
Implementing Healthcare Innovation via ISO Standards: An
Exploratory Literature Overview
Carlotta D’Alessandro
1a
, Antonio Licastro
1b
, Alberto Bongiorno
1c
,
Katarzyna Szopik-Depczyńska
2d
and Giuseppe Ioppolo
1e
1
Department of Economics, University of Messina, Via del Verdi, Messina, Sicily, Italy
2
Department of Corporate Management, Institute of Management, University of Szczecin, Poland
Keywords: Healthcare, ISO, Drivers, Barriers, Digital Technologies.
Abstract: The healthcare sector faces increasing pressure to improve quality while reducing its environmental impact.
This study presents an exploratory semi-systematic literature review investigating the implementation of the
most important ISO standards (9001, 14001, 45001, 26000, and 50001) in healthcare organizations, focusing
on implementation of drivers, barriers, and the role of digital technologies. Through analysis of peer-reviewed
articles from Web of Science published between 2010 and 2024, the study aimed to examine driving forces
and barriers affecting ISO implementation in healthcare settings, while also investigating the potential role of
digital technologies in addressing implementation obstacles. While ISO 9001 dominates implementations,
driven by desires for process optimization and improved patient care, significant barriers persist, including
lack of commitment, financial constraints, and administrative burdens. Despite limited explicit discussion of
technological solutions in the literature, digital technologies could facilitate ISO implementation, particularly
through integration with healthcare-specific ISO standards. However, technology adoption might exacerbate
existing challenges related to training and organizational commitment. Understanding the implementation
dynamics provides healthcare organizations with insights for decision-making regarding ISO adoption.
Furthermore, the findings can support policymakers in developing targeted initiatives for smoother ISO
standard implementation across the healthcare sector, laying the groundwork for future research in this
important area.
1 INTRODUCTION
The healthcare industry stands as a fundamental pillar
of societal well-being and economic development,
representing one of the largest service sectors in
OECD countries with projections indicating
continued growth in the coming decades (Weisz et al.,
2020).
Nonetheless, its growth might contribute to
climate change (Weisz et al., 2020). Indeed, the
global healthcare sector's annual greenhouse gas
emissions are comparable to those of 514 coal-fired
power plants (Mominkhan et al., 2023). In OECD
a
https://orcid.org/0000-0002-7361-4201
b
https://orcid.org/0000-0002-4735-6237
c
https://orcid.org/0009-0003-1997-5967
d
https://orcid.org/0000-0002-3054-0660
e
https://orcid.org/0000-0003-0262-8435
countries, the healthcare sectors account for 5% of
national carbon dioxide emissions (Mominkhan et al.,
2023). Furthermore, the healthcare sector's
contribution to pollution, in turn, has negative
consequences for public health (Eckelman et al.,
2018).
In response to these challenges, many healthcare
organizations have turned to standardized
management systems. Indeed, various standards for
healthcare operations have been established by the
International Organization for Standardization (ISO).
Implementing ISO standards has been linked to
positive outcomes in healthcare, including greater
224
D’Alessandro, C., Licastro, A., Bongiorno, A., Szopik-Depczy
´
nska, K. and Ioppolo, G.
Implementing Healthcare Innovation via ISO Standards: An Exploratory Literature Overview.
DOI: 10.5220/0013428000003956
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 7th International Conference on Finance, Economics, Management and IT Business (FEMIB 2025), pages 224-231
ISBN: 978-989-758-748-1; ISSN: 2184-5891
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.

patient satisfaction and safety and enhanced
profitability since they provide a robust framework
for process management and continuous
improvement (Villa-Gallón et al., 2024).
A recent study conducted by Creixans-Tenas et al.
(2019) identified the ISO standards with the most
significant implications for healthcare, which are:
ISO 9001 (Quality Management System, ISO 14001
(Environmental Management System, ISO 45001
(Occupational health and safety management
systems), ISO 50001 (Energy Management System),
and ISO 26000 (Guidance on Social Responsibility),
(ISO 2010; ISO 2015a; ISO 2015b; ISO 2018a; ISO
2018b). Indeed, potential benefits of ISO
implementation are well known, as demonstrated in
literature. For instance, quality following ISO 9001
adoption, educational institutions realized sustained
improvements in service (Arribas Díaz et al., 2018).
