
Key Factors in Achieving Intersectoral Interoperability: A Scoping
Review
Eveline Prochaska
1,* a
, Franziska Bathelt
2,* b
, Michelé Zoch
1c
, Antonia Ewald
2
and Elisa Henke
1d
1
Institute for Medical Informatics and Biometry, Faculty of Medicine and University Hospital Carl Gustav Carus,
TUD Dresden University of Technology, Dresden, Germany
2
Thiem-Research GmbH, Cottbus, Germany
Keywords: Healthcare, Intersectoral Interoperability, Scoping Review.
Abstract: Intersectoral interoperability is a fundamental basis for effective collaboration and seamless information
exchange across various sectors of the healthcare system. This paper presents a scoping review to examine
the current state of research into intersectoral interoperability, focusing on the technical, syntactic, semantic,
and organizational levels. Key factors identified include the adoption of international standards for data
formats, terminologies, and communication protocols, as well as the establishment of trusted governance
structures and compliance with ethical and legal requirements. Syntactic interoperability was most frequently
addressed, followed by technical and semantic aspects, with organizational factors also playing a significant
role.
1 INTRODUCTION
Intersectoral interoperability refers to the ability to
seamlessly exchange and use information and data
across different sectors or domains to ensure
coordinated and effective care or collaboration
(Perlin et al., 2016). In healthcare, this particularly
means the integration and collaboration between
different actors and organizations that provide
different services or functions, such as:
General practitioners and specialists: primary
and secondary care sector
Hospitals: tertiary care sector
Public health: for population health, with
system, political and organizational focus.
In this context, interoperability is crucial to
enabling holistic patient care, as it facilitates the
exchange of patient records, diagnoses, treatment plans
and other relevant information. This can improve the
quality of care, reduce redundant examinations and
a
https://orcid.org/0000-0002-7609-1565
b
https://orcid.org/0000-0002-4139-5489
c
https://orcid.org/0000-0002-5577-7760
d
https://orcid.org/0000-0002-5002-2676
* These authors contributed equally to this work
treatments, and optimize coordination between the
various players in the healthcare system. Intersectoral
interoperability requires consideration of the following
four levels of interoperability: (1) technical
interoperability to ensure data exchange between
systems through technical components; (2) syntactic
interoperability to ensure harmonized data formats and
information models; (3) semantic interoperability to
ensure a common understanding of message content
between systems and/or users and (4) organizational
interoperability to ensure that the exchange of
information is secure, effective, and compliant with
legal and data protection requirements (Rezaei et al.,
2014).
Despite technological advances and the
introduction of numerous IT solutions, the seamless
integration of information and processes remains a
challenge. This challenge arises from the diversity of
the systems involved, the differences in the
technologies used, and the varying standards and
protocols employed in different sectors.
914
Prochaska, E., Bathelt, F., Zoch, M., Ewald, A. and Henke, E.
Key Factors in Achieving Intersectoral Interoperability: A Scoping Review.
DOI: 10.5220/0013373500003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th Inter national Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 2: HEALTHINF, pages 914-919
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
The aim of this study is to examine the extent to
which intersectoral interoperability is already being
addressed in the literature, including which core
aspects are particularly emphasized and whether
measures necessary for its implementation can be
derived. Building on this analysis, the study seeks to
develop a comprehensive understanding of the
complexity of intersectoral interoperability and to
formulate actionable recommendations for more
effective integration of the various healthcare sectors.
2 METHODS
To get an overview about current developments,
challenges and perspectives of intersectoral
interoperability in healthcare, we conducted a scoping
review. Our literature search focused on publications
describing intersectoral interoperability in the medical
field, especially the data exchange and/or collaboration
between different sectors of the healthcare system with
the aim of providing healthcare.
