
Approaches to Promoting Patients’ and Citizens’ eHealth Literacy
Sophia Grummt
a
and Brita Sedlmayr
b
Institute for Medical Informatics and Biometry, Carl Gustav Carus Faculty of Medicine,
TUD Dresden University of Technology, Dresden, Germany
Keywords: eHealth Literacy, Digital Competence, Online Health Information, Patient Empowerment.
Abstract: eHealth Literacy (eHL) is of crucial importance in the increasingly digital landscape of healthcare. eHL is
defined as the intersection of general health literacy and digital competencies, expanded to include new facets
such as data literacy and privacy awareness. Current studies indicate that a significant portion of the German
population has low eHL, leading to difficulties in evaluating online health information and challenges in
accessing and utilizing digital health services, which correlate with lower health status. Various measures for
enhancing citizens’ eHL are proposed, including education, public awareness campaigns, and ensuring equal
access to digital health services. Specific initiatives from the "MiHUBx" project are highlighted, such as
developing a knowledge platform for patients and organizing information events focused on digital health
topics. Fostering eHL is a societal responsibility that requires an inclusive and coordinated approach. Strategic
efforts to this end are vital to ensure that all citizens can benefit from advancements in digital healthcare.
1 INTRODUCTION
In an increasingly digitalized world, access to
healthcare information and services has changed
tremendously. From online booking of medical
appointments to the use of health apps and
telemedicine, the digitalization of healthcare is
rapidly progressing. These developments offer
immense opportunities for improving healthcare,
promoting a health-conscious lifestyle and thus
increasing quality of life. However, the successful use
of digital health solutions requires citizens to have the
necessary digital health literacy (Dratva et al., 2024),
also called eHealth Literacy (eHL). That means
people have to possess a multifaceted set of skills that
is fundamentally composed of general health literacy
and digital competencies.
2 E-HEALTH LITERACY
2.1 Defining Health Literacy
Relying on the European Health Literacy study (HLS-
EU), Health Literacy (HL) can be defined as
a
https://orcid.org/0000-0001-5094-1456
b
https://orcid.org/0000-0001-6159-7822
“people’s knowledge, motivation and competences to
access, understand, appraise, and apply health
information in order to make judgments and take
decisions in everyday life concerning healthcare,
disease prevention and health promotion to maintain
or improve quality of life during the life course”
(Sørensen et al., 2012, p. 3). This definition takes into
account not only the participation of individuals in
healthcare but also their prevention and health
promotion activities and considers HL to be a
multidimensional concept (Pelikan et al., 2022;
Sørensen et al., 2012).
2.2 Understanding Digital
Competencies
There are various concepts that address the topic of
digital competencies. One of the best known and most
widely used is the European Reference Framework
for Digital Competences (the so-called DigComp).
According to its definition, “digital competence
involves the confident, critical and responsible use of,
and engagement with, digital technologies for
learning, at work, and for participation in society. It
includes information and data literacy,
758
Grummt, S. and Sedlmayr, B.
Approaches to Promoting Patients’ and Citizens’ eHealth Literacy.
DOI: 10.5220/0013266500003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 758-765
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
communication and collaboration, media literacy,
digital content creation (including programming),
safety (including digital well-being and competences
related to cybersecurity), intellectual property related
questions, problem solving and critical thinking”
(Directorate-General for Education, 2019, p. 10).
Sorko and Irsa (2019) define the term digital
competence to include all the skills and abilities
necessary to successfully meet the new demands
brought about by digitalization. They refer less to an
independent area of competence, but rather to a
content-oriented classification. Accordingly, the term
encompasses specific digital technical,
methodological, social and personal competencies
(Sorko & Irsa, 2019). This approach emphasizes the
practical and contextual orientation in the application
of the concept of competence.
2.3 The eHealth Literacy (eHL)
Concept
eHL is a multidimensional concept that incorporates
the two areas of competence described above. Put
simply, eHL refers to the ability to find, understand,
evaluate and use digital health-related information
(Norman & Skinner, 2006).
