
Ontology-Based Framework for Personalized Home-Based
Rehabilitation in Cerebral Palsy Care
Rahma Haouas Zahwanie
1
, Lilia Cheniti-Belcadhi
1
and Saoussen Layouni
2
1
Sousse University, ISITC, PRINCE Research Laboratory, H-Sousse, Tunisia
2
Physical Medicine and Rehabilitation Department, University of Sousse, Medical Faculty, Sousse, Tunisia
Keywords:
Cerebral Pasly, Rehabilitation, Ontology, Intelligent Framework, Home-Based Exercise Programs.
Abstract:
In the domain of cerebral palsy rehabilitation, advances in machine learning and semantic technologies of-
fer promising solutions to enhance treatment strategies. This paper focuses on developing an ontology-based
framework to support rehabilitation programs for children with cerebral palsy, addressing the need for person-
alized, home-based exercise programs (HEP). These programs aim to improve recovery by enabling patients
to engage in tailored exercises outside clinical settings. However, the effectiveness of HEP depends on ac-
curate monitoring and feedback, as improper execution of exercises can hinder progress. To address this
challenge, we propose an intelligent system framework that integrates ontology-driven knowledge representa-
tion to oversee rehabilitation programs. The system analyzes patient profiles and progress data, recommending
a personalized rehabilitation plan consisting of targeted exercises supported by healthcare professionals. The
ontology serves as the backbone of this framework, enabling semantic representation of rehabilitation con-
cepts and facilitating the management and improvement of cerebral palsy treatment pathways. Furthermore,
this approach enhances patient outcomes by providing structured, context-aware rehabilitation plans while
promoting interoperability and knowledge sharing across healthcare systems. By embedding the ontology
within the framework, we enable greater reusability, semantic comprehension, and adaptability to multilin-
gual healthcare environments. This work highlights the critical role of ontologies in advancing rehabilitation
strategies for cerebral palsy and improving access to high-quality, personalized care.
1 INTRODUCTION
Physical therapy is for enhancing the functional abili-
ties of individuals with disabilities or physical impair-
ments. Research emphasizes its role in improving pa-
tient outcomes, showing a strong correlation between
exercise levels and the success of rehabilitation pro-
grams. Rehabilitation therapy is particularly bene-
ficial for patients after hospital discharge following
an acute stroke or cerebral palsy (O’Neill and For-
man, 2020). However, factors such as limited ac-
cess to appropriate healthcare providers, higher costs
that reduce the amount of care provided, and poor
patient attendance limit the benefits of rehabilitation
therapy. Furthermore, even when patients do benefit
from rehabilitation therapy, it is often provided inter-
mittently, with prolonged intervals between sessions,
which limits the effectiveness of the treatment com-
pared with the recommendations of high-quality clin-
ical studies.
Home-based programs are generally recom-
mended as part of rehabilitation programs to offer
greater flexibility, while healthcare professionals cre-
ate individualised rehabilitation plans with exercise
suggestions. Significantly, more than 90% of rehabil-
itation programs are carried out at home, demonstrat-
ing the widespread adoption of this technique. (Ko-
matireddy et al., 2014). Studies (Chen et al., 2014)
(Ibeneme et al., 2024) (Ge et al., 2024) have shown
that home exercise can be effective in improving vari-
ous aspects of motor function and quality of life in pa-
tients with cerebral palsy. These studies have shown
that home exercise programs, including tele-assisted
robotic rehabilitation, computer-assisted upper limb
exercises, and individualised interactive training, can
lead to significant improvements in ankle range of
motion, muscle strength, balance, self-reported func-
tion, quality of movement, daily activities, and upper
and lower limb function.
A range of intelligent technologies, particularly
those using machine learning, are increasingly be-
ing integrated into patient rehabilitation. Numerous
Zahwanie, R. H., Cheniti-Belcadhi, L. and Layouni, S.
Ontology-Based Framework for Personalized Home-Based Rehabilitation in Cerebral Palsy Care.
DOI: 10.5220/0013472700003932
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Conference on Computer Supported Education (CSEDU 2025) - Volume 1, pages 705-716
ISBN: 978-989-758-746-7; ISSN: 2184-5026
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
705

studies highlight the potential of these technologies
in stroke rehabilitation and home care, respectively.
In (Mennella et al., 2023b) the author highlights the
role of artificial intelligence in remote monitoring and
intelligent assistance, particularly in activity recog-
nition and clinical status prediction. This research
(Fong et al., 2020) extends this discussion to the use
of intelligent robotics and machine learning in func-
tional capacity assessment and rehabilitation, partic-
ularly in the simulation of tasks in a suitable en-
vironment. These studies collectively highlight the
potential of intelligent technologies to improve the
efficiency and accessibility of patient rehabilitation.
Technological advances are revolutionising the reha-
bilitation of people with cerebral palsy. Robotics,
virtual reality, mobile applications, wearable sensors,
and non-invasive brain stimulation all hold promise
for improving movement, providing feedback, and
motivating users (as studies have shown). These ad-
vances can ultimately improve a person’s ability to
carry out daily activities and participate more fully in
life.
Therefore, a coherent conceptual framework and
knowledge representation are highly desirable and
necessary for the selection and recommendation of
appropriate rehabilitation exercises and recovery from
cerebral palsy. Several studies have proposed using
an ontology to represent and model domain knowl-
edge to overcome this problem. Ontology is a power-
ful tool for tackling semantic challenges and harmo-
nizing disparate vocabularies by providing a formal-
ized and structured representation of domain knowl-
edge. This knowledge is encapsulated in a way that
allows for clear definitions of concepts, relationships,
and rules within a particular domain.
In section 1, we review related work, examining
existing research and technological advancements in
the field of cerebral palsy rehabilitation. In section
2, we focus on the architecture of the Ontological
Intelligent Framework for Rehabilitation. This sec-
tion outlines the system’s architecture and core com-
ponents. In section 3, we present a comprehensive
overview of the ontology used in our system, dis-
cussing its structure and the methodology behind its
development. Additionally, we focus on the Seman-
tic Web Rule Language (SWRL) rules applied within
the ontology to enhance its functionality and maintain
semantic coherence. In Section 4, we delve into the
implications of our findings, assess the effectiveness
of the proposed system, and outline potential direc-
tions for future research. Section 5 concludes the arti-
cle with a comprehensive summary of the key insights
and outcomes, highlighting their significance.
2 RELATED WORK
Numerous studies have highlighted the need for rig-
orous monitoring of the development of children with
cerebral palsy throughout their rehabilitation home-
based exercise program. This research underlines the
importance of a personalized approach, adapted to the
specific needs of each child, in order to optimise ther-
apeutic results.
2.1 Intelligent Technologies Used in
Rehabilitation
Artificial intelligence, virtual reality, and wearable
devices enable more personalized and effective reha-
bilitation. Virtual reality immerses patients in simu-
lated environments to relearn movements, while ex-
oskeletons assist those with motor difficulties. Ma-
chine learning analyzes patient data to adapt rehabil-
itation programs in real time, optimizing outcomes.
Ontologies further enhance rehabilitation by structur-
ing and representing knowledge formally. These tech-
nological advances accelerate recovery and improve
the quality of life for individuals with disabilities or
recovering from illness.
The paper (Chu et al., 2022) discusses how smart
rehabilitation clinics are utilizing advanced technolo-
gies to improve patient care. The focus has shifted
towards a holistic approach, prioritizing patient well-
being and active participation for optimal results. The
article examines the defining characteristics of these
clinics, including the integration of digital tools, au-
tomation, big data analysis, and patient monitoring
systems. These technologies have the potential to per-
sonalize and improve rehabilitation experiences. Ul-
timately, the paper presents a promising future for
rehabilitation clinics that embrace cutting-edge tech-
nologies and prioritize patient engagement to improve
overall quality of care and patient well-being.
