
Real-Time 3D Posture Tracking for Surgeons in Pediatric Minimally
Invasive Surgery
Pietro Neroni
1 a
, Giuseppe Caggianese
1 b
, Ciro Esposito
2 c
and Luigi Gallo
1,3 d
1
Institute for High Performance Computing and Networking, National Research Council of Italy,
Via Pietro Castellino 111, 80131, Naples, Italy
2
Azienda Ospedaliera Universitaria Federico II, Via Sergio Pansini 5, 80131, Naples, Italy
3
Depart ples, Italy
pietro.neroni@icar.cnr.it, giuseppe.caggianese@icar.cnr.it, ciroespo@unina.it, luigi.gallo@unipegaso.it
Keywords:
Posture Monitoring, Depth Camera Tracking, Musculoskeletal Disorders, Ergonomics, Surgical Training,
Pediatric Surgery.
Abstract:
Minimally invasive pediatric surgery presents ergonomic challenges that significantly increase the risk of mus-
culoskeletal disorders (MSDs) among surgeons due to prolonged periods of suboptimal posture. This study
introduces a real-time posture monitoring and correction system designed to address this issue. The system uti-
lizes depth camera technology, interactive feedback mechanisms, advanced skeletal tracking, and ergonomic
assessment algorithms to continuously monitor and evaluate surgeons’ posture. Through rapid data processing,
the system provides real-time feedback, enabling immediate posture adjustments during surgical procedures.
It delivers non-intrusive alerts to inform medical staff when incorrect postures are detected, thereby promoting
ergonomic well-being and reducing the incidence of MSDs. Designed for seamless integration into the peri-
operative environment, the system meets strict requirements for privacy, sterility, and operational efficiency.
Beyond its application in surgical practice, the system can also enhance surgical education and training by
providing real-time feedback, enabling personalized learning pathways, and gamified simulation exercises. It
provides detailed analyses of trainee performance, enabling instructors to deliver targeted feedback and de-
velop adaptive training strategies based on detected posture deviations.
1 INTRODUCTION
Minimally invasive pediatric surgery has experienced
exponential growth over the past two decades, of-
fering significant benefits in reducing postoperative
pain, shorter hospital stays, and less invasive scar-
ring (Marinho et al., 2021). However, new chal-
lenges have emerged alongside these evident clini-
cal improvements, mainly related to ergonomics for
the surgical team (Rosenblatt et al., 2013; Marinho
et al., 2020). Although robotic platforms such as the
da Vinci system have enhanced ergonomics through
features like tremor filtering and articulated instru-
ments, they do not entirely resolve posture-related
challenges (Haidegger et al., 2022). Operating in con-
fined spaces with laparoscopic or robotic instruments
a
https://orcid.org/0000-0002-3802-795X
b
https://orcid.org/0000-0001-6607-6591
c
https://orcid.org/0000-0002-8858-6848
d
https://orcid.org/0000-0002-1281-404X
initially designed for adult surgery often forces the
surgeon to maintain static or suboptimal postures for
extended periods. The result is an increased risk of
developing musculoskeletal disorders (MSDs) (Alle-
blas et al., 2017), which can lead to chronic pain and,
in the long term, decreased performance or work ab-
sences.
Recent studies show that 50-85% of surgeons ex-
perience chronic pain and discomfort, mainly in the
neck, shoulders, and back (Anwary et al., 2021;
Bertram et al., 2023). Lower back and neck pain are
among the most common issues surgeons face, af-
fecting their physical well-being and their ability to
concentrate and make decisions during surgical pro-
cedures (Matern, 2009). Numerous studies have high-
lighted how the use of ergonomically unsuitable tools,
the height of operating tables, and the arrangement of
monitors can contribute to incorrect postures (Wong
et al., 2022; Schlussel and Maykel, 2019). Further-
more, the anatomical characteristics of pediatric pa-
tients require surgeons to perform exact maneuvers
Neroni, P., Caggianese, G., Esposito, C. and Gallo, L.
Real-Time 3D Posture Tracking for Surgeons in Pediatric Minimally Invasive Surgery.
DOI: 10.5220/0013504200003932
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Conference on Computer Supported Education (CSEDU 2025) - Volume 1, pages 921-928
ISBN: 978-989-758-746-7; ISSN: 2184-5026
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
921

with minimal margins for error, thereby exacerbat-
ing issues related to posture and movement (Walsh,
2023).
To overcome these difficulties, recent non-
invasive monitoring solutions using depth cameras,
wearables, and machine learning offer real-time pos-
ture feedback for reducing musculoskeletal risks and
improving surgical efficiency (Romeo et al., 2022;
Nadeem et al., 2024; Vermander et al., 2024). Effec-
tive ergonomic operating room monitoring requires
key features: accurate surgeon tracking, ignoring
other personnel (Hu et al., 2022); gesture-based ac-
tivation for sterile, seamless operation (Gallo et al.,
2011; Bigdelou et al., 2012); and privacy via non-
RGB video streams (Srivastav et al., 2019; Flouty
et al., 2018).
