
Affective Computing in Anxiety Disorders:
A Rapid Literature Review of Emotion Recognition Applications
Luigi A. Moretti
1 a
, Miles Thompson
2 b
, Paul Matthews
3 c
, Michael Loizou
4 d
and David Western
1 e
1
UWE Bristol (University of the West of England), School of Engineering, England, U.K.
2
UWE Bristol (University of the West of England), School of Social Sciences, England, U.K.
3
UWE Bristol (University of the West of England), School of Computing and Creative Technologies, England, U.K.
4
University of Plymouth, Faculty of Health, England, U.K.
Keywords: Anxiety Disorders, Affective Computing, Emotion Recognition, Emotion Detection, Social Phobia,
Panic Disorder, Post-Traumatic Stress Disorder (PTSD), Obsessive-Compulsive Disorder (OCD),
Generalised Anxiety Disorder (GAD).
Abstract: Anxiety disorders (ADs) affect roughly one in ten people in the UK, and this number is expected to increase,
intensifying the need for innovation. Digital technologies such as affective computing (AC, technology to
detect human emotions) could foster a more patient-centric approach, enhancing therapy adherence and
optimizing clinician-patient interactions. This paper reviews the literature relevant to the integration of
affective computing in clinical pathways for ADs. A search was conducted on Google Scholar and PubMed
using the keywords “affective computing” and subtypes of anxiety disorders. A total of 355 results were
filtered to focus on peer-reviewed articles that specifically addressed emotion recognition in pathological
anxiety as opposed to simply feeling anxious. Findings underscore prevalent studies focusing on post-
traumatic stress disorder (PTSD) and the widespread use of valence and arousal for emotion quantification.
Various approaches for both eliciting and detecting emotions are explored, offering technical and practical
insights. Diverse applications, from monitoring treatment progression in behavioral therapies to assessing the
efficiency of deep brain stimulation for intractable obsessive-compulsive disorder, highlight affective
computing's versatility and promise. A significant advantage of digital technologies is their potential to
capture longitudinal and contextualized data beyond clinical confines. Such assessments elucidate patients'
daily challenges and triggers, enabling tailored interventions. The literature suggests that AC has the potential
to support mental healthcare and improve patient outcomes. However, further evidence of its effective benefits
is required, especially for ADs beyond PTSD, and further exploration of its implementation in clinical
pathways is needed.
1 INTRODUCTION
In recent years, there has been a concerted effort to
use digital technologies to support mental health and
well-being (De Witte et al., 2021) and several self-
help solutions are available on the market. However,
the integration of these technologies with clinical
pathways, a more complex yet potentially impactful
a
https://orcid.org/0009-0002-6180-0565
b
https://orcid.org/0000-0002-1358-1962
c
https://orcid.org/0000-0003-1021-2683
d
https://orcid.org/0000-0002-9575-7182
e
https://orcid.org/0000-0002-4303-7423
application, has received relatively little attention.
1.1 Anxiety Disorders, a Clinical
Context
According to a 2007 survey in the UK, the prevalence
of any lifetime mental disorder was 45.5% (Slade et
al., 2009). Additionally, a 2014 survey indicated that
Moretti, L. A., Thompson, M., Matthews, P., Loizou, M. and Western, D.
Affective Computing in Anxiety Disorders: A Rapid Literature Review of Emotion Recognition Applications.
DOI: 10.5220/0013322800003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 273-284
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
273

approximately one in ten people in the UK are
affected by ADs (Adult Psychiatric Morbidity Survey,
2014). This situation has been worsened by the
Covid-19 pandemic, in which the necessary
restrictions and social rules introduced (e.g.
lockdowns, quarantines, social distance, etc) have
triggered disorders otherwise somehow controlled,
and sharpened the ones already manifest (Ugbolue et
al., 2020; Shevlin et al., 2020).
In psychiatry there is a continuous debate about
the taxonomy of mental disorders. For a matter of
simplicity, in this text we refer to ‘Anxiety Disorders’
(ADs) based on the definition provided by the U.S.
National Institutes of Mental Health, which includes
five major types (U.S. Department of Health &
Human Services, 2024): Generalized Anxiety
Disorder (GAD), Obsessive-Compulsive Disorder
(OCD), Panic Disorder (PD), Post-Traumatic Stress
Disorder (PTSD), Social Phobia (or Social Anxiety
Disorder, SAD).
Anxiety disorders (ADs) remain significantly
under- and misdiagnosed, partly due to challenges in
distinguishing between subtypes and the prevalence
of co-occurring somatic complaints and
comorbidities. These challenges are particularly
widespread; for instance, comorbidities affect
approximately 90% of patients with obsessive-
compulsive disorder (OCD) (Stein et al., 2019;
Yehuda et al., 2015). Current diagnostic methods face
notable limitations. Standard self-reported
approaches rely paradoxically on patients' ability to
assess their own emotional awareness, a capability
often impaired in ADs (Berking et al., 2011; Berking
& Wupperman, 2012). Structured clinical interviews,
while widely used, frequently lack flexibility,
specificity, and cross-cultural validity. Additionally,
these interviews can fail to detect concealed or
simulated symptoms. For example, only 11% of
PTSD patients are correctly identified through
structured interviews (Yehuda et al., 2015). Beyond
these diagnostic challenges, there is a lack of
objective tools capable of differentiating between
stages of ADs and quantifying their impact on
patients’ quality of life (Stein et al., 2019; Yehuda et
al., 2015). An objective tool is also desirable to
provide data to assess the efficacy of
pharmaceuticals, psychological and alternative
treatments (Bystritsky et al., 2013; Stein et al., 2019;
Yehuda et al., 2015).
Moreover, the healthcare system is under pressure
worldwide due to a shortage of workforce compared
to the increasing demand (Michelutti & Relić, 2022).
This scenario leads to high level of stress and burnout
among the clinicians and to a reduction of time per-
patient. Therefore, more research is needed to
investigate the use of digital technologies to support
patients’ self-management and involvement, as well
as to enable more efficient patient-clinician
interactions.
1.2 Affective Computing in Mental
Health
Emotions are central to the human experience, and
play a crucial role in our lives: they influence our
learning, attention, decision making and perception
(Picard, 1997). From a neurobiological perspective,
emotions are bioregulatory reactions regulated by
chemical and neural responses regarding
‘emotionally competent stimuli’ (i.e. objects,
situations, or memories).
There are mainly two families of classifications
for emotions (Yazdani et al., 2013): 1. Discrete
Emotional Model (DEM) which is a categorical
model based on standard terms used as references,
and the selection of emotions used varies between
studies. Furthermore, there could be cultural biases in
the interpretation of the meaning of each emotion
used. Some of the most common labels used are:
‘anger’, ‘sadness’, ‘joy’, ‘disgust’, ‘surprise’, ‘fear’
(Ekman et al., 1972). 2. Affective Dimensional Model
(ADM) or Continuous Dimensional Model which,
instead, is a system of coordinates for emotions,
which is based on Valence and Arousal for the 2D
models, plus Dominance (Mehrabian, 1997) for the
3D ones (VAD model). The Valence dimension
expresses the degree of pleasantness, while Arousal
captures intensity, ranging from calm to energized;
Dominance is used to represent the level of control
and freedom to act, ranging from submissive to
empowered (Mehrabian & Russell, 1974). Moreover,
some authors (Verma & Tiwary, 2017) proposed a 3D
matrix in which VAD emotion values essentially
serve as coordinates for DEM labels clustered in 5
main groups, bridging the two emotion classification
approaches.