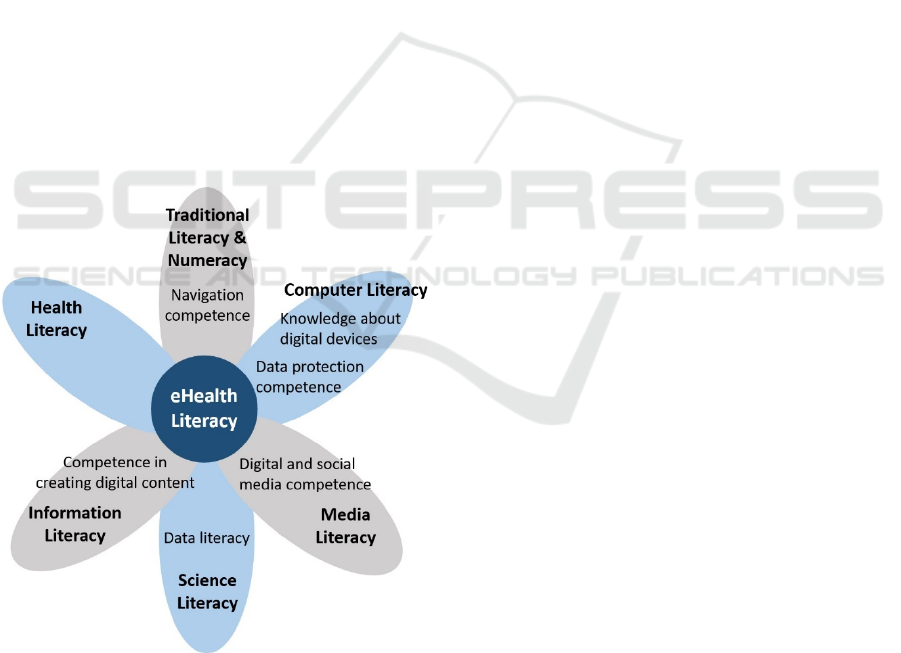
Figure 1: Lily model (adapted from Norman and Skinner,
2006) expanded with new facets according to Dratva
(2024). Bold font: original Lily model competencies,
regular font: conceptually additional digital skills; grey
filling: analytic literacy skills, blue filling: context-specific
literacy skills.
According to Norman and Skinner's Lily model
(Norman & Skinner, 2006), as shown in Figure 1,
eHL includes six core components that can be divided
into analytic literacy skills, which are generically
applicable to several sources and situations, and
context-specific literacy skills, focused on specific
issues, problem types, and contexts.
Since digital information is no longer just
consumed but also produced, provided, and shared
among individuals, more recent concepts also take
this aspect into account (Dratva et al., 2024; Nutbeam
& Muscat, 2021). They recognize additional
important digital skills as part of eHL and have
consequently expanded the original Lily model to
include these facets. According to them, eHL also
describes, for instance, the ability to decide what
information you want to share with third parties and
how you want to handle your own health data that is
collected in an app (data literacy and data protection
and information privacy literacy).
The systematic imparting of all the skills
mentioned above is essential to enable patients and
citizens to meet the new requirements of the digital
age and to exploit the full potential for promoting and
maintaining their own health in the context of the
digitalization of the healthcare system.
2.4 Current State of eHL in Germany
Research reveals that eHL is often low at an
international level and that large parts of the
population have difficulties in dealing with digital
health information (Schaeffer, 2021). Studies also
show that a high level of eHL goes hand in hand with
increased use of the internet and digital information
services (Schaeffer, 2021). As one of the first
comprehensive studies on eHL in Germany, the
second Health Literacy Survey Germany (HLS-GER
2), which is part of the “Health Literacy Population
Survey” (HLS19) of the “WHO Action Network on
Measuring Population and Organizational Health
Literacy” (M-POHL), examined this facet alongside
general HL (Schaeffer, Berens, et al., 2021; The
HLS19 Consortium of the WHO Action Network M-
POHL, 2021). The survey was conducted using
paper-assisted personal interviews with a nationally
representative sample of over 2,000 participants. The
results indicate that a very large proportion of the
German citizens - over three quarters (75.8%) - has a
low level of eHL (Schaeffer, Gille, et al., 2021). The
eHL of the population in Germany is therefore
significantly lower than general HL (58.8% have only
low health literacy) (Schaeffer, Berens, et al., 2021).
