
The Role of Digital Health Literacy and Socioeconomic Factors in
Colorectal Cancer Screening: Machine Learning Analysis of
HINTS Data
Sujin Kim
1a
, Madhav Dahal
1b
, Avinash Bhakta
2c
and Jihye Bae
3d
1
Division of Biomedical Informatics, University of Kentucky, 725 Rose Street, Lexington, KY, U.S.A.
2
Deptment of Electrical and Computer Engineering, University of Kentucky, 512 Administration Drive, Lexington, KY, U.S.A.
3
Department of Surgery, University of Kentucky, 800 Rose Street, Lexington, KY, U.S.A.
Keywords: Colorectal Cancer Screening, Digital Health Literacy, Socioeconomic Factors, Machine Learning,
Health Information National Trend Surveys (HINTS).
Abstract: While colorectal cancer (CRC) screening rates are on the rise, significant disparities persist, particularly
among underserved populations, highlighting ongoing challenges in achieving equitable access to preventive
care. This study utilizes machine learning models to analyze multi-year data from the Health Information
National Trends Survey (HINTS), identifying critical factors influencing CRC screening adherence across
three distinct time periods (2003–2008, 2011–2013, 2018–2020). Using Random Forest and Logistic
Regression models, interpreted through Shapley Additive exPlanations values, we examine the impact of
sociodemographic characteristics, digital health engagement, and digital literacy on CRC screening behaviors.
Findings reveal that age, prior screening behavior, and digital literacy are key predictors; individuals with
higher digital literacy, for example, exhibited a 22% higher likelihood of adhering to CRC screening
guidelines. Age emerged as a dominant factor, with screening rates peaking at 43% in the 50–64 age group.
These results suggest that interventions targeting digital health literacy and enhancing provider
communication may effectively improve CRC screening rates among underserved populations. This study
underscores the value of data-driven approaches in informing public health strategies to increase CRC
screening adherence and reduce health disparities.
1 INTRODUCTION
Colorectal cancer (CRC) remains one of the most
prevalent cancers globally and is the second leading
cause of cancer-related deaths, even as advancements
in screening and treatment have contributed to
declining incidence and mortality rates (Siegel, 2022;
Bray, 2018). In the United States, CRC
predominantly affects adults aged 65-74, with
screening rates increasing over recent decades due to
the adoption of colonoscopy and non-invasive
methods such as multitarget stool DNA (FIT-DNA)
testing (Keum, 2019). However, a concerning trend is
the rising incidence of early-onset colorectal cancer
(EOCRC) among adults under 50, a rate projected to
a
https://orcid.org/0000-0002-7878-4322
b
https://orcid.org/0009-0002-1016-428X
c
https://orcid.org/0000-0003-2471-3681
d
https://orcid.org/0000-0002-6609-9782
Corresponding Author: sujinkim@uky.edu
double by 2030 and driven by complex, interacting
risk factors not fully understood (Zhen, 2024; Sun,
2024). Disparities in CRC screening persist,
influenced by sociodemographic factors such as
income, education, and race, as well as health
behaviors. These multifaceted barriers, often studied
in isolation, underscore the need for a more integrated
approach to understanding and addressing CRC
screening uptake.
Digital health interventions, including telehealth,
patient portals, and mobile health (mHealth)
applications, offer promising avenues to address these
complex challenges in CRC screening by making
screening information, reminders, and test results
more accessible to diverse populations (Miller, 2018;
228
Kim, S., Dahal, M., Bhakta, A. and Bae, J.
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data.
DOI: 10.5220/0013310700003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 228-239
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.

McIntosh, 2024). For instance, studies have shown
that digital health interventions can improve
screening adherence in vulnerable groups compared
to standard care, and patient portal reminders paired
with mailed test kits have increased adherence among
average-risk populations (Miller, 2018; McIntosh,
2024). The Health Information National Trends
Survey (HINTS) provides a valuable, nationally
representative dataset on health behaviors, digital
literacy, and sociodemographic factors that impact
CRC screening. Leveraging machine learning (ML)
such as Random Forest (RF) and Logistic Regression
(LR) to analyze multi-year HINTS data enables the
identification of nuanced relationships among digital
health literacy, socioeconomic variables, and
screening adherence, offering a more holistic, data-
driven approach to improve CRC screening rates and
reduce disparities in an increasingly digital healthcare
environment.
2 BACKGROUNDS
CRC screening uptake is shaped by a wide range of
demographic, psychosocial, and access-related
factors. Insights from the HINTS dataset reveal
crucial predictors that influence CRC screening
decisions, providing a nuanced view of how different
factors affect adherence. For example, Atarere
(2024c) found that smokers are 30% less likely to
adhere to CRC screening protocols than non-smokers,
highlighting the potential of health information
technology interventions to increase participation
among high-risk groups (Atarere, 2024b). Further,
Atarere et al. (2024) reported that patients engaged in
telehealth primary care visits had a 20% higher
likelihood of discussing CRC screening with their
providers, suggesting that Health IT (HIT) tools like
telehealth can significantly improve screening
discussions and adherence in populations typically
resistant to CRC screening (Atarere, 2024a; Atarere,
2024c).
Beyond access to HIT, cultural and social
influences are critical in shaping CRC screening
behaviors. Jun and Oh (2013) found that cancer
fatalism among Asian and Hispanic Americans was
associated with a 15% reduction in CRC screening
likelihood, pointing to cultural perceptions as barriers
to uptake. Similarly, Idowu et al. (2016) observed that
U.S. adults born outside the United States were 18%
less likely to be up-to-date with CRC screening,
underscoring the informational and cultural barriers
faced by immigrant populations. Additionally,
Finney Rutten et al. (2009) found that only 56% of
the general public understood CRC risk and
prevention guidelines accurately, linking low public
knowledge to reduced screening adherence. These
findings highlight a complex interplay of
sociocultural and informational barriers, which
Nawaz et al. (2014) further supported by showing that
CRC screening offered in hospital settings resulted in
a 35% higher uptake rate, suggesting that more
accessible, opportunistic screening efforts could be
effective in improving national screening rates.
Early studies using HINTS 123 data (2003–2008)
identified foundational barriers to CRC screening,
including limited awareness, inadequate knowledge
of guidelines, and socioeconomic and cultural
disparities. For instance, Geiger et al. (2008),
analyzing HINTS 1 data, pinpointed knowledge gaps
and access issues as central barriers. Similarly, Hay et
al. (2006) reported that perceived risk was a decisive
factor in CRC screening uptake, with substantial
demographic differences in risk perception. More
recent HINTS data (HINTS 5, 2018-2020), however,
indicate a shift toward increased digital literacy and
greater use of HIT, both of which are positively
correlated with screening adherence. The growth of
telehealth and online health resources appears to
support CRC screening behaviors, marking a
significant change in how technology influences
preventive health actions.