Some researchers emphasise the key role that
affective assessment plays in psychotherapy: both to
assist patients in their therapeutic journey and to
provide the clinician with a framework for
intervention (Greenberg & Safran, 1990). There are
also studies supporting the role of arousal in
facilitating anxiety reduction in fear-avoidance
problems (Greenberg & Safran, 1989), such as PTSD
(Hyer et al., 1991).
Affective Computing (AC) is a multidisciplinary
field which studies emotions through technology
(Calvo et al., 2015). Many studies have explored how
HEALTHINF 2025 - 18th International Conference on Health Informatics
274
AC can detect common anxiety, which is the normal
and expected response to everyday challenges or
stress. However, fewer studies have focused on
pathological anxiety, an anxiety that is too intense,
lasts too long, or occurs in ways that disrupt daily life.
This work aims to explore how AC techniques have
been developed and evaluated specifically for ADs.
2 METHODOLOGY
A previous overview of affective computing solutions
in healthcare found that 28.3% of the publications
prior to 2020 were related to mental health, excluding
studies that referred to the use of wearables other than
eye tracking, which differentiates it from the present
work (Apablaza & Cano, 2020). In a 2014 review, 34
studies on digital solutions for anxiety disorders were
examined, emphasizing the Ecological Momentary
Assessment (EMA) approach's ability to provide
insights into the temporal variability of symptoms and
associations among daily affect, behaviors, and
situational cues thanks to the collection of
longitudinal data. The study also noted successful
combinations of EMA with ambulatory assessment of
physiological variables and treatment evaluations
(Walz et al., 2014). Other literature reviews focused
on specific data modalities and/or techniques in come
ADs sub-disorders (e.g. machine learning (ML) for
speech analysis in PTSD (Anitha, 2022; Suneetha &
Anitha, 2024), or fMRI in SAD (Hattingh et al.,
2013)).
The research question that this paper aims to
address can be summarised as follows: How
effectively has affective computing proven to be for
supporting clinical pathways in anxiety disorders, and
what are the technological and pragmatic challenges
that shape its implementation? Under this main
question, sub-questions can help in addressing this
aim comprehensively:
a. Technical Feasibility: What types of affective
computing technologies have shown potential in
detecting and assessing anxiety disorders symptoms?
What evidence exists regarding their accuracy,
robustness, and usability?
b. Clinical Feasibility and Integration: To what
extent have these technologies been incorporated into
clinical pathways, and what specific use cases have
shown promise?
c. Sociological and Ethical Considerations: What
cultural considerations could influence the
widespread integration of AC in ADs?
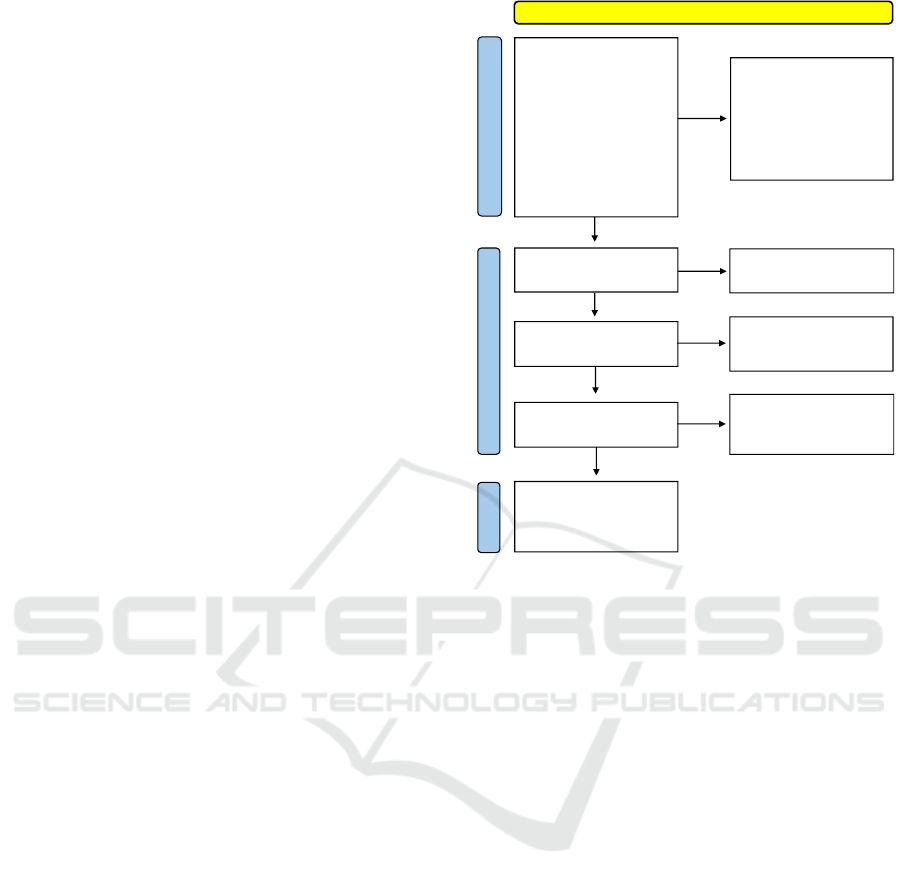
Figure 1: PRISMA 2020 flow diagram adapted for this
rapid literature review.
2.1 Search Strategy and Data Sources
This literature review sets various challenges given the
use of similar terminology from different fields within
different meanings. An example of this semantic
overlap relates to the keywords "emotion detection" or
"emotion recognition": while in psychology this refers
to the capability of individuals of understanding others’
emotions, in technology this refers to AC solutions
capable of finding emotional patterns in certain data
modalities. In order to overcome these challenges, a
bivalent research approach has been proposed and
implemented. This approach comprises two distinct
methods. The first is conducted through the databases'
native interfaces, while the second exploits certain
features of the free software "Publish or Perish 8"
(https://harzing.com/). The latter method utilises the
software's “search in the references” feature. The two
approaches were carried out using two distinct
databases to provide comprehensive coverage across
all academic disciplines: Google Scholar and PubMed.
An overview of the methodology and a quantification
of the results are presented in Fig. 1.
The prompt used within the native interfaces of
the aforementioned databases was adapted to their
respective features and constraints.
Affective Computing in Anxiety Disorders: A Rapid Literature Review of Emotion Recognition Applications
275

- in PubMed: (("affective computing" OR "emotion
recognition" OR "emotion detection"[Title/Abstract])
AND (*disorder*[Title/Abstract]))
- in Google Scholar: for title only: allintitle: "affective
computing" OR "emotion recognition" OR "emotion
detection" "*disorder*”. Where *disorder* was
substituted with the followings in different entries:
obsessive compulsive disorder, OCD, post-traumatic
disorder, PTSD, panic disorder, panic attack, social
anxiety, social phobia, generalised anxiety disorder,
GAD.