Integrated ISO systems can lead to operational
efficiency in the manufacturing sector (Fahmi et al.,
2021), as well as improved operational processes and
customer relations in the food industry (Agus et al.,
2020). Furthermore, simultaneous implementation
of ISO 45001 and ISO 14001 can reduce
administrative overhead and lead to more robust
management systems (Pauliková et al., 2022).
Nevertheless, obstacles to ISO implementation
remain significant in healthcare organizations. Such
is the case of constraints on resources, high costs
related to certification, or opposition within
organizations, (Carrillo-Labella et al., 2020; Mitchell
& Fakhruddin, 2022). Such challenges largely depend
on the heterogeneity of organizational types, sizes
and missions, creating various degrees of needs and
capabilities for implementing ISO standards.
A possible solution to address such issues might
lie in digital technologies. For instance, Artificial
intelligence (AI) or Machine Learning (ML) can
transform healthcare, leading to a future with
increased personalization, precision, predictive
capabilities, and portability (Channapatna 2023).
Previous reviews have focused on specific
aspects: Rakhmawati et al.'s (2014) comprehensive
review of ISO 9001 in healthcare revealed that while
quality management standards are widely adopted,
there is no clear evidence of their effectiveness in
driving broader sustainability outcomes. Similarly,
Sherman et al.'s (2020) systematic review identified a
critical need for standardized approaches to measure
and improve environmental performance in
healthcare, but did not explore how existing ISO
frameworks could fulfil this need.
Indeed, an overview focusing specifically on
healthcare remains unexplored. In addition, an
exploration of how technologies might foster ISO
implantation is also needed. Considering this, the aim
of this exploratory review is to provide an overview
of the primary factors leading to ISO implementation
or hindering as well as exploring which digital
technologies can overcome implementation issues.
Hence, this research aims to address the following
questions:
• What are the primary factors promoting and
hindering the adoption of the most relevant ISO
standards (14001, 45001, 9001, 26000, and
50001) in healthcare institutions?
• What technologies can healthcare organizations
employ to effectively overcome ISO
implementation barriers?
Understanding these implementation dynamics is
important for developing effective strategies that
promote widespread ISO adoption in the healthcare
sector, thus overcoming its environmental challenges.
The subsequent sections of this paper are
structured as follows: first, the Methodology section
details the systematic approach used for literature
selection
and
analysis;
second,
the
Results
and
Discussion section presents and discuss the key
findings, followed by conclusive remarks.
2 METHODOLOGY
To answer the abovementioned research questions
this study adopted an exploratory semi- systematic
literature review. A semi-systematic review merges
the exhaustive nature of systematic reviews with the
interpretative adaptability of narrative ones (Snyder,
2019). To ensure methodological soundness and
clarity, the researchers strictly adhered to the
Preferred Reporting Items for Systematic Reviews
and Meta-Analyses (PRISMA) guidelines (Page et
al., 2021).
The research focused exclusively on Web of
Science as the primary academic database. Keywords
selection encompassed the most relevant ISO
standards according to Creixans-Tenas et al. (2019).
Hence, the study concentrated on five specific ISO
standards: ISO 9001, ISO 45001, ISO 14001, ISO
26000, and ISO 50001, all contextualized within the
healthcare domain.