ML applications in CRC research have
increasingly used electronic health record (EHR) data
to enhance predictive models, especially in EOCRC
studies. For example, studies by Sun et al. (2024) and
Zhen et al. (2024) showed high predictive accuracy
for EOCRC among individuals under the standard
screening age, with area under the curve (AUC)
scores reaching up to 0.888 when using RF models.
These studies illustrate the clinical value of EHR data
in identifying risk factors such as immune and
digestive disorders, allowing for the development of
models that can flag high-risk patients who may
benefit from early diagnostic interventions.
While EHR-based ML models provide valuable
insights into clinical risk factors, they often overlook
behavioral elements influencing CRC screening
adherence, such as health literacy, digital literacy, and
risk perception—areas extensively covered in the
HINTS dataset. Unlike EHR data, which primarily
capture clinical encounters, HINTS data offer a
comprehensive view of health behaviors, allowing for
broader exploration of sociobehavioral factors like
health literacy and digital engagement. Integrating
these broader factors is essential for understanding
screening behaviors, as digital literacy,
socioeconomic status, and perceived cancer risk have
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data
229

become key determinants of screening adherence,
especially with the evolution of HIT over time.
In this study, we examine these broader
behavioral factors by analyzing HINTS data across
three significant temporal milestones—HINTS 123
(2003-2008), HINTS 4 (2011-2013), and HINTS 5
(2018-2020). This approach allows us to track
changes in CRC screening attitudes, HIT
engagement, and health information access over
nearly two decades. By combining HINTS data with
ML, we aim to uncover complex, time-varying
relationships between behavioral factors and
screening outcomes, thereby informing tailored
interventions designed to improve CRC screening
rates across diverse populations.
3 METHODS
3.1 Data Source and Study Variables
The HINTS datasets offer a robust, nationally
representative sample capturing U.S. adults' cancer
knowledge, perceptions, information-seeking
behaviors, and digital health tool adoption over time.
Each HINTS cycle introduces unique variables to
reflect emerging HIT trends, while maintaining core
questions that allow for cross-cycle comparisons on
foundational topics such as cancer knowledge,
perception, and health information access. For this
study, we grouped three survey cycles within each of
three temporal groups, focusing on CRC screening-
related variables while noting differences in HIT
priorities across cycles:
• Group 1: Merged HINTS Cycles 1-3 (2003,
2005, 2008) – This grouping consolidates early
cycles with a focus on CRC-related variables,
including “Awareness of CRC screening,”
“Frequency of CRC screening conversations
with healthcare providers,” and “CRC screening
completion history.” Predating widespread
digital tool adoption, this group establishes a
baseline of public knowledge and screening
behaviors (Ford, 2006; Geiger, 2008; Hay,
2006).
• Group 2: Merged HINTS Cycle 4 (2011, 2012,
2013) – Reflecting the era’s shift toward digital
health adoption, this group includes variables
like “Access to EHRs,” “Use of telehealth for
health information,” and “Frequency of patient
portal usage,” though certain CRC-specific
questions are omitted in favour of HIT-focused
variables.
• Group 3: Merged HINTS Cycle 5 (2018, 2019,
2020) – Emphasizing advanced HIT usage and
digital health literacy, this group includes
variables such as “Confidence in locating reliable
health information online,” “Frequency of
telehealth usage,” and “Patient portal
engagement for preventive care.” Although
CRC-specific questions are less prominent,
consistent HIT variables allow for comparison
across cycles.
This grouping allows for a comprehensive
examination of CRC screening behaviors over time,
highlighting the growing influence of digital tools on
CRC engagement. The primary outcome variable,
Ever_Tested_Colon, is binary, coded as 1 for
individuals who reported undergoing a colorectal
cancer screening test and 0 for those who did not.
Predictor variables include multiple categories
representing demographic characteristics (e.g., age,
gender, race/ethnicity), socioeconomic status (e.g.,
income, education level), health behaviors (e.g.,
smoking status, physical activity), access to
healthcare (e.g., health insurance coverage, regular
healthcare provider), and digital health engagement
(e.g., frequency of internet use for health information,
use of electronic health records, and telehealth usage).
This comprehensive set of predictors allows for a
nuanced analysis of factors influencing CRC
screening uptake, considering both individual health
characteristics and the broader context of healthcare
access and technology use.
3.2 Data Processing and Feature
Engineering
To ensure data consistency across cycles, we
standardized variable names using the HINTS 5
Cycle 4 format and encoded all categorical variables
numerically. Race was expanded into binary
indicators (Hispanic, White, Black, Asian, and
Other), and marital status was binarized, with
“Married” coded as 1 and all others as 0. Missing
values were replaced with -1 to retain cases, with
verification that imputing -1 did not distort
predictions. Group 1’s multiple-response categorical
variables were converted into binary format for
simplicity, and non-informative variables, duplicates,
and weight variables were excluded. Feature selection
focused on variables consistently present across
cycles, including demographics, health information-
seeking behaviors, digital health adoption, and CRC
screening history. Final dataset sizes were 11,710
rows and 1,022 columns for Group 1, 10,534 rows
HEALTHINF 2025 - 18th International Conference on Health Informatics
230

and 475 columns for Group 2, and 12,391 rows and
535 columns for Group 3, where each row indicates
each individual sample, and each column represents
variables extracted from HINTS datasets.
3.3 Predictive Model Development
This study utilized Python (version 3.8) within the
Google Colab environment, leveraging cloud
resources for efficient data processing, model
training, and interpretation. Key libraries included
Pyreadstat for SAS file handling, Pandas and NumPy
for data manipulation, and Scikit-Learn for machine
learning model implementation, pre-processing, and
validation. Model interpretability was achieved using
SHapley Additive exPlanations (SHAP), enabling a
detailed examination of feature contributions to
specific predictions. All data were securely accessed
and processed via Google Drive integration, ensuring
data consistency and reproducibility. Regarding
ethics and data privacy, this study exclusively
analysed publicly available, de-identified data from
the HINTS thereby maintaining strict confidentiality
and compliance with data privacy standards. As no
personally identifiable information (PII) was present,
this secondary data analysis was exempt from
Institutional Review Board (IRB) oversight.
We employed two predictive models, Random
Forest (RF) and Logistic Regression (LR) with
Elastic Net regularization, to predict colorectal cancer
(CRC) screening outcomes (CRC Screened or Not).