The parallel search strategy based on Publish or
Perish focused on the term "affective computing"
within the text, including references, to ensure a
thorough exploration of relevant literature. The
search strategy involved filtering articles with titles
containing specific keywords related to anxiety
disorders (i.e. the aforementioned in *disorder*).
2.2 Screening and Selection
Of the 355 reports initially found combining the two
research approaches, 152 have been discarded as
duplicates. For the subsequent selection process,
exclusion criteria were established to ensure the
relevance and quality of the chosen papers.
Excluded papers included non-peer-reviewed
sources such as books, theses, and magazine articles
(n=8), as well as works in languages other than
English (n=2). Additionally, meta-analysis or
review papers (n=7), as well as papers focused on
non-pathological anxiety or on aspects other than
emotion recognition and detection through
technology (e.g. virtual reality implementation)
were omitted (n=31).
2.3 Results Overview
38 papers met the inclusion criteria. Of these two are
purely theoretical without involving
experimentation (Hinduja et al., 2024; Howard et
al., 2014), one was a pivot study (Cohn et al., 2018)
of another (Provenza et al., 2021), and another one
(Kathan et al., 2024) an integration study of a
previous one (Kathan et al., 2023). In Fig. 2 has been
reported the distribution of papers over the years and
which sub-type of anxiety disorders they focus on.
The most evident insights from this stacked column
chart is that PTSD is the most studied sub-disorder
and that there is a consistent increasing research
effort in this field in the last seven years (data
updated to October 2024).
3 FINDINGS AND DISCUSSION
In this section the results of the literature review will
be contextualised within the three research questions
introduced in the methodology.
Figure 2: Annual distribution (up to October 2024*) and
classification by anxiety sub-disorders of the publications
included in this review.
3.1 Technical Feasibility of AC for ADs
By comparing the studies found in this review it is
important to consider the diversity among anxiety
sub-disorders, data modalities implemented, and
dataset used. These aspects are summarised in Tab. 1,
with a particular attention for the data used as this is
useful not only to evaluate the reliability of the
studies, but also to consider the mentioned datasets
for future research. Some of the studies, for instance,
utilized previous works or distinct datasets as
benchmarks (Attas et al., 2022) to assess the
generalization capabilities of ML algorithms
(Chappidi Suneetha, 2024), or to develop multimodal
approaches, which appear to outperform their
unimodal counterparts (Kalanadhabhatta et al., 2023).
Moreover, ML models (transformers above all)
require a huge quantity of data to be trained, leading
to the need of merging different datasets or taking
advantage of alternative methods, such as transfer
learning (Dia et al., 2024). However, not all the works
reviewed relied on ML, in fact a third of the studies
opted for pure statistical solutions, which, whenever
applicable, offer more straightforward and
explainable results.
The results declared by several studies, included
in Tab. 1, are promising for future in-wild or clinical
explorations. However, it is mandatory to also refer
to the dimension of the datasets used for testing them
as well as the nature of the data, given that real-case
scenario data are often noisier and more difficult to
manage. From a pragmatic perspective it’s also
important to consider the kind of implementation for
HEALTHINF 2025 - 18th International Conference on Health Informatics
276

which each technology is suggested for, as different
requirements and characteristics might be prioritised.
Of the reviewed studies 43.3% referred to DEM,
56.7% to ADM emotion classifications. However, in
both cases there is not an absolute consistency in the
number or types of labels used. For example two
studies only included dominance in their ADM
emotion evaluations (Kathan et al., 2023; Serrano et
al., 2019), and one study referred to positive and
negative emotions (Zhu et al., 2024). This
heterogeneity is a further challenge for the comparison
of different ML approaches and for the implementation
of different datasets in the same work.
When studying emotions and emotional responses,
the first step faced is the need of triggering the target
emotions. Emotional elicitation methods varied, with
most studies employing clinical situations (e.g.
interviews, therapy, cognitive tasks), while some
altered environmental conditions (e.g. reproducing
natural sounds (Ge et al., 2023; Sundaravadivel et al.,
2020) or using virtual reality (VR) (Moussaoui et al.,
2007)) or utilized Ecological Momentary Assessments
(EMAs) in period of time ranging from 3 (Boukhechba
et al., 2018) to 8 weeks (Olesen et al., 2023). The next
step consists of the proper emotion detection. Emotion
labelling has been performed following three main
approaches: a) using standardized self-reported survey
to define emotion labels (e.g. Kruskal-Wallis test (Ge
et al., 2023), or "Positive and Negative Affect
Schedule" (Watson et al., 1988), combined with
"Somatic Arousal – Fear questionnaire" (NIH, 2024)
and "10-item Perceived Stress Scale" (Cohen et al.,
1983)); b) relaying on previously validated datasets
(e.g. RECOLA or RAVDESS); c) expert annotations
of subjects’ responses to stimuli (e.g. clinical
interviews); d) using already validated emotional-
related proxies ML models and/filters (e.g. General
Purpose Emotion Lexicon (GPEL) for text analysis
(Bandhakavi et al., 2017), GeMAPS from openSMILE
toolkit for speech analysis (Eyben et al., 2016)). Both
for emotion eliciting and labelling, using standardized
approaches not only reduces the workload required for
designing a new experiment, but also brings benefits in
terms of reproducibility and evaluation.
3.2 Clinical Integration and
Applications in Anxiety Pathways
Ten studies proposed innovations suitable for clinical
pathways (Cohn et al., 2018; Attas, 2022; Ding et al.,
2021; Flechsenhar et al., 2024; Hinduja et al., 2024;
Moussaoui et al., 2007; Olesen et al., 2023; Popovic
et al., 2006; Provenza et al., 2021; Wörtwein &
Scherer, 2017), while most of the works were more
oriented towards pure scientific exploration, such as
analysing alexithymia (i.e. the impairment of
recognition and description of one's own emotional
states) in ADs, or optimizing technological solutions
such as ML models in AC for ADs, or improving our
understanding of how people affected by ADs
experience emotions and which are the characteristic
differences that can help in detecting and monitoring
them. (Bakker et al., 2014) underlined the importance
of incorporating the dimension of Dominance to
achieve a more comprehensive understanding of the
emotional spectrum. Integrating Dominance poses a
challenge due to the scarcity of datasets that label this
dimension. Therefore, the development of more
datasets including the three scales would be greatly
valued for the research community (Verma & Tiwary,
2017). It is also been discussed that alterations in the
dominance motivation, dominant and subordinate
behaviour, and responsivity to perceptions of power
and subordination are linked to a broad range of
psychopathologies (Johnson et al., 2012).
Despite the consistent number of papers, there is
a lack of prior work on detecting PTSD in daily
activities, especially in non-military populations
(Kalanadhabhatta et al., 2023). It is reasonable to
assume that military organizations offer financial
support for PTSD research given its correlation with
combat experiences and provide easy environments
for participant recruitment, mitigating two major
research challenges. Hyperarousal is considered
symptomatic in PTSD during re-experiencing
traumatic memories (Fontana, 2022), and an altered
disgust perception is considered a relevant feature in
OCD (Serrano et al., 2019), hence they have been
explored for detection and monitoring using affective
computing solutions.