This paper presents the development of an inno-
vative system designed to assist surgeons in pediatric
minimally invasive surgery by proactively addressing
ergonomic challenges. It aims to reduce the risk of
posture-related musculoskeletal issues, enhance the
comfort of medical staff during operations, and sup-
port sustained concentration throughout surgical pro-
cedures. The underlying idea of this research is to
combine the acquisition of 3D data through depth sen-
sors with real-time processing techniques to immedi-
ately alert the surgeon of any deviations from opti-
mal ergonomic parameters (Romeo et al., 2022; Wang
et al., 2024). The feedback interface, designed to be
non-invasive and adaptable to the operative workflow,
represents a further advancement in making the oper-
ating room safer and more comfortable for the entire
team (Ayvaz et al., 2023). The anticipated outcome
is not only the improvement of individual surgeons’
posture but also a broader enhancement of ergonomic
standards in minimally invasive pediatric surgery, ul-
timately reducing the prevalence of posture-related
disorders and the associated socio-health costs (Ay-
vaz et al., 2023). Finally, this paper includes case
studies exploring the co-building of posture monitor-
ing in surgical education and training. The study ana-
lyzes these technologies to understand how they affect
short-term performance improvements and long-term
ergonomics awareness among surgical trainees.
2 RELATED WORK
Research on posture monitoring and ergonomic as-
sessment in minimally invasive surgery has steadily
increased, reflecting growing concerns about the im-
pact of surgeons’ posture on their well-being (Van Det
et al., 2008). Traditionally, ergonomic evaluations
have relied on post hoc methods, including question-
naires, perceived exertion measures (e.g., the Borg
scale), and manual video analysis (Wong et al., 2022;
Weitbrecht et al., 2023). One of the most widely used
tools for ergonomic assessment is the Rapid Upper
Limb Assessment (RULA) method, which enables the
static analysis of key postures by evaluating trunk,
neck, and upper limb joint angles (McAtamney and
Corlett, 1993). RULA has been applied across var-
ious healthcare professions, including cleaning staff
(Koskas and Vignais, 2024), laparoscopic surgeons,
surgical assistants, nurses (Pazouki et al., 2017),
and otolaryngologists performing endoscopic sinus
surgery (Dabholkar et al., 2020). However, these con-
ventional methods present significant limitations, as
their reliability often depends on evaluator subjectiv-
ity, and post hoc assessments do not facilitate real-
time posture correction (Schlussel and Maykel, 2019;
Ayvaz et al., 2023).
In recent years, several studies have explored
more objective and automated techniques for posture
detection. Notably, there has been increasing interest
in the use of wearable inertial sensors, such as Inertial
Measurement Units (IMUs), for tracking joint move-
ments (Stefana et al., 2021; Haidegger et al., 2022;
Zhou et al., 2006). These devices enable continu-
ous and non-invasive data collection; however, they
present challenges related to surgeon comfort and the
need for individual sensor calibration (Romeo et al.,
2022). Moreover, cables or wearable modules may
introduce obstacles in the highly sterile and regu-
lated environment of the operating room (Wang et al.,
2024).
Computer vision systems based on RGB-D cam-
eras have gained increasing attention for their ability
to non-invasively detect posture and body position in
space (Huang et al., 2021; Antico et al., 2021). Orig-
inally developed for the gaming industry and later
adapted for clinical research, depth cameras enable
the extraction of detailed 3D posture information, al-
lowing for precise calculations of joint angles and
postural deviations (Vermander et al., 2024). Many
approaches leverage computer vision and machine
learning algorithms to extract and analyze skeletal
data, facilitating real-time applications with high re-
liability (Romeo et al., 2022; Gallo, 2013; Bertram
et al., 2023). Additionally, some methods incor-
porate dynamic statistical models (Chai and Hod-
gins, 2007) and data reliability integration techniques
(Shum et al., 2013; Zhou et al., 2014) to mitigate
noise and inaccuracies typical of RGB-D sensing de-
vices. Advanced data structures, such as the Filtered
Pose Graph (Plantard et al., 2017), have also been pro-
posed to ensure continuity even in the presence of oc-
clusions. Recent studies have explored the potential
ERSeGEL 2025 - Workshop on Extended Reality and Serious Games for Education and Learning
922
of Microsoft Kinect sensors for automating the RULA
assessment method. Research suggests that Kinect
sensors can reliably capture joint angle data and com-
pute RULA scores in assembly line operations (Jara
et al., 2022; Jiang et al., 2017). Moreover, the ac-
curacy of Kinect-based RULA assessments has been
validated through expert evaluations and comparisons
with standard motion capture systems.