The most difficult aspect for respondents is, by far,
Approaches to Promoting Patients’ and Citizens’ eHealth Literacy
759

assessing the trustworthiness and neutrality of digital
health information. The opaque coexistence of
serious and dubious information in online
information channels seems to make handling digital
information extremely challenging nowadays (Dratva
et al., 2024). This is not specific to Germany. The
other 13 countries that surveyed eHL in the HLS19
reached the same conclusion (The HLS19
Consortium of the WHO Action Network M-POHL,
2021).
In another empirical study conducted as part of a
panel survey with a population-representative sample
of 8,500 adults living in Germany, 52.4% of the
participants showed limited eHL (Zeeb et al., 2022).
It should be noted that all participants in this study
were recruited and surveyed online, so it is not
representative in terms of internet use. Although both
studies used the Digital Health Literacy Instrument
DHLI (van der Vaart & Drossaert, 2017) to measure
eHealth literacy, the version of the questionnaire used
in this case contained twice as many items (21 items)
as the HLS-GER 2 (ten items). The study authors
attribute the difference from the results of the HLS-
GER 2 study to the different participant groups and
evaluation strategies, pointing to the limited
comparability between the two studies. However,
both studies concluded that users have great difficulty
in evaluating the quality of the online information
they encounter. Additionally, Zeeb et al. (2022) found
that a poorer health status was statistically
significantly associated with lower eHL.
2.5 The Importance of Enhancing eHL
The above-mentioned survey results underline that
there is an urgent need for action to strengthen eHL
in the general population. The consequences of a lack
of eHL can be far-reaching: inadequate use of digital
health services, misinformation and even adverse
health outcomes are possible consequences. Without
sufficient eHL, citizens cannot take full advantage of
digital health services and are more vulnerable to
health information of dubious quality. Improving
eHL is of central importance for several reasons:
1. Improved access to health information and
services and participation in health decisions: High
eHL enables citizens to find and evaluate quality-
assured health information on the internet, actively
participate in medical decision-making processes,
and better understand their own health decisions
(German Federal Ministry of Health, 2022). This
could increase self-efficacy and decision-making
ability in health matters (Farley, 2020).
2. Reduction of health inequalities: eHL can help
reduce health inequalities by enabling all population
groups to access digital health information and
services (Dratva et al., 2024). Digitally competent
citizens can better utilize digital health services,
which can contribute to improved healthcare,
particularly in rural areas and underserved
communities.
3. Promotion of a healthy lifestyle, prevention,
and early detection: Competent use of health apps and
wearables allows citizens to actively monitor and
promote their health (German Federal Ministry of
Health, 2022), contributing to disease prevention and
early detection, and potentially leading to a long-term
reduction in chronic diseases.
4. Increased efficiency in healthcare: Citizens
with high eHL could relieve the healthcare system
and contribute to cost efficiency by utilizing digital
health services.
5. Promotion of medical research: According to a
population-representative survey, more than 86
percent of Germans would agree to the use of health
data for publicly funded medical research without
individual consent (Richter et al., 2024), provided
that data usage and access are legally regulated and
adequately controlled. However, more than two thirds
of respondents wanted a larger supply of information
on medical research with health data in order to make
an informed decision about whether to participate in
data donation. An opt-out regulation (the omission of
case-by-case consents) thus requires expanded
information offerings to strengthen health data
literacy and trust in medical research (Richter et al.,
2024).
