
Evidence on Robotic Prostatectomy: Discussing the Limitations of
Real-World Data
Maciej Dzik
a
, Kacper Mucha and Monika Zaleska
Agency for Health Technology Assessment and Tariff System, Warsaw, Poland
Keywords: Prostate Cancer, Radical Prostatectomy, Real-World Evidence.
Abstract: INTRODUCTION: The aim of this research is to evaluate Real-World Data (RWD) related to prostatectomy
outcomes for prostate cancer with a focus on identifying potential biases and data limitations. METHODS:
This study was based on the financial records collected in the database the Polish National Health Fund. The
sample included 14,376 patients who underwent robot-assisted radical prostatectomy (RARP), laparoscopic
radical prostatectomy (LRP) or conventional radical prostatectomy (CRP) between 20 September 2022 and
31 December 2023. Comparative analysis focused exclusively on the duration of hospitalisation. Additional
outcomes included mortality. RESULTS: In total 6,609 patients had RARP. RARP compared to both CRP
and LRP was associated with a reduction in inpatient days by 2.81 (95% CI: -2.98, -2.65; p<0.0001) and 0.91
(95% CI: -1.02, -0.8; p<0.0001) respectively. Patient admitted as emergencies had statistically longer hospital
stays by 1.03 days (p<0.0001). CONCLUSIONS: The overall length of hospitalization has been reduced, but
interpreting the results obtained from RWD in terms of relative benefits is challenging. The analysis faced
several challenges, including interpreting outcome measures and validating their clinical significance,
handling outliers, addressing non-random assignment, and accounting for unobserved covariates. These
limitations underscore the need for further research to enhance the quality of comparisons.
1 INTRODUCTION
The aim of this research is to evaluate Real-World Data
(RWD) related to prostatectomy outcomes for prostate
cancer with a focus on identifying potential biases and
data limitations. This study builds on the previous
work in the field of robotic prostatectomy by Dzik et
al. (2024). Early data from the first few months of
financial records from the Polish National Health Fund
indicated the Robot-Assisted Radical Prostatectomy
(RARP) was associated with shorter hospital stays and
fewer transfusions of blood products than conventional
prostatectomy. In this study we focus on the duration
of hospitalization to highlight challenges in the
interpretation of the outcomes.
2 BACKGROUND
RWD is defined as data related to patient health,
experiences, or care delivery that is collected outside
a
https://orcid.org/0000-0001-9069-7566
of controlled clinical trials (NICE, 2022). RWD is of
significant interest in the regulatory context, as
evidenced by the efforts of multiple state institutions
to publish guidance on the use of RWD (NICE, 2022;
CADTH, 2023; EMA, 2023) and international
initiatives aimed generation, gathering and sharing
RDW such as European Health Data Space and
DARWIN-EU. Unlike the rigorously controlled
clinical trials, the quality of evidence derived with
RWD can be a cause of concern. Guidance
extensively mentions limitations of the RWD,
including biases due to non-random assignment to
treatment, unblinded ascertainment of outcomes and
errors in the data generation and entry (NICE, 2022;
CADTH, 2023; EMA, 2023).
To better understand the aforementioned
limitations, we conducted an analysis of evidence
derived from the financial records of the Polish
National Health Fund regarding the Robotic-Assisted
Radical Prostatectomy (RARP), a procedure that has
been publicly funded since April 2022. In our previous
work, using data from part of 2022, we found that
694
Dzik, M., Mucha, K. and Zaleska, M.
Evidence on Robotic Prostatectomy: Discussing the Limitations of Real-World Data.
DOI: 10.5220/0013248100003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 694-697
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
RARP, compared to both Conventional Radical
Prostatectomy (CRP) and Laparoscopic Radical
Prostatectomy (LRP), was associated with a reduction
in inpatient days by 1.13 (95% CI: -1.27, -0.99;
p<0.0001) and 0.83 (95% CI: -1.02, -0.64; p<0.0001),
respectively (Dzik et al., 2024). In this study, we aim
to review the outcomes with an expanded sample and
discuss the limitations evident in the data.