3 CLINICAL REQUIREMENTS
ANALYSIS
A focus group was conducted with the Pediatric
Surgery Unit at the Federico II University of Naples
to define the system’s clinical requirements. During
these sessions, surgeons highlighted key ergonomic
issues in pediatric minimally invasive surgery, includ-
ing the prolonged maintenance of static postures and
the difficulty of correcting them in real-time without
disrupting surgical workflow. The following section
outlines the key requirements that guided its design:
1. Surgeon Recognition and Tracking. The system
must accurately recognize and track the surgeon
among the surgical team members. This function-
ality is essential to ensure that posture monitoring
is applied exclusively to the intended subject, pre-
venting interference or data contamination from
other personnel present in the room. By isolating
relevant parameters, the system enhances the ac-
curacy of postural analysis.
2. Gesture-Based Identification. To optimize sur-
geon identification and eliminate the need for
manual interactions, the system must incorporate
a gesture-based identification mechanism, per-
formed by the surgeon at the beginning of the pro-
cedure. This approach significantly reduces auto-
matic identification errors and ensures swift and
reliable control. A predefined, system-recognized
gesture allows medical personnel to initiate postu-
ral monitoring automatically, eliminating the need
for touchscreen interfaces or manual devices. This
feature enhances operational efficiency while ad-
hering to the strict hygiene and sterility require-
ments of the surgical environment.
3. Privacy Protection. To safeguard the privacy of
both medical personnel and patients, the system
must avoid the use of RGB video streams, which
could inadvertently capture and reveal sensitive
visual information.
4. Non-Interference with Surgical Equipment.
The system must operate without disrupting ex-
isting surgical equipment or restricting the mobil-
ity of medical personnel. Its integration should
be seamless, ensuring unobstructed workflow and
adherence to standard surgical protocols.
5. Minimal Interaction and Intuitive Interface.
The system must require minimal interaction from
the surgeon, thereby reducing distractions and op-
erational downtime. Additionally, posture-related
notifications should be designed to be clear, non-
invasive, and seamlessly integrated into the surgi-
cal workflow, ensuring effective communication
without disrupting the procedure.
4 THE PROPOSED SOLUTION
The proposed solution employs a depth camera inte-
grated with advanced skeletal tracking software to au-
tomatically identify and monitor human body joints.
This system is designed to continuously assess the
surgeon’s posture during surgical procedures. Upon
detecting an incorrect posture, the system generates
real-time visual notifications on the operating room
display. These alerts enable the surgeon to promptly
adjust their position, thereby mitigating the risk of
musculoskeletal injuries and promoting ergonomic
practices in the operating environment.
4.1 Hardware Configuration
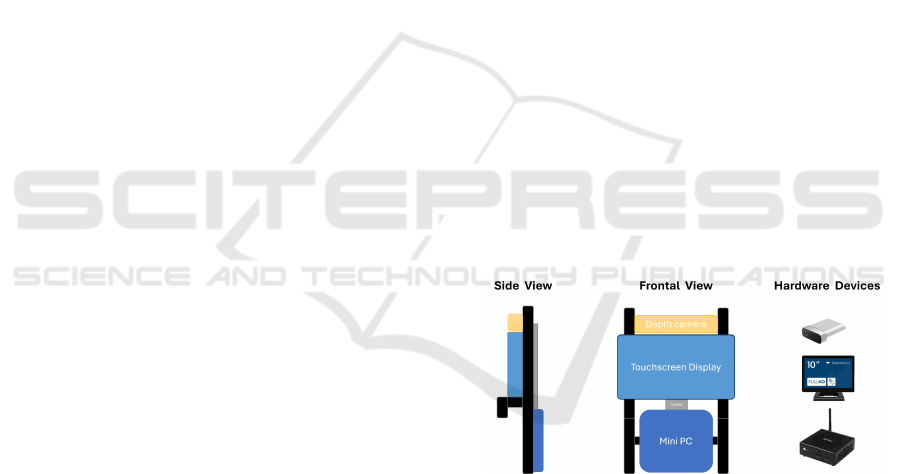
Figure 1: Hardware configuration of the proposed solution.
The hardware configuration is illustrated in Fig-
ure 1. To ensure seamless integration without in-
terfering with surgical equipment, the detection de-
vice is strategically positioned at an elevated loca-
tion above the primary operating room display. This
placement minimizes obstruction to surgical proce-
dures and avoids hindering the operators’ movements.
Furthermore, the system is designed to be easily re-
movable or adjustable, facilitating quick modifica-
tions as needed. The selected devices have been op-
timized for miniaturization to reduce physical clutter
and maintain an unobtrusive presence in the operating
environment.
Real-Time 3D Posture Tracking for Surgeons in Pediatric Minimally Invasive Surgery
923

For surgeon tracking, the system utilizes the Mi-
crosoft Azure Kinect DK, a depth camera that em-
ploys time-of-flight technology to generate three-
dimensional skeletal maps. This approach eliminates
the need for processing color images, focusing exclu-
sively on detecting joint positions and tracking the
surgeon’s movements. This design choice not only
safeguards privacy but also reduces computational de-
mands, thereby enhancing system efficiency. Figure 2
depicts the joint mapping capabilities of the sensor.