Only English peer-reviewed articles and reviews
published in academic journals were considered,
aligning with recommendations from scholarly
research that emphasize the superior utility of such
publications (Ceulemans et al., 2015; Saunders et al.,
2009). To ensure contemporaneity and relevance, the
temporal boundary was defined from 2010 to 2024,
Implementing Healthcare Innovation via ISO Standards: An Exploratory Literature Overview
225
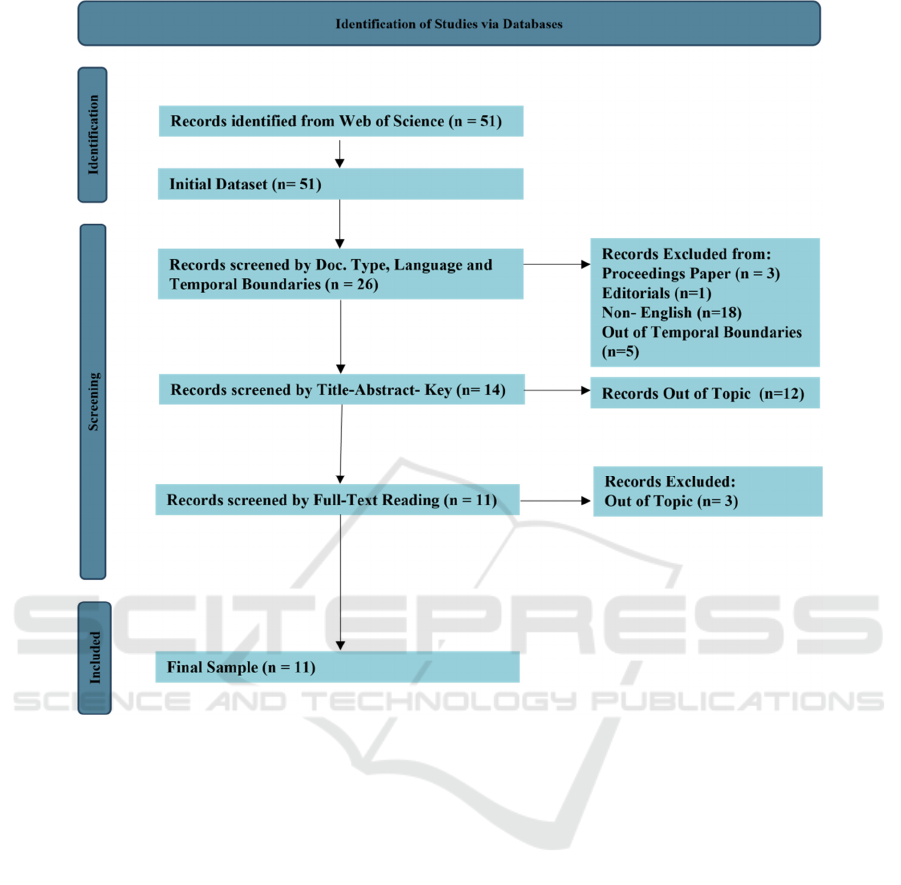
Figure 1: PRISMA Flowchart.
coinciding with the issuance of ISO 26000 in 2010.
Studies were selected if there are explicit mentions of
challenges, barriers, drivers, or benefits related to ISO
standards in healthcare contexts.
An initial search generated 51 potential studies,
which were subsequently refined through progressive
filtering. Document type, language constraints and
temporal filter further narrowed the selection to 26
articles. Examination of titles and abstracts
culminated in 14 studies, with a final selection of 11
articles after full text reading. The selection process
is illustrated in figure 1.
3 RESULTS AND DISCUSSION
Among the 11 articles analyzed, the overwhelming
majority (9 out of 11) mentioned ISO 9001:2015 as the
most important standard to be implemented in
healthcare. This dominance of ISO 9001 reflects a
traditional focus on quality management in healthcare
organizations, driven by patient safety concerns and
regulatory requirements. While such focus
demonstrates a clear understanding of its immediate
benefits for patient care, it also suggests that
healthcare organizations may need guidance in
recognizing the value of other ISO standards that
could complement their quality management efforts.
Indeed, this inadvertently overshadows other crucial
aspects of healthcare operations that could benefit
from standardization.