3 MATERIALS AND METHODS
This study was based on the financial records
collected in the database the Polish National Health
Fund. Comparative analyses used records on patients
who had RARP, laparoscopic radical prostatectomy
(LRP) or open (conventional) radical prostatectomy
(CRP) between 20 September 2022 and 31 December
2023. The cut-off date for mortality data was 1
September 2024. All patients were diagnosed
with malignant neoplasm of the prostate (ICD-10
C61) and had to meet the following clinical criteria to
be eligible for the procedure:
Gleason Score: 6-10 (ISUP 1-5), disease
limited to the prostate, staged as cT1-2 N0 M0;
Locally advanced disease, staged as cT3a-b
N0-1 M0;
No distant metastases (M0), confirmed by
negative bone scintigraphy or whole-body
magnetic resonance imaging;
Erectile function score (IIEF-5) greater than 21.
Patients were considered outliers and excluded if
they had more than one record of radical
prostatectomy.
Following outcomes were evaluated: duration of
hospitalisation and the number of deaths.
To identify potential confounders, both
continuous and categorical covariates were used.
Exact age was calculated as the number of days
between the date of admission and the date of birth,
divided by 365.25. To test for provider-related
effects, patients were divided into subgroups based on
whether they were treated in hospitals equipped with
a robot. A hospital was considered to have a robot if
at least one robotic-assisted radical prostatectomy
(RARP) had been reported. Additionally, patients
were stratified based on whether they had an
anaesthesiologic consultation prior to hospitalization
and whether they were admitted as an emergency.
We employed a variety of statistical tests to ensure
robust and comprehensive results. The T test was used
to compare the means between two groups, while
the Chi-Squared Pearson test assessed the association
between categorical variables. For comparing means
across multiple groups, we utilized ANOVA (Analysis
of Variance). To control for potential confounding
variables, ANCOVA (Analysis of Covariance) was
applied. Finally, post hoc comparisons were conducted
using the Tukey HSD Test to identify specific group
differences following a significant ANOVA result. The
threshold for statistical significance was set at 0.05.
Statistical analyses were performed in R version 4.4.
4 RESULTS
The sample included 14,376 patients who underwent
radical prostatectomy. Six patients were excluded
from the comparison due to having undergone more
than one radical prostatectomy. Specifically, two
patients had LRP followed by CRP, two had RARP
followed by LRP, one had two RARPs, and another
had two LRPs.
Of the remaining 14,370 patients 64.6% were
treated in hospitals equipped with a robot.
Anaesthesiologic consultations were provided to 24%
of patients. 97% of patients were admitted as
scheduled or through a fast track route, while only 3%
were admitted as emergencies.
Patients ranged in age from 40 to 80 years, with
an average age of 66.4 years. The ANOVA, followed
by the Tukey’s HSD test revealed that the patients in
RAPR group were statistically younger than those in
the LRP and CRP groups with adjusted p-values less
than 0.0001 for both comparisons. The age difference
between CRP and LRP was not statistically
significant (p-value = 0.1816).
Table 1: Baseline characteristics.
Category CRP LRP RARP Total
N 1,951 5,810 6,609 14,370
Mean age (SD) 67.3 (5.8)
67.0
(6.1)
65.7 (6.8) 66.4 (6.4)
Emergency
admission (%)
68
(3.5%)
191
(3.5%)
235
(3.6%)
494
(3.4%)
Anaesthesio-
logic
consultation
before
hospitaliza-tion
(%)
415 (21%)
1,134
(20%)
1,910
(29%)
3,459
(24%)
Hospital
equipped with a
robot (%)
433
(22%)
2,246
(39%)
6,609
(100%)
9,288
(65%)
The groups differed significantly in the
proportion of anaesthesiologic consultations received
(p-value < 0.0001). However, there were no
significant differences between the groups regarding
the proportion of emergency admissions (p-value =
Evidence on Robotic Prostatectomy: Discussing the Limitations of Real-World Data
695
0.7096). Baseline characteristics are summarized in
the Table 1.