Authors in (Lopes et al., 2021) emphasize the im-
portance of digital platforms in optimizing health-
care in pandemics like COVID-19. Scientific re-
search is crucial before deploying any digital prod-
ucts in this sector. The researchers also explore AI
in biomedicine, healthcare care, and medical educa-
tion, highlighting its potential for improved diagnos-
tics, personalized treatment plans, and enhanced edu-
cation.
The research (Senbekov et al., 2020) examines a
new rehabilitation system for schizophrenia patients
using virtual reality (VR) and serious games. The sys-
tem focuses on patient engagement and includes three
core modules: data integration, game design, and data
visualization. The research suggests integrating this
EKM 2025 - 8th Special Session on Educational Knowledge Management
706

system with traditional treatments to create a compre-
hensive rehabilitation program in healthcare facilities.
2.2 Rehabilitation-Based Home
Exercises in Healthcare
Chung et al. (Chung et al., 2019) discuss the appli-
cation of IoT in healthcare, with a particular focus on
exercise in cardiac rehabilitation at home. The sys-
tem comprises a wearable device, a smartphone ap-
plication, and a medical station to facilitate patient-
provider interaction, accurate heart rate measurement,
real-time exercise intensity recommendations, and ex-
ercise record tracking. The system has proven to be
effective in maintaining heart rate within prescribed
limits during exercise.
In addition, the main approach proposed in the
study (Triantafyllidis et al., 2018) is the development
of a computerized decision support system (DSS) for
home-based rehabilitation in cardiovascular disease
patients leverages rule-based logic to guide personal-
ized exercise programs. By focusing on heart rate and
movement accuracy, the system helps patients per-
form exercises effectively. Evaluations through simu-
lations and real-life studies demonstrate its efficacy in
maintaining optimal heart rate zones during exercise.
In (Mennella et al., 2023a), the researcher evalu-
ates the use of deep learning-based systems to assess
rehabilitation exercises, focusing on human pose esti-
mation, movement classification, and the detection of
compensatory movements. The systems discussed in
the review show promising results in accurately clas-
sifying exercise movements and providing real-time
feedback to patients during home-based rehabilitation
programs.
Therefore, AI-based systems in rehabilitation of-
fer real-time feedback, correct exercise execution,
detect compensatory movements, and improve out-
comes. Integration enhances patient engagement, en-
ables cost-effective monitoring, and supports HEP. AI
technologies accurately classify movements and de-
tect patterns, improving physical function and qual-
ity of life in various populations. Further, validation
studies in clinical settings are needed to assess their
effectiveness fully.
2.3 Ontology-Driven Rehabilitation
Frameworks
Existing ontologies in rehabilitation, such as the Re-
habilitation Treatment Specification System (RTSS)
(Gibson et al., 2023) and the Ontology for Neurolog-
ical Rehabilitation (NeuRO) (Hier and Brint, 2020),
provide foundational models for rehabilitation pro-
cesses but lack specificity for cerebral palsy (CP) re-
habilitation. RTSS standardizes rehabilitation treat-
ments, including therapeutic exercises and modali-
ties, but does not cover CP-specific interventions like
spasticity management or neurodevelopmental facili-
tation. Similarly, NeuRO focuses on stroke and brain
injury rehabilitation, omitting pediatric CP subtypes
such as dyskinetic CP and adaptations for home-based
exercises. In contrast, our ontology explicitly ad-
dresses these gaps by structuring CP-specific con-
cepts (e.g., Motor Rehabilitation Techniques, Neu-
ropsychological Rehabilitation), integrating home-
based exercise programs (HEP) with severity-driven
rules (e.g., SWRL-based intensity adjustments), and
linking motor assessments to personalized interven-
tions, such as using ankle range-of-motion scores to
trigger targeted exercises.
2.4 Rehabilitation HEP in Cerebral
Palsy
In this section, we provide detailed information on ar-
ticles relating to the type of study, study design, and
intervention concerning HEP for cerebral palsy, de-
tailed in the table 1.
Table 1: HEP for cerebral palsy. F: Feasibility study, E:
Efficacy study, C: Comparative study, RCT: Randomized
controlled trial, N-RCT: Non-Randomized controlled trial.
Authors Study
type
Intervention
(ling Chen
et al., 2014)
E Home-based Constraint-
Induced Therapy
(Racic et al.,
2014)
C Home-based habilitation
programme
(Demeke
et al., 2023)
F Home-based therapy
programs for children
with cerebral palsy
(Lorentzen
et al., 2015)
N-
RCT
Interactive home-based
training delivered
through the internet.
(Beckers
et al., 2017)
F Home-based occu-
pational therapy and
physiotherapy pro-
grammes
(Junior et al.,
2021)
F Home-based physiother-
apy programmes
(Goswami
et al., 2021)
E
(RCT)
Home-centered activity-
based therapy
(Macintosh
et al., 2020)
F Video game
(Ejaz et al.,
2024)
E Home-based intensive
bimanual training
Ontology-Based Framework for Personalized Home-Based Rehabilitation in Cerebral Palsy Care
707
To summarize, home-based rehabilitation treat-
ment programs, including various therapies such as
intelligent training, restraint therapy, and virtual re-
ality therapy, seem to ensure that children with cere-
bral palsy progress in their motor skills, useful abil-
ities, and exercises of daily living. These methods
offer potential rewards in terms of improved access,
cost-effectiveness, and comfort for patients and their
families. In-depth research is needed to optimize the
agreements, evaluate long-term results, and decide on
the most persuasive approaches for specific subsets
of children with cerebral palsy. By leveraging ad-
vanced methodologies stakeholders can refine their
approaches, ensuring that interventions are not only
evidence-based but also highly adaptable to individ-
ual circumstances. This effort will pave the way for
more impactful outcomes in their rehabilitation.