The complete absence of ISO 26000:2010
implementation studies in the sample is particularly
noteworthy, implying an important gap between
healthcare organizations' social responsibilities and
their management practices. Healthcare organizations
bear significant social responsibility towards both
patients and employees, and ISO implementation
could help achieve sustainable development
objectives (ISO 2010). This gap is especially
concerning given healthcare's central role in
FEMIB 2025 - 7th International Conference on Finance, Economics, Management and IT Business
226

community wellbeing and social equity. The lack of
ISO 26000 adoption might indicate either limited
awareness of the standard's potential benefits or
challenges in translating social responsibility
principles into concrete healthcare practices. Indeed,
current approaches to promoting ISO standards in
healthcare appear be too narrowly focused on
operational aspects while overlooking broader
societal impacts.
The limited exploration of ISO 14001:2015 and
ISO 50001:2018 in the literature (found in only 3
articles) suggests that environmental and energy
management remain secondary priorities in healthcare
organizations' standardization efforts. This finding is
particularly relevant given the healthcare sector's
significant environmental footprint. Organizations
might benefit from an integrated implementation
framework that demonstrates how environmental and
energy management standards can support and
enhance quality management objectives, rather than
competing with them for resources and attention. Dion
et al. (2023) demonstrated that adopting ISO
50001:2018 guidelines can lead to better energy
efficiency in hospitals, providing concrete evidence of
potential benefits. However, the limited adoption of
these standards might indicate a disconnect between
healthcare organizations' environmental impact
awareness and their willingness to implement
systematic solutions. Seifert's (2018) findings
regarding barriers to ISO 14001:2015 implementation
- particularly lack of commitment and awareness -
point to deeper organizational challenges. These
barriers might reflect broader institutional resistance
to environmental initiatives in healthcare settings,
where immediate patient care concerns often
overshadow longer-term sustainability goals. This
suggests a need for better integration of environmental
management with core healthcare operations.
The heavy focus on quality management with
limited attention to environmental, energy, and social
responsibility standards, raises questions about the
healthcare sector's readiness to address its broader
societal impacts. This imbalance might need to be
addressed through policy interventions, enhanced
awareness programs, or revised implementation
frameworks that better integrate different ISO
standards.
3.1 Barriers and Drivers
Nearly half of the analyzed articles signaled lack of
commitment, awareness and knowledge of either the
top management or employees, as the predominant
form of barrier to ISO implementation. Indeed,
efficient fulfilment of standards can be realized only
with a strong level of commitment (López-Púa et al.,
2023). The fact that this barrier persists across different
types of institutions suggests potential systemic issues
in how ISO standards are introduced and promoted
within healthcare organizations. This could indicate a
need for more sector-specific implementation
approaches that account for healthcare's unique
organizational dynamics.
ISO implementation can also become very
financially demanding (Dion et al., 2023; López-Púa
et al., 2023). Financial demands come in the form of
certification fees, training the employees and
logistics. Securing funds in the context of public
hospitals, for the purpose of financing certifications,
can be problematic (Veronese et al. 2020). This is
particularly significant for public healthcare
institutions, where the competing demands of
immediate patient care needs and long-term quality
improvements create complex resource allocation
challenges. The variation in financial challenges
between public and private institutions suggests a
need for differentiated support mechanisms and
implementation strategies.
The numerous administrative tasks required for
obtaining certification may also impede ISO
implementation (Franchina et al., 2023; López-Púa et
al., 2023).
As mentioned at the beginning, the diverse nature
of healthcare organizations can create obstacles in
implementing ISO standards. Indeed, Different
organizations may have distinct experiences
(López-Púa et al., 2023; Nurcahyo et al., 2020) and
may implement ISO standards in their own unique
ways (López-Púa et al., 2023). While this diversity
complicates standardization efforts, it may also shed
light onto how ISO standards can be adapted to
different healthcare contexts. The organizational
changes triggered by ISO implementation suggest
that these standards act not just as management tools
but as catalysts for broader institutional
transformation (Johannesen & Wiig, 2020).
Additional hurdles in ISO implementation include
insufficient training (Silva et al., 2017; Seifert 2018;
Franchina et al., 2023) and limited understanding
among stakeholders about green operations and
comparative energy costs, especially in relation to
energy management systems (Dion et al., 2023).
Moreover, the ability to access various IT
systems has been recognized as an impediment to
implementing ISO 9001:2015 (Avruscio et al., 2022).