2.6 Possible Measures to Strengthen
eHL
To generally strengthen eHL in the population,
targeted measures are necessary. These should be
implemented at various levels. The following
exemplary list provides an initial overview of
promising starting points and is intended serve as a
source of inspiration. How the recommended
measures can be implemented in practice would have
to be worked out in detail with the relevant social,
political and medical players.
1. Education and training: Development and
implementation of educational programs that train
citizens in the use of digital health services and in
dealing with digital health information. Media and
health literacy should already be systematically
linked and specifically promoted in the school setting
(Bittlingmayer et al., 2020).
HEALTHINF 2025 - 18th International Conference on Health Informatics
760

2. Enablement through healthcare providers:
Healthcare providers should be actively involved in
teaching digital health skills to their patients
(Konstantinidis et al., 2022). This can be done
through training, information events and the
provision of easy-to-understand digital resources.
3. Low-threshold offers: Develop, promote and
publicize low-threshold, easily accessible offers such
as free online courses, tutorials and mobile apps that
are specifically tailored to the needs of different target
groups (e.g. adapted to age, occupational group,
medical condition and/or skill level).
4. Public awareness: Implementation of
multimedia education campaigns to raise awareness
of the importance of eHL, promote the critical use of
health information on the internet and social media
and motivate citizens to upskill (German Federal
Ministry of Health, 2022).
5. Research and evaluation: Promoting research
on eHL, particularly on how people receive their
health information and how they prefer to be
informed or get access to information in the future,
and continuously evaluating measures to strengthen
eHL in order to assess and improve their effectiveness
(Dratva et al., 2024).
6. Access to digital health services: Ensuring that
all citizens have access to digital health services,
regardless of their social or economic status (Dratva
et al., 2024).
Taking the last point as an example for providing
some insights into how the measures could be
realistically implemented in practice, here are some
more detailed ideas how to support equal access to
digital health services:
Improving Infrastructure
Ensure nationwide access to the internet by
expanding broadband and mobile network
infrastructure, particularly in rural and
economically disadvantaged regions.
Provide free internet access, for example, by
offering complimentary Wi-Fi in public
facilities such as libraries, schools, and
hospitals.
Reducing Financial Barriers
Offer subsidized digital devices through
programs that provide low-income households
with affordable or free tablets, smartphones, or
computers.
Ensure that essential digital health services and
applications are free of charge or covered by
the healthcare system.
Promoting Education and Training
Enhance eHL by integrating training on the use
of digital health services into programs offered
by adult education centers, employment
agencies, and social organizations.
Provide individual support by establishing
contact points where citizens can receive
technical assistance and guidance, such as
through "eHealth hotlines" or on-site services
in community centers.
Ensuring User-Friendliness
Develop accessible digital health solutions that
are user-friendly and inclusive, ensuring they
are easily usable for individuals with
disabilities or limited digital skills.
Offer multilingual health services and
information to facilitate access for migrants
and refugees.
Establishing Political Frameworks
Create a legal framework that enshrines the
right to access digital health services in the
Social Code.
These measures can help to ensure that all citizens
in Germany, regardless of their social or economic
background, have access to digital health services,
which is essential for systematically fostering eHL
across the population.
2.7 Initial Approaches to Strengthen
eHL in the German Population as
Part of the Project “MiHUBx”
The digital progress hub “Medical Informatics Hub in
Saxony” (MiHUBx), funded by the German Federal
Ministry of Education and Research, aims to make
healthcare data from routine care accessible for
research purposes and strengthen collaboration in
healthcare (MiHUBx, n.d.). To this end, the German
medical informatics initiative is establishing a digital
infrastructure with processes and tools that will
enable healthcare facilities to make routine data
available for research. To ensure the usability of this
digital infrastructure, measures are being devised and
implemented to promote the acceptance of the
project’s digital solutions developed and to enhance
digital competencies. This includes enabling patients
to gain a better understanding of digitality in
healthcare and thereby increasing overall acceptance
of digital applications in this context. To this end,
various measures have been implemented or initiated
to date, including the following:
Approaches to Promoting Patients’ and Citizens’ eHealth Literacy
761

2.7.1 Digital Knowledge Platform for
Patients and Citizens
The aim of strengthening digital (health)
competencies in the population is to be achieved,
among other approaches, with the help of a
knowledge platform embedded in the MiHUBx
project website, which is currently being developed
(Grummt et al., 2024). The information webpages for
patients and citizens can be accessed at
https://mihubx.de/wissen-patienten/. Patients are
currently supported by the web subpages in
strengthening digital competencies by providing
them with information on topics such as health data,
digital medicine, and corresponding applications.