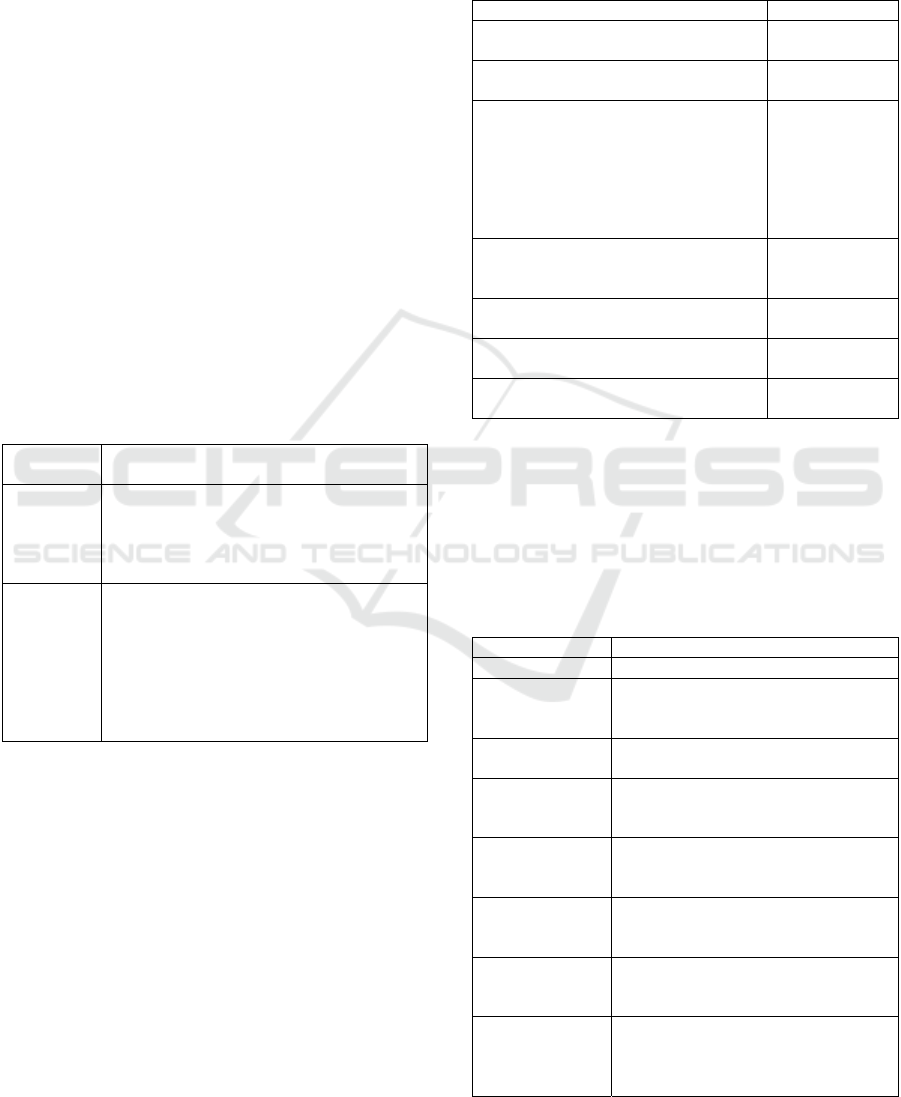
Table 1: Search strings used for the literature search in
PubMed and Web of Science.
Publication
database
Search string
PubMed
(medic* OR health*) AND (((intersectoral OR
inter sectoral OR inter-sectoral) OR
(crosssectoral OR cross-sectoral OR cross
sectoral) OR (multisectoral OR multi sectoral
OR multi-sectoral)) AND interoperability)
Web of
Science
(ALL=(medic*) OR ALL=(health*)) AND
(((ALL=(intersectoral) OR ALL=(inter
sectoral) OR ALL=(inter-sectoral)) OR
(ALL=(crosssectoral) OR ALL=(cross-
sectoral) OR ALL=(cross sectoral)) OR
(ALL=(multisectoral) OR ALL=(multi
sectoral) OR ALL=(multi-sectoral))) AND
ALL=(interoperability))
We followed the PRISMA guidelines (Moher et
al., 2009) and used two publication databases (i.e.
