
Predicting Falls from Operational Data: Insights and Limitations of
Using a Non-Specialized Database
Julien R
¨
aker
1 a
, Patrick Elfert
1 b
, Cletus Brauer
2 c
, Marco Eichelberg
1 d
,
Frerk M
¨
uller-von Aschwege
1 e
and Andreas Hein
1 f
1
R&D Division Health, OFFIS - Institute for Information Technology, Oldenburg, Germany
2
Johanniter-Unfall-Hilfe e.V., Oldenburg, Germany
fi
Keywords:
Fall Prediction, Machine Learning, Health Data, Elderly Care, Predictive Analytics.
Abstract:
Falls among the elderly are a significant public health concern. This study investigates the feasibility of
predicting falls using an operational dataset from Johanniter-Unfall-Hilfe (JUH) home emergency call system,
which was not created under laboratory conditions for scientific purposes. An anonymized dataset containing
records from 160,281 participants in Germany was analyzed. Statistical analysis identified 104 out of 400
features significantly associated with falls, though with weak correlations (Cramer’s V ranging from 0.006 to
0.071). A one-class Support Vector Machine (SVM) was employed due to the absence of explicit non-fall
cases, achieving a true positive rate of 55.10%. The lack of explicit non-fall data prevented evaluation of
specificity and overall accuracy. The study demonstrates the potential of using operational datasets for fall
prediction but highlights significant limitations due to data quality issues, such as the lack of explicit fall
records, absence of non-fall cases, lack of temporal data, and missing values. Recommendations are made to
improve data collection practices to enhance the utility of such datasets for predictive modeling.
1 INTRODUCTION
The global demographic shift towards an aging
population presents significant challenges for
healthcare systems (Nicholas and Smith, 2006).
With advances in medicine and public health,
people are living longer, but this increased longevity
often comes with a higher prevalence of chronic
conditions and age-related impairments. One of the
most significant risks associated with aging is the
increased likelihood of falls (Comans et al., 2013).
Falls remain one of the leading cause of injury and
morbidity in individuals aged 65 and older, often
resulting in severe consequences such as fractures,
hospitalization, and loss of independence (Comans
et al., 2013; Pfortmueller et al., 2014).
Preventing falls is thus a critical component in
improving the quality of life for older adults and
a
https://orcid.org/0009-0005-5153-906X
b
https://orcid.org/0000-0002-9834-0702
c
https://orcid.org/0000-0002-2924-7934
d
https://orcid.org/0000-0002-8590-3318
e
https://orcid.org/0009-0001-4960-4097
f
https://orcid.org/0000-0001-8846-2282
reducing the economic burden on healthcare systems
(Becker and Rapp, 2011; Walther et al., 2008).
Traditional preventive strategies include physical
therapy paired with home modifications, Checking for
incompatibilities or unwanted interactions with the
current medication or managing fear of falling (Zeeh
et al., 2017; Becker and Rapp, 2011; Jansen et al.,
2021).
In recent years, machine learning (ML) including
artificial intelligence (AI) have emerged as promising
tools for enhancing preventive healthcare efforts
(Vuppalapati et al., 2019). Through predictive
analytics, AI models can analyze large datasets to
identify risk factors and early warning signs of
health events such as falls, potentially enabling timely
interventions (Chattu, 2021).
Numerous studies have explored the use of ML
for fall prediction, utilizing various datasets and
methodologies. Most of these studies have relied on
data collected from sensors, which can be broadly
categorized into wearable and non-wearable devices.
Wearable devices often include inertial measurement
units (IMUs) that track movement and detect
anomalies indicative of a fall (El-Bendary et al.,
2013; Usmani et al., 2021). Approximately two-
774
Räker, J., Elfert, P., Brauer, C., Eichelberg, M., Müller-von Aschwege, F. and Hein, A.
Predicting Falls from Operational Data: Insights and Limitations of Using a Non-Specialized Database.
DOI: 10.5220/0013298600003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 774-780
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.

thirds of these studies initially collected data under
controlled laboratory conditions to ensure data quality
and reliability (Usmani et al., 2021). A notable study
using non-sensor data was conducted by Marschollek
et al., who aimed to predict whether a patient would
fall during an inpatient stay in a geriatric center based
on medical records (Marschollek et al., 2012). They
analyzed the medical records of over 5,000 patients
over a period of 1.5 years. Using the C4.5 decision
tree algorithm, trained on the binary attribute of fall
or no fall, the model achieved an accuracy of 66%,
with a sensitivity of 55.4% and a specificity of 67.1%.
