
Introducing Virtuality - Virtual Care Process Simulator: A Concept
Utilizing Synthetic Data and a Digital Health Sandbox for Care
Process Simulations
Fanny Apelgren
a
, Mattias Seth
b
, Hoor Jalo
c
, Bengt Arne Sjöqvist
d
and
Stefan Candefjord
e
Department of Electrical Engineering, Chalmers University of Technology, Gothenburg, Sweden
Keywords: Synthetic Health Data, Digital Health Sandbox, Simulations, Artificial Intelligence, Machine Learning, Fall
Accidents, Stroke, Trauma, Motor Vehicle Crashes, Virtuality, Virtual Care Process Simulator.
Abstract: To design effective and safe IT systems for healthcare is a significant technical and societal challenge, and it
is of highest importance to confirm safety of patients when implementing new innovations. It would be
beneficial if new innovations could be verified and validated in a realistic and safe digital environment using
data that preserve patient integrity and safety, before going into real clinical trials and market release. In this
article we introduce and describe Virtuality - Virtual Care Process Simulator, a concept for realistic simulation
of healthcare scenarios in a digital sandbox environment using synthetic health data. The concept represents
a safe environment to develop, test and prepare systems and digital tools for usage in healthcare.
1 INTRODUCTION
To design effective and safe IT systems for healthcare
is a major challenge, and there is plenty of examples
of systems that have not fulfilled the goal of
facilitating provision of high-quality care (Campion-
Awwad et al., 2014; Hertzum et al., 2022). For
example, The National Programme for IT in the NHS
(NPfIT) in the UK, a large IT programme for the
public sector, was cancelled after delays, stakeholder
opposition and implementation issues (Campion-
Awwad et al., 2014). Some of the highlighted
problems with NPfIT was confidentiality and security
of patients, unreliable software and lack of
engagement with end-users (Campion-
Awwad et al., 2014). In Sweden, IT system
functionality deficiencies and lack of a standardized
infrastructure are reported to cause technostress
leading to critical incidents (Stadin et al., 2020), and
to be a barrier to innovation such as precision
medicine and developing Clinical Decision Support
a
https://orcid.org/0009-0006-6138-0619
b
https://orcid.org/0000-0002-3737-3316
c
https://orcid.org/0000-0001-6975-8520
d
https://orcid.org/0000-0002-6564-737X
e
https://orcid.org/0000-0001-7942-2190
Systems (CDSS) (Fioretos et al., 2022;
Frisinger & Papachristou, 2023). These are all issues
that urge the importance to prepare systems for
implementation, through sufficient testing and
thought-through requirement specifications.
In the healthcare industry, safety of patients is of
highest importance. Regulations put high demands on
devices, digital tools and systems being safe to use
and free of bugs. One important step for new
innovations before entering the market is passing
clinical trials, which requires confirmed effectiveness
and safety for the patients and users. This necessitates
extensive verification and validation and access to
high quality data. There is a need to boost innovation
and speed up the development process of new
technologies and systems for healthcare, enabling
promising research to reach the market earlier, while
ensuring regulatory compliance. A new
complementary method to traditional product
development is virtual tests with simulated healthcare
processes and synthetic data. Early research shows
Apelgren, F., Seth, M., Jalo, H., Sjöqvist, B. A. and Candefjord, S.
Introducing Virtuality - Virtual Care Process Simulator: A Concept Utilizing Synthetic Data and a Digital Health Sandbox for Care Process Simulations.
DOI: 10.5220/0013401300003911
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 18th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2025) - Volume 1, pages 1127-1135
ISBN: 978-989-758-731-3; ISSN: 2184-4305
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
1127

high potential for usage of synthetic data
(Chan et al., 2022; Dahmen & Cook, 2019;
Walonoski et al., 2018) and digital sandboxes
(Leckenby et al., 2021) for simulations in healthcare.
These technologies are suggested as important
building blocks for virtual testing environments.
In the Care@Distance group at Chalmers
University of Technology in Sweden, a concept and
solution for simulation and testing of digital tools for
healthcare is under development. The concept, called
Virtuality - Virtual Care Process Simulator, has been a
stepwise process over the past 10 years, as a result of
insights from several projects and practical experiences
(Andersson Hagiwara et al., 2019; Bakidou et al.,
2023; Candefjord et al., 2024; Fhager et al., 2018; Lee
et al., 2023; Maurin Söderholm et al., 2019). It consists
of several different parts that together build a virtual
simulation environment: synthetic health data, Digital
Health Sandbox (DHS) and third-party applications.
Through Virtuality, digital systems and tools can be
tested in a safe environment, before going into real
clinical trials, implementing systems and entering the
market.
The Care@Distance group performs research on
digital solutions for healthcare, with focus on
improving the care process by introducing new CDSS
based on innovative methods and Artificial
Intelligence (AI).
By using virtual care process simulations, we
could prepare systems and tools for the clinical
environment and avoid iterating clinical trials again
when potential problems and bugs in the systems
arise. An important part of virtual care process
simulations is usage of digital health sandbox
environments, i.e. environments in which developers
can test and modify innovations in collaboration with
clinicians, adding and removing features or
combining them with other related innovations
(Ribiere & Tuggle, 2010). DHS acts as a safe-space
in which algorithms and tools for healthcare can be
tested and further developed iteratively, before tested
in the real-world clinical settings
(Leckenby et al., 2021).
For Virtuality to be useful in performing realistic
simulations, it needs to have access to relevant and
high-quality data. The demand of high-quality data
for medical and healthcare research are increasing
and the challenges with accessing those data are
highlighted by many (Kokosi & Harron, 2022;
Moniz et al., 2009; Tsao et al., 2023;
Walonoski et al., 2018). The information kept in
Electronic Health Records (EHR) is highly sensitive
and usage of real data should respect integrity,
confidentiality and security for the patients.