Following Min-Max normalization, 15% of the
dataset was allocated for testing. Hyperparameter
optimization was conducted through 5-fold cross-
validation using a grid search approach. For RF, we
searched across key hyperparameters, including the
number of trees (n_estimators: 100–500, step 50),
maximum tree depth (max_depth: 5–20, step 1),
minimum samples required to split a node
(min_samples_split: 2–10, step 1), and minimum
samples per leaf node (min_samples_leaf: 1–5, step
1). For LR, optimization included searching over
regularization strength (C: 0.1–1.0, step 0.1), the
balance between L1 and L2 penalties (l1_ratio: 0.5–
0.9, step 0.1), and iteration limits (max_iter: 100–
1000, step 100). The configurations yielding the
highest average cross-validation accuracy were
applied to the testing set, with performance evaluated
across key metrics: accuracy, precision, recall, F1
score, and area under the curve (AUC) (Table 3).
The optimal hyperparameters for RF varied
across datasets. For HINTS123, the best RF
configuration included 400 trees, a maximum depth
of 12, a minimum of 7 samples per split, and 2
samples per leaf, achieving a cross-validation
accuracy of 98.25%. In HINTS4, the optimal
configuration used 400 trees, a depth of 14, a
minimum of 8 samples per split, and 1 sample per
leaf, achieving a cross-validation accuracy of
81.84%. For HINTS5, the best RF model used 400
trees, a depth of 15, 9 samples per split, and 2 samples
per leaf, with a cross-validation accuracy of 80.61%.
For LR, the optimal configuration across datasets
involved a regularization strength of 0.1, an L1/L2
ratio of 0.5, and 800 iterations, yielding a cross-
validation accuracy of 80.86% in HINTS5. Test set
performance metrics for both models across datasets
were summarized in Table 3, demonstrating the
models' strengths in predicting CRC screening
outcomes under varying data conditions.
3.4 Model Interpretability with SHAP
Analysis
To interpret model predictions and identify top
predictors of CRC screening, we calculated SHAP
values for the optimized RF model. SHAP values
were chosen for their consistency and additive feature
contributions, providing insights into how each
variable influence on the CRC screening prediction.
Focusing on the 15 most impactful variables in each
group, we visualized these features to clarify the key
drivers of CRC screening across different periods and
demographic groups. This interpretability step
enhances our understanding of the predictors behind
screening behaviors and the evolving role of HIT.
This methodology—combining multiple HINTS
cycles, consistent variable standardization, and
advanced modelling with interpretability—offers a
comprehensive, time-sensitive analysis of CRC
screening behaviors. By integrating SHAP analysis,
we achieved transparent, interpretable predictions,
allowing us to pinpoint essential factors influencing
CRC screening adherence across various
demographic and HIT-related contexts.
4 RESULTS
4.1 Patient Characteristics of CRC
Screened or not
Across the three groups, CRC screening uptake
showed a clear upward trend over time. In Group 1
(2003–2008), the screening rates started with 40.12%
tested in 2003, dipping to 33.33% in 2005, and rising
to 37.52% in 2008, resulting in an overall group rate
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data
231

of 36.94% tested. Group 2 (2011–2013) saw a more
substantial increase, with a 50.02% overall screening
rate, increasing steadily from 49.32% in 2011 to
52.28% in 2013. Group 3 (2018–2020) had the
highest screening rates, with a group average of
62.15%. Notably, 60.90% were tested in 2018,
60.02% in 2019, and this rose to 64.49% by 2020.
This progression highlights a positive trend in CRC
screening uptake, suggesting increased awareness
and access to screening over the years.
SES Characteristics Among Three Groups
Table 1 presents a comparison of socioeconomic
(SES) and digital factors among CRC screening-
tested individuals across the three HINTS groups in
abridged format highlighting underserved groups,
while Appendix A provides comprehensive details
on additional variables. The findings from Table 1
reveal significant disparities in colorectal cancer
(CRC) screening rates among underserved
populations, particularly when compared to their
counterparts—groups not explicitly represented in
the table. Individuals aged 18–49 years displayed
consistently lower screening participation, with rates
rising from 5.36% in Group 1 to 10.90% in Group 2
but falling again to 7.56% in Group 3. In contrast,
their counterparts aged 50 and above, particularly the
50–64 age group, dominated screening adherence,
consistent with guideline recommendations targeting
this demographic. This trend highlights a critical age
disparity, emphasizing the need for enhanced
outreach and interventions tailored to younger
populations.
Table 1: Comparison of CRC Screening Tested Amon
g
Three HINTS group – Underserved.
Variable Category
Group
1
Tested
N (%)
Group
2
Tested
N (%)
Group
3
Tested
N (%)
Age 18-49
232
(5.36)
574
(10.90)
582
(7.56)
Gender Female
2735
(63.22)
2969
(56.35)
4327
(56.19)
Educatio
n
< 12
y
ears
409
(9.45)
484
(9.18)
519
(6.75)
Income < $20K
661
(15.28)
971
(18.43)
1269
(16.48)
Employ
ment
Unempl
o
y
e
d
2732
(63.15)
3099
(58.82)
2729
(35.44)
Race
Non-
White
826
(19.07)
2101
(39.88)
3146
(40.88)
Further disparities emerged in education and income
levels. Individuals with less than a high school
education (<12 years) showed persistently lower
screening rates, declining from 9.45% in Group 1 to
6.75% in Group 3. Compared to individuals with at
least a high school diploma or higher, this group
remains significantly underserved, underscoring the
influence of education and health literacy on
screening adherence. Similarly, CRC screening
among individuals earning below $20,000 annually
increased from 15.28% in Group 1 to 18.43% in
Group 2 but slightly dropped to 16.48% in Group 3.
This income disparity reflects barriers such as
affordability and access to preventive healthcare,
which disproportionately affect lower-income
populations.
Racial disparities were also notable, with non-
White populations increasing their representation
from 19.07% in Group 1 to 40.88% in Group 3. While
this improvement is promising, non-White
individuals remain under-screened compared to
White populations, who consistently demonstrate
higher screening rates. Gender and employment
disparities also persisted; although females
consistently represented a higher proportion of those
screened, their participation rates declined from
63.22% in Group 1 to 56.19% in Group 3.
Conversely, males, historically less represented in
screening, may have experienced incremental
improvements over time. Meanwhile, unemployed
individuals saw significant reductions in screening
rates—from 63.15% in Group 1 to 35.44% in Group
3—remaining significantly underserved compared to
their employed counterparts, who likely benefit from
better healthcare access.
In summary, underserved groups—such as
younger individuals aged 18–49, those with lower
educational attainment, lower incomes,
unemployment, and non-White populations—
consistently lag behind their counterparts (older
individuals, those with higher education or income,
the employed, and White populations) in CRC
screening participation. These disparities highlight
the need for targeted public health interventions,
policy reforms, and culturally sensitive outreach
strategies to promote CRC screening among these
vulnerable groups. Addressing these gaps is essential
to reducing health inequities and improving
population-level outcomes.