While their dataset included results from various
geriatric assessments, which significantly influenced
the outcomes, such assessments are cost-intensive and
not routinely performed, limiting the generalizability
of the model. In contrast, general patient-related data
such as age, gender, pre-existing conditions (such
as chronic diseases or walking impairments), and
medication are more commonly available and have
also been shown to influence the occurrence of falls
(Jansenberger, 2011). However, there is a lack of
studies that utilize such general data for fall prediction
without relying on specialized assessments or sensor
data. This gap highlights the need to explore whether
more readily available patient data can be leveraged to
predict fall risk, potentially making predictive models
more accessible and scalable in real-world settings.
In this study, we aimed to address this gap
by exploring the potential of using an existing,
non-research-specific database from the Johanniter-
Unfall-Hilfe (JUH) home emergency call system to
predict falls. The JUH system provides emergency
support to elderly or disabled individuals, allowing
them to call for help in case of incidents, many of
which involve falls (J
¨
org L
¨
ussem, Thomas M
¨
ahnert,
Hubertus v. Puttkamer, 2021). The database was
originally designed for operational purpose, not for
research, and thus lacks explicit fall records and
comprehensive temporal data. The data includes
personal information such as age, medication and
previous illnesses, which were recorded once when
the home emergency call system was activated (more
details in section 2.1). Fall-related incidents were
inferred from emergency call records, where falls
were often cited as the reason for the call, introducing
several limitations in the dataset’s applicability for
predictive modeling.
We aim to assess whether a ML model,
specifically a one-class Support Vector Machine
(SVM), can be used to predict falls based on the
available data. The one-class SVM was selected
due to the dataset’s imbalanced nature, containing
only fall-related cases and no explicit records of
individuals who have not fallen. This exploratory
study seeks to evaluate the feasibility of leveraging
a general-purpose dataset for predictive healthcare
and to identify key limitations, particularly those
inherent to this type of dataset, that future studies
must address.
2 METHODS
2.1 Data Source
The data used in this study originates from the JUH
home emergency call system, a service designed to
assist elderly or disabled individuals by providing
immediate emergency support (J
¨
org L
¨
ussem, Thomas
M
¨
ahnert, Hubertus v. Puttkamer, 2021). The dataset
spans from January 1, 2012, to October 16, 2020, and
includes anonymized records of participants located
in Lower Saxony and Bremen, Germany.
2.1.1 Data Characteristics
The initial dataset comprised records from 160,281
participants, with an average age of 82.73 years
(±9 years) and a predominance of female participants
(71.84%). The dataset included:
• Demographic Information: Age, gender, and
living conditions.
• Medical History: Chronic conditions, prior
illnesses, and medications.
• Emergency Call Records: Details of emergency
calls, including timestamps and free-text
comments describing the nature of the incident.
• Care Level: Classified according to the German
care insurance system, indicating the degree of
care required by the individual (Nadash et al.,
2018).
This is static data that was recorded once when
the patient joined the home emergency call system,
with the exception of the degree of care, which was
updated depending on the status.
2.1.2 Data Limitations
Fall incidents were not systematically documented
but had to be inferred from free-text comments in
the emergency call logs, which were recorded by
the operator during or after the call. Consequently,
explicit records were also unavailable for individuals
who did not experience falls, as the information
on falls was derived solely from emergency calls.
This introduces a challenge, as people may fall
Predicting Falls from Operational Data: Insights and Limitations of Using a Non-Specialized Database
775

without contacting emergency services, complicating
the creation of a reliable control group.
2.2 Data Preprocessing
The following preprocessing steps were undertaken to
prepare the data for analysis:
1. Extraction of Fall Incidents:
• A keyword search on the free-text comments
was applied in the emergency call records to
identify potential fall incidents. Keywords
included different terms of the word
”
fall“
in German(e.g.
”
gefallen“,
”
gest
¨
urzt“,
”
hingefallen“).
• To increase accuracy, the text has been
converted to lower case and umlauts have been
removed.
2. Handling Missing Values:
• Due to the significant proportion of missing
data, with only 33.57% of participants having
complete data available, individuals with
incomplete datasets were excluded from the
analysis.