3 ARCHITECTURE OF THE
ONTOLOGICAL INTELLIGENT
FRAMEWORK FOR
REHABILITATION
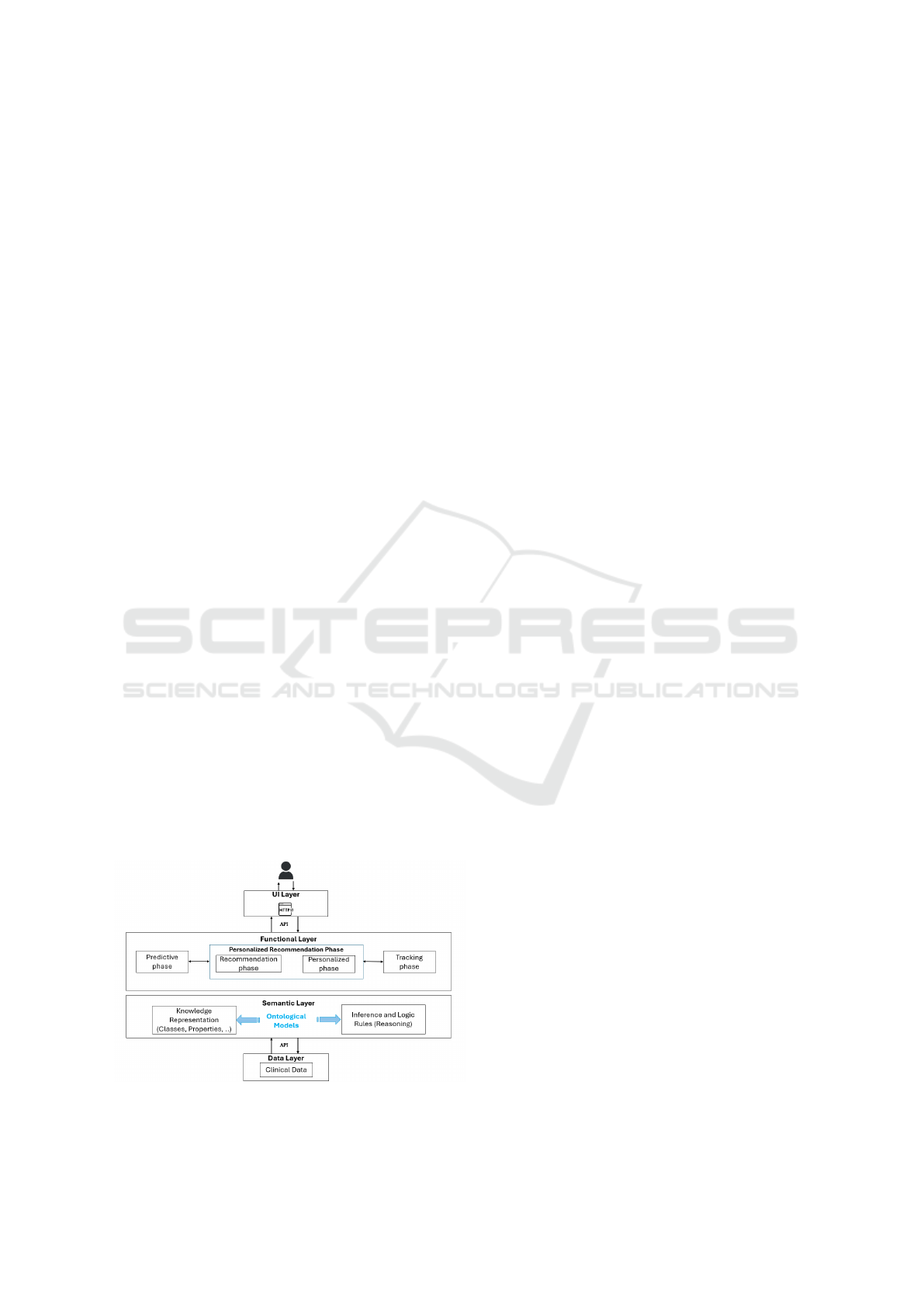
The proposed system architecture for home-based ex-
ercise programs (HEP) follows an interactive frame-
work. The user submits a request through the inter-
face, which is processed by the functional layer via
an API. This layer leverages predictive models and
personalized recommendations, generating a seman-
tically coherent response with support from the se-
mantic layer, which applies ontologies and inference
rules. The data layer supplies necessary information
for reasoning, and the final response is delivered back
to the user, completing the interaction cycle.
Our architecture is composed of 4 layers (user
layer, functional layer, semantic layer, data layer) as
presented in the figure below:
Figure 1: Architecture of HEP framework.
• The user layer (UI Layer) is the point of inter-
action between the user and the system. It takes
the form of various interfaces, such as web or mo-
bile applications. Thanks to this layer, users can
not only formulate queries and consult the corre-
sponding results, but also personalize their expe-
rience by configuring their preferences according
to their specific needs.
• The functional layer manages all the system’s
functionalities, focusing on a personalized user
experience. Using predictive models, it antici-
pates the user’s needs by analysing their histor-
ical data and current context. These predictions
form the basis for personalized recommendations
that are continually refined as a function of the
user’s interactions with the system. In this way,
the functional layer ensures that the user’s prefer-
ences are monitored and analysed over time, mak-
ing it possible to improve the relevance of recom-
mendations over time and create an increasingly
tailored user experience.
• The semantic layer constitutes the cognitive heart
of the system, guaranteeing the coherence and
unified interpretation of information. It houses
a structured representation of the application do-
main’s knowledge, using ontological models to
define a common vocabulary and the relationships
between concepts. These models, combined with
inference and logic rules, enable the system to rea-
son about the data and draw relevant conclusions.
In this context, cerebral palsy rehabilitation, the
semantic layer can establish links between spe-
cific symptoms and probable diseases, facilitating
diagnosis and decision-making.
• The data layer contains a variety of clinical data
such as examination results, treatment history and
general medical information about the patient.
This layer thus provides the raw material essen-
tial for the other layers of the system to carry out
their treatments and generate relevant results.
This architecture offers a number of significant ad-
vantages. It offers a high degree of customisation by
adapting its responses to the specific needs of each
user. Moreover, its flexibility is ensured by the use
of ontologies, making it easy to extend the system to
new domains and integrate new knowledge. In ad-
dition, the reliability of the results is guaranteed by
rigorous inference rules, while the explicability of the
reasoning is reinforced by the transparency of the on-
tological models used, enabling a better understand-
ing of the system’s decision-making processes.
Participation to physical activity therapy by pa-
tients is seen as a crucial element in enhancing their
EKM 2025 - 8th Special Session on Educational Knowledge Management
708

overall health and wellness. It has been discovered
that home-based physical activity therapies, used in
homes or other settings, improve daily assessment
and tutoring and help patients take part in regular
physical exercise. Such interventions become much
more valuable when they may be used conveniently,
anytime, and unsupervised. This helps patients live
independently. As a result, intelligent, individual-
ized, durable, and adaptable computer systems for
exercise-based rehabilitation are needed to meet pa-
tients’ evolving needs and produce the desired health
results.
The goal is to develop a system that provides
patients with protected access to their personal pro-
file, enables them to monitor their progress, and re-
ceives personalized recommendations for HEP. It ex-
plores the application of predictive analytics in fol-
lowing and assessing patients’ rehabilitation progress
in a smart HEP system and develops and evaluates
video recommendation algorithms for HEP in an in-
telligent system. The approach consists of process-
ing patient data, such as medical history, recent exer-
cises, and progressive data, to generate personalized
exercise recommendations: The implementation of
a video recommendation algorithm in the intelligent
HEP for rehabilitation introduces an important new
feature to the system, offering a more interactive and
engaging rehabilitation experience for patients by giv-
ing them tailor-made exercise videos that match their
specific needs and abilities.
4 ONTOLOGICAL DESCRIPTION
FOR REHABILITATION
Ontologies are crucial in rehabilitation medicine, es-
pecially in robotics, patient education, and physio-
therapy (Palagin et al., 2023) (Spoladore et al., 2024).
They provide structured information about rehabil-
itation robots, aid researchers and experts, develop
multi-agent platforms for medical rehabilitation, as-
sist physiotherapists in managing patients’ evolution,
and facilitate a formal model of rehabilitation in-
terventions in computer-based decision support sys-
tems (Abdullah et al., 2022). Ontologies facilitate
the development of multi-agent, semantic technology-
supported rehabilitation interventions. They provide a
foundational framework for home rehabilitation, en-
abling knowledge integration and sharing across do-
mains. By defining relationships between key con-
cepts such as patient status, therapy types, and feed-
back mechanisms, ontologies help create intelligent,
personalized environments that optimize therapy ef-
fectiveness. Moreover, they enhance interoperability
between different rehabilitation systems, ensuring a
seamless and coherent experience. Ontologies also
reduce experts’ workload by simplifying the develop-
ment of rehabilitation practices, which is essential for
maintaining patient engagement and improving out-
comes. Ultimately, they play a crucial role in sup-
porting a more effective and personalized approach to
home rehabilitation.
The purpose of this work is to provide a frame-
work for the ontology-based cerebral palsy rehabili-
tation system. Open Biomedical Ontologies (OBO)
Foundry, one of the most popular and detailed ap-
proaches for ontology construction, serves as the
foundation for the methodological approach used to
create, execute, and portray the ontology in this study
(Karray et al., 2021). The OBO Ontology recovery
serves as the foundation for the OBO Foundry, which
is a cooperative work within ontology researchers
who have previously committed to implementing a
wider range of norms outlining best practices for on-
tology development. These guidelines aim to guar-
antee a progressive enhancement of formal accuracy
and reliability in ontologies, in order to satisfy the in-
creasing needs of data and information integration in
the biomedical field. In the following, we detail our
ontology according to the proposed methodology.