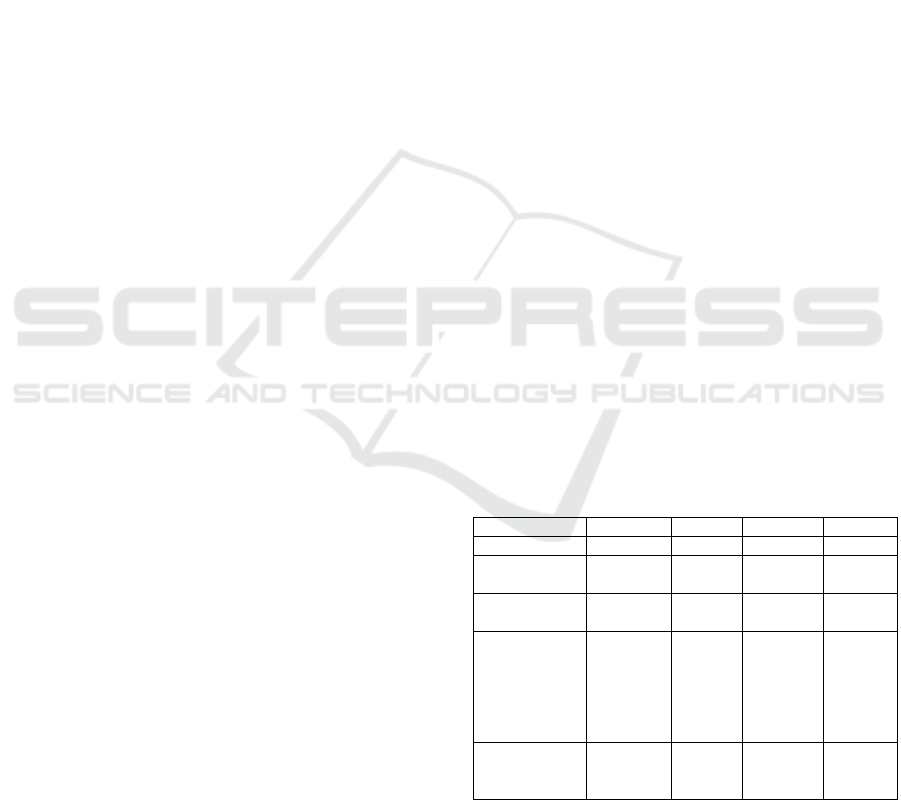
Average duration of hospitalization was 4.8
(ranging from 1 to 128) days. The length of
hospitalization in RARP group was nearly one day
shorter than in LRP and three days shorter than CRP
(Figure 1.). The differences were statistically
significant. Results are summarized in the Table 2.
Table 2: Duration of hospitalization across treatments.
Comparison
Difference
(
da
y
s
)
95% confidence
interval
LRP vs. CRP -1.91* -2.07; -1.74
RARP vs.CRP -2.81* -2.98; -2.65
RARP vs. LRP -0.91* -1.02; -0.80
*p-value=0.0
Figure 1: Mean duration of hospitalization.
The impact of age on the length of hospitalization
was tested using ANCOVA, but it was found to be
non-significant (p-value=0.3286).
The average length of stay was shorter in
hospitals equipped with a robot compared to other
hospitals (4.3 vs. 5.7 respectively; p-value<0.0001).
Notably, for the same procedures, hospitals with
robotic equipment reported shorter hospital stays for
LRP (MD=-0.7, p-value<0.0001) but not CRP (MD=-
0.2, p-value = 0.3950).
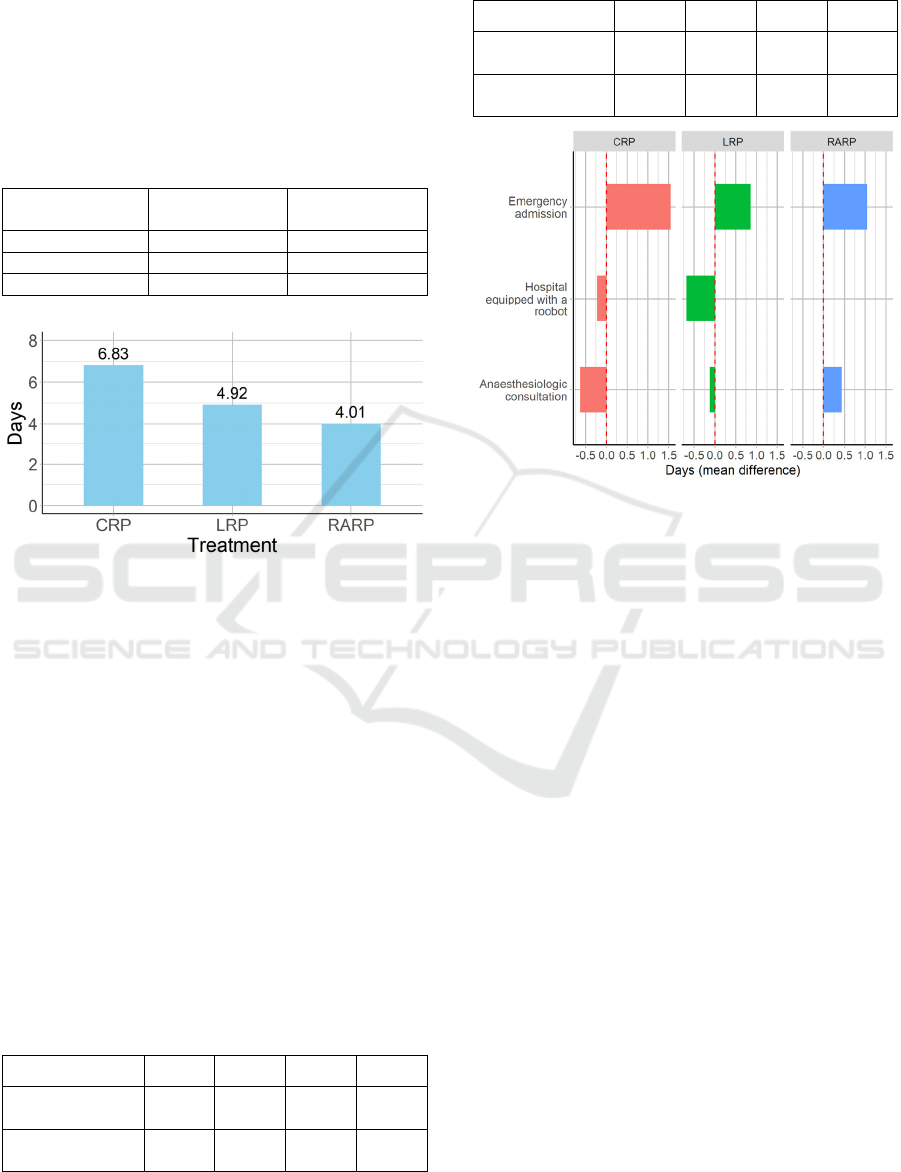
Regarding other confounders, emergency
admissions were associated with longer hospital stays
overall and for all procedures, whereas
anesthesiological consultations were not (Table 3.,
Table 4.). Impact of the confounders on the
hospitalization duration is presented on Figure 2.
Table 3: Duration of hospitalization for emergency
admissions.
Comparison CRP LRP RARP Overall
Emergency
admission
8.32 5.75 5.02 5.76
MD versus no
emer
g
enc
y
1.55* 0.86* 1.05* 1.03*
*p-value<0.0001
Table 4: Duration of hospitalization Anaesthesiologic
consultations.
Comparison CRP LRP RARP Overall
Anaesthesiologic
consultation