Institutions are primarily motivated by the
potential for internal management enhancement and
process optimization (Avruscio et al., 2022; Corsi et
Implementing Healthcare Innovation via ISO Standards: An Exploratory Literature Overview
227

al., 2020). This manifests through the establishment
of better-quality processes, systematic internal audits,
and robust risk management approaches (Franchina et
al., 2023).
The drive for continuous improvement emerges as
a recurring theme across multiple studies (Franchina
et al., 2023; López-Púa et al., 2023; Silva et al., 2017),
suggesting its fundamental role in ISO adoption.
From a patient-centric perspective, healthcare
organizations are motivated by the potential to
enhance patient satisfaction (Dion et al., 2023;
López-Púa et al., 2023) and improve patient safety
through better diagnosis processes and measurement
quality (Farfán-Vargas et al., 2024; Huf et al., 2024).
The economic dimension also plays a significant role,
with institutions seeking cost efficiency and
improved staff productivity (Dion et al., 2023).
External factors, such as governmental requirements,
can also serve as catalysts for ISO implementation
(Nurcahyo et al., 2019).
Furthermore, the standards' implementation is
viewed as a strategic tool for enhancing
competitiveness (Farfán-Vargas et al., 2024) and
promoting sustainability in healthcare systems (Silva
et al., 2017).
3.2 Digital
Innovations
and
ISO
Standards in Healthcare
Despite the potential of digital technologies to
facilitate ISO implementation in healthcare, this
review reveals limited explicit discussion of
technological solutions in the current literature.
However, some studies highlight both existing
applications and future needs. The implemented
technologies range from basic digitalization and
automation processes to more sophisticated IT
systems (Huf et al., 2024). Telemedicine emerges as
a notable technological application in healthcare
settings pursuing ISO compliance (Farfán-Vargas et
al., 2024), representing an interesting convergence of
quality management and digital innovation. This
intersection suggests that digital technologies might
serve dual purposes: facilitating ISO compliance
while simultaneously modernizing healthcare
delivery. However, the limited explicit discussion of
technological solutions in the literature points to a
potential disconnect between quality management
practices and digital transformation initiatives in
healthcare organizations.
The need for digital tools and innovative
solutions to support ISO implementation is explicitly
recognized (Dion et al., 2023; Franchina et al., 2023),
suggesting an important opportunity for integration
with existing healthcare-specific ISO standards for
digital technologies. For instance, while healthcare
organizations are increasingly adopting digital
medical technologies to enhance accessibility and
flexibility (Senbekov et al., 2020), standards like ISO
13131 for telehealth services could complement
quality management systems by ensuring patient
safety in digital environments (ISO 2021; Meijer &
Taylor, 2022). Similarly, as healthcare organizations
implement sustainability-focused technologies such
as real-time consumption monitoring software and
renewable energy systems (Dion et al., 2023), they
could benefit from integrating these with existing
digital health standards. The healthcare sector's
digital transformation, encompassing Internet of
Medical Things (IoMT), telemedicine systems, and
electronic health records (EHRs) (Rahim et al., 2024),
suggests that a more integrated approach to ISO
implementation could be beneficial. This could
include combining traditional management system
standards with healthcare-specific digital standards
like ISO 11073 for remote patient monitoring (ISO
2008) and ISO 27799 for healthcare information
security (ISO 2016). Such integration could create
synergies that address both operational efficiency and
digital innovation needs while ensuring compliance
with quality, environmental, and safety requirements.
This gap between the recognized need for
technological innovation and actual implementation
suggests an important area for future research and
development. The limited discussion of digital
technologies in the reviewed literature, coupled with
explicit calls for more innovative tools, indicates an
emerging awareness of technology's potential role in
facilitating ISO implementation, even though concrete
applications remain underexplored.
4 CONCLUSIONS
This exploratory review has provided an overview of
the implementation dynamics of ISO standards in
healthcare organizations, addressing the drivers,
barriers, and potential role of digital technologies.