General information on digitalization in the
healthcare sector is presented in layman's terms in the
“Grundlagenwissen (Basic Knowledge)” section. In
the “Digitale Kompetenz (Digital Competence)”
section, users are informed about how they can assess
the quality of health information on the internet and
are provided with corresponding checklists and
guidance. The HLS19 and HLS-GER 2 studies have
shown that most people find it difficult to assess the
content of digital health information (Schaeffer,
Gille, et al., 2021; The HLS19 Consortium of the
WHO Action Network M-POHL, 2021), which is
why we want to support them in this important aspect.
Additionally, the "Gesundheitsportale (Health
Portals)" section offers a comprehensive compilation
of valid health information sources and websites with
information on topics such as digital health
applications, data protection and security. The
“Weiterbildungen (Education)” section refers to
numerous free educational offerings for target groups
such as patients and citizens with a focus on (digital)
health, data (literacy), and artificial intelligence.
Under “Podcasts”, our podcast recommendations
offer knowledge to listen to on current topics in
healthcare, digitalization in medicine and general
medical knowledge. A comprehensive “Glossar
(Glossary)” explains technical terms from the fields
of digital medicine, medical informatics, and
digitalization. The knowledge webpages for patients
provide a wide range of information and educational
resources on digital health, all in one digital location.
This is intended to increase acceptance of and
participation in the digital transformation of the
healthcare system. Incidentally, the next step will be
implementing knowledge pages tailored specifically
to the needs of physicians and medical staff.
2.7.2 (Online) Events for Patients and
Citizens
To strengthen the eHL of patients and their relatives,
(online) events are designed and conducted that
provide an overview and education on digital health
topics and offer opportunities for skill development.
For example, MiHUBx took part in the 21st Dresden
Science Night in June 2024, a format where scientific
topics are introduced to the general public in a
playful, accessible manner. Visitors to our stand were
able to get an all-round view of the topics “digital
medicine”, “artificial intelligence”, “use of patient
data for medical research and broad consent” and
“work of a data integration centre” using interactive
offers and leave their opinions on an opinion board.
The participants experienced a high level of openness
and interest from visitors leading to insightful
discussions.
In November 2024, we hosted an event on
digitalization and data usage in healthcare for patients
and interested parties in collaboration with the
Complex Regional Pain Syndrome (CRPS) Patient
Network. In meetings with board members of the
network, we discussed which digital health topics are
particularly relevant and interesting for CRPS
patients, and developed a corresponding agenda. In an
interactive online format, with a mix of lectures,
discussions, and Q&A sessions, topics such as the
electronic patient record (basics and access
management), handling health data, as well as digital
health applications and support options for CRPS
have been addressed. The participants asked many
questions and reported on their previous experiences
in dealing with personal health data, which led to
several interesting discussions. Unfortunately, we
had to end the event after more than two and a half
hours (two hours were originally planned), but based
on the questions and the need for discussion, it could
certainly have lasted even longer. Our aim is to
continue organizing similar themed events for various
patient organizations and networks.
2.7.3 Informational Flyers in Plain
Language
In an analogue format, we provide patients and
citizens with information about health data and its
secondary use for medical research through
informational flyers in plain language. These flyers
are designed to help individuals understand complex
topics, such as data donation, privacy protections, and
the benefits of health data usage for medical research,
in a straightforward and accessible way. By
HEALTHINF 2025 - 18th International Conference on Health Informatics
762

addressing common questions and concerns, the
flyers aim to build trust and promote transparency
regarding the use of health data in research.
