due to the porous
nature of the layers) and chemical affinity (due to lig-
ands bound to the functionalized sensors). Molecules
with lower adsorption or weaker chemical affinity
travel faster and reach the sensors earlier, generating a
multi-peak resistance profile. Each peak corresponds
to a distinct molecule from the original mixture, as
illustrated in Figure 1.
This spatio-temporal detection at each layer gen-
erates a multidimensional signal as shown in Figure 2,
enabling multi-channel detection and analysis. Each
layer (or channel) captures different aspects of the
evaluated mixture, reflecting its diverse properties.
3.2 Experimental Setup
Two experiments (see Figure 3) are designed to differ-
entiate environments based on the presence of various
Deep Learning Characterization of Volatile Organic Compounds with Spectrometer-on-Card
199
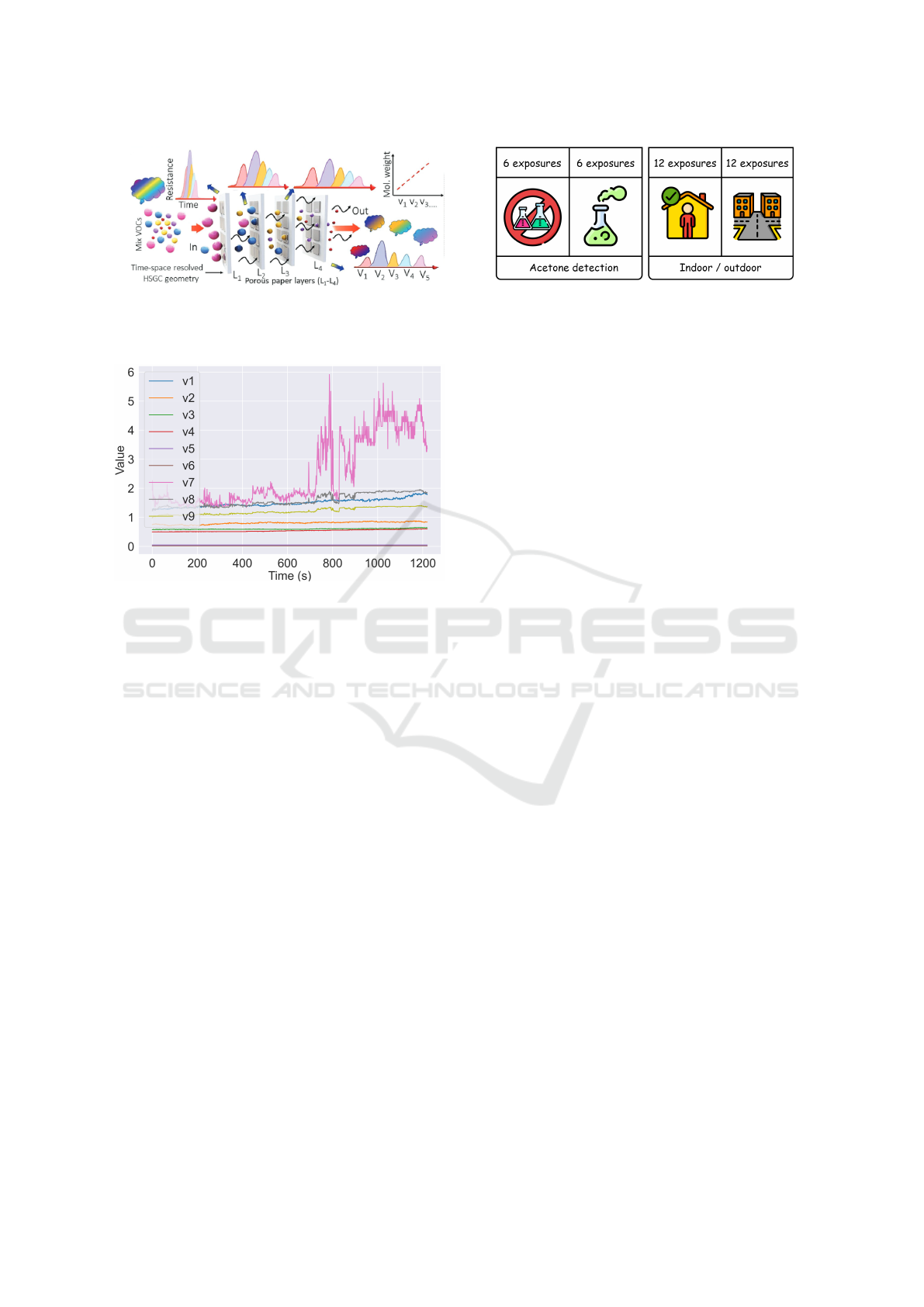
Figure 1: Graphical representation of the SPOC mechanism
for identifying different VOCs in a mixture. Figure taken
from Maity et al. (2022).
Figure 2: Example of raw signal captured in open air. The
x-axis represents the time interval of exposure (sampling
frequency was established to 1 Hz, hence the signals rep-
resent information from 1200 s. The y-axis represents the
resistance signal in omhs in each of the 8 channels.
VOC mixtures. The first experiment involves expos-
ing the SPOC to a semi-controlled environment with
a well-known source of VOCs (acetone). In contrast,
exposures without a direct VOC-emitting source are
captured in an indoor environment for artificial intel-
ligence (AI)-based characterization. The objective of
the first use case is to see the capabilities of the pro-
posed AI-driven approach to differentiate patterns in
the signals in an environment where there is a clear
presence of VOCs combined with a possible pres-
ence of unknown mixtures of compounds. This is
a more complex situation than a laboratory environ-
ment, which typically has clean air containing only
the selected compounds. A total of 12 samples have
been collected, each lasting about 30 minutes. Six of
these samples are exposed to an acetone dissolution
inside a closet, while the remaining six were exposed
to indoor air at a desk in the office. (see Table 1 for a
detailed description).
The second use case is designed to assess the ca-
pabilities of the proposed AI-based methodology (see
subsection 3.3) in a scenario widely studied in the
state-of-the-art for indoor and outdoor environment
characterization (Vardoulakis et al., 2020). Previous
Figure 3: Representation of the two use cases considered
in this study and the number of exposures taken for each
environment.
works indicate that, in general, the concentration of
VOCs is higher indoors. For that reason, the readings
of the device should be differentiable in both environ-
ments. In this phase, exposures collected in an office
environment are compared with those from a nearby
outdoor industrial area. The SPOC device was posi-
tioned at a designated office desk for indoor sampling,
while the outdoor sampling area was located close to
the office, near a lightly trafficked road and alongside
a river. For this experiment a total of 24 samples are
collected, each taking approximately 20 minutes: 12
samples from outside and 12 from inside (Table 1).