3. Feature Selection:
• The Pearson chi-square test of independence
was used to identify features significantly
associated with fall incidents (see section 2.3).
4. Encoding Categorical Variables:
• Categorical variables were converted into
numerical format using one-hot encoding to
make them suitable for ML algorithms.
5. Feature Scaling:
• Numerical features were standardized to ensure
that all features contribute equally to the model
training process.
6. Data Splitting:
• The dataset was split into training and testing
sets using a 70/30 ratio.
2.3 Statistical Analysis
To identify features significantly associated with fall
incidents, a Pearson chi-square test was applied to
the dataset. This test evaluates the relationship
between categorical variables (e.g., age group,
chronic conditions) and the likelihood of a fall by
comparing observed frequencies of falls within one
year with expected frequencies under the assumption
of independence. The strength of these associations
was quantified using Cramer’s V, to provide insights
into which feature were most relevant to fall
prediction.
2.4 Predictive Modeling
Since the dataset contains only one class, the selection
of suitable models is limited. We used algorithms
from the field of outlier or anomaly detection for
this purpose. Examples of this are one-class SVMs,
Isolation Forest or Local Outlier Factor.
Given that one-class SVMs are well-suited for
problems where the goal is to identify patterns
in datasets containing only positive instances (An
et al., 2015), they were chosen for this task. The
participants were divided into two groups. Those
who made one or more calls calls due to falls within
one year, and those who made no fall-related call
within that year. To ensure all features have values
in the same range, the data was scaled using the
StandardScaler by scikit-learn. Furthermore, the
dataset was split into training and test sets, with
the training exclusively conducted on the class of
participants who experienced falls, and the testing
carried out on all data.
2.4.1 Model Evaluation
Due to the absence of non-fall records, model
evaluation was conducted by focusing on the models
ability to correctly identify actual fall instances within
the test set. The following metrics were used to
evaluate model performance:
• True Positive Rate (Sensitivity): Proportion of
actual falls correctly identified by the model.
• False Negative Rate (Specificity): Proportion of
actual falls incorrectly classified as non-falls.
3 RESULTS
3.1 Descriptive Statistics
For the chi-square test, a total of 146,263 participants
were included. The participants had an average age
of 83.81 years (±8.14 years), with ages ranging from
53 to 110. The majority of participants were female
(71.75%), while 27.32% were male. 15,262 (10.43%)
of those participants are marked as fallen. For 89.57%
of participants, no information is available as to
whether they have fallen or not.
For the predictive model, only the participants
who are marked as fallen and did not have any missing
values were included into analysis. The dataset was
HEALTHINF 2025 - 18th International Conference on Health Informatics
776

thus reduced to a total of 6038 participants, with
an average age of 84.65 (±7.39 years), ranged from
53 to 105. Here too, women were more frequently
represented (63.23%) than men (36.40%).
3.2 Statistical Associations
The Pearson chi-square test was applied to identify
features significantly associated with fall incidents.
Among the 400 features analyzed, 104 demonstrated
a statistically significant association with falls
(p < 0.05).
The strength of these associations was quantified
using Cramer’s V, with values ranging from 0.006 to
0.071, indicating a very weak correlation. The 20
features with the highest correlation can be seen in
Table 1.
3.3 Model Performance
A one-class SVM was employed to predict fall
incidents within a year based on the significant
features identified in the statistical analysis. The
OneClassSVM class from scikit-learn was used for
this task. A grid search was performed to identify
the best parameters. It was found that the default
settings with the sigmoid kernel performed best. The
following performance metrics were obtained:
• The model achieved a sensitivity of 55.10%,
meaning it correctly identified 55.10% of
individuals who experienced falls.
• The false negative rate was 44.90%, indicating
the proportion of fall incidents that the model
failed to predict.
• The model classified overall 45.39% of the test
participants as at risk of falling.
The confusion matrix (shown in Table 2)
summarizes the model’s performance.
4 DISCUSSION AND
CONCLUSION
This study investigated the feasibility of using a non-
research-specific, operational dataset from the JUH
home emergency call system to predict falls among
the elderly using a one-class SVM. The findings
highlight both the potential and the limitations of
leveraging such datasets for predictive healthcare
modeling.