Cerebral palsy is a neurological disorder affect-
ing movement and coordination, often resulting from
brain damage before, during, or after birth. Rehabil-
itation plays a crucial role in treatment, focusing on
improving motor function, communication, and so-
cial participation. The ontology we propose aims to
support home-based rehabilitation for cerebral palsy
patients by integrating tools and treatments. Its de-
velopment begins with a requirements analysis phase,
identifying key concepts, attributes, relationships, and
axioms. In the design phase, a structured conceptual
model is created, progressively increasing in com-
plexity to ensure coherence and effectiveness.
4.1 Ontology Overview
The ontology can be developed using editors such as
Prot
´
eg
´
e or OWLGrinder. In this work, Prot
´
eg
´
e was
used for ontology creation. This allowed for the trans-
formation of knowledge about the required function-
alities of the proposed rehabilitation software for chil-
dren with cerebral palsy from an informal model into
a semi-formal model accessible to both domain ex-
perts and ontology developers. To enhance the on-
tology’s robustness and expressiveness, a comprehen-
sive glossary was created, detailing key concepts and
basic terminologies with precise definitions and ex-
plicit links to relevant resources.
Ontology-Based Framework for Personalized Home-Based Rehabilitation in Cerebral Palsy Care
709
The hierarchical structure of our model is ex-
plained in Figure 2. his structure organizes the key
components of the pediatric rehabilitation ontology,
enabling a comprehensive and systematic representa-
tion of the domain. In the following section, we will
explore each class within the hierarchical structure
of the pediatric rehabilitation ontology in greater de-
tail. Pediatric rehabilitation focuses on improving
the physical, cognitive, social, and emotional well-
being of children with disabilities or developmental
challenges. It aims to enhance their independence and
quality of life through targeted interventions and ther-
apies.
Figure 2: The hierarchical classes of the ontology.
This part in figure 3 of the ontology focuses on
Equipment and Technical Aids. It categorizes dif-
ferent types of aids into three subclasses: Technolog-
ical Aids, Specific Adaptations, and Mobility Aids.
• Technological Aids include various assistive tech-
nologies such as Environmental Control Systems,
Computer Assistance Technologies, Communica-
tion Devices, Adapted Digital Interfaces, and Per-
sonalized Learning Tools. These are designed to
enhance communication, learning, and environ-
mental interaction for children in rehabilitation.
• Specific Adaptations cover customized solutions
like Compensatory Technologies, Sensory Stim-
ulation Equipment, School Adaptations, and
Adapted Wheelchairs, tailored to meet the unique
needs of each child in educational and daily living
environments.
• Mobility Aids include Locomotion Aids, Or-
thoses and Appliances, and Positioning Systems,
which support physical mobility, posture, and
alignment, contributing to improved indepen-
dence and comfort.
This part of the ontology (figure 4) explores the In-
terdisciplinary Approach, emphasizing collabora-
tive methods for providing holistic care. It is divided
into two main subclasses: Family-Centered Approach
and Care Coordination.
Figure 3: The sub-classes of the Equip-
ment and technical aids class.
Figure 4: The sub-classes of the Interdisciplinary approach
class.
• Family-Centered Approach includes strategies
that prioritize the involvement and support of the
family in the rehabilitation process. It encom-
passes Parental Support Strategies, Family Educa-
tion, Comprehensive Support, and Resources and
Support Networks, aiming to empower families
with knowledge, tools, and networks necessary
for effective participation in their child’s care.
• Care Coordination focuses on the organized
and collaborative efforts among healthcare pro-
fessionals. This includes Communication Be-
tween Professionals, Multidisciplinary Consulta-
tion Meetings, Regular Monitoring and Adjust-
ment, and the creation of a Personalized Treat-
ment Plan. These elements ensure that care is in-
tegrated, consistently monitored, and adapted to
meet the evolving needs of the child.
This part of the ontology (figure 5) focuses on Motor
and Functional Therapy, outlining key components
of motor therapy. It is categorized into three main
subclasses: Specialized Interventions, Initial Motor
Assessment and Motor Rehabilitation Techniques.
EKM 2025 - 8th Special Session on Educational Knowledge Management
710
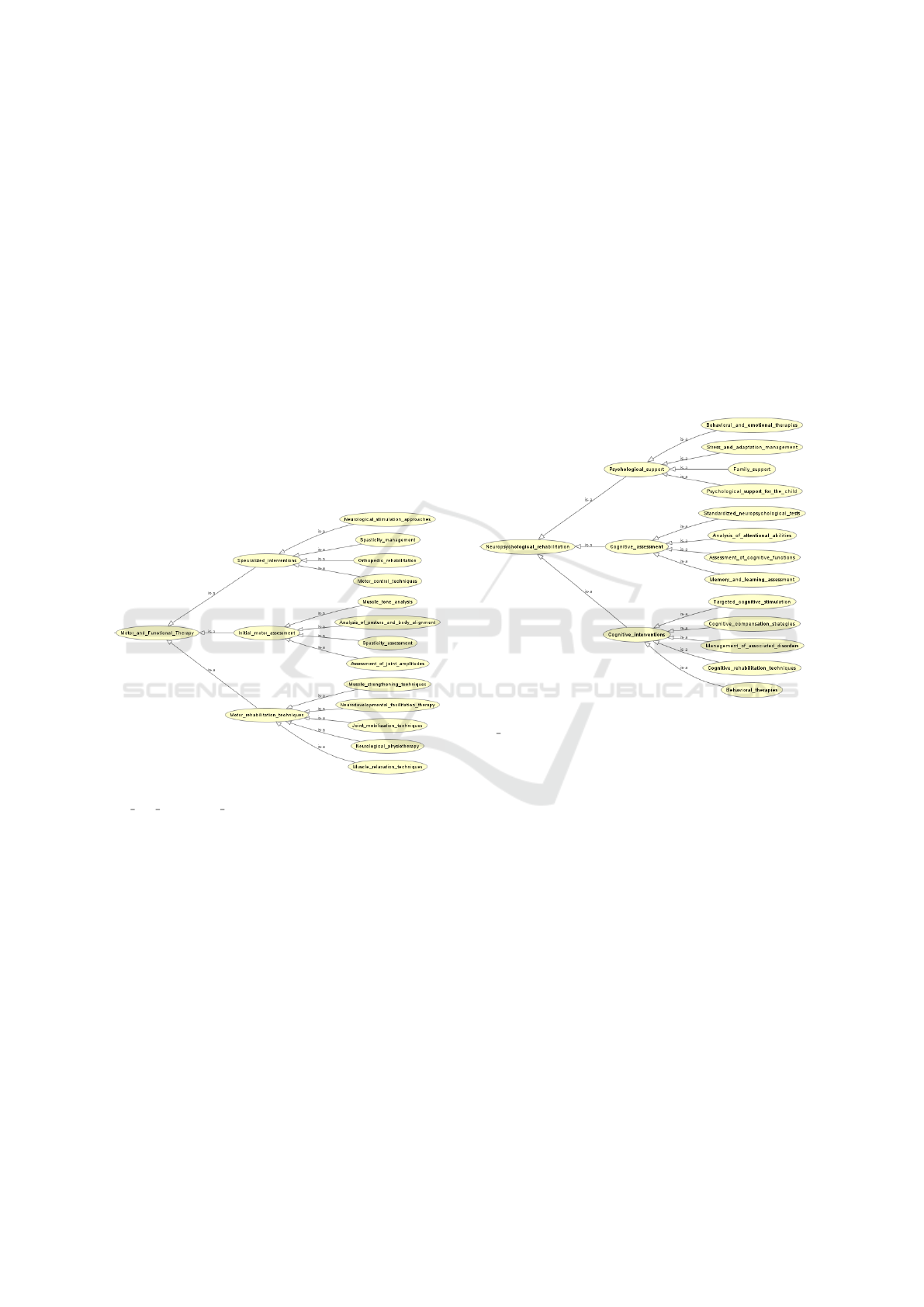
• Specialized Interventions include targeted ther-
apies such as Neurological Stimulation Ap-
proaches, Spasticity Management, Orthopedic
Rehabilitation, Motor Control Techniques, and
Muscle Tone Analysis. These interventions ad-
dress specific motor impairments and aim to en-
hance motor control and reduce spasticity.