PubMed, and Web of Science) to search for relevant
publications until to May 30, 2024 (without starting
time limit) written in German or English
(Table 1).
This review was a two-step process consisting of a
title-abstract screening (TAS) and a full-text
screening (FTS). Both screening processes used the
same exclusion criteria listed in Table 2.
The screening team consisted of four reviewers
(FB, EH, MZ, AE). The TAS was carried out by two
reviewers (FB, EH) in Rayyan (Ouzzani et al., 2016)
blind mode so that each reviewer could label the
publication independently. The blind mode was
deactivated after all publications had been labeled and
the conflicts discussed and resolved. Thereafter, all
included publications were loaded as a new project
for FTS in Rayyan. The subsequent FTS was
conducted by four reviewers (AE, MZ, EH, FB).
Table 2: Exclusion criteria applied.
Description of criterion Label
Publication does not cover the medical
field in the sense of health care.
no_medic
Publication cites medical field as just one
p
otential area of application.
medic_
mentione
d
Publication does not deal with
intersectoral interoperability; it only
considers one sector (e.g. hospitals) or no
data exchange with the aim of healthcare
provision. This category also includes
telemedicine systems that do not focus on
combining data from different sectors.
no_intersec_
interop
Publication only mentions (intersectoral)
interoperability as a potential field of
application.
intersec_
interop_
mentione
d
Publication is available in a language
other than German or English.
foreign_
language
Publication is only an abstract, a keynote,
a letter to the editor or a tutorial.
wrong_publicati
ontype
Publication is not accessible or available
as full text.
no_fulltext
The FTS was also conducted in blind mode and
followed the same review process as the TAS. After
the FTS, we extracted the content of all included
publications based on the categories listed in Table 3.
The extracted content was stored in a table to enable
further analyses.
Table 3: Categories for data extraction.
Categor
y
Description
Countr
y
Country of the considered system
Connected
healthcare
p
roviders
Home, Hospital, General Practice,
Public Health Institutions
Level of
implementation
Concept, Proof of Concept, Routine
Technical
interoperability
aspects
How is technical interoperability
achieved?
Syntactical
interoperability
aspects
How is syntactical interoperability
achieved?
Semantical
interoperability
aspects
How is semantical interoperability
achieved?
Organizational
interoperability
aspects
How is organizational interoperability
achieved?
Further
interoperability
categories
and aspects
Are there other categories named in
publication? (How is interoperability in
this category achieved?)
Key Factors in Achieving Intersectoral Interoperability: A Scoping Review
915
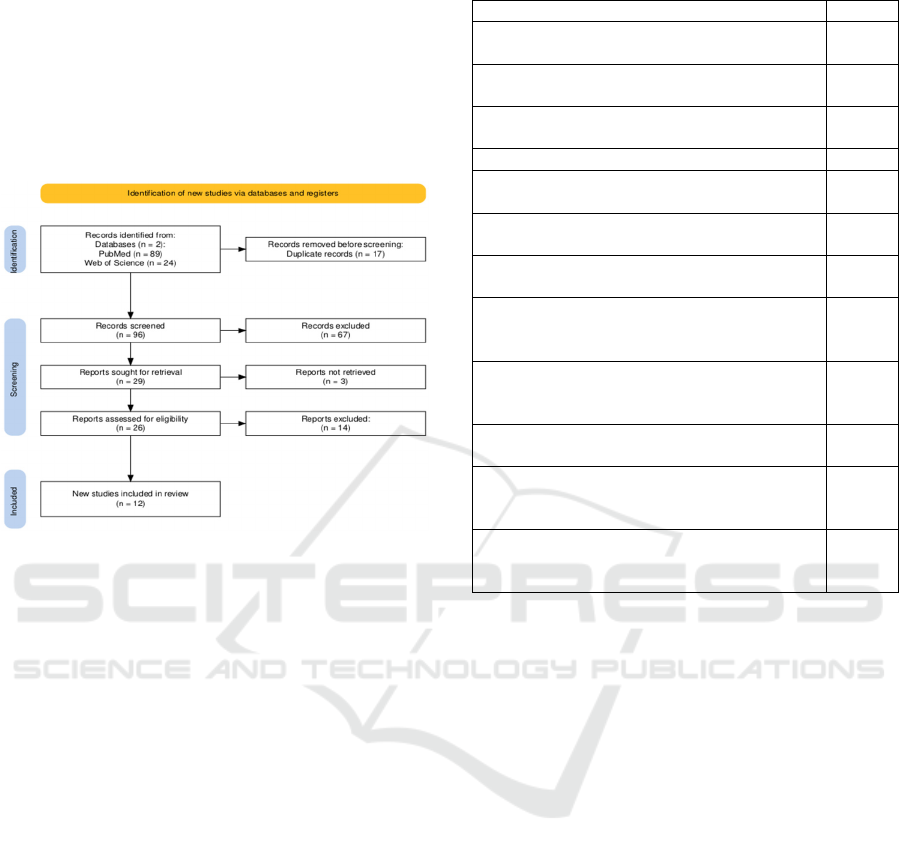
3 RESULTS
The literature search resulted in 113 publications.
After removing 17 duplicates, 96 publications were