4.1 Interpretation of Results
The one-class SVM achieved a true positive rate
(sensitivity) of 55.10%, correctly identifying over
half of the fall incidents in the test set. However,
a significant proportion of actual falls (44.90%)
were not detected by the model. The statistical
analysis revealed that 104 out of 400 features
were significantly associated with falls (p < 0.05),
although the strength of these associations was weak
(Cramer’s V ranging from 0.006 to 0.071). However,
it must be considered here that in the Chi-Square
test the group of participants who had fallen was
compared with the unclear group (not known whether
they had fallen or not). The strength of the correlation
can therefore only be viewed with caution.
Notably, several of the 20 features with the highest
Cramer’s V values correspond to known risk factors
for falls, such as walking disabilities, obesity and
parkinson (see Table 1). Only the back pain factor
showed no known connection to falls. Despite
the strong limitation of the data and thus the low
strength of the correlation, it was possible to identify
characteristics that are known to be associated with
falls.
4.2 Limitations of Using Operational
Data
Several inherent limitations of the JUH dataset
impacted the study’s outcomes:
• Fall incidents were not explicitly recorded
but inferred from free-text comments in the
emergency call logs. This method may have led
to underreporting, variations in terminology or
spelling errors.
• The dataset did not include explicit records
of individuals who did not experience falls,
preventing the creation of a control group.
This limitation restricted the modeling approach
to one-class classification and impeded the
evaluation of the models specificity and overall
accuracy.
• When changes are made to the data, the
previous records are simply overwritten, with
no trace left of the alterations. This lack of
historical data prevents tracking whether and
how patient information has been updated over
time. Consequently, it becomes challenging to
incorporate temporal trends and monitor changes
in patients’ conditions. Temporal data, however,
are essential for identifying patterns that may
Predicting Falls from Operational Data: Insights and Limitations of Using a Non-Specialized Database
777
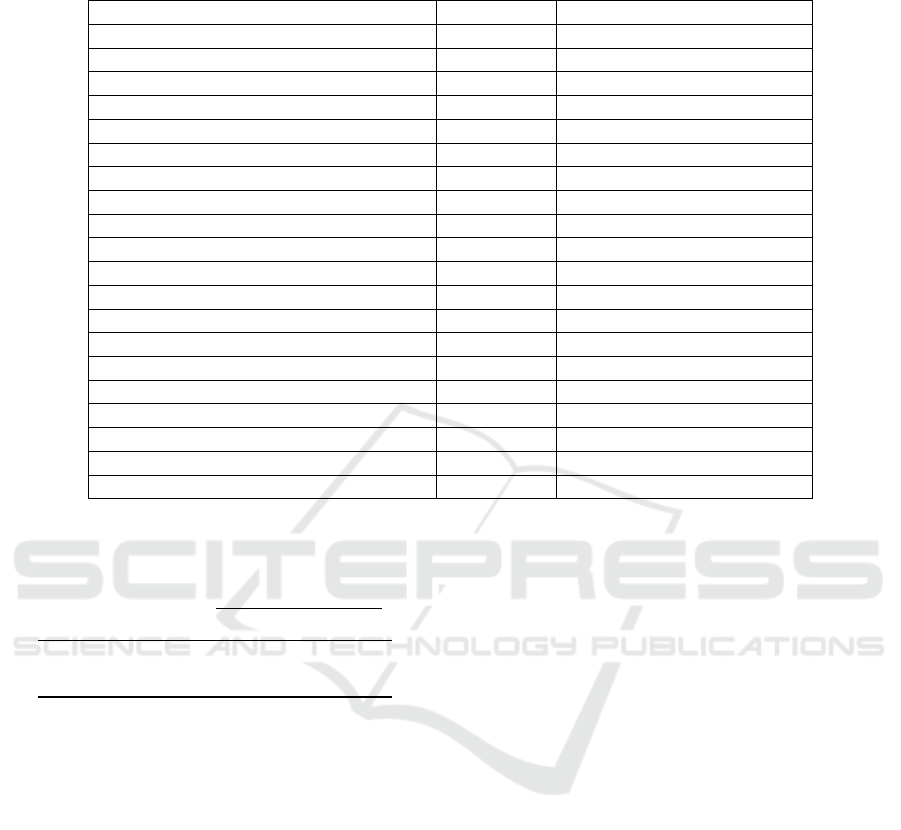
Table 1: The 20 characteristics with the highest Cramer’s V. For characteristics with a specified source, the correlation has
already been established in previous studies. For characteristics without a source, no correlation is known to date.