These experiments are designed to evaluate the
deep learning-based methodology across two differ-
ent use cases in semi-controlled and uncontrolled en-
vironments. The first use case is designed to evaluate
the characterization performance of the pipeline when
having a direct exposure to a VOC-emitting source.
In the second use case, the evaluation is carried with
signals obtained when the device is exposed to un-
known mixtures of compounds in both, indoor and
outdoor environment, as seen in previous works (Var-
doulakis et al., 2020). This second use case serves
to showcase the potential of the proposed methodol-
ogy for the characterization of environments closer to
real-world conditions.
3.3 Environment Characterization
Environment characterization is done through a time
series analysis of the exposures (E) captured in the
environments described in subsection 3.2 (Figure 3).
Each exposure ( j) with a duration of n seconds is di-
vided into windows (w) of size p (see equation (1)).
The whole exposure analysis process is depicted in
Figure 4,
E = {e
1
, ..., e
j
, ..., e
m
} (1)
W = {w
11
, ..., w
j(n−p+1)
, ..., w
m(n−p+1)
}
Then the window (w
i j
) is provided to the AI model
to assign a probability (p
ji
) for the i-th window indi-
cating the resemblance to a certain environment. The
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
200
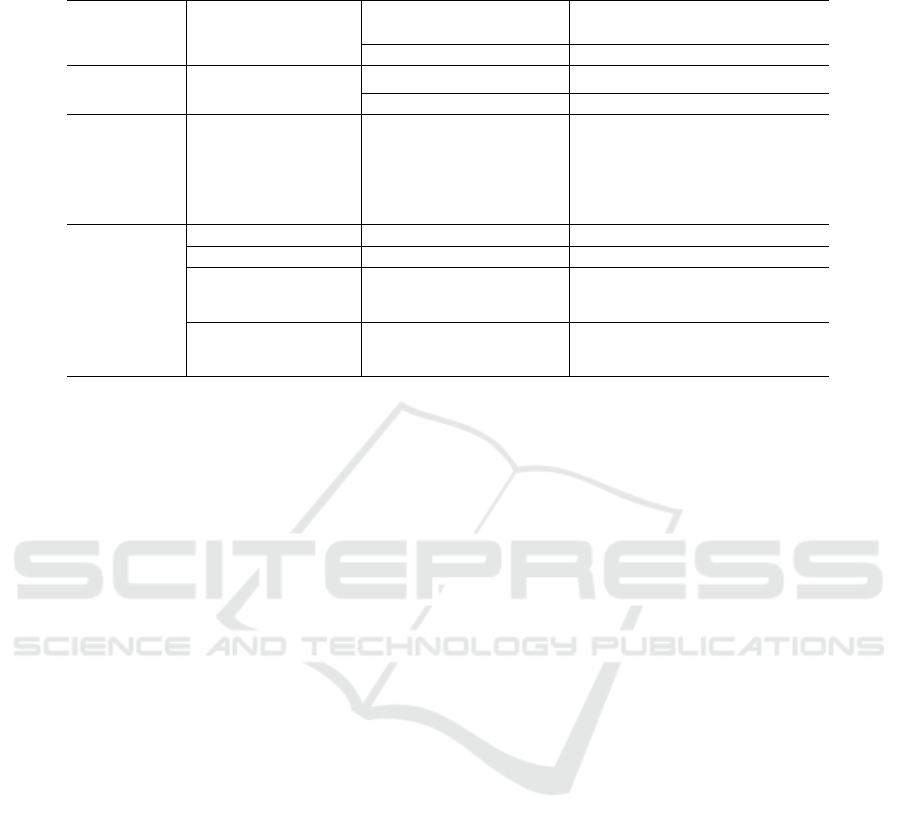
Table 1: Data description of the acetone detection and indoor / outdoor environment characterization use cases. For each use
case, the features used to train the proposed artificial intelligence (AI) models are detailed after applying the sliding window.
Group Features
Acetone detection Indoor / outdoor
characterization
Yes No Total Indoor Outdoor Total
Count
# Exposures 6 6 12 12 12 24
# Variables 9 channels 9 channels
Duration (s)
Mean 1.821 1.823 1.822 1.502 1.215 1.358
Std 35,03 34,06 32,25 695,00 63,66 504,40
Min 1.772 1.793 1.772 524 1.022 524
Max 1.881 1.886 1.886 3.292 1.263 3.292
AI
Window size 25 25
Step 1 1
Train
# Instances 7.120 7.171 14.291 10.662 9.457 20.119
# Exposures 4 4 8 7 8 15
Test
# Instances 3.662 3.600 7.262 7.056 4.827 11.883
# Exposures 2 2 4 5 4 9
proposed methodology is flexible and can have a vary-
ing number of layers (l) as input.
AI : P
p
× P
l
→ [0, 1] (2)
w
jn
= {v
j1
, ..., v
jl
} → AI(w
ji
) = p
ji
With the list of probabilities (P
j
) assigned to each of
the windows from the j-th exposure, the mean score
is obtained, indicating on average, the resemblance of
the whole exposure with respect to the specific envi-
ronment. Finally, the predicted label ( ˆc
j
) for the j-
th exposure is obtained by rounding the mean score
to either 0 or 1 (see equation (3)). Note that the
split of the exposure in smaller windows generates
a larger number of instances and smaller sequences.
This enables the training of more complex models,
such as recurrent neural networks (RNNs), and re-
quires a lower number of exposures for training. Sim-
ilar approaches have been proposed in previous works
for the classification of long sequences with smaller
windows (Dietterich, 2002; Senthil and Suseendran,
2018; Etemad et al., 2020).
P
j
= {AI(w
ji
)}
n
i=1
(3)
ˆc
j
= Round(Mean(P
j
))
The AI models considered for the environment
characterization task include several algorithms as
well as deep learning-based methods. The first
group of machine learning methods includes: K-
Neares Neighbours (KNN), Support Vector Machine
(SVM), Decision Tree (DT), Stochastic Gradient De-
scent (SGD) and Neural Networks (NN) (Boateng
et al., 2020). The SVM classifier contains a radial
basis function kernel. Note that these algorithms are
not able to have as input two-dimensional windows,
for that reason, the window size (p) is set to one.