To further support digital health literacy,
additional flyers are being planned on topics such as
the electronic patient record or digital health
applications.
With these resources, we aim to provide patients
and the wider public with the knowledge they need to
make informed decisions about their health data and
the use of digital health services and applications.
3 DISCUSSION AND
CONCLUSION
We are aware that our current offerings only reach a
fraction of the population and are likely primarily
targeted at those who already possess higher levels of
eHL since digital competencies are a prerequisite for
assessing online information and participating in
online activities. Events on (digital) health are
probably predominantly attended by individuals who
already have a foundational level of HL and
potentially some scientific knowledge. The major
challenge is reaching those whose eHL is particularly
low and who less frequently take advantage of digital
health-related information opportunities. According
to the findings of the HLS-GER 2 study, these
individuals are primarily the ones with lower general
HL, older adults (65+), individuals with lower
literacy skills, lower educational levels, and/or lower
social status (Schaeffer, Gille, et al., 2021).
Strengthening eHL is thus a societal task that requires
an inclusive and coordinated approach.
In their systematic literature review, Geukes et al.
(2022) emphasize the urgent need for an evidence-
based eHL concept to modify and implement digital
technologies and health information in a target group-
specific and resource-oriented manner. Digital
technologies offer the possibility for individualized
and needs-oriented design of health-related
information. However, to be effective, this
information must be understood by users and, within
setting-based prevention, must be adequately utilized
by organizations and integrated into structural
development processes.
The measures outlined in section 2.6 are
formulated in a rather broad or overarching manner
and leave the stakeholders addressed – such as
educational institutions, medical associations,
political actors (e.g., the Ministry of Health), research
sponsors, and social actors – leeway in their specific
design and implementation. Detailed proposals for
concrete practical implementation would have been
too extensive for this position paper and would have
gone beyond its scope. We are aware of the fact that
some of the proposed measures are very difficult to
put into practice, such as the enablement of citizens
through healthcare providers who usually only have a
very limited amount of time per patient and in some
cases also lack the appropriate eHL and educational
skills. To overcome the absence of digital and
educational skills, medical study curricula or medical
training plans should pay more attention to these core
competencies. The restricted time per patient is a
major general problem for which we unfortunately
cannot offer a quick solution. To overcome this
problem, the entire German healthcare system would
have to change.
Another important point to consider is the
widespread use of social media platforms such as
Instagram, Facebook, Tiktok, and X, which many
people rely on as an additional source of (health)
information (Suarez-Lledo & Alvarez-Galvez, 2021).
Given the limited control over misinformation on
these platforms, it is essential to address the social
media aspect when teaching skills to distinguish
between trustworthy and unreliable sources. Raising
awareness about the ease with which anyone can use
these platforms to disseminate (also unverified or
false) opinions and share misinformation on health
topics should ideally foster a healthy skepticism
toward health-related claims made by private
individuals, companies, and organizations.
Overall, eHL can be a critical competence and a
key predictor for effective health prevention and
promotion (Chang & Schulz, 2018). A meta-analysis
from 2023 also found a positive correlation with
health-related behaviors, suggesting eHL may act as
a mediator between the consumption of health-related
information and subsequent changes in health-related
behaviors (Kim et al., 2023). It must therefore be
fostered through targeted education and awareness-
raising measures. Programs to promote eHL must be
tailored to the specific needs of different user groups
and life environments. Only if these programs are
found, assessed, and adequately applied by users,
they can have a positive impact on health by
supporting effective health promotion and
prevention.
Finally, it is crucial to ensure that all citizens can
benefit from advances in healthcare made possible
by digitalization. This will be essential for
promoting the health and well-being of society in the
digital age.