To avoid unnecessary use of sensitive data,
simulations on artificially generated versions of
patient health data, so-called synthetic health data, is
a suggested solution (Kokosi & Harron, 2022).
Synthetic data mimics the statistical properties of
real-world data and leaves minimal traces to the real
data (Gonzales et al., 2023). Thereby, the possibility
to link the data to individuals is low and the integrity
and safety of individuals is kept.
By connecting synthetic data with DHS and
running simulations enabled by a scenario engine
used for mimicking selected care processes,
Virtuality is a promising concept to solve above
mentioned challenges and needs. Our vision with
Virtuality is to get as close to reality as possible
without involving real patients in testing, and to
validate and simulate new IT-tools improving care
processes. In this article, we will present Virtuality,
describe its parts and motivate the usage of it by
exemplifying two different scenarios of healthcare
processes simulated in the virtual environment. Our
initial target scenarios are for time-critical patient
conditions, i.e. trauma represented by fall at home
and motor vehicle crash, and stroke, which are
important societal problems representing significant
morbidity and mortality.
2 RELATED WORK
In recent years the interest in using digital sandboxes,
synthetic data and simulation environments in the
healthcare sector have increased
(Leckenby et al., 2021; Pezoulas et al., 2024).
The approach of using a sandbox environment can
be divided into two main categories; the sandbox as a
testing environment and the sandbox as regulatory
sandbox approach (Leckenby et al., 2021). Both
categories are often focused on trial of products,
services and business models to confirm their
compliance with existing regulations before they are
implemented in real-world settings.
The concept introduced in this article, Virtuality, is
more focused on development and testing of new
services and systems in a simulated realistic setting. It
is unique in the sense that few similar technologies that
combine a digital sandbox with synthetic health data
are currently in use in a healthcare setting. One closely
related technology in use is the Blue Button Sandbox,
which uses synthetic claims data from U.S. Centers for
Medicare & Medicaid Services (CMS), to develop and
test applications and information systems that will
need to interact with CMS data systems and Medicare
services (Gonzales et al., 2023). The Blue Button
DEMS 2025 - Special Session on Design and Evaluation of Monitoring Systems
1128
Sandbox is oriented towards development of services
that benefits Medicare enrolees, rather than being
applicable to a wider range of data, systems and
services.
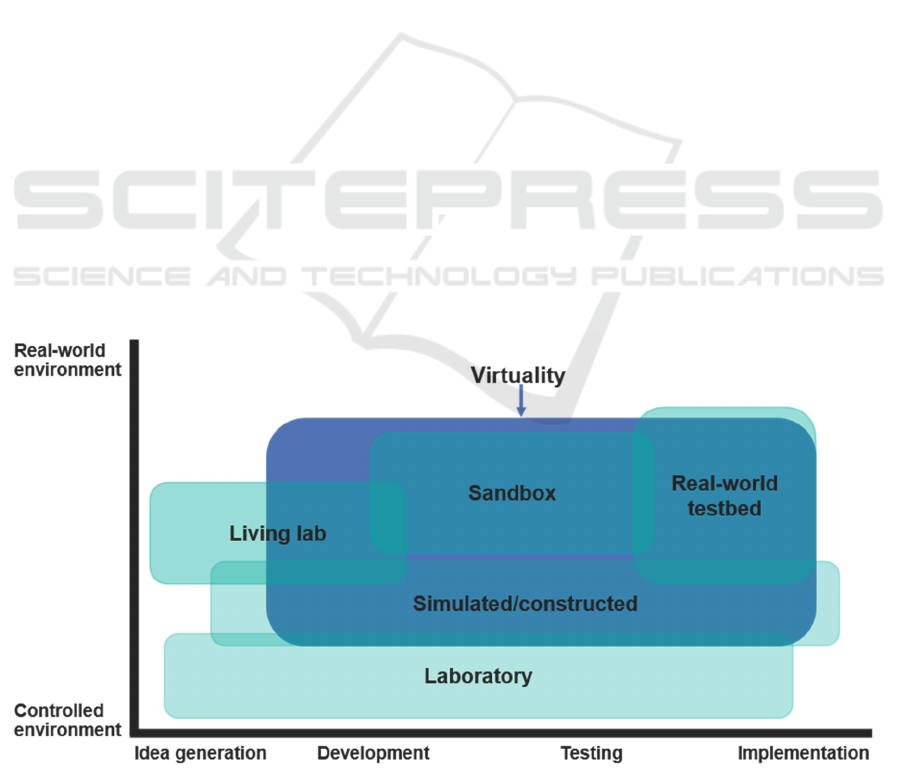
There are several different main testing
environments used for product innovation and
development of systems and tools for healthcare
(Leckenby et al., 2021). In Figure 1, we have
positioned Virtuality in relation to other testing
environments. Compared to sandboxes currently
used, Virtuality aims for a broader scope and to be
useful during a broader extent of the development
process, from idea generation to implementation.
The number of studies on synthetic health data
generation shows an increasing trend between the
years of 2015–2024 (Pezoulas et al., 2024). Synthetic
health datasets are created and used for a broad range
of use cases. Gonzales et al. (2023) summarized
current use cases as a) simulation and prediction
research, b) hypothesis, methods, and algorithm
testing, c) epidemiology/public health research,
d) health IT development, e) education and training,
f) public release of datasets, and g) linking data. The
past years, several public synthetic health datasets
have been published. Some examples of published,
publicly available synthetic health datasets and tools
for synthetic health data generation are: 1) Synthea,
generates synthetic EHRs through statistical
modelling and usage of publicly available health
statistics, clinical guidelines and protocols
(Walonoski et al., 2018), 2) SynSys, a Machine
Learning (ML)-based synthetic data generation
method for generating synthetic time series sensor
data for healthcare application
(Dahmen & Cook, 2019), 3) Medkit-Learn(ing)
Environment, a ML-based synthetic data generation
method for generating synthetic medical datasets
(Chan et al., 2022). All three above synthetic health
data generation methods and datasets are open source,
allowing developers to contribute to further
development.