This setting implies that the classification is done for
each second, attending combinations between the val-
ues read for each of the layers and missing tempo-
ral patterns in the analysis. The second group of
models are based on recurrent neural networks RNNs
(Medsker et al., 2001), which consider large win-
dow sizes and are able to learn spatio-temporal pat-
terns in the signals. More specifically, three varia-
tions of RNNs are employed (see Figure 5): RNN,
Bidirectional RNN (BiRNN) and RNN with a built-
in attention mechanism (AttentionRNN). The RNN
is composed of Long Short-Term Memory (LSTM)
(Hochreiter, 1997) cells that are able to capture infor-
mation in further timesteps.
For the RNN, an additional set of parameters must
be specified such as the optimizer function, which de-
fines how the parameters are updated, the number of
epochs (i.e. the number of passes through the entire
dataset), dropout (i.e. randomly ignores the speci-
fied percentage of neurons from the previous layer to
avoid overfitting) and the learning rate. In addition,
for the Adam optimizer (Bock and Weiß, 2019), β1
and β2 have to be set which are the exponential decay
rates for the first and second moment estimates, re-
spectively. Finally, the batch size is also tuned which
defines the number of instances to introduce in the
network in each step within an epoch.
For the traditional machine learning algorithms,
python’s scikit-learn (Pedregosa et al., 2011) library
is used. In the case of NN, RNN, BiRNN and At-
tentionRN, keras (Gulli and Pal, 2017) is the frame-
work used for the implementation of the proposed
models. The hyperparameters of these deep learning-
based models are automatically adjusted with the Op-
Deep Learning Characterization of Volatile Organic Compounds with Spectrometer-on-Card
201
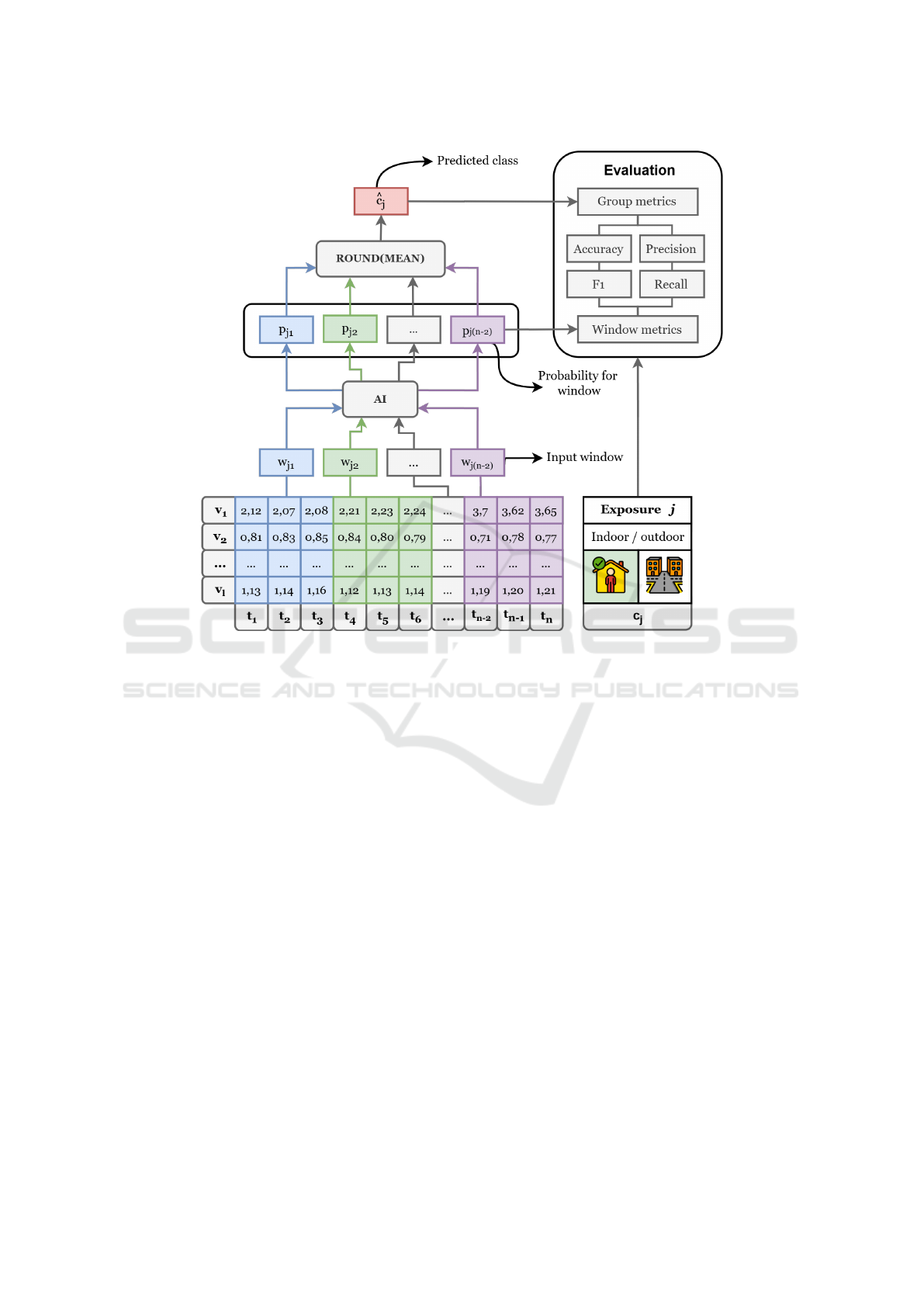
Figure 4: Diagram of the environment characterization process given an exposure. In this example, input data is divided
into windows of size three for indoor and outdoor classification. For each window, an AI model assigns a probability of
resemblance to the outdoor environment. The mean and round functions are then applied to these probabilities to classify the
entire exposure. Evaluation metrics are used to compare the input and predicted data.
tuna (Akiba et al., 2019) framework. Among those
hyperparameters that are optimized by this frame-
work: window size, dropout rate, the RNN number
of neurons, number of feedforward layers, number of
neurons in each feedforward layer. Description of the
data used for the proposed AI models is shown in Ta-
ble 1 after selecting the best window size for the pro-
posed use cases.