Moreover, not all the sub-disorders are equally
represented: PTSD accounted for 21 out of the 38
selected papers (55.26%), while other sub-types such
as OCD (n=6), SAD (n=5), generic ADs (n=4), and
GAD (n=2) were underrepresented. This underlines a
notable gap in the literature that might be filled by
transposing to different sub-disorders approaches
included in this review. 18 studies were based on data
collected ex-novo, instead of pre-built dataset (n=11).
This presented the researchers with the need to assess
the presence and eventually the gravity of the ADs in
their participants. The Hamilton Anxiety Rating Scale
(HAM-A) was used for evaluating broad ADs (Ge et
al., 2023), while specific tests were applied for the
sub-types, including versions for adult or paediatric
populations (on which 4 studies only where focused
(Heyn et al., 2022; Kleberg et al., 2021; Olesen et al.,
2023; Zeghari et al., 2023)), but also to verify the
Affective Computing in Anxiety Disorders: A Rapid Literature Review of Emotion Recognition Applications
277
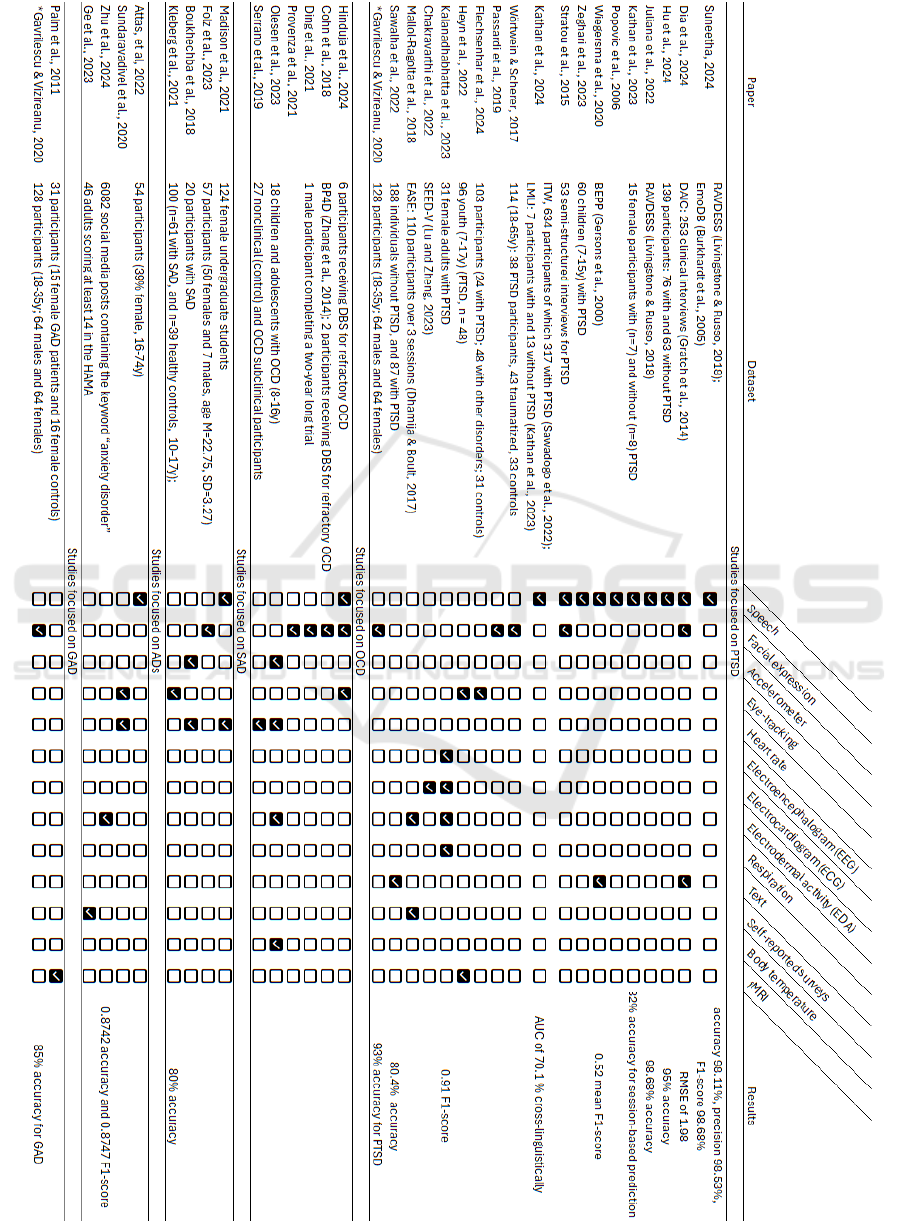
Table 1: Data modalities used for emotion detection (the study marked with an * focuses on both PTSD and GAD).
HEALTHINF 2025 - 18th International Conference on Health Informatics
278

presence of comorbidities (e.g. depression). Some
studies encountered challenges in recruiting male
participants, resulting in either female-only studies
(Kalanadhabhatta et al., 2023; Kathan et al., 2023) or
deliberate focus on females only (Madison et al.,
2021; Serrano et al., 2019).
3.3 Practical and Pragmatic Challenges
Gender and culture significantly influence our
perception and emotional responses, affecting how
mental health disorders are experienced and
manifested (Maner et al., 2008; Stratou et al., 2015).
In according to this assumption, gender-dependent
models outperformed gender-agnostic approaches in
PTSD, underscoring the importance of considering
gender in AC machine learning models for ADs
(Cohn et al., 2018). Some models trained on a
language (e.g. Zhu et al., 2024) might not generalize
that well when applied on other ones, as demonstrated
by (Kathan et al., 2024).
As we navigate the realm of emotions, one of the
most intimate aspects of human nature, it is
imperative to prioritize the privacy and security of the
frameworks proposed. However, apart from one
exception (i.e. Dia et al., 2024), none of the selected
papers gives substantial attention to the ethical
implications of detecting emotions from individuals
or the potential ramifications in future clinical
integrations. However, it is crucial to consider the
ethical dimensions surrounding emotion recognition
technologies, particularly in mental health contexts.
Cameras and microphones, commonly used for
emotion recognition, as confirmed by this review, are
perceived as non-invasive sensors. Yet, their ease of
data collection raises significant privacy concerns,
potentially infringing on individuals' privacy rights
without their consent or awareness. In contrast,
physiological approaches offer users greater control
over data acquisition and minimize the risk of
manipulation compared to facial expression analysis.
However, the deeper privacy implications of
understanding individuals' emotions highlight the
need for a cautious and ethical approach to prevent
misuse and protect individual freedoms (Bunn, 2012).
The sensitive nature of emotion understanding
underscores the importance of ethical considerations
to prevent potential misuse and safeguard privacy
rights. The EU AI Act, the first of its kind,
recognizing ethical emotion detection as a critical
task for AI, emphasizes the need for responsible
practices in this area (European Parliament, 2023).