The importance of conducting full-scale
simulations and their potential in prehospital care was
highlighted by Maurin Söderholm and colleagues
(Maurin Söderholm et al., 2019). By providing an
isolated and controlled environment, stakeholders can
test, validate and confirm their ideas based on
synthetic data, in order to better prepare systems for
wider implementations (Leckenby et al., 2021). This
can guide decision making and allow stakeholders to
draw conclusions comparable to those from real
clinical settings, without the immediate need to
address legal barriers.
3 CONCEPT
The Care@Distance group and collaborators are now
developing a virtual testing environment, called
Virtuality. Virtuality provides all the tools needed to
set up, configure and run realistic healthcare
simulations in isolated environments, facilitating
performing
the first two steps in the Verified
Figure 1: Positioning of Virtuality concept in relation to the main testing environments used in product innovation (adapted
from (Leckenby et al., 2021) and (Arntzen et al., 2019)).
Introducing Virtuality - Virtual Care Process Simulator: A Concept Utilizing Synthetic Data and a Digital Health Sandbox for Care Process
Simulations
1129
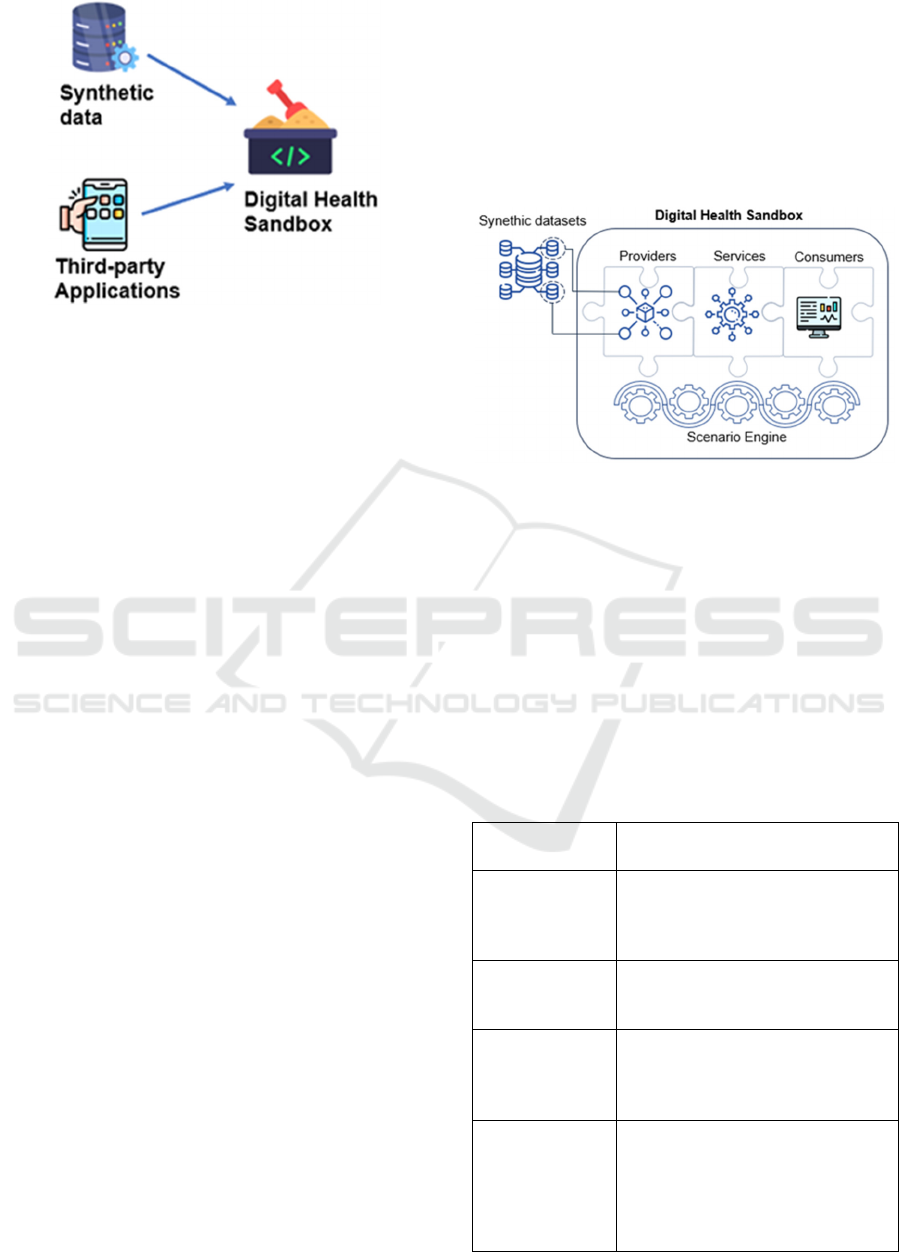
Figure 2: Virtuality consists of 1) synthetic data, 2) third-
party applications, 3) Digital Health Sandbox.
Innovation Process for Healthcare Solutions (VIPHS)
model, which corresponds to defining a prototype
(Lee et al., 2023). This includes synthetic data
generation mechanisms, access to third-party
applications and DHS, see Figure 2.
Virtuality is based on the Acute Support
Assessment and Prioritizing (ASAP) Concept. This
concept emphasizes the importance of aggregating
data from multiple sources to increase decision
precision, streamline workflows and improve patient
safety. By building the Virtuality environment around
the ASAP Concept, it ensures that interoperability
remains the central focus and foundation of all
activities within this environment.