Approaches to Promoting Patients’ and Citizens’ eHealth Literacy
763

ACKNOWLEDGEMENTS
This work is part of the project “Medical Informatics
Hub in Saxony (MiHUBx)” which is funded by the
German Federal Ministry of Education and Research
(grant number 01ZZ2101A).
REFERENCES
Bittlingmayer, U. H., Dadaczynski, K., Sahrai, D., van den
Broucke, S., & Okan, O. (2020). Digitale
Gesundheitskompetenz – Konzeptionelle Verortung,
Erfassung und Förderung mit Fokus auf Kinder
und Jugendliche. Bundesgesundheitsblatt -
Gesundheitsforschung - Gesundheitsschutz, 63(2),
176–184. https://doi.org/10.1007/s00103-019-03087-6
Chang, A., & Schulz, P. J. (2018). The Measurements and
an Elaborated Understanding of Chinese eHealth
Literacy (C-eHEALS) in Chronic Patients in China.
International Journal of Environmental Research and
Public Health, 15(7), Article 7. https://doi.
org/10.3390/ijerph15071553
Directorate-General for Education, Y. (2019). Key
competences for lifelong learning. Publications Office
of the European Union. https://data.europa.
eu/doi/10.2766/569540
Dratva, J., Schaeffer, D., & Zeeb, H. (2024). Digitale
Gesundheitskompetenz der Bevölkerung in
Deutschland: Aktueller Stand, Konzepte und
Herausforderungen. Bundesgesundheitsblatt -
Gesundheitsforschung - Gesundheitsschutz, 67(3),
277–284. https://doi.org/10.1007/s00103-024-03841-5
Farley, H. (2020). Promoting self-efficacy in patients with
chronic disease beyond traditional education: A
literature review. Nursing Open, 7(1), 30–41.
https://doi.org/10.1002/nop2.382
German Federal Ministry of Health. (2022, February 4).
Gesundheitskompetenz stärken. gesund.bund.de.
https://gesund.bund.de/gesundheitskompetenz-digital-
staerken
Geukes, C., Stark, A. L., & Dockweiler, C. (2022). eHealth
Literacy als Grundlage zur Entwicklung digitaler
Technologien in der Gesundheitsförderung und
Prävention? Eine systematische Übersicht der Literatur.
Prävention und Gesundheitsförderung, 17(2), 163–
169. https://doi.org/10.1007/s11553-021-00858-5
Grummt, S., Seim, A., & Glathe, C. (2024). Identifizierung
und Aufbereitung von nutzergruppenspezifischem
Wissen im Bereich der digitalen Medizin am Beispiel
einer Wissensplattform im MiHUBx-Projekt. DocAbstr.
334. https://doi.org/10.3205/24gmds191
Kim, K., Shin, S., Kim, S., & Lee, E. (2023). The Relation
Between eHealth Literacy and Health-Related
Behaviors: Systematic Review and Meta-analysis.
Journal of Medical Internet Research, 25, e40778.
https://doi.org/10.2196/40778
Konstantinidis, S., Leonardini, L., Stura, C., Richter, P.,
Tessari, P., Winters, M., Balagna, O., Farrina, R., van
Berlo, A., Schlieter, H., Mayora, O., & Wharrad, H.
(2022). Digital Soft Skills of Healthcare Workforce –
Identification, Prioritization and Digital Training. In M.
E. Auer, H. Hortsch, O. Michler, & T. Köhler (Eds.),
Mobility for Smart Cities and Regional Development—
Challenges for Higher Education (pp. 1118–1129).
Springer International Publishing. https://doi.org/10.
1007/978-3-030-93907-6_117
MiHUBx. (n.d.). MiHUBx – Ziele und Struktur. Retrieved
November 7, 2024, from https://mihubx.de/ziele-und-
struktur/
Norman, C. D., & Skinner, H. A. (2006). eHealth Literacy:
Essential Skills for Consumer Health in a Networked
World. Journal of Medical Internet Research, 8(2),
e506. https://doi.org/10.2196/jmir.8.2.e9
Nutbeam, D., & Muscat, D. M. (2021). Health Promotion
Glossary 2021. Health Promotion International, 36(6),
1578–1598. https://doi.org/10.1093/heapro/daaa157
Pelikan, J. M., Link, T., Straßmayr, C., Waldherr, K.,
Alfers, T., Bøggild, H., Griebler, R., Lopatina, M.,
Mikšová, D., Nielsen, M. G., Peer, S., & Vrdelja, M.