Additionally, recognizing gender and cultural
differences in emotional expression and experience
(Butler et al., 2007), it is imperative to collect diverse
datasets to train and test AI models before
deployment, ensuring inclusivity and avoiding biases.
Moreover, studies involving individuals with
mental health conditions raise concerns about the
potential triggering of anxiety-related crises during
emotion elicitation tasks. While ethical approval is
obtained from institutional review boards, and
methodologies are often justified by their
resemblance to clinical practices such as exposure
therapy, further caution and attention to this matter
are warranted. Consulting with patients and
clinicians, ideally through a co-production approach,
would not only aid in developing more relevant
solutions but also ensure the design of more
comfortable experimental settings.
4 CHALLENGES AND FUTURE
DIRECTIONS
ML, and the Transformer architecture over all, has
demonstrated promising results in emotion detection
(Dia et al., 2024; Wagner et al., 2023), yet it demands
a substantial quantity of data, a notable limitation in
the affective computing field (Mustaqeem & Brahem,
Haddou, 2023). One potential solution, already
explored by some authors, is to apply transfer
learning, leveraging large datasets for a specific data
modality and fine-tuning the model for emotional
recognition tasks using smaller, specific datasets (e.g.
for ECG (Dentamaro et al., 2023)). Another avenue
to expand available datasets is the utilization of
synthetic data, which can train ML models before
being tested on natural data (Ive, 2022). This
approach also offers reduction of privacy concerns
related to potentially sensitive data, and the potential
to lessen bias by including rare cases that represent
realistic possibilities but may be challenging to source
from authentic data (Gonzales et al., 2023).
Most of the considered studies focus on one sub-
type of ADs exclusively: PTSD. Although this
approach effectively narrows the scope and ensures
adequate representation of subjects within the same
subtype, it may compromise differential diagnosis.
Specifically, it risks attributing certain patterns to a
subtype simply because they differ from non-
pathological cases, such as those in a control group or
data collected at different time points from the same
subject Chappidi (Kathan et al., 2023). While specific
emotion-eliciting conditions may contextualize
collected data, structuring studies to embrace a trans-
diagnostic approach could benefit pragmatic solution
Affective Computing in Anxiety Disorders: A Rapid Literature Review of Emotion Recognition Applications
279

development for clinical implementation. In this
regard, a review work comparing ECG-based
evaluations for different ADs sub-types, is
particularly relevant (Elgendi & Menon, 2019).
More explorative research is welcomed and
needed to fill the aforementioned gaps. However, it is
hoped that, works justifying their limited number of
recruited subjects as pilot studies, will be followed up
with extended research, as exemplified by various
works (Cohn et al., 2018; Provenza et al., 2021).
Failure to do so poses the risk of accumulating
hypothetical considerations that remain distant from
concrete integration in clinical practice.
Digital solutions in mental health are affected by a
significant usage drop-off rate (Nwosu et al., 2022).
There is a risk of developing solutions for longitudinal
data collection (e.g. in EMA) that fail due to user non-
adherence. One solution to this issue would be to
involve the public early on to incorporate their
perspectives, as well as clinicians, to understand how
to integrate patient preferences into scientifically
useful applications. Co-design, also known as co-
production, offers a valuable approach to mitigate
these issues (Esmail et al., 2015), and there are already
valuable examples of this approach for developing
mental health digital solutions (Thieme et al., 2023).
5 LIMITATIONS OF THIS STUDY
This rapid literature review relies solely on two
datasets. Expanding the research to other datasets
(e.g. IEEE Xplore Digital Library, Prospero, Scopus,
etc.) may uncover papers not included in this analysis.
Moreover, a more systematic approach could be
adopted by following specific guidelines for literature
reviews, such as the Cochrane methods guidance
(Garritty et al., 2024; Klerings et al., 2023).
Another intriguing aspect worth considering is the
comparison between studies focused on an AC
approach (i.e. involving emotion recognition) versus
other feature extraction approaches. Is detecting
emotions genuinely valuable? Is it appreciated by
patients and clinicians as an understandable way to
report and interpret collected data, particularly in
longitudinal approaches?
From a technical standpoint, conducting a more
in-depth analysis and comparison regarding the pre-
processing techniques utilized in the reviewed studies
to prepare the data for emotional feature extraction
would be beneficial. This analysis could offer
valuable insights into optimizing the data preparation
process for future research endeavours in different
data modalities for affective computing.
6 CONCLUSIONS
The latest findings indicate that affective computing
(AC) holds significant potential to enhance current
clinical pathways in anxiety disorders (ADs). While
existing studies yield promising results, further
research is essential.
The main insights underlined by this review could
be summarised as follows:
- Some aspects are understudied, including gender
differences, paediatric populations, some sub-
disorders, and their differences.
- The most used data modalities are voice and facial
expressions, while multimodal approaches seem to
outperform unimodal ones.
- There is a lack of large, multimodal, and
standardised AC datasets for ADs to enable direct
comparisons between technical approaches and
account for the diversity of approaches in this field.
- Promising results have been demonstrated in
research and digital environments, but more in-the-
wild data collection and clinical validations are
needed.
By addressing these gaps through
interdisciplinary collaboration, AC can transition
from a promising research avenue to a valuable tool
in clinical practice for anxiety disorders.
REFERENCES
Adult Psychiatric Morbidity Survey: Survey of Mental
Health and Wellbeing, England, 2014. (2014). NHS
England Digital. https://digital.nhs.uk/data-and-
information/publications/statistical/adult-psychiatric-
morbidity-survey/adult-psychiatric-morbidity-survey-
survey-of-mental-health-and-wellbeing-england-2014
Anitha, C. S. (2022). A Survey Of Machine Learning
Techniques OnSpeech Based Emotion Recognition
And Post Traumatic Stress DisorderDetection.
NeuroQuantology, 20(14), 1–11. https://doi.org/10.
48047/nq.2022.20.14.NQ88010
Apablaza, J., & Cano, S. (2020). Affective Computing from
Digital Health: A literature review.
Attas, D., Kellett, S., & Blackmore, C. (2022). Automatic
Time-Continuous Prediction of Emotional Dimensions
During Guided Self Help for Anxiety Disorders. 35–39.
https://doi.org/10.6094/UNIFR/223814
Baker, C., & Kirk-Wade, E. (2024). Mental health statistics:
Prevalence, services and funding in England.
https://commonslibrary.parliament.uk/research-
briefings/sn06988/
Bakker, I., Van Der Voordt, T., Vink, P., & De Boon, J.
(2014). Pleasure, Arousal, Dominance: Mehrabian and
Russell revisited. Current Psychology, 33(3), 405–421.
https://doi.org/10.1007/s12144-014-9219-4
HEALTHINF 2025 - 18th International Conference on Health Informatics
280

Bandhakavi, A., Wiratunga, N., Padmanabhan, D., &
Massie, S. (2017). Lexicon based feature extraction for
emotion text classification. Pattern Recognition Letters,
93, 133. https://doi.org/10.1016/j.patrec.2016.12.009
Berking, M., Poppe, C., Luhmann, M., Wupperman, P.,
Jaggi, V., & Seifritz, E. (2011). Emotion-regulation
skills and psychopathology: Is the ability to modify
emotions the pathway by which other emotion-
regulation skills affect mental health? Journal of
Behavior Therapy and Experimental Psychiatry.