3.1 Digital Health Sandbox
The DHS will be one of the main parts within
Virtuality, enabling effective utilization of synthetic
data and digital technologies to test and validate the
clinical utility of digital innovations, refer to Figure 2
and 3. Regardless of applications, whether it is a fall
detection system, stroke detection or trauma severity
prediction (Bakidou et al., 2023), the goal is to bridge
the gap between stakeholders, enabling clinicians,
engineers and researchers to actively participate in the
design, execution and evaluation of advanced and
realistic simulations (Maurin Söderholm et al., 2019).
The DHS is based around four core building
blocks: ASAP Providers, Services, Consumers and
the Scenario Engine. Each of these blocks, along with
their associated functionality can be seen in Table 1.
Depending on the scope and objective of the
simulation, different number of components within
each building block can be used, and various levels of
complex interaction patterns can be applied. This
means that the Graphical User Interface (GUI) also
adapts to the specific simulation scenario. For
example, in a traffic safety scenario, a user may want
to simulate how AI-algorithms and vehicle sensors
can be utilized to assess the likelihood of injuries in a
motor vehicle crash (Maurin Söderholm, 2023). In
this case, the GUI should adapt to that specific
scenario, meaning that the user should be able to
select the number of cars, car model, car occupants,
crash type, type of AI-model and type of sensor data.
Figure 3: In Virtuality, DHS can be combined with
synthetic datasets to enable realistic simulations and get full
control of the simulation scenario.
Together, the ASAP Building Blocks constitute a
comprehensive and fully customable testing arena
where any combination of devices, algorithms and
platforms can be put together to allow for realistic
simulations. The ASAP Concept supports this, by
promoting open – and standardized interoperability
interfaces, as well as synthetic data to avoid
dependencies on third-party vendors, see Figure 3.
Table 1: The DHS is composed of four building blocks:
Providers, Services, Consumers and Scenario Engine.
ASAP
Buildin
g
Block
Functionality
Providers
Devices or information providers
responsible for initiating a
simulation by sending data to ASAP
Services for further
p
rocessin
g
.
Services
Software modules responsible for
processing information coming from
ASAP Providers.
Consumers
GUI (
Graphical User Interface)
responsible for displaying
information from ASAP Services to
end users.
Scenario Engine
Orchestrator that enables the user to
determine what to simulate and how
it should be conducted, ie., decide on
the simulation scenario, what
components to be used and how they
should fit together.
DEMS 2025 - Special Session on Design and Evaluation of Monitoring Systems
1130

For instance, the synthetic data generator within
Virtuality could be used to create a fictious
smartwatch to be used within the DHS (the ASAP
Provider Building Block in Table 1). This approach
would provide immediate access to realistic data,
refer to Figure 3, eliminating delays typically caused
by dependency on third-party vendors and
applications. The Provider Building block
(smartwatch) could be integrated with an AI-based
trauma algorithm (Bakidou et al., 2023) and a third-
party EHR, represented by the ASAP Service
Building Block and Consumer Building Block,
respectively. The ASAP Concept would guide this
integration process, by specifying open – and
standardized interfaces between and within each
building block.
3.2 Synthetic Data
For the DHS to be effective and useful, data that can
act as ASAP Provider is needed. To get qualitative
real health data can be challenging and requires going
through often extensive data access applications
(Kokosi & Harron, 2022). An alternative data source
to use as ASAP Provider is synthetic data. Synthetic
data is an interesting complement to real data and has
several advantages that motivates why it is useful:
a) accelerate development processes, b) secure
patient anonymity, privacy, integrity and safety,
c) improve data accessibility, d) increase data volume
and diversity, e) account for underrepresented data
and scenarios, f) testing of not yet existing solutions,
g) address regulatory challenges in early
development without using patient data and
h) decrease dependency of data providers.
Synthetic health data can be divided into five main
categories; tabular data, image and video data, time-
series data, radionics data and multimodal
data (Pezoulas et al., 2024). The Care@Distance
group aims to create a database of synthetic data,
which can be used to run simulations on different
scenarios in the DHS. With their primary focus on
improving the prehospital care, synthetic versions of
data accessible in prehospital healthcare settings will
be the primary focus. In a prehospital setting tabular
data like EHR, image and video data of a patient or
accident site and timeseries sensor data are some of
the most interesting categories.
In addition, new data sources with the potential to
improve prehospital care are of high interest. A broad
range of parameters and different kind of data should
be available and possible to use for simulations in
Virtuality. Synthetic data can be used alone or in
combination with real data. The purpose with the
synthetic data is not to completely replace real data,
but rather to enable early verification and validation
of tools and systems before accessing real data
(Kokosi & Harron, 2022).
In a prehospital setting, for example in a motor
vehicle crash, ambulance or smart home, video data
are a promising data source. Video data in
ambulances could enable automated assessment and
informed decision-making during emergencies
(Jalo et al., 2023). To explore the use of synthetic data
and video analysis in the early characterization of
stroke-related eye movements, we generated 69
videos simulating typical eye movements seen in
stroke patients (Ollila et al., 2024). These videos
were reviewed and deemed clinically relevant by a
stroke neurologist, making them suitable for
developing CDSS. The synthetic videos were
combined with real recordings of healthy individuals
mimicking stroke-related eye movements. The use of
synthetic data resulted in creating a larger dataset,
which was crucial for models training and evaluation
to ensure strong performance.