HEALTHINF 2025 - 18th International Conference on Health Informatics
232
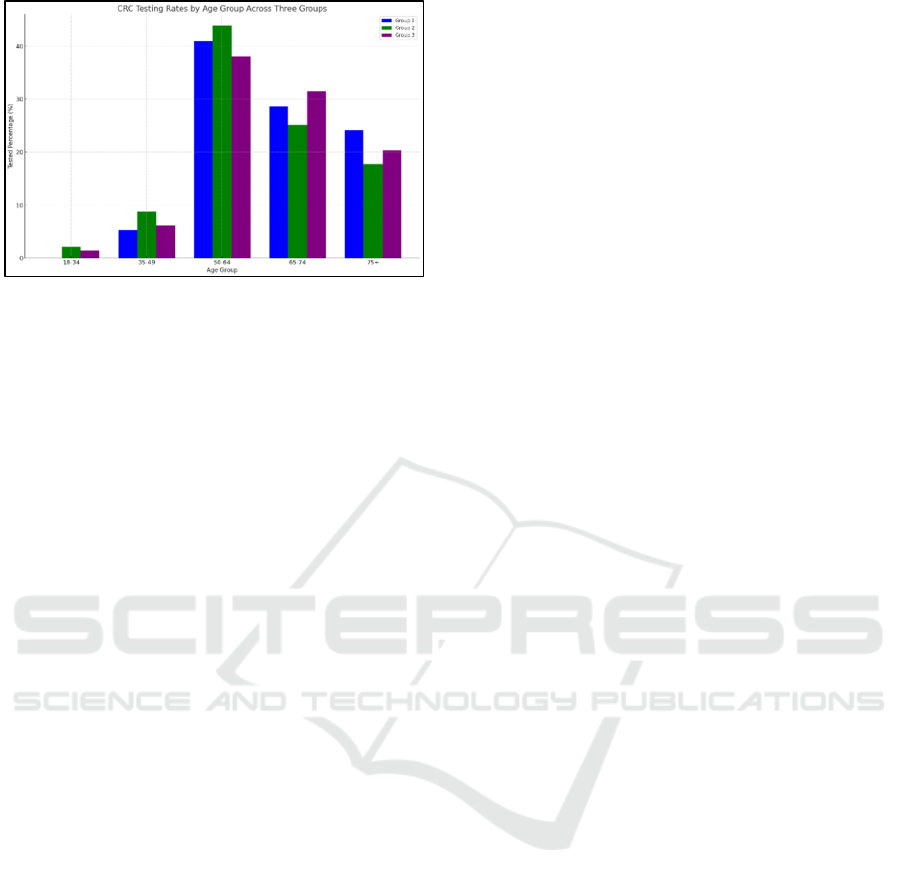
Figure 1: CRC Screening Uptake by Age Groups Among 3
HINTS Groups.
Our further findings on age-specific screening
reflect the impact of recent screening uptake policy
recommendations. Updates to CRC screening
guidelines by the American Cancer Society (ACS)
and the U.S. Preventive Services Task Force
(USPSTF), which now recommend initiating CRC
screening at age 45, may be contributing to a modest
increase in screening rates among individuals aged
45-49, particularly in Groups 2 and 3 (Atarere,
2024b). Figure 1 reveals a gradual increase in testing
rates within the 30-49 age bracket, which could
indicate early adoption of these guideline shifts by
healthcare providers and patients. However,
screening rates for those under 50 remain low
compared to older age groups, highlighting an area
with significant potential for improving adherence.
In the 50-64 age group, screening rates reach their
peak, confirming this as the primary age range for
CRC screening. As shown in Figure 1, Group 2 leads
with a screening rate of 43.88%, followed closely by
Group 1 at 40.92% and Group 3 at 38.06%. This
pattern reflects the age group's alignment with
recommended screening ages and highlights the
effectiveness of CRC screening initiatives targeted
toward this demographic. Recent studies indicate that
high adherence in this group is often driven by regular
healthcare provider recommendations and routine
medical care access (Atarere, 2024b; Wu, 2022).
Among older adults aged 65-74, screening rates
remain substantial, likely due to Medicare coverage,
which facilitates preventive screenings. Figure 1
illustrates that Group 3 has the highest adherence at
31.58%, followed by Group 1 at 28.62% and Group 2
at 25.09%. The sustained adherence in this age group
is likely bolstered by Medicare's support for routine
screenings, as well as a focus on preventive health
among this population (Atarere, 2024a). Group 3’s
elevated rate could reflect improved preventive health
practices among the cohort or more proactive
Medicare utilization.
In the 75+ age group, CRC screening rates drop
markedly, which aligns with current guidelines that
discourage routine screening for older seniors due to
increased procedural risks and lower expected
benefit. In Figure 1, Group 1 has the highest rate at
24.23%, followed by Group 3 at 20.31% and Group 2
at 17.73%. This decline may reflect adherence to
recommendations, though the relatively higher rate in
Group 1 suggests that some seniors continue
screening based on individual decisions or physician
recommendations, despite standard guidelines
(Atarere, 2024c).
Overall, Figure 1, Table 1, and Appendix A
collectively underscore age as a critical factor in CRC
screening uptake, with the highest adherence
observed in the 50-64 and 65-74 age groups. The
variations across groups reveal stronger adherence in
the 50-64 range for Group 2 and the highest rates in
the 65-74 range for Group 3, highlighting the role of
Medicare in supporting screening behaviors. These
findings suggest that CRC screening is highly age-
dependent, following established guidelines, with
Figure 1 clearly depicting age-specific screening
trends. This evidence points to a need for targeted
strategies to improve screening rates among younger
adults, who remain under-screened.
Digital Characteristics Among Three Groups
The findings in Table 2 reveal evolving trends in
digital connectivity, device ownership, and access to
health information resources among CRC-screened
individuals across three HINTS groups. Internet
usage has significantly increased over time, with
Group 3 showing the highest rate at 76.73%,
compared to 69.39% in Group 2 and 54.65% in Group
1, indicating a growing reliance on the internet for
health-related information and resources. Among
connection types, broadband, Wi-Fi, and mobile
internet use have also expanded in recent groups, with
mobile access (“Cell” in Table 2) notably rising from
21.94% in Group 2 to 39.54% in Group 3,
underscoring a shift toward mobile connectivity and
more flexible access to health information.
Device ownership also demonstrates upward
trends, particularly in smartphone ownership, which
reached 71.5% in Group 3, and tablet ownership,
rising from 9.47% in Group 2 to 53.6% in Group 3.
This increased adoption of mobile and digital devices
likely supports easier access to health resources,
potentially influencing CRC screening behaviors.