screened during the TAS. By using the exclusion
criteria defined in Table 2 29 publications were
included for FTS. The screening process and results
are detailed shown in Figure 1.
Figure 1: PRISMA flow diagram according to (Haddaway
et al., 2022).
Finally, 12 studies were included in this review,
which are listed in Table 4 and assigned the sequence
numbers 1 to 12 for further analysis. A complete list
of the results of the literature search is available on
Zenodo (Henke, 2024).
The studies included in this review were
published between 2009 and 2021 and considered
healthcare providers from the following countries:
Denmark, Germany (3), Italy, USA (2), Haiti, Chile,
Thailand, Australia and worldwide. Furthermore, the
providers involved in intersectoral health care were
extracted. In all 12 studies, these were general
practices, in 11 studies hospitals, and in 7 studies
public health institutions. According to the predefined
extraction criteria (Table 3) the level of
implementation resulted in 4 concepts, 3 proof of
concepts and 5 routine uses.
The following Table 5 shows the methods
described in the studies for implementing
intersectoral interoperability in accordance with the
four previously defined interoperability levels. The
numbers 1 to 12 after each method indicate that this
method was considered in the respective study. Table
5 thus provides an overview of the various methods
for implementing interoperability and the frequency
with which these methods are applied.
Table 4: Studies included in this review.
Publication title and reference Number
A shared electronic health record: lessons from
the coalface (Silvester & Carr, 2009)
1
Chile´s National Center for Health Informatio
n
S
y
stems
(
Ca
p
urro et al., 2017
)
2
Cross-enterprise interoperability (Bauer et al.,
2020
)
3
Fosterin
g
g
lobal data sharin
g
(
Austin et al., 2020
)
4
Informatics for public health and health syste
m
collaboration (Lenert et al., 2021)
5
Interoperability after deployment (Kierkegaard,
2015)
6
Steps towards a digital health ecostystem
(
Serbanati et al., 2011
)
7
Success factors for implementing and sustaining
a mature electronic medical record in a low-
resource setting (deRriel et al., 2018)
8
The nephrology eHealth-system of the
metropolitan region of Hannover (Pape et al.,
2019)
9
The role of Integrating the Healthcare Enterprise
(
IHE
)
in telemedicine
(
Ber
g
h et al., 2015
)
10
The Strategic Implementation of Dat
a
Interoperability for Better Health Care Services
in Thailand (Kawtrakul et al., 2012)
11
Utilizing Standard Data Transactions and Public-
Private Partnerships to Support Healthy Weigh
t
Within the Community (Mikles et al., 2017)
12
Another additional aspect of interoperability
mentioned in three studies is the need to ensure an
adequate budget (e.g. for hardware, software, change
management, continuous training and ensuring
sustainability; 1,8,11). Without sufficient funds,
intersectoral interoperability cannot be achieved,
making the necessary budget a prerequisite.