For notifications, a 10-inch Beetronics Mini
Touchscreen Display was selected. This display is
equipped with integrated speakers to provide auditory
feedback in addition to visual alerts when the surgeon
adopts an incorrect posture.
Figure 2: Body joints tracked by the Azure Kinect camera.
Finally, a ZOTAC ZBOX Mini PC equipped with
an Intel Core i7 processor and an NVIDIA RTX
A4500 graphics card featuring 16 GB of dedicated
memory was chosen to handle the graphical process-
ing demands. This hardware configuration ensures ef-
ficient three-dimensional skeletal reconstruction and
real-time management of visual notifications and en-
ables body tracking at approximately 30 FPS.
4.2 Interface
The interface has been designed to minimize interac-
tion requirements, allowing the surgeon to focus en-
tirely on the procedure without disruptions or com-
plications when using the system. The graphical in-
terface consists of a text-based notification system
displayed on a mini-display. Because of the limited
screen size, notifications must be brief enough to be
read easily during surgery, pointing only to relevant
information. The system’s workflow is illustrated in
figure 3, where the top row shows the perspective
from the Azure Kinect sensor, and the bottom row
represents the surgeon’s viewpoint. Initially, before
recognizing the surgeon, the display shows the mes-
sage “Waiting for identification gesture”. To iden-
tify themselves, the surgeon must raise their hand for
two seconds, after which the display updates to “Sur-
geon detected. Monitoring on”. If the surgeon main-
tains a correct posture during surgery, the system dis-
plays “Posture OK. Monitoring...”. However, if a de-
viation from the optimal posture is detected, a spe-
cific alert indicates the nature of the incorrect posture.
The visual notification is supplemented by an unob-
trusive auditory cue that allows surgeons to receive
immediate feedback without looking away from the
surgical field. Therefore, surgeons may immediately
adjust their positioning, mitigating musculoskeletal
strain and reducing the risk of long-term ergonomic
issues.
4.3 Postural Tracking
Postural tracking is based on the three-dimensional
reconstruction of the surgeon’s skeleton, utilizing
algorithms that process data from the depth cam-
era. These algorithms analyze joint positions in real
time to assess the surgeon’s posture during the op-
eration. Among the various techniques for assess-
ing postural risk, we chose to base our approach on
the RULA (Rapid Upper Limb Assessment) method,
given its extensive documentation in the literature.
This method generates a score based on the biome-
chanical and postural load demands of work activ-
ities, with a particular focus on the upper body, in-
cluding the neck, trunk, and upper limbs. Given our
emphasis on analyzing postural discomfort related to
the surgeon’s upper body, the RULA method was de-
termined to be the most appropriate for this study.
This approach is particularly relevant as tracking oc-
curs from the waist upwards, with the operating table
obscuring the lower body.
For the calculation of most of the angles re-
quired for assessment, we referenced (Manghisi et al.,
2017), which uses the Kinect v2 sensor to detect
risky postures according to the RULA method. A
comparative analysis was then conducted between
the joints tracked by the Kinect v2 sensor and those
tracked by the Azure Kinect sensor. Unlike (Manghisi
et al., 2017), which calculates a comprehensive pos-
ture score for the surgeon, our method provides real-
time notifications to alert the surgeon whenever an
improper posture is detected.
Specifically, the system automatically detects and
notifies the surgeon of the following incorrect pos-
tures:
• Trunk Flexion (Forward or Backward) (see fig-
ure 4.a). Occurs when the trunk is excessively in-
ERSeGEL 2025 - Workshop on Extended Reality and Serious Games for Education and Learning
924

Figure 3: System workflow for surgeon posture monitoring. The top row illustrates the Azure Kinect sensor’s perspective,
while the bottom represents the surgeon’s viewpoint. (a) Initially, the system displays ”Waiting for identification gesture.”
(b) When the surgeon raises their hand for two seconds, the display updates to ”Surgeon detected. Monitoring on.” (c) If the
surgeon maintains a correct posture, the display shows ”Posture OK. Monitoring. . . ”. (d) When an incorrect posture (e.g.,
forward trunk flexion) is detected, the system provides real-time feedback through a visual notification, prompting the surgeon
to adjust their posture.
clined either forward or backward from the neu-
tral, upright position. The trunk inclination an-
gle is calculated using the positions of the head,
pelvis, and spine joints. Positive values corre-
spond to forward flexion, while negative values
indicate extension or backward bending.
• Lateral Trunk Inclination (see figure 4.b). Oc-
curs when the trunk is excessively tilted to one
side relative to the vertical position. The lateral
inclination angle is measured based on the posi-
tions of the head, pelvis, and spine joints. Higher
values indicate a greater degree of lateral tilt.
• Trunk Rotation Around the Vertical Axis (see
figure 4.c). Occurs when the trunk undergoes ex-
cessive rotation around the vertical axis, which
is a critical condition leading to asymmetric pos-
tures. The trunk torsion angle is measured by
comparing the rotation of the torso relative to its
initial position, using the relative positions of the
torso and shoulder joints.