Access to electronic health information similarly
improved across groups, with 65.03% of CRC-tested
individuals in Group 3 accessing digital health
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data
233

resources, up from just 15% in Group 1, reflecting an
increase in both digital engagement and the
availability of electronic health information systems
in recent years. Social media engagement saw a
dramatic rise as well, from 13.44% in Group 2 to
57.17% in Group 3, suggesting an emerging role of
social media in health information dissemination and
community support for CRC-screened individuals.
Table 2: Digital Factors Comparison Across Three HINTS
Groups - CRC Screening Tested.
Variable Category
Group
1
Tested
4326
(100%)
Group
2
Tested
5269
(100%)
Group
3
Tested
7701
(100%)
Use Internet Yes
2364
(54.65)
3656
(69.39)
5909
(76.73)
Internet
Type
Dial-Up n/s
272
(5.56)
166
(2.16)
Cell n/s
1156
(21.94)
3045
(39.54)
Broadband n/s
2551
(48.42)
1915
(24.87)
Wi-Fi n/s
1968
(37.35)
4221
(57.41)
Where Use
Internet
Home
1630
(37.68)
n/s
3323
(43.15)
Work
78
(1.8)
n/s
1535
(19.93)
Public
Place
n/s n/s
33
(0.43)
Mobile n/s n/s
3286
(42.67)
Electronic
Health Info
Accessed
649
(15)
2860
(54.28)
5008
(65.03)
Health
Device
Owner
Tablet n/s
499
(9.47)
4128
(53.6)
Smartphone n/s
633
(12.01)
5506
(71.5)
Social
Media
Visited n/s
708
(13.44)
4403
(57.17)
Electronic
Medical
Record
Maintained
1225
(28.32)
4684
(88.9)
6543
(84.96)
Provider
Access
Online
Offered n/s n/s
3374
(43.81)
Health
Tracking
Devices
Wearable n/s n/s 1222
(15.87)
Healthcare provider-driven digital health
initiatives also saw substantial growth. By Group 3,
84.96% of respondents reported that their provider
maintained EHRs, and 43.81% had online access to
their health records, indicating expanding digital
infrastructure that may be contributing to preventive
health engagement, including CRC screening.
Additionally, wearable health-tracking devices were
more commonly used in Group 3, with 15.87%
reporting usage, which suggests an increasing
emphasis on self-monitoring and preventive actions
that could positively impact CRC screening
adherence.
However, an important limitation is the presence
of several "n/s" (not surveyed) entries, indicating that
specific questions were omitted in certain HINTS
cycles. This inconsistency limits our ability to
conduct longitudinal comparisons for some digital
factors, such as types of internet connections, usage
locations, and wearable health-tracking device
adoption. While trends are apparent, these gaps
suggest caution when interpreting results as fully
representative across all cycles. This limitation
emphasizes the need for more consistent data
collection in future cycles to enable comprehensive
trend analysis over time.
Figure 2a: SHAP graph of Group 1 (HINTS123).
4.2 Feature Selection – Critical Factors
Influencing CRC Screening Uptake
Overall Features Among Three Groups
The SHAP analysis across Groups 1, 2, and 3
highlights the most influential factors impacting CRC
screening adherence over time. In Group 1 (2003–
2008), recent fecal occult blood test (FOBT) behavior
(FOB1Yr) emerged as the most impactful feature,
with individuals who had previously undergone
FOBT screening being significantly more likely to
adhere to CRC screening recommendations. This
aligns with the importance of reinforcing preventive
behaviors through past engagement. Related features,
such as stool blood test timing
(BR88WhenStoolBlood, BR89WhyStoolBlood), and
endoscopic procedure timing (EndoYrs), also showed
substantial contributions, emphasizing the role of
HEALTHINF 2025 - 18th International Conference on Health Informatics
234
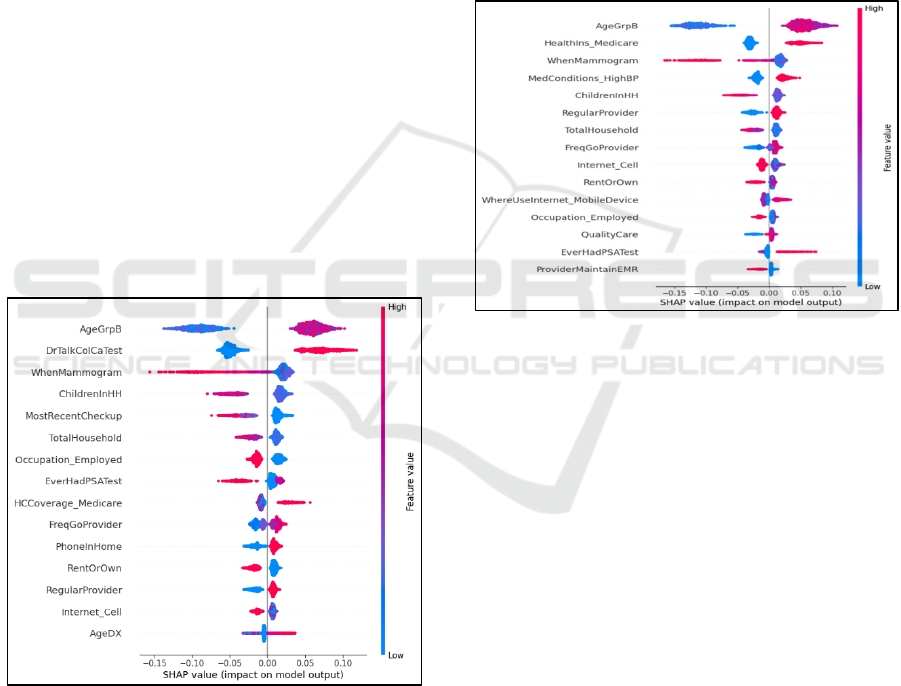
recent screening experiences and provider
recommendations in fostering adherence during this
earlier period. Demographic factors like age
(AgeGrpB) and socioeconomic elements, while
included, played a less dominant role. Figure 2a
shows 15 important features from Group 1.
Extended
Features for further analysis are included in
Appendix B.
In Group 2 (2011–2013), age (AgeGrpB) became
the most significant predictor, reflecting the growing
adherence to age-specific screening guidelines. The
importance of healthcare provider discussions about
CRC screening (DrTalkColCaTest) was also
prominent, highlighting the critical role of provider-
patient communication in increasing screening
uptake. Preventive health behaviors, such as
mammogram participation (WhenMammogram) and
PSA test history (EverHadPSATest), emerged as
secondary influencers, suggesting that individuals
engaged in other preventive health measures were
more likely to comply with CRC screening. Notable
contextual features included household composition
(ChildrenInHH) and routine healthcare checkups
(MostRecentCheckup), which indicated that family
settings and regular medical care contributed to
adherence during this period. Figure 2b shows 15
important features from Group 2.