3.3 Simulation Scenarios
In Sweden, senior citizens have been wearing social
alarms since early 1980s (Lydahl, 2024). These
alarms, consisting of a manual alarm button which
usually looks like a clock or a pendant, are frequently
used in Home Care Services (HCS) and in nursing
homes. Although these social alarms are the most
common welfare technology in the Nordic Countries
(Lydahl, 2024), an alarm from this device might be
difficult to interpret. Does the patient need acute
medical attention, or do they just need to refill a glass
of water? Since these alarms are used in both acute
and non-acute scenarios, it becomes stressful for the
personnel and can pose a danger to the patient if
critical alarms are overlooked or delayed.
Therefore, it could be valuable for the HCS to
investigate alternative setups. Perhaps combining the
social alarm with complementary information from
other sources, as in Figure 4, or analyzing the data
with AI, could give meaningful insights. For
example, if the social alarm data were accompanied
by the patient’s heart rate, angular velocities, gait
patterns and medical history, it could potentially
reveal a frail individual with a history of osteoporosis
who has experienced a fall.
This setup could potentially provide more
valuable insights, allowing the nurse to plan
appropriate interventions in a timely manner and help
in prioritizing among multiple occurring alarms. Such
simulations could be carried out within Virtuality by
Introducing Virtuality - Virtual Care Process Simulator: A Concept Utilizing Synthetic Data and a Digital Health Sandbox for Care Process
Simulations
1131
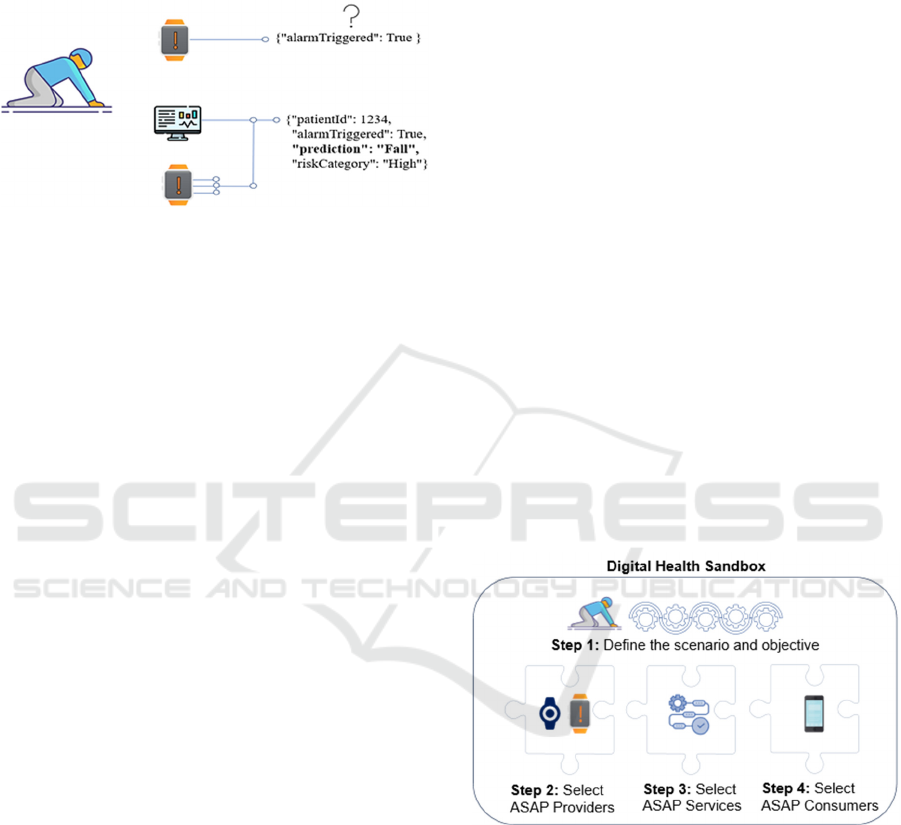
utilizing the DHS and synthetic data, see Figure 4.
The results from the simulation could potentially lead
to an extension of current social alarm services,
enhance patient safety, and optimize care delivery.
Figure 4: By aggregating data from multiple sources,
decision precision can be increased. By utilizing synthetic
data, more valuable insight could potentially be provided to
end-users during system development and tests.
Two different simulation scenarios, and how they
could be set up in Virtuality, will be described below.
Let us first assume that a user wants to investigate
new technologies and workflows to detect falls, as
alternatives or complements to the current social
alarm systems used in nursing homes. This could be
done as a realistic simulation within Virtuality,
utilizing standardized synthetic datasets together with
interoperable health applications.
The first step is to define the scope and objective
of the simulation in the DHS using the Scenario
Engine. This step is essential, as all subsequent
actions are tailored to the specific scenario. In the
case of fall detection simulations in nursing homes,
the user can start by defining a patient persona in the
Scenario Engine (step 1 in Figure 5). With just a few
clicks, a realistic but fictious elderly patient is
generated. This will create a synthetic patient profile,
including information about the patient’s age, sex,
residential address, living situation, medications and
medical history.
In the next step (step 2 in Figure 5), the user
decides what sensors to be included in the simulation.
In this scenario, the user might want to add a
smartwatch together with the social alarm as two
components in the ASAP Provider Building Block.
Based on the previously defined patient profile, the
synthetic sensor data will be dynamically generated
to ensure realistic data that accurately reflects the
patient’s characteristics.
In step 3, the user specifies how the data received
from the ASAP Providers should be processed and
managed. This step includes options for data
processing as well as data storage. For example, the
user could choose to include an AI-algorithm for
binary classification that predicts the probability of a
fall, given that the elderly have pressed the social
alarm button. This AI algorithm will be represented
as the ASAP Service Building Block in Figure 5.
In step 4, the user chooses how the output from
the algorithm will be presented to the nurses. Maybe
the nurse should be notified in a mobile app? This can
be achieved by adding the mobile app as an ASAP
Consumer Building Block. This building block
represents how and when information should be
available and presented to end users. Aspects such as
user-friendliness of the GUI can be practically tested.