3.4 Evaluation
The evaluation of the environment characterization
performance is done in three ways: window metrics,
group metrics and mean probabilities. For both, win-
dow and group metrics, the accuracy and F1 are com-
puted (Dalianis and Dalianis, 2018), being the max-
imum value 100%, which indicates a perfect charac-
terization. Both metrics measure how close the pre-
diction is to the current label. As the exposure is split
into smaller windows, each window is assigned the
same label as the whole exposure. That is, the smaller
windows come from the same environment as the ex-
posure. For each window, the accuracy and F1 scores
are computed, comparing the label of the window and
the label of the whole exposure.
For group metrics, the probabilities of all the win-
dows within the exposure are averaged and rounded,
comparing the predicted class of the exposure with the
actual class. Group metrics indicate the percentage of
exposures in the test set that are correctly classified.
Mean probabilities computed for the acetone detec-
tion use case are differentiated for label 1 (e.g. no
acetone exposure) and label 2 (e.g. acetone exposure)
exposures, obtaining the mean probability assigned
across all the windows inside the exposure. The same
happens for the second use case, where the exposures
captured indoors are assigned with label 1 and those
captured outdoors with label 2.
The selected evaluation scheme is 3-fold cross val-
idation (Berrar et al., 2019), which splits the data into
three folds, and at each time, two folds are used for
training and the remaining one for testing. This en-
sures that the results are not conditioned to the spe-
cific train/test data partition. For that reason, for each
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
202
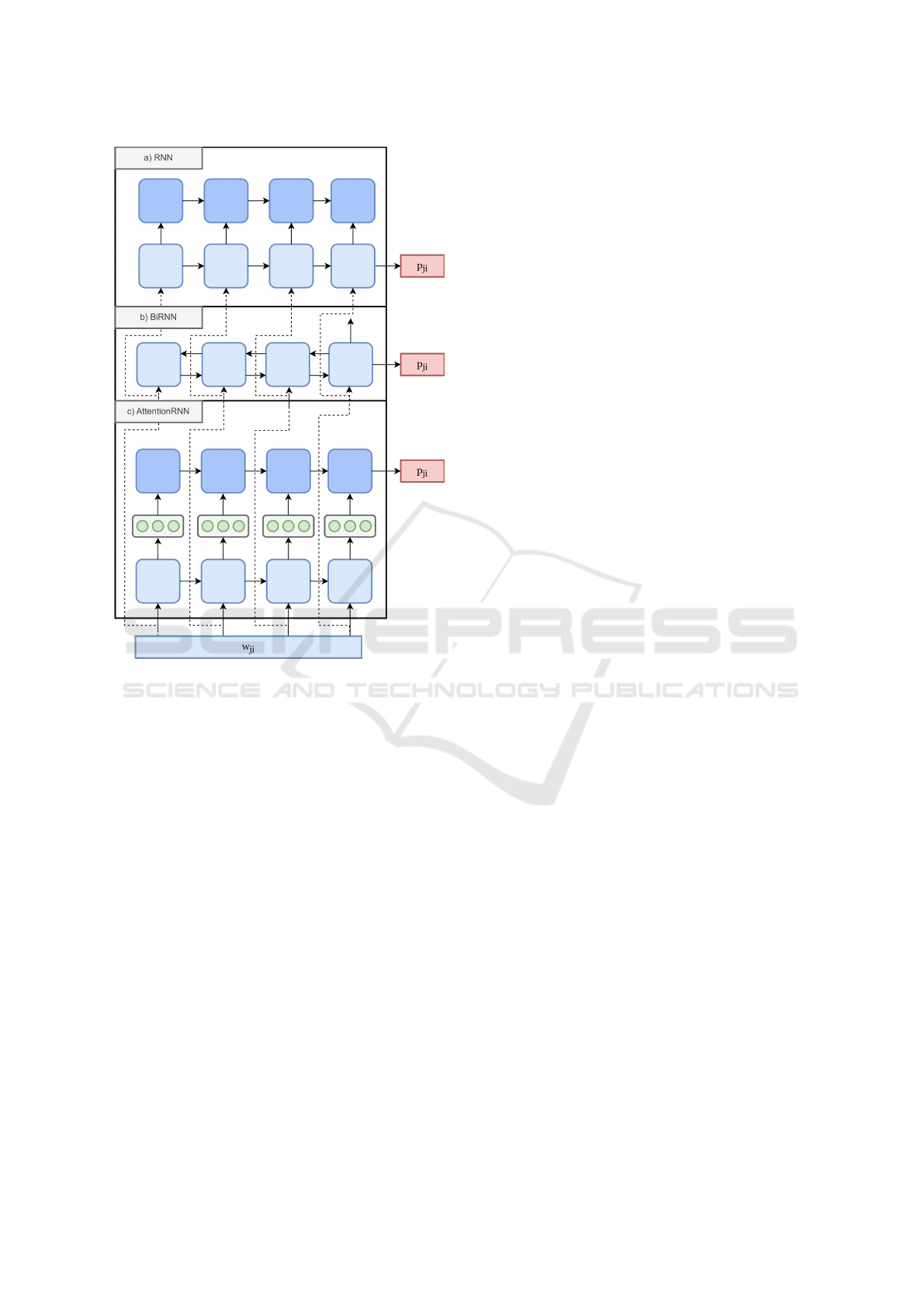
Figure 5: Representation of different recurrent neural net-
work architectures employed in this study: (a) RNN, (b)
BiRNN, and (c) AttentionRNN. For each experiment, one
of these architectures is selected independently and the
number of seconds in the input (p) is tuned to achieve the
best environment characterization performance. In this ex-
ample, the window size (p) is set to four. All the classifiers
have as input a window (w
ji
) and as output a probability
(p
ji
). Note that the algorithms are not combined, but share
the same input and output format.
evaluation metric, the mean value and the standard de-
viation are provided. In addition, the data is stratified,
that is, in the test set half of the exposures are always
from the first environment (label 1) and the other half
from the second environment (label 2).
4 RESULTS
This section presents the findings from the exper-
iments conducted for environment characterization.
First, in subsection 4.1 the performance of the pro-
posed methodology in characterizing environments
based on mixtures of VOCs is detailed, highlighting
key metrics such as accuracy for both use cases. Fol-
lowing this, in subsection 4.2 a comprehensive discus-
sion of these results is provided, contextualizing their
significance and exploring potential implications for
future applications.