• Initial Motor Assessment covers the foundational
evaluation processes like Analysis of Posture and
Body Alignment, Spasticity Assessment, Assess-
ment of Joint Amplitudes, and other diagnostic
measures crucial for creating therapy plans.
• Motor Rehabilitation Techniques consist of meth-
ods like Muscle Strengthening Techniques, Neu-
rodevelopmental Facilitation Therapy, Joint Mo-
bilization Techniques, Neurological Physiother-
apy, and Muscle Relaxation Techniques. These
techniques are designed to improve motor func-
tion, flexibility, and overall physical well-being.
Figure 5: The sub-classes of the Mo-
tor and Functional Therapy class.
This part focuses on the subdomain of Neuropsy-
chological Rehabilitation, a critical area within pe-
diatric rehabilitation that focuses on the intersection
of neurological and psychological care. It aims to ad-
dress the cognitive, emotional, and behavioral chal-
lenges faced by children with neurological conditions
or developmental disorders. It is subdivided into cat-
egories such as Psychological Support, Cognitive As-
sessment, and Cognitive Interventions.
• Psychological Support encompasses therapies
such as Behavioral and Emotional Therapies,
Stress and Adaptation Management, Family Sup-
port, and targeted support like Psychological Sup-
port for the Child, all aimed at addressing emo-
tional well-being and family dynamics.
• Cognitive Assessment includes methods to eval-
uate various cognitive functions, such as Analy-
sis of Attentional Abilities, Assessment of Cog-
nitive Functions, Memory and Learning Assess-
ment, and Targeted Cognitive Stimulation, en-
abling precise diagnostics of cognitive challenges.
• Cognitive Interventions involves strategies for re-
habilitation, including Cognitive Compensation
Strategies, Management of Associated Disorders,
Cognitive Rehabilitation Techniques, and Behav-
ioral Therapies, all focused on improving cogni-
tive and functional abilities. a critical area within
pediatric rehabilitation that focuses on the inter-
section of neurological and psychological care.
Figure 6: The sub-classes of the Neuropsychologi-
cal rehabilitation class.
This ontology represents the structure of Occupa-
tional Therapy within the broader domain of Pedi-
atric Rehabilitation. It is designed to support chil-
dren in achieving greater independence and improv-
ing their quality of life through functional and adap-
tive interventions tailored to their unique needs. The
ontology organizes this domain into key concepts and
categories that reflect the diverse aspects of occupa-
tional therapy.
• Functional Assessment focuses on evaluating the
child’s capabilities through methods such as Anal-
ysis of Home and School Environment, Assess-
ment of Activities of Daily Living, Analysis of
Fine Motor Skills, and Evaluation of Autonomy,
which together provide a comprehensive under-
standing of the child’s functional abilities and ar-
eas for improvement.
• Adaptive Interventions includes practical strate-
gies to improve daily functioning, such as Com-
pensation Techniques, Learning Daily Activities,
Ontology-Based Framework for Personalized Home-Based Rehabilitation in Cerebral Palsy Care
711
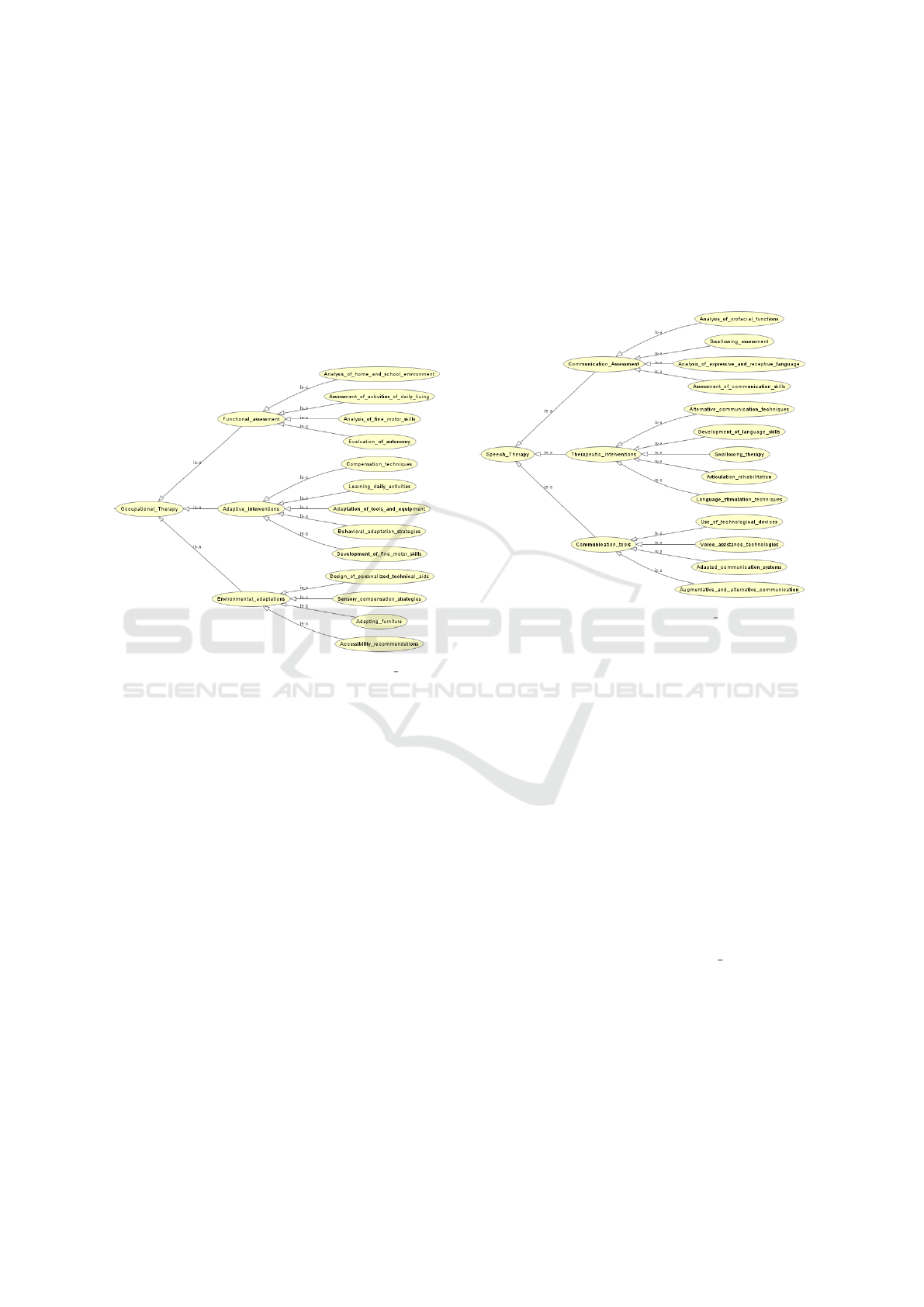
Adaptation of Tools and Equipment, Behavioral
Adaptation Strategies, and Development of Fine
Motor Skills, with an emphasis on personalized
tools and methods.