The dominance of ISO 9001:2015 demonstrates
healthcare organizations' commitment to quality
management yet also reveals potential gaps in
addressing other critical areas. The notable absence
of ISO 26000 implementation studies and limited
adoption of environmental standards suggests
healthcare organizations may be overlooking
opportunities to address their broader societal and
environmental impacts. This imbalance requires
attention from both healthcare leaders, policymakers
FEMIB 2025 - 7th International Conference on Finance, Economics, Management and IT Business
228

as well as researchers to ensure a more
comprehensive approach to standardization.
The prevalence of organizational resistance and
lack of commitment indicates a need for more
effective change management strategies specifically
tailored to healthcare settings. Financial constraints,
particularly evident in public healthcare institutions,
necessitate innovative funding mechanisms and
policy support. Administrative burdens could be
mitigated through better integration of management
systems and strategic use of digital technologies.
The relationship between digital technologies and
ISO implementation emerges as a critical area for
development. While technology shows promise in
addressing certain implementation barriers,
particularly administrative challenges, its successful
integration requires careful consideration of
organizational readiness and capacity. It is important
to note, in fact, that technological solutions might
exacerbate certain challenges, such as the existing
issues with lack of training and commitment, if not
properly managed.
Healthcare organizations must develop
comprehensive strategies that align digital
transformation initiatives with ISO implementation
efforts. Healthcare administrators should consider
developing integrated approaches that balance quality
management with other ISO standards, while
policymakers could work to develop targeted support
mechanisms for public healthcare institutions.
Technology providers might focus on creating
healthcare-specific solutions that address ISO
implementation challenges while minimizing
additional training requirements.
Future research should examine successful ISO
implementation strategies in different healthcare
contexts, analyze the experiences of public versus
private healthcare institutions, and investigate the
barriers to implementing environmental and social
responsibility standards. Empirical studies examining
how digital technologies specifically address ISO
implementation barriers in healthcare settings are
needed. Additionally, scholars should assess the long-
term impacts of integrated ISO systems on healthcare
outcomes and evaluate digital technology's role in
facilitating ISO implementation. Finally, healthcare
administrators and policymakers could benefit from
investigating how digital transformation might
influence organizational commitment and training
requirements in the context of ISO implementation.
Understanding of ISO implementation dynamics,
coupled with strategic technological integration and
targeted policy support, will be crucial for healthcare
organizations to successfully balance quality
improvement, environmental responsibility, and social
impact while maintaining operational efficiency in an
increasingly complex healthcare landscape.
ACKNOWLEDGEMENTS
Co-financed by the Minister of Science under the
"Regional Excellence Initiative" Program.
REFERENCES
Agus, P., Ratna Setyowati, P., Arman, H. A., Masduki, A.,
Innocentius, B., Priyono Budi, S., & Otta Breman, S.
(2020). The effect of implementation integrated
management system ISO 9001, ISO 14001, ISO 22000
and ISO 45001 on Indonesian food industries
performance. Test Engineering and Management,
82(20), 14054-14069.
Arribas Díaz, J. A., & Martínez-Mediano, C. (2018). The
impact of ISO quality management systems on primary
and secondary schools in Spain. Quality Assurance in
Education, 26(1), 2-24.
Ates, S. A., & Durakbasa, N. M. (2012). Evaluation of
corporate energy management practices of energy
intensive industries in Turkey. Energy, 45(1), 81-91.
Avruscio, G., Ragazzo, S., Ceccato, D., Adamo, A., Napoli,
C., Cacco, L., ... & Tussardi, I. T. (2022).
Implementation of a quality management system
according to ISO 9001: 2015 standards in an Angiology
Unit: an Italian experience. Annali di Igiene, Medicina
Preventiva e di Comunità, 34(6).
Carrillo-Labella, R., Fort, F., & Parras-Rosa, M. (2020).
Motives, barriers, and expected benefits of ISO 14001
in the agri-food sector. Sustainability, 12(5), 1724.
Ceulemans, K., Molderez, I., & Van Liedekerke, L. (2015).
Sustainability reporting in higher education: a
comprehensive review of the recent literature and paths
for further research. Journal of Cleaner Production,
106, 127-143.