6.33 4.82 4.32 4.73
MD vs no
consultation
-0.63 -0.12 0.43 -0.04
Figure 2: Effect of Treatment and Covariates on
Hospitalization Duration.
As of 1 September 2024, a total of 127 deaths
were recorded, representing 0.9% of the sample. The
data was deemed insufficiently mature for performing
survival analysis. Specifically, 45 deaths were
reported in the RARP group, 61 in the LRP group,
and 21 in the CRP group. The RARP group had the
lowest proportion of deaths at 0.7%. These
differences were not statistically significant (p-
value=0.06).
5 DISCUSSION
The data demonstrated a substantial and continuous
reduction in the length of hospital stays associated
with radical prostatectomy within less than two years
of the introduction of public funding for RARP in the
Polish healthcare system. Compared to early data
from the first year (Dzik et al., 2024) average length
of hospitalization has decreased by nearly half a day
(4.8 vs 5.2). However, interpretation of the relative
benefit of RARP in comparison to LRP and CRP
remains complex.
Firstly, outcome measure itself is subject to
misinterpretation. We must acknowledge that we
have been operating under the assumption that shorter
hospital stays equate to better performance and
HEALTHINF 2025 - 18th International Conference on Health Informatics
696

subsequently outcomes. In our example the clinical
evidence is abundant. The length of hospitalization
has been already a subject of multiple prior studies
(Ma et al., 2023) which indicates its clinical
importance. In our previous analysis (Dzik et al.,
2024) we have found that patients with RARP had
fewer transfusions than CRP, which could translate to
less invasive operations or fewer complications.