• Environmental Adaptations aims to modify the
child’s surroundings to better suit their needs.
This includes Sensory Compensation Strategies,
Adapting Furniture, Accessibility Recommenda-
tions, and Design of Personalized Technical Aids,
ensuring the environment facilitates the child’s re-
habilitation and independence.
Figure 7: The sub-classes of the Occupational Therapy
class.
This part, shown in figure 8 illustrates the Speech
Therapy domain within Pediatric Rehabilitation.
Speech therapy is a critical discipline aimed at ad-
dressing communication, language, and swallowing
difficulties in children, empowering them to interact
effectively with their environment and enhance their
quality of life. The ontology organizes this domain
into specific categories that reflect the comprehensive
nature of speech therapy interventions.
• Communication Assessment encompasses eval-
uating various aspects of communication, such
as Analysis of Orofacial Functions, Swallowing
Assessment, Analysis of Expressive and Recep-
tive Language, and Assessment of Communica-
tion Skills, while also exploring Alternative Com-
munication Techniques to support children with
specific challenges.
• Therapeutic Interventions targets the develop-
ment and enhancement of communication abili-
ties through methods like Development of Lan-
guage Skills, Swallowing Therapy, Articulation
Rehabilitation, and Language Stimulation Tech-
niques, often integrating Use of Technological
Devices to assist in therapy.
• Communication Tools provides resources to sup-
port speech therapy, including Voice Assistance
Technologies, Adapted Communication Systems,
and Augmentative and Alternative Communica-
tion methods, ensuring tailored support for each
child’s unique needs.
Figure 8: The sub-classes of the Speech Therapy class.
4.2 SWRL Rules
In addition, to enhance the ontology’s reasoning ca-
pabilities, a set of SWRL rules has been meticulously
developed.
These rules, organized in the form of a structured
list, enable new knowledge to be inferred from ex-
isting information within the ontology. This rigorous
approach guarantees a formal and coherent represen-
tation of domain knowledge, enabling the ontology to
be better understood and used more effectively.
Query 1:
Patient(?p) ∧ hasAssessment(?p, ?a) ∧
hasAssessmentType(?a, ”Functional”) ∧
hasAssessmentScore(?a, ?score) ∧
lessThan(?score, 40.0) →
requiresAdaptation(?p, Environmental Adaptation)
This logical rule is designed to automate decision-
making processes within the ontology, ensuring that
patients with limited functional abilities (as indicated
by a low assessment score) are identified for environ-
mental modifications to support their rehabilitation
needs. It incorporates both semantic reasoning and
threshold-based logic for personalized recommenda-
tions.
EKM 2025 - 8th Special Session on Educational Knowledge Management
712
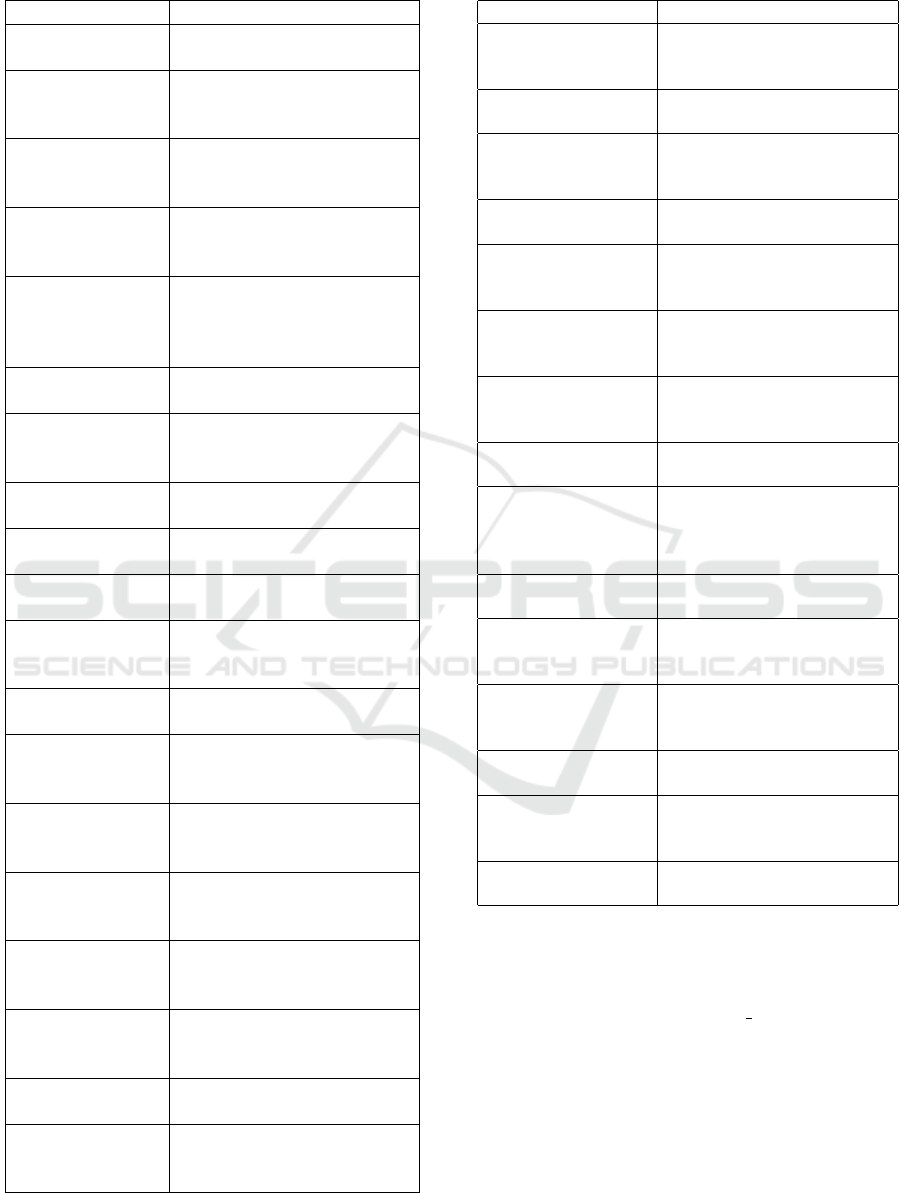
Table 2: Object Properties.
Data properties Definition
PatientID Represents the unique identi-
fier assigned to a patient.
Condition Describes the medical condi-
tion or diagnosis of the pa-
tient.
AdmissionDate Indicates the date on which
the patient was admitted to
the program.
DischargeDate Specifies the date on which
the patient was discharged
from the program.
ProgressScore Represents the progress
score of the patient, mea-
sured on a scale of 0.0 to
10.0.
AssessmentDate Specifies the date when the
assessment was conducted.
AssessmentScore Represents the score ob-
tained in the assessment, on
a scale of 0.0 to 100.0.
AssessmentType Indicates the type or cate-
gory of the assessment.
Recommendation Provides recommendations
based on the assessment.
SessionDate Specifies the date when the
therapy session occurred.
SessionDuration Represents the duration of
the therapy session, in min-
utes.
TherapyGoal Describes the goal or objec-
tive of the therapy session.
ProgressNotes Provides notes about the
progress made during the
session.
Frequency Indicates the frequency of
therapy sessions (e.g., ses-
sions per week).
IntensityLevel Specifies the intensity level
of the therapy session (Low,
Medium, or High).
EquipmentID Represents the unique iden-
tifier assigned to a piece of
equipment.
MaintenanceDate Specifies the date of the last
maintenance of the equip-
ment.