Channapatna, R. (2023). Role of AI (Artificial Intelligence)
and Machine Learning in Transforming Operations in
Healthcare Industry: An Empirical Study. International
Journal, 10(2), 2069-2076.
Corsi, C. A. C., Shoji, M., Scarpelini, K. C. G., Bento,
R.L., Becari, C., Assunção-Luiz, A. V., ... & Martins,
L. G. G. (2020). Implementation and certification of
ISO 9001: 2015 seal in human tissue bank HCFMRP-
USP. Cell and Tissue Banking, 21, 563-571.
Creixans-Tenas, J., Coenders, G., & Arimany-Serrat, N.
(2019). Corporate social responsibility and financial
profile of Spanish private hospitals. Heliyon, 5(10).
Dion, H., Evans, M., & Farrell, P. (2023). Hospitals
management transformative initiatives; towards energy
efficiency and environmental sustainability in
healthcare facilities. Journal of Engineering, Design
and Technology, 21(2), 552-584.
Implementing Healthcare Innovation via ISO Standards: An Exploratory Literature Overview
229

Eckelman, M. J., Sherman, J. D., & MacNeill, A. J. (2018).
Life cycle environmental emissions and health damages
from the Canadian healthcare system: an economic-
environmental-epidemiological analysis. PLoS
medicine, 15(7), e1002623.
Fahmi, K., Mustofa, A., Rochmad, I., Sulastri, E.,
Wahyuni,I. S., & Irwansyah, I. (2021). Effect of ISO
9001: 2015, ISO 14001: 2015 and ISO 45001: 2018 on
operational performance of automotive industries.
Journal of Industrial Engineering & Management
Research, 2(1), 13-25.
Farfán-Vargas, H. M., Espinoza-Morriberon, D., Moya-
Salazar, M. M., Contreras-Pulache, H., & Moya-
Salazar, J. (2024). Systematic review on the
implementation of metrological assurance systems for
medical devices in Latin America. Frontiers in
Medicine, 11, 1281199.
Franchina, V., Stabile, S., Cenna, R., Mannozzi, F.,
Federici, I., Testoni, S., ... & Cagnazzo, C. (2023). ISO
9001: 2015 standard implementation in clinical trial
centers: An exploratory analysis of benefits and barriers
in Italy. Contemporary Clinical Trials
Communications, 33, 101104
Huf, W., Mohns, M., Almeta, E., Lister, R., Buchta, C.,
Demyanets, S., ... & Ettl, B. (2024). Benchmarking
medical laboratory performance on a global scale.
Frontiers in Public Health, 12, 1363957.
International Organization for Standardization (2008). ISO
11073-90101:2008 Health informatics — Point-of-care
medical device communication. Part 90101: Analytical
instruments — Point-of-care test.
International Organization for Standardization (2010). ISO
26000:2010 Guidance on social responsibility.
International Organization for Standardization (2015b).
ISO 14001:2015 Environmental management systems-
Requirements with guidance for use.
International Organization for Standardization (2016). ISO
27799:2016 Health informatics — Information security
management in health using ISO/IEC 27002.
International Organization for Standardization (2018b).
ISO 50001:2018 Energy management systems-
Requirements with guidance for use.
International Organization for Standardization. (2015a).
ISO 9001:2015 Quality management systems-
Requirements.
International Organization for Standardization. (2018a).
ISO 45001:2018 Occupational health and safety
management systems- Requirements with guidance for
use.
International Organization for Standardization. (2021). ISO
13131:2021 Health informatics — Telehealth services
— Quality planning guidelines.
López-Púa, Y., Navasa, M., Trilla, A., Colmenero, J.,
García, R., López, E., ... & Ríos, J. (2023).
Implementation of a quality management system in a
liver transplant programme. BMJ Open Quality, 12(3),
e002440.
Johannesen, D. T. S., & Wiig, S. (2020). Exploring hospital
certification processes from the certification body’s
perspective-a qualitative study. BMC Health Services
Research, 20, 1-12.