Another RWD study of Swiss medical records
reported that the most common complications of the
radical prostatectomy were bleeding, hematoma and
acute bleeding anaemia (von Ahlen et al, 2024).
The limited scope of this study did not allow to
look into other indicators of performance, but
extensions to this ongoing analysis are possible. The
financial records can be studied to identify
information on other procedures performed after the
prostatectomy, as mentioned transfusions, but also
parenteral nutrition and readmissions.
Secondly, regarding readmissions, we have
excluded 6 patients who had two separate records of
radical prostatectomy. This small number could be
considered an outlier. It is possible that these were
data entry errors or failed operations. The latter is
supported by the fact that four patients were reported
to had undergone a different surgical procedure the
second time. For the future investigations it will be
necessary to monitor for more cases like that.
Finally, the interpretation of a relative benefit of
RARP to other treatments remains a concern. We
have demonstrated that hospitals with robotic
equipment reported shorter hospitalizations overall
and for LRP but not for CRP. Concern number one is
existence of hospital-related effects due to differences
in capacity, skills of the personnel and overall
standards of care. These effects can be factored into
analysis with a care selection of additional covariates.
Concern number two is selection bias, which leads
to non-homogeneous groups. Unlike our previous
analysis, our sample predominantly consisted of
RARP cases due to the rapid rise in the popularity of
this procedure in clinical practice. Nevertheless, some
patients continued to undergo CRP even in hospitals
equipped with a robot. There may be unobserved
factors influencing the choice of CRP over RARP for
certain patients. Supporting this reasoning, we
observe that while hospitals with RARP reported
shorter hospitalizations overall and for LRP, there
was no evidence of such a difference for CRP.
Therefore, to estimate relative outcomes further,
analysis including more advanced techniques such as
regression and adjusted matched comparisons may be
necessary.
6 CONCLUSIONS
The RWD indicated that RARP is associated with
shorter hospital stays than LRP and CRP. The
challenges in the analyses included interpreting the
outcome measures and validating their clinical
significance, handling outliers, addressing non-random
assignment, and accounting for unobserved covariates.
These limitations highlight the need for further
research to enhance the quality of comparisons.
ACKNOWLEDGEMENTS
The authors of this study would like to thank
Dr. hab. Anna Kowalczuk of the Agency for Health
Technology Assessment for the support necessary to
develop this study.
REFERENCES
Dzik, M., Płusa, A., Zaleska M., (2024). Real world
evidence on the effectiveness of robotic prostatectomy
in Poland. [Poster Presentation]. Health Technology
Assessment International 2024 Annual Meeting,
Seville, Spain
National Institute for Health and Care Excellence.
(2022). NICE real-world evidence
framework. https://www.nice.org.uk/corporate/ecd9
CADTH. (2023). Guidance for reporting real-world
evidence. https://www.resilienthealthcare.ca/publicatio
ns/cadth-guidance-for-reporting-real-world-evidence
European Medicines Agency. (2023). Real-world evidence
framework to support EU regulatory decision-making:
Report on the experience gained with regulator-led
studies from September 2021 to February 2023.
https://www.ema.europa.eu/en/documents/report/real-
world-evidence-framework-support-eu-regulatory-
decision-making-report-experience-gained-regulator-
led-studies-september-2021-february-2023_en.pdf
Ma, J., Xu, W., Chen, R., Zhu, Y., Wang, Y., Cao, W., Ju,
G., Ren, J., Ye, X., He, Q., Chang, Y., & Ren, S. (2023).
Robotic-assisted versus laparoscopic radical
prostatectomy for prostate cancer: The first separate
systematic review and meta-analysis of randomised
controlled trials and non-randomised studies.
International Journal of Surgery, 109(5), 1350-1359.
https://doi.org/10.1097/JS9.0000000000000193
Von Ahlen, C., Geissler, A., & Vogel, J. (2024).
Comparison of the effectiveness of open, laparoscopic,
and robotic-assisted radical prostatectomies based on
complication rates: A retrospective observational study
with administrative data from Switzerland. BMC
Urology, 24(215). https://doi.org/10.1186/s12894-024-
01597-3.
Evidence on Robotic Prostatectomy: Discussing the Limitations of Real-World Data
697