Berking, M., & Wupperman, P. (2012). Emotion regulation
and mental health: Recent findings, current challenges,
and future directions. Current Opinion in Psychiatry,
https://doi.org/10.1097/YCO.0b013e3283503669
Boukhechba, M., Gong, J., Kowsari, K., Ameko, M. K.,
Fua, K., Chow, P. I., Huang, Y., Teachman, B. A., &
Barnes, L. E. (2018). Physiological changes over the
course of cognitive bias modification for social anxiety.
2018 IEEE EMBS International Conference on
Biomedical & Health Informatics (BHI), 422–425.
https://doi.org/10.1109/BHI.2018.8333458
Bunn, G. C. (2012). The Truth Machine: A Social History
of the Lie Detector. JHU Press.
Butler, E. A., Lee, T. L., & Gross, J. J. (2007). Emotion
regulation and culture: Are the social consequences of
emotion suppression culture-specific? Emotion, 7(1),
30–48. https://doi.org/10.1037/1528-3542.7.1.30
Bystritsky, A., Khalsa, S. S., Cameron, M. E., & Schiffman,
J. (2013). Current Diagnosis and Treatment of Anxiety
Disorders. Pharmacy and Therapeutics, 38(1), 30–57.
Calvo, R. A., D’Mello, S., Gratch, J., Kappas, A., Calvo, R.
A., D’Mello, S., Gratch, J., & Kappas, A. (Eds.).
(2015). The Oxford Handbook of Affective Computing.
Oxford University Press.
Chappidi Suneetha, E. Al. (2024). Enhanced Speech
Emotion Recognition Using the Cognitive Emotion
Fusion Network for PTSD Detection with a Novel
Hybrid Approach. Journal of Electrical Systems, 19(4),
376–398. https://doi.org/10.52783/jes.644
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A
Global Measure of Perceived Stress. Journal of Health
and Social Behavior, 24(4), 385–396. https://doi.
org/10.2307/2136404
Cohn, J. F., Jeni, L. A., Onal Ertugrul, I., Malone, D., Okun,
M. S., Borton, D., & Goodman, W. K. (2018).
Automated Affect Detection in Deep Brain Stimulation
for Obsessive-Compulsive Disorder: A Pilot Study.
Proceedings of the 20th ACM International Conference
on Multimodal Interaction, 40–44.
https://doi.org/10.1145/3242969.3243023
De Witte, N. A. J., Joris, S., Van Assche, E., & Van Daele,
T. (2021). Technological and Digital Interventions for
Mental Health and Wellbeing: An Overview of
Systematic Reviews. Frontiers in Digital Health, 3.
https://doi.org/10.3389/fdgth.2021.754337
Dentamaro, V., Impedovo, D., Moretti, L. A., & Pirlo, G.
(2023). An Approach using transformer architecture for
emotion recognition through Electrocardiogram
Signal(s).
Dia, M., Khodabandelou, G., & Othmani, A. (2024). Paying
attention to uncertainty: A stochastic multimodal
transformer for post-traumatic stress disorder detection
using video. Computer Methods and Programs in
Biomedicine, 257, 108439. https://doi.org/10.1016/
j.cmpb.2024.108439
Ding, Y., Onal Ertugrul, I., Darzi, A., Provenza, N., Jeni, L.
A., Borton, D., Goodman, W., & Cohn, J. (2021).
Automated Detection of Optimal DBS Device Settings.
Companion Publication of the 2020 International
Conference on Multimodal Interaction, 354–356.
https://doi.org/10.1145/3395035.3425354
Ekman, P., Friesen, W. V., & Ellsworth, P. (1972). Emotion
in the human face: Guidelines for research and an
integration of findings (pp. xii, 191). Pergamon Press.
Elgendi, M., & Menon, C. (2019). Assessing Anxiety
Disorders Using Wearable Devices: Challenges and
Future Directions. Brain Sciences, 9(3), 50.
https://doi.org/10.3390/brainsci9030050
Esmail, L., Moore, E., & Rein, A. (2015). Evaluating
patient and stakeholder engagement in research:
Moving from theory to practice. Journal of
Comparative Effectiveness Research, 4(2), 133–145.
https://doi.org/10.2217/cer.14.79
European Parliament. (2023). Artificial intelligence act.
Eyben, F., Scherer, K. R., Schuller, B. W., Sundberg,
J., Andre, E., Busso, C., Devillers, L. Y., Epps, J.,
Laukka, P., Narayanan, S. S., & Truong, K. P. (2016).
The Geneva Minimalistic Acoustic Parameter Set
(GeMAPS) for Voice Research and Affective
Computing. IEEE Transactions on Affective
Computing, 7(2), 190–202. https://doi.org/10.1109/
TAFFC.2015.2457417
Flechsenhar, A., Seitz, K. I., Bertsch, K., & Herpertz, S. C.
(2024). The association between psychopathology,
childhood trauma, and emotion processing.
Psychological Trauma: Theory, Research, Practice, and
Policy, 16(Suppl 1), S190–S203. https://doi.org/10.
1037/tra0001261
Fontana, A. (2022). A Model of Post-Traumatic Stress
Disorders and Dissociative Identity Disorder from the
perspective of Social Emotions. Medical Research
Archives, 10(3). https://doi.org/10.18103/mra.v10i3.
2743
Garritty, C., Hamel, C., Trivella, M., Gartlehner, G.,
Nussbaumer-Streit, B., Devane, D., Kamel, C., Griebler,
U., & King, V. J. (2024). Updated recommendations for
the Cochrane rapid review methods guidance for rapid
reviews of effectiveness. BMJ, 384, e076335.
https://doi.org/10.1136/bmj-2023-076335
Ge, Y., Xie, H., Su, M., & Gu, T. (2023). Effects of the
acoustic characteristics of natural sounds on perceived
tranquility, emotional valence and arousal in patients
with anxiety disorders. Applied Acoustics, 213, 109664.
https://doi.org/10.1016/j.apacoust.2023.109664
Gonzales, A., Guruswamy, G., & Smith, S. R. (2023).
Synthetic data in health care: A narrative review. PLOS
Digital Health, 2(1), e0000082. https://doi.org/10.
1371/journal.pdig.0000082
Affective Computing in Anxiety Disorders: A Rapid Literature Review of Emotion Recognition Applications
281

Greenberg, L. S., & Safran, J. D. (1989). Emotion in
psychotherapy. American Psychologist, 44(1), 19–29.
https://doi.org/10.1037/0003-066X.44.1.19
Greenberg, L. S., & Safran, J. D. (1990). Chapter 3-
emotional-change process in psychotherapy. In R.
Plutchik & H. Kellerman (Eds.), Emotion,
Psychopathology, and Psychotherapy (pp. 59–85).