Feature Cramers‘V References
Walking disability 0.070856 (Bergland et al., 2003)
Degree of care 0.048084 (Palm, 2024)
Obesity 0.046093 (Fjeldstad et al., 2008)
Parkinson 0.042153 (Kerr et al., 2010)
Living condition 0.041385 (Walther et al., 2008)
Antihypertensive medication 0.040181 (Klein et al., 2013)
Hearing, seeing and walking impairment 0.039203 (Bergland et al., 2003)
Hearing aid 0.036770 (Bergland et al., 2003)
Back pain 0.031729 none
Hearing impairment 0.031387 (Bergland et al., 2003)
Arthrosis 0.030739 (Rodrigues et al., 2014)
Alcohol abuse 0.024808 (Lima et al., 2009)
Diabetes mellitus (insulin-dependent) 0.024274 (Vinik et al., 2017)
Unsteady blood pressure 0.024247 (Klein et al., 2013)
Diabetes mellitus 0.022882 (Vinik et al., 2017)
Gender 0.021822 (Stevens and Sogolow, 2005)
Hearing impaired 0.021373 (Bergland et al., 2003)
Insulin 0.020749 (Vinik et al., 2017)
Circulatory disorders 0.020547 (Jansen et al., 2016)
Apoplexy 0.020485 (Su et al., 2021)
Table 2: Confusion matrix of the one-class classification
model.
Predicted
Fallen Unknown
Actual Fallen 0.5510 0.4490
Actual Unknown 0.4485 0.5514
signal an increased risk of falls and for enhancing
the accuracy of predictive models.
• A significant proportion of records had missing
values in key features such as medical history
and medication. It was unclear whether missing
entries indicated the absence of conditions or a
lack of data entry. This uncertainty led to the
exclusion of most participants from the analysis
and potentially introduced bias.
These limitations underscore the challenges of
using operational data not originally designed for
research purpose. Data structure, completeness, and
quality significantly influence the effectiveness of ML
models in healthcare applications.
Still, it makes sense to use operational data
because it is real data. Recording data under
laboratory conditions is time-consuming, costly and
does not necessarily reflect the data in reality. Using
existing data can therefore be effective.
4.3 Recommendations for Improved
Data Collection Practices
To enhance the utility of operational datasets for
predictive modeling, the following recommendations
are proposed:
• The introduction of a structured field in the
emergency call database table in which the
operator can choose between the top n call
reasons. This change would improve the accuracy
and completeness of incident data and facilitate
more precise analyses. Additionally, large
language models (LLMs) could be employed
to classify free-text fields more effectively,
providing further insights in categorizing incident
reasons.
• Collect information on individuals who have
not experienced falls, possibly through periodic
questionnaires or assessments. Participants
could report falls or near-falls annually, along
with updates on health status and medication
changes. This data would enable the creation of
a control group and allow the use of traditional
binary classification models. We are aware
that this approach is difficult to implement and
entails significant effort, requiring considerable
resources and long-term participant commitment.
• Implement mechanisms to retain historical
HEALTHINF 2025 - 18th International Conference on Health Informatics
778

records with timestamps when updates are made
to patients information. Maintaining a temporal
record would allow for the analysis of trends
and the inclusion of time-dependent features in
predictive models, potentially enhancing their
accuracy.
• Differentiate between the absence of a condition
and missing data by including explicit indicators.
For example, use a specific code to denote
”
no
known illness“ versus
”
data not provided“. This
clarification would improve data integrity and
allow for more accurate analyses.
Implementing these recommendations might
enhance the quality and research utility of
operational datasets, facilitating more effective
predictive modeling and contributing to improved
healthcare outcomes. However, we acknowledge that
implementation can be a challenge, as this involves
highly sensitive data (e.g. medication, previous
illnesses) that requires careful handling of the data.
A balanced solution must therefore be found that
meets both the need for comprehensive data and
the requirement to minimize data in order to protect
privacy.
4.4 Contribution to the Field and
Future Work
This study contributes to the field of predictive
healthcare modeling by illustrating both the potential
and challenges of using non-specialized, operational
datasets for fall prediction among older adults. The
findings highlight the critical importance of data
quality, structure, and completeness in developing
effective ML models.