4.1 Environment Characterization
In this section, a set of experiments is presented
for environment characterization in two different use
cases: acetone detection and indoor/outdoor charac-
terization. The main objective is to see if the method-
ology depicted in Figure 4 is able to distinguish the
two environments. The characterization performance
for both use cases may differ as the first one has a di-
rect source of VOC. Classification results are shown
in Table 2.
Table 2 shows the classification results by means
of window and group metrics for acetone detection
and indoor/outdoor characterization. For acetone de-
tection, the best mean window metrics are achieved
by the BiRNN model, with a maximum accuracy of
97,24% and a F1 of 97,25%. Group metrics show that
the four exposures of the test set are correctly clas-
sified for the three RNN-based models, being able to
differentiate the two exposures that were exposed to
acetone. The results obtained by the BiRNN are close
to those obtained by the RNN model for the win-
dow metrics, with a 95,50% of accuracy and a F1 of
95,51%. Regarding the mean probability assigned to
those exposures exposed to an acetone source (label
2), the BiRNN model provides a 99,10% for the ex-
posures in the test set across the different folds, com-
pared to 93,91% achieved by RNN, showcasing a high
precision for BiRNN. This precision seems to affect
the mean probability for those cases where there is no
acetone source (label 1), being the lowest for RNN
with 2,73%.
A comparison of the window metrics between
RNN, the best RNN-based model, with NN, which
is the best model from those that have one as window
size, shows a relative increase in terms of mean ac-
curacy of 15,36% and 14,53% for mean F1. Group
metrics show that the mean accuracy for NN is 83,3%
whereas for RNN is 100%. Considering that the num-
ber of exposures in the test set is 3, on average, the NN
classifies one or two exposures out of three whereas
the RNN is able to correctly characterize the three ex-
posures. These results indicate that the temporal pat-
terns of the signals have a high influence on the envi-
ronment characterization capabilities of the proposed
model.
For indoor / outdoor environments characteriza-
tion, the best score is also achieved by the BiRNN
with a mean accuracy of 92,37% and 92,38% in terms
Deep Learning Characterization of Volatile Organic Compounds with Spectrometer-on-Card
203
Table 2: Results for environment characterization through the classification of the exposures in the test set. The scores for the
evaluation metrics are divided for each of two use cases shown in Figure 2 and given for the window and group metrics. The
best results for each use case are marked in bold.
Window metrics Groups metrics Mean probabilities
Use case Model Accuracy F1 Accuracy F1 Label 1 Label 2
Acetone detection
conditions
KNN 53,03% (±2,47) 50,79% (±19,36) 54,17% (±37,69) 43,33% (±30,15) 16,66% (±0,00) 17,00% (±0,00)
RBF SVM 61,06% (±15,47) 61,01% (±12,43) 54,17% (±37,69) 43,33% (±30,15) 39,04% (±0,00) 38,80% (±0,00)
Decision Tree 63,97% (±1,88) 62,52% (±5,58) 72,92% (±18,84) 66,67% (±0,00) 37,53% (±0,00) 66,67% (±0,10)
SGD 61,64% (±21,57) 60,75% (±15,57) 54,17% (±37,69) 43,33% (±30,15) 12,73% (±3,62) 31,51% (±10,86)
NN 84,29% (±9,27) 84,91% (±8,44) 83,33% (±19,46) 82,22% (±13,73) 18,65% (±27,30) 87,05% (±13,00)
RNN 95,50% (±7,68) 95,51% (±7,65) 100,00% (±0,00) 100,00% (±0,00) 2,73% (±4,51) 93,91% (±10,52)
BiRNN 97,24 % (± 4,75) 97,25% (±4,74) 100,00% (±0,00) 100,00% (±0,00) 4,49% (±7,78) 99,10% (±1,52)
AttentionRNN 90,45% (±9,65) 90,65% (±9,36) 100,00% (±0,00) 100,00% (±0,00) 3,93% (±5,28) 85,09% (±19,13)
Indoor / outdoor
characterization
KNN 65,44% (±13,29) 64,17% (±4,49) 66,67% (±24,62) 62,50% (±9,23) 52,20% (±0,00) 83,77% (±0,00)
RBF SVM 63,05% (±13,88) 61,58% (±5,05) 50,00% (±12,31) 48,57% (±6,33) 55,33% (±0,00) 82,21% (±0,00)
Decision Tree 59,45% (±12,29) 56,49% (±7,88) 66,67% (±0,00) 62,50% (±9,23) 65,11% (±0,59) 85,16% (±0,20)
SGD 67,01% (±14,66) 65,54% (±5,31) 66,67% (±24,62) 62,50% (±9,23) 46,04% (±8,99) 86,26% (±0,87)
NN 89,58% (±5,73) 89,68% (±5,55) 91,66% (±9,73) 91,53% (±6,33) 8,86% (±10,20) 86,24% (±14,49)
RNN 91,86% (±5,54) 91,87% (±5,54) 95,83% (±8,14) 95,77% (±6,29) 7,84% (±7,91) 89,91% (±8,49)
BiRNN 92,37% (±4,78) 92,38% (±4,77) 95,83% (±8,14) 95,77% (±6,29) 6,48% (±6,20) 89,65% (±7,12)
AttentionRNN 88,66% (±6,17) 88,71% (±6,10) 95,83% (±8,14) 95,77% (±6,29) 9,28% (±6,41) 84,70% (±9,95)
of mean F1. Group metrics achieve a mean score of
95,38% in terms of accuracy and 95,77% by means of
mean F1, which implies that from eight exposures in
the test set, on average, 7 to 8 of them are correctly
classified. These results are close to those obtained
by the RNN, with 91,86% and 91,87% of mean ac-
curacy and F1, respectively. The mean probability
assigned to outdoor exposures (label 2) is very sim-
ilar for both RNN and BiRNN, being the mean value
higher for the RNN with 89,91% compared to 89,65%
but the standard deviation is lower for BiRNN. For in-
door exposures (label 1) the mean probability is lower
for BiRNN with a 6,48% compared to the 7,84% pro-
vided by the RNN.
When comparing the best model that uses one as
window size (NN) and the best RNN-based model
(BiRNN), a relative increase of 3,11% is achieved in
terms of mean accuracy and 3,01% in terms of mean
F1. Group metrics for both NN show that, with a
mean accuracy of 91,66% and a standard deviation
of 9,73, at most one exposure is incorrectly classi-
fied. These results, compared to those obtained in the
acetone detection use case, also show a difference in
performance when considering the time component of
the SPOC data, being higher for RNN-based models.