• Excessive Arm Extension (see figure 4.d). Oc-
curs when the elbow is overextended, keeping the
arm rigidly straight without sufficient flexion for
ergonomic movement. The arm flexion angle is
computed by analyzing the positions of the shoul-
der, elbow, and wrist joints. An angle of 0° repre-
sents a fully extended (straight) arm, with insuffi-
cient flexion indicating an incorrect posture.
• Excessive Shoulder Abduction (see figure 4.e).
Occurs when the shoulder is raised laterally be-
yond ergonomic limits. The shoulder abduc-
tion angle is measured by analyzing the three-
dimensional positions of the shoulder, elbow, and
wrist joints. Positive values indicate outward
movement (abduction), while negative values rep-
resent extension or adduction.
5 CASE STUDY: POSTURE
MONITORING IN SURGICAL
EDUCATION AND TRAINING
The real-time posture monitoring system introduced
in this paper holds much promise for changing surgi-
cal education, particularly in pediatric minimally in-
vasive surgery. The system’s introduction into train-
ing programs could help novices and veteran surgeons
become attuned to proper ergonomic practices, possi-
bly reducing the risk of musculoskeletal disorders in
the long term. The primary advantages of utilizing
such a system in surgical education and training are
as follows:
• Real-Time Feedback in Simulated Environ-
ments. An important component of efficient sur-
gical training is the ability to recreate safe and re-
producible real-life scenarios. The posture moni-
toring system gives trainees ongoing feedback on
Real-Time 3D Posture Tracking for Surgeons in Pediatric Minimally Invasive Surgery
925
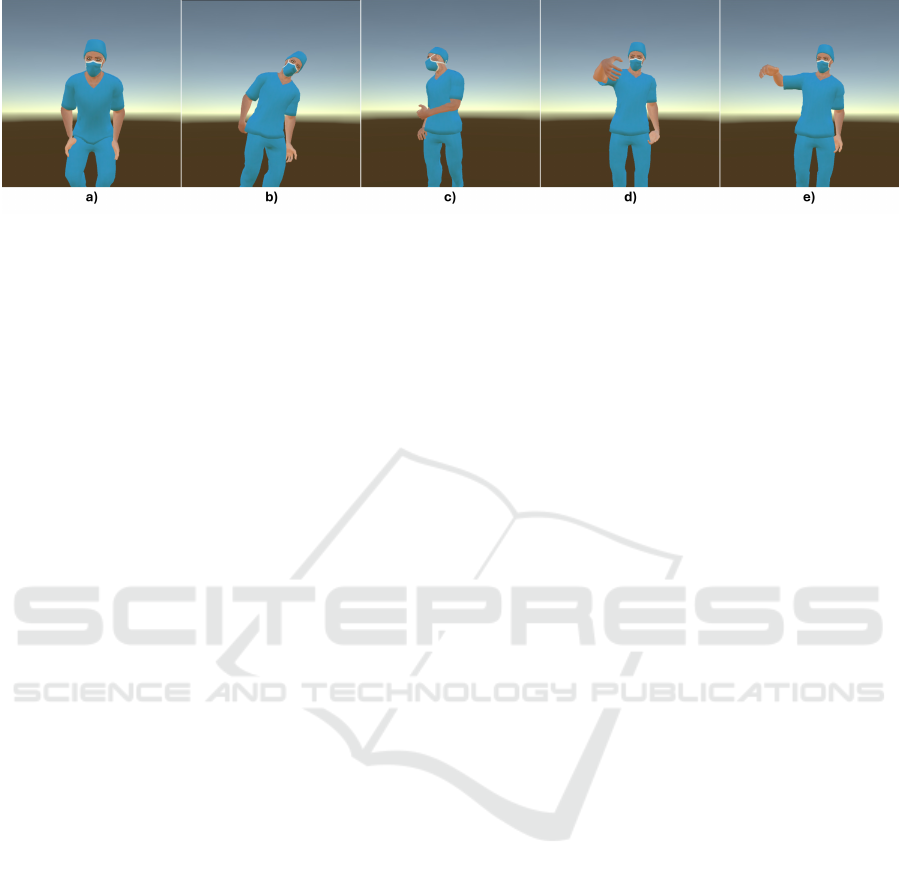
Figure 4: Set of postures tracked by the system: a) Forward trunk flexion; b) Lateral trunk inclination; c) Trunk rotation; d)
Arm extension; e) Shoulder abduction.
their posture in a simulation setting. For exam-
ple, if the trainee strays away from an optimal er-
gonomic position, immediate visual and auditory
signals notify them to correct their stance. Over
time, this instant feedback could reinforce healthy
posture habits. It adds to the real-time monitoring
of surgeries, just like they experience at the simu-
lation center.