On a technical level, web-based services such as
centralized databases, platforms and clouds are the
most frequently mentioned factors (67% of the
studies). International standards such as HL7 or IHE
for communication protocols and message formats
also play an important role (58%). These aspects
make it clear that a stable technological foundation is
essential to enable intersectoral exchange.
The semantic layer is heavily influenced by
international standards for terminology and
classification (67%). These ensure a unified language
and a common understanding between the actors
involved. The importance of shared repositories for
standardizing terms is mentioned less frequently
(25%), but it remains a valuable element for
improving interoperability.
HEALTHINF 2025 - 18th International Conference on Health Informatics
916

Table 5: Methods used for implementing intersectoral
interoperability.
Interoperability level
Mentioned in
stud
y
numbe
r
Sum* (in
%
)
Technical intero
p
erabilit
y
web services (centralize
d
databases, platforms, clouds,
server, public key infrastructure)
for communication
1, 3, 5, 6, 7,
8, 9, 11
8 (67)
international standards fo
r
communication and message
format
(
i.e. HL7, IHE, …
)
1, 3, 5, 8, 10,
11, 12
7 (58)
Semantic intero
p
erabilit
y
international standards fo
r
terminology and organization
systems, such as classifications
1, 2, 3, 8, 9,
10, 11, 12
8 (67)
shared repositories to enable
standardization of terms an
d
metadata
3, 4, 7 3 (25)
Syntactic interoperabilit
y
international standards for dat
a
exchange formats
1, 2, 3, 4, 5,
7, 8, 9, 10,
11, 12
11 (92)
Or
g
anizational intero
p
erabilit
y
trusted entity/authority for projec
t
and s
y
stem mana
g
ement
1, 2, 6, 11 4 (33)
affinity domains (by IHE, SOA
p
latform, …)
3, 7, 9, 10 4 (33)
guidelines for compliance with
local legal and ethical
requirements for data
p
rocessing
and stora
g
e
1, 4, 11, 12 4 (33)
unique national patient identifie
r
(
i.e. master
p
atient index
)
3,5,10 3 (25)
technology monitoring procedures
and licensing or certification o
f
software
2, 4 2 (17)
* of total 12
With 92% of the studies referring to international
standards for data exchange formats, syntactic
interoperability is the most widely recognized key
factor. This high figure shows how important
standardized data formats are for the harmonization
of different systems.
At the organizational level, the role of trusted
authorities (33%) and guidelines for compliance with
legal and ethical requirements (33%) are central. Less
frequently mentioned, but still significant, are the
introduction of national patient identifiers (25%) and
procedures for monitoring and certifying
technologies (17%).
4 DISCUSSION
The aim of this study was to examine which key
factors are addressed in the literature to ensure
intersectoral interoperability. The analysis of the 12
scientific studies highlights central factors that are
important for successful intersectoral
interoperability. These can be assigned to the four
levels of interoperability – semantic, syntactic,
technical and organizational. The goal of the research,
to capture the key factors for a functioning
interoperability, is supported by these results, as they
shed light on specific requirements and measures for
each level.
Summarizing all but one of the studies mentioned
the importance of syntactic standards, followed by
semantic standards and components of the
infrastructure for communication and technical
standards. Factors of organizational interoperability
are only found in approximately one-third of the
publications considered. Assuming that
organizational aspects are absolutely necessary to
achieve interoperability, it can be considered the
included studies did not report all necessary aspects.
The research only considers scientific literature
and disregards national programs, which are often the
driving force behind intersectoral interoperability
activities. Programs such as national health initiatives
or electronic health record projects play a key role in
promoting interoperability, but were not analysed.