Academic Press. https://doi.org/10.1016/B978-0-12-
558705-1.50009-9
Hattingh, C. J., Ipser, J., Tromp, S., Syal, S., Lochner, C.,
Brooks, S. J., & Stein, D. J. (2013). Functional
magnetic resonance imaging during emotion
recognition in social anxiety disorder: An activation
likelihood meta-analysis. Frontiers in Human
Neuroscience, 6. https://doi.org/10.3389/fnhum.
2012.00347
Heyn, S. A., Schmit, C., Keding, T. J., Wolf, R., &
Herringa, R. J. (2022). Neurobehavioral correlates of
impaired emotion recognition in pediatric PTSD.
Development and Psychopathology, 34(3), 946–956.
https://doi.org/10.1017/S0954579420001704
Hinduja, S., Darzi, A., Ertugrul, I. O., Provenza, N., Gadot,
R., Storch, E., Sheth, S., Goodman, W., & Cohn, J.
(2024). Multimodal prediction of obsessive-
compulsive disorder, comorbid depression, and energy
of deep brain stimulation. https://doi.org/10.
36227/techrxiv.23256119.v2
Howard, N., Jehel, L., & Arnal, R. (2014). Towards a
differential diagnostic of PTSD using cognitive
computing methods. 2014 IEEE 13th International
Conference on Cognitive Informatics and Cognitive
Computing, 9–20. https://doi.org/10.1109/ICCI-
CC.2014.6921435
Hyer, L., Woods, M. G., & Boudewyns, P. A. (1991). PTSD
and alexithymia: Importance of emotional clarification
in treatment. Psychotherapy: Theory, Research,
Practice, Training, 28(1), 129–139. https://doi.org/10
.1037/0033-3204.28.1.129
Ive, J. (2022). Leveraging the potential of synthetic text for
AI in mental healthcare. Frontiers in Digital Health, 4,
1010202. https://doi.org/10.3389/fdgth.2022.1010202
Johnson, S. L., Leedom, L. J., & Muhtadie, L. (2012). The
Dominance Behavioral System and Psychopathology:
Evidence from Self-Report, Observational, and
Biological Studies. Psychological Bulletin, 138(4),
692–743. https://doi.org/10.1037/a0027503
Kalanadhabhatta, M., Roy, S., Grant, T., Salekin, A.,
Rahman, T., & Bergen-Cico, D. (2023). Detecting
PTSD Using Neural and Physiological Signals:
Recommendations from a Pilot Study. 2023 11th
International Conference on Affective Computing and
Intelligent Interaction (ACII), 1–8. https://doi.org/10.
1109/ACII59096.2023.10388200
Kathan, A., Bürger, M., Triantafyllopoulos, A., Milkus, S.,
Hohmann, J., Muderlak, P., Schottdorf, J., Musil, R.,
Schuller, B., & Amiriparian, S. (2024). Real-world
PTSD Recognition: A Cross-corpus and Cross-
linguistic Evaluation. Interspeech 2024, 487–491.
https://doi.org/10.21437/Interspeech.2024-493
Kathan, A., Triantafyllopoulos, A., Amiriparian, S.,
Milkus, S., Gebhard, A., Hohmann, J., Muderlak, P.,
Schottdorf, J., Schuller, B. W., & Musil, R. (2023). The
effect of clinical intervention on the speech of
individuals with PTSD: Features and recognition
performances. INTERSPEECH 2023, 4139–4143.
https://doi.org/10.21437/Interspeech.2023-1668
Kleberg, J. L., Löwenberg, E. B., Lau, J. Y. F., Serlachius,
E., & Högström, J. (2021). Restricted Visual Scanpaths
During Emotion Recognition in Childhood Social
Anxiety Disorder. Frontiers in Psychiatry, 12.
https://doi.org/10.3389/fpsyt.2021.658171
Klerings, I., Robalino, S., Booth, A., Escobar-Liquitay, C.
M., Sommer, I., Gartlehner, G., Devane, D., &
Waffenschmidt, S. (2023). Rapid reviews methods
series: Guidance on literature search. BMJ Evidence-
Based Medicine, 28(6), 412–417. https://doi.org/10.
1136/bmjebm-2022-112079
Madison, A., Vasey, M., Emery, C. F., & Kiecolt-Glaser, J.
K. (2021). Social anxiety symptoms, heart rate
variability, and vocal emotion recognition in women:
Evidence for parasympathetically-mediated positivity
bias. Anxiety, Stress, & Coping, 34(3), 243–257.
https://doi.org/10.1080/10615806.2020.1839733
Maner, J. K., Miller, S. L., Schmidt, N. B., & Eckel, L. A.
(2008). Submitting to Defeat: Social Anxiety,
Dominance Threat, and Decrements in Testosterone.
Psychological Science, 19(8), 764–768. https://doi.
org/10.1111/j.1467-9280.2008.02154.x
Mehrabian, A. (1997). Comparison of the PAD and
PANAS as models for describing emotions and for
differentiating anxiety from depression. Journal of
Psychopathology and Behavioral Assessment, 19(4),
331–357. https://doi.org/10.1007/BF02229025
Mehrabian, A., & Russell, J. A. (1974). An approach to
environmental psychology (pp. xii, 266). The MIT
Press.
Michelutti, A. D., & D. Relić. (2022). Health workforce
shortage – doing the right things or doing things right?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9086
817/Picard, R. W. (1997). Affective computing. MIT
Press.
Moussaoui, A., Pruski, A., & Brahim, C. (2007). Emotion
regulation for social phobia treatment using virtual
reality.
Mustaqeem, A. O., & B. Brahem, Y. Haddou. (2023).
Machine-Learning-Based Approaches for Post-
Traumatic Stress Disorder Diagnosis Using Video and
EEG Sensors: A Review | IEEE Journals & Magazine |
IEEE Xplore. 24135–24151. https://doi.org/10.11
09/JSEN.2023.3312172
NIH. (2024). NIH Toolbox Fear/Somatic Arousal FF
Ages 18+ v3.0 [Eeg]. HealthMeasures. https://www.
healthmeasures.net/index.php
Nwosu, A., Boardman, S., Husain, M. M., & Doraiswamy,
P. M. (2022). Digital therapeutics for mental health: Is
attrition the Achilles heel? Frontiers in Psychiatry, 13,
900615. https://doi.org/10.3389/fpsyt.2022.900615
Olesen, K. V., Lønfeldt, N. N., Das, S., Pagsberg, A. K., &
Clemmensen, L. K. H. (2023). Predicting Obsessive-
HEALTHINF 2025 - 18th International Conference on Health Informatics
282

Compulsive Disorder Events in Children and
Adolescents in the Wild Using a Wearable Biosensor
(Wrist Angel): Protocol for the Analysis Plan of a
Nonrandomized Pilot Study. JMIR Research Protocols,
12(1), e48571. https://doi.org/10.2196/48571
Popovic, S., Slamic, M., & Cosic, K. (2006). Scenario Self-
Adaptation in VR Exposure Therapy for PTSD
Provenza, N. R., Sheth, S. A., Dastin-van Rijn, E. M.,
Mathura, R. K., Ding, Y., Vogt, G. S., Avendano-
Ortega, M., Ramakrishnan, N., Peled, N., Gelin, L. F.