Figure 2b: SHAP graph of Group 2 (HINTS4).
In Group 3 (2018–2020), the relative importance of
digital health literacy and access to healthcare
resources became increasingly evident. Age
(AgeGrpB) remained the most significant predictor,
but health insurance coverage through Medicare
(HealthIns_Medicare) and preventive health
behaviors, such as mammograms
(WhenMammogram), gained prominence. Features
related to chronic health conditions
(MedConditions_HighBP) and consistent provider
relationships (RegularProvider) also demonstrated
meaningful contributions. Moreover, digital
engagement variables like internet use through
mobile devices (WhereUseInternet_MobileDevice)
and electronic medical record (EMR) maintenance by
providers (ProviderMaintainEMR) highlighted the
increasing role of digital tools in influencing
screening behaviors. These shifts reflect the growing
integration of digital health technologies and access
disparities into screening decision-making. Figure 2c
shows 15 important features from Group 3.
Figure 2c: SHAP graph of Group 3 (HINTS5).
The SHAP analysis underscores the evolving
predictors of CRC screening adherence, with a shift
from prior screening behaviors and demographic
factors in earlier groups (Group 1) to greater
emphasis on healthcare provider interactions,
preventive health engagement, and digital health
access in later groups (Groups 2 and 3). This
evolution highlights the importance of adapting
public health strategies to leverage digital tools and
target demographic disparities while reinforcing the
role of consistent healthcare provider engagement in
promoting screening adherence.
Digital Features Among Three Groups
In order to focus on critical digital factors, Figure 3
provides a comparative overview of key digital
engagement trends across three HINTS groups,
highlighting significant shifts in digital health
utilization over time. Our findings include:
• Mobile Device and Internet Usage: "
MobileDevice" and "Internet_Cell" consistently
rank high in importance across all groups,
reflecting a growing reliance on mobile and
cellular internet access for health information
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data
235
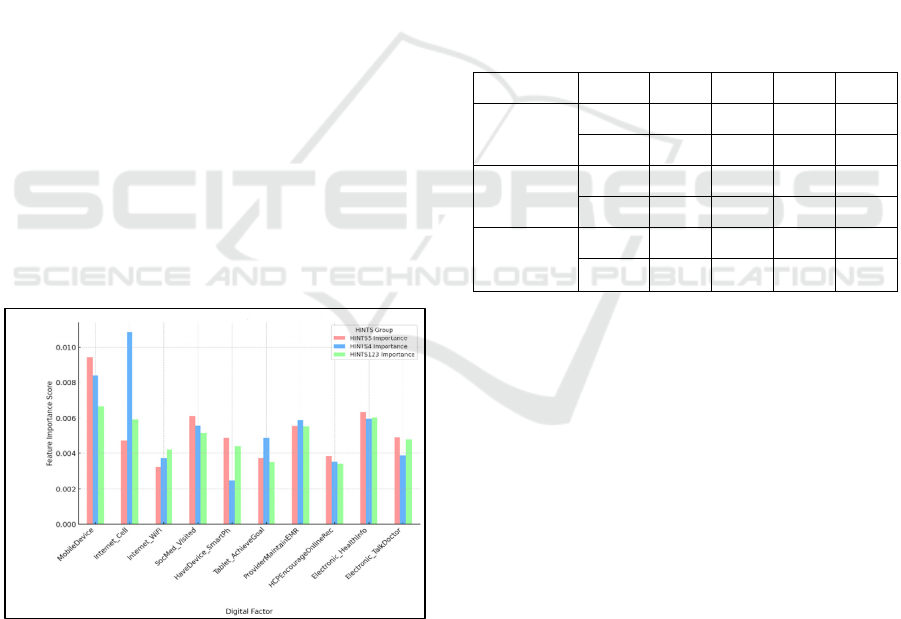
and engagement across Group 1 (HINTS123),
Group 2 (HINTS4), and Group 3 (HINTS5).
• Social Media Engagement: "SocMed_Visited"
shows persistent significance across all groups,
underscoring social media’s role as a major
platform for health-related digital interactions,
particularly for sharing and seeking health
information.
• Device Ownership: Variables like
"HaveDevice_SmartPh" and
"Tablet_AchieveGoal" score higher in Group 3
(HINTS5) and Group 1 (HINTS123), suggesting
a substantial increase in smartphone and tablet use
for health purposes, which supports broader
digital access and convenience in recent years.
• Provider Digital Interactions:
"ProviderMaintainEMR" and
"HCPEncourageOnlineRec" reach their highest
scores in Group 3 (HINTS5), indicating a
strengthened focus on provider-supported digital
health tools, particularly electronic medical
records (EMR), demonstrating deeper integration
of digital interactions within healthcare over time.
• Electronic Health Information Access:
"Electronic_HealthInfo" and
"Electronic_TalkDoctor" have significantly
higher scores in recent groups, particularly in
Group 3 (HINTS5) and Group 2 (HINTS4),
reflecting an upward trend in patients’ access to
electronic health information and digital
communication with healthcare providers.
Figure 3: Comparison of Critical Digital Factors Across
three HINTS groups.
Overall, Figure 3 illustrates a progressive shift
toward digital health resources across the HINTS
groups, marked by increasing mobile internet usage,
social media engagement, provider-supported digital
tools, and enhanced electronic health information
access. This trend underscores the expanding role of
digital tools in facilitating health engagement and
access over time, and subsequent analyses will focus
on these key digital factors to evaluate their impact on
health behaviors and outcomes.
4.3 Comparison of the Machine
Learning Models’ Performance for
CRC Screening Uptake Prediction
This analysis evaluates the performance of LR and
RF models across three HINTS datasets—
HINTS123, HINTS4, and HINTS5—by examining
metrics such as accuracy, precision, recall, F1 score,
and AUC. Each dataset represents unique
characteristics that challenge the models differently,
providing insight into the models' suitability for
various data complexities.
Table 3: Comparison of LR and RF Models on HINTS
Datasets.
Group Model Pr Re F1 AUC
Group 1
HINTS123
LR 99.55 99.1 99.32 99.41
RF 97.55 95.93 96.74 97.23
Group 2
HINTS4
LR 81.2 83.14 82.16 81.84
RF 80.26 85.41 82.75 82.08
Group 3
HINTS5
LR 86.45 82.27 84.31 80.54
RF 83.75 90.92 87.18 80.95
In Group 1, using the HINTS123 dataset, LR
performed exceptionally well across all metrics,
outstripping RF. LR achieved an accuracy of 99.49, a
precision of 99.55, and a recall of 99.1, indicating that
it could classify instances with remarkable accuracy
and minimal error. Its F1 score of 99.32 and AUC of
99.41 further underscore its capability in
distinguishing between classes effectively. In
contrast, while RF also showed strong performance,
its lower recall (95.93) and AUC (97.23) metrics
indicate that it was slightly less effective than LR in
managing this dataset’s characteristics.