(2022). Measuring Comprehensive, General Health
Literacy in the General Adult Population: The
Development and Validation of the HLS19-Q12
Instrument in Seventeen Countries. International
Journal of Environmental Research and Public Health,
19(21), Article 21. https://doi.org/10.3390/
ijerph192114129
Richter, G., Trigui, N., Caliebe, A., & Krawczak, M.
(2024). Attitude towards consent-free research use of
personal medical data in the general German
population. Heliyon, 10(6), e27933. https://doi.org/10.
1016/j.heliyon.2024.e27933
Schaeffer, D., Berens, E.-M., Gille, S., Griese, L., Klinger, J.,
de Sombre, S., Vogt, D., & Hurrelmann, K. (2021).
Gesundheitskompetenz der Bevölkerung in Deutschland
vor und während der Corona Pandemie:
Ergebnisse des HLS-GER 2. Bielefeld: Universität
Bielefeld, Interdisziplinäres Zentrum für
Gesundheitskompetenzforschung. https://doi.org/10.
4119/UNIBI/2950305
Schaeffer, D., Gille, S., Berens, E.-M., Griese, L., Klinger,
J., Vogt, D., & Hurrelmann, K. (2021). Digital Health
Literacy of the Population in Germany: Results of the
HLS-GER 2. Das Gesundheitswesen. https://doi.org/
10.1055/a-1670-7636
Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G.,
Pelikan, J., Slonska, Z., Brand, H., & (HLS-EU)
Consortium Health Literacy Project European. (2012).
Health literacy and public health: A systematic review
and integration of definitions and models. BMC Public
Health, 12(1), 80. https://doi.org/10.1186/1471-2458-
12-80
Sorko, S. R., & Irsa, W. (Eds.). (2019). Interaktive Lehre
des Ingenieursstudiums: Technische Inhalte
handlungsorientiert unterrichten. Springer Berlin
Heidelberg. https://doi.org/10.1007/978-3-662-56224-6
HEALTHINF 2025 - 18th International Conference on Health Informatics
764

Suarez-Lledo, V., & Alvarez-Galvez, J. (2021). Prevalence
of Health Misinformation on Social Media: Systematic
Review. Journal of Medical Internet Research, 23(1),
e17187. https://doi.org/10.2196/17187
The HLS19 Consortium of the WHO Action Network M-
POHL. (2021). International Report on the
Methodology, Results, and Recommendations of the
European Health Literacy Population Survey 2019-
2021 (HLS19) of M-POHL. Austrian National Public
Health Institute. https://m-pohl.net/sites/m-
pohl.net/files/inline-
files/HLS19%20International%20Report.pdf
van der Vaart, R., & Drossaert, C. (2017). Development of
the Digital Health Literacy Instrument: Measuring a
Broad Spectrum of Health 1.0 and Health 2.0 Skills.
Journal of Medical Internet Research, 19(1), e27.
https://doi.org/10.2196/jmir.6709
Zeeb, H., Pohlabeln, H., Preising, A., Schulz, B.,
Naczinsky, A., & Kolpatzik, K. (2022).
Schlüsselqualifikation digitale Gesundheitskompetenz
– empirische Daten aus Deutschland. In K. Rathmann,
K. Dadaczynski, O. Okan, & M. Messer (Eds.),
Gesundheitskompetenz (pp. 1–13). Springer Berlin
Heidelberg. https://doi.org/10.1007/978-3-662-62800-
3_149-1.
Approaches to Promoting Patients’ and Citizens’ eHealth Literacy
765