As a conclusion, the RNN-based models have
achieved a remarkable increase in performance com-
pared to those models that do not take into account the
time domain of the input data. In addition, the best
model has been BiRNN for both use cases, achiev-
ing a 95,25% mean accuracy for the acetone detec-
tion scenario. For the indoor and outdoor environ-
ment characterization use case the BiRNN achieves
a 92,37% of mean accuracy. In the acetone detec-
tion use case all the exposures are correctly classi-
fied, whereas in the indoor and outdoor characteriza-
tion use case, only one exposure is incorrectly classi-
fied. These results show the capabilities of the SPOC
device combined with the proposed methodology for
environment characterization. Optuna framework has
proven to be essential to adjust different hyperparam-
eters and optimize model performance, with the num-
ber of trials to 25 and the NSGA-III algorithm (Deb
and Jain, 2014) as the optimization function.
4.2 Discussion
This study proposes an AI-driven methodology that
incorporates deep learning techniques to character-
ize environments using signals captured by the SPOC
device under two different use cases: acetone detec-
tion and indoor / outdoor characterization. The first
one has a known source of VOCs (acetone), and the
second one is exposed to lower concentration of un-
known mixtures of compounds. Although the first
case directly exposes the device to acetone, other
VOCs may also be present in the air, with acetone
concentration being significantly higher. Given the
high mean classification accuracy of 97,24%, it would
be valuable to compare the signals from other VOCs
to analyze potential differences in the SPOC’s read-
ings.
The motivation for the second use case is sup-
ported by previous research reporting significant dif-
ferences between indoor and outdoor environments,
with VOC concentrations generally being higher in-
doors (Vardoulakis et al., 2020). For this use case, the
model’s performance decreases by around five points
in terms of mean accuracy, which may be attributed to
the characterization of an uncontrolled environment
compared to the semi-controlled environment of the
first use case. In contrast, when measurements are
taken in uncontrolled environments, along with the
presence of environmental noise, the concentration of
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
204

VOCs may be significantly reduced. Another factor
affecting accuracy could be situations where the in-
door and outdoor environments are not differentiable,
possibly due to cleaner indoor air or airflow from the
outside. Thus, exposure classification errors may in-
dicate changes in the mixtures of VOCs in environ-
ments monitored by the SPOC device.
The comparison of results achieved by the models
in Section 4 primarily considers the mean scores of
the proposed metrics. Additionally, a paired t-test was
performed using the standard deviation across the dif-
ferent folds. The results provide no evidence of a sta-
tistically significant difference in performance among
the recurrent neural network-based models. There-
fore, selecting the best model may vary depending
on the score for each use case, computational time,
and preferred mean probability. For example, in the
acetone detection use case, if better detection of pos-
itive cases is prioritized, the BiRNN performs better
(99,10%). However, if the goal is to monitor normal
environmental conditions and reduce false positives,
the RNN may be preferable with a mean probability
of 2,73%. In any case, RNN-based models signifi-
cantly outperform those models limited to a window
size of one (p < 0, 005), demonstrating the advantages
of considering the time domain of the signals.
Future work should consider expanding the num-
ber of environments used for characterization and
evaluating the SPOC and the proposed methodology
on more complex tasks. A deeper analysis of the sig-
nals would be valuable to understand the influence of
each layer in the characterization process, as well as
any patterns indicative of specific VOCs, leveraging
the capabilities of this device compared to previous
approaches like the e-nose.
The proposed methodology has proven to be ef-
fective for environment characterization based on
VOC mixtures using just a few hours of data for
model training. This is achieved by splitting the expo-
sure into windows, generating thousands of instances
for training deep learning models. Additionally, this
solution can be used for real-time monitoring, provid-
ing a probability every second by analyzing the last
25 seconds of data. Therefore, this approach could
potentially be used for other air quality assessments
or the detection of specific health conditions based on
air from exhaled breath. The only requirement would
be to capture a few hours of data to retrain the model
for characterization, eliminating the need for calibra-
tion or new sensors. Then, the predictions could be
provided at each second, depending on the hardware
provided for the inference.
5 CONCLUSIONS
In this work, we propose and evaluate an AI-
based pipeline for environment characterization that
compares several machine learning and deep learn-
ing classifiers, including recurrent neural networks
(RNNs). To assess the capabilities of our approach,
we have captured SPectrometer-On-Card (SPOC)
data in two different use cases. In the first use case,
this pipeline is used for the characterization of an en-
vironment with a direct source of VOC (acetone). In
the second use case, the evaluation is carried out in
indoor and outdoor environments (a common applica-
tion in the state-of-the-art), where the concentration
of unknown mixtures of compounds is lower com-
pared to the first use case. With that aim, our approach
splits the signal into smaller windows and compares
different machine learning algorithms for environ-
ment classification based on SPOC signals generated
as a response to the exposition of complex mixtures of
compounds. The probabilities for these windows are
averaged across the entire exposure and a final predic-
tion is given. The results show that the bidirectional
recurrent neural network (BiRNN) achieves the best
performance with a 97,24% mean accuracy in win-
dow classification and all the exposures are correctly
characterized. For indoor and outdoor characteriza-
tion use cases, a mean accuracy of 92,97% is achieved
for window classification with seven exposures out of
eight correctly classified.
The SPOC device combined with the proposed
data analysis methodology and deep learning mod-
els has been able to correctly characterize and differ-
entiate environments based on complex mixtures of
compounds that flow through the device. In addition,
the BiRNN model is able to provide a prediction each
second by looking at the previous 25 seconds, extend-
ing its use for real-time monitoring of complex envi-
ronments. This device does not need to be calibrated
and is not limited to specific VOCs, delineating its
potential for other use cases such as disease detection
(e.g. cancer), leaks detection in industry, the detec-
tion of uncompleted combustion in urban areas and
environmental monitoring.
ACKNOWLEDGEMENTS
We would like to thank Fundaci
´
on Vicomtech for
funding project DYNASPECTRUM under the Multi-
Area Internal Projects program. We would also like
to express our gratitude to Technion Institute of Tech-
nology for letting us use the SPectrometer-On-Card
(SPOC) device. This research work has also been in-
Deep Learning Characterization of Volatile Organic Compounds with Spectrometer-on-Card
205

spired by the LUCIA EU project (Grant agreement
ID: 101096473) and the necessity to identify VOC re-
lated biomarkers for prompt detection of lung cancer.