Once step 1–4 in Figure 5 has been completed,
corresponding to step 1 in the VIPHS model (Lee et
al., 2023), an ASAP Pipeline has been created. The
ASAP Pipeline represents a selection of ASAP
Building Blocks which can be used for simulating the
effectiveness of the specific setup. For example, the
pipeline created in Figure 5, could be used to examine
the effectiveness of combining real-time smartwatch
data with social alarms, using a binary classification
model to predict falls among elderly at nursing
homes. A summary of the simulation process,
including a detailed description of the integration
process and its components, could be summarized in
a downloadable pdf-report. This report could act as a
recommendation or recipe for how to move this
simulation closer to clinical practice.
Figure 5: Example of a fall simulation conducted within
DHS.
In the case of stroke, timely and accurate
assessment is critical, with subtypes like large vessel
occlusion (LVO) requiring specialized interventions
(Jalo et al., 2023). Stroke mimics, such as seizures or
migraines, can complicate the assessment, making
prehospital triage more challenging. If a user wants to
simulate how AI models and video analysis can
identify whether a patient has a stroke and
characterize the type (e.g., ischemic, hemorrhagic or
LVO) in an ambulance setting, the GUI in the DHS
DEMS 2025 - Special Session on Design and Evaluation of Monitoring Systems
1132
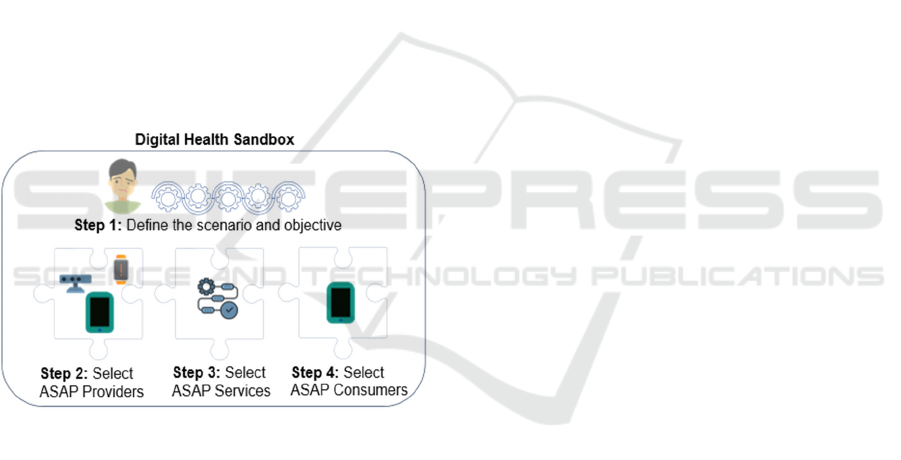
could adapt to support this scenario.
In step 1 in Figure 6, the user could select the
patient population to simulate, which in this case is
generating a synthetic patient exhibiting stroke
symptoms, such as facial asymmetry, abnormal eye
movements and limb paralysis.
In step 2, the user decides on which data sources
to include in the simulations such as cameras installed
in the ambulances, smartwatch, etc. as well as
configuring parameters for the prehospital
environment. In step 3, the user selects the AI models
to test their ability to identify stroke patients based on
the provided data. These models could provide
probability scores for stroke presence, subtype
classification and a recommendation for
transportation destination. In step 4, the simulation
results are tailored for end-user presentation. For
ambulance clinicians, results could be displayed on
devices commonly used in ambulances. For example,
the AI model might generate alerts indicating a high
probability of stroke, with a prediction of an LVO and
recommending transport to a comprehensive stroke
center.
Figure 6: Example of stroke simulation conducted within
DHS.
4 DISCUSSION
Virtuality connects existing tools where research has
been ongoing for several years, like digital sandboxes
and synthetic data (Chan et al., 2022;
Dahmen & Cook, 2019; Leckenby et al., 2021;
Walonoski et al., 2018), and build upon them to create
an easily accessible environment with potential to
boost healthcare innovations. The development of
Virtuality within the Care@Distance group is a result
of successful projects and observations of a rising
need for this type of solution.
As standalone tools, sandboxes and synthetic data
often require the users to do much programming
themselves to implement the available tools and
solutions. By requiring high programming
competence, we may exclude the users that possibly
would benefit the most from doing the simulations.
For example, clinicians could strongly benefit from
trying out new systems and tools in a simulated and
safe environment. Instead, by connecting the tools to
an environment that is easy to use even for non-
programmers, such as clinicians and care givers, we
introduce the possibility for a broader group to test
new systems as integrated with the current clinical
setup of systems. This can be an important step before
procurement of new systems are done, where
challenges in specifying requirements for
interoperability are common (Seth et al., 2024). The
aim with Virtuality is that a broad group of
practitioners working in the healthcare industry
should be able to use and benefit from simulating
healthcare scenarios.
Since 2016, regulatory sandboxes have been used
in the financial sector and later expanded to other
sectors
including the healthcare sector
(Leckenby et al., 2021). The introduction of Medical
Device Regulation (MDR) in Europe is welcomed to
further strengthen the safety of patients, but it has
introduced further challenges in development of new
innovative products and systems. By using sandbox
environments, exploration of processes that may
violate current rules and regulations but have
potentially large benefits if introduced into standard
practice are possible (Leckenby et al., 2021). This
enables taking one step further with innovations,
preparing them for clinical trials, motivating their
need on the market and showing the benefits they
bring. By implementing virtual testing environments
in healthcare innovation development processes, a
shortening of clinical trials is possible, resulting in a
reduction of associated costs.