This limitation could affect the comprehensiveness of
the identified factors. Nevertheless, the results of the
studies provide valuable insight into evidence-based
approaches and provide a solid foundation for further
research.
In summary, no general statement can be made
about the measures necessary to ensure intersectoral
interoperability. However, the literature showed that
the implementation of intersectoral interoperability
requires the consideration of actions at all four levels
of interoperability.
5 CONCLUSIONS
The scoping review examined the presence of
intersectoral interoperability in the literature. The
core aspects and measures for implementing
intersectoral interoperability were presented. It was
shown that aspects of syntactic interoperability were
mentioned most frequently, followed by technical and
semantic interoperability. Activities to implement
organizational interoperability are reported least.
Key Factors in Achieving Intersectoral Interoperability: A Scoping Review
917

The identification and presentation of the key
factors makes it clear that intersectoral
interoperability is based on a combination of
technological standards, uniform data formats,
terminological systems and organizational structures.
Future research should supplement the scientific
literature with findings from national programs to
obtain a more comprehensive picture of the factors
and challenges.
It is evident that further research, incorporating all
four levels of intersectoral interoperability is needed
to gain a more comprehensive understanding of this
subject.
REFERENCES
Austin, C. C., Bernier, A., Bezuidenhout, L., Bicarregui,
J., Biro, T., Cambon-Thomsen, A., Carroll, S. R.,
Diallo, G., Duflot, T., Garcia, L., Gesing, S., Gonzalez-
Beltran, A., Gururaj, A., Harrower, N., & Lin, D.
(2020). Fostering global data sharing: Highlighting the
recommendations of the Research Data Alliance
COVID-19 working group. Wellcome Open Research,
5. https://doi.org/10.12688/wellcomeopenres.16378.1
Bauer, J., Rohner-Rojas, S., & Holderried, M. (2020).
Cross-enterprise interoperability: Challenges and
principles for technical implementation. Radiologe,
60(4), 334–341. https://doi.org/10.1007/s00117-019-
00626-9
Bergh, B., Brandner, A., Heiß, J., Kutscha, U., Merzweiler,
A., Pahontu, R., Schreiweis, B., Yüksekogul, N.,
Bronsch, T., & Heinze, O. (2015). The role of
Integrating the Healthcare Enterprise (IHE) in
telemedicine. Bundesgesundheitsblatt -
Gesundheitsforschung - Gesundheitsschutz, 58(10),
1086–1093. https://doi.org/10.1007/s00103-015-
2226-2
Capurro, D., Echeverry, A., Figueroa, R., Guiñez, S.,
Taramasco, C., Galindo, C., Avendaño, A., García, A.,
& Härtel, S. (2017). Chile’s national center for health
information systems: A public-private partnership to
foster health care information interoperability. Studies
in Health Technology and Informatics, 245, 693–695.
https://doi.org/10.3233/978-1-61499-830-3-693
deRriel, E., Puttkammer, N., Hyppolite, N., Diallo, J.,
Wagner, S., Honoré, J. G., Balan, J. G., Celestin, N.,
Vallès, J. S., Duval, N., Thimothé, G., Boncy, J., Coq,
N. R. L., & Barnhart, S. (2018). Success factors for
implementing and sustaining a mature electronic
medical record in a low-resource setting: A case study
of iSanté in Haiti. Health Policy and Planning, 33(2),
237–246. https://doi.org/10.1093/heapol/czx171
Haddaway, N. R., Page, M. J., Pritchard, C. C., &
McGuinness, L. A. (2022). PRISMA2020: An R
package and Shiny app for producing PRISMA 2020-
compliant flow diagrams, with interactivity for
optimised digital transparency and Open Synthesis.