In Group 2, with the HINTS4 dataset, RF had a
slight advantage over LR, particularly in metrics such
as recall and AUC. While both models performed
comparably in accuracy—RF at 82.1 and LR at
81.85—RF excelled in recall, achieving 85.41
compared to LR’s 83.14. This advantage in recall
suggests that RF was more sensitive in identifying
positive instances within this dataset, a key benefit for
applications prioritizing true positive detection. RF’s
F1 score (82.75) and AUC (82.08) also outpaced
HEALTHINF 2025 - 18th International Conference on Health Informatics
236

Logistic Regression, highlighting its suitability for
more complex data structures like those found in
HINTS4.
In Group 3, which used the HINTS5 dataset, RF
continued to outperform LR, particularly in recall and
F1 score, demonstrating its strength in identifying
positive cases in this dataset. RF achieved an
accuracy of 83.28 and a recall of 90.92, compared to
Logistic Regression’s accuracy of 80.96 and recall of
82.27. Additionally, the F1 score for RF was
significantly higher at 87.18 compared to Logistic
Regression’s 84.31, indicating that RF maintained a
better balance between precision and recall. This
improved performance highlights RF’s ability to
capture nuanced, non-linear patterns in the HINTS5
dataset, making it a more suitable model for datasets
with complex relationships.
In summary, LR showed exceptional performance
in Group 1, making it ideal for datasets with
straightforward, linear relationships like HINTS123.
In contrast, RF proved advantageous in Groups 2 and
3, excelling in datasets with greater complexity, as
seen in HINTS4 and HINTS5. These findings suggest
that LR is highly effective for simpler datasets, while
RF is better suited for complex datasets requiring
high sensitivity and the ability to handle intricate,
non-linear patterns. This comparison serves as a
guide for model selection based on dataset
characteristics and the importance of specific metrics
such as recall or precision in future applications.
5 DISCUSSIONS
This study explored the impact of digital health
literacy and socioeconomic factors on CRC screening
behaviors across different time periods using data
from the HINTS datasets. By applying machine
learning models, we identified critical determinants
influencing CRC screening adherence and uncovered
variations in the influence of socioeconomic and
digital health literacy factors over time.
Our analysis confirms several important trends in
CRC screening behavior, as observed in prior studies,
while also highlighting new insights specific to digital
health engagement. Age, socioeconomic stability,
and digital literacy emerged as consistent predictors
of CRC screening uptake across the HINTS cycles.
This indicates that while digital health interventions,
such as patient portals and telehealth, have gained
prominence, traditional demographic factors continue
to play a substantial role in CRC screening adherence.
The finding aligns with studies like Atarere et al.
(2024a, 2024b, 2024c), which emphasize that while
digital health tools may enhance adherence,
addressing fundamental socioeconomic and
demographic barriers is essential for achieving equity
in CRC screening rates.
The SHAP analysis demonstrated that prior CRC
screening behaviors, age, and patient-provider
interactions were among the strongest predictors of
screening adherence, especially in the earlier HINTS
groups. This reinforces the idea that positive prior
experiences with CRC screening and effective
communication with healthcare providers are crucial
in fostering long-term adherence to screening
recommendations (Wu, et al.2023). Specifically, our
results underscore the role of healthcare providers in
reinforcing CRC screening messages, particularly for
at-risk populations who may be less engaged with
digital health tools.
Chronic conditions, including hypertension and
diabetes, also play a role in shaping CRC screening
behaviors across the HINTS groups. These conditions,
often requiring routine medical attention, may increase
patients’ engagement with healthcare providers,
creating additional opportunities for providers to
recommend CRC screening as part of comprehensive
preventive care. The consistent significance of
variables such as "MedConditions_HighBP" and
"MedConditions_Diabetes" across multiple groups
indicates that individuals managing chronic illnesses
may be more attuned to preventive health measures.
Additionally, health coverage factors, particularly
Medicare (represented by "HCCoverage_Medicare"),
are associated with higher screening rates among those
with chronic conditions, likely reflecting the expanded
access to preventive services Medicare offers to older
adults with chronic health needs.
Collectively, these insights suggest that
psychological readiness, chronic condition
management, and continuous healthcare engagement
are influential in CRC screening decisions.
Addressing psychological barriers, reinforcing
supportive patient-provider communication, and
leveraging routine chronic care visits for screening
recommendations could help enhance screening
adherence, especially among high-risk or less-
engaged populations.
The influence of digital health literacy on CRC
screening behaviors appeared most prominent in the
later HINTS cycles, particularly HINTS 5 (2018-
2020). This suggests that as digital health
technologies become more integrated into routine
healthcare, the ability to navigate these tools may
increasingly shape preventive health behaviors. For
instance, confidence in locating reliable health
information online and regular telehealth usage were
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data
237

associated with higher screening adherence,
indicating that digital health literacy is becoming an
important factor in promoting preventive behaviors
like CRC screening. These findings suggest a need for
targeted interventions to enhance digital literacy
among populations with historically low screening
rates, such as rural communities and lower-income
groups.
Our comparison of LR and RF models across
different HINTS datasets highlighted that model
performance varies with data complexity. LR
outperformed RF on the HINTS123 dataset (2003-
2008), likely due to the dataset's simpler, more linear
structure, while RF excelled in HINTS4 and HINTS5
datasets, which introduced more complex, non-linear
relationships as HIT variables became more
prevalent. This performance variation indicates that
non-linear models like RF may be more effective for
analyzing recent datasets where digital health literacy
factors play a larger role. Future studies aiming to
incorporate digital health engagement factors should
consider leveraging non-linear models to capture the
nuanced behaviors associated with these variables.
This study has several limitations. First,
HINTS data are based on self-reported responses,
which may introduce reporting bias. Additionally, the
focus on the U.S. population limits the
generalizability of our findings to other regions where
digital health adoption and socioeconomic structures
differ significantly. The machine learning models,
while effective in identifying predictive factors, may
not fully capture the dynamic and complex
interactions that influence health behaviors over time.
Further studies could benefit from incorporating
longitudinal data or using more advanced modelling
techniques, such as neural networks, to capture
temporal patterns in digital health engagement.
Future research should explore integrating EHRs
with survey data to enhance the predictive accuracy
of CRC screening models. Additionally, examining
the role of social determinants of health, such as
social support and community engagement, could
provide a more holistic view of factors influencing
CRC screening adherence.