There are several drawbacks with creating testing
and simulation environments that should be used by a
broad target group. First is a potential lack of
complexity in the environment. It is certainly easier
to build an environment with high complexity and
flexibility if the targeted user group has a higher
technical knowledge. The challenge will be to
balance a high complexity and flexibility of the
environment and keep it easy enough to use for users
with lower technical knowledge and skills.
Another challenge will be how to confidently
show that the created scenarios and synthetic data
used within the DHS are sufficiently realistic.
Achieving this requires a close collaboration with
clinicians, both when developing tools and concepts,
Introducing Virtuality - Virtual Care Process Simulator: A Concept Utilizing Synthetic Data and a Digital Health Sandbox for Care Process
Simulations
1133

and while running simulations and tests in the system
(Leckenby et al., 2021). One way to confirm realism
is to run Virtuality for scenarios where the outcome is
known and compare the results.
To confirm quality and realism of the data used is
important, especially when working with synthetic
data (Chen et al., 2021). Therefore, verification and
validation of the data is an important step in the
creation process. The quality of the synthetic data is
strongly related to the methods, models and
underlying data used to create it
(Gonzales et al., 2023). We also need to be aware of
the potential risk of traces from the original data left
in the synthetic dataset, which possibly could be a risk
for the integrity and privacy of patients
(Vallevik et al., 2024). Synthetic data shows high
potential to keep the integrity, privacy and
anonymity, but still the data should be treated with
respect and carefully used. Effort needs to be put in
on choosing appropriate methods and datasets to
work with, showing the realism of the created data
and ensure that the data is disconnected from the
patients in the original dataset.
We want to emphasize that the concept described
in this article is currently on a conceptual and early-
stage level. Further work is needed before Virtuality
is ready to run at full strength and its parts sufficiently
developed and connected. This article has shown the
potential of Virtuality and its building blocks. Now
the building blocks need to be connected, and the
process simulator tried out on realistic scenarios.
Future work includes developing the DHS further and
generating synthetic datasets. The first use cases in
Virtuality will be related to the scenarios exemplified
in this article; trauma represented by fall at home and
motor vehicle crash and stroke. Later, the scenarios
used will be expanded to include other interesting
healthcare scenarios.
5 CONCLUSIONS
In this article we have described Virtuality, a concept
for simulation of care processes in a safe digital
sandbox environment using synthetic health data. We
see a need and possibility to introduce this concept in
healthcare. By exemplifying two scenarios, we have
shown how Virtuality is intended to work and
motivated its potential to speed up development
processes in healthcare.
REFERENCES
Andersson Hagiwara, M., Lundberg, L., Sjöqvist, B. A., &
Maurin Söderholm, H. (2019). The Effects of
Integrated IT Support on the Prehospital Stroke
Process: Results from a Realistic Experiment. Journal
of Healthcare Informatics Research, 3(3), 300–328.
Arntzen, S., Wilcox, Z., Lee, N., Hadfield, C., & Rae, J.
(2019). Testing Innovation in the Real World.
Bakidou, A., Caragounis, E.-C., Andersson Hagiwara, M.,
Jonsson, A., Sjöqvist, B. A., & Candefjord, S. (2023).
On Scene Injury Severity Prediction (OSISP) model for
trauma developed using the Swedish Trauma Registry.
BMC Medical Informatics and Decision Making, 23(1),
206. doi.org/10.1186/s12911-023-02290-5
Campion-Awwad, O., Hayton, A., Smith, L., & Vuaran, M.
(2014). The National Programme for IT in the NHS: A
case study.
Candefjord, S., Andersson Hagiwara, M., Sjöqvist, B. A.,
Karlsson, J.-E., Nordanstig, A., Rosengren, L., &
Maurin Söderholm, H. (2024). Video support for
prehospital stroke consultation: Implications for system
design and clinical implementation from prehospital
simulations. BMC Medical Informatics and Decision
Making, 24(1), 146. doi.org/10.1186/s12911-024-
02539-7
Chan, A. J., Bica, I., Huyuk, A., Jarrett, D., & van der
Schaar, M. (2022). The Medkit-Learn(ing)
Environment: Medical Decision Modelling through
Simulation (No. arXiv:2106.04240). arXiv.
doi.org/10.48550/arXiv.2106.04240
Chen, R. J., Lu, M. Y., Chen, T. Y., Williamson, D. F. K.,
& Mahmood, F. (2021). Synthetic data in machine
learning for medicine and healthcare. Nature
Biomedical Engineering, 5(6), 493–497.
Dahmen, J., & Cook, D. (2019). SynSys: A Synthetic Data
Generation System for Healthcare Applications.
Sensors, 19(5), Article 5. doi.org/10.3390/s19051181
Fioretos, T., Wirta, V., Cavelier, L., Berglund, E.,
Friedman, M., Akhras, M., Botling, J., Ehrencrona, H.,
Engstrand, L., Helenius, G., Fagerqvist, T., Gisselsson,
D., Gruvberger-Saal, S., Gyllensten, U., Heidenblad,
M., Höglund, K., Jacobsson, B., Johansson, M.,
Johansson, Å., … Rosenquist, R. (2022). Implementing
precision medicine in a regionally organized healthcare
system in Sweden. Nature Medicine, 28(10), 1980–
1982.
Frisinger, A., & Papachristou, P. (2023). The voice of
healthcare: Introducing digital decision support systems
into clinical practice - a qualitative study. BMC Primary
Care, 24(1), 67. doi.org/10.1186/s12875-023-02024-6
Gonzales, A., Guruswamy, G., & Smith, S. R. (2023).
Synthetic data in health care: A narrative review. PLOS
Digital Health, 2(1), e0000082.
doi.org/10.1371/journal.pdig.0000082
Hertzum, M., Ellingsen, G., & Cajander, Å. (2022).