• Personalized Learning through Analytics. Data
processing functions of the system keep detailed
records of every candidate’s performance through
posture tracking during practice sessions. Analyz-
ing these data allows the instructors to perceive re-
curring faults, customize their interventions, and
present individually tailored comments to their
trainees through custom-made reports. Trainees
can self-navigate individual learning paths that
encourage continuous improvement in posture
management. Tools like heatmaps—which high-
light areas where a candidate frequently deviates
from proper posture—offer clear visual feedback
that should allow trainees to find and correct their
common mistakes.
• Gamification to Engage in Ergonomics Learn-
ing. Serious games tailored for ergonomic-
focused learning could enhance learning with the
posterior monitoring system. These can simu-
late game-like procedures where trainees perform
simulated surgeries while maintaining an accu-
rate posture with points or levels gained due to
their compliance with ergonomic guidelines. This
gamification approach increases motivation and
engagement, making learning enjoyable and ef-
fective. Challenge scenarios such as maintaining
posture during complex maneuvers or under time
pressure can closely mimic the demands of actual
surgery. Such gaming can replicate the physical
and cognitive stressors imposing conflicts on the
novice in the operating room, giving an all-around
training opportunity. Examples include holding
a posture during critical interventions or working
with multiple tools. Other benefits are real-time
leaderboards that allow friendly competition and
encourage continuous practice.
• Promoting Long-Term Ergonomic Awareness.
Integrating ergonomic education into surgical
training is important to prevent long-term health
problems. Integrating a posture monitoring sys-
tem into residency training highlights the impor-
tance of proper ergonomics from the beginning
of a surgeon’s career. Early exposure to these
concepts helps protect physical well-being in the
long run, which, in turn, has a positive effect on
surgical performance. Using theoretical lessons
and practical simulations supported by monitoring
tools like the one proposed, surgical trainees may
better understand ergonomics in practice. Work-
shops and training modules should integrate theo-
retical content with practical tutorial sessions us-
ing the monitoring system, laying the foundation
for fostering an ergonomic culture within surgical
teams.
• Research Opportunities in Educational Set-
tings. Future investigations should concentrate
on how such a monitoring system impacts sur-
gical training in parametric and clinical envi-
ronments. Researchers could consider establish-
ing measurements of musculoskeletal complaints,
RULA scoring improvement, and surgical perfor-
mance metrics. Moreover, this study could as-
sess how automated alerts about posture influ-
enced participant and instructor stress and fo-
cus in a simulated surgical environment. Feed-
back from participants and instructors’ quantita-
tive data related to ICT usage would supplement
other measurement methods to give a more holis-
tic view of usability and educational benefits. Ul-
timately, these studies will contribute to the ex-
panding body of literature supporting the integra-
tion of advanced posture monitoring technologies
into medical education. This, in turn, will en-
able future research to demonstrate clear benefits
ERSeGEL 2025 - Workshop on Extended Reality and Serious Games for Education and Learning
926

for both health and learning outcomes, reinforc-
ing the role of ergonomic training as a standard
component of surgical education.
6 CONCLUSION AND FUTURE
WORK
Minimally invasive pediatric surgery presents signifi-
cant ergonomic challenges that may increase the risk
of MSDs among surgeons. This study introduced a
real-time posture monitoring system that leverages
depth sensors and 3D skeletal tracking to provide
immediate feedback on postural deviations, with the
goal of enhancing both surgeon well-being and pro-
cedural efficiency. The system ensures privacy pro-
tection and offers seamless, unobtrusive integration
into the operating room without disrupting workflow.
While the system shows promise, further validation
in routine surgical environments is necessary. Critical
aspects to assess include its stability in tracking the
surgeon despite occlusions from medical staff, accu-
racy under varying lighting conditions, and the poten-
tial for false alarms that could interfere with concen-
tration. Beyond surgical practice, this study also ex-
plored the integration of posture monitoring into sur-
gical education and training. Real-time feedback, per-
sonalized learning pathways, and gamification strate-
gies could enhance trainee engagement and encour-
age the early adoption of proper ergonomic habits.
Future research will focus on experimental valida-
tion and evaluating the system’s applicability across
different surgical specialties. Additionally, long-term
studies will examine the impact of integrating posture
monitoring technology into educational programs, as-
sessing its effects on ergonomic awareness, trainee
evaluation, and improvements in occupational health
outcomes.
REFERENCES
Alleblas, C. C., De Man, A. M., Van Den Haak, L., Vier-
hout, M. E., Jansen, F. W., and Nieboer, T. E. (2017).
Prevalence of musculoskeletal disorders among sur-
geons performing minimally invasive surgery: a sys-
tematic review. Annals of surgery, 266(6):905–920.
Antico, M., Balletti, N., Laudato, G., Lazich, A., Notaran-
tonio, M., Oliveto, R., Ricciardi, S., Scalabrino, S.,
and Simeone, J. (2021). Postural control assessment
via microsoft azure kinect dk: An evaluation study.
Computer Methods and Programs in Biomedicine,
209:106324.