6 CONCLUSIONS
CRC screening rates in the United States have shown
improvements over time, yet significant disparities
persist, particularly among underserved populations
such as younger individuals, non-White racial groups,
and those with lower socioeconomic status or limited
digital health literacy. Leveraging machine learning
models and SHAP analysis on HINTS data across
three temporal groups revealed evolving predictors of
CRC screening adherence. Key findings emphasize
the persistent influence of traditional
sociodemographic factors like age, income, and
education, alongside the growing importance of
digital health literacy and access to health
technologies. Targeted interventions focusing on
enhancing digital health engagement, improving
access to preventive care, and addressing
socioeconomic barriers are critical to bridging these
disparities. These findings highlight the importance
of integrating digital tools with equitable public
health strategies to improve CRC screening uptake
and reduce health inequities across diverse
populations.
ACKNOWLEDGEMENTS
Funding: This publication was supported by the
University of Kentucky College of Medicine
Artificial Intelligence in Medicine Research Alliance
and the Center for Clinical and Translational Science,
which is funded by the National Center for Research
Resources and the National Center for Advancing
Translational Sciences, National Institutes of Health,
through Grant UL1TR001998. The content is solely
the responsibility of the authors and does not
necessarily represent the official views of the NIH.
REFERENCES
Atarere, J., Chido-Amajuoyi, O., Mensah, B., Onyeaka, H.,
Adewunmi, C., Umoren, M., & Kanth, P. (2024a).
Primary care telehealth visits and its association with
provider discussion on colorectal cancer screening in
the United States. Telemedicine and e-Health, 30(5),
1325-1329.
Atarere, J., Haas, C., Akhiwu, T., Delungahawatta, T.,
Pokharel, A., Adewunmi, C., & Barrow, J. (2024b).
Prevalence and predictors of colorectal cancer
screening in the United States: Evidence from the
HINTS database 2018 to 2020. Cancer Causes &
Control, 35(2), 335-345.
Atarere, J., Haas, C., Onyeaka, H., Adewunmi, C.,
Delungahawatta, T., Orhurhu, V., & Barrow, J.
(2024c). The role of health information technology on
colorectal cancer screening participation among
smokers in the United States. Telemedicine and e-
Health, 30(2), 448-456.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre,
L. A., & Jemal, A. (2018). Global cancer statistics
2018: GLOBOCAN estimates of incidence and
mortality worldwide for 36 cancers in 185 countries.
HEALTHINF 2025 - 18th International Conference on Health Informatics
238

CA: A Cancer Journal for Clinicians, 68(6), 394–424.
De La Garza, Á. G., Blanco, C., Olfson, M., & Wall, M. M.
(2021). Identification of suicide attempt risk factors in
a national US survey using machine learning. JAMA
Psychiatry, 78(4), 398-406.
Finney Rutten, L. J., Hesse, B. W., Moser, R. P., McCaul,
K., & Rothman, A. J. (2009). Public understanding of
cancer prevention, detection, and survival/cure:
Comparison with state-of-science evidence for colon,
skin, and lung cancer. Journal of Cancer Education,
24(1), 40-48.
Ford, J. S., Coups, E. J., & Hay, J. L. (2006). Knowledge of
colon cancer screening in a national probability sample
in the United States. Journal of Health Communication,
11(Suppl 1), 19-35.
Geiger, T. M., Miedema, B. W., Geana, M. V., Thaler, K.,
Rangnekar, N. J., & Cameron, G. T. (2008). Improving
rates for screening colonoscopy: Analysis of the health
information national trends survey (HINTS I) data.
Surgical Endoscopy, 22(2), 527-533.
Hay, J., Coups, E., & Ford, J. (2006). Predictors of
perceived risk for colon cancer in a national probability
sample in the United States. Journal of Health
Communication, 11(Suppl 1), 71-92.
Idowu, K. A., Adenuga, B., Otubu, O., Narasimhan, K.,
Kamara, F., Hunter-Richardson, F., Larbi, D., Sherif, Z.
A., & Laiyemo, A. O. (2016). Place of birth, cancer
beliefs, and being current with colon cancer screening
among US adults. Annals of Gastroenterology, 29(3),
336-340.
Jun, J., & Oh, K. (2013). Asian and Hispanic Americans’
cancer fatalism and colon cancer screening. American
Journal of Health Behavior, 37(2), 145-154.
Keum, N., & Giovannucci, E. (2019). Global burden of
colorectal cancer: emerging trends, risk factors and
prevention strategies. Nature reviews Gastroenterology
& Hepatology, 16(12), 713-732.
McIntosh, J. G., Jenkins, M., Wood, A., Chondros, P.,
Campbell, T., Wenkart, E., ... & Emery, J. D. (2024).
Increasing bowel cancer screening using SMS in
general practice: the SMARTscreen cluster randomised
trial. British Journal of General Practice, 74(741),
e275-e282.
Miller Jr, D. P., Denizard-Thompson, N., Weaver, K. E.,
Case, L. D., Troyer, J. L., Spangler, J. G., ... & Pignone,
M. P. (2018). Effect of a digital health intervention on
receipt of colorectal cancer screening in vulnerable
patients: a randomized controlled trial. Annals of
Internal Medicine, 168(8), 550-557.
Mirzaei, A., Aslani, P., & Schneider, C. R. (2022).
Healthcare data integration using machine learning: A
case study evaluation with health information-seeking
behavior databases. Research in Social and
Administrative Pharmacy, 18(12), 4144-4149.
Nawaz, H., Via, C., Shahrokni, A., Ramdass, P., Raoof, A.,
Sunkara, S., & Petraro, P. (2014). Can the inpatient
hospital setting be a golden opportunity to improve
colon cancer screening rates in the United States?
Health Promotion Practice, 15(4), 506-511.
Siegel, R. L., Miller, K. D., Fuchs, H. E., & Jemal, A.
(2022). Cancer statistics, 2022. CA: A Cancer Journal
for Clinicians, 72(1), 7–33.
Sun, C., Mobley, E., Quillen, M., Parker, M., Daly, M.,
Wang, R., & Xu, J. (2024). Predicting early-onset
colorectal cancer in individuals below screening age
using machine learning and real-world data. medRxiv,
2024-07.
Wu, S., Zhang, X., Chen, P., Lai, H., Wu, Y., Shia, B. C.,
& Qin, L. (2022). Identifying the predictors of patient-
centered communication by machine learning methods.
Processes, 10(12), 2484.
Zhen, J., Li, J., Liao, F., Zhang, J., Liu, C., Xie, H., & Dong,
W. (2024). Development and validation of machine
learning models for young-onset colorectal cancer risk
stratification. NPJ Precision Oncology, 8(1), 239.
The Role of Digital Health Literacy and Socioeconomic Factors in Colorectal Cancer Screening: Machine Learning Analysis of HINTS Data
239