Also many thanks to the ENACT EU project (Grant
agreement ID: 101157151) for letting us understand
the importance of air quality in non-communicable
diseases.
REFERENCES
Akiba, T., Sano, S., Yanase, T., Ohta, T., and Koyama, M.
(2019). Optuna: A next-generation hyperparameter op-
timization framework. In Proceedings of the 25th ACM
SIGKDD International Conference on Knowledge Dis-
covery & Data Mining, pages 2623–2631. ACM.
Anzivino, R., Sciancalepore, P. I., Dragonieri, S., Quaranta,
V. N., Petrone, P., Petrone, D., Quaranta, N., and Carpag-
nano, G. E. (2022). The role of a polymer-based e-nose
in the detection of head and neck cancer from exhaled
breath. Sensors, 22(17):6485.
Berrar, D. et al. (2019). Cross-validation.
Boateng, E. Y., Otoo, J., and Abaye, D. A. (2020). Ba-
sic tenets of classification algorithms k-nearest-neighbor,
support vector machine, random forest and neural net-
work: A review. Journal of Data Analysis and Informa-
tion Processing, 8(4):341–357.
Bock, S. and Weiß, M. (2019). A proof of local convergence
for the adam optimizer. In 2019 international joint con-
ference on neural networks (IJCNN), pages 1–8. IEEE.
Dalianis, H. and Dalianis, H. (2018). Evaluation metrics
and evaluation. Clinical Text Mining: secondary use of
electronic patient records, pages 45–53.
Danieli, M. G., Casciaro, M., Paladini, A., Bartolucci, M.,
Sordoni, M., Shoenfeld, Y., and Gangemi, S. (2024). Ex-
posome: Epigenetics and autoimmune diseases. Autoim-
munity Reviews, page 103584.
Deb, K. and Jain, H. (2014). An evolutionary many-
objective optimization algorithm using reference-point-
based nondominated sorting approach, part i: Solving
problems with box constraints. IEEE Transactions on
Evolutionary Computation, 18(4):577–601.
Deshmukh, S., Kamde, K., Jana, A., Korde, S., Bandyopad-
hyay, R., Sankar, R., Bhattacharyya, N., and Pandey, R.
(2014). Calibration transfer between electronic nose sys-
tems for rapid in situ measurement of pulp and paper in-
dustry emissions. Analytica chimica acta, 841:58–67.
Dietterich, T. G. (2002). Machine learning for sequen-
tial data: A review. In Structural, Syntactic, and Sta-
tistical Pattern Recognition: Joint IAPR International
Workshops SSPR 2002 and SPR 2002 Windsor, Ontario,
Canada, August 6–9, 2002 Proceedings, pages 15–30.
Springer.
Dincer, F., Odabasi, M., and Muezzinoglu, A. (2006).
Chemical characterization of odorous gases at a landfill
site by gas chromatography–mass spectrometry. Journal
of chromatography A, 1122(1-2):222–229.
Dutta, D., Chong, N. S., and Lim, S. H. (2018). Endogenous
volatile organic compounds in acute myeloid leukemia:
origins and potential clinical applications. Journal of
Breath Research, 12(3):034002.
Elbir, T., Cetin, B., Cetin, E., Bayram, A., and Odabasi, M.
(2007). Characterization of volatile organic compounds
(vocs) and their sources in the air of izmir, turkey. Envi-
ronmental Monitoring and Assessment, 133:149–160.
Erzin, G. and G
¨
ul
¨
oks
¨
uz, S. (2021). The exposome paradigm
to understand the environmental origins of mental disor-
ders. Alpha Psychiatry, 22(4):171.
Etemad, M., Etemad, Z., Soares, A., Bogorny, V., Matwin,
S., and Torgo, L. (2020). Wise sliding window segmenta-
tion: A classification-aided approach for trajectory seg-
mentation. In Advances in Artificial Intelligence: 33rd
Canadian Conference on Artificial Intelligence, Cana-
dian AI 2020, Ottawa, ON, Canada, May 13–15, 2020,
Proceedings 33, pages 208–219. Springer.
Fialkov, A. B., Lehotay, S. J., and Amirav, A. (2020).
Less than one minute low-pressure gas chromatography-
mass spectrometry. Journal of Chromatography A,
1612:460691.
Gulli, A. and Pal, S. (2017). Deep learning with Keras.
Packt Publishing Ltd.
Ho, S. S. H., Wang, L., Chow, J. C., Watson, J. G., Xue, Y.,
Huang, Y., Qu, L., Li, B., Dai, W., Li, L., et al. (2018).
Optimization and evaluation of multi-bed adsorbent tube
method in collection of volatile organic compounds. At-
mospheric Research, 202:187–195.
Hochreiter, S. (1997). Long short-term memory. Neural
Computation MIT-Press.
Katsouyanni, K. (2003). Ambient air pollution and health.
British medical bulletin, 68(1):143–156.
Kumar, A. and V
´
ıden, I. (2007). Volatile organic com-
pounds: sampling methods and their worldwide profile
in ambient air. Environmental monitoring and assess-
ment, 131:301–321.
Lai, S. Y., Deffenderfer, O. F., Hanson, W., Phillips, M. P.,
and Thaler, E. R. (2002). Identification of upper respi-
ratory bacterial pathogens with the electronic nose. The
Laryngoscope, 112(6):975–979.
Langford, V. S., Graves, I., and McEwan, M. J. (2014).
Rapid monitoring of volatile organic compounds: a com-
parison between gas chromatography/mass spectrometry
and selected ion flow tube mass spectrometry. Rapid
Communications in Mass Spectrometry, 28(1):10–18.
Li, C., Li, Q., Tong, D., Wang, Q., Wu, M., Sun, B., Su,
G., and Tan, L. (2020). Environmental impact and health
risk assessment of volatile organic compound emissions
during different seasons in beijing. Journal of Environ-
mental Sciences, 93:1–12.
Li, Q.-L., Yuan, D.-X., and Lin, Q.-M. (2004). Evalua-
tion of multi-walled carbon nanotubes as an adsorbent
for trapping volatile organic compounds from environ-
mental samples. Journal of Chromatography A, 1026(1-
2):283–288.