Specification Describes the technical spec-
ifications of the equipment.
AvailabilityStatus Indicates whether the equip-
ment is currently available
(True) or not (False).
Table 3: Data Properties.
Object properties Definition
hasTherapist Associates a patient with
a therapist responsible for
their rehabilitation.
assignedTo Links a therapist to a specific
rehabilitation program.
participatesIn Indicates that a patient par-
ticipates in a given therapy
session.
supervises Specifies that a therapist su-
pervises a therapy session.
requiresEquipment Indicates that a therapy ses-
sion requires specific techni-
cal equipment.
hasAssessment Links a patient to an as-
sessment that evaluates their
abilities or needs.
follows Indicates that a patient fol-
lows a specific treatment
plan.
collaboratesWith Represents collaboration be-
tween two therapists.
supportedBy Associates a patient with
a family member providing
support during their rehabil-
itation.
usesTool Specifies that speech therapy
uses a communication tool.
appliesTechnique Indicates that motor therapy
applies a specific rehabilita-
tion technique.
requiresAdaptation Indicates that a patient re-
quires environmental adapta-
tions for their rehabilitation.
utilizesAid Specifies that a patient uses a
mobility aid during therapy.
hasIntervention Indicates that a therapy ses-
sion includes a specific ther-
apeutic intervention.
conductsAssessment Specifies that a therapist con-
ducts a given assessment.
Query 2:
Patient(?p) ∧ hasProgressScore(?p, ?score) ∧
lessThan(?score, 6.0) =⇒
requiresAssessment(?p, Cognitive Assessment)
This rule identifies patients who need a cognitive
assessment based on their progress score. If a Patient
(?p) has a Progress Score (?score) below the thresh-
old of 6.0, the system infers that the patient requires
a Cognitive Assessment. This ensures that cogni-
tive evaluations are prioritized for individuals show-
ing signs of limited progress, potentially highlighting
areas requiring intervention.
Ontology-Based Framework for Personalized Home-Based Rehabilitation in Cerebral Palsy Care
713

Query 3:
Patient(?p) ∧ hasAssessment(?p, ?a) ∧
hasAssessmentScore(?a, ?score) ∧
lessThan(?score, 50.0) ∧
hasTherapyType(?p, Motor Therapy) =⇒
hasIntensityLevel(?p, ”High”)
This rule focuses on adjusting the intensity of mo-
tor therapy based on assessment scores. If a Patient
(?p) has undergone an Assessment (?a) with an As-
sessment Score (?score) below 50.0 and is already
undergoing Motor Therapy, the system recommends
increasing the therapy’s intensity by setting the Inten-
sity Level of the patient to ”High”. This rule supports
personalized treatment plans by dynamically adjust-
ing motor therapy intensity based on a patient’s per-
formance and needs.
5 DISCUSSION
The development and implementation of our
ontology-based framework for cerebral palsy reha-
bilitation presents several significant contributions
and implications for home-based exercise programs
(HEP). Our findings highlight both the potential
benefits and challenges in implementing such a
semantic framework for rehabilitation. The proposed
ontological framework demonstrates several key
advantages for cerebral palsy rehabilitation. The
hierarchical structure of our ontology successfully
integrates diverse aspects of rehabilitation, from
equipment and technical aids to specialized therapies.
This comprehensive approach ensures that all crucial
elements of rehabilitation are systematically repre-
sented and interlinked. By adopting OBO Foundry
principles, our ontology promotes standardization
and interoperability with existing biomedical ontolo-
gies. This compatibility enhances the potential for
knowledge sharing across different healthcare sys-
tems and rehabilitation platforms. Furthermore, the
framework’s ability to capture complex relationships
between patient characteristics, rehabilitation tech-
niques, and outcomes enables highly personalized
treatment recommendations, which is particularly
valuable for home-based exercise programs where
individualized guidance is crucial.
The implementation of our framework has several
important implications for clinical practice. The se-
mantic rules and relationships defined in our ontol-
ogy provide a robust foundation for clinical decision
support systems, allowing healthcare providers to
leverage this structured knowledge to make more in-
formed decisions about rehabilitation protocols. The
framework’s comprehensive modeling of rehabilita-
tion concepts enables better remote monitoring of pa-
tient progress, which is essential for home-based ex-
ercise programs and particularly relevant given the
increasing importance of telerehabilitation solutions.
Additionally, the standardized representation of re-
habilitation concepts and procedures helps maintain
consistency in treatment delivery and assessment,
even in remote settings. Several technical aspects
warrant discussion in our implementation. While our
ontology successfully models the complex domain
of cerebral palsy rehabilitation, considerations must
be made for scaling the system to handle larger pa-
tient populations and additional rehabilitation proto-
cols. The implementation of semantic rules through
SWRL presents challenges in terms of computational
efficiency and real-time processing, suggesting that
future work should focus on optimizing rule execu-
tion for time-sensitive applications. Moreover, the
comprehensive nature of our ontology raises impor-
tant considerations about data privacy and security,
particularly when handling sensitive patient informa-
tion in home-based settings.
Based on our findings, several areas merit further
investigation. Future work should explore the inte-
gration of machine learning algorithms with our on-
tological framework to enhance the adaptive capabil-
ities of rehabilitation recommendations. The frame-
work should be expanded to accommodate cultural
and linguistic variations in rehabilitation practices,
ensuring broader applicability across different health-
care systems. Large-scale clinical validation studies
are needed to assess the framework’s effectiveness in
improving rehabilitation outcomes compared to tradi-
tional approaches. Additionally, the development of
mobile applications that can seamlessly interact with
the ontological framework would enhance accessibil-
ity and user engagement in home-based settings.
Several limitations of our current work should be
acknowledged. The current validation of the ontology
has been primarily theoretical and would benefit from
extensive real-world testing in clinical settings. The
implementation of our framework requires significant
technical infrastructure, which may limit its adoption
in resource-constrained environments. While com-
prehensive for cerebral palsy rehabilitation, the ontol-
ogy may require substantial modifications for appli-
cation to other rehabilitation domains.
The proposed ontology-based framework repre-
sents a significant step forward in structuring and de-
livering home-based rehabilitation programs for cere-
bral palsy patients. However, its successful imple-
mentation will require careful consideration of both
technical and practical challenges, along with contin-
EKM 2025 - 8th Special Session on Educational Knowledge Management
714

ued refinement based on clinical feedback and tech-
nological advancements.
6 CONCLUSION
In conclusion, our ontology for cerebral palsy reha-
bilitation marks a significant advancement in home-
based exercise programs. By integrating diverse re-
habilitation components within a hierarchical struc-
ture and adhering to OBO Foundry principles, it en-
sures standardization and interoperability with ex-
isting biomedical ontologies. This comprehensive
framework facilitates personalized treatment recom-
mendations and supports clinical decision-making
through well-defined semantic rules and relation-
ships.
The implementation has shown great potential in
enhancing remote monitoring and ensuring consis-
tency in treatment delivery, which is especially vital
for home-based rehabilitation. However, challenges
remain, such as scalability and optimizing rule execu-
tion for time-sensitive applications, indicating areas
for future improvement.
Future research should prioritize integrating ma-
chine learning algorithms to improve adaptability, ad-
dressing cultural and linguistic diversity, and validat-
ing the framework through large-scale clinical stud-
ies. Developing accessible mobile applications could
enhance user engagement in home-based settings.
While challenges such as real-world testing and tech-
nical infrastructure persist, the framework establishes
a solid foundation for advancing rehabilitation prac-
tices.
REFERENCES
Abdullah, Z. H., Zakaria, L. Q., Ismail, W., and Ismail,
S. (2022). Developing an exercise games ontology
towards standard rehabilitation clinical terms. In
2022 Euro-Asia Conference on Frontiers of Computer
Science and Information Technology (FCSIT), pages
173–176. IEEE.