Anwary, A. R., Cetinkaya, D., Vassallo, M., Bouchachia,
H., et al. (2021). Smart-cover: A real time sitting
posture monitoring system. Sensors and Actuators A:
Physical, 317:112451.
Ayvaz,
¨
O.,
¨
Ozyıldırım, B. A.,
˙
Is¸sever, H.,
¨
Oztan, G., Atak,
M., and
¨
Ozel, S. (2023). Ergonomic risk assessment
of working postures of nurses working in a medical
faculty hospital with reba and rula methods. Science
Progress, 106(4):00368504231216540.
Bertram, J., Kr
¨
uger, T., R
¨
ohling, H. M., Jelusic, A.,
Mansow-Model, S., Schniepp, R., Wuehr, M., and
Otte, K. (2023). Accuracy and repeatability of the mi-
crosoft azure kinect for clinical measurement of motor
function. PLoS One, 18(1):e0279697.
Bigdelou, A., Schwarz, L., and Navab, N. (2012). An adap-
tive solution for intra-operative gesture-based human-
machine interaction. In Proceedings of the 2012
ACM international conference on Intelligent User In-
terfaces, pages 75–84.
Chai, J. and Hodgins, J. K. (2007). Constraint-based mo-
tion optimization using a statistical dynamic model.
In ACM SIGGRAPH 2007 papers, pages 8–es. ACM.
Dabholkar, T., Dabholkar, Y. G., Yardi, S., and Sethi, J.
(2020). An objective ergonomic risk assessment of
surgeons in real time while performing endoscopic si-
nus surgery. Indian Journal of Otolaryngology and
Head & Neck Surgery, 72(3):342–349.
Flouty, E., Zisimopoulos, O., and Stoyanov, D. (2018).
Faceoff: Anonymizing videos in the operating rooms.
In Stoyanov, D., Taylor, Z., Sarikaya, D., McLeod,
J., Gonz
´
alez Ballester, M. A., Codella, N. C., Mar-
tel, A., Maier-Hein, L., Malpani, A., Zenati, M. A.,
De Ribaupierre, S., Xiongbiao, L., Collins, T., Re-
ichl, T., Drechsler, K., Erdt, M., Linguraru, M. G.,
Oyarzun Laura, C., Shekhar, R., Wesarg, S., Celebi,
M. E., Dana, K., and Halpern, A., editors, OR 2.0
Context-Aware Operating Theaters, Computer As-
sisted Robotic Endoscopy, Clinical Image-Based Pro-
cedures, and Skin Image Analysis, pages 30–38,
Cham. Springer International Publishing.
Gallo, L. (2013). A study on the degrees of freedom in
touchless interaction. In SIGGRAPH Asia 2013 Tech-
nical Briefs, pages 1–4. ACM.
Gallo, L., Placitelli, A. P., and Ciampi, M. (2011).
Controller-free exploration of medical image data:
experiencing the kinect. In 2011 24th Interna-
tional Symposium on Computer-Based Medical Sys-
tems (CBMS), page 1–6. IEEE.
Haidegger, T., Speidel, S., Stoyanov, D., and Satava,
R. M. (2022). Robot-assisted minimally invasive
surgery—surgical robotics in the data age. Proceed-
ings of the IEEE, 110(7):835–846.
Hu, H., Hachiuma, R., Saito, H., Takatsume, Y., and Ka-
jita, H. (2022). Multi-camera multi-person tracking
and re-identification in an operating room. Journal of
Imaging, 8(8):219.
Huang, W., Chen, J., Zhao, X., and Liu, Q. (2021). Per-
formance evaluation of azure kinect and kinect 2.0
and their applications in 3d key-points detection of
students in classroom environment. In International
Conference on Artificial Intelligence in Education
Technology, pages 177–193. Springer.
Jara, H. V., Orejuela, I. Z., and Baydal-Bertomeu, J. (2022).
Study of the ergonomic risk in operators of an assem-
Real-Time 3D Posture Tracking for Surgeons in Pediatric Minimally Invasive Surgery
927

bly line using the rula method in real working condi-
tions through the application of a commercial sensor.
Materials Today: Proceedings, 49:122–128.
Jiang, S., Liu, P., Fu, D., Xue, Y., Luo, W., and Wang,
M. (2017). A low-cost rapid upper limb assessment
method in manual assembly line based on somatosen-
sory interaction technology. In AIP Conference Pro-
ceedings, volume 1834. AIP Publishing.
Koskas, D. and Vignais, N. (2024). Physical ergonomic as-
sessment in cleaning hospital operating rooms based
on inertial measurement units. Bioengineering,
11(2):154.
Manghisi, V. M., Uva, A. E., Fiorentino, M., Bevilacqua, V.,
Trotta, G. F., and Monno, G. (2017). Real time rula as-
sessment using kinect v2 sensor. Applied ergonomics,
65:481–491.
Marinho, M. M., Harada, K., Deie, K., Ishimaru, T., and
Mitsuishi, M. (2021). Smartarm: Suturing feasibility
of a surgical robotic system on a neonatal chest model.