Implementing Large-Scale Electronic Health Records:
Experiences from implementations of Epic in Denmark
and Finland. International Journal of Medical
DEMS 2025 - Special Session on Design and Evaluation of Monitoring Systems
1134

Informatics, 167, 104868.
doi.org/10.1016/j.ijmedinf.2022.104868
Jalo, H., Borg, A., Thoreström, E., Larsson, N., Lorentzon,
M., Tryggvasson, O., Johansson, V., Redfors, P.,
Sjöqvist, B. A., & Candefjord, S. (2023). Early
Characterization of Stroke Using Video Analysis and
Machine Learning. Emerging Technologies in
Healthcare and Medicine, 116(116).
doi.org/10.54941/ahfe1004359
Jalo, H., Seth, M., Pikkarainen, M., Häggström, I., Jood, K.,
Bakidou, A., Sjöqvist, B. A., & Candefjord, S. (2023).
Early identification and characterisation of stroke to
support prehospital decision-making using artificial
intelligence: A scoping review protocol. BMJ Open,
13(5), e069660. doi.org/10.1136/bmjopen-2022-
069660
Kokosi, T., & Harron, K. (2022). Synthetic data in medical
research. BMJ Medicine, 1(1), e000167.
doi.org/10.1136/bmjmed-2022-000167
Leckenby, E., Dawoud, D., Bouvy, J., & Jónsson, P. (2021).
The Sandbox Approach and its Potential for Use in
Health Technology Assessment: A Literature Review.
Applied Health Economics and Health Policy, 19(6),
857–869.
Lee, E., Sjöqvist, B. A., Andersson Hagiwara, M., Maurin
Söderholm, H., & Candefjord, S. (2023). Development
of Verified Innovation Process for Healthcare Solutions
(VIPHS): A Stepwise Model for Digital Health. Studies
in Health Technology and Informatics.
doi.org/10.3233/SHTI230250
Lydahl, D. (2024). Good care and adverse effects:
Exploring the use of social alarms in care for older
people in Sweden. Health, 28(4), 559–577.
Maurin Söderholm, H. (2023, March). TEAPaN 1 SoSSUM
- Traffic Event Assessment, Prioritizing and
Notification. https://www.vinnova.se/en/p/teapan-1-
sossum---traffic-event-assessment-prioritizing-and-
notification-steg1-simulations-and-demonstrators/
Maurin Söderholm, H., Andersson, H., Andersson
Hagiwara, M., Backlund, P., Bergman, J., Lundberg, L.,
& Sjöqvist, B. A. (2019). Research challenges in
prehospital care: The need for a simulation-based
prehospital research laboratory. Advances in
Simulation, 4(1), 3. doi.org/10.1186/s41077-019-0090-
0
Moniz, L., Buczak, A. L., Hung, L., Babin, S., Dorko, M.,
& Lombardo, J. (2009). Construction and Validation of
Synthetic Electronic Medical Records. Online Journal
of Public Health Informatics, 1(1).
doi.org/10.5210/ojphi.v1i1.2720
Ollila, S., Ström, E., Khatiri, R., Svensson, T., &
Westerberg, J. (2024). Tidig karaktärisering av stroke
genom videoanalys, maskininlärning och
ögonspårning.
http://hdl.handle.net/20.500.12380/308310
Pezoulas, V. C., Zaridis, D. I., Mylona, E., Androutsos, C.,
Apostolidis, K., Tachos, N. S., & Fotiadis, D. I. (2024).
Synthetic data generation methods in healthcare: A
review on open-source tools and methods.
Computational and Structural Biotechnology Journal,
23, 2892–2910.
Ribiere, V. M., & Tuggle, F. D. (Doug). (2010). Fostering
innovation with KM 2.0. VINE, 40(1), 90–101.
Seth, M., Jalo, H., Lee, E., Bakidou, A., Medin, O., Björner,
U., Sjöqvist, B. A., & Candefjord, S. (2024). Reviewing
Challenges in Specifying Interoperability Requirement
in Procurement of Health Information Systems. Studies
in Health Technology and Informatics.
doi.org/10.3233/SHTI230917
Stadin, M., Nordin, M., Fransson, E. I., & Broström, A.
(2020). Healthcare managers’ experiences of
technostress and the actions they take to handle it – a
critical incident analysis. BMC Medical Informatics
and Decision Making, 20(1), 244.
doi.org/10.1186/s12911-020-01261-4
Tsao, S.-F., Sharma, K., Noor, H., Forster, A., & Chen, H.
(2023). Health Synthetic Data to Enable Health
Learning System and Innovation: A Scoping Review.
Studies in Health Technology and Informatics.
doi.org/10.3233/SHTI230063
Vallevik, V. B., Babic, A., Marshall, S. E., Elvatun, S.,
Brøgger, H. M. B., Alagaratnam, S., Edwin, B.,
Veeraragavan, N. R., Befring, A. K., & Nygård, J. F.
(2024). Can I trust my fake data—A comprehensive
quality assessment framework for synthetic tabular data
in healthcare. International Journal of Medical
Informatics, 185, 105413.
doi.org/10.1016/j.ijmedinf.2024.105413
Walonoski, J., Kramer, M., Nichols, J., Quina, A., Moesel,
C., Hall, D., Duffett, C., Dube, K., Gallagher, T., &
McLachlan, S. (2018). Synthea: An approach, method,
and software mechanism for generating synthetic
patients and the synthetic electronic health care record.
Journal of the American Medical Informatics
Association, 25(3), 230–238.
Introducing Virtuality - Virtual Care Process Simulator: A Concept Utilizing Synthetic Data and a Digital Health Sandbox for Care Process
Simulations
1135