Future Work: In the future, collaboration
with data providers, such as JUH, to enhance
data collection practices can improve the quality
of operational datasets. Additionally, exploring
advanced modeling techniques, such as semi-
supervised learning, may improve the predictive
performance. Another promising area is the
integration of additional data sources, such as
electronic health records or sensor data from wearable
devices, to provide a more comprehensive view of
patient health and further enhance model accuracy.
Finally, conducting longitudinal studies that preserve
temporal data will enable a deeper analysis of how
changes over time correlate with fall risk, providing
valuable insights into long-term patient outcomes.
4.5 Conclusion
In conclusion, while operational datasets like the
JUH home emergency call records hold promise
for predictive healthcare applications, significant
challenges remain due to data limitations. The
study demonstrates that, despite certain predictive
capability exists, the effectiveness of ML models is
heavily dependent on the quality and structure of the
underlying data.
Enhancing data collection and management
practices is essential to unlock the full potential of
such datasets. By implementing the recommended
improvements, organizations could transform
operational data into more valuable resources for
research, ultimately contributing to better healthcare
outcomes for the older population.
ACKNOWLEDGMENTS
This work was carried out as part of the project
”
LivingSmart - Wohnquartiere neu gedacht –
Service-gesteuert: lebensnah, integrativ, intelligent,
innovativ“ (Elfert et al., 2023) funded by the
German Federal Ministry of Education and Research
(reference: 02K17A052). We would like to thank the
JUH, especially Alexandra Kolozis, for providing the
database used in this research.
REFERENCES
An, W., Liang, M., and Liu, H. (2015). An improved
one-class support vector machine classifier for outlier
detection. Proceedings of the institution of mechanical
engineers, part c: Journal of mechanical engineering
science, 229(3):580–588.
Becker, C. and Rapp, K. (2011). St
¨
urze in der geriatrie. Der
Internist, 52(8):939–945.
Bergland, A., Jarnlo, G.-B., and Laake, K. (2003).
Predictors of falls in the elderly by location. Aging
clinical and experimental research, 15:43–50.
Chattu, V. K. (2021). A review of artificial intelligence,
big data, and blockchain technology applications in
medicine and global health. Big Data and Cognitive
Computing, 5(3):41.
Comans, T. A., Currin, M. L., Quinn, J., Tippett, V., Rogers,
A., and Haines, T. P. (2013). Problems with a great
idea: referral by prehospital emergency services to
a community-based falls-prevention service. Injury
prevention, 19(2):134–138.
El-Bendary, N., Tan, Q., Pivot, F. C., and Lam, A. (2013).
Fall detection and prevention for the elderly: A review
of trends and challenges. International Journal on
Smart Sensing and Intelligent Systems, 6(3).
Predicting Falls from Operational Data: Insights and Limitations of Using a Non-Specialized Database
779

Elfert, P., Eichelberg, M., and Hein, A. (2023).
LivingSmart: Intelligente Auswerte- und
Informationsmodule zur Notfallpr
¨
adiktion und -
pr
¨
avention f
¨
ur hochaltrige Personen, pages 21–36.
Springer Vieweg, hmd edition.
Fjeldstad, C., Fjeldstad, A. S., Acree, L. S., Nickel, K. J.,
and Gardner, A. W. (2008). The influence of obesity
on falls and quality of life. Dynamic Medicine, 7(1):1–
6.
Jansen, C.-P., Gross, M., Kramer-Gmeiner, F.,
Blessing, U., Becker, C., and Schwenk, M.
(2021). Empfehlungspapier f
¨
ur das k
¨
orperliche
gruppentraining zur sturzpr
¨
avention bei
¨
alteren,
zu hause lebenden menschen. Zeitschrift f
¨
ur
Gerontologie und Geriatrie, pages 1–11.
Jansen, S., Bhangu, J., de Rooij, S., Daams, J., Kenny,
R. A., and van der Velde, N. (2016). The association
of cardiovascular disorders and falls: a systematic
review. Journal of the American Medical Directors
Association, 17(3):193–199.
Jansenberger, H. (2011). Sturzpr
¨
avention in Therapie und
Training. Georg Thieme Verlag.