IEEE Transactions on Medical Robotics and Bionics,
3(1):253–256.
Marinho, M. M., Ishida, H., Harada, K., Deie, K., and Mit-
suishi, M. (2020). Virtual fixture assistance for sutur-
ing in robot-aided pediatric endoscopic surgery. IEEE
Robotics and Automation Letters, 5(2):524–531.
Matern, U. (2009). Ergonomic deficiencies in the operat-
ing room: examples from minimally invasive surgery.
Work, 33(2):165–168.
McAtamney, L. and Corlett, E. N. (1993). Rula: a sur-
vey method for the investigation of work-related upper
limb disorders. Applied ergonomics, 24(2):91–99.
Nadeem, M., Elbasi, E., Zreikat, A. I., and Sharsheer, M.
(2024). Sitting posture recognition systems: Compre-
hensive literature review and analysis. Applied Sci-
ences, 14(18):8557.
Pazouki, A., Sadati, L., Zarei, F., Golchini, E., Fruzesh,
R., and Bakhtiary, J. (2017). Ergonomic chal-
lenges encountered by laparoscopic surgeons, sur-
gical first assistants, and operating room nurses in-
volved in minimally invasive surgeries by using rula
method. Journal of Minimally Invasive Surgical Sci-
ences, 6(4):344–6.
Plantard, P., H. Shum, H. P., and Multon, F. (2017). Fil-
tered pose graph for efficient kinect pose reconstruc-
tion. Multimedia Tools and Applications, 76:4291–
4312.
Romeo, L., Marani, R., Perri, A. G., and D’Orazio, T.
(2022). Microsoft azure kinect calibration for three-
dimensional dense point clouds and reliable skeletons.
Sensors, 22(13):4986.
Rosenblatt, P. L., McKinney, J., and Adams, S. R. (2013).
Ergonomics in the operating room: protecting the
surgeon. Journal of minimally invasive gynecology,
20(6):744.
Schlussel, A. T. and Maykel, J. A. (2019). Ergonomics
and musculoskeletal health of the surgeon. Clinics in
colon and rectal surgery, 32(06):424–434.
Shum, H. P., Ho, E. S., Jiang, Y., and Takagi, S. (2013).
Real-time posture reconstruction for microsoft kinect.
IEEE transactions on cybernetics, 43(5):1357–1369.
Srivastav, V., Gangi, A., and Padoy, N. (2019). Human pose
estimation on privacy-preserving low-resolution depth
images. In International conference on medical image
computing and computer-assisted intervention, pages
583–591. Springer.
Stefana, E., Marciano, F., Rossi, D., Cocca, P., and Toma-
soni, G. (2021). Wearable devices for ergonomics: A
systematic literature review. Sensors, 21(3):777.
Van Det, M., Meijerink, W., Hoff, C., Van Veelen, M., and
Pierie, J. (2008). Ergonomic assessment of neck pos-
ture in the minimally invasive surgery suite during
laparoscopic cholecystectomy. Surgical endoscopy,
22:2421–2427.
Vermander, P., Mancisidor, A., Cabanes, I., and Perez, N.
(2024). Intelligent systems for sitting posture moni-
toring and anomaly detection: an overview. Journal
of NeuroEngineering and Rehabilitation, 21(1):28.
Walsh, C. M. (2023). Enhancing ergonomics in pediatric
endoscopy training and practice. Gastrointestinal En-
doscopy Clinics, 33(2):235–251.
Wang, S.-A., Lu, M.-H., Lee, A.-T., Chen, C.-Y., and
Lee, L.-W. (2024). Performance of microsoft azure
kinect dk as a tool for estimating human body segment
lengths. Scientific Reports, 14(1):15811.
Weitbrecht, M., Holzgreve, F., Fraeulin, L., Haenel, J.,
Betz, W., Erbe, C., Maurer-Grubinger, C., Wanke,
E. M., Brueggmann, D., Nienhaus, A., et al. (2023).
Ergonomic risk assessment of oral and maxillofa-
cial surgeons–rula applied to objective kinematic data.
Human Factors, 65(8):1655–1673.
Wong, S. W., Ang, Z. H., Yang, P. F., and Crowe, P. (2022).
Robotic colorectal surgery and ergonomics. Journal
of Robotic Surgery, pages 1–6.
Zhou, H., Hu, H., Harris, N. D., and Hammerton, J. (2006).
Applications of wearable inertial sensors in estimation
of upper limb movements. Biomedical Signal Pro-
cessing and Control, 1(1):22–32.
Zhou, L., Liu, Z., Leung, H., and Shum, H. P. (2014). Pos-
ture reconstruction using kinect with a probabilistic
model. In Proceedings of the 20th ACM Symposium
on Virtual Reality Software and Technology, pages
117–125.
ERSeGEL 2025 - Workshop on Extended Reality and Serious Games for Education and Learning
928