Beckers, L., Schnackers, M., Janssen-Potten, Y., Kleijnen,
J., and Steenbergen, B. (2017). Feasibility and ef-
fect of home-based therapy programmes for children
with cerebral palsy: a protocol for a systematic review.
BMJ Open, 7(2).
Chen, K., Ren, Y., Gaebler-Spira, D., and Zhang, L.-Q.
(2014). Home-based tele-assisted robotic rehabili-
tation of joint impairments in children with cerebral
palsy. In 36th Annual International Conference of the
IEEE Engineering in Medicine and Biology Society.
Chu, E. C.-P., Yun, S. M. H., Hau, K. H. Y., and Piong,
S. Z. (2022). Smart rehabilitation clinic. Journal of
Contemporary Chiropractic, 5:7–12.
Chung, H., Lee, H., Kim, C., Hong, S., and Lee, J. (2019).
Patient-provider interaction system for efficient home-
based cardiac rehabilitation exercise. IEEE Access,
7:14611–14622.
Demeke, Z. D., Assefa, Y. A., Abich, Y., and Chala, M. B.
(2023). Home-based therapy and its determinants for
children with cerebral palsy, exploration of parents’
and physiotherapists’ perspective, a qualitative study,
ethiopia. PLoS One, 18(2).
Ejaz, F., Tanveer, F., Shoukat, F., Fatima, N., and Ahmad,
A. (2024). Effectiveness of routine physical therapy
with or without home-based intensive bimanual train-
ing on clinical outcomes in cerebral palsy children: a
randomised controlled trial. Physiotherapy Quarterly,
32(1):78–83.
Fong, J., Ocampo, R., Gross, D. P., and Tavakoli, M. (2020).
Intelligent robotics incorporating machine learning al-
gorithms for improving functional capacity evaluation
and occupational rehabilitation. Journal of Occupa-
tional Rehabilitation, 30:362–370.
Ge, Y., Zhao, W., Zhang, L., Zhao, X., Shu, X., Li, J., Qiao,
L., Liu, Y., and Wang, H. (2024). Home physical ther-
apy versus telerehabilitation in improving motor func-
tion and quality of life in parkinson’s disease: a ran-
domized controlled trial. BMC Geriatrics, 24(1):968.
Gibson, J., Sampford, J., Myers-Ingram, R., and Jones,
G. D. (2023). Embedding the rehabilitation treatment
specification system (rtss) into clinical practice: an
evaluation of a pilot teaching programme. BMC Med-
ical Education, 23(1):85.
Goswami, J. N., Sankhyan, N., and Singhi, P. (2021). Add-
on home-centered activity-based therapy vs conven-
tional physiotherapy in improving walking ability at
6-months in children with diplegic cerebral palsy:
A randomized controlled trial. Indian Pediatrics,
58:826–832.
Hier, D. B. and Brint, S. U. (2020). A neuro-ontology for
the neurological examination. BMC Medical Infor-
matics and Decision Making, 20:1–9.
Ibeneme, S. C., Chimereze, N. R., Fortwengel, G., John,
J. N., Ibeneme, G. C., and Nwosu, A. O. (2024). Ef-
fectiveness of home-based exercise programme in im-
proving function, activity and participation for chil-
dren with cerebral palsy: a systematic review and
meta-analysis.
Junior, P. R. F., Souza, P. P., dos Reis, K. K. M., and Filoni,
E. (2021). Home-based physiotherapy programmes
for individuals with neurological diseases: systematic
review. Fisioterapia em Movimento, 32.
Karray, M., Otte, N., Rai, R., Ameri, F., Kulvatunyou, B.,
Smith, B., Kiritsis, D., Will, C., Arista, R., et al.
(2021). The industrial ontologies foundry (iof) per-
spectives.
Komatireddy, R., Chokshi, A., Basnett, J., Casale, M.,
Goble, D., and Shubert, T. (2014). Quality and quan-
tity of rehabilitation exercises delivered by a 3-d mo-
tion controlled camera: A pilot study. International
Journal of Physical Medicine & Rehabilitation.
ling Chen, C., chung Lin, K., ju Kang, L., and yi Wu, C.
(2014). Potential predictors of functional outcomes
Ontology-Based Framework for Personalized Home-Based Rehabilitation in Cerebral Palsy Care
715

after home-based constraint-induced therapy for chil-
dren with cerebral palsy. The American Journal of
Occupational Therapy, 68.
Lopes, R. P., Barroso, B., Deusdado, L., Novo, A.,
Guimar
˜
aes, M., Teixeira, J. P., and Leit
˜
ao, P. (2021).
Digital technologies for innovative mental health re-
habilitation. Electronics, 10:2260.
Lorentzen, J., Greve, L. Z., Kliim-Due, M., Rasmussen, B.,
Bilde, P. E., and Nielsen, J. B. (2015). Twenty weeks
of home-based interactive training of children with
cerebral palsy improves functional abilities. BMC
Neurology, 15:1–12.
Macintosh, A., Vignais, N., Desailly, E., Biddiss, E., and
Vigneron, V. (2020). A classification and calibration
procedure for gesture specific home-based therapy ex-
ercise in young people with cerebral palsy. IEEE
Transactions on Neural Systems and Rehabilitation
Engineering, 29:144–155.
Mennella, C., Maniscalco, U., Pietro, G. D., and Esposito,
M. (2023a). A deep learning system to monitor and
assess rehabilitation exercises in home-based remote
and unsupervised conditions. Computers in Biology
and Medicine, 166:107485.
Mennella, C., Maniscalco, U., Pietro, G. D., and Esposito,
M. (2023b). The role of artificial intelligence in future
rehabilitation services: a systematic literature review.
IEEE Access, 11:11024–11043.
O’Neill, D. and Forman, D. E. (2020). The importance of
physical function as a clinical outcome: assessment
and enhancement. Clinical Cardiology, 43:108–117.
Palagin, O., Kaverinsky, V., Petrenko, M., and Malakhov,
K. (2023). Digital health systems: Ontology-based
universal dialog service for hybrid e-rehabilitation ac-
tivities support. In 2023 IEEE 12th International
Conference on Intelligent Data Acquisition and Ad-
vanced Computing Systems: Technology and Applica-
tions (IDAACS), volume 1, pages 84–89. IEEE.
Racic, M., Kusmuk, S., and Krstovic-Spremo, V. (2014).
Effectiveness of the home-based habilitation pro-
gramme for children with cerebral palsy.
Senbekov, M., Saliev, T., Bukeyeva, Z., Almabayeva, A.,
Zhanaliyeva, M., Aitenova, N., Toishibekov, Y., and
Fakhradiyev, I. (2020). The recent progress and ap-
plications of digital technologies in healthcare: a re-
view. International Journal of Telemedicine and Ap-
plications.
Spoladore, D., Colombo, V., Fumagalli, A., Tosi, M.,
Lorenzini, E. C., and Sacco, M. (2024). An
ontology-based decision support system for tailored
clinical nutrition recommendations for patients with
chronic obstructive pulmonary disease: Development
and acceptability study. JMIR Medical Informatics,
12:e50980.
Triantafyllidis, A., Filos, D., Buys, R., Claes, J., Cor-
nelissen, V., Kouidi, E., Chatzitofis, A., Zarpalas, D.,
Daras, P., Walsh, D., et al. (2018). Computerized
decision support for beneficial home-based exercise
rehabilitation in patients with cardiovascular disease.
Computer Methods and Programs in Biomedicine,
162.
EKM 2025 - 8th Special Session on Educational Knowledge Management
716