F., Xing, D., Jeni, L. A., Ertugrul, I. O., Barrios-
Anderson, A., Matteson, E., Wiese, A. D., Xu, J.,
Viswanathan, A., Harrison, M. T., … Borton, D. A.
(2021). Long-term ecological assessment of
intracranial electrophysiology synchronized to
behavioral markers in obsessive-compulsive disorder.
Nature Medicine, 27(12), 2154–2164. https://doi.org/
10.1038/s41591-021-01550-z
Serrano, M. Á., Rosell-Clari, V., & García-Soriano, G.
(2019). The Role of Perceived Control in the
Psychophysiological Responses to Disgust of
Subclinical OCD Women. Sensors, 19(19), Article 19.
https://doi.org/10.3390/s19194180
Shevlin, M., McBride, O., Murphy, J., Miller, J. G.,
Hartman, T. K., Levita, L., Mason, L., Martinez, A. P.,
McKay, R., Stocks, T. V. A., Bennett, K. M., Hyland,
P., Karatzias, T., & Bentall, R. P. (2020). Anxiety,
depression, traumatic stress and COVID-19-related
anxiety in the UK general population during the
COVID-19 pandemic. BJPsych Open, 6(6), e125.
https://doi.org/10.1192/bjo.2020.109
Slade, T., Johnston, A., Oakley Browne, M. A., Andrews,
G., & Whiteford, H. (2009). 2007 National Survey of
Mental Health and Wellbeing: Methods and Key
Findings. Australian & New Zealand Journal of
Psychiatry, 43(7), 594–605. https://doi.org/10.1080/
00048670902970882
Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C.,
Reddy, Y. C. J., Shavitt, R. G., van den Heuvel, O. A.,
& Simpson, H. B. (2019). Obsessive–compulsive
disorder. Nature Reviews. Disease Primers, 5(1), 52.
https://doi.org/10.1038/s41572-019-0102-3
Stratou, G., Scherer, S., Gratch, J., & Morency, L.-P.
(2015). Automatic nonverbal behavior indicators of
depression and PTSD: The effect of gender. Journal on
Multimodal User Interfaces, 9(1), 17–29.
https://doi.org/10.1007/s12193-014-0161-4
Sundaravadivel, P., Goyal, V., & Tamil, L. (2020). i-RISE:
An IoT-based Semi-Immersive Affective monitoring
framework for Anxiety Disorders. 2020 IEEE
International Conference on Consumer Electronics
(ICCE), 1–5. https://doi.org/10.1109/ICCE46568.2020.
9043156
Suneetha, C., & Anitha, R. (2024). Advancements in
Speech-Based Emotion Recognition and PTSD
Detection through Machine and Deep Learning
Techniques: A Comprehensive Survey. International
Journal of Electronics and Communication
Engineering, https://doi.org/10.14445/23488549/
IJECE-V11I5P121
Thieme, A., Hanratty, M., Lyons, M., Palacios, J., Marques,
R. F., Morrison, C., & Doherty, G. (2023). Designing
Human-centered AI for Mental Health: Developing
Clinically Relevant Applications for Online CBT
Treatment. ACM Transactions on Computer-Human
Interaction, 30(2), 27:1-27:50.
Ugbolue, U. C., Duclos, M., Urzeala, C., Berthon, M.,
Kulik, K., Bota, A., Thivel, D., Bagheri, R., Gu, Y.,
Baker, J. S., Andant, N., Pereira, B., Rouffiac, K.,
Clinchamps, M., Dutheil, F., & on behalf of the
COVISTRESS Network. (2020). An Assessment of the
Novel COVISTRESS Questionnaire: COVID-19
Impact on Physical Activity, Sedentary Action and
Psychological Emotion. Journal of Clinical Medicine,
9(10), Article 10. https://doi.org/10.3390/jcm9103352
U.S. Department of Health & Human Services. (2024).
Anxiety Disorders. National Institute of Mental
Health https://www.nimh.nih.gov/health/topics/anxiety-
disorders
Verma, G., & Tiwary, U. S. (2017). Affect Representation
and Recognition in 3D Continuous Valence-Arousal-
Dominance Space. Multimedia Tools and Applications,
76. https://doi.org/10.1007/s11042-015-3119-y
Wagner, J., Triantafyllopoulos, A., Wierstorf, H., Schmitt,
M., Burkhardt, F., Eyben, F., & Schuller, B. W. (2023).
Dawn of the Transformer Era in Speech Emotion
Recognition: Closing the Valence Gap. IEEE
Transactions on Pattern Analysis and Machine
Intelligence, 45(9), 10745–10759. IEEE Transactions
on Pattern Analysis and Machine Intelligence.
https://doi.org/10.1109/TPAMI.2023.3263585
Walz, L. C., Nauta, M. H., & aan het Rot, M. (2014).
Experience sampling and ecological momentary
assessment for studying the daily lives of patients with
anxiety disorders: A systematic review. Journal of
Anxiety Disorders, 28(8), 925–937. https://doi.org/10.
1016/j.janxdis.2014.09.022
Watson, D., Clark, L. A., & Tellegen, A. (1988).
Development and validation of brief measures of positive
and negative affect: The PANAS scales. Journal of
Personality and Social Psychology, 54(6), 1063–1070.
https://doi.org/10.1037/0022-3514.54.6.1063
Wörtwein, T., & Scherer, S. (2017). What really matters—
An information gain analysis of questions and reactions
in automated PTSD screenings. 2017 Seventh
International Conference on Affective Computing and
Intelligent Interaction (ACII), 15–20. https://doi.
org/10.1109/ACII.2017.8273573
Yazdani, A., Skodras, E., Fakotakis, N., & Ebrahimi, T.
(2013). Multimedia content analysis for emotional
characterization of music video clips. EURASIP
Journal on Image and Video Processing, 2013(1), 26.
https://doi.org/10.1186/1687-5281-2013-26
Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E.,
Lanius, R. A., Nievergelt, C. M., Hobfoll, S. E.,
Koenen, K. C., Neylan, T. C., & Hyman, S. E. (2015).
Post-traumatic stress disorder. Nature Reviews Disease
Primers, 1(1), 15057. https://doi.org/10.1038/nrdp.
2015.57
Affective Computing in Anxiety Disorders: A Rapid Literature Review of Emotion Recognition Applications
283

Zeghari, R., Gindt, M., König, A., Nachon, O., Lindsay, H.,
Robert, P., Fernandez, A., & Askenazy, F. (2023).
Study protocol: How does parental stress measured by
clinical scales and voice acoustic stress markers predict
children’s response to PTSD trauma-focused therapies?
BMJ Open, 13(5), e068026. https://doi.org/10.1136/
bmjopen-2022-068026
Zhu, J., Zhang, Z., Guo, Z., & Li, Z. (2024). Sentiment
Classification of Anxiety-Related Texts in Social
Media via Fuzing Linguistic and Semantic Features.
IEEE Transactions on Computational Social Systems,
11(5), 6819–6829. IEEE Transactions on
Computational Social Systems. https://doi.org/10.1109/
TCSS.2024.3410391.
HEALTHINF 2025 - 18th International Conference on Health Informatics
284