J
¨
org L
¨
ussem, Thomas M
¨
ahnert, Hubertus v. Puttkamer
(2021). Aus liebe zum leben: Jahresbericht 2020 der
johanniter-unfall-hilfe e.v. https://assets.johanniter.
de/JUH/Bundesgeschaeftsstelle/Dokumente/
Jahresberichte/2020 Jahresbericht Johanniter.pdf.
(besucht am 26.07.2022).
Kerr, G. K., Worringham, C. J., Cole, M. H., Lacherez,
P. F., Wood, J. M., and Silburn, P. (2010). Predictors
of future falls in parkinson disease. Neurology,
75(2):116–124.
Klein, D., Nagel, G., Kleiner, A., Ulmer, H., Rehberger, B.,
Concin, H., and Rapp, K. (2013). Blood pressure and
falls in community-dwelling people aged 60 years and
older in the vhm&pp cohort. BMC geriatrics, 13:1–7.
Lima, M. C. P., Sim
˜
ao, M. O., Oliveira, J. B. d.,
Cavariani, M. B., Tucci, A. M., and Kerr-Correa, F.
(2009). Alcohol use and falls among the elderly in
metropolitan s
˜
ao paulo, brazil. Cadernos de saude
publica, 25:2603–2611.
Marschollek, M., G
¨
overcin, M., Rust, S., Gietzelt,
M., Schulze, M., Wolf, K.-H., and Steinhagen-
Thiessen, E. (2012). Mining geriatric assessment
data for in-patient fall prediction models and high-risk
subgroups. BMC medical informatics and decision
making, 12(1):1–6.
Nadash, P., Doty, P., and von Schwanenfl
¨
ugel, M.
(2018). The german long-term care insurance
program: evolution and recent developments. The
Gerontologist, 58(3):588–597.
Nicholas, P. K. and Smith, M. F. (2006). Demographic
challenges and health in germany. Population
Research and Policy Review, 25:479–487.
Palm, R. (2024). Inkontinenz und st
¨
urze erschweren die
pflege zu hause. MMW-Fortschritte der Medizin,
166(3):40–41.
Pfortmueller, C. A., Kunz, M., Lindner, G., Zisakis, A.,
Puig, S., and Exadaktylos, A. K. (2014). Fall-related
emergency department admission: fall environment
and settings and related injury patterns in 6357
patients with special emphasis on the elderly. The
Scientific World Journal, 2014.
Rodrigues, I. G., Fraga, G. P., and Barros, M. B. d. A.
(2014). Falls among the elderly: risk factors in
a population-based study. Revista Brasileira de
Epidemiologia, 17(3):705–718.
Stevens, J. A. and Sogolow, E. D. (2005). Gender
differences for non-fatal unintentional fall related
injuries among older adults. Injury prevention,
11(2):115–119.
Su, Q., Gao, Y., Zhang, J., Tang, J., Song, M., Song, J.,
Mao, Y., and Pi, H. (2021). Prevalence of fear of
falling and its association with physical function and
fall history among senior citizens living in rural areas
of china. Frontiers in public health, 9.
Usmani, S., Saboor, A., Haris, M., Khan, M. A., and Park,
H. (2021). Latest research trends in fall detection
and prevention using machine learning: a systematic
review. Sensors, 21(15):5134.
Vinik, A. I., Camacho, P., Reddy, S., Valencia, W. M.,
Trence, D., Matsumoto, A. M., and Morley, J. E.
(2017). Aging, diabetes, and falls. Endocrine
practice, 23(9):1120–1142.
Vuppalapati, J. S., Kedari, S., Ilapakurti, A., Vuppalapati,
C., Vuppalapati, R., and Kedari, S. (2019). Machine
learning infused preventive healthcare for high-risk
outpatient elderly. In Intelligent Systems and
Applications: Proceedings of the 2018 Intelligent
Systems Conference (IntelliSys) Volume 2, pages 496–
511. Springer.
Walther, L., Nikolaus, T., Schaaf, H., and H
¨
ormann, K.
(2008). Schwindel und st
¨
urze im alter. HNO,
56(8):833–842.
Zeeh, J., Reinhardt, Y., and Heppner, H.-J. (2017). St
¨
urze
im alter. MMW-Fortschritte der Medizin, 159(13):52–
58.
HEALTHINF 2025 - 18th International Conference on Health Informatics
780