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
206

Li, Y., Wei, X., Zhou, Y., Wang, J., and You, R. (2023). Re-
search progress of electronic nose technology in exhaled
breath disease analysis, microsystems& nanoengi-
neering, 9, 129.
Licen, S., Di Gilio, A., Palmisani, J., Petraccone, S.,
de Gennaro, G., and Barbieri, P. (2020). Pattern recogni-
tion and anomaly detection by self-organizing maps in a
multi month e-nose survey at an industrial site. Sensors,
20(7):1887.
Liu, L., Li, W., He, Z., Chen, W., Liu, H., Chen, K., and Pi,
X. (2021). Detection of lung cancer with electronic nose
using a novel ensemble learning framework. Journal of
Breath Research, 15(2):026014.
Liu, T., Guo, L., Wang, M., Su, C., Wang, D., Dong, H.,
and Wu, W. (2023). Review on algorithm design in elec-
tronic noses: Challenges, status, and trends. Intelligent
Computing, 2:0012.
Machado, R. F., Laskowski, D., Deffenderfer, O., Burch,
T., Zheng, S., Mazzone, P. J., Mekhail, T., Jennings, C.,
Stoller, J. K., Pyle, J., et al. (2005). Detection of lung
cancer by sensor array analyses of exhaled breath. Amer-
ican journal of respiratory and critical care medicine,
171(11):1286–1291.
Maity, A., Milyutin, Y., Maidantchik, V. D., Pollak, Y. H.,
Broza, Y., Omar, R., Zheng, Y., Saliba, W., Huynh, T.-
P., and Haick, H. (2022). Ultra-fast portable and wear-
able sensing design for continuous and wide-spectrum
molecular analysis and diagnostics. Advanced Science,
9(34):2203693.
Medsker, L. R., Jain, L., et al. (2001). Recurrent neural
networks. Design and Applications, 5(64-67):2.
Nicolas, J., Romain, A.-C., Wiertz, V., Maternova, J., and
Andr
´
e, P. (2000). Using the classification model of an
electronic nose to assign unknown malodours to environ-
mental sources and to monitor them continuously. Sen-
sors and Actuators B: Chemical, 69(3):366–371.
Pang, X., Nan, H., Zhong, J., Ye, D., Shaw, M. D., and
Lewis, A. C. (2019). Low-cost photoionization sensors
as detectors in gc× gc systems designed for ambient
voc measurements. Science of The Total Environment,
664:771–779.
Pedregosa, F., Varoquaux, G., Gramfort, A., Michel, V.,
Thirion, B., Grisel, O., Blondel, M., Prettenhofer, P.,
Weiss, R., Dubourg, V., Vanderplas, J., Passos, A., Cour-
napeau, D., Brucher, M., Perrot, M., and Duchesnay, E.
(2011). Scikit-learn: Machine learning in Python. Jour-
nal of Machine Learning Research, 12:2825–2830.
Persaud, K. C. (2005). Medical applications of odor-sensing
devices. The international journal of lower extremity
wounds, 4(1):50–56.
Rabehi, A., Helal, H., Zappa, D., and Comini, E. (2024).
Advancements and prospects of electronic nose in vari-
ous applications: A comprehensive review. Applied Sci-
ences, 14(11):4506.
Saasa, V., Beukes, M., Lemmer, Y., and Mwakikunga, B.
(2019). Blood ketone bodies and breath acetone analysis
and their correlations in type 2 diabetes mellitus. Diag-
nostics, 9(4):224.
Scheepers, P. T., Van Wel, L., Beckmann, G., and Anzion,
R. B. (2017). Chemical characterization of the indoor air
quality of a university hospital: penetration of outdoor
air pollutants. International Journal of Environmental
Research and Public Health, 14(5):497.
Senthil, D. and Suseendran, G. (2018). Efficient time series
data classification using sliding window technique based
improved association rule mining with enhanced support
vector machine. International Journal of Engineering &
Technology, 7(3.3):218.
Smolander, M. (2003). The use of freshness indicators
in packaging. In Ahvenainen, R., editor, Novel Food
Packaging Techniques, Woodhead Publishing Series in
Food Science, Technology and Nutrition, pages 127–
143. Woodhead Publishing.
Soni, V., Singh, P., Shree, V., and Goel, V. (2018). Effects of
vocs on human health. Air pollution and control, pages
119–142.
Sun, X., Shao, K., and Wang, T. (2016). Detection of
volatile organic compounds (vocs) from exhaled breath
as noninvasive methods for cancer diagnosis. Analytical
and bioanalytical chemistry, 408:2759–2780.
Tanaka, P. L., Oldfield, S., Neece, J. D., Mullins, C. B., and
Allen, D. T. (2000). Anthropogenic sources of chlorine
and ozone formation in urban atmospheres. Environmen-
tal science & technology, 34(21):4470–4473.
Vardoulakis, S., Giagloglou, E., Steinle, S., Davis, A.,
Sleeuwenhoek, A., Galea, K. S., Dixon, K., and Craw-
ford, J. O. (2020). Indoor exposure to selected air pollu-
tants in the home environment: a systematic review. In-
ternational journal of environmental research and public
health, 17(23):8972.
Vermeulen, R., Schymanski, E. L., Barab
´
asi, A.-L., and
Miller, G. W. (2020). The exposome and health: Where
chemistry meets biology. Science, 367(6476):392–396.
Wang, P. and Zhao, W. (2008). Assessment of ambient
volatile organic compounds (vocs) near major roads in
urban nanjing, china. Atmospheric Research, 89(3):289–
297.
Won, S. R., Ghim, Y. S., Kim, J., Ryu, J., Shim, I.-K.,
and Lee, J. (2021). Volatile organic compounds in un-
derground shopping districts in korea. International
Journal of Environmental Research and Public Health,
18(11):5508.
Woolfenden, E. (2010). Sorbent-based sampling methods
for volatile and semi-volatile organic compounds in air.
part 2. sorbent selection and other aspects of optimizing
air monitoring methods. Journal of Chromatography A,
1217(16):2685–2694.
Zhang, X., Tang, B., Yang, X., Li, J., Cao, X., and Zhu, H.
(2024). Risk assessment of volatile organic compounds
from aged asphalt: Implications for environment and hu-
man health. Journal of Cleaner Production, 440:141001.
Deep Learning Characterization of Volatile Organic Compounds with Spectrometer-on-Card
207