Campbell Systematic Reviews, 18(2).
https://doi.org/10.1002/cl2.1230
Henke, E. (2024). Data Set of this scoping review at
Zenodo. Results of the TAS and FTS.
https://doi.org/10.5281/zenodo.13841978
Kawtrakul, A., Kijsanayotin, B., & Mulasastra, I. (2012).
The Strategic Implementation of Data Interoperability
for Better Health Care Services in Thailand.
Proceedings of the European Conference on E-
Government (ECEG), 369–377.
Kierkegaard, P. (2015). Interoperability after deployment:
Persistent challenges and regional strategies in
Denmark. International Journal for Quality in Health
Care, 27(2), 147–153.
https://doi.org/10.1093/intqhc/mzv009
Lenert, L. A., Ding, W., & Jacobs, J. (2021). Informatics
for public health and health system collaboration:
Applications for the control of the current COVID-19
pandemic and the next one. Journal of the American
Medical Informatics Association,
28(8), 1807–1811.
https://doi.org/10.1093/jamia/ocab066
Mikles, S. P., Wiltz, J. L., Reed-Fourquet, L., Painter, I. S.,
Iv, ;, & Lober, W. B. (2017). Utilizing Standard Data
Transactions and Public-Private Partnerships to
Support Healthy Weight Within the Community.
Generating Evidence & Methods to Improve Patient
Outcomes (EGEMS), 1(5), 21.
https://doi.org/10.5334/egems.242
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Antes,
G., Atkins, D., Barbour, V., Barrowman, N., Berlin, J.
A., Clark, J., Clarke, M., Cook, D., D’Amico, R.,
Deeks, J. J., Devereaux, P. J., Dickersin, K., Egger, M.,
Ernst, E., Gøtzsche, P. C., … Tugwell, P. (2009).
Preferred reporting items for systematic reviews and
meta-analyses: The PRISMA statement. PLoS
Medicine, 6(7).
https://doi.org/10.1371/journal.pmed.1000097
Ouzzani, M., Hammady, H., Fedorowicz, Z., &
Elmagarmid, A. (2016). Rayyan-a web and mobile app
for systematic reviews. Systematic Reviews, 5(1).
https://doi.org/10.1186/s13643-016-0384-4
Pape, L., Schneider, N., Schleef, T., Junius-Walker, U.,
Haller, H., Brunkhorst, R., Hellrung, N., Prokosch, H.
U., Haarbrandt, B., Marschollek, M., & Schiffer, M.
(2019). The nephrology eHealth-system of the
metropolitan region of Hannover for digitalization of
care, establishment of decision support systems and
analysis of health care quality. BMC Medical
Informatics and Decision Making, 19(1).
https://doi.org/10.1186/s12911-019-0902-0
Perlin, J. B., Baker, D. B., Brailer, D. J., Evolution
Partners, H., & Fridsma, D. B. (2016). Information
Technology Interoperability and Use for Better Care
and Evidence A Vital Direction for Health and Health
Care About the Vital Directions for Health and Health
Care Series. NAM Perspectives, 6(9).
https://doi.org/10.31478/201609r
Rezaei, R., Chiew, T. K., Lee, S. P., & Shams Aliee, Z.
(2014). Interoperability evaluation models: A
HEALTHINF 2025 - 18th International Conference on Health Informatics
918

systematic review. Computers in Industry, 65(1), 1–23.
https://doi.org/10.1016/J.COMPIND.2013.09.001
Serbanati, L. D., Ricci, F. L., Mercurio, G., & Vasilateanu,
A. (2011). Steps towards a digital health ecosystem.
Journal of Biomedical Informatics, 44(4), 621–636.
https://doi.org/10.1016/j.jbi.2011.02.011
Silvester, B. V., & Carr, S. J. (2009). A shared electronic
health record: lessons from the coalface. Medical
Journal of Australia (MJA), 190(11), 113–116.
https://doi.org/10.5694/j.1326-5377.2009.tb02615.x
Key Factors in Achieving Intersectoral Interoperability: A Scoping Review
919