Massoud, M. A., Fayad, R., Kamleh, R., & El-Fadel, M.
(2010). Environmental management system (ISO
14001) certification in developing countries: challenges
and implementation strategies.
Meijer, W., & Taylor, A. (2022). ISO/IEC-Standards on
Quality and Safety of Telehealth Services and Mobile
Medical Apps. In MEDINFO 2021: One World, One
Health–Global Partnership for Digital Innovation (pp.
508-511). IOS Press.
Mitchell, C., & Fakhruddin, B. (2022). An Analysis of
Barriers to the Implementation of an ISO Certified
Quality Management System for National
Meteorological and Hydrological Services in the
Anglophone Caribbean. Meteorological Applications,
29(4), e2086.
Mominkhan, D., Alamri, F. A., Balharith, M., Alharbi, M.,
Alshebli, A., Alshareef, S. Y., ... & Alabdulaali, M. K.
(2023). The current state and potential evolution of
carbon emissions in the healthcare sector: a narrative
review article. Frontiers in Sustainable Energy Policy,
2, 1230253.
Nurcahyo, R., Kristiningrum, E., & Sumaedi, S. (2020).
ISO 9001-certified public healthcare center’s efficiency
and re-certification. International Journal of
Productivity and Performance Management, 69(4),
794-812.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I.,
Hoffmann, T. C., Mulrow, C. D., ... & Moher, D.
(2021). The PRISMA 2020 statement: an updated
guideline for reporting systematic reviews. bmj, 372.
Pauliková, A., Chovancová, J., & Blahová, J. (2022).
Cluster modeling of environmental and occupational
health and safety management systems for integration
support. International journal of environmental
research and public health, 19(11), 6588.
Rahim, M. J., Rahim, M. I. I., Afroz, A., & Akinola, O.
(2024). Cybersecurity Threats in Healthcare IT:
Challenges, Risks, and Mitigation Strategies. Journal of
Artificial Intelligence General Science (JAIGS) ISSN:
3006-4023, 6(1), 438-462.
Rakhmawati, T., Sumaedi, S., & Judhi Astrini, N. (2014).
ISO 9001 in health service sector: a review and future
research proposal. International Journal of Quality and
Service Sciences, 6(1), 17-29.
Senbekov, M., Saliev, T., Bukeyeva, Z., Almabayeva, A.,
Zhanaliyeva, M., Aitenova, N., ... & Fakhradiyev, I.
(2020). The recent progress and applications of digital
technologies in healthcare: a review. International
journal of telemedicine and applications, 2020(1),
8830200.
Saunders, M. (2009). Research methods for business
students. Person Education Limited.
Seifert, C. (2018). The barriers for voluntary environmental
management systems—The case of EMAS in hospitals.
Sustainability, 10(5), 1420.
Sherman, J. D., Thiel, C., MacNeill, A., Eckelman, M. J.,
Dubrow, R., Hopf, H., ... & Bilec, M. M. (2020). The
green print: advancement of environmental
FEMIB 2025 - 7th International Conference on Finance, Economics, Management and IT Business
230

sustainability in healthcare. Resources, Conservation
and Recycling, 161, 104882.
Silva, S. D., & Fonseca, A. (2017). Portuguese primary
healthcare–sustainability through quality management.
International Journal of Quality & Reliability
Management, 34(2), 251-264.
Snyder, H. (2019). Literature review as a research
methodology: An overview and guidelines. Journal of
business research, 104, 333-339.
Villa-Gallón, J. E., Valencia-Bernal, J. A., & Garcés-
Gómez, Y. A. (2024). ISO Standards in Healthcare
Organizations: Research Evolution and Trends from a
Bibliometric Analysis. Publications, 12(3), 27.
Weisz, U., Pichler, P. P., Jaccard, I. S., Haas, W., Matej, S.,
Bachner, F., ... & Weisz, H. (2020). Carbon emission
trends and sustainability options in Austrian health
care. Resources, Conservation and Recycling, 160,
104862.
Implementing Healthcare Innovation via ISO Standards: An Exploratory Literature Overview
231
